Abstract
Understanding the determinants of risk perception for COVID‐19 might help to promote self‐preventive behaviours. This scoping review aimed to map the extent, variety and characteristics of the evidence on the possible determinants of risk perception for COVID‐like diseases. PubMed, Scopus and Web of Science were searched for original, peer‐reviewed English‐written articles published up to March 2020 and investigating risk perception determinants for respiratory infectious diseases in adults. Titles and abstracts were screened, and full texts were analysed by the first author; when unsure, eligibility was discussed with the last author. Data were collected according to an extraction sheet developed by the first and last authors. The cross‐sectional evidence covers a variety of diseases, countries and timings of testing. Mostly, questionnaires recorded socio‐demographics, media exposure, trust in institutions, disease proximity and knowledge; psychological variables, including personality traits, distress and self‐efficacy, were less investigated. A miscellaneous operationalization of risk perception emerged, including the likelihood of getting sick, perceived dangerousness, concerns or a combination of them. A comprehensive understanding of the substantial amount of evidence may be challenging due to methodological heterogeneity. Referring to uniform theoretical frameworks is recommended; also, longitudinal research may be implemented to probe causal relationships.
Keywords: containment measures, COVID‐19, respiratory infectious diseases, risk perception, risk perception determinants
INTRODUCTION
Optimal compliance with preventive measures is of crucial importance to the containment of COVID‐19; then, what drives people's behaviours in a similar scenario? Former studies on other coronavirus outbreaks, such as the severe acute respiratory syndrome (SARS), generally relied on the idea that people's actions are influenced by both likelihood and desirability of what they expect it may happen adopting (or not) certain behaviours (Leppin & Aro, 2009). Risk perception is usually defined as the estimate of the possibility that a specific harm can occur (Brug et al., 2009); however, our perception of risk is also influenced by the acknowledgement of the potential harmfulness of that event. Indeed, according to the protection motivation theory (Rogers, 1975, 1983) and the health belief model (Sheeran & Abraham, 1996) people's engagement in adaptive preventive actions is strictly related to the perceived threat, including the perceived likelihood of getting sick, namely one's personal susceptibility, and the perceived harmfulness for one's health, or disease severity. Nonetheless, risk perception has an affective dimension that refers to people's outbreak‐related emotions; feelings from mild concerns to intense fear are certainly expected during a pandemic, yet they might differently modulate the overall perceived risk and people's compliance with preventive actions (Leppin & Aro, 2009; Slovic et al., 2004). If people do not have a truthful perception of risk, they might not comply properly with the recommended measures, even when compulsory.
Intense exposure to disease‐related information through the media has been reported to influence the perception of risk for respiratory infectious diseases (Abbate et al., 2006; Barennes et al., 2010; Choi et al., 2017; Han et al., 2014; Oh et al., 2015), especially if trust in the information received is high (Fang et al., 2012; Kim & Kim, 2018; Yang & Cho, 2017). Furthermore, Wise et al. (2020) have recently reported that ‘health messages spread through government and the media can be effective in raising awareness of the risk’ for COVID‐19. Accordingly, risk communications should promote a realistic risk appraisal; a proper understanding of how people perceive the risk during respiratory infectious outbreaks is preparatory. Indeed, the understanding of which factors can shape risk perception, and how, is mandatory to design efficacious messages and to identify those targets who might benefit the most of a risk re‐appraisal and of an extra‐communicative effort.
A huge amount of research has been done to identify the most relevant predictors of risk perception for COVID‐like diseases such as SARS, the Middle East respiratory syndrome (MERS), H1N1 influenza pandemic and avian influenza. These diseases have symptomatology and transmission routes close to COVID‐19; symptoms harmfulness and/or systems affected conceivably influence the perceived threat, whereas the mode of transmission influences the perceived chance to be exposed to the virus and avoid the contagion. Therefore, these studies may represent the best candidates to draw some useful knowledge about the possible predictors of risk perception for COVID‐19. In 2009, Leppin and Aro reviewed the previous evidence on the topic focusing on the theoretical models and concepts adopted in the empirical research on risk perception for SARS and avian influenza. In 2011, Koh and colleagues reported a comprehensive systematic review about risk perception for emerging infectious diseases in healthcare workers. Thus, an updated ad comprehensive review about the possible determinants of risk perception for COVID‐like diseases is missing although it might be especially helpful to acknowledge researchers, clinicians and stakeholders about which factors might be modulated to favour a realistic risk appraisal and who might benefit more of such re‐evaluation.
A scoping review was conducted to map the existing literature on risk perception determinants for respiratory infectious diseases and identify possible gaps in knowledge. The following research questions were formulated: (1) What is known so far about those variables that can shape risk perception for respiratory infectious diseases such as COVID‐19 in the overall adult population? (2) Which is the extent, variety and methodological characteristics of previous evidence? And (3) which are the relevant issues to be addressed by future investigations?
METHODS
A scoping review was conducted according to the PRISMA extension for Scoping Reviews (PRISMA—ScR) (Tricco et al., 2018). The review protocol was developed in line with guidelines (Moher et al., 2015), and it will be available on request. Original articles published at any time in peer‐reviewed journals have been considered if written in English and if they reported on the possible factors of influence on risk perception for respiratory infectious diseases in adult participants. Studies were identified exclusively by searching PubMed, Scopus and Web of Science using the term ‘risk perception’ in combination with ‘virus’, ‘infection’, ‘flu’ and specific infectious agents such as ‘SARS’, ‘coronavirus’, ‘MERS’ and ‘influenza’ (see Appendix S1 for the detailed search paths). The last search was run in March 2020. No author was contacted to identify additional sources.
A preliminary eligibility check based on titles and abstracts was performed by the first author after duplicates were removed; the remaining full texts were analysed, and the reference lists were screened to identify additional pertinent articles by the same author. When unsure, eligibility was discussed with the last author. If needed, disagreements were resolved by consensus and discussion. Data were collected by the first author according to an extraction sheet previously developed with the last author. Relevant information was retrieved by full texts, and no direct contact with any of the authors was necessary. No specific assumptions or simplifications were made. The following information was collected:
Infectious disease
Period of testing
Country
Sample size
Sample details and demographics
Method
Independent and dependent variables
Effect size (we computed effect sizes starting from raw data when not available)
Analyses performed
Main results
After data were charted, the variety of infectious diseases considered, dimensions of risk investigated and methodologies adopted across all studies were identified and the percentage of records for each category was computed to be used as a reference point by researchers interested in the field. Then, the range of the possible predictors of risk perception considered in the studies was identified; overall, gender, age, health status, education, disease‐related knowledge, socio‐economic factors, psychological factors, exposure to the disease, exposure to disease‐related information and trust in stakeholders were recognized as possible determinants of the perceived risk. Findings concerning the association between risk perception and each possible predictor were identified across all the records, and a narrative synthesis of results was made by grouping the results by specific or similar factors. A quantitative synthesis of results was not performed due to heterogeneity of the designs adopted and the variety of dependent variables considered across the studies.
