Abstract
Background
The economic impacts of the coronavirus disease 2019 (COVID‐19) have drastically increased food insecurity in the United States. Initial data, collected a few months into the pandemic, showed that families, particularly those experiencing food insecurity, reported detrimental changes to their home food environment and parent feeding practices, compared to before COVID‐19.
Objective
This follow‐up study obtained longitudinal data from a sample of parents in the United States to quantify changes in food security status, the home food environment, and parent feeding practices, from before to across COVID‐19 as the pandemic continued to persist.
Methods
Parents (N = 433) completed online surveys May (T1) and September (T2) 2020 during COVID‐19. Food security, home food environment, and parent feeding practices were reported at each timepoint. At T1, parents also retrospectively reported on these factors pertaining to before COVID‐19. Chi square analyses and repeated measure mixed models examined associations among study variables.
Results
Low or very low food security increased from before COVID‐19 (37%) to T1 (54%) and decreased by T2 (45%). About 30% of families who became food insecure, and 44% who stayed food insecure from T1 to T2, reported a decrease in total food in their home; only 3%–6% who became/stayed food secure reported this decrease. Parents' concern for child overweight and use of monitoring increased from before COVID‐19 to T1, and decreased by T2, but remained elevated above pre–COVID‐19 values.
Conclusion
Rates of food insecurity remain high as this pandemic persists. Continued assessment of nutrition‐related factors and increased economic supports are critical for families to endure COVID‐19 and prevent long‐term obesity and health risks.
Keywords: child weight, coronavirus, food insecurity, nutrition, pandemic, parent feeding
1. INTRODUCTION
The severe economic impact of the coronavirus disease 2019 (COVID‐19) pandemic has drastically increased food insecurity for families in the United States. 1 , 2 Food insecurity—defined as limited or uncertain access to adequate food 3 —is associated with detrimental health outcomes 4 and disproportionately affects racial/ethnic minority populations facing long‐standing health inequities and greater obesity risk. 5 The social and behavioral ramifications resulting from COVID‐19, such as greater unstructured time due to in‐person school closures and canceled activities, have also raised concern regarding the potential for increased childhood obesity rates. 6 Thus, there is a need for empirical, longitudinal data collected throughout this pandemic to examine food insecurity and nutrition‐related factors in this changing environment to inform our understanding of the impact of COVID‐19 on child obesity risk.
Previously reported on data from this study team quantified changes in family's food security status, home food environment, and parent feeding practices about 2 months into COVID‐19 being declared a pandemic. These results found a drastic increase in the percentage of families reporting very low food security with reported changes to their home food environment and parent feeding practices, compared to before COVID‐19. 7 For example, more than half of families with very low food security decreased the total amount of food in their home and increased the amount of nonperishable processed foods. 7 Parents also reported a greater concern for child overweight and controlling feeding practices, with an even greater increase in concern for child overweight and pressure to eat among for families experiencing food insecurity. 7 Since these initial data were collected, nationwide rates of food insufficiency have remained elevated, 2 yet policy changes have occurred through stimulus bills (i.e., coordinated economic measures from the government to stimulate and support the economy) and government assistance programmatic flexibilities to provide some economic relief and address food insecurity. 8 , 9 Furthermore, over the course of COVID‐19, families (regardless of food security status) might have experienced additional changes in income, increased government assistance benefits, reduced perceived threat of food shortages, and fluctuations in stay‐at‐home orders. Collectively, these factors could influence family's food purchasing behaviors and feeding practices as the pandemic progresses. It is therefore important to examine if the initial changes observed during COVID‐19 are sustained months later.
The aim of this follow‐up study was to obtain longitudinal data from a sample of the US parents regarding food insecurity, the home food environment, and parent feeding practices during COVID‐19. The initial survey was completed at the peak of school closures and stay‐at‐home orders (May 2020). 7 This follow‐up survey was completed in September 2020, at another key timepoint during COVID‐19 that coincides with children's return to school. Specifically, changes in food security status, the home food environment, and parent feeding practices were quantified across three timepoints: before COVID‐19 (retrospective), May 2020, and September 2020. Next, analyses examined if longitudinal changes in the home food environment and parent feeding practices differed by changes in food security status during this time.
2. METHODS
2.1. Study design and participants
This observational study utilized an online survey to quantify longitudinal changes in food security status, the home food environment, and parent feeding practices. The first survey was administered in May 2020 (T1) where parents reported on their situation before COVID‐19 (retrospective report), as well as currently at that time. In September 2020 (T2), parents completed a follow‐up survey regarding the same factors, to permit longitudinal assessment at two timepoints during COVID‐19. Complete study methods are described elsewhere. 7
Parents ≥18 years of age, living in the United States, and with a child 5–18 years of age were eligible to participate. Recruitment occurred primarily through Facebook advertisements that targeted individuals most vulnerable to COVID‐19 (e.g., had lower educational attainment, lived in lower income ZIP codes). Social media advertisements were also posted on parenting groups and Virginia Commonwealth University Facebook pages. Additional participants were recruited using a snowball technique by sharing the survey link across various community sectors (e.g., Young Men's Christian Associations [YMCAs], nonprofit organizations, and schools) and professional organization listservs. Full recruitment details can be found in Adams et al. 7 The secure Qualtrics platform (Provo, Utah) was used to administer online surveys. Initial screening questions assessed eligibility. If eligible, parents were directed to complete the full survey. An informational letter describing the study was provided at the start of survey. Participants advancing to the survey served as passive consent for participation. In the event that parents had more than one child 5–18 years of age, they were asked to complete the first survey when thinking about their child whose weight most concerns them; for the second survey, parents answered the survey in reference to that same child. The first survey consisted of 144 questions and took approximately 20 min to complete. The second survey consisted of 80 questions and took approximately 10 min to complete. At the end of the first survey, parents provided their contact information so that the study team could send compensation ($10 gift card for each completed survey) and follow‐up surveys. Identifiable information was not linked to participants' responses in any way.
