Abstract
Background: Hand hygiene (HH) is one of the most important measures to prevent healthcare‐associated infections. Data on HH compliance in companion animal veterinary institutions in Europe are sparse.
Methods: This observational study assessed HH according to WHO standards in three large and two medium‐sized clinics and two primary care practices in Switzerland. Associations with HH indication, professional group, clinical area and institution were determined using a generalized linear mixed effects model.
Results: Based on 2056 observations, overall HH compliance [95% confidence interval] was 32% [30%‐34%]. HH compliance was highest in the consultation area (41% [38%‐45%]) and after contact to body fluids (45% [40%‐50%]), and lowest in the pre‐OR area (20% [15%‐24%]) and before clean/aseptic procedures (12% [9%‐15%]). Veterinarians showed a higher HH compliance (37% [34%‐40%]) than veterinary nurses (25% [22%‐28%]). HH compliance was lower before clean/aseptic procedures compared to all other indications (all p < 0.015 except ‘before touching a patient’ in medium‐sized clinics/practices, p = 0.095) and higher in the consultation area compared to all other areas in large clinics (all p < 0.04).
Conclusion: Effective HH training should urgently be promoted for all veterinary personnel with special emphasis on the importance of HH before clean/aseptic procedures.
INTRODUCTION
Hand hygiene (HH) is considered one of the most important infection control measures in human healthcare 1 , 2 and the most efficient way to reduce transmission of pathogens between healthcare workers and patients. 1 , 3 , 4 Guidelines for proper HH performance have been established to reduce the incidence of healthcare‐associated infections and the transmission of nosocomial pathogens. 3 The World Health Organization (WHO) defines five moments for HH which indicate the five situations with highest risk of hand contamination of healthcare workers and transmission of pathogens (Table 1). Strict adherence to the five HH indications can interrupt the transmission chain in these at‐risk situations and reduce the incidence of nosocomial infections. 1 , 5 Despite these benefits, HH compliance in human healthcare workers has often been reported to be poor, and highly variable HH compliance rates between 5% and 89% have been described. 1 , 6 , 7 Several studies have shown that training and educational campaigns such as individual trainings, lectures and reminders can improve HH compliance in healthcare workers. 1 , 8 For instance, a multimodal campaign over a period of 3 years held in a Swiss university hospital improved HH compliance from 48% to 66%. 9
TABLE 1.
Specification of the WHO five moments for hand hygiene. Modified from CleanHands: Handbuch, Swissnoso, Switzerland ∗
| Moment | Definition | Examples |
|---|---|---|
| Before clean/aseptic/invasive procedures | Hand hygiene immediately before an clean/aseptic/invasive procedure during patient care |
‐ Punctures (blood sampling, injections, placement of intravascular/urinary catheters, suction/change of urine bags) and endotracheal intubation ‐ Manipulation of vascular/urogenital accesses/drainage and infusion systems ‐ Wound care ‐ Handling of sterile material |
| After body fluid exposure risk | Hand hygiene immediately after completion of any procedure with exposure to body fluids, even after removal of gloves |
‐ Contamination of hands with blood, urine, feces or other body fluids ‐ Blood sampling‐ Change of dressings‐ Manipulation of urine drainage systems |
| After touching a patient | Hand hygiene after direct patient contact, i.e., when leaving the patient or patient surroundings | ‐ Medical examination‐ Fur care |
| Before touching a patient | Hand hygiene before first contact with the patient | ‐ Medical examination |
| After touching patient surroundings | Hand hygiene after touching objects/surfaces in the immediate vicinity of the patient even without direct physical contact to the patient | ‐ Contact with animal cage, infusion equipment, monitors and other medical equipment |
CleanHands: Handbuch, Swissnoso, National Centre for Infection Prevention, Bern, Switzerland. https://www.swissnoso.ch/fileadmin/module/cleanhands/Dokumente/cleanhands_manual_D.pdf. Accessed 8 July 2020.
In companion animal medicine, the concept of the WHO five moments for HH has so far gained little attention, although the work performed by veterinary professionals in companion animal clinics and practices is comparable to that of human healthcare workers. The recent progress in companion animal intensive care has led to the establishment of large and highly specialized clinics. In these settings, the risk of pathogen transmission can be assumed to be high due to the high density of hospitalized patients, the many animals with conditions that compromise immune response to infection, the high number of invasive procedures and consequently a high number of at‐risk situations for hand contamination of the veterinary personnel. 8 In line with this, companion animal clinics have recently been shown to play a role in the development and spread of multidrug‐resistant organisms, and outbreaks with methicillin‐resistant Staphylococcus aureus 10 and Staphylococcus pseudintermedius, 11 highly resistant Acinetobacter spp. 12 , 13 and carbapenemase‐producing Enterobacteriaceae have been reported. 14 , 15 Furthermore, there is evidence for a transfer of multidrug‐resistant organisms between companion animal patients, the clinical environment, veterinary staff and pet owners. 16 , 17 , 18 This underlines that good infection prevention and control (IPC) standards in veterinary clinics are of public health importance; HH implementation with special emphasis on HH training of the personnel plays a key role in IPC concepts.
