Abstract
Aims
To examine the nurses' burnout and associated risk factors during the COVID‐19 pandemic.
Design
We followed the Cochrane criteria and the Preferred Reporting Items for Systematic Reviews and Meta‐Analysis guidelines for this systematic review and meta‐analysis.
Data Sources
PubMed, Scopus, ProQuest, Cochrane COVID‐19 registry, CINAHL and pre‐print services (medRχiv and PsyArXiv) were searched from January 1 to November 15, 2020 and we removed duplicates.
Review Methods
We applied a random effect model to estimate pooled effects since the heterogeneity between results was very high.
Results
Sixteen studies, including 18,935 nurses met the inclusion criteria. The overall prevalence of emotional exhaustion was 34.1%, of depersonalization was 12.6% and of lack of personal accomplishment was 15.2%. The main risk factors that increased nurses' burnout were the following: younger age, decreased social support, low family and colleagues readiness to cope with COVID‐19 outbreak, increased perceived threat of Covid‐19, longer working time in quarantine areas, working in a high‐risk environment, working in hospitals with inadequate and insufficient material and human resources, increased workload and lower level of specialized training regarding COVID‐19.
Conclusion
Nurses experience high levels of burnout during the COVID‐19 pandemic, while several sociodemographic, social and occupational factors affect this burnout.
Impact
We found that burnout among nurses is a crucial issue during the COVID‐19 pandemic. There is an urgent need to prepare nurses to cope better with COVID‐19 pandemic. Identification of risk factors for burnout could be a significant weapon giving nurses and health care systems the ability to response in a better way against the following COVID‐19 waves in the near future.
Keywords: burnout, COVID‐19, mental health, meta‐analysis, nurses, prevalence, SARS‐CoV‐2, systematic review
1. INTRODUCTION
In December 2019, the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) and related disease (coronavirus disease 2019, COVID‐19) emerged from the Wuhan, capital of Hubei province, China (Chan et al., 2020). The spread of SARS‐CoV‐2 infection is much broader than other recent epidemic infections (SARS, MERS) (Jiang et al., 2020) resulting on 58,712,326 cases globally and 1,388,528 deaths by November 24, 2020 (WHO Coronavirus Disease (COVID‐19) Dashboard, 2020).
Health care workers (HCWs) represent a high‐risk group for SARS‐CoV‐2 infection since the seroprevalence of SARS‐CoV‐2 antibodies among HCWs (Galanis et al., 2020) is higher than the general population (Chen et al., 2020b) worldwide (8.7% vs. 5.3%). A meta‐analysis with data until 8 May 2020 found that 25.3% of deaths from COVID‐19 among HCWs were nurses (259 of 1024), while mental health nurses were the highest risk group for deaths (Bandyopadhyay et al., 2020). According to the International Council of Nurses, 1500 nurses have died from COVID‐19 in 44 countries up to 28 October 2020 (International Council of Nurses, 2020). In the USA, as of 16 September 2020, 31.9% (143 of 448) of the hospital HCWs who have died were nurses, while 12.4% (213 of 1718) of the HCWs who have died were nurses (National Nurses United, 2020). It is extremely likely that these numbers are probably an underestimation of the true number of deaths.
1.1. Background
Several systematic reviews and meta‐analyses have already shown that nurses present moderate to high levels of burnout syndromes (Adriaenssens et al., 2015; De la Fuente‐Solana et al., 2019; Gómez‐Urquiza et al., 2016; López‐López et al., 2019; Owuor et al., 2020; Pradas‐Hernández et al., 2018; Woo et al., 2020). The prevalence of burnout syndromes is different between geographical regions and specialties. In particular, Central Asia and Europe had the lowest burnout symptoms prevalence, while the Sub‐Saharan Africa region had the highest (Owuor et al., 2020; Woo et al., 2020). Also, paediatric, oncology and emergency nurses had the highest burnout symptoms prevalence (Gómez‐Urquiza et al., 2016, 2017; Parola et al., 2017; Pradas‐Hernández et al., 2018). Burnout among nurses is a serious and frequent health issue carrying serious negative implications not only for nurses but also for patients, colleagues and health care organizations.
Nurses play an instrumental role in the health systems response to COVID‐19 pandemic since they are the frontline health care workers directly involved in the treatment and care of patients (Hu et al., 2020; Liu et al., 2020; Zhan et al., 2020). Nurses are under extreme and persistent psychological pressure since they are particularly exposed to the threat of SARS‐CoV‐2 infection, and they become overwhelmed by fear for the safety of their own health, their close family members, and their patients (Joo & Liu, 2021). Under these circumstances nurses experience severe psychological and mental problems that could lead to burnout, and then to lower productivity, errors in clinical settings, and lack of concern in handling patients (Al Maqbali et al., 2021; Pappa et al., 2020; Salari et al., 2020). Since the second wave of COVID‐19 is hitting worldwide, health care facilities with exhausted nurses are the worst scenario to confront the pandemic. To our knowledge, there is no systematic review to emphasize in nurses and especially in burnout during the COVID‐19 pandemic. Also, given the exponential increase of studies on this research area a comprehensive review to examine the nurses' burnout during the COVID‐19 pandemic is needed.
2. THE REVIEW
2.1. Aims
We aimed to examine the nurses' burnout and associated risk factors during the COVID‐19 pandemic.
2.2. Design
We followed the Cochrane criteria and the Preferred Reporting Items for Systematic Reviews and Meta‐Analysis (PRISMA) guidelines for this systematic review and meta‐analysis (Higgins et al., 2019; Moher et al., 2009).
2.3. Search methods
PubMed, Scopus, ProQuest, Cochrane COVID‐19 registry, CINAHL and pre‐print services (medRχiv and PsyArXiv) were searched from January 1, 2020 to November 15, 2020 and we removed duplicates. We used the following strategy: ((nurs* OR “nursing staff” OR “health personnel” OR “healthcare workers” OR “healthcare personnel” OR “health care personnel” OR “health care workers”) AND (COVID‐19 OR SARS‐COV‐2)) AND (burnout). Also, we searched the full reference lists of all selected articles.
2.4. Search outcomes
We initially screened title and abstract of the records and then full‐text. Two independent authors performed study selection and disagreements were resolved by a third, senior author. We applied the following inclusion criteria: studies that were published in English, studies examining nurses' burnout and associated risk factors during the COVID‐19 pandemic; studies that used standardized and valid instruments to measure burnout; studies that included all types of nurses working in hospitals that treat COVID‐19 patients. We excluded studies reporting results in total for HCWs and not separately for nurses. Also, we excluded case reports, qualitative studies, reviews, protocols, editorials and letters to the Editor and studies that did not measure nurses' burnout.
2.5. Quality appraisal
We assessed the quality of studies included using the Joanna Briggs Institute critical appraisal tools (Santos et al., 2018). This tool consisted of 9 items for prevalence studies, 8 items for cross‐sectional studies and 11 items for cohort studies. One reviewer extracted the data and assessed the quality for all studies and a second reviewer checked this information for validity and completeness.
2.6. Data abstraction
We used structured forms to extract data from each study, such as authors, location, gender, age, sample size, study design, sampling method, assessment tool, response rate, data collection time, publication (journal or pre‐print service), number of nurses with burnout, scores on burnout scales, factors associated with burnout and the level of analysis (univariate or multivariable).
2.7. Synthesis
For each study, we extracted the sample size and the number of nurses that experienced burnout according to scores on burnout scales. Then, we calculated the prevalence of burnout and the 95% confidence interval (CI) for each included study. Prevalence from each study was transformed with the Freeman‐Tukey Double Arcsine method before pooling (Barendregt et al., 2013). We used the Hedges Q statistic and I2 statistics to assess between‐studies heterogeneity. A p‐value <0.1 for the Hedges Q statistic indicates statistically significant heterogeneity, while I2 values higher than 75% indicates high heterogeneity(Higgins, 2003). We applied a random effect model to estimate pooled effects since the heterogeneity between results was very high (Higgins, 2003). A priori, we considered sample size, publication type (journal or pre‐print service), and the continent that studies were conducted as sources of heterogeneity. Due to the limited variability of these variables and the limited number of studies, we decided to perform meta‐regression analysis only with sample size as the independent variable. We performed a leave‐one‐out sensitivity analysis to determine the influence of each study on the overall effect. We used a funnel plot and the Egger's test to assess the publication bias with a p‐value <0.05 indicating publication bias (Egger et al., 1997). We did not a perform meta‐analysis for the risk factors associated with nurses' burnout since the data were very limited and highly heterogeneous. Statistical analysis was performed with OpenMeta[Analyst] (Wallace et al., 2009).
3. RESULTS
3.1. Identification and selection of studies
Flowchart of the literature search is presented in Figure 1 according to PRISMA guidelines. Initially, we identified 439 potential records through electronic databases and 270 were left after removing duplicates. After the screening of the titles and abstracts, we removed 212 records and we added four more records found by the reference lists scanning. Finally, we included 16 studies (Aydin Sayilan et al., 2020; Buselli et al., 2020; Chen et al., 2020a; Chor et al., 2020; Cortina‐Rodríguez & Afanador, 2020; Ferry et al., 2020; Hoseinabadi et al., 2020; Hu et al., 2020; Jalili et al., 2020; Khasne et al., 2020; Manzano García & Ayala Calvo, 2020; Matsuo et al., 2020; Prasad et al., 2020; Ruiz‐Fernández et al., 2020; Tan et al., 2020; Zhang et al., 2020) in this systematic review that met our inclusion criteria and among them six studies in the meta‐analysis included the appropriate data.
