Abstract
Background
Fangcang Hospitals (cabin hospitals) played a key role in isolation and control of the infection sources during COVID‐19 epidemic. Many patients at Fangcang Hospitals had complications or mental stress. As the doctors, nurses and paramedics presented in the emergency, there was a growing demand for clinical pharmacists to provide pharmaceutical care for the affected patients with chronic diseases via telemedicine.
Objective
This study was a retrospective study to evaluate the usefulness of clinical prevention and control measures of clinical pharmacists at Jianghan Fangcang Hospital. Besides, this study proposed innovative strategies for developing pharmacy services to ensure the medication compliance, accuracy and cure rates under the epidemic.
Methods
A total of 374 patients filled in the questionnaires and 349 patients were enrolled in this study. Patients who refused to receive pharmaceutical care were not included in this study. The pharmaceutical care included medication education via broadcast station, medication reconciliation, optimisation of drug use, monitor of adverse drug events and psychological comfort via WeChat one‐to‐one service. The data were collected from patients’ interviews and the questionnaires of inpatients and discharged patients.
Results
In Jianghan Fangcang Hospital, many patients had complications with hypertension (12.9%), hyperlipidaemia (9.2%), thyroid disease (8.9%), diabetes (7.2%), heart disease (3.4%), nephropathy (1.7%), cancer (1.1%) and other diseases (12.6%). After 35 days’ pharmacy service, about 200 different questions had been solved by our clinical pharmacists, including drug usage (65.38%), medication reconciliation (55.13%), drug precautions (23.1%), adverse drug reactions (35.9%) and psychological counselling (32.05%). Most patients were satisfied with clinical pharmacist service (66.7% great, 18.0% good).
Conclusion
The results of the retrospective study indicated that clinical pharmacist can effectively reduce and prevent drug‐related, life‐related and COVID‐19‐related problems for COVID‐19 patients, which is important for the disease recovery. This study also demonstrated that clinical pharmacist played a key role for patients’ healthcare during the pandemic.
What’s known
Thanks for your kind reminding. We have answered this question herein and submission form, read as “The roles and functions of Fangcang hospital had been reported for the isolation and control of the infection sources during COVID‐19 epidemic. Meanwhile the development, characteristics of Fancang hospital had also been reported. A few papers also gave some advice on the pharmacy service during the coronavirus pandemic, including how to address drug shortages, how to adjust pharmacist workflow, deliver multimedia educational materials and so on”.
What’s new
Thanks for your kind reminding. We have answered this question herein and on the submission form, read as “Due to the high demand of medication consultation for patients, and the non‐contact circumstance of Fangcang hospitals, we created a novel work mode for remote pharmaceutical care for 349 patients. This study concluded our work experiences in detail, and also evaluated the role and usefulness of clinical pharmacists at Jianghan Fangcang Hospital. To our knowledge, this kind of study had never been reported”.
1. INTRODUCTION
In December, 2019, Wuhan city, the capital of Hubei province in China, became the centre of an outbreak of COVID‐19 of unknown cause. 1 Since then, COVID‐19 has spread quickly across China and all over the world. 2 On March 11, the World Health Organisation (WHO) has declared the coronavirus a global pandemic. 3 As of June 24, 2020, SARS‐CoV‐2 has caused 9,239,536 infections and 472,755 deaths worldwide, causing a great threat to global health. 4 The spectrum of COVID‐19 ranges from mild to severe and even death. 5 , 6 , 7 Up to now, more than 80% of the confirmed cases of COVID‐19 are mild or common illness. 8 , 9 , 10 Currently there are no specific antiviral treatment for COVID‐19. 8 , 9 , 10
Since the SARS‐CoV‐2 is highly infectious, in order to control the spread of the epidemic, Fangcang Hospitals were quickly established for the treatment of patients with mild and moderate COVID‐19, which solved the problem of insufficient beds in a short period of time. 11 Until Feb.24th, 2020, there have been 16 Fangcang Hospitals established for more than 12,000 patients with mild and common COVID‐19 in China. Over 1 month, most patients were cured and discharged, and only a few patients were transferred to designated hospitals for further treatment because of exacerbations. 12 As a new major public health facility, Fangcang Hospital had large space, multiple beds and possessed multiple functions, including emergency treatment, clinical examination and centralised management. 11 , 12 As a requisite functional module of the Fangcang Hospital, the Fangcang pharmacy also played an important role in ensuring the supply and safety of therapeutic drugs for the COVID‐19 patients 13 .
As the largest Fangcang Hospital, Jianghan Fangcang Hospital was the first one to open up for mild/moderate COVID‐19 patients with 1500 beds. The medical staff is in short supply as the ratio of doctors: nurses: patients was 1:2:60. Because of the lack of specific drugs for COVID‐19 and the fear of the epidemic, most patients took therapeutic drugs without indication. Meanwhile, the large number and complicated sources of patients with mental stress and comorbidities make the treatment more complicated and difficult. There were also many special patients, such as child, pregnant and senile ones resulting in a great difficulty of treatment assignment.