A critical quality appraisal of individual sources of evidence was performed by one of the reviewers, providing crucial information about the strength and weakness of the evidence gained so far and the possible need to increase future research methodological rigour. The level of evidence for each study was established through the rating system developed by Melnyk and Fineout‐Overholt (2011), with level 1 assigned to systematic review and meta‐analysis of randomized controlled trials (i.e. the highest possible level of evidence), and level 7 assigned to expert opinions (Melnyk & Fineout‐Overholt, 2011). Ratings are reported in Table S1.
RESULTS
Overall, 3496 records were identified; at the end of the screening process (see Figure 1), 38 studies were identified for inclusion in the review. Seventeen studies were founded by public agencies and one by a private research university. Five studies received no financial support; in fifteen studies, funding information was not reported.
FIGURE 1.
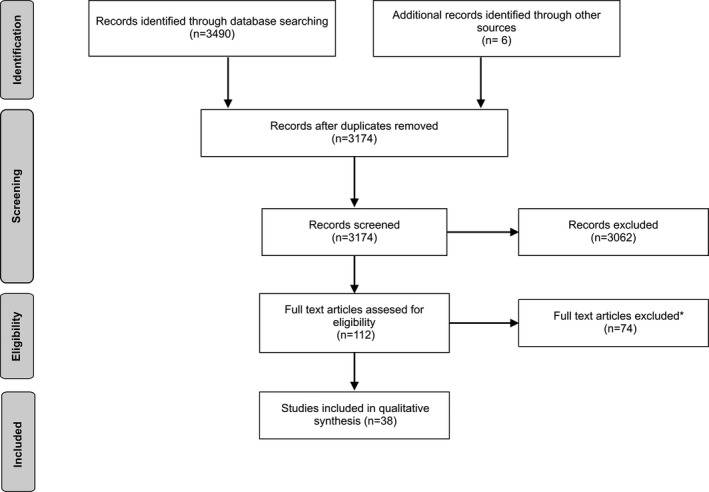
The figure illustrates the selection process. *Reasons for exclusion were the following: no full text available, review articles, no evaluation of perceived risk and/or investigation of the determinants of risk perception
Characteristics of studies
As illustrated in detail in Table S1, several studies focused on H1N1 influenza pandemic (34%), followed by avian influenza (21%), MERS (21%) and SARS (18.5%). Most of the studies were conducted in South‐East Asia (49%) or Europe (24%); fewer were conducted in the United States (10%), Australia (7%), Middle East area (5%) or Canada (5%). Concerning the timing of the investigation, more than a half of the records measured risk perception during the outbreak, whereas 21 per cent of them was conducted after the outbreak; a minority of the studies (10.5%) referred to a ‘hypothetical outbreak’ or did not specify the timing of the research relative to the outbreak (16%).
Both the cognitive and affective dimensions of risk perception have been considered. Fourteen studies (37%) focused on one single measure of risk perception: perceived personal susceptibility, perceived risk of contagion and/or spreading of the disease and an outbreak, disease severity, disease‐related emotions, the perceived risk derived by the media and overall, undefined risk. More studies (39%) focused on several combinations of the mentioned measures, plus acceptance of risk and/or risk of exposure, or risk avoidance. Finally, 9 out of 38 records (24%) considered composite measures of risk perception combining some of the mentioned dimensions in one single index, such as the product of personal susceptibility and severity.
Concerning the instrument adopted, most of the studies (60%) asked participants to complete a self‐report questionnaire; in fewer studies, participants were interviewed using a structured (34%) or semi‐structured protocol (3%). Only one study investigated people's perceptions of risk through focus groups. Concerning the statistical methods, most of studies adopted a regression analysis approach (37%), followed by those relying on between‐groups comparisons (e.g. old vs. young, females vs. males) (16%). The adoption of other approaches such as bivariate correlational analyses (8%), structural equation modelling (8%), thematic analyses (5%) or path analyses (3%) was less frequent; in nine studies (23%), a different combination of the mentioned methods was used.
Quality appraisal of studies
According to the quality appraisal of the studies revised, the findings reported in this scoping review may be partially affected by some methodological biases. The first issue concerns the studies' design and the level of evidence. Indeed, many of the reviewed studies adopted a cross‐sectional, correlational design (Level of Evidence: 4), while four adopted a descriptive/qualitative design (Level of Evidence: 6; Melnyk & Fineout‐Overholt, 2011). However, cross‐sectional, correlational designs (not even mentioning descriptive/qualitative designs) prevent researchers to draw conclusions on the causal effects among the variables of interest (Melnyk & Fineout‐Overholt, 2011).
Also, most of the studies investigated risk perception through an ideographic approach (e.g. through ad hoc single questions, within a semi‐structured interview) or by using dissimilar, multiple‐item measures, whose internal validity was not examined through rigorous psychometric testing. This could putatively explain part of the heterogeneity in previous findings and effect sizes, resulting in a difficult comparison across studies. Also, although they often considered different predictors of risk perception (further increasing the design heterogeneity), they mainly focused on socio‐demographic variables possibly neglecting other significant predictors, such as psychological variables.
Synthesis of results
Gender
A significant positive association was reported between female gender and perceived susceptibility (Brug et al., 2004; Cui et al., 2017; De Zwart et al., 2009, 2010; Ibuka et al., 2010), severity (Cui et al., 2017; Yang & Cho, 2017), overall concerns of getting sick (Alqahtani et al., 2017; Jang et al., 2020) and of getting sick by contact with affected/unaffected people (Yang & Cho, 2017), harmfulness for the community/risk of future outbreaks (Yang & Cho, 2017) and composite measures of risk (Choi et al., 2017; De Zwart et al., 2007, 2009; Kim & Choi, 2016; Van et al., 2010). Female healthcare workers were more likely to report high avoidance of patients, fear of getting sick, intention to change job and low acceptance of risk (Imai et al., 2005). One study reported no effect of gender on risk perception in students of health‐related topics, but female gender was associated with higher risk perception among students of disciplines not related to health (Akan et al., 2010). Only one study reported that men were more likely to perceive a higher risk of an outbreak, but the significance level was marginal (p = .05) (Barennes et al., 2010). Thus, the records analysed show that women usually perceive more risk than men, although many studies did not find any significant relationship between gender and risk perception (Abbate et al., 2006; Barennes et al., 2010; Barr et al., 2008; Commodari, 2017; Fang et al., 2012; Grace et al., 2004; Han et al., 2014; Kim et al., 2015; Kim & Kim, 2018; Koh et al., 2005; Liao et al., 2010; Lin & Lagoe, 2013; Oh et al., 2015; Von Gottberg et al., 2016; Wang et al., 2018; Williams et al., 2012; Xu & Peng, 2015). Furthermore, sex differences in risk perception might be levelled out in certain circumstances, such as when people conceivably have proper knowledge on the topic (i.e. among students of health‐related topics compared with other students; Akan et al., 2010).