A total of n = 1342 parents started the first survey, and n = 584 parents provided complete, valid data. All n = 584 parents were provided with the second survey link via email. Of these, N = 433 completed the second survey (74% retention) and comprise the sample for the current report. Parents who did not complete the second survey were more likely to be from racial (i.e., Black) and ethnic (i.e., Hispanic/Latino) minority backgrounds (ps < 0.05). No other demographic differences or differences in food security status were observed based on retention. All study and consent procedures were approved by the Institutional Review Board at Virginia Commonwealth University.
2.2. Survey measures
2.2.1. Demographics and COVID‐19‐related questions
Demographic questions asked at T1 included parent and child age, sex, race, and ethnicity; parent education and marital status; family income and insurance status; and parent‐perceived child weight status. At T2, parents reported if their child had gained, lost, or remained the same weight since T1. Parents who reported a change in child weight were then asked how many pounds their child gained or lost during this period of time. COVID‐19‐related questions asked at T1 and T2 included items related to family COVID‐19 diagnoses, working from home, income changes, unemployment benefits, and the use of local food banks and/or government assistance benefits (Supplemental Nutrition Assistance Program [SNAP]; Special Supplemental Nutrition Program for Women, Infants, and Children [WIC]; and school‐provided meals).
2.2.1.1. Food insecurity
The six‐item United States Department of Agriculture Household Food Security Module was used to assess household food security status at each timepoint. 10 This brief measure has high specificity and sensitivity, with minimal bias. 11 Given the rapidly changing environment during COVID‐19 and need for acute measures of food insecurity, one question was modified to ask parents to report on the number of days they cut/skipped meals within the past 30 days, rather than in the past 12 months. 10 Responses of ≥3 days were considered as an affirmative response. All affirmative responses were summed, with total scores ranging 0–6. Families were then categorized as having high (0–1), low (2–4), or very low (5–6) food security status at each timepoint based on their total score.
Within‐family changes in food security status from T1 to T2 were quantified. Categories of low and very low food security were collapsed into a single “food insecure” category, due to a lower percentage of families in each of these categories and to be consistent with methods used in prior research. 5 This resulted in two categories at each timepoint: food secure versus food insecure. Within‐family comparisons of categories at T1 and T2 were characterized as remained food secure, remained food insecure, became food secure, or became food insecure, corresponding to family's stability or change in food security status from T1 to T2.
2.2.2. Household food environment
Five questions quantified changes in the amount and types of food in family's home, 7 asking if the amount of (1) total food, (2) high‐calorie snack foods (e.g., chips), (3) desserts and sweets (e.g., cookies), (4) fresh foods (e.g., fruits and vegetables), and (5) nonperishable processed food (e.g., canned food) in their home was more or less at T2, compared to at T1. Response options were provided on a 5‐point Likert scale ranging “much less,” to “much more.” Responses were collapsed into three categories representing an increase (much more/slightly more), a decrease (much less/slightly less), or no change from T1 to T2.
2.2.3. Parent feeding practices
The Child Feeding Questionnaire (CFQ) was used to quantify parent feeding practices at each timepoint. Four subscales were used from this validated measure, 12 including parents' concern for child overweight, restriction (i.e., restricting child's access to certain foods), pressure to eat (i.e., pressuring child to eat more food), and monitoring (i.e., parent supervision of child's eating). Response options were rated on a 5‐point Likert scale. All items within each subscale were averaged. Possible scores ranged from 1–5.
3. STATISTICAL ANALYSIS
Descriptive statistics were calculated using means and standard deviations for continuous variables and percentages for categorical variables. For Aim 1, patterns of food security status, the home food environment, and parent feeding practices were examined for the overall sample. Food security status was examined using a chi‐square analysis (3 × 3) to examine distribution differences in three food security categories (food secure; low food security; and very low food security) at each timepoint (before COVID‐19; T1; and T2). Home food environment changes were reported as the percentage of parents who responded to each categorical response option at each timepoint. Longitudinal patterns in parent feeding practices were examined using mixed models that accounted for repeated measures within families across time. A main effect of time was the independent variable, and CFQ subscales were the dependent variables tested in separate models. Post hoc comparisons examined where specific differences occurred between timepoints, with “before COVID‐19” serving as the reference group. Values are presented as adjusted means and 95% confidence intervals.
For Aim 2, differences in patterns of the home food environment and parent feeding practices by change in food security status were examined. A chi square analysis (3 × 4) examined home food environment changes at three timepoints by four food security status categories that represented a change from T1 to T2 (became food insecure; stayed food insecure; became food secure; stayed food insecure). Results indicate distribution differences across these categories and timepoints. Differences in longitudinal patterns in parent feeding practices by change in food security status were examined using mixed models that accounted for repeated measures within families across time. An interaction (time × change in food security status category) was the independent variable, and CFQ subscales were the dependent variables, tested in separate models. In the presence of a significant interaction term, models were stratified by change in food security status category to permit post hoc comparisons and examine where specific differences occurred between timepoints. “Before COVID‐19” served as the reference group, and a Tukey post hoc comparison was applied to correct for multiple testing. Values are presented as adjusted means and 95% confidence intervals. In the absence of a significant interaction term, post hoc comparisons were not examined. All analyses were conducted in SAS statistical software version 9.4 (SAS Institute Inc). Significance was defined a priori as p < 0.05.
