Abstract
Vaccine administration is under way worldwide to combat the current COVID‐19 pandemic. The newly developed vaccines are highly effective with minimal adverse effects. Recently, the AstraZeneca ChadOx1 nCov‐19 vaccine has raised public alarm with concerns regarding the rare, but serious, development of thrombotic events, now known as vaccine‐induced immune thrombotic thrombocytopenia (VITT). These thrombotic events appear similar to heparin‐induced thrombocytopenia, both clinically and pathologically. In this manuscript, the ISTH SSC Subcommittee on Platelet Immunology outlines guidelines on how to recognize, diagnose and manage patients with VITT.
Keywords: AstraZeneca ChadOx1 nCov‐19 vaccine, COVID‐19, platelet activation, thrombocytopenia, thrombosis
1. INTRODUCTION
The COVID‐19 pandemic has resulted in significant morbidity and mortality worldwide.1., 2. Clinically, critically ill COVID‐19 patients develop coagulation abnormalities, leading to significant thrombosis and death.3., 4., 5., 6. Recent studies by Althaus et al. and Nazy et al. indicate that platelet activation by immunoglobulin G‐immune complexes can activate platelets in critically ill COVID‐19 patients via platelet FcγRIIa.7., 8.
COVID‐19 vaccination campaigns with several vaccine types are currently under way. Europe have described patients who developed thrombosis and thrombocytopenia 5 to 28 days after administration of AstraZeneca ChadOx1 nCov‐19 vaccine.9., 10. These include rare thrombotic events such as cerebral sinus vein and splanchnic vein thrombosis.9., 10. This rare syndrome is known as vaccine‐induced immune thrombotic thrombocytopenia (VITT).9., 10. Although data on VITT is limited, some clinical and laboratory features of VIIT have similarities to those observed in patients with severe COVID‐19 infection and in patients with autoimmune heparin‐induced thrombocytopenia (HIT). The SSC Platelet Immunology felt that a brief communication paper could help physicians and laboratory staff manage these cases.
2. POSSIBLE MECHANISMS
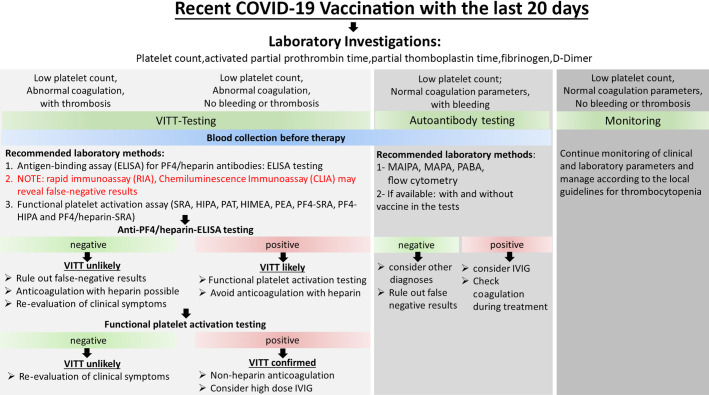
Preliminary data suggests that VITT after AstraZeneca vaccination has some clinical and serological similarities to HIT such as the presence of high‐titer anti‐PF4/heparin antibodies that cause platelet activation in functional assays. In addition, mRNA vaccines for COVID‐19 have been associated with severe thrombocytopenia and bleeding.11 Recent studies have implicated an antibody‐mediated platelet activation as the mechanism of the clotting events.9., 10. This requires immediate clinical recognition followed by confirmatory laboratory diagnosis, using specialized tests (Figure 1 ).
FIGURE 1.
Recommendations for laboratory diagnosis and patient management following bleeding and/or thrombosis after vaccination with the AstraZeneca Vaccine for COVID‐19
3. RECOMMENDATIONS FOR LABORATORY INVESTIGATION
Besides complete blood count, prothrombin time (PT), activated partial thromboplastin time (APTT), fibrinogen, and D‐dimer testing, the following actions should be considered:
-
1.
All samples for VITT testing should be collected into serum or plasma tubes based on the requirement of the testing facility, before the administration of any treatment, especially intravenous immunoglobulin (IVIG) and danaparoid. In addition, these samples should be conserved for future testing and to be used for improvingtesting and validation of these newly developed assays.
-
2.
A negative rapid immunoassay against PF4 such as particle centrifugation assay and chemiluminescence immunoassay may reveal false‐negative results. Once again, samples for VITT testing should be conserved until modified test methods are validated.
