Abstract
Background
Changes in relationships, sleep rhythms, and physical activity caused by school closures instituted to curb the spread of COVID‐19 influenced children’s mental health. We explored changes in children’s daily life and effects on their mental health during school closures.
Methods
Participants included elementary and junior high school students 9 years of age and older seen in the outpatient clinic during school closures and were required to complete the Japanese version of WHO Five Well‐Being Index (WHO‐5‐J). The results were compared with those of students seen after schools reopened.
Results
Participants included 78 students in the school closure group and 113 in the school reopening group. Although those in the closure group devoted more time to family and sleep, their sleep rhythms, eating habits, and physical activities were disrupted. Although there were no significant differences between the two groups in total WHO‐5‐J scores, single WHO‐5‐J items such as activity and vigor and interest were significantly worse and rest was significantly better in the school closure group.
Conclusion
Although school closures resulted in elementary and junior high school students spending more time with family and sleeping, their sleep rhythms, eating habits, and physical activities were disrupted. As the children’s living environment changed, they felt less active and vigorous and had difficulty finding things that interested them. However, their sleep improved and overall, the number of children with potential mental health problems did not change.
Keywords: child, COVID‐19, mental health, school closure
In February 2020, the Japanese Government ordered the closure of all schools in the country from March 2 until the end of spring break in an effort to prevent the spread of coronavirus disease 2019 (COVID‐19). Following that order, elementary and junior high school students in eastern Tochigi Prefecture, the area served by our hospital, stopped going to school on March 2. In early April, elementary and junior high schools in eastern Tochigi Prefecture began the new school year as usual. However, on April 7, the Japanese Government declared a state of emergency in seven prefectures, and schools were closed again indefinitely only a few days after opening. On April 16, the Japanese Government expanded the scope of the state of emergency to the entire country. Therefore, it was decided that elementary and junior high schools would remain closed until early May, and students and their families were directed to avoid leaving their homes at all times except in case of necessity. Thereafter, school reopening was postponed several times while monitoring the extent of the spread of infection in the area. Schools finally reopened and resumed their usual schedules on June 1, approximately 3 months after closing.
It is known that children’s mental health is influenced by factors such as relationships with friends 1 , 2 , sleep rhythms 3 , physical activity 4 , use of digital media 5 , 6 etc. Therefore, it has been conjectured that changes in these factors caused by the school closures would influence children’s mental health in some way. Therefore, we examined elementary and junior high school students who visited our outpatient clinic for scheduled appointments, to investigate what changes they experienced in their daily life during school closure and what effect these changes had on their mental health.
Methods
Patients
We use the term “school closure” to indicate the interval from March 1 to May 31, 2020, although there were two or three days in April when usual school activities resumed. The subjects of this study were elementary and junior high school students 9 years and older who had appointments at the Haga Red Cross Hospital Pediatrics Department in May 2020, after schools had been closed for approximately two months. The control subjects were elementary and junior high school students 9 years and older who had appointments at the same clinic in October 2020, 4 months after schools had reopened. In October, although disease prevention measures such as mask wearing and social distancing continued in eastern Tochigi Prefecture, no restrictions were imposed on going outside. At this time, some school activities were suspended, and events were held on a smaller scale than in a typical year, but classes were conducted as usual while wearing masks and even after‐school club activities had resumed. From March through April, Tochigi Prefecture experienced an outbreak wherein the number of new patients infected with the coronavirus increased by up to five per day with almost no interruption. From May through June, however, the number of new cases per day was often zero. After schools reopened, in July and September, the number of new cases began to increase again, peaking at 12 on one day in July, and 17 on one day in September. However, in October, the number of new cases decreased, continuing at a pace of approximately five per day.
