Summary
Background
There is concern regarding how the COVID‐19 pandemic may impact the psychological and physical health of children, but to date, studies on mental health during the pandemic in children are limited. Furthermore, unprecedented lifestyle stressors associated with the pandemic may aggravate the childhood obesity epidemic, but the role of BMI on child activity levels and psychological outcomes during COVID‐19 is unknown.
Objectives
We investigated how emotional responses (positive/negative affect), physical activity (PA) and sedentary behaviours related to anxiety among U.S. children with healthy weight and overweight/obesity during the pandemic.
Methods
Sixty‐four typically developing children (63% girls, 53% healthy weight) aged 9 to 15 years completed two virtual visits during the height of ‘stay‐at‐home’ measures from April 22 to July 29, 2020. Children completed 24‐hours PA recalls, state portion of State‐Trait Anxiety Inventory for Children and the 10‐item Positive and Negative Affect Schedule for Children.
Results
Independent of child BMI status, child anxiety scores were over five standard deviations greater than normative values from paediatric populations prior to the pandemic. Higher positive affect and PA were each associated with reduced anxiety levels in children with overweight/obesity, whereas higher positive affect was associated with reduced anxiety in children with healthy weight. Greater leisure screen time was associated with higher negative affect irrespective of child BMI status.
Conclusions
These associations highlight the potential mental health benefits of maintaining positive affect, engaging in PA and limiting leisure screen time for children during the pandemic and suggest that these associations may be particularly relevant for children with overweight/obesity.
Keywords: affect, COVID‐19, leisure screen time, obesity, physical activity, state anxiety, U.S. children
Abbreviations
- BMI
body mass index
- COVID‐19
coronavirus disease 2019
- MET
metabolic equivalent
- MVPA
moderate‐to‐vigorous physical activity
- NHANES
National Health and Nutrition Examination Survey
- PANAS‐C
positive and negative affect schedule for children
- STAIC
state‐trait anxiety inventory for children
- VPA
vigorous physical activity
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) was declared a national public health emergency in the United States in March 2020. In order to prevent the spread of the virus, U.S. state and local governments implemented unprecedented ‘stay‐at‐home’ orders starting in mid‐March 2020, including closures of primary and secondary schools across the nation. 1 Consequently, children's access to social support resources and opportunities for physical activity may have been limited during home confinement.
In addition to the high COVID‐19 death toll, which surpassed 250 000 in the United States by the end of November 2020, 2 there is increasing concern regarding the potential collateral damage to physical and mental health, particularly among children, during the COVID‐19 pandemic. While little is known about the impact of the pandemic on the mental health of children, school‐aged children in China reported experiencing depressive symptoms during their nationwide lockdown, 3 and in the United States, the proportion of mental health‐related emergency department visits increased 24% for children aged 5 to 11 and 31% for children aged 12 to 17 years during the pandemic compared with 1 year earlier. 4 Furthermore, other recent studies in China, Italy and the United States have also shown that children are reporting less engagement in physical activity and increased sedentary behaviour and screen time during the pandemic. 5 , 6 , 7
Correspondingly, studies conducted prior to the pandemic demonstrated a clear link between psychological well‐being and lifestyle behaviours. Prior studies have shown that positive affect, defined as the tendency of an individual to experience positive emotions, such as enthusiasm and joy, 8 is negatively correlated with symptoms and diagnoses of anxiety and depression. 9 , 10 Multiple reports have established that physical activity is associated with reduced symptoms of anxiety among children. 11 , 12 Conversely, studies have shown that during childhood and adolescence, both sedentary time and screen time are associated with increased risk for depressive symptoms and negative affect, which refer to the tendency to experience more intense negative emotions. 13 , 14
Poor mental health outcomes have been identified as independent risk factors for several chronic conditions such as obesity, diabetes and cardiometabolic disease 15 , 16 ; additionally, low physical activity levels, heightened screen time and increased sedentary time are also associated with these chronic conditions. 17 , 18 Prior studies during the COVID‐19 pandemic have shown that adults with obesity may be particularly vulnerable to poor physical and mental health outcomes during the pandemic. 19 , 20 Specifically, adults with obesity have reported disproportionally sharper declines in mental health and higher incidences of weight gain compared to healthy weight individuals as a result of COVID‐19 ‘stay‐at‐home’ orders. 19 While Pietrobelli et al reported that children with obesity experienced unfavourable changes in health behaviours during a COVID‐19 lockdown period in Italy, 5 other studies that examined associations between child activity levels and/or psychological outcomes during the pandemic have failed to include assessments of child BMI. 3 , 6 , 7 , 21 , 22 Furthermore, and to the best of our knowledge, no study has investigated how children's mental health and lifestyle behaviours during the COVID‐19 pandemic may be related in both children with overweight/obesity and healthy weight. Given that health behaviour trajectories in childhood are likely to endure through adulthood (see review by Shrestha and Copenhaver 18 ), and the growing concerns that the unprecedented stressors associated with the COVID‐19 pandemic may aggravate the childhood obesity epidemic, 23 understanding how lifestyle behaviours and mental health are associated during the pandemic in both children with overweight/obesity and healthy weight is particularly important for paediatric public health.
While COVID‐19 restrictions may be associated with poor psychological and physical health outcomes in children, to our knowledge, no prior studies have examined how positive and negative affect, physical activity and sedentary behaviours are associated with anxiety levels among children with healthy weight and children with overweight/obesity. The aim of the current study was to examine associations between lifestyle behaviours, emotional regulatory states and anxiety during the COVID‐19 pandemic in children with overweight/obesity and healthy weight.
2. METHODS
2.1. Participants
Participants in this study were recruited from the existing BrainChild study, an observational study on neuroendocrine programming associated with gestational diabetes mellitus (GDM) exposure in utero, 24 that includes healthy, typically developing children who were recruited at ages 7 to 11 years during years 2014 to 2018 for entry into the study and followed with annual visits. The studies reported here were completed between 1 and 4 years after initial entry into the study. Children in the BrainChild cohort were born at a Kaiser Permanente Southern California (KPSC) Hospital and had no history of psychiatric, neurological or other significant medical disorders. Each mother's GDM status was determined from electronic medical records.