FIGURE 1.
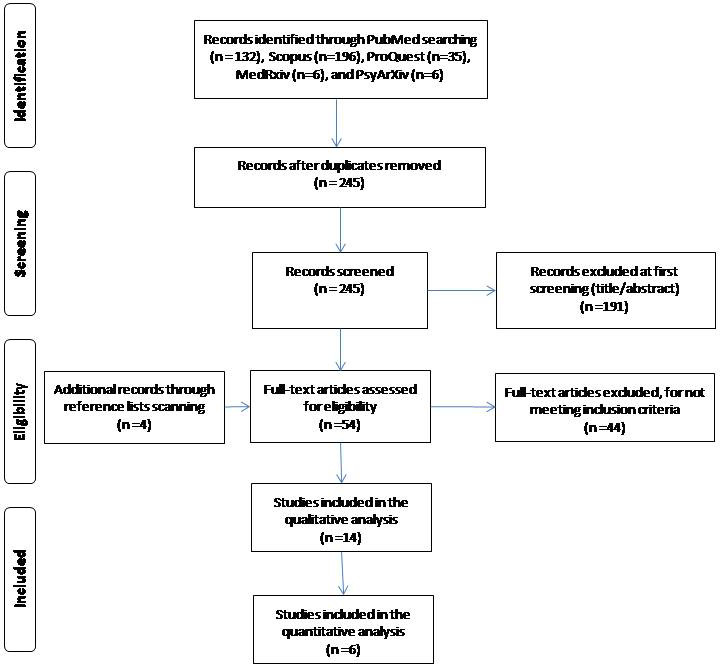
Flowchart of the literature search according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analysis.
3.2. Characteristics of the studies
Main characteristics of the 16 studies included in our systematic review are shown in Table 1. Study population included only nurses in six studies (Aydin Sayilan et al., 2020; Chen et al., 2020a; Hoseinabadi et al., 2020; Hu et al., 2020; Manzano García & Ayala Calvo, 2020; Zhang et al., 2020), while ten studies (Buselli et al., 2020; Chor et al., 2020; Cortina‐Rodríguez & Afanador, 2020; Ferry et al., 2020; Jalili et al., 2020; Khasne et al., 2020; Matsuo et al., 2020; Prasad et al., 2020; Ruiz‐Fernández et al., 2020; Tan et al., 2020) included HCWs in general. A total of 18,935 nurses were included in this systematic review, while two studies (Matsuo et al., 2020; Prasad et al., 2020) did not report the number of nurses. All studies were cross‐sectional, while 13 studies (Buselli et al., 2020; Chen et al., 2020a; Chor et al., 2020; Hoseinabadi et al., 2020; Hoseinabadi et al., 2020; Hu et al., 2020; Jalili et al., 2020; Khasne et al., 2020; Manzano García & Ayala Calvo, 2020; Matsuo et al., 2020; Prasad et al., 2020; Ruiz‐Fernández et al., 2020; Tan et al., 2020; Zhang et al., 2020) used a convenience sampling method, two studies (Cortina‐Rodríguez & Afanador, 2020; Ferry et al., 2020) used a snowball sampling method, and one study used a random sampling method (Aydin Sayilan et al., 2020). Ten studies (Aydin Sayilan et al., 2020; Chen et al., 2020a; Chor et al., 2020; Hoseinabadi et al., 2020; Hu et al., 2020; Jalili et al., 2020; Khasne et al., 2020; Matsuo et al., 2020; Tan et al., 2020; Zhang et al., 2020) were conducted in Asia (China, India, Japan, Turkey, Singapore, Taiwan and Iran), four studies (Buselli et al., 2020; Ferry et al., 2020; García & Calvo, 2020; Ruiz‐Fernández et al., 2020) in Europe (United Kingdom, Spain and Italy) and two studies (Cortina‐Rodríguez & Afanador, 2020; Prasad et al., 2020) in North America (USA and Puerto Rico). Thirteen studies (Aydin Sayilan et al., 2020; Buselli et al., 2020; Chen et al., 2020a; Chor et al., 2020; Hoseinabadi et al., 2020; Hu et al., 2020; Khasne et al., 2020; Manzano García & Ayala Calvo, 2020; Matsuo et al., 2020; Prasad et al., 2020; Ruiz‐Fernández et al., 2020; Tan et al., 2020; Zhang et al., 2020) were published in journals and three studies (Cortina‐Rodríguez & Afanador, 2020; Ferry et al., 2020; Jalili et al., 2020) in pre‐print services. Limited data were available regarding response rate, gender and age.
TABLE 1.
Main characteristics of the studies included in this systematic review.
| Reference | Location | Females (%) | Age, mean (SD) | Sample size (n) | Study design | Sampling method | Assessment tool | Response rate (%) | Data collection time | Publication in |
|---|---|---|---|---|---|---|---|---|---|---|
| Chen et al. (2020a) | China and Taiwan | 95.6 | 33.1 (7.5) | 12,596 | Cross‐sectional | Convenience sampling | MBI | NR | April | Journal |
| Aydin Sayilan et al. (2020) | Turkey | 75.3 | 28 (6) | 267 | Cross‐sectional | Random sampling | MBI | 69.5 | May 10–20 | Journal |
| Buselli et al. (2020) | Italy | NR | NR | 133 | Cross‐sectional | Convenience sampling | ProQOL‐5 | NR | April 1 to May 1 | Journal |
| Chor et al. (2020) | Singapore | NR | NR | 210 | Cross‐sectional | Convenience sampling | CBI | 55.7 | May | Journal |
| Cortina‐Rodríguez and Afanador (2020) | Puerto Rico | NR | NR | 23 | Cross‐sectional | Snowball sampling | MBI | NR | April 25 to May 25 | Pre‐print service |
| Ferry et al. (2020) | United Kingdom | NR | NR | 286 | Cross‐sectional | Snowball sampling | CBI | NR | June 17–24 | Pre‐print service |
| Hu et al. (2020) | China | 87.1 | 31 (6.2) | 2101 | Cross‐sectional | Convenience sampling | MBI | 99.6 | February 13–24 | Journal |
| Khasne et al. (2020) | India | NR | NR | 198 | Cross‐sectional | Convenience sampling | CBI | NR | NR | Journal |
| Jalili et al. (2020) | Iran | NR | NR | 300 | Cross‐sectional | Convenience sampling | MBI | NR | NR | Pre‐print service |
| Manzano García and Ayala Calvo (2020) | Spain | 90 | 42.4 (11.4) | 771 | Cross‐sectional | Convenience sampling | SBI | 39 | April 15–30 | Journal |
| Matsuo et al. (2020) | Japan | 126 | NR | NR | Cross‐sectional | Convenience sampling | MBI | NR | April 6–19 | Journal |
| Prasad et al. (2020) | USA | NR | NR | NR | Cross‐sectional | Convenience sampling | Mini‐Z | NR | April 14–25 | Journal |
| Ruiz‐Fernández et al. (2020) | Spain | NR | NR | 398 | Cross‐sectional | Convenience sampling | ProQoL‐5 | NR | March 30 to April 16 | Journal |
| Zhang et al. (2020) | China | 90.7 | 30.3 (5.5) | 107 | Cross‐sectional | Convenience sampling | MBI | 97 | March 10–14 | Journal |
| Tan et al. (2020) | Singapore | NR | NR | 1394 | Cross‐sectional | Convenience sampling | OLBI | 31.1 | May 29 to May 24 | Journal |
| Hoseinabadi et al. (2020) | Iran | 45.7 | 31.9 (6.5) | 151 | Cross‐sectional | Convenience sampling | OLBI | 92 | March 10 to April 3 | Journal |
Abbreviations: CBI: Copenhagen Burnout Inventory; MBI: Maslach Burnout Inventory; NR: not reported; OLBI: Oldenburg Burnout Inventory; ProQOL‐5: Professional Quality of Life Scale version 5; SBI: Spanish Burnout Inventory; SD: standard deviation.
3.3. Measurement tools for burnout
Six standardized and valid questionnaires were used to measure burnout among nurses. The majority of studies (Aydin Sayilan et al., 2020; Chen et al., 2020a; Cortina‐Rodríguez & Afanador, 2020; Hu et al., 2020; Jalili et al., 2020; Matsuo et al., 2020; Zhang et al., 2020) used the Maslach Burnout Inventory (MBI), three studies (Chor et al., 2020; Ferry et al., 2020; Khasne et al., 2020) used the Copenhagen Burnout Inventory, two studies (Buselli et al., 2020; Ruiz‐Fernández et al., 2020) used the Professional Quality of Life Scale version 5, two studies (Hoseinabadi et al., 2020; Tan et al., 2020) used the Oldenburg Burnout Inventory (OLBI), one study (Prasad et al., 2020) used the Mini‐Z and one study (García & Calvo, 2020) used the Spanish Burnout Inventory.
