The whole world has been struggling to cope with the SARS‐CoV‐2 pandemic since the beginning of 2020.
The measures initially used to combat the epidemic were nonpharmaceutical, such as physical distancing, mask wearing, tightened basic hygiene, quarantine, and even curfews. These measures were applied, accepted, and effective to varying degrees, depending on the country.
Their application did reduce the transmission of SARS‐CoV‐2 and decreased the virus reproductive number R0. However, the epidemic flared up from time to time and new waves of epidemic appeared, undoubtedly due to noncompliance and/or the partial lifting of containment measures such as curfews and movement restriction.
Such measures effectively control the transmission of other viral pathogens with or without respiratory tropism, 1 , 2 as has been demonstrated in the Southern Hemisphere. 3 But few data are available on the circulation of respiratory syncytial viruses (RSV) and rhinoviruses during the SARS‐CoV‐2 pandemic as the surveillance networks are more concerned with influenza.
Our university hospital has been monitoring these three types of virus for the past 10 years. We have found that RSVs are first detected at the beginning of winter, usually between Weeks 40 and 43 (the second half of October) while influenza viruses appear later, from mid‐December to early January. Unlike these viruses, rhinoviruses are endemic throughout the year and their prevalence in winter varies from 20% to 35% in our area depending on the year.
The circulation of flu, RSV and rhinoviruses during the first winter in which SARS‐CoV‐2 was controlled using only nonpharmaceutical methods was quite special. The effectiveness of these measures seems to depend on the prior circulation of the particular virus (Figure 1).
Figure 1.
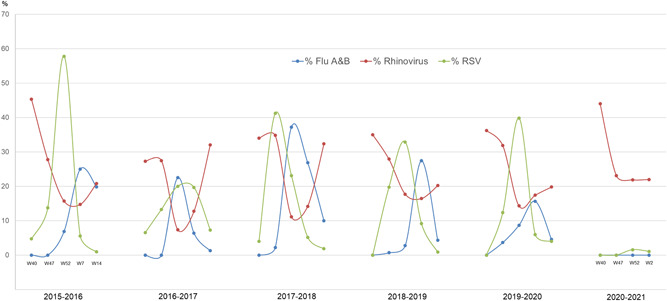
Schematic winter distribution (% of positive samples) for Flu A and B viruses, respiratory syncytial viruses, and rhinoviruses, from 2015–2016 to 2020–2021. The prevalences were reported at Weeks 40, 47, 52, 7, and 14 (except for winter 2020–2021 in which the fourth and last date corresponds to the second week of 2021)
The measures were effective for influenza viruses and RSV, whose circulation is only epidemic (i.e., not detected before winter). They were not detected even in children under 6 years old, who are currently exempt from wearing a mask and continue to go to school in France. In contrast, the response of rhinoviruses, which circulate all year round, was quite different. Their prevalence was stable, and the figures were the same as in previous years. However, the patients who tested positive for rhinoviruses were younger than those identified during past winters. The ages of those patients infected during the winter 2020/2021 (median: 1.21, interquartile range [IQR]: [0.17; 4.28]) differed significantly from those of patients infected during the two previous winters (2018/2019 and 20109/2020; median: 1.82, IQR: [0.24; 60.25], p = .01 by Wilcoxon test).
The reasons for these differences in prevalence are difficult to pinpoint and probably multifactorial, each of varying importance. Virus tropism could be determinant, with flu and RSV preferentially targeting the lower respiratory tract and rhinoviruses propagating in the upper tract. The longer infectious period of rhinoviruses could be partially responsible for them being more infectious than RSV despite the fact that their R0 was lower than that of RSV. 4 In addition, given the absence of an envelope, rhinoviruses are less sensitive to hydroalcoholic solutions, which might contribute to their persistent circulation during the winter of 2020–2021 as we also observed for adenoviruses.
We believe that the differing responses of viral epidemic episodes to nonpharmaceutical control measures should be known and fully understood to design defenses against future viral epidemics.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Jean‐Michel Mansuy conducted the study and wrote the manuscript. Maximin Bourcier recovered the data. Pauline Trémeaux reviewed and corrected the manuscript. Chloé Dimeglio analyzed the data. Jacques Izopet supervised the study.
REFERENCES
- 1. Sakamoto H, Ishikane M, Ueda P. Seasonal influenza activity during the SARS‐CoV‐2 outbreak in Japan. JAMA. 2020;323:1969‐1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu D, Liu Q, Wu T, Wang D, Lu J. The impact of COVID‐19 control measures on the morbidity of varicella, herpes zoster, rubella and measles in Guangzhou, China. Immun Inflamm Dis. 2020;8(4):844‐846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Olsen SJ, Azziz‐Baumgartner E, Budd AP, et al. Decreased influenza activity during the COVID‐19 pandemic—United States, Australia, Chile, and South Africa. Morb Mortal Wkly Rep. 2020;69:1305‐1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Spencer JA, Shutt DP, Moser SK, et al. Epidemiological parameter review and comparative dynamics of influenza, respiratory syncytial virus, rhinovirus, human coronavirus, and adenovirus. medRxiv. 2020. 10.1101/2020.02.04.20020404 [DOI] [Google Scholar]