Due to the COVID‐19 pandemic, participants were unable to complete in‐person consents to participate in this sub‐study. Therefore, an amendment to the original Institutional Review Board (IRB) protocol was sent to the IRBs at the University of Southern California (#HS‐15‐00540) and KPSC (#10282) for virtual follow‐up visits. Both USC and KPSC IRBs approved this sub‐study if participants had a recent in‐person follow‐up visit that occurred within a year. During the prior in‐person follow‐up visit, participants' parents gave written informed consent, and children provided written informed assent to participate in longitudinal studies. Additionally, participants gave verbal informed consent prior to participating in the phone or video interviews. Of the 162 participants enrolled in the larger BrainChild Study, 82 participants had recent 1‐year follow‐up visits and, therefore, were eligible to participate in this ancillary study. During in‐person visits that had occurred within 1 year of the virtual visits, height (cm) to the nearest 0.1 cm was collected using a stadiometer and weight (kg) was collected using a calibrated digital scale. BMI was calculated using the standard formula, weight (kg) divided by height (m2). BMI z‐scores, BMI percentiles (age and sex‐specific standard deviation scores) and BMI status (healthy weight or overweight/obese) were determined based on Center for Disease Control (CDC) standards. 25 Children with BMI percentiles less than 85 were classified with healthy weight and children with BMI percentiles greater than or equal to 85 were classified with overweight/obesity.
2.2. Exposure
All of the children were residents of California, which was under a statewide ‘stay‐at‐home’ lockdown starting 19 March 2020. Data collection took place during Phase 1/Phase 2 of the order from 22 April to 29 July 2020, wherein all schools were closed for in‐person instruction from March 16 until further notice. 26 Phase 1 of the order consisted of mandatory ‘stay‐at‐home’ orders unless going to an essential job or to shop for essential needs, with all in‐person gatherings not allowed and outdoor public parks/spaces closed. 27 During phase 2, which started on 8 May 2020, schools remained closed until further notice, low risk businesses and some outdoor parks/spaces were allowed to reopen with restrictions, 28 but steadily were reclosed on 13 July 2020 due to rising COVID‐19 cases.
2.3. Phone visit
Trained staff members contacted participants' parents from the existing BrainChild cohort. The study included two phone or video call visits with both the participant and a parent present. Each visit occurred on average 34 days apart ranging from 27 to 73 days, interquartile range 30 to 35 days. The first visit occurred from 22 April to 26 June 2020. The second visit occurred from 22 May to 29 July 2020. All questionnaires were read aloud to each participant by the trained staff member, and then the participant gave their answers verbally.
2.4. Physical activity assessment
At each phone call visit, physical activity was assessed using a 24‐hour physical activity recall (PAR). 29 , 30 The 24‐hour PAR has previously been used in paediatric studies and validated with objective measures of physical activity using accelerometer devices. 30 , 31 A trained staff member asked participants, with a parent present to offer input, to recall all of their activities from 7:00 am to 12:00 am in 30‐minute blocks for the day prior. The activities were recorded and classified based on a 73‐item reference list. The participant was also asked to rate the intensity of each activity as either ‘Light’ (slow breathing, little/no movement), ‘Moderate’ (normal breathing and some movement), ‘Hard’ (increased breathing and moderate movement) or ‘Very Hard’ (hard breathing and quick movement). Each activity was then categorized as either sedentary, moderate‐to‐vigorous physical activity (MVPA) or vigorous physical activity (VPA), with their associated metabolic equivalent (MET) values obtained from the Compendium of Physical Activities. 29 Activities with MET values >1 and ≤1.5 were classified as sedentary, METs ≥3 as MVPA and METs ≥6 as VPA. Sleep blocks were classified as METs = 1.0. Examples of physical activity classifications include: walking (MVPA) or swimming laps (VPA). Examples of sedentary activities include reading a book, sitting in class and any sedentary screen time activities. In addition, leisure screen time (MET = 1.5 per 30‐minute block) was obtained by adding time spent in the following leisure activities: watching TV or movies, playing video games and surfing the internet while sedentary.
2.5. State‐trait anxiety inventory for children
At each phone call visit, state anxiety was assessed via the State‐Trait Anxiety Inventory for Children (STAIC). The STAIC has been previously validated to assess both state and trait anxiety in 1551 children aged 6 to 14 years, 32 and it additionally has high Cronbach α reliability coefficients for both state and trait anxiety between different testing settings. 33 Only items for the state‐anxiety (S‐Anxiety) scale were completed, given that the research question was concerned with how children were acutely responding to the pandemic, and by design, S‐Anxiety scores are influenced by the child's immediate environment. 32 The STAIC S‐Anxiety scale is composed of 20 statements, and children are instructed to base their answers on how they feel at that particular moment. Each STAIC S‐Anxiety item is a three‐point rating scale with a stem of ‘I feel’; half of the items are reflective of the presence of anxiety (ie, nervous, worried), while the other half are indicative of the absence of anxiety (ie, calm, pleasant). 32 Values of 1, 2 or 3 are assigned for each of the three answer choices, and scores range from 20 to 60, with higher scores representing higher state anxiety.
2.6. Positive and negative affect schedule for children
At each phone call visit, both positive and negative affect were assessed using the Positive and Negative Affect Schedule for Children (PANAS‐C). The current study utilized the shortened 10‐item PANAS‐C, which includes a five‐item positive affect scale (joyful, cheerful, happy, lively, proud) and a five‐item negative affect scale (miserable, mad, afraid, scared, sad), with a five‐point Likert scale ranging from 1 (‘very slightly or not at all’) to 5 (‘extremely’). 34 The shortened PANAS‐C has previously been validated in 779 typically developing children and has high Cronbach α coefficients for both positive and negative affect compared to the original 30‐item PANAS‐C. 34 The participants were instructed to answer each item reflecting to what extent they have felt this way during the past few weeks in order to capture a wider temporal range of affect during the pandemic. Scores range from 5 to 25 for each affect sub‐scale, with higher scores representing higher affect.