Data collection
All children were asked to fill out the Japanese‐language version of the WHO Five Well‐Being Index (hereinafter, WHO‐5‐J) and the questionnaire while waiting for their examination. In the questionnaire, children were asked about: (i) learning environment; (ii) family members with which they spent more time than before; (iii) state of contact with friends; (iv) home activities to which they devoted more or less time than before; and (v) changes in daily routine and physical condition. We also collected information on gender, age, and treatment details from previous medical records. If the WHO‐5‐J was completed during the study period, children were not required to complete it subsequently. Questionnaires completed by children who were unable to answer the questionnaire, which had missing responses or mistakes when completing the questionnaire were excluded. Children who had been previously diagnosed with mental health problems and were undergoing treatment such as psychotherapy before school closure were also excluded.
The Japanese‐language version of the World Health Organization Five Well‐Being Index (WHO‐5‐J)
This study was conducted using the WHO‐5‐J instrument along with a questionnaire about home life and mood. Developed by WHO, the WHO‐5‐J is a mental health measurement scale that is extremely easy to use. 7 The age of the subjects was 9 years and older. The WHO‐5‐J is composed of five questions about the respondent’s mood in the preceding two weeks. The responses include six options, namely: (i) all of the time; (ii) most of the time; (iii) more than half of the time; (iv) less than half of the time; (v) some of the time; and (vi) at no time. The score is calculated by summing the scores for the five questions. Scores thus range from 0 to 25, where 0 is associated with the worst and 25 with the best mental health status. Total scores under 13 points are considered indicative of suspected mental health problem.
Statistical analysis
Statistical analyses were performed with JMP 9.0.0 software (SAS Institute, Cary, NC, USA). To analyze the characteristics of the two groups of subjects, those examined during school closures and those examined after school reopening, a Pearson's chi‐square test was performed for gender and learning environment, and a Student's t‐test was performed for age. A Wilcoxon signed‐rank test was used to analyze the differences between the two groups in terms of total scores and scores for single items of the WHO‐5‐J. A Pearson's chi‐square test was used to analyze the changes in daily life and relationship with friends and family for the two groups. Statistical analysis results with P <0.05 were considered significant.
Ethical considerations
This study was approved by the Institutional Review Board of the Haga Red Cross Hospital (approval no.: R2‐4). An explanation on the use of personal information was given to the guardians of the children together with an explanation of the purpose of this study. Receipt of a completed questionnaire was considered to indicate consent.
Results
Demographics and characteristics of participants
There were 111 elementary and junior high school students 9 years and older that came to the hospital for a scheduled appointment and who agreed to participate in the study in May 2020, when schools had been closed for approximately 2 months (school closure group), and 166 in October 2020, four months after schools had reopened (school reopening group). After excluding children who had difficulties responding, missing responses, or were already receiving psychotherapy, 78/111 (70%) remained in the school closure group and 113/166 (68%) remained in the school reopening group. The school closure group included 48 males (48/78, 62%) at an average age of 11.4 (1.7) years, with no significant difference from the school reopening group (Table 1).
Table 1.
Demographics and characteristics of participants
| School closure group | School reopening group | P‐value | |
|---|---|---|---|
| n = 78 | n = 113 | ||
| Male : Female | 48 : 30 | 62 : 51 | 0.3591 |
| Age, years (SD) | 11.4 (1.7) | 11.6 (1.8) | 0.4740 |
| Learning environment | |||
| Online classes | 29/78 (37%) | 6/113 (5%) | <0.0001* |
| Regular classes | 0/78 (0%) | 96/113 (85%) | <0.0001* |
P < 0.05.
In the school closure group, no children were attending classes as usual, and 29 (37%) were attending online classes. In the school reopening group, 96 children (85%) were attending classes as usual.
Changes in relationships with family and friends and daily routine
The school closure group included more children who had spent more time with family (Fig. 1a) (68/78, 87%) and with siblings (61/78, 78%) than the school reopening group. However, few children reported spending more time with their fathers (12/78, 15%) and there was no change in time spent alone (8/78, 10%). For most children, time spent playing with friends had decreased 7/78, 73%), and many were not in contact with their friends at all (41/78, 53%).
Fig. 1.