Age
A positive association between age and susceptibility (Cui et al., 2017; de Zwart et al., 2010; Van et al., 2010), severity (Ibuka et al., 2010), possible epidemic‐related damages for the community/likelihood of re‐emerging of the disease (Yang & Cho, 2017) and composite risk (Fang et al., 2012) was reported. Furthermore, respondents older than 65 were significantly more likely than younger counterparts to judge ‘very/extremely likely’ an imminent outbreak (Barr et al., 2008) and they perceived significantly higher susceptibility to and seriousness of the contagion (Commodari, 2017).
However, a negative association between age, perceived susceptibility (Kim et al., 2015), risk of contagion (Von Gottberg et al., 2016) and concerns about getting sick (Yang & Cho, 2017) was reported. Moreover, respondents aged more than 70 were less likely to perceive a high risk of spread of the epidemic, but more likely to have concerns about the contagion than younger counterparts (Jang et al., 2020).
Therefore, the majority of studies reveals that risk perception increases with age, although some studies reported the opposite evidence and thirteen studies did not report any significant association (Brug et al., 2004; Choi et al., 2017; De Zwart et al., 2009; Di Giuseppe et al., 2008; Han et al., 2014; Ibuka et al., 2010; Kim & Choi, 2016; Kim & Kim, 2018; Liao et al., 2010; Oh et al., 2015; Wang et al., 2018; Williams et al., 2012; Xu & Peng, 2015). Accordingly, confounding factors may modulate the relationship between risk perception and age. For instance, age was reported to be positively associated with perceived risk in Europe but not in Asia (De Zwart et al., 2007); thus, cultural issues might have a role. Also, older healthcare workers were less inclined to avoid affected patients and more prone to accept the risk of contagion as part of their professional duty (Imai et al., 2005). Hence, professional aptitude to be involved in risk‐related circumstances and sound experience on how to handle safely these situations might mediate the effect of age on risk perception. It is not clear why age per se should influence risk perception; in fact, other factors tightly associated with age might be conceivably more relevant. For instance, elders likely have worse health; thus, they might perceive a higher threat.
Health status
Poor self‐reported health has been associated with a higher perceived likelihood of infectious outbreak and concerns about getting sick (Barr et al., 2008; Jacobs et al., 2010), higher risk of contagion (Xu & Peng, 2015) and higher composite risk (Kim & Kim, 2018) when compared to good health. Having poor immunity was as a reason to be moderately/highly concerned about getting sick (Alqahtani et al., 2017); individuals with chronic conditions were significantly more likely to be concerned (Alqahtani et al., 2017). In line with these observations, it has been qualitatively observed that participants who were feeling well believed they could not get sick (Cava et al., 2005). Thus, it seems that people who feel to be physically more vulnerable are reliably more prone to perceive higher risk and they worry the most. Only one study reported no effect of the health status on risk perception, but we might note that it considered healthcare workers rather than the lay public (Grace et al., 2004), that is individuals who are expected to have specific illness‐related knowledge and to be specifically trained on how to avoid infections, possibly reducing the sense of vulnerability associated with poor health.
Socio‐economic factors
Low income predicted higher perceived composite risk (Choi et al., 2017); moreover, the percentage of respondents who perceived the chance of an influenza pandemic ‘very/extremely likely’ was significantly higher in those employed but with the lowest income than in those unemployed or with high income (Barr et al., 2008). Respondents with middle income were more likely to report less perceived risk (Jacobs et al., 2010). Nevertheless, the association between employment status and risk perception was not confirmed further (Commodari, 2017; Van et al., 2010) and four studies reported no significant association between income and risk perception (Han et al., 2014; Kim & Kim, 2018; Wang et al., 2018; Xu & Peng, 2015). The perceived risk of (Di Giuseppe et al., 2008) and concerns about (Jang et al., 2020) getting sick were reported to be higher in low socio‐economic classes; however, no association was reported in another study (Kim & Kim, 2018). Household size was negatively associated with predicted dead tool and positively with susceptibility (Ibuka et al., 2010).
Overall, it seems that the lower is the perceived financial welfare, the higher is the perceived risk: expectations about proper access to medical care or therapies might explain this finding. Indeed, perceived risk was reported to be higher also in ethnic minorities (Kim et al., 2015; Van et al., 2010) (though no association was also found; de Zwart et al., 2010; Grace et al., 2004), who usually claim more financial, cultural, and linguistic barriers to adequate health care. However, previous results are not unanimous when considering the relationship between welfare and risk perception. Thus, possible confounding factors might mediate this relationship. This might be the case of age and education, which are known to be related to one's socio‐economic status but influence risk perception. Indeed, about half of the mentioned records did not correct for age and education when considering the possible relationship between individuals' financial welfare and the perceived risk. However, it is not possible to detect a dissimilar pattern of results between those studies that did or did not consider the concurrent effect of multiple demographic variables.
Finally, fewer studies considered the family status, reporting both a positive association between having young children, perceived susceptibility (de Zwart et al., 2010; Kim et al., 2015) and concerns (Kim et al., 2015) and no significant association (Abbate et al., 2006; Barr et al., 2008; Commodari, 2017; Koh et al., 2005; Wang et al., 2018).
Education and disease‐related knowledge
Education was found to be negatively associated with composite perceived risk (Di Giuseppe et al., 2008), concerns about getting sick (Brug et al., 2004; Kim et al., 2015), perceived severity (Commodari, 2017; De Zwart et al., 2009) and susceptibility (Commodari, 2017; De Zwart et al., 2009, 2010; Xu & Peng, 2015). Moreover, the percentage of respondents who judged ‘very/extremely likely’ the chance of an imminent influenza pandemic was significantly high among those participants without formal qualification (Barr et al., 2008). Conversely, a positive association between education, perceived risk of an outbreak (Barennes et al., 2010) and composite risk perception (Fang et al., 2012) was reported, whereas respondents with a university degree were more likely to be concerned than less educated participants (Jang et al., 2020). Therefore, people with low education more frequently perceive high risk than the opposite; however, the experimental evidence is not sufficient to draw strong conclusions, also because nine studies did not report any significant association between education and perceived risk (Choi et al., 2017; Cui et al., 2017; Jang et al., 2020; Kim & Choi, 2016; Kim & Kim, 2018; Oh et al., 2015; Von Gottberg et al., 2016; Wang et al., 2018).
Furthermore, one may argue that the effect of education on risk perception might not be aspecific but rather related to the possibility to understand, critically analyse and search for disease‐related information and acquire sound knowledge on the topic. Lay people trained on avian influenza were significantly more likely to perceive a higher risk than those not trained (Barennes et al., 2010) and nursing students who received specific education on MERS had higher fear of getting sick than those who did not (Kim & Choi, 2016).