Only three studies performed in Canada and the United States have evaluated HH compliance in companion animal veterinary institutions based on HH observations. 19 , 20 , 21 One study from Ontario, Canada, performed video observations in 38 primary care companion animal clinics and mixed animal clinics and assessed the effectiveness of a poster campaign to improve HH compliance. The study reported an overall poor HH compliance of 14%. 21 HH was performed in 3% and 26% of moments before and after patient contact, respectively, and a poster intervention had no significant effect on HH compliance. The other two studies used direct HH observation and reported an overall HH compliance of 21% and 27%, respectively 19 , 20 ; HH compliance improved to 42% in one of these studies after training campaigns. 20 To our knowledge, no study has yet assessed HH compliance in different types of companion animal veterinary institutions in Europe, including Switzerland, using direct observation and protocols recommended by the WHO. Thus, the aims of this observational study were to evaluate HH compliance according to the WHO five moments for HH in large and medium‐sized companion animal clinics and primary care practices in Switzerland using an online application tool and to investigate whether HH compliance differs between the types of institutions, the clinical areas and the professional groups.
MATERIALS AND METHODS
Companion animal clinics and practices
For this observational study, seven companion animal veterinary institutions were recruited. The institutions were chosen to be located in different parts of Switzerland (South, West, Central and East of Switzerland) and to cover different clinic/practice types. The institutions included both university hospitals and private clinics/practices and comprised three large clinics (Clinic A‐C), two medium‐sized clinics (Clinic D and E) and two small primary care practices (Practice F and G). Details on the seven institutions are given in File S1‐S3; the IPC standards in these institutions have been assessed and described in the previous study. 14 The two small practices received first opinion cases, whereas medium‐sized and large clinics also received referred cases. The large clinics additionally offered a 24/7 emergency service and an intensive care unit. Participation in the study was voluntary and was not reimbursed.
HH observations
Based on published studies 19 , 21 and the first 200 observations obtained in this study, a HH compliance of 30% was assumed, and a sample size of 500 HH events in Clinics A‐C (100 observations per study area) and 130 HH events in Clinics/Practices D‐G was calculated to allow to differentiate a 10%‐difference in HH compliance between large clinics and a 20%‐difference between all institutions. 22 All HH observations were performed between September 2018 and May 2019 as direct observations. The reason for the observations was announced to the clinical staff at the beginning of the study. To omit an observer bias, all observations were done by the same person (Janne S. Schmidt) who received training for three full working days prior to the start of the observation period by an infection control practitioner with extensive experience and knowledge in HH observation. The clinical area, the observation times during the day and the healthcare workers were randomly chosen to omit a selection bias. The observations were performed based on recommended protocols. 22 , 23 At the beginning of each observation, the observer located herself discreetly in one of the clinical areas at a position where she had a good view of the workflow. A full clinical procedure in a patient was observed from the beginning to the end whenever possible, but observation was ended within a procedure when the patient was moved to another clinical area. A maximum of three to five people were observed in parallel. 23 In areas with intensive workflow, the observer focused on all people involved in the clinical procedures of a patient. The direct observation session was concluded after around 20 min or after completion of a full procedure. 22 No feedback was given during or after the observation session. The HH observations were recorded using the CleanHands application (Swissnoso, National Centre for Infection Prevention, Bern, Switzerland) which allows direct electronic data collection and analysis of HH events based on the concept of the WHO five moments for HH 1 , 5 , 23 ; details on how the HH observations were allocated to the indications are given in Table 1. When opportunities for HH involved more than one indication, only a single indication was retained by applying the following published priority rules: before clean/aseptic procedure > after body fluid exposure risk > after touching a patient > before touching a patient > after touching patient surroundings. 22 HH actions that occurred without an indication were recorded as non‐coded actions and were excluded from statistical analyses. In accordance with the WHO standards both hand disinfection with alcohol‐based handrubs and hand washing with water and soap but not the use of gloves were considered successful HH procedures. 1 , 22 , 24 Medical gloves are indicated in certain situations such anticipated contact with blood or another body fluid or when handling patients under contact precautions. Wearing gloves cannot fully prevent hand contamination and the transmission of pathogens by the hands of healthcare workers; therefore, the HH indications exist regardless of glove use. 1 Data on the use of gloves could not be collected with the CleanHands application version that was available at the time when the study was performed.
The HH events were allocated to three professional groups: 1) veterinarians, 2) veterinary nurses and 3) others (e.g., students, technicians and cleaning staff). HH observations were conducted in five different areas in the Clinics A‐C: 1) pre‐operating preparation area (pre‐OR), 2) intensive care unit (ICU), 3) ward (animal housing area), 4) consultation area (where consultations are held with the patient owners) and 5) examination area (where hospitalized and ambulatory patients are examined and treated). Due to more limited infrastructure in Clinics/Practices D‐G, HH observations were only performed in the examination area (D and G), ward (E) and consultation area (D‐G) in these institutions.
Statistical analysis
HH compliance (%, number of correct HH events per total number of observed HH events) with [95% confidence intervals] based on Wilson binomial confidence intervals was calculated by using the software R 25 and the Hmisc package. 26 Data from Clinics A‐C and Clinics/Practices D‐G were analysed separately to account for different infrastructure and thus differences in the clinical areas included in the institutions (see above). Association of HH with the type of institution, the HH indication, the professional group and the area within the clinic was investigated using generalized linear mixed models and conditional inference trees. Conditional inference trees are based on recursive partitioning, selecting covariates to split and recurse the outcome variable. In order to account for potential clustering within practice/clinic, generalized linear mixed effects models with the five HH indications, the professional groups and the clinical areas as fixed effects and the individual practice or clinic as random effect were performed using the R package nlme. 27 Adjustment for multiple comparisons was performed using Tukey's approach available in the multcomp package. 28 Conditional inference trees were obtained with the package partykit with the software package R. 25 , 29
Ethics approval and consent to participate
The investigations were part of a study on infection prevention and control standards in companion animal clinics in Switzerland that was approved by the ethics committee of the Canton of Berne, Switzerland (KEK‐BE Nr.: 2018‐00866). Each participating institution gave informed consent to participate in the study. Healthcare workers were not identified during observation sessions for confidentiality reasons, and no data from any individual person were collected in this study. The personnel of each institution were informed on the study set‐up. In large clinics an information session was held prior to the start of the study.