2.7. Statistical analysis
To minimize data reporting errors, measures taken from each of the two visits were averaged and used for all analyses. Using paired t‐tests, we found that there were no significant mean differences between the two visits except children tended to have less negative affect during Visit 2 (P = .03). Descriptive statistics including mean ± SD, median (IQR), ranges and frequencies were reported. In both overweight/obesity and healthy weight groups, correlations and linear regression models were used to test associations between emotional regulatory processes (positive affect and negative affect), physical activity (MVPA) and sedentary behaviours (leisure screen time, sedentary time) with state anxiety. Because the number of children who engaged in any VPA was relatively low in stratified analyses, further analyses with VPA were not conducted. Covariates included in each linear regression model were child age, sex, socioeconomic status (SES) and GDM exposure because these are factors known to influence mental health and physical activity levels. 24 , 35 , 36 , 37 SES was assessed using household income at birth, estimated based on census tract of residence and expressed as a continuous variable, and maternal education at birth, extracted from birth certificates in the electronic medical record as a categorical variable with the following categories: ‘high‐school or some high‐school’, ‘some college’ and ‘college and post‐education’. 38 Time spent in MVPA was not normally distributed, and a square‐root transformation was applied to normalize the distribution prior to regression analyses. P values <.05 were interpreted as statistically significant. SAS 9.4 statistical software (SAS Institute, Cary, North Carolina) was used for all data analyses.
3. RESULTS
Of the 82 participants from the BrainChild study who had completed at least one longitudinal follow‐up visit, 65 participants completed one phone‐call or video visits during the state mandated ‘stay‐at‐home’ order, and 64 of these participants completed a second phone‐call or video visit approximately 1 month later. Child age ranged from 9 to 15 years and 53% were of healthy weight while 16% had overweight and 31% had obesity as shown in Table 1, which include detailed demographic data.
TABLE 1.
Participant and maternal characteristics a
| Variable | Children with overweight/obesity (N = 30) | Children with healthy weight (N = 34) | P value b |
|---|---|---|---|
| Child age (years) | 11.7 (1.2) | 11.9 (1.2) | .51 |
| BMI percentile | 96.1 (3.5) | 49.1 (24.9) | <.001 |
| Sex |
Girls: 17 (57%) Boys: 13 (43%) |
Girls: 23 (68%) Boys: 11 (32%) |
.37 |
| GDM exposure |
Unexposed: 10 (33%) GDM‐exposed: 20 (67%) |
Unexposed: 17 (50%) GDM‐exposed: 17 (50%) |
.18 |
| Positive affect | 15.9 (3.7) | 16.4 (4.4) | .63 |
| Negative affect | 8.4 (2.6) | 8.1 (3.2) | .68 |
| State anxiety | 47.0 (3.1) | 47.7 (3.2) | .39 |
| Median MVPA | 45.0 (75.0) | 60.0 (60.0) | .65 |
| MVPA category |
MVPA > median: 13 (43%) MVPA ≤ median: 17 (57%) |
MVPA > median: 18 (53%) MVPA ≤ median: 16 (47%) |
.44 |
| Median VPA | 0 (15.0) | 0 (15.0) | .88 |
| VPA category |
VPA > 0:8 (27%) VPA = 0:22 (73%) |
VPA > 0:9 (26%) VPA = 0:25 (74%) |
.99 |
| Sedentary time (minutes) | 674.0 (116.2) | 681.2 (106.0) | .80 |
| Screen time (minutes) | 402.5 (181.5) | 353.8 (161.9) | .26 |
| Family income ($) | 65 474.8 (26 734.9) | 53 408.4 (21 627.6) | .05 |
| Maternal education |
High School: 2 (7%) Some College: 7 (23%) College and Above: 21 (70%) |
High School: 4 (12%) Some College: 12 (35%) College and Above: 18 (53%) |
.38 |
Data presented as N (%) or Mean (SD) or Median (25th quartile, 75th quartile).
From t‐test for means, Wilcoxon two‐sample test for medians, and Chi‐square test/Fisher's exact test for proportions, to test for group differences between children with overweight/obesity and children with healthy weight.
Compared to paediatric studies conducted prior to the pandemic that included healthy, typically developing children, 32 , 39 , 40 , 41 in our cohort, children with overweight/obesity had significantly lower positive affect and higher negative affect (Table S1), whereas children with healthy weight did not differ in mean positive affect or negative affect. Independent of BMI status, children reported significantly greater state anxiety compared to studies conducted prior to the pandemic (Table S1) such that state anxiety in our cohort was five standard deviations greater than mean state anxiety levels from healthy paediatric studies conducted prior to the pandemic.
The percentage of children in our cohort with overweight/obesity who met the World Health Organization MVPA guidelines 42 and the Physical Activity guidelines for Americans for MVPA 43 did not differ from the National Health and Nutrition Examination Survey (NHANES) dataset, whereas the percentage of children in our cohort with healthy weight who met the MVPA guidelines of 60 min/day was significantly lower (Table 2). Independent of BMI status, the percentage of children (6%) who met the American Academy of Paediatrics' guidelines for leisure screen time of less than 2 hours a day 44 was significantly lower compared to the NHANES dataset (54%; Table 2). Similarly, independent of BMI status, children engaged in significantly more sedentary minutes per day compared to the NHANES dataset. 45
TABLE 2.
Activity level comparisons to national health and nutrition examination survey
| In children with overweight/obesity | |||
|---|---|---|---|
| Variable (N, %) | BrainChild (N = 30) | NHANES (N = 246) 37 | P value * |
| Met guidelines for MVPA a | 13 (43%) | 141 (57%) | .17 |
| Met AAP screen time guidelines b | 1 (3%) | 109 (44%) | <.001 |
| Variable (Mean, SE) | BrainChild (N = 30) | NHANES (N = 412) 45 | P value * |
| Sedentary time (min/day) | 674.0 (116.2) | 463.3 (231.4) | <.001 |
| In children with healthy weight | |||
|---|---|---|---|
| Variable (N, %) | BrainChild (N = 34) | NHANES (N = 963) 37 | P value * |
| Met WHO/CDC guidelines for MVPA a | 18 (53%) | 703 (73%) | .02 |
| Met AAP screen time guidelines b | 3 (9%) | 534 (55%) | <.001 |
| Variable (Mean, SE) | BrainChild (N = 34) | NHANES (N = 766) 45 | P value * |
| Sedentary time (min/day) | 681.2 (106.0) | 442.2 (199.3) | <.001 |
World Health Organization Guidelines and Physical Activity Guidelines for Americans for moderate‐vigorous physical activity: at least 60 min/day of MVPA for children 42 , 43 .
