Abstract
Background
The restrictions imposed by the COVID‐19 pandemic impact heavily the management of chronic diseases like asthma. This study aimed to evaluate the management of adults and children with asthma during COVID‐19‐related lockdown.
Methods
A survey was launched by the European Academy of Allergy and Clinical Immunology (EAACI) via e‐mail, website, and social media to EAACI members and members of peer societies.
Results
The survey was completed by 339 healthcare professionals from 52 countries. 79% of follow‐up consultations were replaced by phone calls, whereas 49% of newly referred patients attended the clinic. 62%, 76%, 66%, 76%, and 87% of responders did not conduct spirometry, impulse oscillometry, bronchodilator test, FeNO, or methacholine provocation, respectively, for asthma diagnosis in adults. The numbers were similar for children. 73% of responders based the initial asthma diagnosis and the prescription of inhaled therapy on clinical parameters only. Lung function tests were used in 29% of cases to monitor asthma worsening, and only 56% of participants were recommended to their patients ambulatory peak expiratory flow (PEF) measurements. Using a 1 (not at all) to 5 (very much) scale, the responders considered that the quality of healthcare provided and the patients’ asthma status had deteriorated during the lockdown with 3.2 points and 2.8 points, respectively.
Conclusion
Collectively, these results suggest that all necessary resources should be allocated to ensure the performance of lung function tests for initial diagnosis, whereas digital remote monitoring should be reinforced for the follow‐up of children and adults with asthma.
Keywords: asthma, COVID‐19 lockdown, exacerbations, lung function test, peak expiratory flow
During the first wave of COVID‐19 pandemic, 38% of new and 77% of follow‐up consultations for pediatric and adult asthma patients were performed by phone calls. In 10% of cases, both types of consultations continued as face‐to‐face visits, whereas in 6% of cases all consultations were cancelled. Forced spirometry was not conducted during the initial assessment and subsequent monitoring of 56%‐62% of pediatric and adult asthma patients. Only 56% of HCP encouraged asthma patients to perform regular ambulatory peak expiratory flow measurement. Lung function tests were conducted in only 29% of children and adults with asthma who reported a worsening of their clinical condition. Using a 1 (nothing) to 5 (very much) scale, HCP scored with 2.8 the deleterious impact of COVID‐19 lockdown on the health status of children and adults with asthma.
Abbreviations: COVID‐19, coronavirus disease 2019; HCP, health care providers; PEF, peak expiratory flow

1. INTRODUCTION
The COVID‐19 pandemic challenges the capacity of healthcare systems to provide adequate management of chronic diseases. 1 , 2 , 3 Among other factors, discontinuation of face‐to‐face visits and the inability to perform diagnostic tests have a great impact on disease severity and degree of control. 4 A recent survey conducted by the Pediatric Asthma in Real Life (PEARL) think tank showed that the COVID‐19 pandemic significantly impacts pediatric asthma services: 39%, 47%, and 75% of them ceased physical appointments, stopped accepting new patients, and limited patients’ visits, respectively. Importantly, consultations were almost halved to a median of 20 patients per week, and virtual clinics and helplines were launched in most centers. 5 Another recent survey conducted among Chinese adult asthmatics reported that 75% of them did not attend any follow‐up consultation since the beginning the pandemic. 6
Both the initial diagnosis and subsequent monitoring of asthma largely rely on lung function tests (LFTs), which have a well‐documented value and are required by all international guidelines. 7 Forced spirometry (FS), among other LFTs, has raised safety concerns, especially due to the potential generation of SARS‐CoV‐2‐carrying bioaerosols. 8 Of note, the act of forced exhalation generates oral fluid droplets of variable size that can harbor infectious particles. While large droplets fall quickly to the ground, small droplets can dehydrate and linger as bioaerosols in the air, thus functioning as vectors for viral transmission. 9 A recent study revealed that the mere pronunciation of the words “stay healthy” generates 227–347 droplets depending on the lung volume of the speaker. 10
To evaluate the impact of the lockdown restrictions related to COVID‐19 pandemic on the management and health status of children and adults with asthma, the Asthma Section of the European Academy of Allergy and Clinical Immunology (EAACI) conducted a survey among EAACI members and members of other international scientific societies in July 2020. Of note, all countries around the world had been affected by the first wave of the pandemic at that moment. 11
2. MATERIAL & METHODS
2.1. Survey generation
The survey was generated by the authors. The specific topics on asthma management evaluated are listed in Appendix S1 in the online supplementary material.