3.4. Quality assessment
Quality assessment of cross‐sectional studies in this review is shown in Table S1. The most frequent biases were that the studies did not take into account confounding factors and did not apply multivariable methods to eliminate them. Other frequent biases were that the study subjects and the settings were not described in detail and the criteria for inclusion in the sample were not clearly defined.
3.5. Meta‐analysis
Data regarding burnout scales were highly heterogeneous. Regarding the most frequent tool to measure burnout (MBI), the prevalence of nurses' burnout in three subscales (emotional exhaustion, depersonalization and personal accomplishment) was measured in six studies (Aydin Sayilan et al., 2020; Chen et al., 2020a; Cortina‐Rodríguez & Afanador, 2020; Hu et al., 2020; Jalili et al., 2020; Zhang et al., 2020), while the mean burnout scores and standard deviations were measured in four studies (Aydin Sayilan et al., 2020; Chen et al., 2020a; Hu et al., 2020; Zhang et al., 2020). Four different studies (Buselli et al., 2020; Chor et al., 2020; García & Calvo, 2020; Ruiz‐Fernández et al., 2020) measured total mean burnout score with four different instruments, while five other studies (Ferry et al., 2020; Khasne et al., 2020; Matsuo et al., 2020; Prasad et al., 2020; Tan et al., 2020) measured the prevalence of total burnout with four different instruments making the synthesis of these results in meta‐analysis models counterintuitive. Thus, we decided to include in the meta‐analysis the six studies (Aydin Sayilan et al., 2020; Chen et al., 2020a; Cortina‐Rodríguez & Afanador, 2020; Hu et al., 2020; Jalili et al., 2020; Zhang et al., 2020) that calculated the prevalence of nurses' burnout in three subscales of the MBI to improve comprehensiveness and clarity.
Descriptive statistics for nurses' burnout according to the measurement tools used in the studies included in this systematic review and meta‐analysis are shown in Table 2.
TABLE 2.
Descriptive statistics for nurses' burnout scales according to the measurement tools used in the studies included in this systematic review.
| Reference | Assessment tool |
Emotional exhaustion No. of nurses Mean score (SD) |
Depersonalization No. of nurses Mean score (SD) |
Lack of personal accomplishment No. of nurses Mean score (SD) |
Total burnout No. of nurses Mean score (SD) |
Sample size |
|---|---|---|---|---|---|---|
| García & Calvo Chen et al. (2020a) | MBI |
2709 19.1 (10) |
2279 5.5 (4.6) |
145 19 (8.4) |
NR | 12,596 |
| Aydin Sayilan et al. (2020) | MBI |
90 23.7 (7.9) |
3 17.1 (4.6) |
0 17.6 (4.1) |
NR | 267 |
| Buselli et al. (2020) | ProQOL‐5 | NR | NR | NR | 19.9 (4.7) | 133 |
| Chor et al. (2020) | CBI | NR | NR | NR |
112 51.3 (19.6) |
210 |
| Cortina‐Rodríguez and Afanador (2020) | MBI |
16 32 (NR) |
9 9.8 (NR) |
12 32.7 (NR) |
NR | 23 |
| Ferry et al. (2020) | CBI | NR | NR | NR | 245 | 286 |
| Hu et al. (2020) | MBI |
835 23.4 (13.8) |
556 6.8 (7.1) |
771 34.8 (10) |
NR | 2101 |
| Khasne et al. (2020) | CBI |
Personal burnout 101 |
Work‐related burnout 76 |
Pandemic‐related burnout 96 |
NR | 198 |
| Jalili et al. (2020) | MBI | 159 | 40 | 1 | 300 | |
| Manzano García and Ayala Calvo (2020) | SBI | NR | NR | NR | 2.5 (0.3) | 771 |
| Matsuo et al. (2020) | MBI | NR | NR | NR | 59 | 126 |
| Prasad et al. (2020) | Mini‐Z | NR | NR | NR | 83 | 104 |
| Ruiz‐Fernández et al. (2020) | ProQoL‐5 | NR | NR | NR | 24.3 (5.7) | 398 |
| Zhang et al. (2020) | MBI |
6 12.3 (7.1) |
2 2.1 (2.8) |
52 16.5 (8.4) |
NR | 107 |
| Tan et al. (2020) | OLBI |
Exhaustion 2.52 (0.46) |
Disengagement 2.39 (0.43) |
NR | 990 | 1394 |
| Hoseinabadi et al. (2020) | OLBI |
Exhaustion 2.6 (0.2) |
NR | NR | NR | 151 |
Abbreviations: CBI: Copenhagen Burnout Inventory; MBI: Maslach Burnout Inventory; NR: not reported; OLBI: Oldenburg Burnout Inventory; ProQOL‐5: Professional Quality of Life Scale version 5; SBI: Spanish Burnout Inventory; SD: standard deviation.
The overall prevalence of emotional exhaustion among nurses according to the MBI was 34.1% (95% CI: 22.5–46.6%) (Figure 2). The prevalence of emotional exhaustion ranged from 5.6% to 69.6% with a very high heterogeneity between results (I2=98.9%, p‐value for the Hedges Q statistic <0.001). According to meta‐regression analysis, the prevalence was independent of the sample size (p = 0.39). A leave‐one‐out sensitivity analysis showed that removal of studies had an influential effect on the pooled prevalence, which varied between 29.3% (95% CI: 17.9–42.2%), with Cortina‐Rodríguez and Afanador (2020) excluded, and 41.4% (95% CI: 28.2–55.2%), with Zhang et al. (2020) excluded (Figure S1). The asymmetrical shape of the funnel plot (Figure S2) and p‐value <0.05 for Egger's test implied potential publication bias.
FIGURE 2.
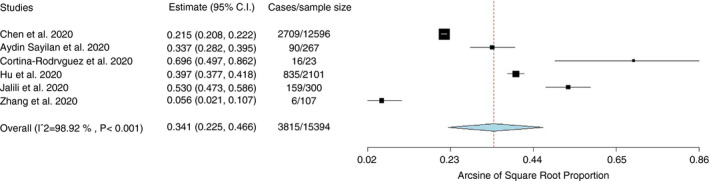
Forest plot of the prevalence of emotional exhaustion among nurses according to the Maslach Burnout Inventory.
Regarding nurses' depersonalization according to the MBI, the pooled prevalence was 12.6% (95% CI: 6.9–19.7%) (Figure 3), while the sample size did not affect it (p = 0.57). The heterogeneity between results was very high (I2=98%, p‐value for the Hedges Q statistic <0.001). Sensitivity analysis showed that removal of studies had a slight effect on the prevalence, which varied between 10.3% (95% CI: 5–17.3%), with Cortina‐Rodríguez and Afanador (2020) excluded, and 16.3% (95% CI: 10.7–22.9%), with Aydin Sayilan et al. (2020) excluded (Figure S3). The funnel plot (Figure S4) and Egger's test (p‐value <0.05) indicated potential publication bias.
FIGURE 3.
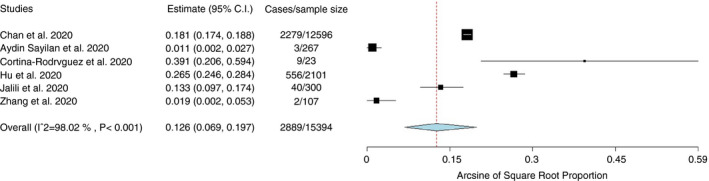
Forest plot of the prevalence of depersonalization among nurses according to the Maslach Burnout Inventory.
The overall prevalence of nurses' lack of personal accomplishment according to the MBI was 15.2% (95% CI: 1.4–39.8%) (Figure 4). Very high heterogeneity between results was identified (I2 = 99.8%, p‐value for the Hedges Q statistic <0.001). Meta‐regression analysis showed that the prevalence was independent of the sample size (p = 0.34). According to leave‐one‐out sensitivity analysis, removal of studies had a moderate effect on the prevalence, which varied between 10.2% (95% CI: 0–34.9%), with Cortina‐Rodríguez and Afanador (2020) excluded, and 20.8% (95% CI: 2.2–51.2%), with Aydin Sayilan et al. (2020) excluded (Figure S5). The asymmetrical shape of the funnel plot (Figure S6) and p‐value<0.05 for Egger's test implied potential publication bias.
FIGURE 4.
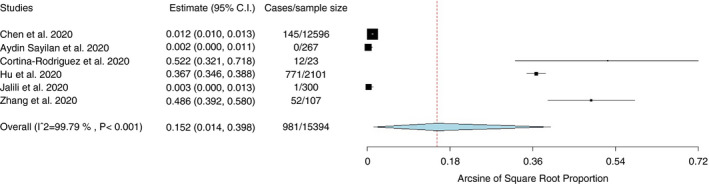
Forest plot of the prevalence of lack of personal accomplishment among nurses according to the Maslach Burnout Inventory.
3.6. Risk factors for burnout
Five studies (Aydin Sayilan et al., 2020; Chen et al., 2020a; García & Calvo, 2020; Hu et al., 2020; Zhang et al., 2020) investigated risk factors for nurses' burnout during the COVID‐19 pandemic and among them three (Aydin Sayilan et al., 2020; Chen et al., 2020a; García & Calvo, 2020; Hu et al., 2020; Zhang et al., 2020) used multivariable models to eliminate confounding factors (Table 3).