The standard treatment for patients in the Fangcang Hospitals included, as necessary, antiviral agents, Traditional Chinese Medicines, immunomodulator, glucocorticoid, intestinal microecological modulators and other medicines for chronic diseases. Under this circumstance, there are many drug‐related problems such as off‐label use of drugs, improper drug selection, drug interactions, improper dosage and adverse drug reactions etc Therefore, it is important for clinical pharmacists to provide pharmaceutical service for patients to improve medication compliance, accuracy and cure rates.
To support medical care for patients in Jianghan Fangcang Hospital, clinical pharmacists provided telehealth pharmacy services through electronic information systems supported by cloud platforms including radio station, WeChat APP (WeChat APP is the largest social software in China, and the number of monthly active accounts has reached to 1.165 billion) or other media education. This retrospective study was performed to assess the benefit of pharmaceutical care for patients in Jianghan Fangcang Hospital. Data were collected from medical records, patient questionnaire and WeChat online service records. After 35 days’ pharmaceutical care, clinical pharmacist help 349 patients solved about 196 different questions concluded in this paper. Most patients were satisfied with clinical pharmacist service (66.7% great, 18.0% good).
2. METHODS
2.1. Patients
A retrospective study was performed on the patients who were diagnosed with COVID‐19 and received pharmaceutical care services at the Jianghan Fangcang Hospital, from February 5th, 2020 to March 10th, 2020. A total of 374 patients filled in the questionnaires and 349 patients were enrolled in this study. Patients who refused to receive pharmaceutical care were not included in this study.
2.2. Pharmacists’ daily activity
Pharmacists played key roles in drug supplies and clinical pharmaceutical care for patients in Fangcang Hospital. Early on in the outbreak of the pandemic, the numbers and types of drugs could not meet the demands of most patients. The pharmacists adjusted the inventory in time according to the clinical demands after online communication with patients. Then pharmacists delivered the drugs to Fangcang Hospital twice a day according to the refreshed drug inventory. After finishing the drug supply, pharmacists provided clinical pharmaceutical care for patients including drug efficacy, drug interactions, adverse drug reactions etc at least once a day. Besides, pharmacists also joined the online Multidisciplinary Treatment (MDT) to provide pharmaceutical service when necessary. At night, pharmacists discussed and solved the patients’ drug‐related problems in the clinical pharmacist team through WeChat. The careful pharmacy service helped patients with the rational drug use and drug consultation.
2.3. Online pharmaceutical care service
Clinical pharmacist team explored the online pharmaceutical care service mode according to the special conditions of the Fangcang Hospitals including telehealth counselling, multimedia health education and no‐contact services mainly through WeChat, so as to ensure one‐on‐one communication with the patients and solve their medication problems timely and effectively. Our pharmaceutical care plan including:
A series of "Rational Drug Use" science broadcasting programs were opened to introduce the common medical knowledge to patients, including medical instructions, drug usage, drug interactions and adverse drug reactions etc The programs cover various aspects of treatment, including antiviral agents, antibiotics Traditional Chinese Medicines, nutritious diet, postdischarge management, emotional regulation etc
The WeChat ID of "clinical pharmacist in the Fangcang hospital" was established and actively publicised, so that patients in need of help could voluntarily contact clinical pharmacists, and fill in the online "self‐reported questionnaire ". Thus, the basic information about initial symptoms of COVID‐19, basic comorbidities and their medication could be obtained by online consultation.
Pharmacists were assigned to patients according to patients’ disease conditions from the inpatients’ questionnaire. For example, patients with hypertension or cardiovascular disease were assigned to cardiovascular pharmacists, patients with diabetes were assigned to endocrine pharmacists, patients with nephropathy were assigned to chronic kidney disease pharmacist, patients with multiple symptoms of COVID‐19 were assigned to respiratory clinical pharmacist etc The clinical pharmacists provided 24‐h online pharmaceutical care in case patients had drug‐related problems or negative emotions, and recorded every consultation.
COVID‐19 patients were required to acquire the first pharmaceutical care and follow‐up visit within 24 hours of the next day, ensuring that all patients could timely obtain service.
Patients received follow‐up visit after discharge to monitor their physical condition.