2.2. Survey dissemination
The survey was launched on 1 July 2020 and remained open until 14 July 2020. The link to the survey was featured in the home page of EAACI website and was disseminated through a first mass e‐mail to EAACI members (9343 contacts) on 1 July 2020 followed by a reminder mass e‐mail on 13th July. The day the first mass e‐mail was sent 2270 contacts (24%) opened the e‐mail and 217 (10% of those who opened the e‐mail) clicked the link heading to the survey. The link to the survey was also posted on EAACI and EAACI Junior Member official Facebook and Twitter accounts on 1 and 12 July 2020. Finally, the link was also shared with representatives from European Respiratory Society, American Academy of Allergy, Asthma and Immunology, and World Allergy Organization who posted it in their social media channels at different time points during the days the survey remained open.
2.3. Instructions to reply to the survey
Because EAACI membership includes professionals who do not take care of asthma patients (basic scientists, dermatologists, ENT surgeons, dieticians, etc.), only clinicians and allied health professionals (eg nurses) totally or partially committed to adult and/or pediatric asthma were asked to reply to the survey. Moreover, the responders were instructed to refer to the hardest moment of the lockdown.
3. RESULTS
3.1. Profile of the participants
Overall, 339 individuals from Europe (76%), America (18%), Asia (4%), Africa (2%), and Australia (0.3%) (52 different countries, see Appendix S1) participated in the survey, of whom 74% replied to all questions. The most frequent profile of the responder was an allergy specialist (60%), working in a University Hospital (36%) and taking care of both children and adults (41%) (Figure 1).
FIGURE 1.
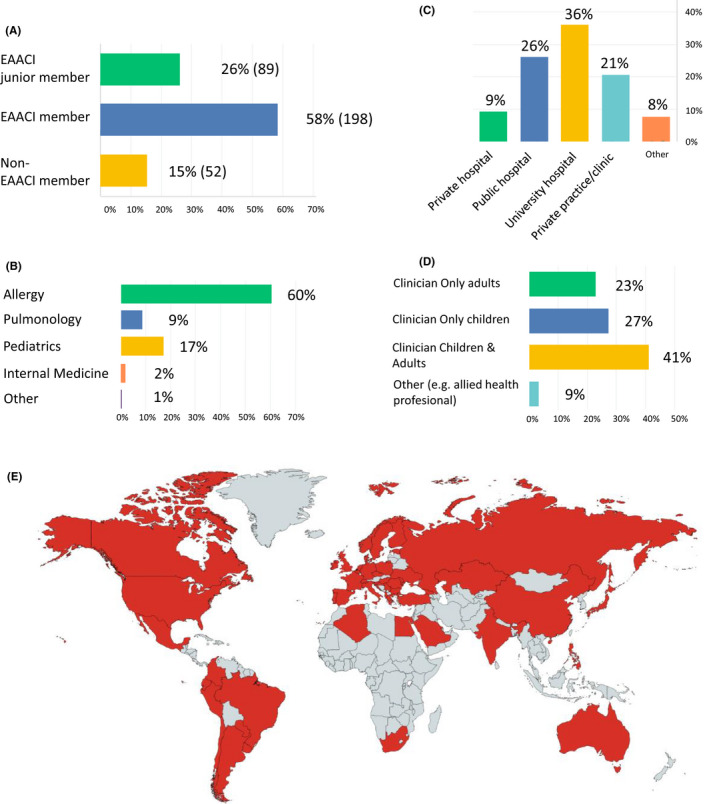
Features of the individuals participating in the survey in relation to scientific society membership (A), medical specialty (B), working environment (C), and type of patient taking care of (D). The numbers besides/above the bars indicate the proportion of participants who selected the different options. (E) shows in red color the countries of practice of the participants. EAACI, European Academy of Allergy and Clinical Immunology
3.2. Availability of guidelines for asthma management during the pandemic
The survey first interrogated the participants for the availability of national guidelines on asthma management during COVID‐19 pandemic. These documents existed in most countries (37 of 52), and 74% of responders followed their recommendations. Nevertheless, 39% of participants were already following a similar approach before being aware of the guidelines.