TABLE 3.
Risk factors for nurses' burnout during the COVID‐19 pandemic.
| Reference | Emotional exhaustion | Depersonalization | Lack of personal accomplishment | Total burnout | Level of analysis |
|---|---|---|---|---|---|
| Chen et al. (2020a) |
|
|
|
Multivariable | |
| Aydin Sayilan et al. (2020) |
|
Multivariable | |||
| Hu et al. (2020) |
|
|
|
Univariate | |
| Manzano García and Ayala Calvo (2020) |
|
Multivariable | |||
| Zhang et al. (2020) |
|
|
|
Univariate |
Abbreviations: CI: confidence interval; OR: odds ratio; SE: standard error.
Sociodemographic factors (gender, age, educational level and degree) affected nurses' burnout. In particular, two studies (Chen et al., 2020a; Hu et al., 2020) found that females had higher levels of emotional exhaustion, but males had higher level of depersonalization (Hu et al., 2020) and lower level of personal accomplishment (Chen et al., 2020a). Also, younger age (Aydin Sayilan et al., 2020; Zhang et al., 2020), higher educational level (Aydin Sayilan et al., 2020; Hu et al., 2020) and higher degree (Zhang et al., 2020) increased nurses' burnout.
Several social factors increased nurses' burnout such as decreased social support (García & Calvo, 2020), having a relative/friend diagnosed with COVID‐19 (Aydin Sayilan et al., 2020), low family and colleagues readiness to cope with the COVID‐19 outbreak (Hu et al., 2020), increased perceived threat of Covid‐19 (García & Calvo, 2020), and longer working time in quarantine areas (Zhang et al., 2020).
Occupational factors affected nurses' burnout during the COVID‐19 pandemic to a large extent. Nurses that work in a high‐risk environment e.g. a COVID‐19 designated hospital, a COVID‐19 unit or a critical care unit (Aydin Sayilan et al., 2020; Chen et al., 2020a) had higher level of burnout as well as nurses that work in hospitals with inadequate and insufficient material and human resources (García & Calvo, 2020). Also, nurses with lower levels of specialized training regarding COVID‐19, job experience and self‐confidence in caring for COVID‐19 patients experienced burnout more frequently (Hu et al., 2020; Zhang et al., 2020). Increased workload, decreased self‐confidence in self‐protection and decreased working safety while caring for COVID‐19 patients were associated with increased burnout (García & Calvo, 2020; Hu et al., 2020; Zhang et al., 2020).
4. DISCUSSION
We conducted a comprehensive systematic review to investigate the prevalence of nurses' burnout during the COVID‐19 pandemic and to identify associated risk factors. Also, we performed a meta‐analysis examining the prevalence of three aspects of nurses' burnout according to the MBI; emotional exhaustion, depersonalization and lack of personal accomplishment.
We found a significant prevalence of nurses' burnout during the COVID‐19 pandemic according to the MBI. In particular, 34.1%, 15.2% and 12.6% of nurses experienced high levels of emotional exhaustion, low personal accomplishment and depersonalization respectively. These levels of burnout are higher by far even among nurses working in a highly stressful environment such as palliative care; the prevalence of emotional exhaustion, low personal accomplishment and depersonalization is 19.5%, 9.3%, 8.2% respectively (Parola et al., 2017). Another meta‐analysis (Woo et al., 2020) included data from 49 countries and found that the overall prevalence of burnout symptoms among nurses is 11.23%. Nurses during the COVID‐19 pandemic have a higher level of emotional exhaustion, but lower level of depersonalization and higher level of personal accomplishment than mental health nurses (López‐López et al., 2019), nurses in primary health care services (Monsalve‐Reyes et al., 2018), nurses in gynecology and obstetrics services (De la Fuente‐Solana et al., 2019), paediatric nurses (Pradas‐Hernández et al., 2018) and emergency nurses (Gómez‐Urquiza et al., 2017). Nurses' daily emotions have been greatly challenged during the COVID‐19 pandemic since they are a high‐risk group, they have close contact with COVID‐19 patients, and they are afraid of the consequences of the disease. The negative emotions and feelings of patients, colleagues and family members can trigger similar emotions and feelings in nurses influencing perceived stress among them and making them more vulnerable to emotional exhaustion (Joshi & Sharma, 2020). Also, higher job demands, workload, job complexity, job pressure and working time during the COVID‐19 pandemic increases work‐related stress among nurses leading to emotional exhaustion. On the other hand, nurses during the COVID‐19 pandemic experienced depersonalization and low personal accomplishment but not in higher levels than nurses working in a stressful environment such as mental health nurses, nurses in primary health care services, nurses in gynecology and obstetrics services, paediatric nurses and emergency nurses. This may be explained because of empathy and feelings that nurses have developed toward COVID‐19 patients during a frightening situation that impacts all individuals' lives such as a pandemic. A pandemic may trigger compassionate behaviours among nurses connecting them with patients in a deeper level. Also, the effective treatment and care of COVID‐19 patients improve nurses' moral feeling competent and successful in their duty.
Apart from burnout, HCWs experience several other negative psychological outcomes during the COVID‐19 pandemic like depression, anxiety, post‐traumatic stress disorder, psychological distress, sleep disturbances, insomnia and fear (Carmassi et al., 2020; Galli et al., 2020; Kisely et al., 2020; Luo et al., 2020; Pan et al., 2020; Pappa et al., 2020; Raudenská et al., 2020; Salari et al., 2020; Salazar de Pablo et al., 2020; Sanghera et al., 2020; Serrano‐Ripoll et al., 2020; Shaukat et al., 2020; Stuijfzand et al., 2020). The situation is even worse for nurses since it is well‐known that they struggle with burnout symptoms and other psychological issues more often than other HCWs resulting in negative consequences for themselves, their patients, their family members, their colleagues and the health care organizations (Pappa et al., 2020; Parola et al., 2017). Nurses who are exposed and in contact with verified or suspected COVID‐19 patients are more often distressed, nervous and frightened (Rana et al., 2020). Moreover, nurses have extra concerns in the COVID‐19 pandemic like the shortage of personal protective equipment, and the fear of being exposed at work, spreading the SARS‐CoV‐2, and taking the virus home to their close family members (Kisely et al., 2020). Thus, nurses are facing a continuous stress that may trigger post‐traumatic stress, suicide ideation and suicide (Okechukwu et al., 2020). Also, this stress leads to burnout which will negatively affect the quality of health care that nurses provide to patients (Rupert & Morgan, 2005).
We found that several sociodemographic, social and occupational factors increase nurses' burnout during COVID‐19 burnout. Gender is a controversial issue since our review showed that females have higher levels of emotional exhaustion, but males have higher level of depersonalization and lack of personal accomplishment. Also, three studies (Aydin Sayilan et al., 2020; García & Calvo, 2020; Zhang et al., 2020) did not find relation between gender and nurses' burnout increasing the uncertainty about this relation. After exposure to stressful events, females were more likely to be traumatized than males (De Stefano et al., 2018; Jones et al., 2020; Olff et al., 2007). In contrast, a meta‐analysis (Cañadas‐De la Fuente et al., 2018) with 57 studies found that being male is related to a higher level of burnout among nurses. Moderator variables (age, job satisfaction, position, clinical experience, etc.) should be taken into consideration to infer more valid results regarding the role of gender on nurses' burnout. Younger nurses are more likely to exhibit burnout during the COVID‐19 pandemic than older nurses and this might be related to the fact that younger are less familiar with infection control and protective measures and less experienced in handling extreme events such as a pandemic (Tam et al., 2004). Probably, younger nurses are more vulnerable when facing difficult situations such as patients suffer and die from COVID‐19 especially in cases where HCWs cannot offer the standard health care due to sources limitations.
According to our review, decreased social support is related to increased nurses' burnout during the COVID‐19 pandemic. Psychological support that HCWs received during and after a pandemic can significantly influence their feelings and emotions handling in a better way during the negative effects of such a devastating event (Balicer et al., 2006; Kahn et al., 2016). Also, we found that longer working time in quarantine increases nurses' burnout. This result is confirmed by studies with nurses that work in quarantine areas during epidemics where loneliness has been recognized as a significant stressor (Hall et al., 2003; Kim, 2018). Loneliness is magnified in cases that nurses have to separate from their families and stay at designated hospitals as has happened in Wuhan, China (Zhang et al., 2020). Especially family and social support is an essential weapon for nurses to confront the psychological distress that have during epidemic outbreaks (Chan, 2004). A systematic review found that lack of social support is a crucial risk factor for the development of psychological problems in HCWs during disasters (Naushad et al., 2019). Support from families, friends, colleagues and health care organizations gives nurses the opportunity to control effectively and avoid negative feelings and emotions decreasing the danger of burnout syndrome. In particular, several studies show that a strong social support network during the COVID‐19 pandemic can decrease feelings of isolation and strength resilience among HCWs (Hou et al., 2020; Southwick & Southwick, 2020; Wu et al., 2020).