RESULTS
HH in the seven companion animal clinics and practices
A total of 2123 HH opportunities were observed in the seven institutions. Non‐coded actions (HH actions without an indication for HH, n = 67) were excluded resulting in 2056 observations included in the analyses. The distributions of the data of the seven institutions related to clinical area, professional group and HH indication are shown in Figures 1a‐1c, respectively. The results of HH compliance separated by institution, HH indication, clinical area and professional group are given in Table 2. The overall HH compliance in the clinics/practices was 32% [30%‐34%], ranging from 26% (Clinic E) to 47% (Practice F). HH compliance was not significantly different between large clinics (A‐C: 31% [28%‐33%]) and mediumsized clinics/practices (D‐G, 35% [31%‐39%]). When only HH compliance in the consultation area was compared, which was assessed in all institutions, highest HH compliance was found in Clinic A (52% [42%‐62%]), followed by Practice F (47% [39%‐56%]), Clinic B (46% [36%‐55%]), Clinic D (46% [35%‐57%]), Clinic C (40% [31%‐50%]), Clinic E (33% [23%‐44%]) and Practice G (27% [20%‐35%]). HH compliance differed significantly between the five HH indications, the five clinical areas and the three professional groups (Table 2). HH compliance was highest after body fluid exposure risk (45% [40%‐50%]) and lowest before clean/aseptic procedure (12% [9%‐15%]). HH compliance was highest in the consultation area (41% [38%‐45%]) and lowest in the pre‐OR area (20% [15%‐24%]), and veterinarians showed a higher adherence to HH (37% [34%‐40%]) than veterinary nurses (25% [22%‐28%]).
FIGURE 1.
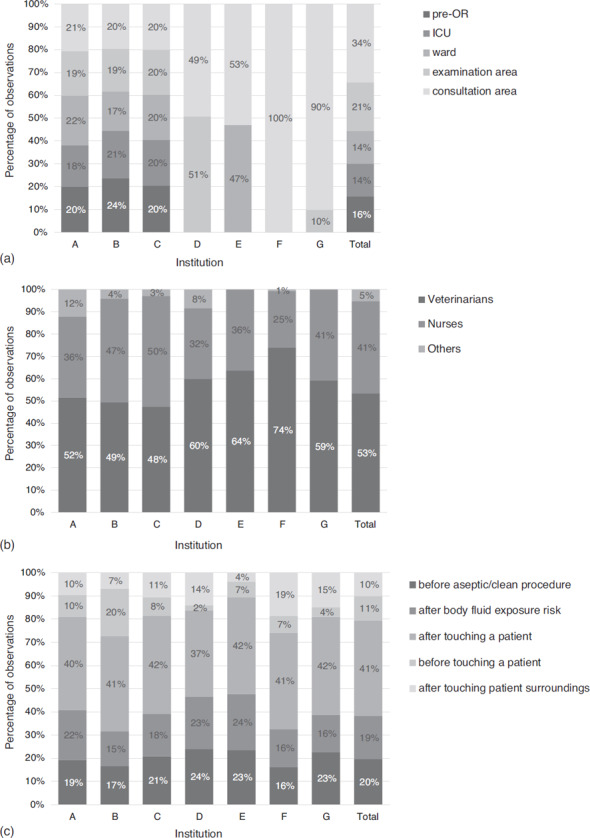
(a) Distribution of HH observations among different clinical areas in Clinics/Practices A‐G. Percentages of HH observations per clinical area are indicated for each institution and for all institutions. (b) Distribution of HH observations among different professional groups in Clinics/Practices A‐G. Percentages of HH observations per professional group are indicated for each institution and for all institutions. (c) Distribution of HH observations among different HH indications in Clinics/Practices A‐G. Percentages of HH observations per HH indication are indicated for each institution and for all institutions
Abbreviations: ICU, intensive care unit; nurse, veterinary nurses; others, working personnel not allocated to veterinary nurses or veterinarians (i.e. students, technicians and cleaning staff); pre‐OR, pre‐operating preparation area; ward, animal housing area.
TABLE 2.