American Academy of Pediatrics guidelines for leisure screen time: 2 h/day or less for children 44 .
Significance test used: Chi‐square test/Fisher's exact test for proportions or one sample t‐test for means, at significance level P < .05.
In children with overweight/obesity, in both unadjusted and models adjusted for child age, sex, SES and GDM exposure, state anxiety was significantly associated with positive affect and MVPA levels (Table 3; Figure 1). Before and after adjusting for covariates, negative affect, sedentary time and screen time were unrelated to state anxiety (Table 3). Negative affect was positively correlated with both sedentary and screen time (Table 4).
TABLE 3.
Summary of unadjusted and adjusted models with state anxiety as the outcome variable stratified by child BMI category
| Independent variables | Positive affect | Negative affect | MVPA | Sedentary time | Screen time |
|---|---|---|---|---|---|
| Model 1 | ß (95% CI) | ß (95% CI) | ß (95% CI) | ß (95% CI) | ß (95% CI) |
| Children with Overweight/obesity | −0.50 (−0.75, −0.25)* | 0.08 (−0.37, 0.52) | −0.41 (−0.65, −0.17)* | 0.003 (−0.007, 0.013) | 0.002 (−0.004, 0.008) |
| Children with healthy weight | −0.32 (−0.54, −0.10)* | −0.10 (−0.44, 0.25) | −0.11 (−0.50, 1.55) | 0.002 (−0.01, 0.01) | 0.002 (−0.004, 0.009) |
| Model 2 | ß (95% CI) | ß (95% CI) | ß (95% CI) | ß (95% CI) | ß (95% CI) |
| Children with overweight/obesity | −0.51 (−0.77, −0.25)* | 0.12 (−0.35, 0.59) | −0.45 (−0.74, −0.16)* | 0.008 (−0.004, 0.019) | 0.003 (−0.004, 0.01) |
| Children with healthy weight | −0.29 (−0.56, −0.01) | −0.11 (−0.52, 0.31) | −0.08 (−0.41, 0.25) | −0.003 (−0.014, 0.009) | 0.002 (−0.005, 0.009) |
| Model 3 | ß (95% CI) | ß (95% CI) | ß (95% CI) | ß (95% CI) | ß (95% CI) |
| Children with overweight/obesity | −0.53 (−0.78, −0.29)* | 0.12 (−0.35, 0.59) | −0.43 (−0.74, −0.12)* | 0.008 (−0.003, 0.02) | 0.004 (−0.003, 0.01) |
| Children with healthy weight | −0.25 (−0.51, 0.02) | −0.11 (−0.52, 0.31) | −0.14 (−0.45, 0.17) | 0.002 (−0.01, 0.01) | 0.006 (−0.001, 0.01) |
Note: Model 1: Unadjusted. Model 2: Adjusted for child age, sex and SES. Model 3: Adjusted for child age, sex, SES and GDM exposure.
Abbreviation: MVPA, square‐root transformed moderate‐to‐vigorous physical activity.
P‐values < .05.
FIGURE 1.
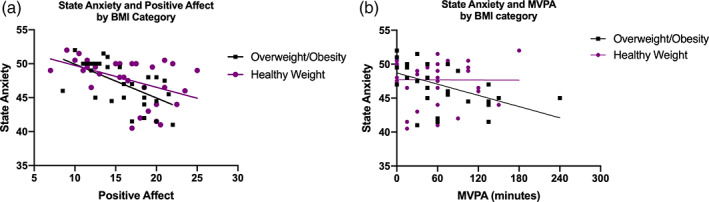
Scatterplots of, A, State Anxiety and Positive Affect stratified by BMI category, B, State Anxiety and Moderate‐to‐Vigorous Physical Activity stratified by BMI category. A, In children with overweight/obesity (Unadjusted Spearman Correlation Coefficient [r s ] = −0.60; P < .001); In children with healthy weight (r s = −0.47; P = .005). B, In children with overweight/obesity (r s = −0.60; P < .001); In children with healthy weight (r s = −0.07; P = .68). MVPA, moderate‐to‐vigorous physical activity average minutes per day
TABLE 4.
Adjusted Pearson R correlations between lifestyle behaviours, emotional regulatory states and state anxiety in children with overweight/obesity, N = 30
| State anxiety | Sedentary time | Leisure screen time | Positive affect | Negative affect | MVPA | |
|---|---|---|---|---|---|---|
| State anxiety | 1.00 | 0.29 | 0.20 | −0.63* | 0.12 | −0.52* |
| Sedentary time | 0.29 | 1.00 | 0.71* | −0.11 | 0.50* | −0.46* |
| Leisure screen time | 0.20 | 0.71* | 1.00 | 0.02 | 0.62* | −0.39 |
| Positive affect | −0.63* | −0.11 | 0.02 | 1.00 | −0.09 | 0.26 |
| Negative affect | 0.12 | 0.50* | 0.62* | −0.09 | 1.00 | −0.33 |
| MVPA | −0.52* | −0.46* | −0.39 | 0.26 | −0.33 | 1.00 |
Abbreviation: MVPA, moderate‐to‐vigorous physical activity. MVPA square‐root transformed.
Denotes P‐value <.05. Adjusted for child age, sex, SES and GDM exposure.
In children with healthy weight, positive affect was significantly associated with state anxiety (Table 3; Figure 1). This association became marginally associated after adjusting for child age, sex, SES and GDM exposure. Before and after adjusting for the same covariates, negative affect, MVPA levels, sedentary time and screen time were unrelated to state anxiety (Table 3). Between affect scores and PA levels, screen time was positively correlated with negative affect and negatively associated with positive affect (Table 5).