-
3.The clinical picture should guide management and laboratory investigation:
-
a.Thrombocytopenia, bleeding, and normal coagulation parameters (normal PT, APTT, PT, fibrinogen, and D‐dimer levels) may indicate an immunization‐associated immune thrombocytopenia (ITP), and depending on bleeding risk, strong consideration is recommended for high dose IVIG without anticoagulation.
- a.
-
b.Thrombocytopenia and thrombosis: this may indicate a HIT‐like syndrome (VITT), and management should be initiated with non‐heparin anticoagulation upon suspicion, PF4‐ELISA and SRA confirmation as per HIT syndrome. Testing should follow the algorithm below (where available): if VITT testing is positive and diagnosis is confirmed, continue nonheparin anticoagulation with consideration for high‐dose IVIG.
-
c.Thrombocytopenia without bleeding or thrombosis but abnormal coagulation parameters (at least one of: PT, APTT, fibrinogen, and D‐dimer, especially with dynamic change): this may indicate an early VITT syndrome and consideration should be given to initiate thromboprophylaxis with non‐heparin anticoagulation until the results of confirmatory testing are available.
-
d.Thrombocytopenia without bleeding or thrombosis and normal coagulation parameters: there is a potential for vaccine associated isolated thrombocytopenia. It is currently unclear whether these cases are induced by the vaccine such as drug‐induced thrombocytopenia or by primary ITP. Monitor and manage as per local guidelines for thrombocytopenia, based on bleeding risk.
-
a.
4. VITT TESTING ALGORITHM
Testing for VITT should begin with a binding assay (such as platelet factor 4 [PF4] ELISA) to identify the presence of anti‐PF4/polyanion antibodies (Figure 1).
-
1.
If the PF4 binding assay is negative, this patient does not have HIT or HIT‐like VITT.
-
2.
If the PF4 binding assay is positive (or not available), the sample should be tested in one or multiple HIT functional assays as available, such as the serotonin release assay (SRA),16 heparin‐induced platelet activation assay,17 platelet aggregation test,18 heparin‐induced multiple electrode aggregometry,19 PF4‐dependant P‐selectin expression assay,20 PF4‐SRA,21 and PF4/heparin‐SRA.22 A positive result strongly suggests this person has VITT in the appropriate clinical context.
5. CONCLUSION AND FUTURE ASPECTS
Although VITT is an extremely rare event in the context of COVID‐19‐specific vaccinations, it can be associated with severe morbidity and mortality. Data is emerging regarding details on the clinical presentation and mechanism(s) leading to the disease, including PF4/heparin associated antibodies and potentially other immune complexes related to platelet activation. To ensure these cases are recognized, diagnosed, and properly treated, the recommendations proposed here provide direction to allow clinicians and laboratories to perform initial testing currently known to aid in the diagnosis of VITT. It is important to mention that recommendations provided in this letter are made based on expert consensus based on limited data on the pathophysiology of VITT. It is almost certain that an update will be needed once more data is available. Thus, it is important that samples are conserved for future testing once the pathophysiology of VITT is fully understood and novel assays are developed.
Future directions will focus on correlating clinical presentations with laboratory findings including an international surveillance registry for all VITT due to the various COVID‐19 vaccines.
CONFLICT OF INTEREST
The authors declare no competing financial interests.
AUTHOR CONTRIBUTION
All the authors designed the study, wrote the manuscript, and revised the intellectual content of the manuscript. All authors approved the final version of the manuscript.
