Abstract
The recent pandemic of COVID‐19 revealed that a highly transmissible virus threatens all humanity because extensive mobility, migration, and millions of passengers who travel worldwide shape our globalized environment and make containment of a virus more difficult. In a war between humans and viruses, we should have the necessary weapons, such as masks, gloves, ventilators, and so forth. However, during the COVID‐19 outbreak, there was a shortage of this basic medical and personal protective equipment (MAPPE), even for the health workers. This note focuses on this issue and suggests that a global organization, which stores and renews basic MAPPE would be beneficial in the fight against the next pandemic and that such an organization can be established without significantly increasing the public expenses of the countries.
Keywords: COVID‐19, globalization, healthcare systems, pandemic, PPE
Highlights
-
•
During the COVID‐19 outbreak, there was a shortage of basic medical equipment.
-
•
There is a need for a global organization to stockpile medical equipment.
-
•
This stockpile should be renewed regularly to ensure modern equipment.
-
•
We suggest a procedure that satisfies the abovementioned and involves low cost.
-
•
The organization can reduce the economic consequences of the pandemic and death toll, as well as promote solidarity.
INTRODUCTION
The year 2020 will be remembered as the year of the COVID‐19 pandemic outbreak. By November 30, 2020, more than 62 million confirmed cases had been recorded globally and more than 1.45 million of these patients have died.1 To reduce the spread of the virus throughout the world, several restrictions were imposed by government authorities, such as mobility restrictions, social distance measures, and lockdowns. This unprecedented global health crisis and the protective measures taken to slow the spread of the disease generated a blend of negative economic (Almond & Mazumder, 2005; Keogh‐Brown et al., 2010), psychological (Kumar & Nayar, 2020), and social (Bonaccorsi et al., 2020) consequences.
These extreme conditions would lead to blame games (Roy et al., 2020), and a characteristic conflict took place during the early stages of the pandemic outbreak between the U.S President and the World Health Organization (WHO). President Trump accused WHO for “…severely mismanaging and covering up the spread of the coronavirus,”2 while the Director‐General of the WHO Tedros Adhanom Ghebreyesus said that WHO “…declared the international emergency at the right time when there were only 82 cases outside of China and no deaths and the rest of the world had enough time to respond.”3 Afterward, several conspiracy theories on the origin of the virus emerged (Nie, 2020).
This note does not take a side in these conflicts. Many studies have been presented in the international literature, in several fields of study, from health and medicine to logistics and socioeconomics, and suggest policies to resolve deficiencies and correct omissions that were revealed during the COVID‐19 pandemic. Instead, this note focuses on an issue that emerged during the early stages of the pandemic: the significant shortage of basic Medical and Personal Protective Equipment, such as masks, gloves, ventilators (hereafter “MAPPE”).
A BRIEF TIMELINE OF THE COVID‐19 OUTBREAK AND OUR MOTIVATION FOR THE STUDY
A brief timeline of the COVID‐19 outbreak is the following: on December 31, 2019, the WHO China Country Office was informed of clustered cases of unknown etiology pneumonia in Wuhan City, China. The Chinese authorities identified a new type of coronavirus and the WHO named the novel coronavirus, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS‐CoV‐2) and the disease coronavirus disease (COVID‐19).4 On January 30, 2020, WHO declared the outbreak a Public Health Emergency of International Concern, and on March 11, COVID‐19 was declared a pandemic.5
In the early stages of the COVID‐19 outbreak, many politicians and government authorities declared that “we are at war with an invisible enemy,” but, at the same time, there were alarming reports about critical shortages of basic weapons: MAPPE.6, 7, 8, 9
To illustrate this paradox, I use a Google Trends code that enables me to present the Google Searches Index from all over the world for the terms “Coronavirus,” “Medical Masks,” and “Medical Masks Shortage” (Figure 1). The “Coronavirus” index is used as a fear sentiment index (Vasileiou, 2020) in which higher index indicates higher fear. A basic MAPPE is a medical mask, which is a highly recommended protective measure against the spread of the virus. However, as Figure 1 shows, when the searches for the medical masks were at their highest levels there was a shortage in the market, which means that during the early stages we did not have the weapons to fight the invisible enemy.
Figure 1.
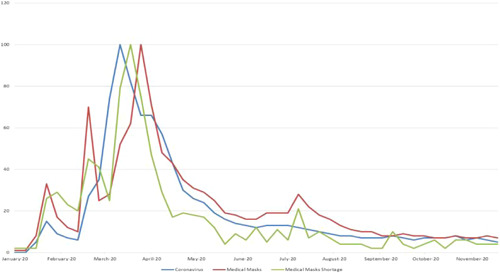
Google Trends searches
The COVID‐19 outbreak echoed a 2015 TED speech in which Bill Gates warned of the strong likelihood of a future pandemic outbreak, and the fact that humanity needs an army for a war against germs, that is, “A Global Alert and Response System,” which aims to:
-
•
strengthen health systems in poor countries,
-
•
create a medical corps,
-
•
run germ games, and
-
•
step up research development (Gate, 2015).