4. RESULTS
Results are presented below starting with longitudinal patterns of food security status, the home food environment and parent feeding practices, followed by how longitudinal patterns of the home food environment and parent feeding practices differed by families' change or stability in food security status across COVID‐19.
4.1. Demographics and COVID‐19‐related factors
Parent and child demographics are listed in Table 1. Approximately 30% of parents reported child weight gain from T1 to T2 (average gain: 4.4 ± 3.2 kg), while few (7.4%) parents reported child weight loss (average loss: 3.8 ± 2.7 kg); 63.1% reported no change in child weight. Of those who reported child weight gain, 48.4% classified their child as having normal weight, and 41.4% as having overweight/obesity at T1. There were no differences in child weight change by food security status from T1 to T2 (p = 0.11).
TABLE 1.
Parent and child demographics, as well as COVID‐19‐related factors, in a sample of the US parents with a child 5–18 years of age (N = 433)
| Demographics | Parent | Child |
|---|---|---|
| Age, years (mean ± SD) | 40.4 ± 7.4 | 9.4 ± 3.8 |
| Female sex (%) | 94.5 | 50.6 |
| Race (%) | ||
| Asian | 3.9 | 5.1 |
| African American/Black | 6.7 | 10.6 |
| Caucasian/White | 84.8 | 84.8 |
| Other | 6.7 | 8.3 |
| Not Hispanic or Latino (%) | 88.5 | 85.2 |
| Married or living with domestic partner (%) | 77.4 | |
| Education (%) | ||
| Some college or less | 34.2 | |
| Associates or bachelor's degree | 39.0 | |
| Some graduate training or more | 26.8 | |
| Family income (%) | ||
| <$50,000/year | 47.8 | |
| $50,000–100,000/year | 29.1 | |
| >$100,000/year | 23.1 | |
| Insurance (%) | ||
| Medicaid | 35.8 | |
| Private insurance | 58.2 | |
| None | 6.0 | |
| Child weight status (%) a | ||
| Underweight | 12.5 | |
| Normal weight | 60.3 | |
| Overweight/obese | 27.3 | |
Abbreviation: COVID‐19, coronavirus disease 2019.
Parent‐reported; all demographics were reported at T1 in May 2020.
Family diagnoses of COVID‐19 occurred for 10.4% of families at T1 and 18.7% of families at T2. About half (51.3%) of parents worked outside the home at T1 and one‐third (33.0%) worked outside the home at T2. Most children (63.1%) attended virtual school at T2, while 19.4% attended in‐person, and 17.6% attended a hybrid option.
Most (58.9%) families reported a recent decrease in income at T1, while fewer (39.7%) reported a recent decrease at T2. Unemployment benefits were filed or received by 36.0% of families at T1 and 19.2% of families at T2. One‐fourth (26.1%) of families received school‐provided meals at T2; of these, 24.8% had not been participating in the school lunch program prior to COVID‐19. Almost one‐third (29.3%) of families received SNAP benefits at T2; of these, 27.0% had not been receiving these benefits prior to COVID‐19. Few (9.0%) families received WIC benefits at T2; of these, 12.8% had not been receiving these prior to COVID‐19. Lastly, 13.4% of families received meals from local food banks; of these, 50% had not been receiving these benefits prior to COVID‐19.
4.2. Longitudinal patterns of food security status, the home food environment, and parent feeding practices
4.2.1. Food security status
The percentage of families in each food security category at each timepoint is illustrated in Figure 1. The percentage of families with food insecurity (low or very low) increased from before COVID‐19 (37%) to T1 (54%) and decreased by T2 (45%). From T1 to T2, 6.2% of families became food insecure, while 15.0% of families became food secure. The remaining families either remained food secure (40.0%) or remained food insecure (38.8%).
FIGURE 1.
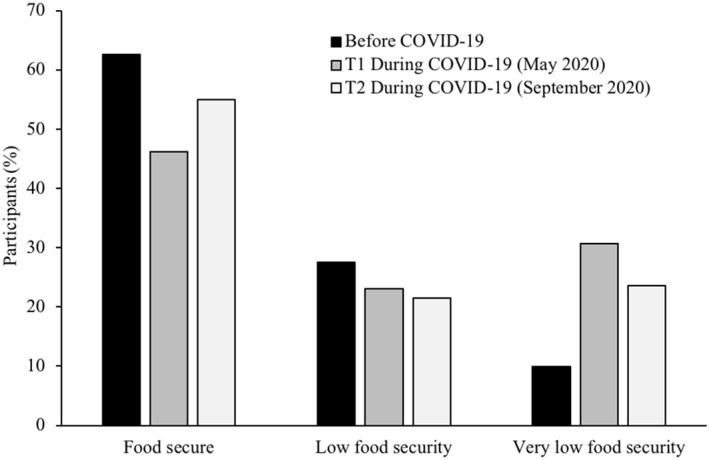
Distribution of families experiencing food security and food insecurity before the COVID‐19 pandemic (retrospective report) and at two timepoints during the COVID‐19 pandemic (T1 = May 2020; T2 = September 2020), in a nationwide sample of the US parents with a child 5–18 years of age (N = 433). COVID‐19, coronavirus disease 2019
4.2.2. Home food environment
Changes in families' home food environments from T1 to T2 are shown in Table 2. About half of all families did not change the amount of different types of foods in their home. Of those who did, a greater percentage decreased (rather than increased) the amount of high‐calorie snack foods and desserts/sweets, while a greater percentage of families increased (rather than decreased) the amount of fresh foods and nonperishable processed foods in their home.