Moreover, we found that nurses having a relative/friend diagnosed with COVID‐19 experience a higher level of burnout. The COVID‐19 pandemic and public health response to it ultimately had changed work and life conditions such as other epidemic outbreaks e.g. SARS. In that case, nurses worry more about the health of their close family members/friends/colleagues than their own (Maunder et al., 2003; Tam et al., 2004). Nurses try to avoid close contact in purpose, to reduce the spread of SARS‐CoV‐2 to their family members/friends/colleagues. Thus, nurses' home and social life are significantly disrupted resulting in fear, anxiety and psychological distress. Also, caring for relatives/friends/colleagues as patients is emotionally difficult and exhausted. Especially in the case that nurses take care of their colleagues suffer from the fear of their own personal vulnerability (Maunder et al., 2003; Tam et al., 2004).
We found that nurses working in a high‐risk clinical environment (a COVID‐19 designated hospital, a COVID‐19 unit, hospitals with inadequate and insufficient material and human resources, low working safety while caring for COVID‐19 patients, etc.) have a higher level of burnout. This finding is confirmed by previous research during the SARS outbreak (Lee et al., 2007). A high‐risk clinical environment is an important source of distress for nurses increasing feelings of loss of control or vulnerability and concerns about the spread of SARS‐CoV‐2, the health of family members/friends/colleagues, and changes in home and work life (Wong et al., 2005). In addition, the severe shortage in personal protective equipment and nursing staff and the increasing number of suspected and actual COVID‐19 cases add more pressure to nurses (Chan‐Yeung, 2004).
Our review identified that poor working conditions like increased workload, low level of specialized training regarding COVID‐19, and increased working times increase the level of burnout among nurses. Several studies have already shown that nurses exhibit burnout due to the prolonged direct personal contact with a great number of patients (Levert et al., 2000; van der Doef et al., 2012) as well as the inadequate staffing and resources (Klopper et al., 2012; Nantsupawat et al., 2017; Toh et al., 2012). Also, poor working conditions are an important risk factor for work‐related stress and job dissatisfaction that end up on high levels of emotional exhaustion, depersonalization and low level of personal accomplishment among nurses (Chayu & Kreitler, 2011; Garrosa et al., 2010; Lasebikan & Oyetunde, 2012; Lee & Akhtar, 2011). A low level of specialized training regarding COVID‐19 is an issue that needs special attention since knowledge, control measures and personal protective equipment against COVID‐19 are limited. Pandemic (H1N1) 2009 (Imai et al., 2010) and SARS epidemic (Liu et al., 2012) underline nurses' concern about inadequate training and expertise in handling challenging health care issues. There is a need for nurses to obtain new knowledge and skills about COVID‐19 to built their confidence in providing health care under this extreme situation. Well‐trained nurses could improve their self‐efficacy that is necessary to confront disasters such a pandemic (Kılıç & Şimşek, 2019).
It is worth noting that protective factors regarding nurses' burnout were found in some studies such as belief in readiness to cope with COVID‐19 outbreak, willingness to participate in frontline work, prior training and experience in COVID‐19 patients' management, protection safety during the clinical work, and increased social support (García & Calvo, 2020; Hu et al., 2020). Since burnout is a multifactorial issue researchers should emphasize the importance of protective factors revealing at least the most important of them.
Another issue that should be addressed is that some variables found not be significantly associated with burnout in multivariable regression analysis but may have important implications and there is a need for further investigation. For instance, working in a COVID‐19 unit, caring for COVID‐19 patients who died, role conflict, role ambiguity and autonomy were not related to burnout (Aydin Sayilan et al., 2020; Chen et al., 2020a; García & Calvo, 2020).
4.1. Limitations
There were some limitations in this systematic review and meta‐analysis. There were different sources of bias. First, only three studies of 16 eliminated confounding through multivariable methods. Usually, control of confounding decreases the value of measures of effect (e.g. odds ratio) and the number of independent variables that are related to the dependent variable (e.g. nurses' burnout). Probably this is the case in our review also but the real effect of confounding on nurses' burnout is impossible to determine. Since nine studies included health care professionals in general and not only nurses, the study subjects and the settings were not described in detail in many studies included in our review. Thus, due to the limited data and the limited number of studies, subgroup analysis and meta‐regression analysis using nurses' characteristics (e.g. gender, age, response rate, etc.) as the independent variables cannot be performed. Another frequent bias was that the criteria for inclusion in the study sample were not clearly defined. In that case, we cannot be certain about the direction of effects on nurses' burnout since we cannot understand the study participants in a clear way. Finally, in some cases, the exposure was not measured in a valid and reliable way and a misclassification bias is possible.
Also, only one study used a random sample, nine studies had a small sample size (≤300 nurses), and three studies collected data from China. Thus representativeness may be a potential limitation and studies with large random samples worldwide should be conducted.
Data regarding risk factors for nurses' burnout during the COVID‐19 pandemic were available only in five studies and among them, three used multivariable methods to eliminate confounders. Also, several risk factors (social support, relatives diagnosed with COVID‐19, insufficient resources and longer working time in quarantine areas) were examined only in one study and further research is needed to infer valid results.
Moreover, we searched five major databases and pre‐print services as well as the full reference lists of all selected articles but there is still the probability to not identify some studies e.g. in grey literature. Also, we did not use MeSH terms in our search strategy and papers may be omitted. The heterogeneity between results was very high and we applied random effects model to handle this issue. Additionally, we included studies that used standardized and valid instruments to measure burnout but these data are still self‐reported and inherently subjective. Moreover, only cross‐sectional studies with convenience or snowball sampling method were identified making definite causal relationships impossible.
5. CONCLUSION
Nurses experience high levels of burnout during the COVID‐19 pandemic, while several sociodemographic, social and occupational factors affect this burnout. The COVID‐19 pandemic is a significant challenge for nurses worldwide and learning lessons from the first wave is imperative to prepare better strategies for the subsequent waves. Several measures could be introduced to mitigate the mental health impact of the COVID‐19 pandemic on nurses, e.g. screening for mental health illness and early supportive interventions for high‐risk nurses, immediate access to mental health care services, designated rest periods, social support through hospital support groups to reduce feelings of isolation, sufficient personal protective equipment for all nurses to provide security etc. As the second wave of the COVID‐19 pandemic is hitting worldwide and there are predictions for the following waves in the near future, there is a need to decrease nurses' burnout and improve their mental health. Governments, health care organizations, and policymakers should act in this direction to prepare health care systems, individuals and nurses for a better response against the COVID‐19 pandemic.
CONFLICTS OF INTEREST
None.
AUTHOR CONTRIBUTIONS
P.G., I.V. and D.K. were responsible for the conception and design of the study. P.G., I.V., D.F. and A.B. were responsible for the acquisition, analysis and interpretation of the data. All the authors drafted the article or revised it critically for important intellectual content, and provided final approval of the version to be submitted.
Peer Review
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.14839.
Supporting information
Fig S1
Fig S2
Fig S3
Fig S4
Fig S5
Fig S6
Table S1
Funding information
None.