2.4. The inpatients’ questionnaire survey items
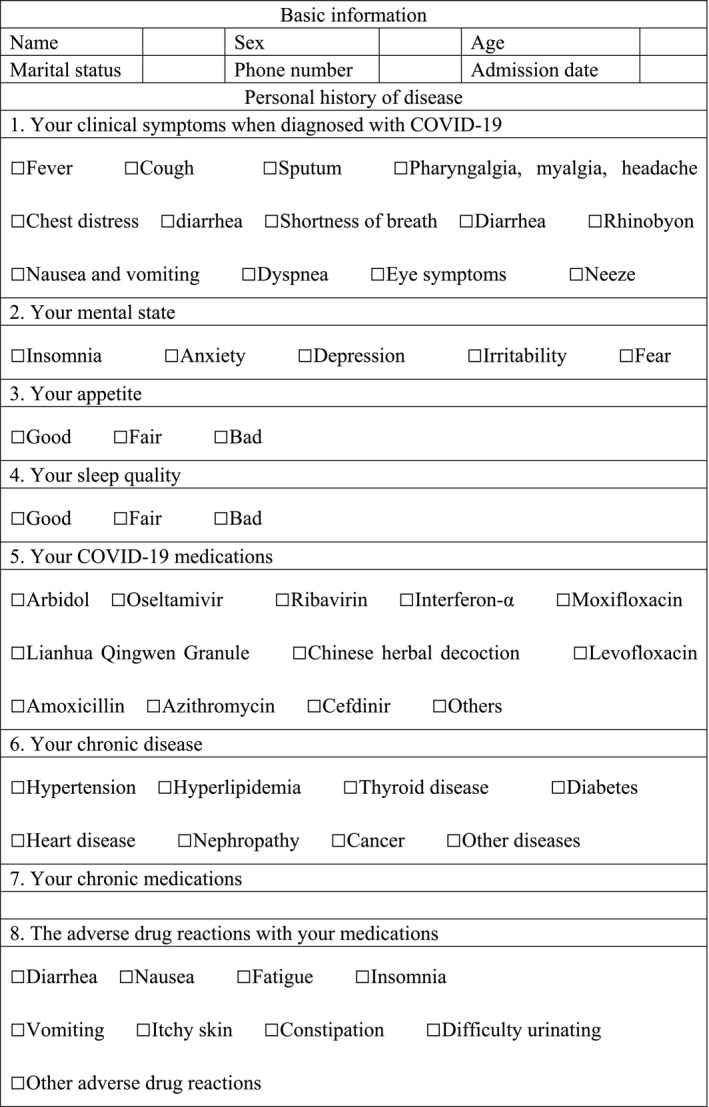
Each item was independently created by the clinical pharmacists taking into consideration of usual pharmaceutical care. The survey included patient basic information, initial symptoms of COVID‐19, patient's mental state, comorbidities, the medications including antivirals, antibiotics and other drugs, adverse drug reactions etc as shown in Table 1. The questionnaire was administered to the patients before they received clinical pharmacist online service. Patients refused to service were excluded from this study.
TABLE 1.
Self‐reported questionnaire of inpatients at Jianghan Fangcang Hospital
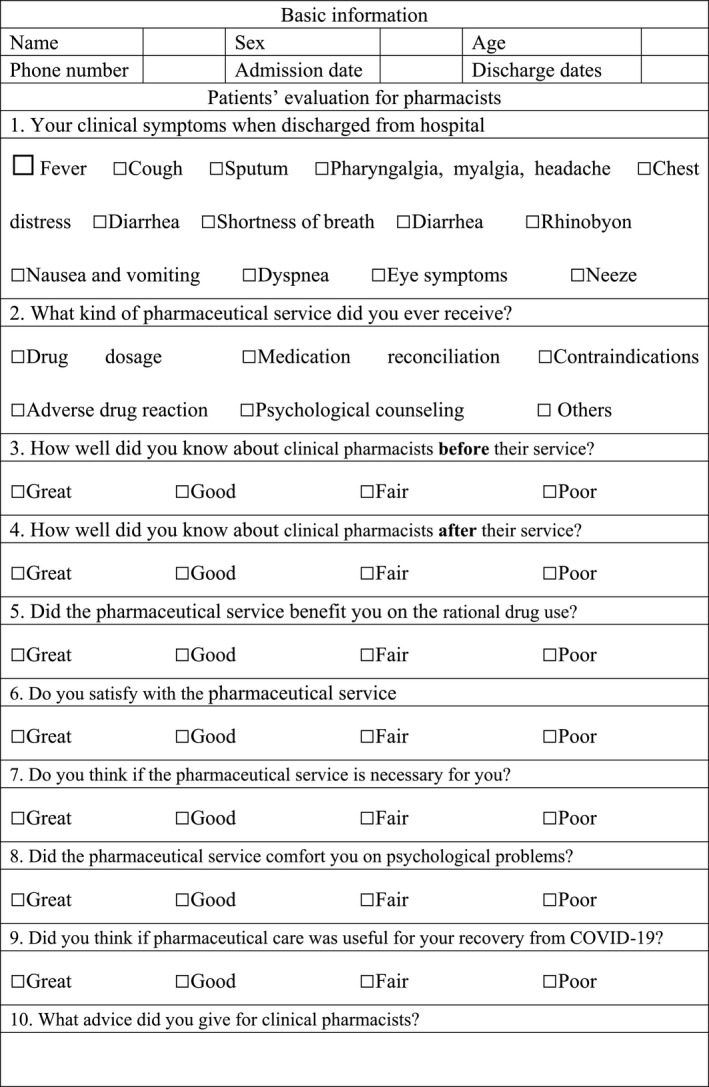
2.5. Usefulness of the online pharmaceutical care service
Between February 5th and March 10th 2020, the discharged patients’ questionnaire was administered to 78 patients who received pharmaceutical care service at the Jianghan Fangcang Hospital as shown in Table 2. The survey included the days for antiviral and antibiotic therapy, the usefulness of pharmacist care service on patients’ rational medication and mental state, the satisfaction with clinical pharmacist service. Patients who did not receive pharmacist service or unwilling to fill in the questionnaire were excluded.
