Abstract
Objective
The aim of this study was to assess attitudes toward coronavirus disease 2019 (COVID‐19) vaccination and the degree of fear of COVID‐19 among those living with obesity.
Methods
Two samples were recruited for an online survey: one sample was a representative sample of Canadians living with overweight and obesity (n = 1,089), and the second was a convenience sample of individuals recruited from obesity clinical services or patient organizations (n = 980). Respondents completed ratings of their comfort receiving a COVID‐19 vaccination along with the Vaccine Hesitancy Scale and the Fear of COVID‐19 Scale.
Results
Approximately one‐third of respondents, regardless of sample or weight category, were not comfortable receiving a vaccination, and one‐half expressed moderate or greater perceived risks of vaccination. Confidence in vaccinations was extremely low, especially for those in the clinical sample. Fear of COVID‐19 was substantial and predicted attitudes toward vaccination. Females were less comfortable receiving the vaccine and perceived more risks than males.
Conclusions
These results suggest those living with obesity are highly ambivalent about COVID‐19 vaccination. Despite their being at high risk, their confidence in vaccines is very low. Results suggest the need for patient‐centered counseling, with a focus on shared decision‐making to strengthen confidence and reduce perceived risk.
Study Importance.
What is already known?
-
►
Obesity is a risk factor for hospitalization, intensive care unit admission, and mortality from coronavirus disease 2019 (COVID‐19).
-
►
Vaccines have been developed to combat COVID‐19 but are dependent on acceptance by the population; hence, vaccine attitudes and fear play a strong role in achieving herd immunity.
What does this study add?
-
►
Approximately 40% of those living with obesity were not comfortable receiving a COVID‐19 vaccination.
-
►
In the context of significant fear of COVID‐19, especially for those in higher weight categories, confidence in vaccination programs was very low, especially in those pursuing obesity management.
How might these findings change the focus of clinical practice?
-
►
In light of the significant ambivalence concerning COVID‐19 vaccination among those living with obesity, significant attention should be placed on communication skills promoting shared decision‐making to reduce ambivalence and build trust in medical recommendations.
INTRODUCTION
Obesity is a chronic complex disease and a serious risk factor for health and quality of life complications, both short and long term (1). Globally, the prevalence of overweight (BMI > 25 kg/m2) or obesity (BMI > 30 kg/m2) is greater than 20% (2, 3). The prevalence has nearly tripled since 1975 (4), and by 2025, 21% of females and 18% of males are projected to be living with obesity (5, 6). These alarming statistics are mirrored in data from the United States as well as Canada (7, 8).
In December 2019, the first cases of coronavirus disease 2019 (COVID‐19) were confirmed. This virus quickly became a pandemic, spreading worldwide with severe medical, psychological, social, and economic consequences. The link between obesity and COVID‐19 has been extensively evaluated. A systematic review of approximately 400,000 patients revealed that individuals with obesity were at a greater than 46% higher risk for COVID‐19 infection, 113% higher risk for hospitalization, and 74% higher risk for intensive care unit admission and they had a 40% increase in mortality (9). Clearly, COVID‐19 is a threat to individuals living with obesity. To measure threat perception, the Fear of COVID‐19 (FCV) Scale (10) has recently been developed but has not been used specifically in persons with obesity.
Now that vaccines against COVID‐19 have been developed, the task is to distribute them globally. However, in order for a vaccination program to control the virus by herd immunity, it is necessary to have a safe and effective vaccine administered to at least 75% to 85% of the population (11). However, the uptake of vaccination is dependent on the attitudes and concerns of the individual. As such, vaccination is a behavioral issue. The consequence of a delay in vaccination has been seen with other viruses, where there is regional clustering of infections from measles, mumps, and diphtheria (12, 13). Vaccine hesitancy has become a significant public health concern. The World Health Organization ‐ Strategic Advisory Group of Experts on Immunization (WHO‐SAGE) standardized a scale measuring vaccine attitudes (14, 15). The Vaccine Hesitancy Scale (VHS) assesses confidence in vaccines as well as perceived risks (16). This scale was initially developed to assess parents’ attitudes toward vaccinating their children but was adapted to assess personal attitudes toward vaccination (17).
In an attempt to understand the psychosocial and behavioral impact of the COVID‐19 pandemic on individuals living with overweight and obesity, we recently completed a survey‐based study called EPOCH: Evaluation of the Pandemic on Obesity Care and Health.
The EPOCH survey included a broad assessment of the impact of the pandemic on behavior, emotions, and psychosocial functioning of those living with overweight and obesity. Of specific relevance to this paper, we included questions assessing comfort level in receiving a COVID‐19 vaccine, the VHS and the FCV Scale. This paper reports on the results of these measures in those living with overweight and obesity. Given the timeliness of understanding attitudes toward vaccines, we decided to publish this subset of data independent from the entire data collected.
Our main questions in this paper include the following:
How comfortable are individuals living with obesity in receiving a COVID‐19 vaccine?
How confident are individuals living with obesity in vaccine programs in general, and what level of risk do they perceive?
How common are fears of COVID‐19?
To what extent does degree of obesity (overweight, class 1 obesity, class 2 obesity, class 3 obesity) impact attitudes toward vaccination?