TABLE 5.
Adjusted Pearson R correlations between lifestyle behaviours, emotional regulatory states and state anxiety in children with healthy weight, N = 34
| State anxiety | Sedentary time | Leisure screen time | Positive affect | Negative affect | MVPA | |
|---|---|---|---|---|---|---|
| State anxiety | 1.00 | 0.06 | 0.28 | −0.32 | −0.14 | −0.17 |
| Sedentary time | 0.06 | 1.00 | 0.41* | −0.19 | 0.16 | −0.48* |
| Leisure screen time | 0.28 | 0.41* | 1.00 | −0.44* | 0.38* | −0.02 |
| Positive affect | −0.32 | −0.19 | −0.44* | 1.00 | −0.23 | 0.11 |
| Negative affect | −0.14 | 0.16 | 0.38* | −0.23 | 1.00 | −0.05 |
| MVPA | −0.17 | −0.48* | −0.02 | 0.11 | −0.05 | 1.00 |
Abbreviation: MVPA, moderate‐to‐vigorous physical activity. MVPA square‐root transformed.
Denotes P‐value <.05. Adjusted for child age, sex, SES and GDM exposure.
4. DISCUSSION
We provide the first results from the United States that examined how emotional regulatory responses, measured from positive and negative affect scores, related to anxiety levels and physical activity levels among children with both healthy weight and overweight/obesity during the pandemic. In California, the ‘stay‐at‐home’ orders began in late March 2020 and were partially lifted with restrictions at the end of May. During this time, we collected questionnaires on affect, state anxiety, physical activity and sedentary behaviours during the peak of the ‘stay‐at‐home’ order to infer the role of positive and negative affect and physical activity levels on anxiety levels in children with overweight/obesity and healthy weight. We found that state anxiety levels of children in our cohort during the ‘stay‐at‐home’ order were more than five standard deviations greater than the mean reported by other healthy paediatric populations prior to the pandemic independent of child BMI status. 32 , 39 , 40 Additionally, irrespective of BMI status, children reported greater screen and sedentary time than similarly aged children from the NHANES, 37 , 45 and the frequency of children who met the WHO guidelines for moderate to vigorous physical activity was lower than the NHANES dataset for children with healthy weight. Interestingly, positive affect and negative affect scores in our cohort were similar to those reported by other paediatric studies conducted prior to the pandemic in children with healthy weight only. 39 , 41 Children with overweight/obesity in our cohort reported lower positive affect and higher negative affect scores compared to prior paediatric studies. 39 , 41 Although previous studies have demonstrated that obesity is associated with reduced engagement in physical activity, increased time spent in sedentary activities and risk of poor mental health outcomes in children, 46 , 47 , 48 we found that children with overweight/obesity compared to children with healthy weight did not have differences in reported activity levels, affect or anxiety during the pandemic. However, given that we conducted this study during an unprecedented period of stress and state‐mandated school closures and home confinement, activity and anxiety level homogeneity between BMI groups during the pandemic may not be unexpected.
Prior studies in countries first struck by the pandemic noted an increase in reported symptoms of depression and anxiety in children. 3 , 21 , 22 However, none of these studies have investigated the relationships between affect and mental health during the pandemic. Our study showed that positive affect was significantly related to lower state anxiety levels in children with overweight/obesity, and we observed a similar trending relationship among healthy weight children, independent of age, sex, socioeconomic status and GDM‐exposure. These findings are in keeping with larger cross‐sectional studies in adolescents and young adults, suggesting that positive affect is associated with reduced anxiety during stressful times. 49 , 50 Therefore, promoting methods to maintain positive affect, such as educational interventions that encourage practicing gratitude 51 and mindfulness, 52 may be beneficial to children during times of heightened stress, such as the COVID‐19 pandemic. However, future studies are needed to test this possibility.
The impact of COVID‐19 restrictions on child mental health is sparse. 3 , 21 , 22 Similar to a study published in children during the COVID‐19 lockdown in China, 3 we found that children during the ‘stay‐at‐home’ order reported greater state anxiety compared to other paediatric samples prior to the pandemic. 32 , 39 , 40 Notably, Xie et al hypothesized that a reduction in outdoor activities and social interactions may have contributed to increased depression and anxiety symptoms. 3 Correspondingly, multiple randomized controlled trials have found that engaging in physical activity is beneficial for mental health. 53 , 54 , 55 Interestingly, we found that children with overweight/obesity, who reported more time spent in physical activity had less reported state anxiety during the pandemic, independent of age, sex, socioeconomic status and GDM‐exposure. Taken together, these findings suggest physical activity may be important for promoting the well‐being of children with overweight/obesity, particularly during stressful periods.
Similar to other studies in children during the ‘stay‐at‐home’ order, we found an increase in reported sedentary and leisure screen time compared to nationally representative paediatric samples before the ‘stay‐at‐home’ order. 5 , 6 , 7 , 37 Prior to the pandemic, the American Academy of Pediatrics recommended that children engage in less than 2 hours a day of leisure screen time. 37 However, children in our cohort reported an average of 6 hours a day of leisure screen time. Additionally, children reported spending 11 hours a day being sedentary and in leisure screen time. Importantly, prior studies in youth have shown that excessive screen and sedentary time are associated with increased depressive symptoms and negative affect. 13 , 14 Similarly, we found that increased sedentary and leisure screen time were associated with negative affect in children with overweight/obesity, and that leisure screen time was positively correlated with negative affect among children with healthy weight. While our study design does not allow us to determine the directionality of the relationship between leisure screen time and negative affect, our findings are in concert with previous large cross‐sectional studies demonstrating a dose‐dependent relationship between screen‐based activities and depressive symptomatology, such as negative affect in children. 14 , 56 Interestingly, some longitudinal studies suggest there is a bidirectional relationship between mental health and physical activity/sedentary time, with mental health predicting decreased physical activity engagement and increased sedentary time in the future, and baseline levels of physical activity/sedentary time predicting mental health outcomes at a later time point. 57 , 58 Future studies should consider investigating if limiting excessive leisure screen time could reduce the risk for negative affect among children.