3.3. Effect of the pandemic on the evaluation of asthma patients
During the lockdown, follow‐up consultations were replaced by phone calls in 77% of cases, whereas only 49% of newly referred patients could attend the clinic in person. Of note, only in 10% of cases face‐to‐face visits were not somehow restricted (Figure 2). Regarding the performance of LFTs, 62%, 78%, 66%, 76%, and 87% of responders who had the test available at their department did not conduct FS, impulse oscillometry (IOS), bronchodilator test (BDT), fractional exhaled nitric oxide (FeNO) measurement or airway hyperresponsiveness (AHR) tests (eg methacholine bronchial provocation), respectively, for asthma diagnosis in adults (Figure 3A). Similarly, 56%, 62%, 61%, and 70% of participants with access to the tests did not use FS, IOS, BDT, and AHR test for the diagnosis of pediatric asthma. The numbers were similar for the monitoring using LFT both for children and adults with asthma (Figure 3B). Importantly, 65% of participants did not conduct any LFT during the lockdown, and only in 15% of cases, more than one test per day and per device was performed.
FIGURE 2.
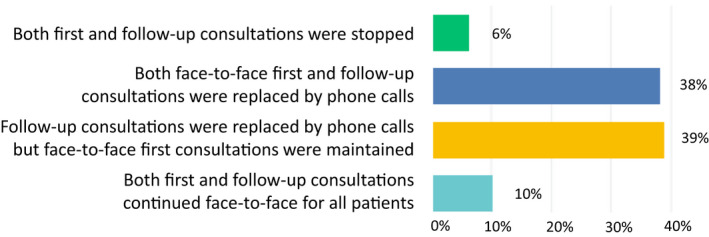
Impact of the restrictions related to COVID‐19 pandemic on the medical visit of asthma patients. The numbers besides the bars indicate the proportion of participants who selected the different options
FIGURE 3.
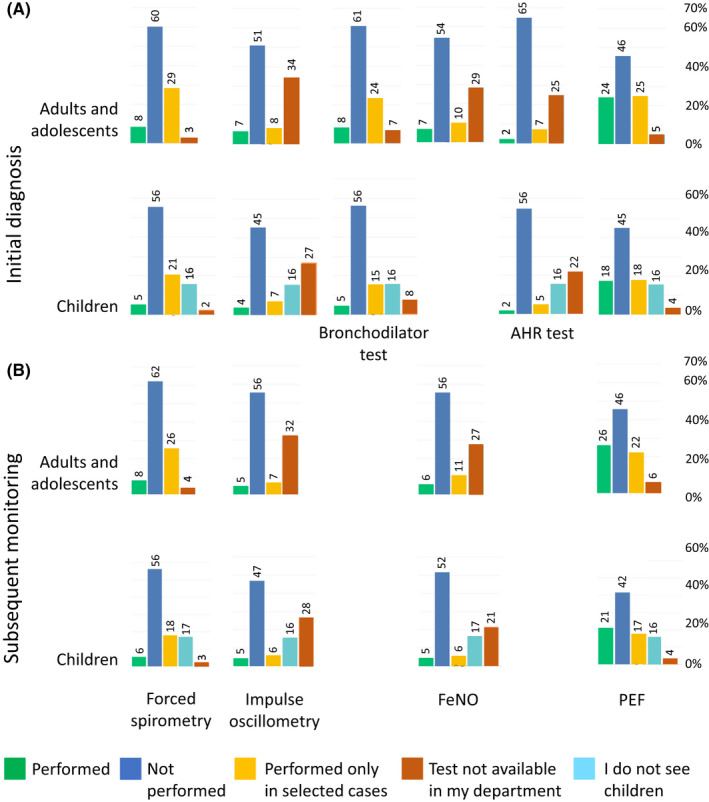
Performance of lung function tests during the pandemic. The numbers above the bars indicate the proportion of participants who selected the different options. FeNO, fractional exhaled nitric oxide; AHR test, airway hyperresponsiveness test (eg methacholine bronchial challenge); PEF, peak expiratory flow
3.4. Effect of the pandemic on asthma diagnosis and management
In a third step, the survey analyzed how asthma was managed during the pandemic. In 73% of cases, the physicians diagnosed asthma and prescribed inhaled therapy based on suggestive symptoms only (Figure 4A). Only 19% of participants conducted a full diagnostic workup for asthma diagnosis. Regarding patient monitoring, 69%–72% of responders used only the current symptoms and the asthma history to adjust the treatment. LFTs were used in only 29% of cases to monitor patients reporting a clinical worsening (Figure 4B).