TABLE 2.
Home food environment changes across two timepoints during the COVID‐19 pandemic in a nationwide sample of the US parents with a child 5–18 years of age (N = 433)
| Change in food security status from T1 to T2 | ||||||
|---|---|---|---|---|---|---|
| Overall (N = 433) | Became food insecure (n = 27) | Stayed food insecure (n = 173) | Became food secure (n = 65) | Stayed food secure (n = 168) | p value | |
| Total food | <0.01 | |||||
| Increased (%) | 26.6 | 18.5 | 18.5 | 38.5 | 31.2 | |
| Decreased (%) | 21.0 | 29.6 | 44.1 | 6.2 | 2.9 | |
| Stayed the same (%) | 52.4 | 51.9 | 37.5 | 55.4 | 65.9 | |
| High‐calorie snack foods | <0.01 | |||||
| Increased (%) | 17.3 | 18.5 | 16.1 | 18.5 | 17.9 | |
| Decreased (%) | 29.3 | 33.3 | 41.7 | 26.2 | 17.9 | |
| Stayed the same (%) | 53.4 | 48.2 | 42.3 | 55.4 | 64.2 | |
| Desserts and sweets | <0.01 | |||||
| Increased (%) | 15.5 | 3.7 | 14.3 | 15.4 | 18.5 | |
| Decreased (%) | 32.8 | 37.0 | 47.0 | 30.8 | 19.1 | |
| Stayed the same (%) | 51.7 | 59.3 | 38.7 | 53.9 | 62.4 | |
| Fresh foods | <0.01 | |||||
| Increased (%) | 36.3 | 44.4 | 32.7 | 49.2 | 33.5 | |
| Decreased (%) | 17.3 | 18.5 | 32.1 | 7.7 | 6.4 | |
| Stayed the same (%) | 46.4 | 37.0 | 35.1 | 43.1 | 60.1 | |
| Nonperishable processed food | <0.01 | |||||
| Increased (%) | 33.3 | 44.4 | 40.5 | 35.4 | 23.7 | |
| Decreased (%) | 17.3 | 7.4 | 21.4 | 13.9 | 16.2 | |
| Stayed the same (%) | 49.4 | 48.2 | 38.1 | 50.8 | 60.1 | |
Note: Results presented for the overall sample and by categories indicating changes in food security status across two timepoints during COVID‐19.
Increased = greater at T2, compared to T1, during the COVID‐19 pandemic.
Decreased = lower at T2, compared to T1, during the COVID‐19 pandemic.
Stayed the same = no reported change from T1 to T2 during the COVID‐19 pandemic.
p Values represent significance for chi‐square analyses conducted for home food environment variables by food security status (3 × 4) to indicate overall distribution differences.
Abbreviations: COVID‐19, coronavirus disease 2019; T1, timepoint 1 (May 2020); T2, timepoint 2 (September 2020).
4.2.3. Parent feeding practices
Parents' concern for child overweight increased from before COVID‐19 to T1, and decreased by T2, but remained above pre‐COVID‐19 values (Table 3). Parents use of restriction and pressure to eat increased from before COVID‐19 to T1 and returned to comparable pre‐COVID‐19 values by T2. Use of monitoring increased from before COVID‐19 to T1 and plateaued at T2.
TABLE 3.
Subscale scores for parent feeding practices reported on the Child Feeding Questionnaire, pertaining to before, and at two timepoints during, the COVID‐19 pandemic in a nationwide sample of the US parents of children 5–18 years of age (N = 433)
| Change in food security status (T 1 –T 2) | ||||||
|---|---|---|---|---|---|---|
| Overall (N = 433) | Became food insecure (n = 27) | Stayed food insecure (n = 173) | Became food secure (n = 65) | Stayed food secure (n = 168) | p value | |
| Concern about child overweight | <0.01 | |||||
| Before COVID‐19 | 2.4 (2.3–2.5) | 1.6 (1.1–2.1) | 2.5 (2.3–2.7) | 2.5 (2.2–2.8) | 2.3 (2.1–2.5) | |
| T1 during COVID‐19 | 2.8 (2.7–2.9) | 1.9 (1.3–2.4) | 3.0 (2.8–3.3) | 3.1 (2.8–3.5) | 2.6 (2.4–2.8) | |
| T2 during COVID‐19 | 2.5 (2.4–2.7) | 2.4 (1.9–2.9) | 2.8 (2.6–3.0) | 2.7 (2.4–3.1) | 2.2 (2.0–2.4) | |
| Restriction | 0.04 | |||||
| Before COVID‐19 | 3.1 (3.0–3.2) | 2.9 (2.5–3.2) | 3.2 (3.0–3.3) | 3.3 (3.1–3.6) | 3.1 (2.9–3.2) | |
| T1 during COVID‐19 | 3.4 (3.3–3.5) | 3.1 (2.7–3.4) | 3.4 (3.3–3.6) | 3.6 (3.3–3.8) | 3.2 (3.1–3.4) | |
| T2 during COVID‐19 | 3.2 (3.1–3.3) | 3.4 (3.0–3.7) | 3.2 (3.0–3.3) | 3.3 (3.0–3.5) | 3.1 (2.9–3.2) | |
| Pressure | <0.01 | |||||
| Before COVID‐19 | 2.6 (2.5–2.7) | 2.7 (2.3–3.2) | 2.8 (2.6–2.9) | 2.8 (2.5–3.1) | 2.4 (2.2–2.6) | |
| T1 during COVID‐19 | 2.8 (2.7–2.9) | 2.8 (2.4–3.2) | 3.1 (2.9–3.3) | 3.0 (2.7–3.3) | 2.4 (2.2–2.6) | |
| T2 during COVID‐19 | 2.5 (2.4–2.6) | 2.7 (2.3–3.1) | 2.7 (2.6–2.9) | 2.7 (2.5–3.0) | 2.3 (2.1–2.4) | |
| Monitoring | 0.67 | |||||
| Before COVID‐19 | 3.4 (3.3–3.5) | 3.2 (2.7–3.6) | 3.3 (3.2–3.5) | 3.6 (3.3–3.9) | 3.4 (3.2–3.6) | |
| T1 during COVID‐19 | 3.6 (3.5–3.7) | 3.3 (2.9–3.7) | 3.6 (3.4–3.7) | 3.7 (3.5–4.0) | 3.5 (3.3–3.7) | |
| T2 during COVID‐19 | 3.6 (3.5–3.7) | 3.5 (3.1–3.9) | 3.6 (3.4–3.7) | 3.8 (3.6–4.1) | 3.5 (3.3–3.6) | |
Note: Results presented for the overall sample and by categories indicating changes in food security status across two timepoints during COVID‐19. Possible subscale scores ranged 1–5.