More broadly, good overall disease‐related knowledge has been associated with high perceived severity (De Zwart et al., 2009), composite risk perceptions (Kim & Kim, 2018) and concerns of contagion from affected people/risk of future outbreaks (Yang & Cho, 2017), but a negative association was reported with the perceived risk of contagion (Di Giuseppe et al., 2008), concerns about one's health (Brug et al., 2004) and susceptibility (de Zwart et al., 2010). Only one study did not find any association (Williams et al., 2012). Thus, having good knowledge about the disease does seem related to risk perception, even though it is not clear whether it is associated with higher or lower perceived risk. Both directions might be plausible. Good knowledge might make people more confident about how to face the threat and stay safe, but it might favour a clearer understanding of the likelihood of contagion and possible outcomes, increasing the perceived risk. Indeed, perceived lack of disease‐related information has been associated both negatively (Di Giuseppe et al., 2008) and positively with risk perception, in quantitative (Abbate et al., 2006) and qualitative (Jiang et al., 2009) studies. This inconsistency might be related not only to the adoption of dissimilar and composite measures, including knowledge on symptoms and transmission route (De Zwart et al., 2009), but also to the death rate, available treatments and vaccine (de Zwart et al., 2010), overall understanding of quarantine and social distancing measures (Yang & Cho, 2017). Results might be clearer when considering how knowledge of specific aspects possibly affects risk perception. For instance, familiarity with available treatments was associated with low susceptibility (Kim et al., 2015), possibly because people might be reassured by the fact that the disease can be treated. However, the mentioned records cannot clarify whether people perceive lower/higher risk because of their dissimilar level of disease‐related knowledge or whether people who have different risk perceptions are differently determined to seek information. For instance, higher overall perceived risk (Abbate et al., 2006) and physicians' avoidance of affected patients (Imai et al., 2005) have been related to good knowledge about how to prevent the contagion. In principle, this applies to all the variables measured in cross‐sectional, correlational studies and must be kept in mind when considering the findings below. Differently, certain variables such as sex, age, health status, socio‐economic factors and education can be hardly affected by risk perception so that a causal effect might be assumed.
Exposure to disease‐related information
The amount of disease‐related information received has been positively associated with perceived severity and susceptibility (De Zwart et al., 2009). Relying on television (Abbate et al., 2006) for disease‐related information and the exposure to mass media (Choi et al., 2018), entertainment media (Oh et al., 2015) and the Internet (Choi et al., 2018; Han et al., 2014; Oh et al., 2020) were positively associated with perceived risk. Respondents who owned a TV, have heard recently about avian influenza and who could recall at least one message about the disease were more likely to perceive a higher risk of an outbreak (Barennes et al., 2010). Perceived trustworthiness of the media was positively associated with perceived risk (Choi et al., 2018; Fang et al., 2012; Kim & Kim, 2018; Yang & Cho, 2017), but the perceived adequacy of official information was not related to susceptibility (Grace et al., 2004); conversely, low perceived consistency of media messages has been qualitatively reported to be a factor possibly lowering risk perception (Cava et al., 2005).
Thus, intense exposure to disease‐related information through the media might increase the perceived threat, possibly by reinforcing the perceived harmfulness of and proximity to the disease. However, trust in the information received and consistency of the messages might mediate the effect of media exposure. In line with this hypothesis, people who are more exposed and dependent on the media as a source of information are those who think that disease‐related information received through the media makes them feel at risk (Lin & Lagoe, 2013). Furthermore, also informal disease‐related information might play a role. For instance, a high rate of interpersonal communication about the disease seems to amplify the perceived risk (Han et al., 2014) and trust in informal information has been negatively associated with perceived susceptibility but positively with concerns (Liao et al., 2010).
Attention paid to the media, in addition to the overall exposure, was positively associated with perceived risk (Han et al., 2014), and participants who adopted a systematic (rather than heuristic) processing of information were more likely to perceive a higher risk (Choi et al., 2017). On the other hand, a higher perceived ability to gather disease‐related information predicts low perceived risk (Choi et al., 2018). Therefore, individuals might be differently receptive to disease‐related communications and interindividual variability might interplay within the relationship between exposure to disease‐related information and risk perception.
Exposure to the disease
A close threat is generally perceived as more dreadful than a distant hazard; thus, factors influencing the perception of closeness to the disease may affect risk perception. Knowing someone affected positively correlates with both susceptibility and concerns (Grace et al., 2004; Kim et al., 2015), and having family members or friends infected was a reason to be ‘moderately/highly concerned’ about getting sick (Alqahtani et al., 2017). Also, healthcare workers previously exposed to other infectious diseases perceived a higher risk of contagion, but no significant association between the experience of influenza‐like symptoms during an outbreak and risk perception was reported (Grace et al., 2004; Wang et al., 2018). Being exposed to affected patients because of one's job was reported as a reason to be concerned about getting sick (Alqahtani et al., 2017), whereas healthcare workers who have rare contact with affected patients were more likely to perceive a low risk of exposure to the disease (Koh et al., 2005). Likewise, municipal employees with daily contact with costumers perceived higher risk than employees with sporadic interactions (Von Gottberg et al., 2016).
More broadly, perceiving the living environment to be unsafe has been qualitatively reported as a possible factor associated with higher perceived risk (Jiang et al., 2009). For instance, crowded places might be perceived as at high risk of contagion. The level of urbanization has been positively associated with perceived severity and personal susceptibility (De Zwart et al., 2009), and people living in metropolitan areas were more likely to have high concerns than people living in non‐metropolitan locations (Jang et al., 2020). Nevertheless, the percentage of people who perceived an infectious outbreak as ‘very/extremely likely’ was significantly higher among those respondents living in rural than in urban locations (Barr et al., 2008), and people living in rural areas were more likely to report high composite risk (Barennes et al., 2010; Jacobs et al., 2010) than people living in urban regions; only one study did not find any association between living in rural/urban locations and risk perception (Wang et al., 2018). Less availability of healthcare services in the rural areas might explain these findings. Inconsistent results might be explained considering that the criteria used to distinguish between what is rural and what is urban/metropolitan are not usually specified across studies; thus, incoherent categorizations might be expected.
Within the same country, people living in more affected areas were more likely to perceive high severity (Alqahtani et al., 2017) and susceptibility (Ibuka et al., 2010). Moreover, the presence of laboratory‐confirmed cases in one's area was a reason to be ‘moderately/highly concerned’ about getting sick (Alqahtani et al., 2017). Only one study reported no significant association between living in affected/unaffected areas and risk perception (Jang et al., 2020); thus, the higher is the perceived geographical closeness to the disease, the higher is the perceived risk, at least within the national borders. When comparing different countries, results are less conclusive. Susceptibility for SARS was reported to be higher in Asia (more affected) than in Europe (De Zwart et al., 2009) but the perceived severity of SARS (De Zwart et al., 2009) and perceived risk (i.e. severity × susceptibility) for avian influenza (De Zwart et al., 2007) were higher in Europe (less affected) than in Asia. Likewise, Chinese students perceived higher composite risk than US students, although more US than Chinese respondents claimed to have been infected (Han et al., 2014). Cultural issues conceivably interplay with epidemiological factors (i.e. the rate of infection) in shaping risk perception at the international level. Cho and Lee (2015) reported that US respondents perceived lower susceptibility (but not severity) for H1N1 influenza than Koreans (although the infection and mortality rates were higher in the United States), suggesting that people from individualistic cultures—the US respondents—tend to be more overconfident than people from collectivistic cultures—the Koreans. Furthermore, the perceived harmfulness for oneself was a stronger predictor of the adoption of preventive measures in the—individualistic—US respondents, whereas subjective norms (i.e. what others think) were more relevant among the—collectivistic—Koreans.