Our study collected repeated measures of affect, anxiety and behavioral health questionnaires in children over 2 months during the peak of the ‘stay‐at‐home’ orders, but we did not have baseline measures of affect or anxiety in this cohort prior to the pandemic to compare to the measures collected during the pandemic. While we did compare affect, anxiety and activity levels in our cohort to other healthy paediatric populations prior to the pandemic, it is worth noting that the normative comparisons that we used for anxiety were either limited in sample size 39 , 40 or not recent. 32 However, to the best of our knowledge, there are no recent and large sample size normative STAIC state‐anxiety comparisons available in U.S. children and/or adolescents. Moreover, we assessed a limited number of behavioural factors that predicted levels of anxiety among children during COVID‐19 restrictions. Future pandemic‐related studies should consider assessing other potential environmental and psychosocial risk and protective factors for anxiety in children, such as sleep 59 and social support. 60 Children with healthy weight tended to be from families with lower income at birth when compared to children with overweight/obesity in our cohort, which may have influenced anxiety and MVPA levels and sedentary/screen time during the COVID‐19 pandemic. Additionally, we used a self‐reported physical activity recall, which is subject to participant bias. However, self‐report recalls provided pertinent information about specific physical activities engaged in during the ‘stay‐at‐home’ order. Finally, our small sample size may limit the generalizability of our findings.
5. CONCLUSIONS
Overall, independent of child BMI status, this study observed that during the height of the COVID‐19 ‘stay‐at‐home’ measures, children exhibited increased anxiety scores compared to normative values from paediatric populations prior to the pandemic. However, children who reported higher positive affect scores had lower levels of state anxiety, and children with overweight/obesity who reported more time spent in physical activity also reported lower anxiety scores. Additionally, children who reported greater leisure screen time had higher negative affect scores, irrespective of their BMI status. Collectively, our findings suggest that positive affect, physical activity levels and leisure screen time may be important for mental health outcomes during stressful periods.
CONFLICT OF INTEREST
The authors have nothing to disclose.
AUTHOR CONTRIBUTIONS
Jasmin M. Alves performed statistical analyses, drafted the initial manuscript and reviewed and revised the manuscript. Alexandra G. Yunker collected and organized data, drafted the initial manuscript and reviewed and revised the manuscript. Alexis DeFendis collected and organized data. Anny H. Xiang contributed to study concept and design, obtained funding and provided study supervision, performed statistical analyses, drafted the initial manuscript and reviewed and revised the manuscript. Kathleen A. Page contributed to study concept and design, obtained funding and provided study supervision, drafted the initial manuscript and reviewed and revised the manuscript. All authors critically reviewed the manuscript for important intellectual content, approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Supporting information
Appendix S1: Supporting Information
ACKNOWLEDGEMENTS
The authors would like to thank the families who participate in the BrainChild Study. The authors would also like to thank Ana Romero for managing the BrainChild study, Mayra Martinez and Janet Mora‐Marquez for recruiting volunteers and helping collect participant data. This work was supported by an American Diabetes Association Pathway Accelerator Award (#1‐14‐ACE‐36) (PI: Dr. Page) and in part by the National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) R01DK116858 (PIs: Drs. Page and Xiang) and the National Institute Of Mental Health of the National Institutes of Health under Award Number F31MH115640 (PI: Dr. Alves). A Research Electronic Data Capture, REDCap, database was used for this study, which is supported by the Southern California Clinical and Translational Science Institute (SC CTSI) through NIH UL1TR001855.
Alves JM, Yunker AG, DeFendis A, Xiang AH, Page KA. BMI status and associations between affect, physical activity and anxiety among U.S. children during COVID‐19. Pediatric Obesity. 2021;16:e12786. 10.1111/ijpo.12786
Jasmin M. Alves and Alexandra G. Yunker contributed equally as co‐first authors.
Kathleen A. Page and Anny H. Xiang contributed equally as co‐senior authors.
Funding information American Diabetes Association Pathway Accelerator Award, Grant/Award Number: #1‐14‐ACE‐36; National Institute of Diabetes and Digestive and Kidney Diseases, Grant/Award Number: R01DK116858; National Institute of Mental Health, Grant/Award Number: F31MH115640; Southern California Clinical and Translational Science Institute (SC CTSI), Grant/Award Number: NIH UL1TR001855
DATA AVAILABILITY STATEMENT
The datasets generated during and analysed during the current study are available from the corresponding author (K.A.P.) on reasonable request.
REFERENCES
- 1. UNESCO . Education: From disruption to recovery. UNESCO. 2020. https://en.unesco.org/covid19/educationresponse. Accessed June 12, 2020.
