A 61‐year‐old woman with no background medical conditions was hospitalized with coronavirus disease 2019 (COVID‐19) at our hospital. She received remdesivir, interferon‐alpha, and systemic corticosteroid. She did not require intubation and mechanical ventilation, and was discharged after 2 weeks of hospitalization.
One week after discharge, she developed right hemifacial pain with no other sinonasal symptoms, including nasal congestion, rhinorrhea, or discharge. She then gradually developed right hemifacial numbness, decreased visual acuity, and chemosis, and was readmitted to our hospital. On examination, she was afebrile and was not in respiratory distress. There was a black eschar on the skin overlying the right lateral nasal wall, and malar and periorbital regions (Figure 1A). Ophthalmic examination revealed right‐sided proptosis, frozen eye, complete loss of vision, and fixed mydriasis. Polymerase chain reaction assay was positive for COVID‐19. Blood sugar levels were elevated without ketoacidosis.
FIGURE 1.
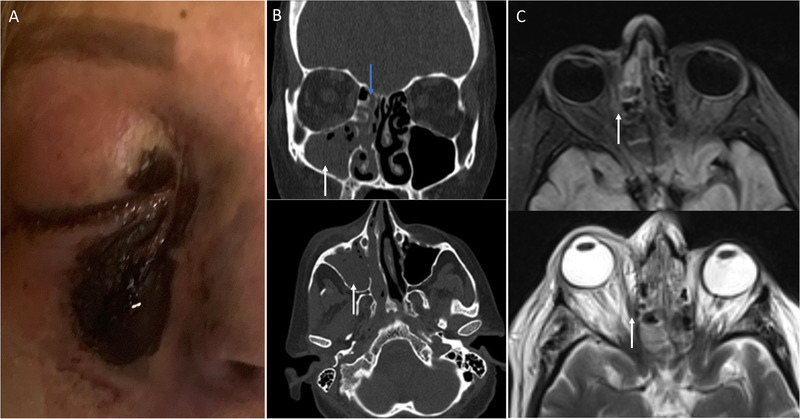
Rhino‐orbital mucormycosis in a patient with COVID‐19. (A) Black eschar over the right nasal wall, and malar and periorbital regions. (B) Complete opacification of the right maxillary sinus (white arrows) and anterior ethmoidal air cells (blue arrow) on noncontrast computed tomography. (C) Abnormal focal signal intensity in the right intraorbital fat (arrows) without abscess formation on magnetic resonance imaging of the orbits. COVID‐19, coronavirus disease 2019.
Noncontrast computed tomography of the paranasal sinuses revealed complete opacification of the right maxillary sinus and anterior ethmoidal air cells with internal foci of air that were representative of acute sinusitis (Figure 1B). Magnetic resonance imaging of the orbits in the T2‐weighted and fluid‐attenuated inversion recovery sequences showed abnormal focal signal intensity within the right intraorbital fat adjacent to the lamina papyracea without signs of abscess formation, which was suggestive of invasive fungal infection (Figure 1C).
The diagnostic sinonasal endoscopy revealed extensive necrosis of the mucosa of the right lateral nasal wall, inferior and middle turbinates, and septum. She was treated with insulin and systemic antifungals and underwent urgent extensive endonasal endoscopic debridement of necrotic tissue, and unfortunately right eye exenteration. Histopathology of the tissue specimens and sinonasal secretions confirmed mucormycosis.
Mucormycosis is an opportunistic infection caused by organisms in the order Mucorales. 1 These organisms are ubiquitous in nature but, as shown in this case, can cause devastating rhino‐orbito‐cerebral infection in susceptible patients. 2 The new‐onset glucocorticoid‐induced diabetes and immunosuppression by steroid may have predisposed this patient to invasive mucormycosis. There may have conceivably been a contribution by COVID‐19, which was present at the time of readmission, to susceptibility to mucormycosis. COVID‐19 induces endothelialitis and microvascular thrombosis in the pulmonary and extrapulmonary vascular beds, 3 which may compound the angioinvasive impact of mucormycosis that typically results in the infarction of the infected tissues. Additionally, COVID‐19 can cause immune dysregulation (e.g., by inducing lymphopenia). 4 Thus, combined with steroid‐induced immunosuppression, it may predispose to an opportunistic infection such as mucormycosis.
Clinicians should be familiar with the manifestations of this rare but devastating invasive mucormycosis for its prompt diagnosis in susceptible patients with COVID‐19 who receive systemic corticosteroids during the current pandemic.
CONFLICT OF INTEREST
None provided.
AUTHOR CONTRIBUTIONS
Mahboobeh Karimi‐Galougahi: concept, data collection, and interpretation, writing. Shima Arastou: concept, data collection, and interpretation, writing. Sara Haseli: concept, data collection, and interpretation, writing.
Karimi‐Galougahi M, Arastou S, Haseli S. Fulminant mucormycosis complicating coronavirus disease 2019 (COVID‐19). Int Forum Allergy Rhinol. 2021;11:1029–1030. 10.1002/alr.22785
View this article online at wileyonlinelibrary.com.
REFERENCES
- 1. Hibbett DS, Binder M, Bischoff JF, et al. A higher‐level phylogenetic classification of the Fungi. Mycol Res. 2007;111(5):509‐547. [DOI] [PubMed] [Google Scholar]
- 2. Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;1(5):634‐653. [DOI] [PubMed] [Google Scholar]
- 3. Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid‐19. N Engl J Med. 2020;383(2):120‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bermejo‐Martin JF, Almansa R, Menéndez R, Mendez R, Kelvin DJ, Torres A. Lymphopenic community acquired pneumonia as signature of severe COVID‐19 infection. J Infect. 2020;80(5):e23‐e24. [DOI] [PMC free article] [PubMed] [Google Scholar]