FIGURE 4.
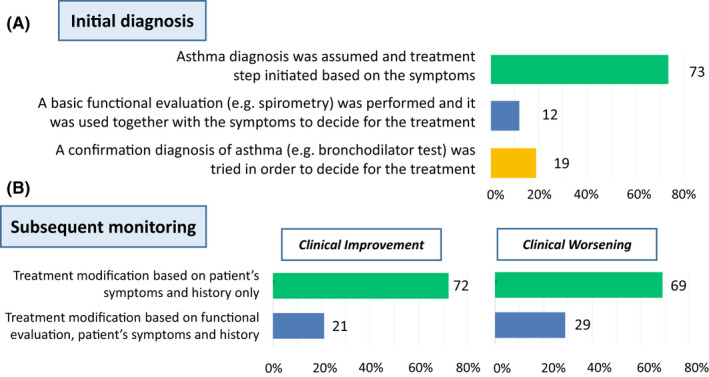
Asthma management during the COVID‐19 pandemic. The numbers besides the bars indicate the proportion of participants who selected the different options
The survey particularly focused on the ambulatory measurement of peak expiratory flow (PEF), as this test can be performed using portable devices and can assist in monitoring asthma control, together with asthma symptoms, as part of a management plan. 7 , 8 During the lockdown, 56% of responders encouraged their patients to conduct repeated ambulatory PEF measurements, while 41% considered PEF measurement not reliable for proper monitoring.
3.5. Asthma management after the end of the lockdown
When the survey was launched, restrictions associated with the first wave of the pandemic were loosening in many countries. 11 Therefore, the next step of the questionnaire evaluated the timeline to resume LFTs and the optimal strategy for future months. As per July 2020, only a minority of centers had reinitiated LFTs (17%–48% depending on the LFT type). Of note, in 53% of cases there was no specific timeline to resume AHR tests (Figure 5A). As for the remaining period of the pandemic, 63% of responders stated that LFTs should be restricted to selected patients and only performed after the healthcare facilities have been adapted to the new safety requirements. Importantly, only 17% of participants believed that the number of LFTs should remain similar to that prior to the lockdown (Figure 5B).
FIGURE 5.
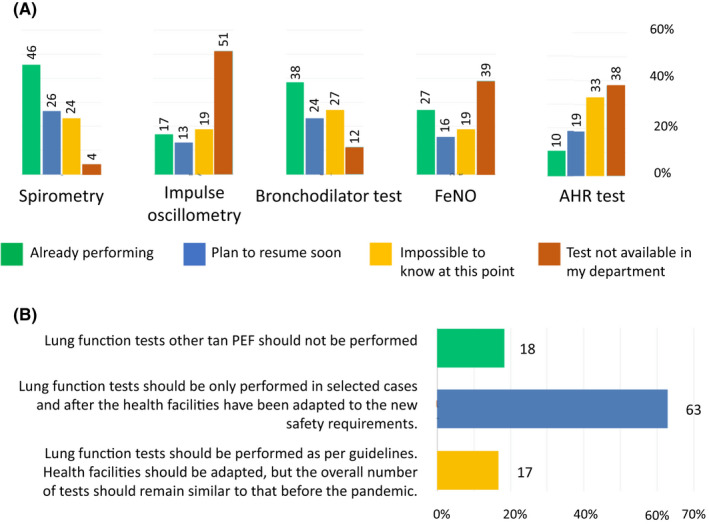
Timeline to resume lung function testing during the COVID‐19 pandemic (A) and approach suggested by the participants in relation to the performance of lung function tests during the remaining months of the pandemic (B). The numbers above/besides the bars indicate the proportion of participants who selected the different options. FeNO, fractional exhaled nitric oxide; AHR test, airway hyperresponsiveness test (eg methacholine bronchial challenge)
3.6. Estimation of the effects of the lockdown on health indicators
In a last step of the survey, participants were asked to appreciate the deleterious impact of the pandemic on the management and evolution of asthma patients. Using a 1 (not at all) to 5 (very much) scale, the responders considered that both the quality of asthma‐related health care provided and the patients’ asthma status had deteriorated during lockdown with 3.2 points and 2.8 points, respectively (Figure 6). Although 15%–17% of participants considered that the quality of health care had decreased very much (5 of 5 points), only 6%–7% identified a very important (5 of 5 points) worsening in the clinical condition of asthma patients. Nevertheless, the opinions of the responders were highly polarized as illustrated by the 41% and 22% of participants who scored the deleterious impact of the restrictions for LFT performance on patients’ health status with 1 or 2 points and with 4 or 5 points, respectively.