However, as Gates notes, the budgetary requirements of such a system were unknown. Like Gates, we cannot estimate the budget of such an organization, but we can present a policy that could resolve the MAPPE shortage without significant costs to national and international budgets, and which would prove beneficial for the entire world.
NEED FOR MEDICAL AND BASIC PERSONAL PROTECTION EQUIPMENT: WHY THERE WAS A SHORTAGE AND WHAT WE SHOULD LEARN FROM THE COVID‐19 PANDEMIC
COVID‐19 showed that it is too difficult to increase the production of basic MAPPE equipment, such as masks, gloves, ventilators, in the midst of an emergent pandemic.10, 11, 12, 13, 14 Moreover, when the pandemic hits a country that accounts for a large share of the global production of this equipment, supply chains collapse. For instance, China, which is a major global producer of masks, was the first country to suffer from the new disease during the first months of 2020.15 For this reason, management of MAPPE supplies was even harder than it would have been if the disease had broken out in another country. How can we address this problem? Part of the solution could be a MAPPE stock, which would enable us to respond to the increased demand for medical equipment when cases increase, and this way give time to industries to produce more MAPPE.
Therefore, at least one of the following should be done: (i) the production of basic MAPPE should not be over‐reliant on a specific country, (ii) national MAPPE stockpiles should be established, and/or (iii) a global reserve should be readily available for use when and where it is needed. (i) and (ii) should be explored by governments around the globe as they involve various socioeconomic parameters, which are specific to each individual country, a fact that adds complexity to the analysis of such efforts and goes beyond this note's scope. (iii)—though seemingly more complex—can prove more reliable and sustainable than the others.
Additionally, COVID‐19 was a hard lesson for humanity because the risk of a pandemic had been underestimated and humanity was not ready to effectively respond to these extreme health stress conditions. As Gates mentions in his speech, many countries have reserves in military weapons, but they do not have enough reserves in “medical weapons,” such as masks, ventilators, or gloves for a war against a virus. Otherwise, we will encounter significant shortages in the future as supplies will again outpace demand, jeopardizing humanity's efforts to contain the spread of contagious viruses.
Moreover, our experience with COVID‐19 revealed that the shortage of basic MAPPE was apparent during the COVID‐19 outbreak and had a significant impact not only on citizens but also on healthcare workers (Ming et al., 2020).16, 17, 18 It is like sending our troops to war without the appropriate equipment. Failing to protect healthcare workers not only constitutes a moral failure but it also puts immense pressure on healthcare systems, which are then forced to deal with a surge in patients while understaffed.
Therefore, it is clear that a MAPPE reserve should exist, but why did it not? As mentioned above, one reason is that the likelihood or severity of a pandemic was underestimated even though there were documented warnings about the dangers of a pandemic before the emergence of COVID‐19 (Jonas, 2013). A second argument could be associated with economic reasons, for example.
-
•
the cost of the surplus equipment, which may be significantly high for some poor countries to afford, and
-
•
a national stockpile strategy may be neglected even in wealthy countries when an economic recession comes and/or contractionary fiscal policies need to be implemented.
A third reason could be associated with poor management: for example, there were countries that had tried to have a MAPPE reserve, but during the COVID‐19 pandemic there was news concerning national repositories, which had not been renewed. As a result, when the crisis broke out, this equipment had expired.19
The COVID‐19 outbreak may give us many lessons regarding the cost of a pandemic, ways to avoid a virus spread, and policies on how to respond rapidly in similar situations in the future. Any policy on medical stock equipment should be feasible and sustainable because we do not know exactly when and where a new life‐threatening virus will emerge, so we must always be prepared. Swift action is required no matter what the economic conditions are.
Therefore, the following question arises when we consider the events that unfolded during the initial stages of the COVID‐19 pandemic: Should the MAPPE reserve be national or international? A possible argument could be that similarly to national security, for which each country has its own army equipment, each country should be responsible for its own national medical equipment stockpile. However, there are certain disadvantages to this approach.
Beyond the economic and administrative issues surrounding a sustainable national MAPPE, the COVID‐19 experience shows that during pandemics we should act together as a global community and not as individual countries. In a globalized environment with global mobility and migration, a highly transmissible virus could travel around the world in a matter of days (Vasileiou et al., 2020). In such a case, even the strong healthcare systems of advanced economies, for example, the United States, France, the United Kingdom, Spain, Italy, and so forth, cannot respond effectively20 and no national reserve is adequate if a country is badly hit by a pandemic. Therefore, a strategic plan to build a large MAPPE reserve that will be both affordable and sustainable might have a greater chance of success under the auspices of a joint international effort rather than a single country.
What will happen if the next pandemic emerges in a low‐income country? Should other countries let these people fight against the virus on their own? Additionally, a virus can easily spread beyond national borders and a national emergency can quickly escalate to an international one. A global and immediate response is required to ensure that an outbreak is effectively contained at a local level before the spread becomes uncontrollable.