TABLE 2.
The discharge patients’ questionnaire at Jianghan Fangcang Hospital
3. RESULTS
3.1. Demographic
A total of 1848 patients were hospitalised in Jianghan Fangcang Hospital and 349 patients accepted the pharmaceutical care through WeChat voluntarily. The patients were enrolled in this study with an average age of 45.5 ± 10.6 years and 57.6% were women. All these patients were diagnosed with mild COVID‐19, who had fever (79.7%), cough (60.5%) with 43.6% sputum, pain with pharyngalgia, myalgia, headache (57.3%), shortness of breath (42.7%), chest distress (38.4%), diarrhoea (35.8%), nausea and vomiting (24.9%), dyspnoea (24.4%), eye symptoms (18.3%), sneeze (17.2%), rhinobyon (14.0%). Besides, many patients had chronic diseases such as hypertension (12.9%), hyperlipidaemia (9.2%), thyroid disease (8.9%), diabetes (7.2%), heart disease (3.4%), nephropathy (1.7%), cancer (1.1%) and other diseases (12.6%). Details of patient's characteristics are summarised in Table 3. Thus, it was of great significance for clinical pharmacist to provide medication reconciliation and other pharmaceutical care for the patients in Fangcang Hospital to improve medication compliance, accuracy and cure rates.
TABLE 3.
Demographics and clinical characteristics of patients
| Characteristics | No. (%) of patients (n = 349) |
|---|---|
| Gender | |
| Women | 201 (57.6%) |
| Men | 148 (42.4%) |
| Age (y) | 45.5 ± 10.6 |
| Clinical symptoms with COVID‐19 | |
| Fever (temperature ≥37.3°C) | 278 (79.7%) |
| Cough | 211 (60.5%) |
| Pharyngalgia, Myalgia, headache | 200 (57.3%) |
| Shortness of breath | 149 (42.7%) |
| Chest distress | 134 (38.4%) |
| Diarrhoea | 125 (35.8%) |
| Nausea and vomiting | 87 (24.9%) |
| Dyspnoea | 85 (24.4%) |
| Eye symptoms | 64 (18.3%) |
| Sneeze | 60 (17.2%) |
| Rhinobyon | 49 (14.0%) |
| Comorbidity | |
| Hypertension | 45 (12.9%) |
| Hyperlipidaemia | 32 (9.2%) |
| Thyroid disease | 31 (8.9%) |
| Diabetes | 25 (7.2%) |
| Heart disease | 12 (3.4%) |
| Nephropathy | 6 (1.7%) |
| Cancer | 4 (1.1%) |
| Others | 44 (12.6%) |
| None | 214 (61.3%) |
3.2. Medications and adverse drug reactions
Patients at Fangcang Hospital were treated with various antivirals, antibiotic, Traditional Chinese Medicine and other symptomatic treatment drugs as shown in Table 4. The antivirals taken by patients included Arbidol (70.8%), Oseltamivir (82.5%), Chinese patent medicine of Lianhua Qingwen Granule (92.8%), Chinese herbal decoction (64.8%), Ribavirin (4.9%), Interferon‐α (1.7%). With the weakened immune system, some COVID‐19 patients were companied with pulmonary bacterial infections, thus antibiotics were taken. The antibiotics include moxifloxacin (73.1%), cefdinir (36.7%), levofloxacin (32.1%), amoxicillin (6.3%), and azithromycin (3.2%). Drug abuse was common at the beginning of admission, partly because of the unclear infection disease and anxiety mentality of patients. The chronic medications in Fangcang Hospital included hypotensive drugs (12.9%, 45/349), hypoglycaemic drugs (7.2%, 25/349), antilipemic (9.2%, 32/349), thyroid drugs (8.9%, 31/349), anti‐cancer drugs (1.1%, 4/349), drugs for heart diseases (3.4%, 12/349) etc as shown in Table 4. Pharmacists should pay close attention to drug reconciliation and optimisation for these patients.
TABLE 4.