What are the correlates of vaccine hesitancy? For this question, we considered selected demographic behavioral and psychological factors.
METHODS
Sample
The EPOCH survey (English only, June 22 to October 9, 2020) was conducted online and involved 2 samples. First, the survey was disseminated widely to medically supervised participants of obesity clinics and organizations throughout Canada and abroad (see online Supporting Information for details). We refer to these respondents as our clinical sample. Second, a survey company (Inet International, Thornhill, Ontario) collected responses from a representative sample of ~1,000 Canadians living with overweight or obesity. We refer to these respondents as our survey sample.
Study measures
This paper focuses specifically on attitudes and concerns about potential vaccination against COVID‐19. The following measures were part of the EPOCH survey and were completed by all respondents. First, respondents were asked to rate their degree of agreement (using a 7‐point Likert scale) with the following 2 statements: “To what extent would you feel comfortable receiving a vaccine against COVID‐19 if it became available?” and “To what extent would you feel comfortable giving your children a vaccine against COVID‐19 if it became available?” Items were written such that the responses ranged from “Not at all” (1), through “Moderately” (4), to “Extremely” (7).
Two validated scales were also administered:
VHS (17): This scale has 9 items that compose 2 subscales: Confidence in Vaccines (7 items) and Perceived Risks of Vaccines (2 items). Responses were coded on a 7‐point Likert scale. Items were written such that the responses ranged from “Not at all” (1), through “Moderately” (4), to “Extremely” (7). We replicated a factor analysis based on this 7‐point ranking and verified the original 2‐factor structure (Cronbach α = 0.96 for Confidence subscale; 0.68 for the Perceived Risks subscale).
FCV Scale (10): This 7‐item rating scale was shown to be reliable and have good construct validity, with a single factor. Unlike the other scales, these items were rated on a 5‐point Likert scale, to preserve the format of the validated scale. Items were written such that the responses ranged from “Strongly disagree” (1), through “Neither agree or disagree” (3), to “Strongly agree” (5). Using our data, we confirmed strong internal consistency of this measure (Cronbach α = 0.87). A factor analysis revealed 2 factors, in contrast to the original paper. Factor 1 (accounting for 39.0% of variance), called the Physiological Fear subscale, was composed of the following items: “My hands become clammy when I think about coronavirus‐19”; “I cannot sleep because I am worrying about getting coronavirus‐19”; and “My heart races or palpitates when I think about getting coronavirus‐19.” This factor accounted for 38.9% of the variance. Factor 2 (33.1% of variance), the Psychological Fear subscale, included the following items: “I am afraid of COVID‐19”; “It makes me uncomfortable to think about COVID‐19”; and “I am afraid of losing my life because of coronavirus‐19.” The item “When watching news and stories about coronavirus‐19 on social media, I become nervous and anxious” loaded almost equally on both factors. Because of the item content, it was assigned to the Psychological Fear subscale.
Data analyses
Descriptive analyses were used to describe the main results. Mean scores on the subscales of the VHS and the FCV Scale as well as the 2 specific questions assessing comfort receiving the COVID‐19 vaccine were reported and compared using within‐subjects ANOVA. Percentage responses to the items were also calculated where appropriate.
Our sample size was sufficient to allow for a comparison between the survey‐based and clinical samples as well as the category of weight (overweight, class 1 obesity, class 2 obesity, and class 3 obesity). These comparisons were conducted using a 2‐factor ANOVA, with one 2 level factor (survey and clinical) and one 4 level factor (overweight, class 1 obesity, class 2 obesity, class 3 obesity).
Finally, we conducted a regression analysis to explore correlates for vaccine hesitancy. Separate regression equations were calculated for the Confidence and Perceived Risks subscales of the VHS and also for the rating of degree of comfort receiving a COVID‐19 vaccination. For each regression equation, we conducted a stepwise analysis. Demographic factors were entered as step 1, then behavioral factors were entered as step 2, and finally, psychological factors were entered as step 3 in the analysis.
A full analysis of the EPOCH survey database will be published elsewhere.
RESULTS
Respondents
A total of 2,078 respondents completed the survey. Of these, 1,098 were from the representative Canadian survey (9.4% [103] with overweight, 56.0% [615] with class 1 obesity, 19.5% [214] with class 2 obesity, and 15.1% [166] with class 3 obesity) and 980 from the clinical survey (9.3% [91] with overweight, 20.4% [200] with class 1 obesity, 20.8% [204] with class 2 obesity, and 49.5% [485] with class 3 obesity). Detailed analyses of the demographic data will be published in a separate paper. Nonetheless, it is notable that there were strong differences between the samples. The clinical sample was heavier than the survey sample, with almost 50% of the sample having BMI above 40 and more than 70% of the sample having BMI above 35 (only ~35% of the survey sample had BMI above 35). Expectedly, the clinical sample was primarily female (82.5%), whereas the survey sample was balanced (50.2% female). In addition, almost none of the survey sample had undergone bariatric surgery, whereas more than 20% of the clinical sample had had bariatric surgery, and another 20% were awaiting or considering surgery. Although we attempted to recruit an international sample of clinical respondents, only 3.8% were from the US and 1.2% from other countries.