- 2. Mortality Analyses . Johns Hopkins coronavirus resource center. 2020. https://coronavirus.jhu.edu/data/mortality
- 3. Xie X, Xue Q, Zhou Y, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020;24:174‐900. 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leeb RT. Mental Health‐Related Emergency Department Visits Among Children Aged 18 Years During the COVID‐19 Pandemic—United States. MMWR Morb Mortal Wkly Rep. 2020;2020:69. 10.15585/mmwr.mm6945a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pietrobelli A, Pecoraro L, Ferruzzi A, et al. Effects of COVID‐19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity. 2020;28:1382–1385. 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dunton G, Do B, Wang S. Early effects of the COVID‐19 pandemic on physical activity and sedentary behavior in U.S. children. 2020. [DOI] [PMC free article] [PubMed]
- 7. Xiang M, Zhang Z, Kuwahara K. Impact of COVID‐19 pandemic on children and adolescents' lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020;63:531‐532. 10.1016/j.pcad.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gruber J, Moskowitz JT. Positive Emotion: Integrating the Light Sides and Dark Sides. Oxford, England: Oxford University Press; 2014. [Google Scholar]
- 9. Peterson JC, Charlson ME, Hoffman Z, et al. Randomized controlled trial of positive affect induction to promote physical activity after percutaneous coronary intervention. Arch Intern Med. 2012;172(4):329‐336. 10.1001/archinternmed.2011.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. J Abnorm Psychol. 1988;97(3):346‐353. 10.1037//0021-843x.97.3.346. [DOI] [PubMed] [Google Scholar]
- 11. Parfitt G, Pavey T, Rowlands AV. Children's physical activity and psychological health: the relevance of intensity. Acta Paediatr. 2009;98(6):1037‐1043. 10.1111/j.1651-2227.2009.01255.x. [DOI] [PubMed] [Google Scholar]
- 12. Kiluk BD, Weden S, Culotta VP. Sport participation and anxiety in children with ADHD. J Atten Disord. 2009;12(6):499‐506. 10.1177/1087054708320400. [DOI] [PubMed] [Google Scholar]
- 13. Sund AM, Larsson B, Wichstrøm L. Role of physical and sedentary activities in the development of depressive symptoms in early adolescence. Soc Psychiatry Psychiatr Epidemiol. 2011;46(5):431‐441. 10.1007/s00127-010-0208-0. [DOI] [PubMed] [Google Scholar]
- 14. García‐Hermoso A, Hormazábal‐Aguayo I, Fernández‐Vergara O, Olivares PR, Oriol‐Granado X. Physical activity, screen time and subjective well‐being among children. Int J Clin Health Psychol. 2020;20(2):126‐134. 10.1016/j.ijchp.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Golden SH, Lazo M, Carnethon M, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299(23):2751‐2759. 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rudisch B, Nemeroff CB. Epidemiology of comorbid coronary artery disease and depression. Biol Psychiatry. 2003;54(3):227‐240. 10.1016/S0006-3223(03)00587-0. [DOI] [PubMed] [Google Scholar]
- 17. Byun W, Dowda M, Pate RR. Associations between screen‐based sedentary behavior and cardiovascular disease risk factors in Korean youth. J Korean Med Sci. 2012;27(4):388‐394. 10.3346/jkms.2012.27.4.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shrestha R, Copenhaver M. Long‐term effects of childhood risk factors on cardiovascular health during adulthood. Clin Med Rev Vasc Health. 2015;7:1‐5. 10.4137/CMRVH.S29964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Flanagan EW, Beyl RA, Fearnbach SN, Altazan AD, Martin CK, Redman LM. The impact of COVID‐19 stay‐at‐home orders on health behaviors in adults. Obesity. 2020;29:438–445. 10.1002/oby.23066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Almandoz JP, Xie L, Schellinger JN, et al. Impact of COVID‐19 stay‐at‐home orders on weight‐related behaviours among patients with obesity. Clin Obes. 2020;10(5):e12386. 10.1111/cob.12386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yeasmin S, Banik R, Hossain S, et al. Impact of COVID‐19 pandemic on the mental health of children in Bangladesh: a cross‐sectional study. Child Youth Serv Rev. 2020;117:105277. 10.1016/j.childyouth.2020.105277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID‐19. J Affect Disord. 2020;275:112‐118. 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Storz MA. The COVID‐19 pandemic: an unprecedented tragedy in the Battle against childhood obesity. J Korean Pediatr Soc. 2020;63:477–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Alves JM, Yunker AG, DeFendis A, Xiang AH, Page KA. Prenatal exposure to gestational diabetes is associated with anxiety and physical inactivity in children during COVID‐19. Clin Obes. 2020;11:e12422. 10.1111/cob.12422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. About Child & Teen BMI | Healthy Weight | CDC. 2018.
- 26. Los Angeles County Office of Education . COVID‐19 School Closures. 2020. https://www.lacoe.edu/Home/News-Announcements/Coronavirus-School-Closures. Accessed January 25, 2021.
- 27. Governor Gavin Newsom Issues Stay at Home Order . California Governor. 2020. https://www.gov.ca.gov/2020/03/19/governor-gavin-newsom-issues-stay-at-home-order/. Accessed January 25, 2021.
- 28. California Governor Newsom Announces Certain Businesses May Begin Reopening . 2020. https://www.sullcrom.com/california-governor-newsom-certain-businesses-reopening-may-8-2020. Accessed January 25, 2021.
- 29. Ainsworth BE, Haskell WL, Herrmann SD, et al. Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575‐1581. 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 30. Trost SG, Marshall AL, Miller R, Hurley JT, Hunt JA. Validation of a 24‐h physical activity recall in indigenous and non‐indigenous Australian adolescents. J Sci Med Sport. 2007;10(6):428‐435. 10.1016/j.jsams.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 31. Anderson C, Hagströmer M, Yngve A. Validation of the PDPAR as an adolescent diary: effect of accelerometer cut points. Med Sci Sports Exerc. 2005;37(7):1224‐1230. 10.1249/01.mss.0000170073.57440.df. [DOI] [PubMed] [Google Scholar]
- 32. Spielberger CD, Edwards CDSTAIC. Preliminary Manual for the State‐Trait Anxiety Inventory for Children (“How I Feel Questionnaire”). Menlo Park, CA: Consulting Psychologists Press; 1973. [Google Scholar]
- 33. Papay JP, Spielberger CD. Assessment of anxiety and achievement in kindergarten and first‐ and second‐grade children. J Abnorm Child Psychol. 1986;14(2):279‐286. [DOI] [PubMed] [Google Scholar]
