INTRODUCTION
The COVID‐19 pandemic disrupted medical education and challenged medical educators to transform learning from traditional in‐person to virtual. 1 Aquifer, a nonprofit organization that specializes in web‐based healthcare education, responded to this crisis by offering access to its courses to health professions schools at no cost from mid‐March to June 2020. At the end of this period, programs could continue their access via paid subscription.
Aquifer Geriatrics (AG), the national online curriculum endorsed by the American Geriatrics Society, began as web‐Geriatrics Education Modules (GEMs), a series of online modules created by the geriatrics educators' community through funding by the Reynolds Foundation. 2 AG currently hosts 27 evidence‐based, peer‐reviewed case‐based modules and aims to standardize geriatrics education and bridge curricular gaps. 3 They are designed for diverse learners including medical students, residents, fellows, and interprofessional trainees, and to use in a variety of pedagogies such as self‐directed learning, flipped classrooms, and “bootcamp” sessions.
Our aim is to evaluate the impact of this unique program offered during the pandemic by analyzing the change in the number of AG case completions around the time of the pandemic, as well as overall change in the number and type of health profession programs having access to AG.
METHODS
We computed the monthly total AG case completions by all learners and averaged them for three time periods chosen for comparison: Prepandemic (July 2019–February 2020), grant‐funded (April 2020–June 2020), and subscription‐based access (July 2020–December 2020). We left March 2020 out because it was a month of transition. Additionally, we analyzed the change in the subscribing programs (type and number) from academic year (AY) 2019–2020 to AY 2020–2021.
RESULTS
A total of 489 programs, including existing subscribers, gained access to AG cases, with a staggering 83,800 case completions by learners during the grant‐funded period of the pandemic. The number of subscribing programs to AG increased from 52 in AY 2019–2020 to 219 in AY 2020–2021; there was an increase in subscriptions from all program types including allopathic medical (MD), osteopathic medical (DO), nurse practitioner (NP), physician assistant (PA), and residency/fellowship programs. This increase in programs was most remarkable for PA (2267%), NP (400%), DO (325%), and MD (248%) programs. (Table S1) The average monthly AG case completions increased from 1372 in the prepandemic period to 27,933 in the grant‐funded period; it declined to 7303 in the subscription‐based access period that followed (Figure 1) Average learner satisfaction rating after completion of AG cases increased from 4.24 (out of 5) in the prepandemic period to 4.31 in the grant‐funded period to 4.45 in the subscription‐based access period.
FIGURE 1.
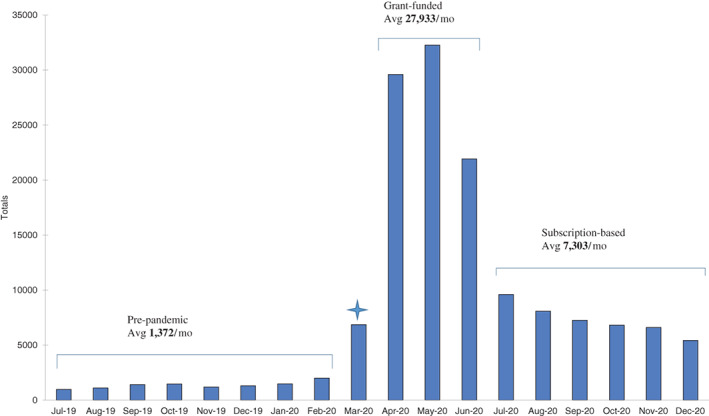
Monthly Aquifer Geriatrics case completions by learners from July 2019 to December 2020
DISCUSSION
The disruption in medical education due to the COVID‐19 pandemic was transformational and led to curricular innovation. Training programs around the country had the opportunity to access AG to fill the curricular void created by shifts in the learning environment. While increased access by programs was not unexpected, there was an exponential 20‐fold uptick in monthly case completion by learners during the grant‐funded period.
Even after completion of grant support, many programs continued their access via subscription, likely from having perceived the educational value of AG cases in their curricula. The pandemic‐related grant support proved to be a catalyst in expanding access to programs nationally, with a 321% increase in subscribing programs from AY 2019–2020 to AY 2020–2021 (Table S1). Average monthly case completions increased by 432% from the prepandemic period in AY 2019–2020 to AY 2020–2021. This indicates not only an increase in subscriber base, but an increase in case use within each subscribing program. Moreover, overall learner satisfaction continued to rise steadily and remain high.
The expansion of AG to disciplines outside of the MD programs was very successful, with the greatest adopters being the PA and NP programs. This emphasizes the relevance of interprofessional principles of geriatric care and the potential for such online curricula to develop the workforce of “little g” geriatrics health professionals with competence in evidence‐based management of geriatric syndromes. 4
Although we have data on the number of subscribing programs and case completions, we lack data on knowledge attainment and retention. On an individual program level, educators and learners will be able to assess knowledge acquisition and identify gaps in learning through use of the recently added self‐assessment questions.
In conclusion, when many institutions transitioned to online learning during the height of the pandemic, AG came to the rescue and provided an engaging way to fill the void of in‐person teaching. Even after the end of the grant‐based access, many programs retained access to AG, indicating that AG cases enriched the educational initiatives and fulfilled learning objectives of training programs nationally across disciplines during this challenging time.
CONFLICT OF INTEREST
All authors serve on the Aquifer Consortium and receive a nominal annual honorarium for their services. Lauren J. Gleason is supported by Health Resources and Services Administration (HRSA) (grant K01HP39479).
AUTHOR CONTRIBUTIONS
All authors contributed in study concept and design, data acquisition, analysis and interpretation, and preparation of manuscript.
SPONSOR'S ROLE
None.
Supporting information
TABLE S1 Number of program subscriptions to aquifer geriatrics by health profession
ACKNOWLEDGMENTS
Funding informationNone
Funding information None
REFERENCES
- 1. Lucey CR, Johnston SC. The transformational effects of COVID‐19 on medical education. JAMA. 2020;324(11):1033‐1034. 10.1001/jama.2020.14136. [DOI] [PubMed] [Google Scholar]
- 2. Ramaswamy R, Leipzig RM, Howe CL, Sauvigne K, Usiak C, Soriano RP. The portal of geriatrics online education: a 21st‐century resource for teaching geriatrics. J Am Geriatr Soc. 2015;63(2):335‐340. 10.1111/jgs.13246. [DOI] [PubMed] [Google Scholar]
- 3. Sehgal M, Syed Q, Callahan KE, et al. Introducing aquifer geriatrics, the American Geriatrics Society National Online Curriculum. J Am Geriatr Soc. 2019;67(4):811‐817. 10.1111/jgs.15813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Callahan KE, Tumosa N, Leipzig RM. Big “G” and little “g” geriatrics education for physicians. J Am Geriatr Soc. 2017;65(10):2313‐2317. 10.1111/jgs.14996. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
TABLE S1 Number of program subscriptions to aquifer geriatrics by health profession