Attitudes toward vaccination
Figure 1A portrays the data on level of comfort to receive a COVID‐19 vaccination as well as on the 2 subscales of the VHS. On average, respondents were moderately comfortable receiving a COVID‐19 vaccination and more comfortable receiving the vaccine themselves than with their child receiving the vaccine (p < 0.001). Strikingly, the mean score on the Confidence subscale of the VHS was very low, significantly lower than any other measure. Furthermore, Perceived Risks scores were in the low to moderate range (higher than the Confidence subscale, p < 0.001, but lower than the COVID‐19 scales, all p < 0.001).
FIGURE 1.
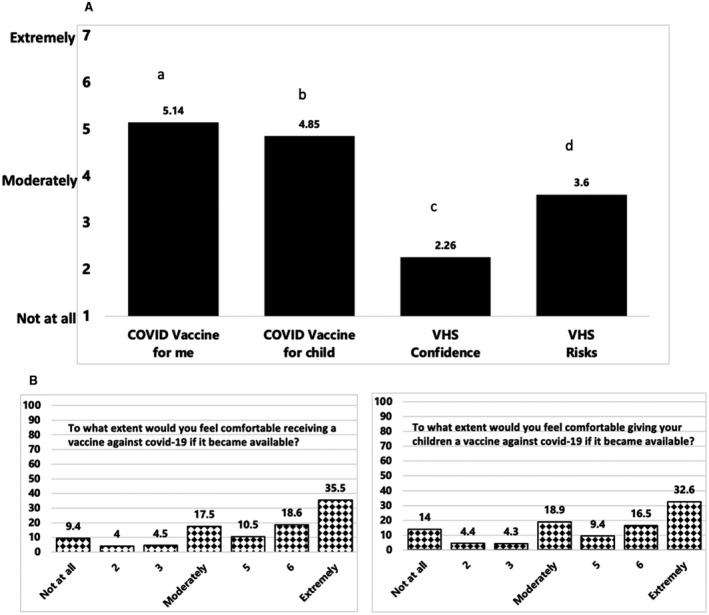
(A) Mean scores on items assessing comfort level in receiving a COVID‐19 vaccine (self and child), as well as mean scores on the Confidence and Perceived Risks subscales of the Vaccine Hesitancy Scale. a,b,c,dWhere letters differ, there are significant differences between means. (B) Percentage breakdown to questions concerning comfort level receiving a COVID‐19 vaccination.
Figure 1B portrays the percentage response to each of the scale ratings for the comfort receiving a vaccine for oneself and one’s child. Only just over half of the sample (54.1%) scored high (6 or 7) on the personal comfort scale, where 34.5% scored low on this scale (4 or less). Comfort with one’s child receiving a COVID‐19 vaccination was slightly lower. Just under half (49.1%) scored 6 or above on this scale, and 41.5% scored low (4 or less).
Given that the mean scores on the VHS were so low, we examined the distribution of scores on each of the scale items (Figure 2). These results were striking. On the Confidence subscale, the large majority of respondents reported very low confidence. The majority of respondents scored low (4 or less) on the following items: “Vaccines are effective” (91.3% low confidence); “Vaccines are important for my health” (92.4% low confidence); “Being vaccinated is important for the health of others in my community” (92.7% low confidence); “All vaccines offered by the government programme in my community are beneficial” (89.4% low confidence); “The information I receive about vaccines from the vaccine programme is reliable and trustworthy” (85.7% low confidence); “Getting vaccines is a good way to protect myself from disease” (91.5% low confidence); and “Generally, I do what my doctor or health care provider recommends about vaccines” (90.2% low confidence). Regarding the Perceived Risks subscale, the majority of respondents perceived some risk, defined as 4 or above: “New vaccines carry more risks than older versions” (59.0%); and “I am concerned about serious side effects of vaccines” (51.0%).
FIGURE 2.
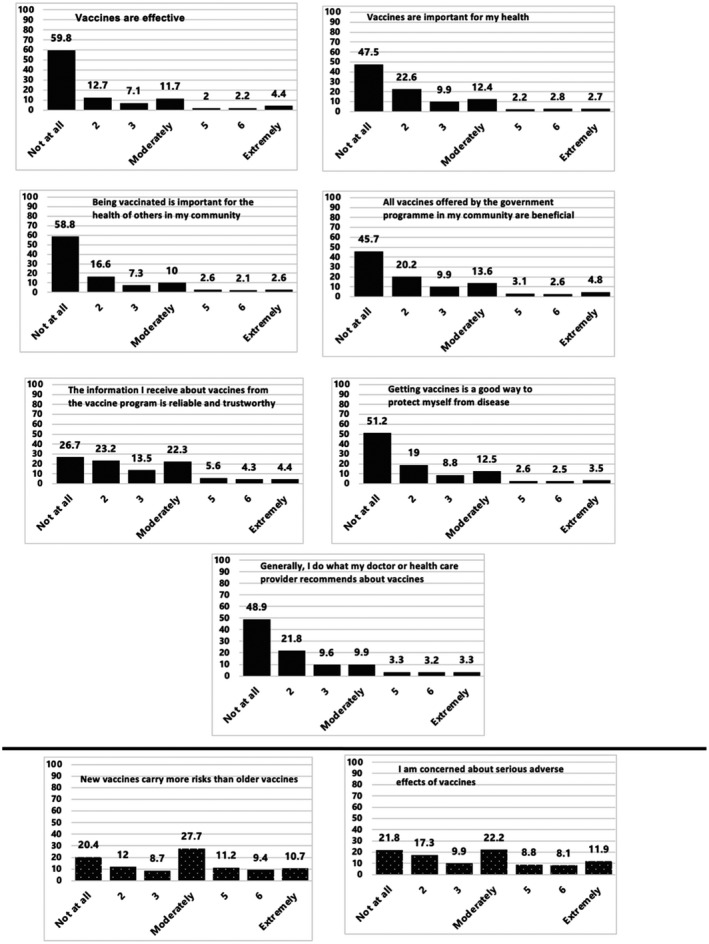
Items of the Vaccine Hesitancy Scale. Above the solid line are the items from the Confidence subscale. Below the solid line are the items from the Perceived Risks subscale.