Hand hygiene compliance in the different institutions, clinical areas and professional groups
| Clinic/practice | n = | HH compliance | 95% CI | Indication | n = | HH compliance | 95% CI | Area | n = | HH compliance | 95% CI | Profession | n = | HH compliance | 95% CI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | 483 | 35% | 31%‐40% | Afterbody fluid exposure risk | 383 | 45% | 40%‐50% | ICU | 295 | 32% | 27%‐38% | Veterinarians | 1097 | 37% | 34%‐40% |
| B | 513 | 29% | 25%‐33% | After touching a patient | 845 | 36% | 32%‐39% | Consultation area | 706 | 41% | 38%‐45% | Veterinary nurses | 851 | 25% | 22%‐28% |
| C | 509 | 28% | 24%‐32% | After touching patient surroundings | 206 | 34% | 28%‐41% | Ward | 356 | 26% | 21%‐31% | Others | 108 | 31% | 23%‐41% |
| D | 142 | 40% | 32%‐49% | Before clean/aseptic procedure | 403 | 12% | 9%‐15% | Examination area | 376 | 30% | 25%‐35% | ||||
| E | 132 | 26% | 19%‐34% | Before touching a patient | 219 | 29% | 23%‐36% | Pre‐OR area | 323 | 20% | 15%‐24% | ||||
| F | 135 | 47% | 39%‐56% | ||||||||||||
| G | 142 | 26% | 19%‐34% |
Abbreviations: 95% CI, 95% confidence interval; Cons, consultation area; HH, hand hygiene; ICU: intensive care unit; Others, personnel not allocated to veterinarians or veterinary nurses (i.e., students, technicians and cleaning staff); pre‐OR: pre‐operative preparation area.
Association of HH compliance with indication, clinical area and profession
To further evaluate the association of HH compliance with HH indication, clinical area and veterinary profession, a generalized linear mixed model was applied; data from Clinics A‐C and mediumsized Clinics/Practices D‐G were analysed separately. Results for the pairwise comparisons of the areas, professions and HH indications in the large clinics (A‐C) and medium‐sized clinics/practices (D‐G) are shown in Files S2 and S3, respectively. In Clinics A‐C HH compliance differed significantly between clinical areas (HH indications not sharing the same letter being significantly different: pre‐OR areaa, examination areaab, wardab, ICUb, consultiaton areac), but not between the professional groups. HH compliance was significantly different between the five HH indications (before clean/aseptic procedurea, after body fluid exposure riskb, after touching a patientb, before touching a patientb, after touching patient surroundingsb); HH compliance was significantly lower before clean/aseptic procedure compared to the other indications.
In Clinics/Practices D‐G, HH compliance differed between the professional groups (veterinariansb, veterinary nursesa, othersab), whereas no difference was found in HH compliance between the three clinical areas. HH compliance also differed significantly between the five HH indications (before clean/aseptic procedurea, after body fluid exposure riskc, after touching a patientb, before touching a patientabc, after touching patient surroundingsbc).
Predictors for HH compliance
To depict a model that predicts HH compliance best for the two groups of institutions (Clinics, A‐C; Clinics/Practices D‐G), conditional inference trees were calculated including the data from each group (Figures 2 and 3).
FIGURE 2.
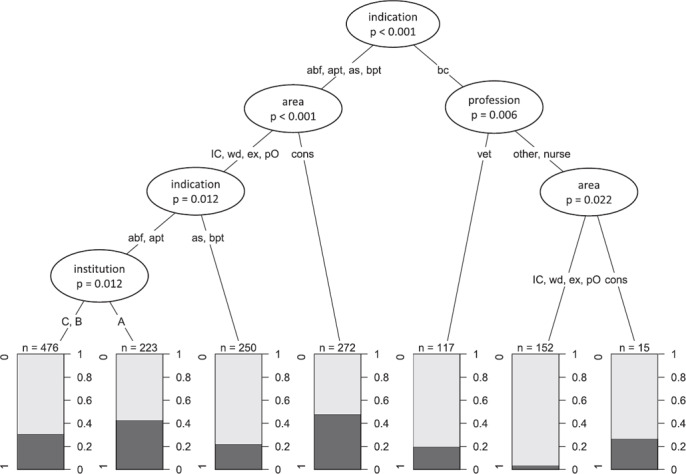
Conditional inference tree for HH observations obtained in Clinics A‐C. A conditional inference tree for the binary outcome HH compliance (1: successful, 0: unsuccessful) and the predictors (indication, area, profession, institution) based on 1505 HH observations is shown. At each predictor node, the p‐value (Bonferroni adjustment) indicating the strength of the statistical association is displayed. In the boxes the proportion of the successful HH procedures is colored in dark grey (left side ‘1') and of the unsuccessful HH procedures in light grey (left side ‘0'); the scale on the right side represents the proportion. With n the number of observations in each terminal branch is indicated
Abbreviations: abf, after body fluid exposure risk; apt, after touching a patient; bpt, before touching a patient; as, after touching patient surroundings; bc, before clean/aseptic procedure; cons, consultation area; ex, examination area; IC, intensive care unit; nurse, veterinary nurses; other: personnel not allocated to veterinarians or veterinary nurses (i.e. students, technicians and cleaning staff); pO, pre‐operating preparation area; wd, ward (animal housing area); vet, veterinarians
FIGURE 3.