Trust in stakeholders
Trust in the central government (Choi et al., 2018; Jang et al., 2020; Yang & Cho, 2017), in health policy and medical professionals (Yang & Cho, 2017) was reported to be negatively associated with perceived risk. In line with these results, trust in the government's capability to prevent the spread of the contagion was qualitatively reported to be a factor associated with lower risk perception (Jiang et al., 2009). However, trust in local government was positively associated with perceived risk (Yang & Cho, 2017) and risk perception increases as the perceived trustworthiness of local governors and health departments increases (Wang et al., 2018). On the other hand, the perceived preparedness of one's institution predicts a higher acceptance of work‐related risks and negatively predicts the willingness to avoid infected patients in healthcare workers (Imai et al., 2005); no effect of perceived preparedness of the institution on risk perception was also found (Grace et al., 2004). Thus, when considering the possible effect of trust in stakeholders on risk perception it seems crucial to distinguish between local and central institutions. Furthermore, we might note that none of the Western studies did consider trust in stakeholders as a possible determinant of risk perception. However, overall deference to and compliance with stakeholders might be significantly different when considering Western or Eastern societies.
Psychological factors
Concerning personality traits, being conscious has been related (may be not surprisingly) to high perceived susceptibility, whereas more ‘imaginative’ people perceived higher seriousness (Commodari, 2017), possibly because they might be more prone to imagine the potential‐related outcomes and implications. A negative association between general self‐efficacy and susceptibility was reported (Commodari, 2017), but one study reported no association (Kim & Kim, 2018). Perceived self‐efficacy might favour a sense of control over the situation, reducing the perceived risk. In line with this hypothesis, high self‐efficacy in avoiding the contagion and dealing with the disease was associated with lower composite risk (Choi et al., 2017; Han et al., 2014) and susceptibility (Brug et al., 2004; Liao et al., 2010); also, municipal employees with a high perceived self‐efficacy about performing their job during a pandemic reported lower perceived risk of getting sick (Von Gottberg et al., 2016). Thus, psychological features, such as personality traits and self‐efficacy, seem related to risk perception. These aspects are typically considered dispositional traits; thus, it is more likely that they do influence risk perception rather than the opposite.
Conversely, feeling at risk might have a deleterious effect on people's psychological well‐being and, in turn, psychological distress possibly increases the perceived threat. A positive association between psychological distress and risk perception has been reported both in the lay public (Jacobs et al., 2010) and in the healthcare workers (Koh et al., 2005); only one study reported no association (Barr et al., 2008). Also, intense rumination has been associated with perceived susceptibility (de Zwart et al., 2010); however, the cross‐sectional and correlational designs adopted in the studies do not allow for causal inferences.
DISCUSSION
This scoping review aims at taking stock about those variables that possibly shape risk perception for respiratory infectious diseases such as COVID‐19, focusing on the extent, variety and characteristics of previous evidence. Overall, a great heterogeneity emerged, preventing a clear comparison between studies and possibly explaining the incongruent results reported. Specifically, the following issues may be kept in mind when considering the reported association between a certain variable of interest and risk perception.
Risk perception of H1N1 influenza pandemic, avian influenza, MERS and SARS was investigated with a similar occurrence; however, several different countries have been involved. This is important to note because our findings suggest that the effect of certain variables (i.e. age, the infection rate in the area) on risk perception might be different across countries. Furthermore, we speculate that also the effect of other variables, and specifically trust media and governments, might be different when comparing Western and Eastern societies. Nevertheless, the possible effect of culture on risk perception has been relatively neglected.
Concerning the timing of the investigation, most of the studies measured risk perception during the outbreak, but some of them followed the epidemic or refer to hypothetical outbreaks. Nevertheless, people's appraisal of threat changes over time (Liao et al., 2010), and possibly also the effect of the variables influencing risk perception.
Furthermore, the records used dissimilar measures of risk perception and the internal validity was often not rigorously tested. However, most of the studies implemented a structured protocol, which was either filled in by participants or administered by the experimenter, ensuring a standard evaluation within participants. This scenario mirrors the lack of a uniform theoretical definition of risk perception, challenging the comparison of different studies and a comprehensive understanding of the experimental evidence. To overcome this issue, future studies should refer to precise and structured theoretical frameworks, which clearly define which dimensions constitute risk perception, how to measure them and how the perceived threat might affect people's behaviours. The protection motivation theory (Rogers, 1975, 1983) and the health belief model (Sheeran & Abraham, 1996) may be considered.
Also, all the studies adopted cross‐sectional, correlational designs, which are inherent to the object of the investigation but prevent the identification of causal effects among the variables considered (Melnyk & Fineout‐Overholt, 2011). This might be especially relevant when considering those variables that could both influence and be influenced by risk perception (e.g. psychological distress, disease‐related knowledge), allowing only speculative interpretations. Conversely, certain other variables, such as sex, age, socio‐economic factors and education, can be hardly affected (or not affected at all) by risk perception; thus, we could assume that they do affect risk perception, rather than the opposite. At least, most of the records adopted statistical models (i.e. regression analysis, path analysis, and structural equation modelling) able to detect the possible effect of each variable on risk perception weighted by the simultaneous effect of all other variables. This is especially valuable when considering multidimensional and complex phenomena in which several factors are expected to interplay, such as risk perception. On the contrary, the exclusive use of correlational analyses and between‐groups comparisons might give a partial picture.
Summary of evidence
Several variables have been associated with risk perception for respiratory infectious diseases. Concerning the socio‐demographic domain, women and elders seem to experience higher risk. Women are known to be more prone to experience negative emotions in response to threats (Vianello et al., 2013), possibly explaining why they perceive higher risk; conversely, it is not clear why age should influence risk perception. However, our findings show that poor health status is reliably associated with a higher perceived risk of getting sick and concerns for one's health. Thus, elders may perceive higher threat because they feel to be more physically vulnerable than younger counterparts. Indeed, the only study that did consider the effect of age on risk perception weighted for participants' health found no significant association (Kim & Kim, 2018). Furthermore, age might be associated with other demographic variables, such as overall education and income. Individuals' level of education seems to affect the perceived risk, but the direction of this association is not clear. Low education has been associated more frequently with higher risk perception than a lower perceived threat, possibly because people with lower education might experience more barriers in the understanding of risk communications, decoding the risk as non‐familiar/uncontrollable and more threatening (Sjöberg, 2000). Similarly, our findings suggest that the lower is the people's financial welfare, the higher is the perceived risk; expectations about access to health care might explain this observation, although results are not unanimous. To sum up, the effect of age on risk perception might be related to the dissimilar level of education and/or income. Indeed, eight records out of eleven reported no association between age and risk perception when considering the concurrent effect of education and/or the socio‐economic status (Brug et al., 2004; Choi et al., 2017; De Zwart et al., 2009; Di Giuseppe et al., 2008; Han et al., 2014; Kim & Kim, 2018; Oh et al., 2015; Xu & Peng, 2015); only two studies found a positive association (Commodari, 2017; Jang et al., 2020), and one reported a negative association (Von Gottberg et al., 2016). Socio‐demographic characteristics likely influence the perceived risk; nevertheless, because of their tight interplay, it might be hard to identify their unique contribution. The concurrent interplay of several factors might explain incongruent results since studies considered different sets of variables.