FIGURE 6.
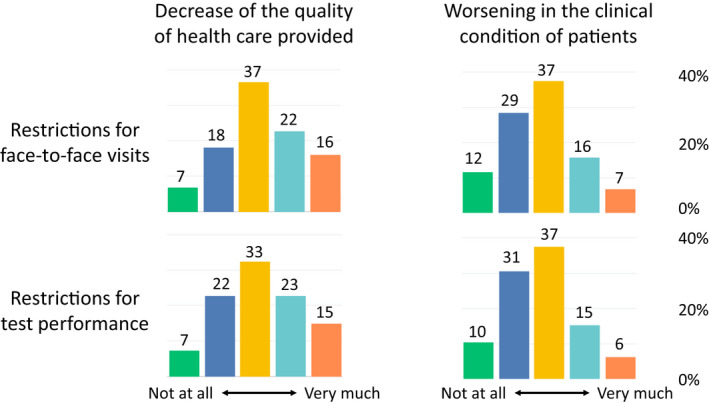
Impact of the restrictions related to COVID‐19 pandemic (face‐to‐face visits and test performance) on the quality of health care provided and the health status of asthma patients. The numbers above the bars indicate the proportion of participants who selected the different options
4. DISCUSSION
This EAACI position paper reports on a real‐life situation experienced by physicians managing asthma patients during the first lockdown of the COVID‐19 pandemic. Although a larger sample size would have been desirable, the number of survey participants is in line with previous multinational studies using a similar methodology. 5 , 12 Even though national guidelines for asthma management during the pandemic existed in most countries, in many cases they were not crucial to determine the strategy to follow, as the responders were following the same approach before being aware of the guidelines. As previously reported, 13 this observation probably reflects that most national documents were mainly based on expert‐consensus just providing common sense recommendations that would be anyways implemented.
The survey reported that most patients referred for initial evaluation underwent phone consultations instead of face‐to‐face visits. Therefore, LFTs could not be not performed and asthma diagnosis was guided only by clinical parameters. As previously demonstrated, this approach is associated with a significant rate of misdiagnosis and overtreatment with inhaled corticosteroids (ICS). 14 , 15 Importantly, ICS therapy is not indicated in all patients with COPD, a disease within the differential diagnosis of asthma. Of note, ICS therapy has been related to a higher risk of both bacterial pneumonia and bone fractures in COPD individuals. 16 , 17 On the other hand, follow‐up consultations were also conducted by phone calls in most cases. In this regard, the use of FS and FeNO measurement for the management of pediatric asthma has been associated with reduced exacerbation rates, among other beneficial outcomes. 18 , 19
Existing evidence indicates that the ambulatory measurement of PEF, as part of a self‐management plan, is useful to monitor the disease and decrease the rate of severe exacerbations in both children and adults with asthma. 20 , 21 , 22 Nevertheless, 41% of responders did not consider this test reliable, yet they acknowledged its additional safety guarantees as compared to LFTs conducted at healthcare facilities. Of note, adherence levels to PEF monitoring have been shown to be as low as 9% and PEF “diary fabrication” as high as 60%. 23 , 24 One potential solution to overcome this limitation is the use of electronic PEF meters linked to smartphone apps allowing reminder notifications and immediate charting. 25 , 26 In a real‐life study, after a period of 6 months, 67% of asthma patients using electronic PEF meters measured their PEF at least once a week. 27 Besides facilitating LFT performance, e‐health resources can help monitor symptoms and medication consumption and can be used by patients to check their level of control. 26 Furthermore, e‐health resources allow an immediate sharing of data with the treating physician, thus facilitating early therapeutic interventions and potentially preventing severe exacerbations. 25