Medications for COVID‐19 patients
| Drug names | No. (%) of patients (n = 349) |
|---|---|
| Lianhua Qingwen Granule | 324 (92.8%) |
| Oseltamivir | 288 (82.5%) |
| Arbidol | 247 (70.8%) |
| Ribavirin | 17 (4.9%) |
| Interferon | 6 (1.7%) |
| Moxifloxacin | 255 (73.1%) |
| Cefdinir | 128 (36.7%) |
| Levofloxacin | 112 (31.1%) |
| Amoxicillin | 22 (6.3%) |
| Chinese medicine | 226 (64.8%) |
| Couh medicine | 31 (8.29%) |
| Ibuprofen | 48 (12.83%) |
| Hypotensive drugs | 45 (12.9%) |
| Hypoglycaemic agents | 25 (7.2%) |
| Antilipemic | 32 (9.2%) |
| Thyoid drugs | 31 (8.9%) |
| Anti‐cancer drugs | 4 (1.1%) |
| Drugs for heart diseases | 12 (3.4%) |
Because of the lack of antiviral drugs for COVID‐19, many patients took more than one antivirals or antibiotics with the same function overtime, which not only failed to achieve the therapeutic curative efficacy, but also caused a variety of adverse drug reactions. Besides, the drugs for patients’ comorbidities may have interactions with antivirals or antibiotics, which may lead to great risks for COVID‐19 patients. The ingredients of Traditional Chinese Medicine are complicated which may have antagonistic effect or synergistic effect with western medicine. 14 Many studies have reported that some herbs could influence the activity of specific metabolising enzymes such as cytochrome P450 enzymes or transporters such as ABCB1, ATP‐binding cassette, subfamily B member 1, which indeed affect western drug metabolism and deposition and cause various adverse drug reaction. 14 Therefore, drug‐related problems need to be paid great attention for clinical pharmacist.
Many patients (61.9%) reported that they had adverse drug reactions, including diarrhoea (27.5%), nausea (27.2%), fatigue (24.4%), insomnia (16%), vomiting (11.7%), itchy skin (10.9%), constipation (5.2%), difficulty urinating (4.6%) and other adverse drug reactions (6.9%) as shown in Table 5. As some adverse drug reactions are similar to the symptoms of COVID‐19, clinical pharmacists needed to help patients to understand the concept of adverse drug reactions appropriately, and know how to distinguish minor side effects and severe drug reactions that needs medical intervention using the causality assessment tool of Naranjo Adverse Reaction Probability Scale (APS). 15 After the online patient interviews, we found that 38% nausea (46/74), 39% diarrhoea (44/73), most skin pruritus (>90%), moat vomiting (>90%), constipation (>90%) and dysuria (>90%) were adverse drug reactions and other reported reactions were caused by COVID‐19. Most adverse reaction was alleviated after drug discontinuation.
TABLE 5.
Reported adverse drug reaction by COVID‐19 patients
| Symptoms | No. (%) of patients (n = 349) |
|---|---|
| Nausea | 74 (21.2%) |
| Diarrhoea | 73 (20.9%) |
| Fatigue | 70 (20.1%) |
| Sleeplessness | 38 (10.9%) |
| Skin pruritus | 33 (9.5%) |
| Vomiting | 32 (9.2%) |
| Constipation | 13 (3.7%) |
| Dysuria | 13 (3.7%) |
| Others | 19 (5.4%) |
| None | 88 (25.2%) |
3.3. Clinical pharmacists’ medication interventions
In recent decades, clinical pharmacists have provided kinds of pharmaceutical care for patients with different diseases. 16 , 17 , 18 The remote pharmacy service such as telepharmacy has benefited numerous patients in settings where the pharmacists are not available. 19 , 20 The remote pharmaceutical care was provided for COVID‐19 patients to ensure the timely supply of preventive and treatment medications during the coronavirus pandemic. After 35 days’ pharmaceutical care, we sifted and got 196 different questions from patients which were classified into five aspects, including COVID‐19‐related problems (29.1%), COVID‐19 medication‐related problems (41.8%), chronic disease‐related problem (12.2%), life‐related problems (7.7%), matters of discharge (9.2%), as shown in Table 6. These contents had been compiled into a book which were used as guidelines for patients at other Fangcang Hospitals. In total, pharmacists provided 149 interventions in response to drug‐related problems. The most common interventions were drug selections (60.4%), including impropriate drug selection (8.1%), unclear indication for drug treatment (13.4%), duplication of therapeutic group (20.1%), untreated indication (18.8%). The second common interventions were dose selection (20.1%), including the impropriate dose (13.4%) or frequency (6.7%). Many patients took drugs over the course of medication (19.5%), partly because of the lack of specific drugs for COVID‐19 and the fear of this epidemic. Most of the proposed advice or explanations were accepted by patients after our pharmaceutical care.
TABLE 6.