Next, we compared the mean scores on vaccine attitude items between samples (clinical and survey) and between those in different weight categories using a 2‐factor ANOVA. For the scales assessing comfort receiving a COVID‐19 vaccine for oneself or one’s child, there were no differences based on the clinical versus survey samples nor were there any differences between those in the different weight categories, and there was no interaction between these 2 factors (all p values nonsignificant [ns]). The same lack of differences between survey and clinical samples and among weight categories or the interaction of the 2 factors occurred for Perceived Risks (all p values ns). However, for the Confidence subscale of the VHS survey, respondents reported higher confidence than the clinical sample (mean = 2.38 vs. 2.14, p < 0.001). Follow‐up analyses of the item scores showed lower confidence for the clinical sample on the following items: “Vaccines are important for my health” (Survey = 2.22, Clinical = 1.91, p < 0.001); “Vaccines are effective” (Survey = 2.31, Clinical = 2.04, p < 0.001); “Being vaccinated is important for the health of others in my community” (Survey = 2.12, Clinical = 1.82, p < 0.001); “All vaccines offered by the government programme in my community are beneficial” (Survey = 2.45, Clinical = 2.25, p < 0.018); “Getting vaccines is a good way to protect myself from disease” (Survey = 2.29, Clinical = 2.06, p < 0.002); and “Generally, I do what my doctor or health care provider recommends about vaccines” (Survey = 2.34, Clinical = 2.04, p < 0.001). There were no differences in scores on the Confidence subscale (either total or item scores) among weight categories and no interaction effects between survey/clinical and weight category (all p values ns).
FCV Scale
The results from the FCV Scale are shown in Figure 3. Mean scores were generally low to moderate for each item and the mean of the scale. However, the score on the item “I am afraid of COVID‐19” was elevated. On this item, 65.2% of respondents reported either “Agree” or “Strongly agree.” In addition, a substantial proportion of respondents reported “Agree” or “Strongly agree” with the following items: “It makes me uncomfortable to think about COVID‐19” (38.2%); “I am afraid of losing my life because of coronavirus‐19” (37.5%); and “When watching news and stories about coronavirus‐19 on social media, I become nervous and anxious” (32.2%).
FIGURE 3.
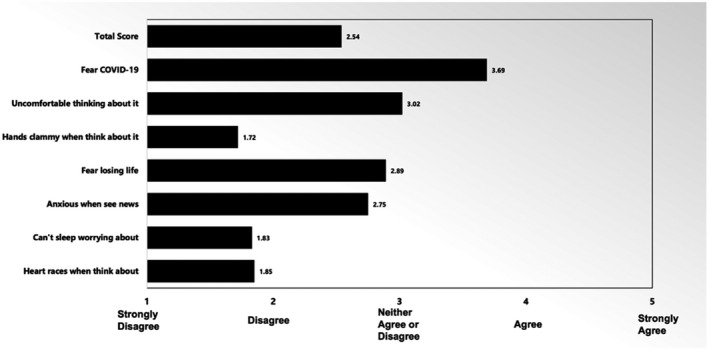
Mean responses to the Fear of COVID‐19 Scale, total score, and mean item scores.
Comparisons based on the factor scores are presented in Figure 3. The Psychological Fear score was significantly higher than the Physiological Fear score (3.09 [1.01] vs. 1.80 [0.88], p < 0.001). We recoded these scale scores into low (response mean 2 or less) or high (4 and higher). Only 4.2% of respondents scored high (4 or 5 on the 5‐point scale) on the Physiological Fear subscale, whereas 55.9% of respondents scored high on the Psychological Fear subscale.
Next, we compared the Physiological and Psychological Fear subscale scores between the survey versus clinical samples and for those in the different weight categories using a 2‐factor ANOVA as described here previously. Regarding survey compared with clinical samples, we found that the clinical sample scored significantly higher than the survey sample on the Psychological scale (Survey = 2.97, Clinical = 3.23, p < 0.001) There was no difference between groups on the Physiological scale (ns).