The timeline to resume LFTs reflects the evolution of the pandemic worldwide, the precautions regarding the second wave, and the availability of resources to adapt the healthcare facilities to the new situation. 11 Of note, most participants assumed that, given the circumstances, the best possible approach is to perform a reduced number of LFTs during the remaining months of the pandemic. This finding is probably connected with the moderate impact of the restrictions for LFTs performance (2.8–3.2 of 5 points) identified on average by the participants. This appreciation is also consistent with the results of previous studies on the topic. According to specialists in pediatric asthma, only 10% of patients experienced a clinical worsening during the pandemic, 5 whereas only 8% of Chinese adult asthmatics believed that their clinical condition had aggravated during the lockdown. 6 Nevertheless, beyond the average score, EAACI survey also detected highly polarized opinions. This finding is probably explained by the evolving environment the pandemic is taking place in. On one hand, social distancing, sheltering at home, the use of face masks, and the lockdown of workplaces and schools might have reduced exposure to the main triggers of acute asthma symptoms such as rhinoviruses, outdoor seasonal allergens, physical exercise, or ambient pollution during the first wave of the pandemic in Europe (March‐June 2020). 28 On the other hand, the high burden of indoor allergens (eg house dust mites) 29 during the second and subsequent waves (from October 2020 onwards in Europe) together with the lack of proper monitoring for the previous months can be expected to increase uncontrolled asthma burden on healthcare systems in the future months. Our results are also consistent with the first international survey investigating practical aspects and tolerability of allergen immunotherapy (AIT) during the COVID‐19 pandemic. 30 Although the responders expressed no concern of reduced safety of AIT in real‐life circumstances, the survey showed a significant under use of AIT during the pandemic. Although temporary, this phenomenon could be associated with a long‐lasting negative impact on the clinical care of patients with airway allergy.
The EAACI survey indicates that beyond SARS‐CoV‐2 infection, the restrictions related to the lockdown significantly impact the quality of health care provided to asthma patients. Unlike previous studies focusing on specific age ranges or countries, 5 , 6 the EAACI survey reflects the impact of COVID‐19 on adult and pediatric patients from different geographical areas. On the other hand, part of the data collected in EAACI survey is only indicative of the subjective appreciation of the responders. Moreover, similar to previous multinational surveys on allergy, 5 , 12 our study has a predominance of European responders, especially from Mediterranean countries. This finding likely reflects both the origin of EAACI membership and the regional differences in the implementation of Allergy specialty. In summary, given the well‐established reliability of LFTs for asthma management, 7 , 13 , 18 , 19 , 20 , 21 , 22 all necessary resources should be allocated to ensure the performance of LFTs for initial asthma diagnosis, whereas PEF measurement should be reinforced for asthma tele‐monitoring, both in children and in adults (Table S1). In this regard, several national societies have recently published recommendations for safe lung function testing during the COVID‐19 pandemic. 31 , 32 , 33 , 34 All these actions are necessary steps to guarantee the best possible health status of children and adults with asthma during present and future pandemics.
CONFLICT OF INTEREST
MC reports a permanent employment contract with Roche outside the submitted work. SdG reports grants and personal fees from AstraZeneca, GSK and Novartis and personal fees from Sanofi‐Regeneron, Menarini, Chiesi, and Boehringer‐Ingelheimoutside the submitted work. The other authors have no conflict of interest to disclose in relation to this work.