REFERENCES
- Adriaenssens, J. , De Gucht, V. , & Maes, S. (2015). Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. International Journal of Nursing Studies, 52(2), 649–661. 10.1016/j.ijnurstu.2014.11.004 [DOI] [PubMed] [Google Scholar]
- Al Maqbali, M. , Al Sinani, M. , & Al‐Lenjawi, B. (2021). Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID‐19 pandemic: A systematic review and meta‐analysis. Journal of Psychosomatic Research, 141, 110343. 10.1016/j.jpsychores.2020.110343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aydin Sayilan, A. , Kulakaç, N. , & Uzun, S. (2020). Burnout levels and sleep quality of COVID‐19 heroes. Perspectives in Psychiatric Care, 10.1111/ppc.12678 [DOI] [PubMed] [Google Scholar]
- Balicer, R. D. , Omer, S. B. , Barnett, D. J. , & Everly, G. S. (2006). Local public health workers' perceptions toward responding to an influenza pandemic. BMC Public Health, 6(1), 99. 10.1186/1471-2458-6-99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandyopadhyay, S. , Baticulon, R. E. , Kadhum, M. , Alser, M. , Ojuka, D. K. , Badereddin, Y. , Kamath, A. , Parepalli, S. A. , Brown, G. , Iharchane, S. , Gandino, S. , Markovic‐Obiago, Z. , Scott, S. , Manirambona, E. , Machhada, A. , Aggarwal, A. , Benazaize, L. , Ibrahim, M. , Kim, D. , … Khundkar, R. (2020). Infection and mortality of healthcare workers worldwide from COVID‐19: A systematic review. BMJ Global Health, 5(12), e003097. 10.1136/bmjgh-2020-003097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barendregt, J. J. , Doi, S. A. , Lee, Y. Y. , Norman, R. E. , & Vos, T. (2013). Meta‐analysis of prevalence. Journal of Epidemiology and Community Health, 67(11), 974–978. 10.1136/jech-2013-203104 [DOI] [PubMed] [Google Scholar]
- Buselli, R. , Corsi, M. , Baldanzi, S. , Chiumiento, M. , Del Lupo, E. , Dell'Oste, V. , Bertelloni, C. A. , Massimetti, G. , Dell'Osso, L. , Cristaudo, A. , & Carmassi, C. (2020). Professional quality of life and mental health outcomes among health care workers exposed to Sars‐Cov‐2 (Covid‐19). International Journal of Environmental Research and Public Health, 17(17), 6180. 10.3390/ijerph17176180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cañadas‐De la Fuente, G. , Ortega, E. , Ramirez‐Baena, L. , De la Fuente‐Solana, E. , Vargas, C. , & Gómez‐Urquiza, J. (2018). Gender, marital status, and children as risk factors for burnout in nurses: A meta‐analytic study. International Journal of Environmental Research and Public Health, 15(10), 2102. 10.3390/ijerph15102102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi, C. , Foghi, C. , Dell'Oste, V. , Cordone, A. , Bertelloni, C. A. , Bui, E. , & Dell'Osso, L. (2020). PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID‐19 pandemic. Psychiatry Research, 292, 113312. 10.1016/j.psychres.2020.113312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, A. O. M. (2004). Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occupational Medicine, 54(3), 190–196. 10.1093/occmed/kqh027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, J.‐W. , Yuan, S. , Kok, K.‐H. , To, K.‐W. , Chu, H. , Yang, J. , Xing, F. , Liu, J. , Yip, C.‐Y. , Poon, R.‐S. , Tsoi, H.‐W. , Lo, S.‐F. , Chan, K.‐H. , Poon, V.‐M. , Chan, W.‐M. , Ip, J. D. , Cai, J.‐P. , Cheng, V.‐C. , Chen, H. , … Yuen, K.‐Y. (2020). A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person‐to‐person transmission: A study of a family cluster. The Lancet, 395(10223), 514–523. 10.1016/S0140-6736(20)30154-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan‐Yeung, M. (2004). Severe acute respiratory syndrome (SARS) and healthcare workers. International Journal of Occupational and Environmental Health, 10(4), 421–427. 10.1179/oeh.2004.10.4.421 [DOI] [PubMed] [Google Scholar]
- Chayu, T. , & Kreitler, S. (2011). Burnout in nephrology nurses in Israel. Nephrology Nursing Journal: Journal of the American Nephrology Nurses' Association, 38(1), 65–77, quiz 78. [PubMed] [Google Scholar]
- Chen, R. , Sun, C. , Chen, J.‐J. , Jen, H.‐J. , Kang, X. L. , Kao, C.‐C. , & Chou, K.‐R. (2020a). A large‐scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID‐19 pandemic. International Journal of Mental Health Nursing, 30(1), 102–116. 10.1111/inm.12796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, X. , Chen, Z. , Azman, A. S. , Deng, X. , Chen, X. , Lu, W. , Zhao, Z. , Yang, J. , Viboud, C. , Ajelli, M. , Leung, D. T. , & Yu, H. (2020b). Serological evidence of human infection with SARS‐CoV‐2: A systematic review and meta‐analysis [Preprint]. Epidemiology, 10.1101/2020.09.11.20192773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chor, W. P. D. , Ng, W. M. , Cheng, L. , Situ, W. , Chong, J. W. , Ng, L. Y. A. , Mok, P. L. , Yau, Y. W. , & Lin, Z. (2020). Burnout amongst emergency healthcare workers during the COVID‐19 pandemic: A multi‐center study. The American Journal of Emergency Medicine, 10.1016/j.ajem.2020.10.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortina‐Rodríguez, G. , & Afanador, Y. (2020). Burnout in the clinical personnel of Puerto Rico during the COVID‐19 pandemic [Preprint]. Behavioral Sciences. 10.20944/preprints202007.0451.v1 [DOI] [Google Scholar]
- De la Fuente‐Solana, E. I. , Suleiman‐Martos, N. , Pradas‐Hernández, L. , Gomez‐Urquiza, J. L. , Cañadas‐De la Fuente, G. A. , & Albendín‐García, L. (2019). Prevalence, related factors, and levels of burnout syndrome among nurses working in gynecology and obstetrics services: A systematic review and meta‐analysis. International Journal of Environmental Research and Public Health, 16(14), 2585. 10.3390/ijerph16142585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Stefano, C. , Orri, M. , Agostinucci, J. M. , Zouaghi, H. , Lapostolle, F. , Baubet, T. , & Adnet, F. (2018). Early psychological impact of Paris terrorist attacks on healthcare emergency staff: A cross‐sectional study. Depression and Anxiety, 35(3), 275–282. 10.1002/da.22724 [DOI] [PubMed] [Google Scholar]
- dos Santos, W. M. , Secoli, S. R. , & Püschel, V. A. d. A. (2018). The Joanna Briggs Institute approach for systematic reviews. Revista Latino‐Americana De Enfermagem, 26, 10.1590/1518-8345.2885.3074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger, M. , Smith, G. D. , Schneider, M. , & Minder, C. (1997). Bias in meta‐analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferry, A. V. , Wereski, R. , Strachan, F. E. , & Mills, N. L. (2020). Predictors of healthcare worker burnout during the COVID‐19 pandemic. MedRxiv, 2020.08.26.20182378. 10.1101/2020.08.26.20182378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanis, P. , Vraka, I. , Fragkou, D. , Bilali, A. , & Kaitelidou, D. (2020). Seroprevalence of SARS‐CoV‐2 antibodies and associated factors in health care workers: A systematic review and meta‐analysis. Journal of Hospital Infection, 108, 120–134. 10.1016/j.jhin.2020.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galli, F. , Pozzi, G. , Ruggiero, F. , Mameli, F. , Cavicchioli, M. , Barbieri, S. , Canevini, M. P. , Priori, A. , Pravettoni, G. , Sani, G. , & Ferrucci, R. (2020). A systematic review and provisional metanalysis on psychopathologic burden on health care workers of coronavirus outbreaks. Frontiers in Psychiatry, 11, 568664. 10.3389/fpsyt.2020.568664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrosa, E. , Rainho, C. , Moreno‐Jiménez, B. , & Monteiro, M. J. (2010). The relationship between job stressors, hardy personality, coping resources and burnout in a sample of nurses: A correlational study at two time points. International Journal of Nursing Studies, 47(2), 205–215. 10.1016/j.ijnurstu.2009.05.014 [DOI] [PubMed] [Google Scholar]
- Gómez‐Urquiza, J. , Aneas‐López, A. , Fuente‐Solana, E. , Albendín‐García, L. , Díaz‐Rodríguez, L. , & Fuente, G. (2016). Prevalence, risk factors, and levels of burnout among oncology nurses: A systematic review. Oncology Nursing Forum, 43(3), E104–E120. 10.1188/16.ONF.E104-E120 [DOI] [PubMed] [Google Scholar]
- Gómez‐Urquiza, J. L. , De la Fuente‐Solana, E. I. , Albendín‐García, L. , Vargas‐Pecino, C. , Ortega‐Campos, E. M. , & Cañadas‐De la Fuente, G. A. (2017). Prevalence of burnout syndrome in emergency nurses: A meta‐analysis. Critical Care Nurse, 37(5), e1–e9. 10.4037/ccn2017508 [DOI] [PubMed] [Google Scholar]
- García, M. , & Calvo, A. (2020). The threat of COVID‐19 and its influence on nursing staff burnout. Journal of Advanced Nursing, 77(2), 832–844. 10.1111/jan.14642 [DOI] [PubMed] [Google Scholar]
- Hall, L. M. , Angus, J. , Peter, E. , O'Brien‐Pallas, L. , Wynn, F. , & Donner, G. (2003). Media portrayal of nurses' perspectives and concerns in the SARS crisis in Toronto. Journal of Nursing Scholarship, 35(3), 211–216. 10.1111/j.1547-5069.2003.00211.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. T. (2003). Measuring inconsistency in meta‐analyses. BMJ, 327(7414), 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. T. , Thomas, J. , Chandler, J. , Cumpston, M. , Li, T. , Page, M. , & Welch, V. (2019). Cochrane handbook for systematic reviews of interventions (2nd ed.). WILEY Blackwell. [Google Scholar]