Furthermore, differences in risk perception related to sex, age and health status can be levelled out when individuals have specific health‐related knowledge. This might increase the perceived familiarity and control over the situation, attenuating that part of vulnerability related to specific demographic groups. In line with this hypothesis, those studies focused on healthcare workers did not report any effect of sex, age, and health status on risk perception and the contribution of disease‐related knowledge on risk perception has been reported, even though it is not clear whether it is associated with higher or lower perceived risk. People with good knowledge might feel more prepared to face the outbreak and avoid the contagion; indeed, higher perceived self‐efficacy has been related to lower perceived risk. However, a clear understanding of contagion mechanisms and the possible outcomes could increase the perceived likelihood and severity of the threat. Likewise, also an intense exposure to disease‐related information through the media has been related to higher risk perception. Nevertheless, people who perceive higher risk might actively seek more information and acquire better knowledge. Furthermore, also professional exposure, knowing some affected and living in more affected areas possibly increase risk perception by modulating people's perceived proximity to the threat.
Finally, preliminary results suggest a significant relationship between risk perception, self‐efficacy, personality traits and psychological distress, but records on the topic are rare. Also, other psychological dimensions likely impact people's capability to face stressful situations, perceived safety, and control, thus possibly influencing risk perception: coping strategies, locus of control and attachment may be good candidates. Future investigations may provide further evidence on the possible psychological factors influencing risk perception.
Limitations of the review process
Possible limitations related to our review process might be noted. First, only one reviewer performed the screening of potential articles and charted data. However, clear criteria were adopted, preventing possible individual biases, and when in doubt, a second opinion was sought. Second, we included only studies written in English possibly limiting the coverage of our investigation. Nevertheless, English is adopted internationally by the scientific community; thus, we expected more relevant researches to be published in this language. Finally, we focused on records concerning COVID‐like diseases since this was the richest source of evidence up to March 2020, but our findings might be integrated with the latest studies on COVID‐19 itself.
CONCLUSIONS
To guarantee optimal adhesion to preventive measures, risk‐related communications should encourage a risk appraisal that matches the real threat. This could mean either increasing or decreasing the perceived risk, according to the actual vulnerability of each target. The mentioned findings point out that risk biases exist, and thus, they should be taken into high consideration when designing risk communications aimed to promote a veridical risk appraisal. Indeed, our results may help policy‐makers in focusing the available, and possibly limited, resources on those groups most likely to have biased risk perceptions. For instance, young people, men and those believing to be in good health or to be able to face efficaciously the disease might be too optimistic and this might be a deterrent to the adoption of self‐preventive measures. Providing concrete examples that also these categories can be affected and significantly harmed might favour a functional re‐appraisal. Conversely, elders, women, those with poor health and those perceiving low self‐efficacy might (unnecessarily) overreact, experiencing intense fear and psychological distress: we speculate that as much as people perceive the threat as inescapable as much as they might be discouraged to adopt self‐protective behaviours. In this case, interventions aimed at promoting people's empowerment and providing psychological support might be of help.
Also, risk communications might be differentiated and properly tailored to the group's needs when specific targets are identified. For example, people from lower socio‐economic classes, with low education and ethnic minorities seem to be exposed to risk perception biases. Therefore, risk communications may purposely address these groups, taking into consideration possible linguistic and/or intellectual barriers. Indeed, providing proper knowledge on the topic seems to be crucial, possibly explain why the effect of socio‐demographic variables seems attenuated among healthcare workers.
Indeed, the media have a crucial role in shaping people's risk appraisal, as they represent a fundamental source of information. Lack of credibility because of incoherent communications might attenuate the perceived risk and discourage people to engage in precautionary behaviours; however, disproportionate media coverage and a sensationalistic approach might induce unnecessary pessimism.
Concluding, our findings provide useful complementary knowledge about infectious diseases such as COVID‐19, which might be especially helpful to policy‐makers and clinicians facing the challenge of an efficacious communication of disease‐related information to the public. However, we may note that people's compliance with preventive behaviours may be related to factors other than risk perception, such as the presence (or not) of compulsory government regulations and people's motivation to comply with the social norms (e.g. in collectivistic cultures). This might explain why risk perception usually explains only a small proportion of variance in the adoption of preventive measures (Bish & Michie, 2010). Nevertheless, this review may be useful to guide the design of upcoming studies and to interpret the future findings on risk perception of COVID‐19.
CONFLICT OF INTEREST
The authors declare no competing interests.
ETHICS STATEMENT
The present work was realized in accordance with the Ethical principles of psychologists and code of conduct (American Psychological Association, 2002, http://www.apa.org/ethics)
Supporting information
Appendix S1
Tagini S, Brugnera A, Ferrucci R, et al. It won't happen to me! Psychosocial factors influencing risk perception for respiratory infectious diseases: A scoping review. Appl Psychol Health Well‐Being. 2021;13:835–852. 10.1111/aphw.12274
Gabriella Pravettoni and Barbara Poletti equally contributed to this study
DATA AVAILABILITY STATEMENT
All relevant data are provided within the article or can be retrieved by the original works reviewed.