Results of analyses comparing fear scores between the different weight categories showed significant differences based on weight status for both the Physiological (p = 002) and the Psychological Fear subscale (p = 0.001) scores. These differences are shown in Figure 4. There was a clear pattern whereby those in higher weight categories expressed greater fear scores.
FIGURE 4.
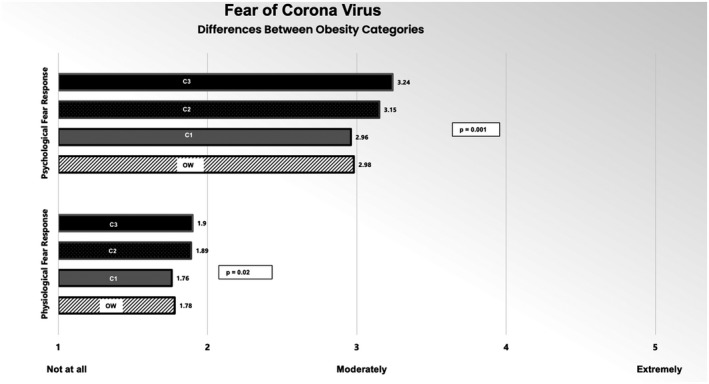
Significant differences between weight statuses for the Fear of COVID‐19 Scale; Physiological Fear and Psychological Fear subscales. C1, class 1 obesity; C2, class 2 obesity; C3, class 3 obesity; OW, overweight.
Finally, we were interested in understanding the relationship between fear of COVID‐19 and vaccine attitudes. Regression equations were calculated using the Physiological and Psychological Fear subscales to predict VHS Confidence in Vaccines and Perceived Risks of Vaccines scores as well as comfort receiving the COVID‐19 vaccination. Because there were differences in fear scores between survey and clinical samples as well as among weight categories, we used a stepwise regression model whereby sample and weight category were entered as step 1 and the fear scales as step 2.
Results indicated that fear was a predictor of vaccine attitudes for all dependent measures. Considering the Psychological Fear subscale, higher scores predicted higher Perceived Risks of Vaccines scores (Beta = 0.112, p < 0.001), lower Confidence in Vaccines scores (Beta = −0.172, p < 0.001), and higher comfort receiving the COVID‐19 vaccine scores (Beta = 0.115, p < 0.001).
For the Physiological Fear subscale, higher scores were associated with higher scores on the Confidence in Vaccines subscale (Beta = 0.047, p = 0.032) and higher scores on the Perceived Risks of Vaccines subscale (Beta = 0.166, p < 0.001). The Physiological Fear subscale did not predict the score on comfort receiving the COVID‐19 vaccine.
Correlates of vaccine hesitancy
Given that EPOCH was a broad survey of the experience of the pandemic by those living with overweight and obesity, we collected a number of additional measures beyond those focusing on vaccination and fear of the virus. We selected specific demographic, behavioral, and mental health factors to examine how they relate to vaccine attitudes. Regarding demographic factors, we included age, gender, geographic location, number of people living in a household, comorbidities, and history of bariatric surgery. Regarding behavioral factors, the EPOCH survey included items assessing engagement in social distancing, eating changes and challenges, activity, substance use, participation in flu vaccination, and access to medical care during the pandemic. Finally, regarding mental health, we included weight stigma and scores on the General Anxiety Disorder scale (18) and the Center for Epidemiologic Studies‐Depression (CES‐D) depression screening scale (19). To control for compounding error rates, we used a stepwise regression analysis for each of the vaccine attitudes scores (Confidence and Perceived Risks subscales of the VHS as well as extent of comfort receiving a COVID‐19 vaccine). Specifically, we entered demographic factors on step 1, behavioral factors on step 2, and mental health factors on step 3. We report on the significance and percentage of variance accounted for at each step of the regression and also report the Beta weight and p values of any significant predictor at that step. Results are shown in Table 1.
TABLE 1.
Results of regression equations predicting vaccine attitudes
| Comfort receiving COVID‐19 vaccine | VHS: confidence in vaccines | VHS: perceived risks of vaccines | |||||||
|---|---|---|---|---|---|---|---|---|---|
| p | % Var | Beta | p | % Var | Beta | p | % Var | Beta | |
| Demographics (step 1) | <0.001 | 2.9% | — | 0.001 | 1.4% | — | <0.001 | 1.9% | — |
| Gender | 0.001 | — | −0.087 | — | — | — | 0.001 | — | 0.085 |
| No comorbidities | 0.034 | — | −0.055 | 0.001 | — | 0.088 | — | — | — |
| Number in household | — | — | — | — | — | — | 0.001 | — | 0.089 |
| Behavioral factors (step 2) | <0.001 | 14.0% | — | <0.001 | 21.0% | — | <0.001 | 7.2% | — |
| Social distance | <0.001 | — | 0.143 | <0.001 | — | 0.187 | 0.021 | — | 0.069 |
| Flu vaccine | <0.001 | — | −0.333 | <0.001 | — | 0.397 | <0.001 | — | 0.227 |
| Increased smoking | — | — | — | 0.002 | — | 0.077 | 0.042 | — | 0.054 |
| Increased cannabis | — | — | — | — | — | — | 0.046 | — | 0.056 |
| Challenged in healthy eating | — | — | — | — | — | — | <0.001 | — | 0.131 |
| Psychological factors (step 3) | 0.042 | 0.5% | — | 0.018 | 5.7% | — | 0.007 | 0.7% | — |
| CES‐D | 0.021 | — | −0.096 | 0.004 | — | 0.166 | — | — | — |
Numbers in bold indicate statistically significant predictors.