Questions from COVID‐19 patients and pharmacists’ medication interventions
| Question classification | No. (%) of questions (n = 196) |
|---|---|
| COVID‐19‐related problems | 57 (29.1%) |
| Initial symptoms, disease progression, sequelae, relapse | 19 (9.7%) |
| Complications | 20 (10.2%) |
| Disease detection index | 18 (9.2%) |
| COVID‐19 medication‐related problems | 82 (41.8%) |
| Drug selection problems and drug precautions | 35 (17.9%) |
| Adverse drug reaction | 16 (8.2%) |
| Treatment of asymptomatic infections | 14 (7.1%) |
| Drug interaction problem | 11 (5.6%) |
| Basic chronic disease‐related problems | 24 (12.2%) |
| Diabetes‐related problems, such as medication reconciliation | 9 (4.6%) |
| Cardiovascular and cerebrovascular diseases related problems | 10 (5.1%) |
| Other chronic disease‐related problems | 5 (2.5%) |
| Life‐related problems | 15 (7.7%) |
| Diet‐ and nutrition‐related problems | 4 (2.0%) |
| Exercise at Fangcang hospital | 2 (1.0%) |
| Others | 9 (4.6%) |
| Matters of discharge | 18 (9.2%) |
| Discharge‐related problems | 11 (9.2%) |
| Medications out of hospital | 3 (1.5%) |
| Pharmacist interventions | No. (%) of interventions(n = 149) |
|---|---|
| Drug selection problem | 90 (60.4%) |
| Impropriate drug selection | 12 (8.1%) |
| Unclear indication for drug treatment | 20 (13.4%) |
| Duplication of therapeutic group or active ingredients | 30 (20.1%) |
| Untreated indication | 28 (18.8%) |
| Dose selection | 30 (20.1%) |
| Drug dose too high or too low | 20 (13.4%) |
| Drug regimen frequent or not frequent | 10 (6.7%) |
| Impropriate course of medication | 29 (19.5%) |
3.4. Psychological effects of the COVID‐19 outbreak
Patients are usually significantly stressed by the big public health emergencies such as SARS. 11 Because of the concern and fear of the COVID‐19 epidemic, many patients suffered from severe psychological burden. Before we initiated our pharmaceutical care, we had a preliminary understanding of the patient's psychological status. We found that 59.0% patients had insomnia, 42.3% patients were anxious and 28.2% patients were afraid of disease, 20.5% depressed and 10.3% irritable. We paid more attention to their psychological conditions when communicated with these patients. We also helped the patients to understand the COVID‐19 pandemic situation properly and encouraged them to combat with COVID‐19 from positive perspectives. Besides, we enhanced the visit frequency to the patients and recorded their emotional changes every day. After 35 days’ service, we found our service had positive effect on their mental stress (16.7% great, 43.6% good, 26.9% fair), as shown in Table 7.
TABLE 7.
Satisfaction of clinical pharmaceutical care for patients (n = 78)
| Survey items | Great No. (%) | Good No. (%) | Fair No. (%) | Poor No. (%) |
|---|---|---|---|---|
| The knowledgement of clinical pharmacists before servicePlease consider changing the word “knowledgement” here and subsequent occurrences. | 6.4% | 5.1% | 14.1% | 74.4% |
| The knowledgement of clinical pharmacists after service | 9.0% | 35.9% | 42.3% | 12.8% |
| Patients’ recognition | 46.2% | 42.3% | 7.7% | 3.9% |
| Patients’ benefit on rational drug use | 38.5% | 52.6% | 0 | 9.0% |
| Satisfaction with this service | 66.7% | 18.0% | 14.1% | 1.3% |
| Necessary of this service | 62.8% | 32.1% | 5.1% | 0 |
| Benefit on psychological help | 16.7% | 43.6% | 26.9% | 12.8% |
| Usefulness of pharmaceutical care for outcome of disease | 21.8% | 43.6% | 33.3% | 1.3% |
| Frequency of service | Once a day (48.7%) | Once per 2 days (20.5%) | Once per 3 days (7.7%) | Once a week (14.1%) |
|---|---|---|---|---|
| Pharmaceutical care services | Drug dosage (65.4%) | Medication reconciliation (55.1%) | Contraindications (23.1%) | |
| Adverse drug reaction (35.9%) | Psychological counselling (32.1%) | Others (21.8%) | ||
3.5. Satisfaction of pharmaceutical care service
In order to evaluate the pharmaceutical care provided by clinical pharmacists, we designed a questionnaire for discharged patients. Many patients joined the pharmaceutical service group on admission, but unwilling to participate in the group after they recovered from hospital, partly because they concerned about the leakage of personal information or the disgust with questionnaire research. Thus, only 78 patients voluntarily completed the questionnaire. According to the survey results, shown in Table 7, 48.7% patients communicated with the clinical pharmacist at least once a day, 28.2% patients communicate with the clinical pharmacist every 2‐3 days.
Through 35 days’ services, the recognition of clinical pharmacist was greatly improved, from 25.6% to 87.2%, as shown in Table 7. Most patients were satisfied with clinical pharmacist service (66.7% great, 18.0% good), and they thought pharmaceutical care provided by clinical pharmacist was necessary for treatment and rehabilitation at Fangcang Hospital (62.8% great, 32.1% good). Besides, most patients thought the service had positive effect on their mental stress (16.7% great, 43.6% good, 26.9% fair).