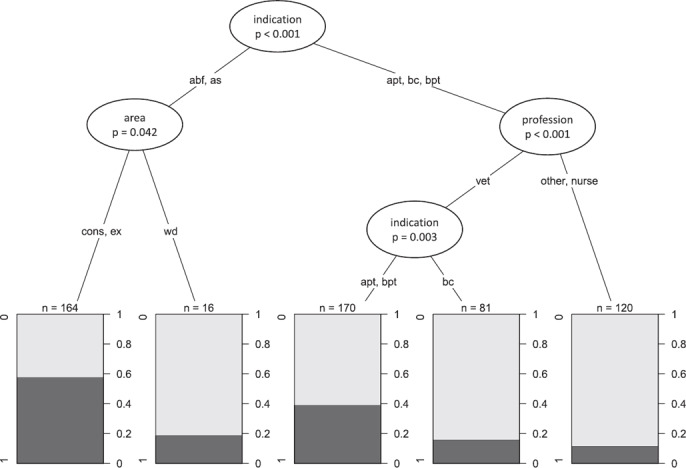
Conditional inference tree for HH observations obtained in Clinics/Practices D‐G. A conditional inference tree for the binary outcome HH compliance (1: successful, 0: unsuccessful) and the predictors (indication, area, profession, institution) based on 551 HH observations is shown. At each predictor node, the p‐value (Bonferroni adjustment) indicating the strength of the statistical association is displayed. In the boxes, the proportion of the successful HH procedures is colored in dark grey (left side ‘1') and of the unsuccessful HH procedures in light grey (left side ‘0'); the scale on the right side represents the proportion. With n the number of observations in each terminal branch is indicated
Abbreviations: abf, after body fluid exposure risk; apt, after touching a patient; bpt, before touching a patient; as, after touching patient surroundings; bc, before clean/aseptic procedure; cons, consultation area; ex, examination area; nurse, veterinary nurses; other, personnel not allocated to veterinarians or veterinary nurses (i.e. students, technicians and cleaning staff); vet, veterinarians; wd, ward (animal housing area)
In Clinics A‐C, HH compliance was in a first step influenced by the HH indication (before clean/aseptic procedure vs. other indications, Figure 2). For the indication ‘before clean/aseptic procedure’, veterinarians showed a higher adherence to HH than veterinary nurses and others, and the latter showed a higher HH compliance for this indication in the consultation area compared to other areas. For the other HH indications, HH compliance was influenced by the clinical area and higher in the consultation area compared to other clinical areas.
In Clinics/Practices D‐G, HH compliance was also primarily influenced by the HH indication (after body fluid exposure risk, after touching patient surroundings vs. after touching a patient, before clean/aseptic procedure, before touching a patient, Figure 3). HH compliance after body fluid exposure risk and after touching patient surroundings was higher in the consultation and examination area compared to the ward. For the other three indications (after touching a patient, before clean/aseptic procedure and before touching a patient), veterinarians showed a higher HH compliance than veterinary nurses and others, and HH compliance in veterinarians was lowest before clean/aseptic procedures.
DISCUSSION
The present study investigated HH compliance in different types of companion animal veterinary institutions in Switzerland and found an overall poor HH compliance ranging from 26% to 47% across institutions. Our findings are in line with three previous studies that reported an overall HH compliance of 14%‐27% in companion animal clinics in Canada and the USA. 19 , 20 , 21 Differences in study set‐up and evaluation of HH do not allow to directly compare the reported HH compliance between these studies. However, the reported HH compliance is worryingly low in all studies and can be interpreted as largely insufficient to break the transmission chains of pathogens in veterinary institutions. Both infections with zoonotic and non‐zoonotic pathogens are of relevance in companion animals. 30 Furthermore, highly resistant bacteria such as carbapenemase‐producing Enterobacteriaceae or methicillin‐resistant staphylococci play an increasing role in companion animal medicine 31 and have also been documented in the environment and in patients of some of the companion animal clinics included in this study. 14 , 32 Most recently, HH has gained considerable public health attention due to the SARS‐CoV‐2 pandemic. Although originally assumed to be limited to humans, active SARS‐CoV‐2 infections have in the meantime been documented in companion animals, especially in felids and mustelids, with some of them exhibiting respiratory or gastrointestinal signs. 33 In the light of this, proper HH adherence is of upmost importance not only for the safety of the animal patients, but also for the protection of staff exposed to patients carrying zoonotic or antimicrobial resistant pathogens.
HH compliance was higher in the consultation area compared to the other four areas evaluated (wards, examination area, pre‐OR area and ICU). The low HH compliance in the ICU and pre‐OR is of special importance since patients admitted to these areas are often in a critical condition and receive invasive procedures such as intubation, ventilation and placement of urinary or venous catheters, which makes them susceptible to infections for example with multidrug‐resistant organisms. 34 These areas are further characterized by a high density of patients and high traffic of patients and personnel which increase the risk of pathogen transmission by the hands of healthcare workers. 34 Our results are in line with studies in human hospitals where low HH compliance in intensive care areas and the pre‐OR area was also reported. 8 , 35 The findings were explained by the greater number of HH indications in these areas during daily work when compared to consultation areas. 8 , 35 Pittet et al showed that a ‘high activity index’ in critical care areas as well as procedures that carry a high risk for contamination are associated with low HH compliance. 36
HH compliance was also remarkably low in the wards where dogs and cats not admitted to the ICU are hospitalized. This is of importance since the risks of pathogen transmission in ward areas can be assumed to be high. Patient traffic occurs frequently, and parenteral application of medications is common in this area. Furthermore, most of the work in the wards is performed by veterinary nurses. In contrast to results from human medicine, HH compliance overall was lower in veterinary nurses than in veterinarians in our study. This was also found in medium‐sized clinics and primary care practices. Our results concur with the study by Anderson et al 21 that showed a better HH compliance among veterinary doctors compared to veterinary nurses but they are in contrast to the study by Smith et al 19 which found a higher HH compliance in veterinary nurses. We hypothesize that veterinarians in our study may have had better knowledge regarding the risks of exposure and transmission of pathogens. Our results show that veterinary nurses must be included in future efforts to improve HH in veterinary clinics and practices in Switzerland. Of note, investigations in human hospitals showed that veterinary nurses show a better compliance after HH training, whereas the effect of training is much less pronounced in doctors. 9 , 37 , 39
When looking at the differences among HH indications, HH was most frequently performed after body fluid exposure risk and after patient contact. This is in line with two previous studies in veterinary personnel that found a higher HH compliance after patient contact and after ‘dirty procedures’ when compared to before clean/aseptic procedures. 19 , 21 Studies in human healthcare workers also revealed that HH is more commonly performed after body fluid exposure risk and after patient contact when compared to before clean/aseptic procedures. 39 , 40 These findings suggest that in the absence of HH education, HH is carried out mostly for reasons of self‐protection or in moments of obvious contamination of the hands rather than for the protection of patients. Clean and aseptic procedures carry a high risk for the transmission of pathogens in patients. 1
Wearing gloves is not considered an HH procedure by the WHO. 1 Therefore, HH indications exist regardless of glove use. Medical gloves are indicated when a contact to blood or body fluids is anticipated and when handling patients under contact precautions. Controversial data exist on the impact of gloves on HH compliance, but a decreased HH adherence when wearing gloves has been reported in several studies in human healthcare settings. 41 , 42 , 43 Universal gloving has even been associated with a significant increase of device‐related infections in humans. 43 Since the CleanHands application version available at the time of this study did not allow to record the use of gloves by healthcare workers, the impact of wearing gloves on HH compliance in the veterinary personnel could not be assessed in this study.