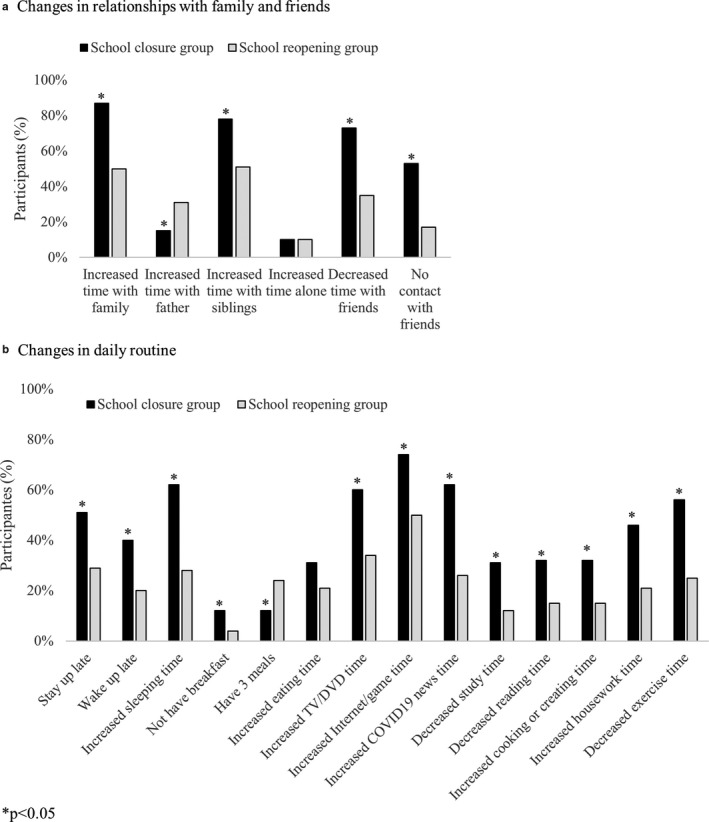
(a) The school closure group included more children who had experienced an increase in time spent with family and siblings than the school reopening group. Few children spent more time with their fathers and there was no change in time spent alone. Time spent playing with friends decreased, and many were not in contact with their friends at all in the school closure group. (b) The school closure group included more children who were staying up later at night, had more difficulty getting up in the morning, and whose hours of sleep had increased than the school reopening group. More children in the school closure group had skipped breakfast, fewer ate three meals per day, experienced an increase in time spent watching TV or DVDs, playing video games or on the Internet, and watching news about COVID‐19. This group included more children who experienced a decrease in time spent studying and time devoted to physical activity. (■), school closure group; ( ), school reopening group.
), school reopening group.
With regard to daily routine (Fig. 1b), the school closure group included more children who stayed up later at night (40 /78, 51%), had more difficulty getting up in the morning (31/78, 40%), and whose hours of sleep had increased (48/78, 62%) than the school reopening group. More children skipped breakfast (9/78, 12%) and fewer ate three meals per day (9/78, 12%); however, there was no change in daily meal fluctuations (increased for 24/78, 31%, decreased for 10/78, 13%). Many children increased their time spent watching TV or DVDs (47/78, 60%) time spent on the Internet or playing video games (58/78, 74%), and time spent watching news about COVID‐19 (48/78, 62%). An increase in time spent cooking and doing chores (25/78, 32%) and helping with housework (36/78, 46%) was more common in this group as well. Conversely, this group included more children who spent less time studying (24/78, 31%) and time devoted to physical activity (44/78, 56%). As for physical condition, the school closure group included 5/78 children (6%) whose physical condition had worsened, 8/78 (10%) who felt fatigued, and 15/78 (19%) who became irritated more easily. However, there were no significant differences with the school reopening group.
WHO‐5
There were 14 children who scored under 13 points in the WHO‐5‐J in the school closure group (18%) and 23 in the school reopening group (20%), with no significant difference between the two groups. There was no difference in total scores as well (Table 2). However, a comparison of single WHO‐5‐J items revealed that the scores for “I have felt active and vigorous” and “My daily life has been filled with things that interest me” were significantly lower in the school closure group, and the scores for “I woke up feeling fresh and rested” were significantly higher in the school closure group. A comparison of subjects under 13 years with those 13 years and older revealed that, in children under 13, scores for the “activity and vigor” and “interest” items were significantly lower in the school closure group, but there was no difference in scores for the “rest” item. In children aged 13 years and older, the school closure group scores for “interest” were lower, and those for “rest” were significantly higher.