AUTHOR CONTRIBUTIONS
IEG, MvdB, CB, MB, CC, MC, FOE, MR, SSG, and IA designed the survey and disseminated it. IEG and IA analyzed the replies and wrote the manuscript, which was reviewed by the rest of the authors. SdG, MJ, and IA supervised the work of the rest of the authors.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
The authors express their gratitude to Ana Antunes, the rest of the EAACI headquarters staff and EAACI Junior Members for fine‐tuning and disseminating the survey, to representatives from the American Academy of Allergy, Asthma and Immunology (AAAAI), the World Allergy Organization (WAO), and the European Respiratory Society (ERS) for promoting this initiative, and to all physicians and allied health professionals who replied to the survey for sharing their valuable experience.
Funding information
EAACI funded initiative.
REFERENCES
- 1. Klimek L, Jutel M, Bousquet J, et al. Management of patients with chronic rhinosinusitis during the COVID‐19 pandemic ‐ an EAACI Position Paper. Allergy 2021;76(3):677‐688. [DOI] [PubMed] [Google Scholar]
- 2. Leonardi A, Fauquert JL, Doan S, et al. Managing ocular allergy in the time of COVID‐19. Allergy 2020;75(9):2399‐2402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Klimek L, Jutel M, Akdis C, et al. Handling of allergen immunotherapy in the COVID‐19 pandemic: an ARIA‐EAACI statement. Allergy 2020;75(7):1546‐1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bousquet J, Jutel M, Akdis CA, et al. ARIA‐EAACI statement on asthma and COVID‐19 (June 2, 2020). Allergy 2021;76(3):689‐697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Papadopoulos NG, Custovic A, Deschildre A, et al. Impact of COVID‐19 on pediatric asthma: practice adjustments and disease burden. J Allergy Clin Immunol Pract. 2020;8(8):2592‐2599.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chang C, Zhang L, Dong F, et al. Asthma control, self‐management, and healthcare access during the COVID‐19 epidemic in Beijing. Allergy 2021;76(2):586‐588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. The Global Initiative for Asthma (GINA) 2020 update. https://ginasthma.org/. Accessed November 8, 2020.
- 8. Riggioni C, Comberiati P, Giovannini M, et al. A compendium answering 150 questions on COVID‐19 and SARS‐CoV‐2. Allergy 2020;75(10):2503‐2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marr LC, Tang JW, Van Mullekom J, Lakdawala SS. Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J R Soc Interface. 2019;16(150):20180298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Anfinrud P, Stadnytskyi V, Bax CE, Bax A. Visualizing speech‐generated oral fluid droplets with laser light scattering. N Engl J Med. 2020;382(21):2061‐2063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. World Health Organization . Coronavirus disease (COVID‐19) pandemic. https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019. Accessed November 8, 2020.
- 12. Caminati M, Antolín‐Amérigo D, Bonini M, et al. The EAACI‐AAAAI‐WAO Junior Members’ joint survey: a worldwide snapshot of Allergy and Clinical Immunology specialty. Allergy 2020;75(3):588‐595. [DOI] [PubMed] [Google Scholar]
- 13. Crimi C, Impellizzeri P, Campisi R, Nolasco S, Spanevello A, Crimi N. Practical considerations for spirometry during the COVID‐19 outbreak: literature review and insights. Pulmonology. 2020. 10.1016/j.pulmoe.2020.07.011. S2531‐0437(20)30175‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. LindenSmith J, Morrison D, Deveau C, Hernandez P. Overdiagnosis of asthma in the community. Can Respir J. 2004;11(2):111‐116. [DOI] [PubMed] [Google Scholar]
- 15. McGrath KW, Fahy JV. Negative methacholine challenge tests in subjects who report physician‐diagnosed asthma. Clin Exp Allergy. 2011;41(1):46‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Suissa S, Patenaude V, Lapi F, Ernst P. Inhaled corticosteroids in COPD and the risk of serious pneumonia. Thorax 2013;68(11):1029‐1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gonçalves PA, Dos Santos NR, Neto LV, et al. Inhaled glucocorticoids are associated with vertebral fractures in COPD patients. J Bone Miner Metab. 2018;36(4):454‐461. [DOI] [PubMed] [Google Scholar]