In the present study, HH compliance was evaluated by direct observation since this method represents the WHO gold standard to estimate HH compliance in human healthcare facilities. 22 HH observations were always performed by the same person to omit differences in the interpretation of HH between different observers. 22 In order to generate representative data, as many different veterinary healthcare workers in patient contact as possible were observed across institutions and HH evaluation took place at different time points during the day because HH compliance can differ depending on the density of the HH indications. 22 Furthermore, direct HH observation allows to include a broad range of clinical areas. On the other hand, awareness of being observed can lead to behavioral changes of the study subject, known as the Hawthorne Effect. 44 This could have resulted in an overestimated HH compliance in our study as already shown in other studies. 45 , 46 The Hawthorne Effect might have had a bigger effect on HH compliance in the consultation areas because of the low number of people and limited space which makes a person more aware of being observed. This is in contrast to the observations collected in the ICU and pre‐OR areas which are usually characterized by a more intense work‐flow and higher density of personnel. The Hawthorne Effect is assumed to be transient and most pronounced at the beginning of the observation period. 22 However, even if our results might overestimate the real HH compliance, HH compliance was still worryingly low in all companion animal institutions included in this study.
In conclusion, low HH compliance was found in all companion animal clinics and practices in this study. Veterinary nurses showed a lower HH compliance than veterinarians, and HH compliance was remarkably low in the pre‐OR and wards and before clean/aseptic procedure. In order to prevent the transmission of pathogenic microorganisms, including multidrug‐resistant bacteria, multimodal educational interventions as established in human healthcare settings should urgently be implemented in companion animal veterinary institutions, and their effect needs to be assessed in future studies.
ACKNOWLEDGEMENTS
We are grateful to all clinics and practices who participated in the study and to Alexandra Ebert, Division of Infectious Diseases and Hospital Epidemiology, University Hospital Zurich, Switzerland, for her invaluable support.
FUNDING AND COMPETING INTERESTS STATEMENT
The study was supported by the Swiss Federal Food Safety and Veterinary Office (FSVO project number: 1.18.10). The funding body had no role in the design of the study and collection, analysis and interpretation of data and in writing the manuscript. The authors declare no competing interest.
AUTHOR CONTRIBUTIONS
Barbara Willi and Stefan P. Kuster conceived the study. Barbara Willi, Stefan P. Kuster and Simone Schuller were responsible for the coordination of the study. Stefan P. Kuster was responsible for the training in hand hygiene observation, and Janne S. Schmidt collected the data. Sonja Hartnack, Janne S. Schmidt and Barbara Willi analysed the data, and Sonja Hartnack and Janne S. Schmidt did the statistical analyses. Barbara Willi, Stefan P. Kuster and Janne S. Schmidt drafted the manuscript, and all authors edited the manuscript. All authors read and approved the final manuscript.
How to cite this article: Schmidt JS, Hartnack S, Schuller S, Kuster SP, Willi B. Hand hygiene compliance in companion animal clinics and practices in Switzerland: An observational study. Vet Rec. 2021;e307. https://doi.org/10.1002/vetr.307
Supporting information
Additional supporting information may be found online in the Supporting Information section at the end of the article.
SUPPORTING INFORMATION
REFERENCES
- 1. World Health Organization . WHO guidelines on hand hygiene in health care: a summary. First global patient safety challenge clean care is safer care. 2009. https://www.who.int/gpsc/5may/tools/who_guidelines-handhygiene_summary.pdf. Accessed 8 July 2020. [PubMed]
- 2. Allegranzi B, Pittet D. Role of hand hygiene in healthcare‐associated infection prevention. J Hosp Infect. 2009;73:305–15. [DOI] [PubMed] [Google Scholar]
- 3. Pittet D, Boyce JM. Hand hygiene and patient care: pursuing the Semmelweis legacy. 2001. Lancet Infect Dis. 2001;1:9–20.11871420 [Google Scholar]
- 4. Canadian Committee on Antibiotic Resistance . Infection prevention and control best practices for small animal veterinary clinics. 2008. https://www.wormsandgermsblog.com/files/2008/04/CCAR-Guidelines-Final2.pdf. Accessed 8 July 2020.