CES‐D, Center for Epidemiologic Studies‐Depression; COVID‐19, coronavirus disease 2019; VHS, Vaccine Hesitancy Scale.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Regarding being comfortable receiving a COVID‐19 vaccination, females were more comfortable than males, as were those with comorbidities. Those less likely to follow social distancing were more comfortable receiving the COVID‐19 vaccination, as were those who obtained a flu vaccination. Finally, those with higher scores on the CES‐D depression screening scale were less comfortable receiving the COVID‐19 vaccination.
Next, considering the Confidence in Vaccines subscale, those with comorbidities had lower confidence scores. Those who resist social distancing rules scored higher on the Confidence subscale, and those who received a flu vaccination scored lower on the Confidence subscale. Those reporting increased cannabis use during the pandemic reported higher Confidence scores. Finally, those with higher depression scores reported greater Confidence scores.
Finally, considering the Perceived Risks of Vaccines subscale, females reported higher risks, as did those with a greater number of people in their household. Those less likely to social distance had higher risk scores, as did those who did not receive a flu vaccination. Those who struggled with healthy behaviors, such as increased smoking, increased cannabis use, and increased challenges in eating healthy, also scored higher on the Perceived Risks subscale.
DISCUSSION
With the availability of a COVID‐19 vaccination program, vaccine attitudes have become critical. Recent general population surveys have suggested that many people are reluctant to be vaccinated. In the US, 25% to 50% of Americans were willing to accept a vaccination against COVID‐19 when available (20, 21). Data from Statistics Canada in June 2020 revealed that 57.5% of Canadians were very likely to obtain a COVID‐19 vaccine when available, and an additional 19.0% were somewhat likely to get vaccinated. Approximately 5.1% were somewhat unlikely, 9.0% were very unlikely, and 9.4% remained unsure whether they would accept a COVID‐19 vaccination when available (22). An Angus Reid poll published on December 14, 2020, revealed that 48% of Canadians would receive a vaccination as soon as available, 31% would accept a vaccine after a wait, 14% would not accept a vaccine, and 7% remained unsure (23). Attitudes among those living with obesity are particularly important to understand, because obesity is a significant risk factor for poorer COVID‐19 outcomes and is associated with conditions that themselves are independent risk factors for severe COVID‐19 (24, 25, 26, 27).
Our survey results from those living with overweight and obesity are striking. Approximately one‐third (34.5%) reported low comfort in receiving the COVID‐19 vaccination, with lower comfort ratings regarding having one’s child vaccinated. These results were independent of degree of obesity or of being a survey or clinical respondent. Comfort levels were positively associated with being male, having more comorbidities, having lower depression scores, as well as not practicing social distancing and past acceptance of flu vaccinations. These results require replication but suggest that specific subgroups (e.g., females, those with no comorbidities or avoiding flu vaccinations, or those in emotional distress) might benefit from counseling based on communication and shared decision‐making interventions. Although we intended to recruit a multinational sample of clinical respondents, we were not successful, recruiting only 3.8% of respondents from the US. In a post hoc analysis comparing the mean comfort score for receiving a vaccine between the US and Canadian respondents, the US sample was more confident (mean = 5.84) compared with the Canadian sample (mean = 5.04, p < 0.016). One needs to be cautious in interpreting this difference because of the small sample size, but this finding might suggest regional differences in vaccine attitudes.
Integral to the success of a vaccination program is one’s confidence related to a vaccine. In our survey, confidence in vaccinations in general was extremely low, including perceived vaccine efficacy, their role in preserving good health, trust in government vaccination programs, and confidence in their health care practitioners’ recommendations. These may be challenging attitudes to alter and again suggest the need for effective communication interventions.
Respondents participating in clinical obesity management programs were less confident in vaccinations than the general survey respondents. This may reflect greater skepticism or disillusionment related to the weight bias experienced from the medical system by most individuals with obesity (28). It may be that a certain level of trust is required in this rapidly changing pandemic and that these respondents are less trusting relative to the survey sample. Further research attempting to understand the drivers of vaccine confidence is needed. Respondents with higher physiologic COVID‐19 fear response, those with no comorbidities, those who were less likely to social distance, those who avoided a flu vaccination, and those who reported higher levels of depression and substance use reported greater confidence, although overall confidence scores were still low. These results clearly indicate a need for communication strategies that assess confidence, identify drivers of low confidence, and encourage cognitive reframing using shared decision‐making.
Risk perception is also an integral aspect of vaccination attitudes. More than 50% of our respondents considered newer vaccines less safe and to carry more serious risks than older vaccines. Perceived risk was associated with avoidance of flu vaccination, substance use, and less social distancing. Women and those who struggled with healthy eating also reported higher perceived risk.