REFERENCES
- Abbate, R. , Di Giuseppe, G. , Marinelli, P. , & Angelillo, I. (2006). Knowledge, attitudes, and practices of avian influenza, poultry workers, Italy. Emerging Infectious Diseases, 12(11), 1762–1765. 10.3201/eid1211.060671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akan, H. , Gurol, Y. , Izbirak, G. , Ozdatl, S. , Yilmaz, G. , Vitrinel, A. , & Hayran, O. (2010). Knowledge and attitudes of university students toward pandemic influenza: A cross‐sectional study from Turkey. BMC Public Health, 10, 1–8. 10.1186/1471-2458-10-413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alqahtani, A. S. , Rashid, H. , Basyouni, M. H. , Alhawassi, T. M. , & BinDhim, N. F. (2017). Public response to MERS‐CoV in the Middle East: iPhone survey in six countries. Journal of Infection and Public Health, 10(5), 534–540. 10.1016/j.jiph.2016.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barennes, H. , Harimanana, A. N. , Lorvongseng, S. , Ongkhammy, S. , & Chu, C. (2010). Paradoxical risk perception and behaviours related to Avian Flu outbreak and education campaign, Laos. BMC Infectious Diseases, 10, 294. 10.1186/1471-2334-10-294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr, M. , Raphael, B. , Taylor, M. , Stevens, G. , Jorm, L. , Giffin, M. , & Lujic, S. (2008). Pandemic influenza in Australia: Using telephone surveys to measure perceptions of threat and willingness to comply. BMC Infectious Diseases, 8, 1–14. 10.1186/1471-2334-8-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bish, A. , & Michie, S. (2010). Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. British journal of health psychology, 15(4), 797–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brug, J. , Aro, A. R. , Oenema, A. , de Zwart, O. , Richardus, J. H. , & Bishop, G. D. (2004). SARS risk perception, knowledge, precautions, and information sources, the Netherlands. Emerging Infectious Diseases, 10(8), 1486–1489. 10.3201/eid1008.040283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brug, J. , Aro, A. R. , & Richardus, J. H. (2009). Risk perceptions and behaviour: Towards pandemic control of emerging infectious diseases. International Journal of Behavioral Medicine, 16(1), 3–6. 10.1007/s12529-008-9000-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cava, M. A. , Fay, K. E. , Beanlands, H. J. , McCay, E. A. , & Wignall, R. (2005). Risk perception and compliance with quarantine during the SARS outbreak. Journal of Nursing Scholarship, 37(4), 343–347. 10.1111/j.1547-5069.2005.00059.x [DOI] [PubMed] [Google Scholar]
- Cho, H. , & Lee, J. S. (2015). The influence of self‐efficacy, subjective norms, and risk perception on behavioral intentions related to the H1N1 flu pandemic: A comparison between K orea and the US. Asian Journal of Social Psychology, 18(4), 311–324. [Google Scholar]
- Choi, D. , Shin, D.‐H. , Park, K. , & Yoo, W. (2018). Exploring risk perception and intention to engage in social and economic activities during the South Korean MERS outbreak. International Journal of Communication, 12, 3600–3620. [Google Scholar]
- Choi, D. , Yoo, W. , Noh, G. , & Park, K. (2017). The impact of social media on risk perceptions during the MERS outbreak in South Korea. Computers in Human Behavior, 72, 422–431. 10.1016/j.chb.2017.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Commodari, E. (2017). The role of sociodemographic and psychological variables on risk perception of the flu. SAGE Open, 7(3). 10.1177/2158244017718890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui, B. , Liao, Q. , Lam, W. W. T. , Liu, Z. P. , & Fielding, R. (2017). Avian influenza A/H7N9 risk perception, information trust and adoption of protective behaviours among poultry farmers in Jiangsu Province, China. BMC Public Health, 17(1), 1–13. 10.1186/s12889-017-4364-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Zwart, O. , Veldhuijzen, I. K. , Elam, G. , Aro, A. R. , Abraham, T. , Bishop, G. D. , Richardus, J. H. , & Brug, J. (2007). Avian influenza risk perception, Europe and Asia. Emerging Infectious Diseases, 13(2), 290–293. 10.3201/eid1302.060303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Zwart, O. , Veldhuijzen, I. K. , Elam, G. , Aro, A. R. , Abraham, T. , Bishop, G. D. , Voeten, H. A. C. M. , Richardus, J. H. , & Brug, J. (2009). Perceived threat, risk perception, and efficacy beliefs related to SARS and other (emerging) infectious diseases: Results of an international survey. International Journal of Behavioral Medicine, 16(1), 30–40. 10.1007/s12529-008-9008-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Zwart, O. , Veldhuijzen, I. K. , Richardus, J. H. , & Brug, J. (2010). Monitoring of risk perceptions and correlates of precautionary behaviour related to human avian influenza during 2006–2007 in the Netherlands: Results of seven consecutive surveys. BMC Infectious Diseases, 10, 1–15. 10.1186/1471-2334-10-114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Giuseppe, G. , Abbate, R. , Albano, L. , Marinelli, P. , & Angelillo, I. F. (2008). A survey of knowledge, attitudes and practices towards avian influenza in an adult population of Italy. BMC Infectious Diseases, 8, 1–8. 10.1186/1471-2334-8-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang, D. , Fang, C. L. , Tsai, B. K. , Lan, L. C. , & Hsu, W. S. (2012). Relationships among trust in messages, risk perception, and risk reduction preferences based upon avian influenza in Taiwan. International Journal of Environmental Research and Public Health, 9(8), 2742–2757. 10.3390/ijerph9082742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace, S. L. , Hershenfield, K. , Robertson, E. , & Stewart, D. E. (2004). Factors affecting perceived risk of contracting severe acute respiratory syndrome among academic physicians. Infection Control & Hospital Epidemiology, 25(12), 1111–1113. 10.1086/502352 [DOI] [PubMed] [Google Scholar]
- Han, G. K. , Zhang, J. M. , Chu, K. R. , & Shen, G. (2014). Self‐other differences in H1N1 flu risk perception in a global context: A comparative study between the United States and China. Health Communication, 29(2), 109–123. 10.1080/10410236.2012.723267 [DOI] [PubMed] [Google Scholar]
- Ibuka, Y. , Chapman, G. B. , Meyers, L. A. , Li, M. , & Galvani, A. P. (2010). The dynamics of risk perceptions and precautionary behavior in response to 2009 (H1N1) pandemic influenza. BMC Infectious Diseases, 10, 296. 10.1186/1471-2334-10-296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, T. , Takahashi, K. , Hoshuyama, T. , Hasegawa, N. , Lim, M. K. , & Koh, D. (2005). SARS risk perceptions in healthcare workers, Japan. Emerging Infectious Diseases, 11(3), 404–410. 10.3201/eid1103.040631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs, J. , Taylor, M. , Agho, K. , Stevens, G. , Barr, M. , & Raphael, B. (2010). Factors associated with increased risk perception of pandemic influenza in Australia. Influenza Research and Treatment, 2010, 1–7. 10.1155/2010/947906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang, W. M. , Kim, U.‐N. , Jang, D. H. , Jung, H. , Cho, S. , Eun, S. J. , & Lee, J. Y. (2020). Influence of trust on two different risk perceptions as an affective and cognitive dimension during Middle East respiratory syndrome coronavirus (MERS‐CoV) outbreak in South Korea: Serial cross‐sectional surveys. British Medical Journal Open, 10(3), e033026. 