- 5. Sax H, Allegranzi B, Uçkay I, Larson E, Boyce J, Pittet D. ‘My five moments for hand hygiene': a user‐centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007;67:9–21. [DOI] [PubMed] [Google Scholar]
- 6. Raskind CH, Worley S, Vinski J, Goldfarb J. Hand hygiene compliance rates after an educational intervention in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2007;28:1096–8. [DOI] [PubMed] [Google Scholar]
- 7. Berg DE, Hershow RC, Ramirez CA, Weinstein RA. Control of nosocomial infections in an intensive care unit in Guatemala City. Clin Infect Dis. 1995;21:588–93. [DOI] [PubMed] [Google Scholar]
- 8. Alshehari AA, Park S, Rashid H. Strategies to improve hand hygiene compliance among healthcare workers in adult intensive care units: a mini systematic review. J Hosp Infect. 2018;100:152–8. [DOI] [PubMed] [Google Scholar]
- 9. Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, Perneger TV. Effectiveness of a hospital‐wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet. 2000;356:1307–1312. 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]
- 10. Grönlund Andersson U, Wallensten A, Hæggman S, Greko C, Hedin G, Hökeberg I, et al. Outbreaks of methicillin‐resistant Staphylococcus aureus among staff and dogs in Swedish small animal hospitals. Scand J Infect Dis. 2014;46:310–4. [DOI] [PubMed] [Google Scholar]
- 11. Grönthal T, Moodley A, Nykäsenoja S, Junnila J, Guardabassi L, Thomson K, et al. Large outbreak caused by methicillin resistant Staphylococcus pseudintermedius ST71 in a Finnish Veterinary Teaching Hospital‐from outbreak control to outbreak prevention. PLoS One. 2014;9:e110084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Francey T, Gaschen F, Nicolet J, Burnens AP. The role of Acinetobacter baumannii as a nosocomial pathogen for dogs and cats in an intensive care unit. J Vet Intern Med. 2000;14:177–83. [DOI] [PubMed] [Google Scholar]
- 13. Van Der Kolk JH, Endimiani A, Graubner C, Gerber V, Perreten V. Acinetobacter in veterinary medicine, with an emphasis on Acinetobacter baumannii. J Glob Antimicrob Resist. 2019;16:59–71. [DOI] [PubMed] [Google Scholar]
- 14. Schmidt JS, Kuster SP, Nigg A, Dazio V, Brilhante M, Rohrbach H, et al. Poor infection prevention and control standards are associated with environmental contamination with Carbapenemase‐producing Enterobacterales and other multidrug‐resistant bacteria in Swiss companion animal clinics. Antimicrob Resist Infect Control. 2020;23(9):93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nigg A, Brilhante M, Dazio V, Clément M, Collaud A, Gobeli Brawand S, et al. Shedding of OXA‐181 carbapenemase‐producing Escherichia coli from companion animals after hospitalisation in Switzerland: an outbreak in 2018. Euro Surveill. 2019;24:1900071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Morris DO, Boston RC, O'Shea K, Rankin SC. The prevalence of carriage of meticillin‐resistant staphylococci by veterinary dermatology practice staff and their respective pets. Vet Dermatol. 2010;21:400–7. [DOI] [PubMed] [Google Scholar]
- 17. Paul NC, Moodley A, Ghibaudo G, Guardabassi L. Carriage of methicillin‐resistant Staphylococcus pseudintermedius in small animal veterinarians: indirect evidence of zoonotic transmission. Zoonoses Public Health. 2011;58:533–9. [DOI] [PubMed] [Google Scholar]
- 18. Endimiani A, Brilhante M, Bernasconi OJ, Perreten V, Schmidt JS, Dazio V, et al. Employees of Swiss veterinary clinics colonized with epidemic clones of carbapenemase‐producing Escherichia coli. J Antimicrob Chemother. 2020;75:766–8. [DOI] [PubMed] [Google Scholar]
- 19. Smith JR, Packman ZR, Hofmeister EH. Multimodal evaluation of the effectiveness of a hand hygiene educational campaign at a small animal veterinary teaching hospital. J Am Vet Med Assoc. 2013;243:1042–8. [DOI] [PubMed] [Google Scholar]
- 20. Shea A, Shaw S. Evaluation of an educational campaign to increase hand hygiene at a small animal veterinary teaching hospital. J Am Vet Med Assoc. 2012;240:61–4. [DOI] [PubMed] [Google Scholar]
- 21. Anderson ME, Sargeant JM, Weese J. Video observation of hand hygiene practices during routine companion animal appointments and the effect of a poster intervention on hand hygiene compliance. BMC Vet Res. 2014;10:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sax H, Allegranzi B, Chraïti MN, Boyce J, Larson E, Pittet D. The World Health Organization hand hygiene observation method. Am J Infect Control. 2009;37:827–34. [DOI] [PubMed] [Google Scholar]
- 23. Swissnoso, National Centre for Infection Prevention . CleanHands: Handbuch. 2015. https://www.swissnoso.ch/fileadmin/module/cleanhands/Dokumente/cleanhands_manual_D.pdf. Accessed 8 July 2020.