At least 65% of all respondents acknowledged moderate to severe fear of COVID‐19 infection; fear response was more psychological than physiological. Many respondents strongly related to a fear of dying of this infection as well as a level of anxiety thinking about or being exposed to information related to COVID‐19. The greater one’s weight the more intense the psychological fear reported. This may be due to a heightened knowledge about the association between obesity and increased susceptibility, severity, hospitalization, intensive care unit admissions, and mortality from the COVID‐19 infection (29, 30). Further, respondents recruited through clinical obesity initiatives experienced significantly higher levels of fear compared with the general survey respondents. This may be due to increased exposure to the warnings associated with this infection for people living with obesity. Finally, those with heightened levels of fear reported increased comfort in receiving a COVID‐19 vaccination but struggled with increased perceived risk of the vaccine.
Published literature suggests that several correlates exist that relate to COVID‐19 vaccine hesitancy. In a US study (21), there was a higher level of refusal for vaccination in women. Further, those concerned about contracting COVID‐19 infection were less likely to reject vaccination. Higher levels of comfort and confidence were associated to acceptance of a COVID‐19 vaccine (21). An Australian study reported that women, those with low perceived risk of COVID‐19, and those less trustworthy of vaccination programs were more likely to be resistant of vaccination (31). In our survey, women were less comfortable receiving a vaccine and more fearful of risks, consistent with previous research. Fear of contracting COVID‐19 was associated with greater perceived risks. Interestingly, on the Psychological Fear subscale, greater fear predicted lower confidence in vaccinations but greater comfort in the COVID‐19 vaccine. Clearly, further research is needed to better understand the relationships between fear and intentions.
Considering the results of this survey, it is critical to obtain a fulsome understanding of the attitudes and concerns of those living with obesity as the global vaccination program continues. These individuals are at greater risk if they avoid vaccination and present with significant issues concerning their confidence and comfort in being vaccinated during this pandemic. Those in clinical care may be an especially important group, given that they expressed greater concerns and lower confidence than a comparison representative survey sample. Patient‐centered communication and shared decision‐making interventions are likely to prove essential in overcoming the risks of this pandemic.
Limitations of the study include that it is a single‐time cross‐sectional assessment during the first wave of the pandemic. All of the scales reported in this paper were administered as part of EPOCH between June 22 and October 9, 2020. We are unable to comment on changes in attitudes and concerns over time. In addition, when the survey was undertaken, availability of the vaccine was not yet accessible. Now that vaccines are currently available, vaccine fears and attitudes may be further affected as well. In addition, the vast majority of data (including all of the survey respondents) are Canadian, so global generalization is not possible. Finally, we did not include a comparison sample of individuals not living with obesity. However, general survey results reported in the media suggest that the general population is more receptive to vaccination than those living with obesity, particularly those representative of the clinical sample.
Among the strengths of this study are the fact that we sampled both the general population as well as those seeking help for obesity. Further, our sample size is very large, and we have strong representation from those in the high‐BMI category groups. Furthermore, we used validated measurement instruments in an attempt to increase the veracity of the self‐reported data.
The COVID‐19 pandemic has had devastating consequences worldwide for so many individuals. Those living with overweight and obesity are at significantly increased risk for worse outcomes, including increased morbidity and mortality. Despite this, there was low to moderate fear of COVID‐19. This gap in comfort and confidence in the vaccine along with increased understanding of risk must be narrowed such that a successful vaccination program along with other infection control measures can help eradicate this coronavirus. Health authorities must work aggressively to continue to inform and educate about the advantages of a vaccine program while building confidence by transparent and trustworthy communication.
Ethical approval
This study was reviewed and approved by Veritas Institutional Review Board review panel: 16576‐09:19:5811‐06‐2020.
CONFLICT OF INTEREST
The authors declared no conflict of interest.
AUTHOR CONTRIBUTIONS
MV and SG jointly designed this survey. SG obtained funding for the survey and solicited input from clinical services and organization for recruitment. MV conducted the data analysis and prepared the first draft of the manuscript. MV and SG edited the manuscript and approved the manuscript for publication.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
We would like to acknowledge our medical colleagues who promoted the study within their clinical services. We would also like to acknowledge the respondents, who willingly completed this extensive survey.