10.1136/bmjopen-2019-033026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang, X. , Elam, G. , Yuen, C. , Voeten, H. , De Zwart, O. , Veldhuijzen, I. , & Brug, J. (2009). The perceived threat of SARS and its impact on precautionary actions and adverse consequences: A qualitative study among Chinese communities in the United Kingdom and the Netherlands. International Journal of Behavioral Medicine, 16(1), 58–67. 10.1007/s12529-008-9005-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, J. S. , & Choi, J. S. (2016). Middle East respiratory syndrome‐related knowledge, preventive behaviours and risk perception among nursing students during outbreak. Journal of Clinical Nursing, 25(17–18), 2542–2549. 10.1111/jocn.13295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, S. , & Kim, S. (2018). Exploring the determinants of perceived risk of middle east respiratory syndrome (MERS) in Korea. International Journal of Environmental Research and Public Health, 15(6), 1168. 10.3390/ijerph15061168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, Y. , Zhong, W. , Jehn, M. , & Walsh, L. (2015). Public risk perceptions and preventive behaviors during the 2009 H1N1 influenza pandemic. Disaster Medicine and Public Health Preparedness, 9(2), 145–154. 10.1017/dmp.2014.87 [DOI] [PubMed] [Google Scholar]
- Koh, D. , Meng, K. L. , Sin, E. C. , Soo, M. K. , Qian, F. , Ng, V. , Ban, H. T. , Kok, S. W. , Wuen, M. C. , Hui, K. T. , Ng, W. , Muttakin, Z. , Emmanuel, S. , Ngan, P. F. , Koh, G. , Chong, T. K. , Tan, K. B. C. , & Fones, C. (2005). Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore: What can we learn? Medical Care, 43(7), 676–682. 10.1097/01.mlr.0000167181.36730.cc [DOI] [PubMed] [Google Scholar]
- Leppin, A. , & Aro, A. R. (2009). Risk perceptions related to SARS and avian influenza: Theoretical foundations of current empirical research. International Journal of Behavioral Medicine, 16(1), 7–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao, Q. , Cowling, B. , Lam, W. T. , Ng, M. W. , & Fielding, R. (2010). Situational awareness and health protective responses to pandemic influenza A (H1N1) in Hong Kong: A cross‐sectional study. PLoS One, 5(10), e13350. 10.1371/journal.pone.0013350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, C. A. , & Lagoe, C. (2013). Effects of news media and interpersonal interactions on H1N1 risk perception and vaccination intent. Communication Research Reports, 30(2), 127–136. 10.1080/08824096.2012.762907 [DOI] [Google Scholar]
- Melnyk, B. M. , & Fineout‐Overholt, E. (2011). Evidence‐based practice in nursing & healthcare: A guide to best practice. Lippincott Williams & Wilkins. [Google Scholar]
- Moher, D. , Shamseer, L. , Clarke, M. , Ghersi, D. , Liberati, A. , Petticrew, M. , Shekelle, P. , & Stewart, L. A. (2015). Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015 statement. Systematic Reviews, 4(1), 1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh, S. H. , Lee, S. Y. , & Han, C. (2020). The effects of social media use on preventive behaviors during infectious disease outbreaks: The mediating role of self‐relevant emotions and public risk perception. Health Communication, 1–10. 10.1080/10410236.2020.1724639 [DOI] [PubMed] [Google Scholar]
- Oh, S. H. , Paek, H. J. , & Hove, T. (2015). Cognitive and emotional dimensions of perceived risk characteristics, genre‐specific media effects, and risk perceptions: The case of H1N1 influenza in South Korea. Asian Journal of Communication, 25(1), 14–32. 10.1080/01292986.2014.989240 [DOI] [Google Scholar]
- Rogers, R. W. (1975). A protection motivation theory of fear appeals and attitude change. The Journal of Psychology, 91(1), 93–114. 10.1080/00223980.1975.9915803 [DOI] [PubMed] [Google Scholar]
- Rogers, R. W. (1983). Cognitive and psychological processes in fear appeals and attitude change: A revised theory of protection motivation. In Cacioppo J. T. & Petty R. (eds.), Social psychophysiology: A sourcebook (pp. 153–176). Guilford. [Google Scholar]
- Sheeran, P. , & Abraham, C. (1996). The health belief model. Predicting Health Behaviour, 2, 29–80. [Google Scholar]
- Slovic, P. , Finucane, M. L. , Peters, E. , & MacGregor, D. G. (2004). Risk as analysis and risk as feelings: Some thoughts about affect, reason, risk, and rationality. Risk Analysis: An International Journal, 24(2), 311–322. [DOI] [PubMed] [Google Scholar]
- Sjöberg, L. (2000). Factors in risk perception. Risk analysis, 20(1), 1–12. [PubMed] [Google Scholar]
- Tricco, A. C. , Lillie, E. , Zarin, W. , O'Brien, K. K. , Colquhoun, H. , Levac, D. , Moher, D. , Peters, M. D. J. , Horsley, T. , Weeks, L. , Hempel, S. , Akl, E. A. , Chang, C. , McGowan, J. , Stewart, L. , Hartling, L. , Aldcroft, A. , Wilson, M. G. , Garritty, C. , … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA‐ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- Van, D. , McLaws, M. L. , Crimmins, J. , MacIntyre, C. R. , & Seale, H. (2010). University life and pandemic influenza: Attitudes and intended behaviour of staff and students towards pandemic (H1N1) 2009. BMC Public Health, 10, 130. 10.1186/1471-2458-10-130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vianello, M. , Schnabel, K. , Sriram, N. , & Nosek, B. (2013). Gender differences in implicit and explicit personality traits. Personality and Individual Differences, 55(8), 994–999. 10.1016/j.paid.2013.08.008 [DOI] [Google Scholar]
- Von Gottberg, C. , Krumm, S. , Porzsolt, F. , & Kilian, R. (2016). The analysis of factors affecting municipal employees' willingness to report to work during an influenza pandemic by means of the extended parallel process model (EPPM). BMC Public Health, 16(1), 1–12. 10.1186/s12889-015-2663-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, F. , Wei, J. , Huang, S.‐K. , Lindell, M. K. , Ge, Y. , & Wei, H.‐L. (2018). Public reactions to the 2013 Chinese H7N9 Influenza outbreak: Perceptions of risk, stakeholders, and protective actions. Journal of Risk Research, 21(7), 809–833. 10.1080/13669877.2016.1247377 [DOI] [Google Scholar]
- Williams, L. , Regagliolo, A. , & Rasmussen, S. (2012). Predicting psychological responses to Influenza A, H1N1 (Swine flu): The role of illness perceptions. Psychology, Health and Medicine, 17(4), 383–391. 10.1080/13548506.2011.626564 [DOI] [PubMed] [Google Scholar]
- Wise, T. , Zbozinek, T. D. , Michelini, G. , Hagan, C. C. , & Mobbs, D. (2020). Changes in risk perception and self‐reported protective behaviour during the first week of the COVID‐19 pandemic in the United States. Royal Society Open Science, 7, 200742. 10.1098/rsos.200742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, J. , & Peng, Z. (2015). People at risk of influenza pandemics: The evolution of perception and behavior. PLoS One, 10(12), 1–14. 10.1371/journal.pone.0144868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, S. , & Cho, S. I. (2017). Middle East respiratory syndrome risk perception among students at a university in South Korea, 2015. American Journal of Infection Control, 45(6), e53–e60. 10.1016/j.ajic.2017.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Data Availability Statement
All relevant data are provided within the article or can be retrieved by the original works reviewed.