p Values are for the overall tests for interactions. Specific comparisons, where values at T1 and T2 during COVID‐19 differed from before COVID‐19 (reference category), are bolded if significant. Values presented represent adjusted means and 95% confidence intervals.
Abbreviations: COVID‐19, coronavirus disease 2019; T1, timepoint 1 (May 2020); T2, timepoint 2 (September 2020).
Tested for possible interactions in change in food security status × timepoint for each subscale.
4.3. Differences in longitudinal patterns in the home food environment and parent feeding practices by changes in food security status
4.3.1. Patterns of the home food environment by changes in food security status
From T1 to T2, 30% of families who became food insecure, and 44% of families who stayed food insecure, reported a decrease in the total amount of food in their home during this time; only 3%–6% of families who became or stayed food secure during this time reported this decrease. Similar patterns emerged for the amount of high‐calorie snack foods, desserts/sweets, and fresh foods in the home. A greater percentage of families who became or stayed food insecure reported a decrease in the amount of these foods, compared to families who became or stayed food secure. The amount of nonperishable processed foods in the home increased from T1 to T2 for about 40% of families who became or stayed food insecure and for 24% of families who stayed food secure.
4.3.2. Patterns of parent feeding practices by changes in food security status
Parents' concern for child overweight increased, and remained elevated, from before to across COVID‐19 for families who became or remained food insecure; these values increased, but returned to pre‐COVID‐19 values by T2, for families who became or stayed food secure. Restrictive and pressure feeding practices increased for some families from before COVID‐19 to T1 and returned to pre‐COVID‐19 values by T2 for all categories of food security status. Patterns in parents' reported use of monitoring did not differ by changes in food security status categories (p = 0.67).
5. DISCUSSION
This study provides follow‐up data on longitudinal patterns of food security, the home food environment, and parent feeding practices across COVID‐19. Initial patterns showed a large increase in the percentage of families experiencing food insecurity compared to before COVID‐19, with a decrease 4 months later when policy changes were in place to provide some economic relief. However, food insecurity rates in September 2020 remained considerably higher than before COVID‐19. Parents also reported an increase in concern for child overweight from before COVID‐19 to May 2020, which decreased but remained elevated in September 2020, particularly for families who became or stayed food insecure during this time. Parents use of restricting children's access to certain foods, pressuring their child to eat more, and monitoring children's eating initially increased during COVID‐19, while monitoring remained elevated, and restriction and pressure returned to pre‐COVID‐19 values. Lastly, changes in the home food environment were mixed at both timepoints, with some families reporting an increase, and other families reporting a decrease or no change, in the amount of different foods in their home. Given the transient nature of this pandemic, these longitudinal patterns regarding nutrition‐related factors across COVID‐19 provide valuable insight to inform our understanding of how this pandemic is impacting families over time.
The severe economic impacts of this global pandemic have occurred in parallel with a drastic increase in food insecurity in the United States. 13 At the height of government closures and stay‐at‐home orders, 54% of families in this study reported low or very low food security. 7 Four months later, 45% of families reported low or very low food security as this pandemic persisted. These patterns indicate a change in a positive direction yet leave considerable room for further improvement. Throughout these months, unemployment rates declined, 14 stay‐at‐home orders were lifted, 15 and stimulus bills provided some relief. 8 , 9 For example, SNAP issued emergency allotments for families to receive the maximum benefit as well as operating flexibilities, such as the expansion of online purchasing. 8 The Coronavirus Aid, Relief, and Economic Security Act provided a one‐time stimulus payment to families earning below a certain threshold, 9 and based on reported income, approximately 77% of families in this sample qualified for this stimulus payment. While these and other factors may have contributed to a temporary decline in food insecurity, evidence suggests that they are not enough. Only 15% of families in this study became food secure, while 6.2% became food insecure, between May and September 2020. Furthermore, less than half of this sample reported receiving benefits from SNAP, local food banks, unemployment, and school‐provided meals in September 2020. Other policy‐level factors, such as expired supplemental unemployment benefits, 16 failure to pass a second stimulus payment at the time of this study's data collection, 17 and not raising the maximum SNAP benefits that are insufficient to providing nutritious, adequate foods, 18 all likely contribute to persistent elevations in food insecurity. Moving forward, greater legislative efforts are needed to support families with limited access to adequate foods, including continued increased support of federal nutrition assistance programs, programmatic flexibilities and waivers, and enhanced unemployment benefits as our nation endures and recovers from COVID‐19. Furthermore, dissemination and implementation science will be crucial from a scientific perspective to ensure that evidence around food insecurity and child nutrition programs can be adopted and integrated into more equitable and sustainable policies beyond COVID‐19, thus enhancing these program's long‐term public health impact. 19
In May 2020, about one‐third of families in this sample reported an increase in the amount of desserts/sweets in the home. 7 Other studies conducted around this time also showed an increase in children's 20 and adults 21 consumption of unhealthy snack foods, compared to before COVID‐19. A few months later, in September 2020, about 30% of families in this sample reported a decreased amount of high‐calorie snack foods and desserts/sweets in their home, indicating a reduced presence of foods that tend to be calorie‐dense and nutrient‐poor for many families as the pandemic progressed. Greater purchasing of “comfort foods” and panic‐purchasing was seen during the initial months of COVID‐19 when family's lifestyles had suddenly changed. 22 , 23 A few months later, some of these purchasing behaviors may have subsided, as families adapted to new lifestyle changes. Furthermore, a greater percentage of families increased, rather than decreased, the amount of fresh foods in their home, with similar patterns observed for nonperishable processed foods. Future research is needed to examine how varying amounts of different foods in family's home impact children's dietary quality and weight status over time, particularly when children are spending more time at home compared to before COVID‐19, thus the home food environment is likely more salient.