Table 2.
Questionnaire and responses
| Total | School closure group | School reopening group | P‐value |
|---|---|---|---|
| n = 78 | n = 113 | ||
| Q 1. …I have felt cheerful and in good spirits | 4 (0, 5) | 4 (0, 5) | 0.6374 |
| Q 2. …I have felt calm and relaxed | 4 (0, 5) | 4 (0, 5) | 0.3825 |
| Q 3. …I have felt active and vigorous | 3 (0, 5) | 4 (0, 5) | 0.0026* |
| Q 4. …I woke up feeling fresh and rested | 4 (0, 5) | 4 (0, 5) | 0.0227* |
| Q 5. …my daily life has been filled with thing that interest me | 3 (1, 5) | 3 (0, 5) | 0.0096* |
| Total score | 17 (1, 25) | 19 (0, 25) | 0.1262 |
| <13 points | 14 (18%) | 23 (20%) | 0.6793 |
| Children under 13 years of age | n = 57 | n = 78 | |
|---|---|---|---|
| Q 1. | 4 (0, 5) | 4 (1, 5) | 0.2742 |
| Q 2. | 4 (0, 5) | 4 (0, 5) | 0.0879 |
| Q 3. | 3 (0, 5) | 4 (0, 5) | 0.0169* |
| Q 4. | 4 (1, 5) | 4 (0, 5) | 0.2905 |
| Q 5. | 3 (0, 5) | 4 (0, 5) | 0.0414* |
| Total score | 17 (1, 25) | 19 (5, 25) | 0.0816 |
| Children with 13 years of age or older | n = 21 | n = 35 | |
|---|---|---|---|
| Q 1. | 4 (2, 5) | 4 (0, 5) | 0.4780 |
| Q 2. | 4 (1, 5) | 3 (0, 5) | 0.2975 |
| Q 3. | 3 (0, 5) | 3 (0, 5) | 0.0477* |
| Q 4. | 4 (1, 5) | 3 (0, 5) | 0.0242* |
| Q 5. | 2 (0, 5) | 3 (0, 5) | 0.0689 |
| Total score | 16 (9, 25) | 17 (0, 25) | 0.8123 |
Data shown as median (minimum, maximum).
P < 0.05.
Discussion
During school closures, elementary and junior high school students who came to our hospital for scheduled appointments spent more time with their families and devoted more time to sleep. However, they also experienced disruptions in their sleep rhythms, eating habits, and physical activity routines. As the children's living environment changed, they felt less active and vigorous, and had difficulty finding things that interested them. However, their sleep improved and the percentage of children with suspected mental health problem did not change overall. Although prior research includes many reports assessing children’s mental health at a single point during a school closure, 8 , 9 reports of repeated assessments over time are rare. Therefore, this report is considered valuable for those interested in children's mental health.
In 2020, reports of mental health problem caused by school closures initiated to prevent the spread of COVID‐19 have been published in several countries. Tang et al. report that the major mental health problems in primary and secondary school students during school closures were anxiety, depression, and stress, and that high school students had more symptoms of depression, anxiety, and stress than elementary school students. 8 In the present study as well, 18% of elementary and junior high school students’ WHO‐5‐J scores were under 13 points, which suggests the presence of mental health problems. Furthermore, children with suspected mental health problems in this study tended to be older on average than children for whom no mental health problems were suspected. Older children may tend to develop mental health problems related to school closures more easily than younger children. Differences in the emergence of mental health problem by age have also been reported in prior studies. A preliminary study conducted in Shanghai showed that children aged 3–6 years were more likely than older children to manifest symptoms, such as clinginess and fear that family members could contract the infection. Children aged 6–18 years were more likely to show inattention and persistent inquiry. 9 In the present study, the age range of subjects was not as wide as in some previous studies. Nevertheless, it was confirmed that for children with 13 years and older, unlike for those under 13 years, school closures had a positive effect on children's mental state in addition to a negative one. Therefore, it can be conjectured that mental health problems related to school closure vary by age, and assessments of children's mental health after school closures should adopt an approach that accounts for age.