Footnotes
Manuscript handled by: Joost Meijers
Final decision: Joost Meijers, 12 April 2021
REFERENCES
- 1.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of coronavirus disease in China. N Engl J Med. 2019;2020(382):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helms J., Tacquard C., Severac F., et al. High risk of thrombosis in patients with severe SARS‐CoV‐2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klok F.A., Kruip M., van der Meer N.J.M., et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID‐19: an updated analysis. Thromb Res. 2020;191:148–150. doi: 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nahum J., Morichau‐Beauchant T., Daviaud F., et al. Venous thrombosis among critically Ill patients with coronavirus disease 2019 (COVID‐19) JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.10478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Llitjos J.F., Leclerc M., Chochois C., et al. High incidence of venous thromboembolic events in anticoagulated severe COVID‐19 patients. J Thromb Haemost. 2020;18:1743–1746. doi: 10.1111/jth.14869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nazy I., Jevtic S.D., Moore J.C., et al. Platelet‐activating immune complexes identified in critically ill COVID‐19 patients suspected of heparin‐induced thrombocytopenia. J Thromb Haemost. 2021 doi: 10.1111/jth.15283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Althaus K., Marini I., Zlamal J., et al. Antibody‐induced procoagulant platelets in severe COVID‐19 infection. Blood. 2021;137:1061–1071. doi: 10.1182/blood.2020008762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greinacher A., Thiele T., Warkentin T.E., Weisser K., Kyrle P.A., Eichinger S. Thrombotic thrombocytopenia after ChAdOx1 nCov‐19 vaccination. N Engl J Med. 2021 doi: 10.1056/NEJMoa2104840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schultz N.H., Sorvoll I.H., Michelsen A.E., et al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV‐19 vaccination. N Engl J Med. 2021 doi: 10.1056/NEJMoa2104882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee E.J., Cines D.B., Gernsheimer T., et al. Thrombocytopenia following Pfizer and Moderna SARS‐CoV‐2 vaccination. Am J Hematol. 2021;96(5):534–537. doi: 10.1002/ajh.26132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kiefel V., Santoso S., Weisheit M., Mueller‐Eckhardt C. Monoclonal antibody–specific immobilization of platelet antigens (MAIPA): a new tool for the identification of platelet‐reactive antibodies. Blood. 1987;70:1722–1726. [PubMed] [Google Scholar]
- 13.McMillan R., Tani P., Millard F., Berchtold P., Renshaw L., Woods V.L., Jr Platelet‐associated and plasma anti‐glycoprotein autoantibodies in chronic ITP. Blood. 1987;70:1040–1045. [PubMed] [Google Scholar]
- 14.Metzner K., Bauer J., Ponzi H., Ujcich A., Curtis B.R. Detection and identification of platelet antibodies using a sensitive multiplex assay system‐platelet antibody bead array. Transfusion. 2017;57:1724–1733. doi: 10.1111/trf.14122. [DOI] [PubMed] [Google Scholar]
- 15.Rosenfeld C.S., Nichols G., Bodensteiner D.C. Flow cytometric measurement of antiplatelet antibodies. Am J Clin Pathol. 1987;87:518–522. doi: 10.1093/ajcp/87.4.518. [DOI] [PubMed] [Google Scholar]
- 16.Sheridan D., Carter C., Kelton J.G. A diagnostic test for heparin‐induced thrombocytopenia. Blood. 1986;67:27–30. [PubMed] [Google Scholar]
- 17.Greinacher A., Michels I., Kiefel V., Mueller‐Eckhardt C. A rapid and sensitive test for diagnosing heparin‐associated thrombocytopenia. Thromb Haemost. 1991;66:734–736. [PubMed] [Google Scholar]
- 18.Fratantoni J.C., Pollet R., Gralnick H.R. Heparin‐induced thrombocytopenia: confirmation of diagnosis with in vitro methods. Blood. 1975;45:395–401. [PubMed] [Google Scholar]
- 19.Galea V., Khaterchi A., Robert F., Gerotziafas G., Hatmi M., Elalamy I. Heparin‐induced multiple electrode aggregometry is a promising and useful functional tool for heparin‐induced thrombocytopenia diagnosis: confirmation in a prospective study. Platelets. 2013;24:441–447. doi: 10.3109/09537104.2012.724736. [DOI] [PubMed] [Google Scholar]
- 20.Padmanabhan A., Jones C.G., Curtis B.R., et al. A novel PF4‐dependent platelet activation assay identifies patients likely to have heparin‐induced thrombocytopenia/thrombosis. Chest. 2016;150:506–515. doi: 10.1016/j.chest.2016.02.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nazi I., Arnold D.M., Warkentin T.E., Smith J.W., Staibano P., Kelton J.G. Distinguishing between anti‐platelet factor 4/heparin antibodies that can and cannot cause heparin‐induced thrombocytopenia. J Thromb Haemost. 2015;13:1900–1907. doi: 10.1111/jth.13066. [DOI] [PubMed] [Google Scholar]
- 22.Vayne C., Guery E.A., Kizlik‐Masson C., et al. Beneficial effect of exogenous platelet factor 4 for detecting pathogenic heparin‐induced thrombocytopenia antibodies. Br J Haematol. 2017;179:811–819. doi: 10.1111/bjh.14955. [DOI] [PubMed] [Google Scholar]