A considerable percentage of families who became (30%) or stayed (44%) food insecure from May to September 2020 reported a decrease in the total amount of food in their home; while only 3%–6% of families who became/stayed food secure reported this decrease. This is concerning given that families with food insecurity are most affected by policies and structures that impede access to affordable foods, and long‐term decreases in food availability may widen the already‐prominent health disparities. Recent policy efforts have implemented creative ways to continue providing food to families who previously relied on school‐provided meals, 24 yet some families may be experiencing food insecurity for the first time, and logistical challenges and/or state‐wide variability instituting these adaptations may have prevented some families from receiving the full benefits of these programs 25 resulting in low uptake. 26 In this sample, only one‐fourth to one‐third of families were receiving school‐provided meals and SNAP benefits, respectively, and of these, about one‐fourth were not receiving these benefits prior to COVID‐19. During this unprecedented public health crisis, it is imperative that our nation continues to provide creative supports and strengthened initiatives to reach more families and provide food and financial resources to those in need.
Our previous data showed an increase in parents' concern for child overweight from before COVID‐19 to May 2020, 7 and these follow‐up data indicate a sustained increase by September 2020, particularly for families who became or stayed food insecure during this time. Food insecurity has been paradoxically linked with greater obesity risk, yet this relationship remains unclear among children. 27 , 28 In this study, 30% of parents reported child weight gain from May to September 2020, with no differences in these patterns by food security status. Almost half (48%) of children with reported weight gain were initially classified as having a normal weight, while a similar percentage (41%) was classified as having overweight/obesity. This presents the potential that some children may have changed weight class (e.g., normal weight to overweight), while others likely remained in the same weight class. Furthermore, weight gain due to the behavioral impacts of COVID‐19 versus normal child growth over time cannot be disentangled from these data. Nonetheless, these data serve as initial patterns of child weight change during COVID‐19, and more rigorous objective measures are needed in order to better understand the impacts of this pandemic on overweight/obesity risk. Furthermore, recent studies have shown that other obesogenic behaviors, such as children's and adults' physical activity, sedentary behaviors, and screen time have also been negatively impacted by COVID‐19. 29 , 30 Data on changes in multiple health behaviors (e.g., dietary intake, sleep, physical activity, and screen time) over time is needed in the same sample of children to better understand which behaviors, or combination of behaviors, appear to have most impacted children's weight gain during this time.
During the initial wave of COVID‐19, cross‐sectional analyses indicated that greater parental stress was associated with both positive and negative changes in child feeding practices, such as using food to manage children's emotions, creating routines around eating occasions, and engaging with children at mealtime more often. 20 These longitudinal data showed that parents' use of restriction and pressure to eat initially rose during COVID‐19 but returned to baseline values a few months later. This temporary change has positive implications on children's health, given these feeding practices are most commonly associated with child weight and unhealthful eating behaviors. 31 , 32 , 33 , 34 , 35 , 36 Parents' use of monitoring—or keeping track of their child's consumption of different foods—initially rose during COVID‐19 and remained elevated months later. Parents are perhaps more aware and involved in what their children consume, as families are spending more time together during this pandemic. Previous studies have shown mixed findings related to parental monitoring, with positive associations on children's dietary intake, as well as no associations with child diet and weight. 37 It is likely that parental monitoring is beneficial for some children, based on certain characteristics like age and temperament, and for other children too much can become counterproductive. 38 Furthermore, the clinical significance for the magnitude of change in CFQ subscales is uncertain, given the lack of a clinically meaningful change or cut‐off score. Some childhood obesity interventions have modified parent feeding practices at a similar magnitude of change as shown in these data and demonstrated associations with body mass index and dietary intake. 38 , 39 , 40 However, ultimately, these findings should be interpreted as overall patterns showing how parent feeding practices fluctuate alongside the social, environmental, and financial impacts of COVID‐19.
The limitations of this study include the use of a convenience sample, with limited racial/ethnic diversity, that is not nationally representative of all the US parents. While the retention rate was high, the parents lost to follow‐up tended to be from racial/ethnic minoritized backgrounds and given that these populations tend to experience more adverse impacts from COVID‐19, 41 these findings likely represent a smaller magnitude of change than what would be expected among more diverse groups. Other limitations include the use of self‐reported questionnaires subject to recall and response biases, and parenting behaviors could have been differentially influenced by local laws in different states at the time of data collection. Lastly, the limitations of parent‐reported child weight measures are well‐known 42 , 43 ; however, the design of this nationwide study did not permit the use of objectively measured child weight. The largest strengths of this study include the high retention rate and the longitudinal design at two key timepoints during COVID‐19 which allowed for the quantification of within‐family changes across time and provides strengthened data compared to other cross‐sectional studies examining similar constructs during this pandemic.