- Hoseinabadi, T. , Kakhki, S. , Teimori, G. , & Nayyeri, S. (2020). Burnout and its influencing factors between frontline nurses and nurses from other wards during the outbreak of Coronavirus Disease ‐COVID‐19‐ in Iran. Investigación Y Educación En Enfermería, 38(2), e03. 10.17533/udea.iee.v38n2e03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou, T. , Zhang, T. , Cai, W. , Song, X. , Chen, A. , Deng, G. , & Ni, C. (2020). Social support and mental health among health care workers during Coronavirus Disease 2019 outbreak: A moderated mediation model. PLoS One, 15(5), e0233831. 10.1371/journal.pone.0233831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, D. , Kong, Y. , Li, W. , Han, Q. , Zhang, X. , Zhu, L. X. , Wan, S. W. , Liu, Z. , Shen, Q. , Yang, J. , He, H.‐G. , & Zhu, J. (2020). Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID‐19 outbreak in Wuhan, China: A large‐scale cross‐sectional study. EClinicalMedicine, 24, 100424. 10.1016/j.eclinm.2020.100424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai, H. , Matsuishi, K. , Ito, A. , Mouri, K. , Kitamura, N. , Akimoto, K. , Mino, K. , Kawazoe, A. , Isobe, M. , Takamiya, S. , & Mita, T. (2010). Factors associated with motivation and hesitation to work among health professionals during a public crisis: A cross sectional study of hospital workers in Japan during the pandemic (H1N1) 2009. BMC Public Health, 10(1), 672. 10.1186/1471-2458-10-672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Council of Nurses . (2020). ICN confirms 1,500 nurses have died from COVID‐19 in 44 countries and estimates that healthcare worker COVID‐19 fatalities worldwide could be more than 20,000. [Google Scholar]
- Jalili, M. , Niroomand, M. , Hadavand, F. , Zeinali, K. , & Fotouhi, A. (2020). Burnout among healthcare professionals during COVID‐19 pandemic: A cross‐sectional study [Preprint]. Occupational and Environmental Health, 10.1101/2020.06.12.20129650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang, X. , Rayner, S. , & Luo, M. (2020). Does SARS‐CoV‐2 has a longer incubation period than SARS and MERS? Journal of Medical Virology, 92(5), 476–478. 10.1002/jmv.25708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, G. A. L. , Colville, G. A. , Ramnarayan, P. , Woolfall, K. , Heward, Y. , Morrison, R. , Savage, A. , Fraser, J. , Griksaitis, M. J. , & Inwald, D. P. (2020). Psychological impact of working in paediatric intensive care. A UK‐wide prevalence study. Archives of Disease in Childhood, 105(5), 470–475. 10.1136/archdischild-2019-317439 [DOI] [PubMed] [Google Scholar]
- Joo, J. Y. , & Liu, M. F. (2021). Nurses' barriers to caring for patients with COVID‐19: A qualitative systematic review. International Nursing Review, 10.1111/inr.12648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi, G. , & Sharma, G. (2020). Burnout: A risk factor amongst mental health professionals during COVID‐19. Asian Journal of Psychiatry, 54, 102300. 10.1016/j.ajp.2020.102300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn, M.D. , Bulanda, J. J. , Weissberger, A. , Jalloh, S. , Von Villa, E. , & Williams, A. (2016). Evaluation of a support group for Ebola hotline workers in Sierra Leone. International Journal of Culture and Mental Health, 9(2), 164–171. 10.1080/17542863.2016.1153121 [DOI] [Google Scholar]
- Khasne, R. W. , Dhakulkar, B. S. , Mahajan, H. C. , & Kulkarni, A. P. (2020). Burnout among healthcare workers during COVID‐19 pandemic in India: Results of a questionnaire‐based survey. Indian Journal of Critical Care Medicine, 24(8), 664–671. 10.5005/jp-journals-10071-23518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kılıç, N. , & Şimşek, N. (2019). The effects of psychological first aid training on disaster preparedness perception and self‐efficacy. Nurse Education Today, 83, 104203. 10.1016/j.nedt.2019.104203 [DOI] [PubMed] [Google Scholar]
- Kim, Y. (2018). Nurses' experiences of care for patients with Middle East respiratory syndrome‐coronavirus in South Korea. American Journal of Infection Control, 46(7), 781–787. 10.1016/j.ajic.2018.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely, S. , Warren, N. , McMahon, L. , Dalais, C. , Henry, I. , & Siskind, D. (2020). Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta‐analysis. BMJ, 369, m1642. 10.1136/bmj.m1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klopper, H. C. , Coetzee, S. K. , Pretorius, R. , & Bester, P. (2012). Practice environment, job satisfaction and burnout of critical care nurses in South Africa. Journal of Nursing Management, 20(5), 685–695. 10.1111/j.1365-2834.2011.01350.x [DOI] [PubMed] [Google Scholar]
- Lasebikan, V. O. , & Oyetunde, M. O. (2012). Burnout among nurses in a Nigerian general hospital: Prevalence and associated factors. ISRN Nursing, 2012, 402157. 10.5402/2012/402157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, A. M. , Wong, J. G. , McAlonan, G. M. , Cheung, V. , Cheung, C. , Sham, P. C. , Chu, C.‐M. , Wong, P.‐C. , Tsang, K. W. , & Chua, S. E. (2007). Stress and psychological distress among SARS survivors 1 year after the outbreak. The Canadian Journal of Psychiatry, 52(4), 233–240. 10.1177/070674370705200405 [DOI] [PubMed] [Google Scholar]
- Lee, J. S. Y. , & Akhtar, S. (2011). Effects of the workplace social context and job content on nurse burnout. Human Resource Management, 50(2), 227–245. 10.1002/hrm.20421 [DOI] [Google Scholar]
- Levert, T. , Lucas, M. , & Ortlepp, K. (2000). Burnout in psychiatric nurses: Contributions of the work environment and a sense of coherence. South African Journal of Psychology, 30(2), 36–43. 10.1177/008124630003000205 [DOI] [Google Scholar]
- Liu, Q. , Shen, D. , Chen, S. , & Liu, J. (2020). Supporting frontline nurses during the fight against COVID‐19. Journal of the American Psychiatric Nurses Association, 26(6), 525–526. 10.1177/1078390320946825 [DOI] [PubMed] [Google Scholar]
- Liu, X. , Kakade, M. , Fuller, C. J. , Fan, B. , Fang, Y. , Kong, J. , Guan, Z. , & Wu, P. (2012). Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive Psychiatry, 53(1), 15–23. 10.1016/j.comppsych.2011.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- López‐López, I. M. , Gómez‐Urquiza, J. L. , Cañadas, G. R. , De la Fuente, E. I. , Albendín‐García, L. , & Cañadas‐De la Fuente, G. A. (2019). Prevalence of burnout in mental health nurses and related factors: A systematic review and meta‐analysis. International Journal of Mental Health Nursing, 28(5), 1035–1044. 10.1111/inm.12606 [DOI] [PubMed] [Google Scholar]
- Luo, M. , Guo, L. , Yu, M. , Jiang, W. , & Wang, H. (2020). The psychological and mental impact of coronavirus disease 2019 (COVID‐19) on medical staff and general public – A systematic review and meta‐analysis. Psychiatry Research, 291, 113190. 10.1016/j.psychres.2020.113190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuo, T. , Kobayashi, D. , Taki, F. , Sakamoto, F. , Uehara, Y. , Mori, N. , & Fukui, T. (2020). Prevalence of health care worker burnout during the coronavirus disease 2019 (COVID‐19) pandemic in Japan. JAMA Network Open, 3(8), e2017271. 10.1001/jamanetworkopen.2020.17271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder, R. , Hunter, J. , Vincent, L. , Bennett, J. , Peladeau, N. , Leszcz, M. , Sadavoy, J. , Verhaeghe, L. M. , Steinberg, R. , & Mazzulli, T. (2003). The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Canadian Medical Association Journal, 168(10), 1245–1251. [PMC free article] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , & Altman, D. G. ; The PRISMA Group . (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. PLoS Med, 6(7), e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monsalve‐Reyes, C. S. , San Luis‐Costas, C. , Gómez‐Urquiza, J. L. , Albendín‐García, L. , Aguayo, R. , & Cañadas‐De la Fuente, G. A. (2018). Burnout syndrome and its prevalence in primary care nursing: A systematic review and meta‐analysis. BMC Family Practice, 19(1), 59. 10.1186/s12875-018-0748-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nantsupawat, A. , Kunaviktikul, W. , Nantsupawat, R. , Wichaikhum, O.‐A. , Thienthong, H. , & Poghosyan, L. (2017). Effects of nurse work environment on job dissatisfaction, burnout, intention to leave. International Nursing Review, 64(1), 91–98. 10.1111/inr.12342 [DOI] [PubMed] [Google Scholar]
- National Nurses United . (2020). Sins of ommision. How government failures to track Covid‐19 data have led to more than 1,700 health care worker deaths and jeopardize public health. [Google Scholar]
- Naushad, V. A. , Bierens, J. J. , Nishan, K. P. , Firjeeth, C. P. , Mohammad, O. H. , Maliyakkal, A. M. , ChaliHadan, S. , & Schreiber, M. D. (2019). A systematic review of the impact of disaster on the mental health of medical responders. Prehospital and Disaster Medicine, 34(6), 632–643. 10.1017/S1049023X19004874 [DOI] [PubMed] [Google Scholar]