An interesting result of the present study is that children's quality of sleep was better during school closures. In a nationwide study conducted by the Ministry of Education, Culture, Sports, Science and Technology in 2014, 10 the ratio of Japanese elementary and junior high school students who reported that they were not getting enough sleep was approximately 15% for fifth and sixth grade elementary school students, and 25% for junior high school students, close to the proportion of students who reported improvements in their sleep in the present study (24%). Moreover, a study conducted in Tokyo from 2011 through 2016 found that the ratio of high school students who did not get an adequate amount of sleep was 68.9% for boys and 80.4% for girls 11 . In the present study as well, approximately 60% of elementary and junior high school students reported an increase in their hours of sleep, suggesting that a majority of school‐aged children may be chronically sleep deprived. The reason why Japanese children suffer from chronic sleep deprivation can be inferred from reports of child lifestyle. Abe et al. reported that Japanese children who stayed up late showed tendencies with increased attendance at cram schools and more time on TV. 12 The preliminary study conducted in six countries revealed that Japanese, Korean, and Chinese children spend more time studying than American, British, and Russian children, 13 while that Japanese children spend more time on TV than Korean and Chinese children. Based on these reports, the chronic sleep deprivation in Japanese children may be due to the amount of time they spend studying and consuming media. The adequate amount of sleep afforded to the children by school closures improved their quality of sleep. However, although the hours of sleep increased, their time spent studying decreased and their time spent consuming media increased during school closures. Prolonged disruption of their life rhythms due to school closures might put them at increased risk for worsening quality of life.
In assessing the results of this study, it should be noted that children's mental health after schools reopened may not have been the same as their baseline level of mental health before the school closures began. Between the start of school closures in April 2020 and after reopening in October, the number of school‐aged children who died by suicide nationwide was higher than for the same time in preceding years. 14 This suggests that the number of children who suffered from mental health problems was higher than in a typical year, not only during the school closures but after schools reopened as well. However, the present study found no change in the ratio of elementary and junior high school students with suspected mental health problems based on the WHO‐5‐J during school closures and after school reopening. While the WHO‐5‐J total scores tended to improve between the school closures and reopening, this difference was not statistically significant.
In a nationwide study of baseline WHO‐5‐J scores in children between 2002 and 2004, Ando et al. extracted randomized data from 4,478 children aged 10, reporting a total median value (19.7 points) which is close to the present study's total median value after school closures (19.0 points). 15 On this basis, it is conjectured that the state of children's mental health after schools reopened was close to the baseline before school closures. The present study's divergence from nationwide social phenomena may be a consequence of the selection of children with scheduled appointments at a medical institution as subjects. It is possible that, because the research subjects were children whose parents cared about their health and whose families were functional, their resilience was protected and they were at lower risk of developing mental health problems. The fact that family dysfunction increases the risk of mental health problem in children has been reported in many prior studies. 16 , 17 In the present study, even children whose families were considered functional experienced a partial worsening of mental health related to lifestyle changes after school closures. It is possible that, in less resilient children, the effects on mental health would have been more evident and long‐lasting.
The limitations of this research include the fact that, although children’s mental health after schools reopened was considered close to their baseline mental health before school closures, as explained above, this cannot actually be ascertained without repeated assessments over time. Another limitation was, as the survey was conducted in a particular environment, i.e. a medical facility, rather than the usual school or household environment of the subjects, sample size was limited and we were unable to compare results with those from children without the opportunity to visit a medical institution.
Conclusions
In elementary and junior high school students who came to our hospital for scheduled appointments, school closures initiated to prevent the spread of COVID‐19 infections resulted in increased time spent with family and increased time devoted to sleep, but also disrupted sleep rhythms, eating habits, and physical activity routines. As the children’s living environment changed, they felt less active and vigorous, and had difficulty finding things that interested them. However, their sleep improved and the ratio of children with suspected mental health problem did not change overall.