This study indicated that most patients need clinical pharmaceutical care services. The online pharmaceutical care service can not only help patients use drugs rationally, but also relieve the patient's negative emotions and anxiety during the COVID‐19 outbreak.
4. DISCUSSION
Clinical Pharmacists are the guardians of safety medication of the patient's all the time. Because of the unique circumstances of Fangcang Hospital, clinical pharmacists were recommended to preform no‐contact pharmaceutical care, which hindered the efficient and timely service for patients. The online pharmaceutical care service is often provided in places where clinical pharmacists unavailable. 19 , 20 A variety of technologies, models of care are used to develop and provide remote services, serving diversified populations with different pathological conditions. 20 However, the experiences on patients at Fangcang Hospitals are rare. Recently, implementation of pharmaceutical care for patients at Jianghan Fangcang Hospital has been established during the COVID‐19 outbreak. The goals of pharmaceutical care services were to improve medication safety and optimise clinical treatment outcomes and disease prognosis. This study was a retrospective research to analyse the clinical pharmacists’ roles at the Fangcang Hospital. This study showed that many patients had various initiate symptoms, and some had chronic diseases or mental stress, making the treatment complicated and difficult. The drugs were also complicated including different kinds of antivirals, antibiotics and other agents, which often confused patients with the drug selection, drug dose, drug interaction and adverse reactions. Obviously, reduction in medication errors includes drug interactions, adverse drug reactions following the suggestion of clinical pharmacists at Fangcang Hospital has been shown to have a positive impact on COVID‐19 patients. Patients in Fangcang Hospital usually took Lianhuaqingwen Capsule or Chinese Medicine Decoction for the treatment of COVID‐19. The interactions between Chinese Traditional Medicines and western medicines needed to be concerned by pharmacists. Lianhuaqingwen Capsule or Chinese Medicine Decoction contains ephedra herb which may cause different adverse drug interaction in combination with hypotensive drugs such as sartan drugs, α,β‐receptor blockers. Liquorice can also inhibit the activity of Cytochrome P450 enzymes which influence the drug metabolism such as diuretic Furosemide, glucocorticoid etc 21 .
Through continuous instruction of pharmacist inpatient service, patients’ concerns about medication can be alleviated. The clinical pharmacist helps patients solved almost 200 questions, which mainly focused on the drug‐related problems including drug usage (65.38%), medication reconciliation (55.13%), drug precautions (23.1%), adverse drug reactions (35.9%) and psychological counselling (32.05%). In total, pharmacists provided 160 interventions in response to drug‐related problems and most interventions were acceptable for patients, which played an important role for patients’ healthcare during the pandemic. Our study also revealed that, through continued guidance, many patients gained a better understanding of the drug indications, drug interaction and adverse reactions. Moreover, like previous studies reported on the introduction of clinical pharmacist services with a high satisfactory (>80%) and acceptance rate, most patients in Fangcang Hospital were satisfied with clinical pharmaceutical care and thought service was necessary and helpful during their COVID‐19 treatment. 8 , 9 , 10 Besides, the patients’ recognition of the pharmacist has greatly improved.
Because of the specificity of the COVID‐19 epidemic, most of the patients joined in the pharmaceutical service group at the beginning of treatment, but some of participants were disgusted with the research questionnaire, or unwilling to participate in the research after they recovered from hospitals or transferred to the designated hospital when they got worse. Some of this kind of patients usually had simple or little medication problems and did not continue the service. However, the related data (n = 78) we collected were from the patients we followed up closely and received pharmaceutical care for a long time, thus could somehow reflect the real quality and satisfaction with our pharmaceutical services. All these data indicated that our online mode of novel pharmaceutical care service for patients at Fangcang Hospital was safe, effective and acceptable to COVID‐19 patients. Some advices are also provided herein: (1) Online pharmaceutical care service mode should be established not only to COVID‐19 patients but also to the general population as necessary; (2) Taken on heavy responsibility of drug safety guardians, pharmaceutical servicer and drug supplier, the clinical pharmacists in preventing the spread of COVID‐19 should be strengthened.
5. CONCLUSION
We performed pharmaceutical care for patients with mild or moderate COVID‐19 at Jianghan Fangcang Hospital. A retrospective study was followed to evaluate the usefulness of Clinical pharmacists at Fangcang Hospitals, which indicate that clinical pharmacist can effectively reduce and prevent drug‐related, life‐related and COVID‐19‐related problems for COVID‐19 patients. This work may reduce the work pressure of first‐line medical staffs, provide possible work patterns for clinical pharmacist in other hospital and give more professional service for Fangcang Hospital patients.