- 24. Larson EL. APIC guideline for handwashing and hand antisepsis in health care settings. Am J Infect Control. 1995;23:251–69. [DOI] [PubMed] [Google Scholar]
- 25. R-Core-Team . A language and environment for statistical computing. R foundation for statistical computing. 2020. https://www.R-project.org/. Accessed 8 July 2019.
- 26. Harrell FE, Dupont C. Package ‘Hmisc'. Harrell Miscellaneous. 2020. https://CRAN.R-project.org/package=Hmisc. Accessed 8 July 2020.
- 27. Pinheiro J. Package ‘nlme'. Linear and nonlinear mixed effects models. 2020. https://CRAN.R-project.org/package=nlme. Accessed 8 July 2020.
- 28. Hothorn T, Bretz F, Westfall P. Simultaneous Inference in General Parametric Models. Biom J. 2008;50:346–63. [DOI] [PubMed] [Google Scholar]
- 29. Hothorn T, Zeileis A. partykit: a modular toolkit for recursive partytioning in R. J Mach Learn Res. 2015;16:3905–9. [Google Scholar]
- 30. Stull JW, Brophy J, Weese JS. Reducing the risk of pet‐associated zoonotic infections. CMAJ. 2015;187:736–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pomba C, Rantala M, Greko C, Baptiste KE, Catry B, van Duijkeren E, et al. Public health risk of antimicrobial resistance transfer from companion animals. J Antimicrob Chemother. 2017;72:957–68. [DOI] [PubMed] [Google Scholar]
- 32. Dazio V, Nigg A, Schmidt JS, Brilhante M, Mauri N, Kuster SP, et al. Acquisition and carriage of multidrug‐resistant organisms (MDRO) in dogs and cats presented to small animal practices and clinics in Switzerland. J Vet Intern Med. 2021. 35: 970–979. 10.1111/jvim.16038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hossain MG, Javed A, Akter S, Saha S. SARS-CoV-2 host diversity: an update of natural infections and experimental evidence. J Microbiol Immunol Infect. 2020;S1684–1182(20)30147-X. 10.1016/j.jmii.2020.06.006. [DOI] [PMC free article] [PubMed]
- 34. Eggimann P, Pittet D. Infection control in the ICU. Chest. 2001;120:2059–93. [DOI] [PubMed] [Google Scholar]
- 35. Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 2004;141:1–8. [DOI] [PubMed] [Google Scholar]
- 36. Pittet D. Compliance with handwashing in a teaching hospital. Ann Intern Med. 1999;130:126–30. [DOI] [PubMed] [Google Scholar]
- 37. Duggan JM, Hensley S, Khuder S, Papadimos TJ, Jacobs L. Inverse correlation between level of professional education and rate of handwashing compliance in a teaching hospital. Infect Control Hosp Epidemiol. 2008;29:534–8. [DOI] [PubMed] [Google Scholar]
- 38. Rosenthal VD, McCormick RD, Guzman S, Villamayor C, Orellano PW. Effect of education and performance feedback on handwashing: the benefit of administrative support in Argentinean hospitals. Am J Infect Control. 2003;31:85–92. [DOI] [PubMed] [Google Scholar]
- 39. Grayson ML, Russo PL, Cruickshank M, Bear JL, Gee CA, Hughes CF, et al. Outcomes from the first 2 years of the Australian National Hand Hygiene Initiative. Med J Aust. 2011;195:615–9. [DOI] [PubMed] [Google Scholar]
- 40. Moghnieh R, Soboh R, Abdallah D, El-Helou M, Al Hassan S, Ajjour L, et al. Health care workers’ compliance to the My 5 Moments for Hand Hygiene: comparison of 2 interventional methods. Am J Infect Control. 2017;45:89–91. [DOI] [PubMed] [Google Scholar]
- 41. Flores A, Pevalin DJ. Healthcare workers’ compliance with glove use and the effect of glove use on hand hygiene compliance. British J of Infect Control. 2006;7:15–9. [Google Scholar]
- 42. Girou E, Chai SHT, Oppein F, Legrand P, Ducellier D, Cizeau F, et al. Misuse of gloves: the foundation for poor compliance with hand hygiene and potential for microbial transmission? J Hosp Infect. 2004;57:162–9. [DOI] [PubMed] [Google Scholar]
- 43. Bearman GML, Marra AR, Sessler CN, Smith WR, Rosato A, Laplante JK, et al. A controlled trial of universal gloving versus contact precautions for preventing the transmission of multidrug‐resistant organisms. Am J Infect Control. 2007;35(10):650–5. [DOI] [PubMed] [Google Scholar]
- 44. Haas JP, Larson EL. Measurement of compliance with hand hygiene. J Hosp Infect. 2007;66:6–14. [DOI] [PubMed] [Google Scholar]
- 45. Hagel S, Reischke J, Kesselmeier M, Winning J, Gastmeier P, Brunkhorst FM, et al. Quantifying the Hawthorne effect in hand hygiene compliance through comparing direct observation with automated hand hygiene monitoring. Infect Control Hosp Epidemiol. 2015;36:957–62. [DOI] [PubMed] [Google Scholar]
- 46. Eckmanns T, Bessert J, Behnke M, Gastmeier P, Rüden H. Compliance with antiseptic hand rub use in intensive care units: the Hawthorne effect. Infect Control Hosp Epidemiol. 2006;27:931–4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional supporting information may be found online in the Supporting Information section at the end of the article.
SUPPORTING INFORMATION