6. CONCLUSION
This follow‐up study provides novel data on the longitudinal changes in food security, the home food environment, and parent feeding practices across COVID‐19. These findings reveal some positive changes, yet there is substantial room for improvement, particularly related to amount of families experiencing food insecurity. The length of this pandemic remains uncertain, and the lingering effects will likely persist for years to come. As such, empirical data, such as these, are critical to informing public health policies and supports for families in need, in order to reduce the negative impacts of COVID‐19 on family's nutrition and health.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Elizabeth L. Adams and Melanie K. Bean conceptualized the research questions and obtained grant funding. Elizabeth L. Adams completed data collection, data analyses, and drafted the initial version of the manuscript. All authors designed the study, interpreted the data, critically reviewed the manuscript, and approved the final version as submitted.
ACKNOWLEDGMENTS
This study was funded by the Virginia Commonwealth University coronavirus disease 2019 Rapid Research Funding program. This work was also supported by the National Institutes of Health (Grant Number 2T32CA093423) for Elizabeth L. Adams postdoctoral effort.
Adams EL, Caccavale LJ, Smith D, Bean MK. Longitudinal patterns of food insecurity, the home food environment, and parent feeding practices during COVID‐19. Obes Sci Pract. 2021;7(4):415–424. 10.1002/osp4.499
REFERENCES
- 1. Shanzenbach DW, Pitts A. How Much Has Food Insecurity Risen? Evidence from the Census Household Pulse Survey. Institute for Policy Research; 2020. https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjatI-xq7_tAhVSElkFHUDZDtUQFjAAegQIBRAC&url=https%3A%2F%2Fwww.ipr.northwestern.edu%2Fdocuments%2Freports%2Fipr-rapid-research-reports-pulse-hh-data-10-june-2020.pdf&usg=AOvVaw1bwIwhgDUsA8BYvV_OpOKm. [Google Scholar]
- 2. United States Census Bureau . Household Pulse Survey Data Tables; 2020. https://www.census.gov/programs‐surveys/household‐pulse‐survey/data.html. [Google Scholar]
- 3. Measurement Information Page . Food Security in the U.S. United States Department of Agriculture Economic Research Service; 2020. https://www.ers.usda.gov/topics/food‐nutrition‐assistance/food‐security‐in‐the‐us/measurement.aspx. [Google Scholar]
- 4. Feeding America . Child Food Insecurity. Mind the Meal Gap; 2020. https://www.feedingamerica.org/sites/default/files/2020‐06/Map%20the%20Meal%20Gap%202020%20Child%20Food%20Insecurity%20Module.pdf. [Google Scholar]
- 5. Coleman‐Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2018 (ERR‐270). U.S. Department of Agriculture, Economic Research Service; 2019. [Google Scholar]
- 6. Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID‐19–related school closings and risk of weight gain among children. Obesity. 2020;28:1008–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Adams EL, Caccavale LJ, Smith D, Bean MK. Food insecurity, the home food environment, and parent feeding practices in the era of COVID‐19. Obesity. 2020;28:2056‐2063. 10.1002/oby.22996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. United States Department of Agriculture . Food and Nutrition Service. SNAP State Agencies; 2020. https://fns‐prod.azureedge.net/sites/default/files/resource‐files/SNAP‐COVID‐EmergencyAllotmentsGuidance.pdf. [Google Scholar]
- 9. Aid Coronavirus . Relief, and Economic Security Act or the CARES Act. H.R. 748, 116th Congress; 2020. [Google Scholar]
- 10. United States Department of Agriculture Economic Research Service . U.S. Household Food Security Survey Module: Six‐Item Short Form; 2012. https://www.ers.usda.gov/media/8282/short2012.pdf. [Google Scholar]
- 11. Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the household food security scale. Am J Publ Health. 1999;89:1231‐1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Birch LL, Fisher JO, Grimm‐Thomas K, Markey CN, Sawyer R, Johnson Sl. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36:201‐210. [DOI] [PubMed] [Google Scholar]
- 13. Feeding America . The Impact of the Coronavirus on Food Insecurity in 2020; https://www.feedingamerica.org/sites/default/files/2020‐10/Brief_Local%20Impact_10.2020_0.pdf. [Google Scholar]
- 14. U.S. Bureau of Labor Statistics . Economic Situation News Release. The Employment Situation – September 2020; 2020. https://www.bls.gov/news.release/archives/empsit_10022020.htm. [Google Scholar]
- 15. Johns Hopkins University & Medicine Coronavirus Resource Center . Impact of Opening and Closing Decisions by State; 2020. https://coronavirus.jhu.edu/data/state‐timeline/new‐confirmed‐cases/alabama. [Google Scholar]
- 16. U.S. Department of Labor . Unemployment Insurance Relief during COVID‐19 Outbreak; 2020. https://www.dol.gov/coronavirus/unemployment‐insurance. [Google Scholar]
- 17. GovTrack . HR 6800 (116th): The Heroes Act. https://www.govtrack.us/congress/bills/116/hr6800. [Google Scholar]
- 18. Bleich S, Dunn C, Fleischhacker S. The Impact of Increasing SNAP Benefits on Stabilizing the Economy, Reducing Poverty and Food Insecurity amid COVID‐19 Pandemic. Durham, NC: Healthy Eating Research; 2020. http://healthyeatingresearch.org. [Google Scholar]