ETHICS STATEMENT
This study protocol was approved by the Institutional Review Board of Union Hospital, Tongji Medical College of Huazhong University of Science and Technology (IRB Number: 104). This retrospective study was merely the routine service put in place and data were gathered from existing documents based on routine work. Personal information was protected in the aggregated data.
CONFLICT OF INTEREST
The authors have declared no conflict of interest.
ACKNOWLEDGEMENTS
The research reported in this publication was supported by National Key R&D Program of China 2017YFC0909900. Yu Zhang and Yong Han contributed to the concept and design of this article. Dongyuan Wang and Yihui Liu helped for the data analysis and wrote this manuscript. Fang Zeng and Fang Cheng helped for the data collection. Chen Shi helped for the revision of the article.
Wang D, Liu Y, Zeng F, et al. Evaluation of the role and usefulness of clinical pharmacists at the Fangcang Hospital during COVID‐19 outbreak. Int J Clin Pract. 2021;75:e14271. 10.1111/ijcp.14271
Dongyuan Wang and Yihui Liu contributed equally to this article.
Contributor Information
Yong Han, Email: whxhhanyong@163.com.
Yu Zhang, Email: whuh_zhangyu@126.com.
DATA AVAILABILITY STATEMENT
All data used during the study are available from the corresponding author by request.
REFERENCES
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China. Lancet. 2020;395:497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Palacios Cruz M, Santos E, Velázquez Cervantes MA, León Juárez M. COVID‐19, a worldwide public health emergency. Rev Clin Esp. 2020;S0014–S2565(20):30092‐30098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. WHO . Coronavirus Disease 2019 (COVID‐19) Situation Report‐52. https://www.who.int/docs/default‐source/coronaviruse/20200312‐sitrep‐52‐covid‐19.pdf?sfvrsn=e2bfc9c0_2. Accessed Mar 12, 2020.
- 4. Novel Coronavirus (COVID‐19) ‐ HealthMap. https://www.healthmap.org/covid‐19/
- 5. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liu K, Fang YY, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl). 2020;133(9):1025–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cao B, Wang Y, Wen D, et al. A trial of lopinavir‐ritonavir in adults hospitalized with severe Covid‐19. N Engl J Med. 2020;382(19):1787‐1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Li G, De Clercq E. Therapeutic options for the 2019 novel coronavirus (2019‐nCoV). Nat Rev Drug Discov. 2020;19(3):149‐150. [DOI] [PubMed] [Google Scholar]
- 10. Zhang J, Zhou L, Yang Y. Therapeutic and triage strategies for 2019 novel coronavirus disease in fever clinics. Lancet Respir Med. 2020;8(3):e11‐e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yang Y, Zhu Y, Lian J, et al. Discussion on pharmacy management and pharmaceutical care mode in square cabin hospital. Herald Med. 2020;1‐13. [Google Scholar]
- 13. Bhat S, Farraye FA, Moss A. Roles of clinical pharmacists in caring for patients with inflammatory bowel disease during COVID‐19. Gastroenterology. 2020;160(5):1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhang Y, Lyu C, Fong S, et al. Interactions between traditional Chinese medicine and western drugs in Taiwan: a population‐based study. Comput Methods Programs Biomed. 2015;122(3):462‐470. [DOI] [PubMed] [Google Scholar]
- 15. Liang R, Borgundvaag B, McIntyre M, et al. Evaluation of the reproducibility of the naranjo adverse drug reaction probability scale score in published case reports. Pharmacotherapy. 2014;34(11):1159‐1166. [DOI] [PubMed] [Google Scholar]
- 16. Miller G, Franklin BD, Jacklin A. Including pharmacists on consultant‐led ward rounds: a prospective non‐randomised controlled trial. Clin Med. 2011;11:312‐316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nielsen TR, Andersen SE, Rasmussen M, Honorè PH. Clinical pharmacist service in the acute ward. Int J Clin Pharm. 2013;35:1137‐1151. [DOI] [PubMed] [Google Scholar]
- 18. Lombardi N, Wei L, Ghaleb M, et al. Evaluation of the implementation of a clinical pharmacy service on an acute internal medicine ward in Italy. BMC Health Serv Res. 2018;18:259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Omboni S, Tenti M. Telepharmacy for the management of cardiovascular patients in the community. Trends Cardiovasc Med. 2019;29(2):109‐117. [DOI] [PubMed] [Google Scholar]
- 20. Niznik JD, He H, Kane‐Gill SL. Impact of clinical pharmacist services delivered via telemedicine in the outpatient or ambulatory care setting: a systematic review. Res Social Adm Pharm. 2018;14(8):707‐717. [DOI] [PubMed] [Google Scholar]
- 21. He W, Jing Wu J, Ning J, et al. Inhibition of human cytochrome P450 enzymes by licochalcone A, a naturally occurring constituent of licorice. Toxicol In Vitro. 2015;29(7):1569–1576. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used during the study are available from the corresponding author by request.