- 34. Ebesutani C, Regan J, Smith A, Reise S, Higa‐McMillan C, Chorpita BF. The 10‐item positive and negative affect schedule for children, child and parent shortened versions: application of item response theory for more efficient assessment. J Psychopathol Behav Assess. 2012;34(2):191‐203. 10.1007/s10862-011-9273-2. [DOI] [Google Scholar]
- 35. Nader PR, Bradley RH, Houts RM, McRitchie SL, O'Brien M. Moderate‐to‐vigorous physical activity from ages 9 to 15 years. JAMA. 2008;300(3):295‐305. 10.1001/jama.300.3.295. [DOI] [PubMed] [Google Scholar]
- 36. Zhu Y, Chen X, Zhao H, et al. Socioeconomic status disparities affect children's anxiety and stress‐sensitive cortisol awakening response through parental anxiety. Psychoneuroendocrinology. 2019;103:96‐103. 10.1016/j.psyneuen.2019.01.008. [DOI] [PubMed] [Google Scholar]
- 37. Fakhouri THI, Hughes JP, Brody DJ, Kit BK, Ogden CL. Physical activity and screen‐time viewing among elementary school–aged children in the United States from 2009 to 2010. JAMA Pediatr. 2013;167(3):223‐229. 10.1001/2013.jamapediatrics.122. [DOI] [PubMed] [Google Scholar]
- 38. Xiang AH, Wang X, Martinez MP, et al. Association of maternal diabetes with autism in offspring. JAMA. 2015;313(14):1425‐1434. 10.1001/jama.2015.2707. [DOI] [PubMed] [Google Scholar]
- 39. Zink J, Berrigan DA, Broadney MM, et al. The effects of interrupting sitting time on affect and state anxiety in children of healthy weight and overweight: a randomized crossover trial. Pediatr Exerc Sci. 2020;32(2):97‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mestre JM, Turanzas J, García‐Gómez M, et al. Do trait emotional intelligence and dispositional mindfulness have a complementary effect on the children's and adolescents' emotional states? Front Psychol. 2019;10:1496–1502. 10.3389/fpsyg.2019.02817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bauer CCC, Caballero C, Scherer E, et al. Mindfulness training reduces stress and amygdala reactivity to fearful faces in middle‐school children. Behav Neurosci. 2019;133(6):569‐585. 10.1037/bne0000337. [DOI] [PubMed] [Google Scholar]
- 42. Bull FC, Al‐Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451‐1462. 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. US Department of Health and Human Services . Physical activity guidelines for Americans. Vol 2018. 2nd ed. Washington, D.C: US Department of Health and Human Services. 2018;118. [Google Scholar]
- 44. Council on Communications and Media . Children, adolescents, obesity, and the media. Pediatrics. 2011;128(1):201‐208. 10.1542/peds.2011-1066. [DOI] [PubMed] [Google Scholar]
- 45. Carson V, Staiano AE, Katzmarzyk PT. Physical activity, screen time, and sitting among U.S adolescents. Pediatr Exerc Sci. 2015;27(1):151‐159. 10.1123/pes.2014-0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lindberg L, Hagman E, Danielsson P, Marcus C, Persson M. Anxiety and depression in children and adolescents with obesity: a nationwide study in Sweden. BMC Med. 2020;18(1):30. 10.1186/s12916-020-1498-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chung AE, Skinner AC, Steiner MJ, Perrin EM. Physical activity and BMI in a nationally representative sample of children and adolescents. Clin Pediatr (Phila). 2012;51(2):122‐129. 10.1177/0009922811417291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. O'Brien W, Issartel J, Belton S. Relationship between physical activity, screen time and weight status among young adolescents. Sports. 2018;6(3):57. 10.3390/sports6030057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. O'Hara RE, Armeli S, Boynton MH, Tennen H. Emotional stress‐reactivity and positive affect among college students: the role of depression history. Emot Wash DC. 2014;14(1):193‐202. 10.1037/a0034217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sewart AR, Zbozinek TD, Hammen C, Zinbarg RE, Mineka S, Craske MG. Positive affect as a buffer between chronic stress and symptom severity of emotional disorders. Clin Psychol Sci J Assoc Psychol Sci. 2019;7(5):914‐927. 10.1177/2167702619834576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Froh JJ, Bono G, Fan J, et al. Nice thinking! An educational intervention that teaches children to think gratefully. Sch Psychol Rev. 2014;43(2):132‐152. [Google Scholar]
- 52. Kang Y, Rahrig H, Eichel K, et al. Gender differences in response to a school‐based mindfulness training intervention for early adolescents. J Sch Psychol. 2018;68:163‐176. 10.1016/j.jsp.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Crews DJ, Lochbaum MR, Landers DM. Aerobic physical activity effects on psychological well‐being in low‐income hispanic children. Percept Mot Skills. 2004;98(1):319‐324. 10.2466/pms.98.1.319-324. [DOI] [PubMed] [Google Scholar]
- 54. Yook Y‐S, Kang S‐J, Park I. Effects of physical activity intervention combining a new sport and mindfulness yoga on psychological characteristics in adolescents. Int J Sport Exerc Psychol. 2017;15(2):109‐117. 10.1080/1612197X.2015.1069878. [DOI] [Google Scholar]
- 55. Azevedo LB, Burges Watson D, Haighton C, Adams J. The effect of dance mat exergaming systems on physical activity and health—related outcomes in secondary schools: results from a natural experiment. BMC Public Health. 2014;14(1):951. 10.1186/1471-2458-14-951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Yang F, Helgason AR, Sigfusdottir ID, Kristjansson AL. Electronic screen use and mental well‐being of 10–12‐year‐old children. Eur J Public Health. 2013;23(3):492‐498. 10.1093/eurpub/cks102. [DOI] [PubMed] [Google Scholar]
- 57. Sa V, C S, Ms A, Mj S, Ca M. Bidirectional associations between sport involvement and mental health in adolescence. Med Sci Sports Exerc. 2017;49(4):687‐694. 10.1249/mss.0000000000001142. [DOI] [PubMed] [Google Scholar]
- 58. Jerstad SJ, Boutelle KN, Ness KK, Stice E. Prospective reciprocal relations between physical activity and depression in female adolescents. J Consult Clin Psychol. 2010;78(2):268‐272. 10.1037/a0018793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Alfano CA, Ginsburg GS, Kingery JN. Sleep‐related problems among children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(2):224‐232. 10.1097/01.chi.0000242233.06011.8e. [DOI] [PubMed] [Google Scholar]
- 60. Sandler IN, Miller P, Short J, Wolchik SA. Social support as a protective factor for children in stress. Children's Social Networks and Social Supports. Hoboken, NJ: John Wiley & Sons; 1989:277‐307. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting Information
Data Availability Statement
The datasets generated during and analysed during the current study are available from the corresponding author (K.A.P.) on reasonable request.