REFERENCES
- 1. Prospective Studies Collaboration ; Whitlock G, Lewington S, Sherliker P, et al. Body‐mass index and cause‐specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–1096. doi: 10.1016/s0140-6736(09)60318-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lighter J, Phillips M, Hochman S, et al. Obesity in patients younger than 60 years is a risk factor for COVID‐19 hospital admission. Clin Infect Dis. 2020;71:896‐897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. NCD Risk Factor Collaboration (NCD‐RisC). Rising rural body‐mass index is the main driver of the global obesity epidemic in adults. Nature. 2019;569:260‐264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization . Obesity and overweight. Updated June 9, 2021. Accessed December 2, 2020. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- 5. NCD Risk Factor Collaboration (NCD‐RisC) . Trends in adult body‐mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population‐based measurement studies with 19·2 million participants. Lancet. 2016;387:1377–1396. doi: 10.1016/s0140-6736(16)30054-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. NCD Risk Factor Collaboration (NCD‐RisC) . Worldwide trends in body‐mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled snalysis of 2416 population‐based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017‐2018. NCHS Data Brief, no. 360. National Center for Health Statistics; 2020. [PubMed]
- 8. Statistics Canada . Health characteristics, annual estimates. Table 13‐10‐0096‐01. 2019. Accessed December 2, 2020. 10.25318/1310009601-eng. [DOI]
- 9. Popkin BM, Du S, Green WD, et al. Individuals with obesity and COVID‐19: a global perspective on the epidemiology and biological relationships. Obes Rev. 2020;21:e13128. doi: 10.1111/obr.13128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ahorsu DK, Lin C‐Y, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID‐19 scale: development and initial validation [published online March 27, 2020]. Int J Ment Health Addict. 2020. doi: 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Anderson RM, Vegvari C, Truscott J, Collyer BS. Challenges in creating herd immunity to SARS‐CoV‐2 infection by mass vaccination. Lancet. 2020;396:1614‐1616. doi: 10.1016/s0140-6736(20)32318-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Luyten J, Beutels P. The social value of vaccination programs: beyond cost‐effectiveness. Health Aff. 2016;35:212‐218. doi: 10.1377/hlthaff.2015.1088 [DOI] [PubMed] [Google Scholar]
- 13. Coombes R. Europe steps up action against vaccine hesitancy as measles outbreaks continue. BMJ. 2017;16:j4803. doi: 10.1136/bmj.j4803 [DOI] [PubMed] [Google Scholar]
- 14. Berger BE, Omer SB. Could the United States experience rubella outbreaks as a result of vaccine refusal and disease importation? Hum Vaccin. 2010;6:1016‐1020. [DOI] [PubMed] [Google Scholar]
- 15. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- 16. Larson HJ, Jarrett C, Schulz WS, et al. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33:4165‐4175. doi: 10.1016/j.vaccine.2015.04.037 [DOI] [PubMed] [Google Scholar]
- 17. Luyten J, Bruyneel L, van Hoek AJ. Assessing vaccine hesitancy in the UK population using a generalized vaccine hesitancy survey instrument. Vaccine. 2019;37:2494‐2501. doi: 10.1016/j.vaccine.2019.03.041 [DOI] [PubMed] [Google Scholar]
- 18. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD‐7. Arch Intern Med. 2006;166:1092‐1097. [DOI] [PubMed] [Google Scholar]
- 19. Radloff LS. The CES‐D scale: a self‐report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385‐401. [Google Scholar]
- 20. Associated Press. Half of Americans would get a COVID‐19 vaccine, AP‐NORC poll finds. NBC News. May 27, 2020. https://www.nbcnews.com/health/health‐news/half‐americans‐would‐get‐covid‐19‐vaccine‐ap‐norc‐poll‐n1215606. [Google Scholar]
- 21. Callaghan T, Moghtaderi A, Lueck JA, et al. Correlates and disparities of intention to vaccinate against COVID‐19. Soc Sci Med. 2021;272. 113638. doi: 10.1016/j.socscimed.2020.113638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Frank K, Arim R; Statistics Canada. Canadians’ willingness to get a COVID‐19 vaccine when one becomes available: what role does trust play?. Published July 7, 2020. https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00043-eng.htm
- 23. Angus Reid Institute . More Canadians willing to roll up their sleeves right away as national COVID‐19 vaccine rollout begins. Published December 14, 2020. Accessed March 14, 2021. https://angusreid.org/canada-covid-vaccine-december/
- 24. Yang J, Zheng YA, Gou XI, et al. Prevalence of comorbidities and its effects in patients infected with SARS‐CoV‐2: a systematic review and meta‐analysis. Int J Infect Dis. 2020;94:91‐95. doi: 10.1016/j.ijid.2020.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID‐19 cases: A systematic literature review and meta‐analysis. J Infect. 2020;81:e16‐e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Huang R, Zhu LI, Xue L, et al. Clinical findings of patients with coronavirus disease 2019 in Jiangsu province, China: a retrospective, multi‐center study. PLoS Negl Trop Dis. 2020;14:e0008280. doi: 10.1371/journal.pntd.0008280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid‐19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;22:m1985. doi: 10.1136/bmj.m1985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17:941‐964. doi: 10.1038/oby.2008.636 [DOI] [PubMed] [Google Scholar]
- 29. Klang E, Kassim G, Soffer S, Freeman R, Levin MA, Reich DL. Severe obesity as an independent risk factor for COVID‐19 mortality in hospitalized patients younger than 50. Obesity. 2020;28:1595‐1599. doi: 10.1002/oby.22913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Naveed Sattar, McInnes IB, McMurray JJV. Obesity is a risk factor for severe COVID‐19 infection. Circulation. 2020;142:4‐6. doi: 10.1161/circulationaha.120.047659 [DOI] [PubMed] [Google Scholar]
- 31. Edwards B, Biddle N, Gray M, Sollis K. COVID‐19 vaccine hesitancy and resistance: correlates in a nationally representative longitudinal survey of the Australian population. PLoS One. 2021;16:e0248892. doi: 10.1371/journal.pone.0248892 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