- 18. Fielding S, Pijnenburg M, de Jongste JC, et al. Change in FEV(1) and feno measurements as predictors of future asthma outcomes in children. Chest 2019;155(2):331‐341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cevhertas L, Ogulur I, Maurer DJ, et al. Advances and recent developments in asthma in 2020. Allergy 2020;75(12):3124‐3146. [DOI] [PubMed] [Google Scholar]
- 20. Gibson PG, Wlodarczyk J, Hensley MJ, Murree‐Allen K, Olson LG, Saltos N. Using quality‐control analysis of peak expiratory flow recordings to guide therapy for asthma. Ann Intern Med. 1995;123(7):488‐492. [DOI] [PubMed] [Google Scholar]
- 21. Fishwick D, Beasley R. Use of peak flow‐based self‐management plans by adult asthmatic patients. Eur Respir J. 1996;9(5):861‐865. [DOI] [PubMed] [Google Scholar]
- 22. NICE guideline updates team (UK) . Increasing ICS treatment within supported self‐management for children and young people: Asthma: diagnosis, monitoring and chronic asthma management: Evidence review A. London: National Institute of Health and Care Excellence (UK); 2020. [PubMed] [Google Scholar]
- 23. Garrett J, Fenwick JM, Taylor G, Mitchell E, Rea H. Peak expiratory flow meters (PEFMs)—who uses them and how and does education affect the pattern of utilisation? Aust N Z J Med. 1994;24:521‐529. [DOI] [PubMed] [Google Scholar]
- 24. Côté J, Cartier A, Malo JL, Rouleau M, Boulet LP. Compliance with peak expiratory flow monitoring in home management of asthma. Chest 1998;113:968‐972. [DOI] [PubMed] [Google Scholar]
- 25. Elliott T, Shih J, Dinakar C, Portnoy J, Fineman S. American College of Allergy, Asthma & Immunology position paper on the use of telemedicine for allergists. Ann Allergy Asthma Immunol. 2017;119(6):512‐517. [DOI] [PubMed] [Google Scholar]
- 26. Matricardi PM, Dramburg S, Alvarez‐Perea A, et al. The role of mobile health technologies in allergy care: An EAACI position paper. Allergy 2020;75(2):259‐272. [DOI] [PubMed] [Google Scholar]
- 27. Antalffy T, De Simoni A, Griffiths CJ. Promising peak flow diary compliance with an electronic peak flow meter and linked smartphone app. NPJ Prim Care Respir Med. 2020;30(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gallo O, Bruno C, Orlando P, Locatello LG. The impact of lockdown on allergic rhinitis: what is good and what is bad? Laryngoscope Investig Otolaryngol. 2020;5(5):807‐808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Eguiluz‐Gracia I, Mathioudakis AG, Bartel S, et al. The need for clean air: the way air pollution and climate change affect allergic rhinitis and asthma. Allergy 2020;75(9):2170‐2184. [DOI] [PubMed] [Google Scholar]
- 30. Pfaar O, Agache I, Bonini M, et al. COVID‐19 pandemic an allergen immunotherapy‐an EAACI survey. Allergy 2021. 10.1111/all.14793. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Olaguibel JM, Alobid I, Alvarez Puebla M, et al. Upper and lower airways functional examination in asthma and respiratory allergic deseases. Considerations in the SARS‐CoV‐2 post‐pandemic situation. J Investig Allergol Clin Immunol. 2020;31(1):17‐35. [DOI] [PubMed] [Google Scholar]
- 32. Franczuk M, Przybyłowski T, Czajkowska‐Malinowska M, et al. Spirometry during the SARS‐CoV‐2 pandemic. Guidelines and practical advice from the expert panel of Respiratory Physiopathology Assembly of Polish Respiratory Society. Adv Respir Med. 2020;88(6):640‐650. [DOI] [PubMed] [Google Scholar]
- 33. Bignamini E, Cazzato S, Cutrera R, et al. Italian pediatric respiratory society recommendations on pediatric pulmonary function testing during COVID‐19 pandemic. Ital J Pediatr. 2020;46(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gemicioğlu B, Börekçi Ş, Dilektaşlı AG, Ulubay G, Azap Ö, Saryal S. Turkish Thoracic Society Experts Consensus Report: recommendations for pulmonary function tests during and after COVID 19 pandemic. Turk Thorac J. 2020;21(3):193‐200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