- 19. Lane HG, Turner L, Dunn CG. Leveraging implementation science in the public health response to COVID‐19: child food insecurity and federal nutrition assistance programs. Publ Health Rep. 2020;135(6):728‐736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jansen E, Thapaliya G, Aghababian A, Sadler J, Carnell S. Parental stress, food parenting practices and child snack intake during the COVID‐19 pandemic. Appetite. 2021;161:105119. 10.1016/j.appet.2021.105119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Flanagan WE, Beyl RA, Fearnbach SN, Altazan AD, Martin CK, Redman LM. The impact of COVID‐19 stay‐at‐home orders on health behaviors in adults. Obesity (Silver Spring). 2020;29:438‐445. 10.1002/oby.23006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Knoll C. Panicked Shoppers Empty Shelves as Coronavirus Anxiety Rises. The New York Times ; 2020. https://www.nytimes.com/2020/03/13/nyregion/coronavirus‐panic‐buying.html. [Google Scholar]
- 23. Creswell J. ‘I Just Need the Comfort’: Processed Foods Make a Pandemic Comeback. The New York Times ; 2020. https://www.nytimes.com/2020/04/07/business/coronavirus‐processed‐foods.html. [Google Scholar]
- 24. United States Department of Agriculture . Food and Nutrition Service. Child Nutrition COVID‐19 Waivers; 2020. https://www.fns.usda.gov/programs/fns‐disaster‐assistance/fns‐responds‐covid‐19/child‐nutrition‐covid‐19‐waivers. [Google Scholar]
- 25. Kinsey EW, Hecht AA, Dunn CG, et al. School closures during COVID‐19: opportunities for innovative meal service. Am J Publ Health. 2020;110(11):1635‐1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bauer L, Parsons J. Why Extend Pandemic EBT? When Schools are Closed, Many Fewer Eligible Children Receive Meals. The Brookings Institute; 2020. https://www.brookings.edu/blog/up‐front/2020/09/21/why‐extend‐pandemic‐ebt‐when‐schools‐are‐closed‐many‐fewer‐eligible‐children‐receive‐meals/. [Google Scholar]
- 27. Dinour LM, Bergen D, Yeh MC. The food insecurity‐obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc. 2007;107(11):1952‐1961. [DOI] [PubMed] [Google Scholar]
- 28. Franklin B, Jones A, Love D, Puckett S, Macklin J, White‐Means S. Exploring mediators of food insecurity and obesity: a review of recent literature. J Community Health. 2012;37(1):253‐264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yang S, Guo B, Ao L, Yang C, Zhang L, Zhou J, Jia P. Obesity and activity patterns before and during COVID‐19 lockdown among youths in China. Clin Obes. 2020;10(6):e12416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pietrobelli A, Pecoraro L, Ferruzzi A, et al. Effects of COVID‐19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring). 2020;28:1382‐1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: conception to adolescence. J Law Med Ethics. 2007;35:22‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ventura AK, Birch LL. Does parenting affect children's eating and weight status? Int J Behav Nutr Phys Activ. 2008;5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Faith M, Scanlon K, Birch LL, Francis LA, Sherry B. Parent‐child feeding strategies and their relationship to child eating and weight status. Obes Res. 2004;12:1711‐1722. [DOI] [PubMed] [Google Scholar]
- 34. Birch LL, Fisher JO. Development of eating behaviours among children and adolescents. Pediatrics. 1998;101:539‐549. [PubMed] [Google Scholar]
- 35. Fisher JO, Birch LL. Restricting access to foods and children's eating. Appetite. 1999;32:405‐419. [DOI] [PubMed] [Google Scholar]
- 36. Spruijt‐Metz D, Lindquist CH, Birch LL, Fisher JO, Goran MI. Relation between mothers'child‐feeding practices and children's adiposity. Am J Clin Nutr. 2002;75:581‐586. [DOI] [PubMed] [Google Scholar]
- 37. Vaughn AE, Ward DS, Fisher JO, et al. Fundamental constructs in food parenting practices: a content map to guide future research. Nutr Rev. 2016;74(2):98‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Burrows T, Warren JM, Collins CE. The impact of a child obesity treatment intervention on parent child‐feeding practices. Int J Pediatr Obes. 2010;5:43‐50. [DOI] [PubMed] [Google Scholar]
- 39. Steele RG, Jensen CD, Gayes LA, Leibold HC. Medium is the message: moderate parental control of feeding correlates with improved weight outcome in a pediatric obesity intervention. J Pediatr Psychol. 2014;39:708‐717. [DOI] [PubMed] [Google Scholar]
- 40. Holland JC, Kolko RP, Stein RI, et al. Modifications in parent feeding practices and child diet during family‐based behavioral treatment improve child zBMI. Obesity. 2014;22:E119‐E126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Center for Disease Control and Prevention . Health Equity Considerations and Racial and Ethnic Minority Groups; 2020. https://www.cdc.gov/coronavirus/2019‐ncov/community/health‐equity/race‐ethnicity.html. [Google Scholar]
- 42. Lundahl A, Kidwell KM, Nelson TD. Parental underestimates of child weight: a meta‐analysis. Pediatrics. 2014;133(3):e689‐e703. [DOI] [PubMed] [Google Scholar]
- 43. Rietmeijer‐Mentink M, Paulis WD, van Middelkoop M, et al. Difference between parental perception and actual weight status of children: a systematic review. Matern Child Nutr. 2013;9(1):3‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]