Disclosure
No potential conflicts of interest was disclosed.
Author contributions
M.S. designed the study; M.S. and H.M. collected data; M.S. analyzed data and wrote manuscript; A.L. revised the English manuscript; Y.K. and H.M. gave conceptual advice. All authors read and approved the final manuscript.
References
- 1. Matthews T, Danese A, Wertz J et al. Social isolation and mental health at primary and secondary school entry: A longitudinal cohort study. J. Am. Acad. Child Adolesc. Psychiatry 2015; 54: 225–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bayer JK, Mundy L, Stokes I, Hearps S, Allen N, Patton G. Bulling, mental health and friendship in Australian primary school children. Child Adolesc. Mental Health 2018; 23: 334–40. [DOI] [PubMed] [Google Scholar]
- 3. Falbe J, Davison KK, Franckle RL et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics 2015; 135: e367–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lubans D, Richards J, Hillman C et al. Physical activity for cognitive and mental health in youth: A systematic review of mechanisms. Pediatrics 2016; 138: e20161642. [DOI] [PubMed] [Google Scholar]
- 5. Hoge E, Bickham D, Cantor J. Digital media, anxiety, and depression in children. Pediatrics 2017; 140: S76–80. [DOI] [PubMed] [Google Scholar]
- 6. Hale L, Guan S. Screen time and sleep among school‐aged children and adolescents: A systematic literature review. Sleep Med. Rev. 2015; 21: 50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Allgaier AK, Pietsch K, Fruhe B, Prast E, Sigl‐Glockner J, Schulte‐Korne G. Depression in pediatric care: Is the WHO‐Five Well‐Being Index a valid screening instrument for children and adolescents? Gen. Hosp. Psychiatry 2012; 34: 234–41. [DOI] [PubMed] [Google Scholar]
- 8. Tang S, Xiang M, Cheung T, Xiang YT. Mental health and its correlates among children and adolescents during COVID‐19 school closure: The importance of parent‐child discussion. J. Affect. Disord. 2020; 279: 353–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jiao WY, Wang LN, Liu J et al. Behavioral and emotional disorders in children during the COVID‐19 epidemic. J. Pediatr. 2020; 221: 264–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ministry of Education, Culture, Sports, Science and Technology . A survey on the relationship between sleep‐centered lifestyle habits and children’s independence. https://www.mext.go.jp/a_menu/shougai/katei/__icsFiles/afieldfile/2015/04/30/1357460_01_1_1.pdf. (Accessed April 4, 2021). [Google Scholar]
- 11. Ogawa S, Kitagawa Y, Fukushima M et al. Interactive effect of sleep duration and physical activity on anxiety/depression in adolescents. Psychiatry Res. 2019; 273: 456–60. [DOI] [PubMed] [Google Scholar]
- 12. Abe T, Hagihara A, Nobutomo K. Sleep patterns and impulse control among Japanese junior high school students. J. Adolesc. 2010; 33: 633–41. [DOI] [PubMed] [Google Scholar]
- 13. Benesse Educational Research and Development Center . International Survey of Six Cities Preliminary Report. https://berd.benesse.jp/up_images/english/6toshi_english2.pdf. (Accessed April 4, 2021). [Google Scholar]
- 14. Ministry of Health, Labor and Welfare . Suicide Statistics: Basic Data on suicide in the Community. http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000140901.html. (Accessed April 4, 2021). [Google Scholar]
- 15. Ando S, Usami S, Matsubayashi T et al. Age relative to school class peers and emotional well‐being in 10‐year‐olds. PLoS One 2019; 14: e0214359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Allison MA, Attisha E. The link between school attendance and good health. Pediatrics 2019; 143: e20183648. [DOI] [PubMed] [Google Scholar]
- 17. Prime H, Wade M, Browne DT. Risk and resilience in family well‐being during the COVID‐19 pandemic. Am. Psychol. J. 2020; 5: 631–43. [DOI] [PubMed] [Google Scholar]