- Okechukwu, C. , Tibaldi, L. , & La Torre, G. (2020). The impact of COVID‐19 pandemic on mental health of nurses. La Clinica Terapeutica, 5, 399–400. 10.7417/CT.2020.2247 [DOI] [PubMed] [Google Scholar]
- Olff, M. , Langeland, W. , Draijer, N. , & Gersons, B. P. R. (2007). Gender differences in posttraumatic stress disorder. Psychological Bulletin, 133(2), 183–204. 10.1037/0033-2909.133.2.183 [DOI] [PubMed] [Google Scholar]
- Owuor, R. A. , Mutungi, K. , Anyango, R. , & Mwita, C. C. (2020). Prevalence of burnout among nurses in sub‐Saharan Africa: A systematic review. JBI Evidence Synthesis, 18(6), 1189–1207. 10.11124/JBISRIR-D-19-00170 [DOI] [PubMed] [Google Scholar]
- Pan, R. , Zhang, L. , & Pan, J. (2020). The anxiety status of Chinese medical workers during the epidemic of COVID‐19: A meta‐analysis. Psychiatry Investigation, 17(5), 475–480. 10.30773/pi.2020.0127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa, S. , Ntella, V. , Giannakas, T. , Giannakoulis, V. G. , Papoutsi, E. , & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. Brain, Behavior, and Immunity, 88, 901–907. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parola, V. , Coelho, A. , Cardoso, D. , Sandgren, A. , & Apóstolo, J. (2017). Prevalence of burnout in health professionals working in palliative care: A systematic review. JBI Database of Systematic Reviews and Implementation Reports, 15(7), 1905–1933. 10.11124/JBISRIR-2016-003309 [DOI] [PubMed] [Google Scholar]
- Pradas‐Hernández, L. , Ariza, T. , Gómez‐Urquiza, J. L. , Albendín‐García, L. , De la Fuente, E. I. , & Cañadas‐De la Fuente, G. A. (2018). Prevalence of burnout in paediatric nurses: A systematic review and meta‐analysis. PLoS One, 13(4), e0195039. 10.1371/journal.pone.0195039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad, A. , Civantos, A. M. , Byrnes, Y. , Chorath, K. , Poonia, S. , Chang, C. , Graboyes, E. M. , Bur, A. M. , Thakkar, P. , Deng, J. , Seth, R. , Trosman, S. , Wong, A. , Laitman, B. M. , Shah, J. , Stubbs, V. , Long, Q. I. , Choby, G. , Rassekh, C. H. , … Rajasekaran, K. (2020). Snapshot impact of COVID‐19 on mental wellness in nonphysician otolaryngology health care workers: A national study. OTO Open, 4(3), 2473974X20948835. 10.1177/2473974X20948835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rana, W. , Mukhtar, S. , & Mukhtar, S. (2020). Mental health of medical workers in Pakistan during the pandemic COVID‐19 outbreak. Asian Journal of Psychiatry, 51, 102080. 10.1016/j.ajp.2020.102080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenská, J. , Steinerová, V. , Javůrková, A. , Urits, I. , Kaye, A. D. , Viswanath, O. , & Varrassi, G. (2020). Occupational burnout syndrome and post‐traumatic stress among healthcare professionals during the novel coronavirus disease 2019 (COVID‐19) pandemic. Best Practice & Research. Clinical Anaesthesiology, 34(3), 553–560. 10.1016/j.bpa.2020.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz‐Fernández, M. D. , Ramos‐Pichardo, J. D. , Ibáñez‐Masero, O. , Cabrera‐Troya, J. , Carmona‐Rega, M. I. , & Ortega‐Galán, Á. M. (2020). Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID‐19 health crisis in Spain. Journal of Clinical Nursing, 29(21‐22), 4321–4330. 10.1111/jocn.15469 [DOI] [PubMed] [Google Scholar]
- Rupert, P. A. , & Morgan, D. J. (2005). Work setting and burnout among professional psychologists. Professional Psychology: Research and Practice, 36(5), 544–550. 10.1037/0735-7028.36.5.544 [DOI] [Google Scholar]
- Salari, N. , Khazaie, H. , Hosseinian‐Far, A. , Ghasemi, H. , Mohammadi, M. , Shohaimi, S. , Daneshkhah, A. , Khaledi‐Paveh, B. , & Hosseinian‐Far, M. (2020). The prevalence of sleep disturbances among physicians and nurses facing the COVID‐19 patients: A systematic review and meta‐analysis. Globalization and Health, 16(1), 92. 10.1186/s12992-020-00620-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar de Pablo, G. , Vaquerizo‐Serrano, J. , Catalan, A. , Arango, C. , Moreno, C. , Ferre, F. , Shin, J. I. , Sullivan, S. , Brondino, N. , Solmi, M. , & Fusar‐Poli, P. (2020). Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta‐analysis. Journal of Affective Disorders, 275, 48–57. 10.1016/j.jad.2020.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanghera, J. , Pattani, N. , Hashmi, Y. , Varley, K. F. , Cheruvu, M. S. , Bradley, A. , & Burke, J. R. (2020). The impact of SARS‐CoV‐2 on the mental health of healthcare workers in a hospital setting: A systematic review. Journal of Occupational Health, 62(1), e12175. 10.1002/1348-9585.12175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serrano‐Ripoll, M. J. , Meneses‐Echavez, J. F. , Ricci‐Cabello, I. , Fraile‐Navarro, D. , Fiol‐deRoque, M. A. , Pastor‐Moreno, G. , Castro, A. , Ruiz‐Pérez, I. , Zamanillo Campos, R. , & Gonçalves‐Bradley, D. C. (2020). Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta‐analysis. Journal of Affective Disorders, 277, 347–357. 10.1016/j.jad.2020.08.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaukat, N. , Ali, D. M. , & Razzak, J. (2020). Physical and mental health impacts of COVID‐19 on healthcare workers: A scoping review. International Journal of Emergency Medicine, 13(1), 40. 10.1186/s12245-020-00299-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwick, S. M. , & Southwick, F. S. (2020). The loss of social connectedness as a major contributor to physician burnout: Applying organizational and teamwork principles for prevention and recovery. JAMA Psychiatry, 77(5), 449. 10.1001/jamapsychiatry.2019.4800 [DOI] [PubMed] [Google Scholar]
- Stuijfzand, S. , Deforges, C. , Sandoz, V. , Sajin, C.‐T. , Jaques, C. , Elmers, J. , & Horsch, A. (2020). Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: A rapid review. BMC Public Health, 20(1), 1230. 10.1186/s12889-020-09322-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tam, C. W. C. , Pang, E. P. F. , Lam, L. C. W. , & Chiu, H. F. K. (2004). Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers. Psychological Medicine, 34(7), 1197–1204. 10.1017/s0033291704002247 [DOI] [PubMed] [Google Scholar]
- Tan, B. Y. Q. , Kanneganti, A. , Lim, L. J. H. , Tan, M. , Chua, Y. X. , Tan, L. , Sia, C. H. , Denning, M. , Goh, E. T. , Purkayastha, S. , Kinross, J. , Sim, K. , Chan, Y. H. , & Ooi, S. B. S. (2020). Burnout and associated factors among health care workers in Singapore during the COVID‐19 pandemic. Journal of the American Medical Directors Association, 21(12), 1751–1758.e5. 10.1016/j.jamda.2020.09.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toh, S. G. , Ang, E. , & Devi, M. K. (2012). Systematic review on the relationship between the nursing shortage and job satisfaction, stress and burnout levels among nurses in oncology/haematology settings. International Journal of Evidence‐Based Healthcare, 10(2), 126–141. 10.1111/j.1744-1609.2012.00271.x [DOI] [PubMed] [Google Scholar]
- van der Doef, M. , Mbazzi, F. B. , & Verhoeven, C. (2012). Job conditions, job satisfaction, somatic complaints and burnout among East African nurses. Journal of Clinical Nursing, 21(11–12), 1763–1775. 10.1111/j.1365-2702.2011.03995.x [DOI] [PubMed] [Google Scholar]
- Wallace, B. C. , Schmid, C. H. , Lau, J. , & Trikalinos, T. A. (2009). Meta‐Analyst: Software for meta‐analysis of binary, continuous and diagnostic data. BMC Medical Research Methodology, 9(1), 80. 10.1186/1471-2288-9-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Coronavirus Disease (COVID‐19) Dashboard . (2020). (n.d.). Retrieved from https://covid19.who.int/
- Wong, T. W. , Yau, J. K. Y. , Chan, C. L. W. , Kwong, R. S. Y. , Ho, S. M. Y. , Lau, C. C. , Lau, F. L. , & Lit, C. H. (2005). The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. European Journal of Emergency Medicine, 12(1), 13–18. 10.1097/00063110-200502000-00005 [DOI] [PubMed] [Google Scholar]
- Woo, T. , Ho, R. , Tang, A. , & Tam, W. (2020). Global prevalence of burnout symptoms among nurses: A systematic review and meta‐analysis. Journal of Psychiatric Research, 123, 9–20. 10.1016/j.jpsychires.2019.12.015 [DOI] [PubMed] [Google Scholar]
- Wu, P. E. , Styra, R. , & Gold, W. L. (2020). Mitigating the psychological effects of COVID‐19 on health care workers. Canadian Medical Association Journal, 192(17), E459–E460. 10.1503/cmaj.200519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhan, Y. , Ma, S. , Jian, X. , Cao, Y. , & Zhan, X. (2020). The current situation and influencing factors of job stress among frontline nurses assisting in Wuhan in fighting COVID‐19. Frontiers in Public Health, 8, 579866. 10.3389/fpubh.2020.579866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. , Wang, C. , Pan, W. , Zheng, J. , Gao, J. , Huang, X. , Cai, S. , Zhai, Y. , Latour, J. M. , & Zhu, C. (2020). Stress, burnout, and coping strategies of frontline nurses during the COVID‐19 epidemic in Wuhan and Shanghai, China. Frontiers in Psychiatry, 11, 565520. 10.3389/fpsyt.2020.565520 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1
Fig S2
Fig S3
Fig S4
Fig S5
Fig S6
Table S1