What happened during the early stages of the COVID‐19 outbreak? Was there solidarity? Reports concerning bans on the export of medical equipment,21, 22 and accusations of “modern piracy”23 show that the MAPPE shortage not only undermined the efforts to fight the pandemic, but also the solidarity that globalization requires.24
COULD A GLOBAL MEDICAL STOCK ORGANIZATION BE A SOLUTION?
The necessity of a MAPPE reserve has been presented above, and in this section, we present our suggestions for an international and sustainable MAPPE reserve that could resolve all the aforementioned drawbacks. Thus, the reserve should:
-
•
be global, and belong to all countries because when an emergency arises, there are urgent needs that a single country reserve will not be able to meet,
-
•
be easily transported when and where it is needed, which means that it should be ready for use in any battlefield against viruses, just like the army,
-
•
satisfy certain specifications and should not be old and outdated; thus, it should not be stored in a repository for a long time because in case of emergency we will not only need quantity, but also quality, and
-
•
be sustainable and unaffected by economic cycles.
As the recent COVID‐19 experience has revealed that the cost of a pandemic is very high and certainly higher than the cost that such a stockpile requires. Therefore, securing initial funding from a coalition of governments should be identified as a priority after the end of the current pandemic25 and significant information about the needs in MAPPE during the early stages of the COVID‐19 pandemic can help us estimate the cost of a global MAPPE reserve. How and how much should each country contribute to this fund? Several criteria may be set, for example, a country's population, its status as an advanced, emerging, or developing economy, GDP per capita in USD multiplied by its population, and so forth, to find the best solution regarding how much each country should contribute to the MAPPE stock depending on their economic power.
The next issue is to find a solution for the optimal renewal of the MAPPE. Our suggestion is the following: a “first in, first out” procedure should be followed to avoid expiration costs, especially for medical equipment that has a short service life. How can this be achieved? The member countries of this organization will “buy” medical equipment from the organization to meet part of the regular needs of their healthcare systems.26 With the money from these transactions, the organization will renew its stock (Figure 2 presents an example of the suggested procedure). This way, countries will have the necessary equipment to cover part of their regular needs and, at the same time, there will be a modern and ready to ship global stock of medical equipment to meet any sudden surge in demand.
Figure 2.
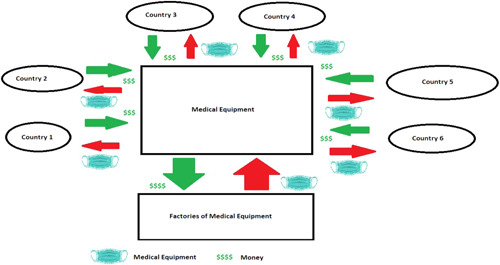
A Global Medical Stock Organization and its “First In, First Out” process to renew equipment
The cost for the maintenance of the global MAPPE surplus for an organization, which will work in this way will not be high. Our intention is to avoid presenting economic data that cannot be measured in most detail and the real economic cost of COVID‐19 will be estimated in the future. However, the costs involved in setting up and running the suggested organization will not be prohibitive, especially when we consider the fact that the measures already taken to mitigate the economic impact of the pandemic include generous stimulus packages: in the United States alone, a $2 trillion stimulus pack has already been announced,27 and the European Central Bank (ECB) also announced a €750 billion Pandemic Emergency Purchase Programme (PEPP),28 while a sharp recession is expected for the following year(s).
If the aim is to protect the economy from a future pandemic, this organization should not be considered a cost, but it should be viewed as insurance/investment because it will help contain the spread of an emerging pathogen by providing medical equipment when the crisis arises and hence lessen the effects of infectious disease on the economy. In the future, we should not send health workers to war against a virus without MAPPE because they are the first line of defense on the battlefield.
We do not claim that the suggested organization will eliminate the total cost of the pandemic, but it will act as a shield in the battle against a virus: it will provide more safety at a low cost and it will save more lives. Additionally, the creation of such an organization emphasizes the need for solidarity among nations and promotes international cooperation in our globalized world. A global surplus means that countries will not need to introduce bans, and there will be no need for “modern piracy” because the repository will give some time to the industries to produce increased volumes of the required equipment.
CONCLUSIONS
The COVID‐19 pandemic, like all crises, may prove to be a useful lesson for all of us if we study the data and the facts carefully. This pandemic has demonstrated that in the globalized contemporary environment we live in, with many economic relationships between the countries, the battle is between humanity and viruses. A highly transmissible virus can travel fast around the world because of population mobility and hundreds of thousands of flights every day.29 Global issues need a global response because if a virus is not contained and spreads beyond its place of origin, such as SARS‐Cov‐2, it can become a pandemic.
The pandemic revealed many deficiencies, and in this study, we choose to focus on the shortage of basic MAPPE, which was observed during the COVID‐19 outbreak, for example, masks, gloves, and ventilators. Humanity did not have the required “medical weapons” in the war against SARS‐CoV‐2, even though it invests enormous amounts in military weapons it might never use (Gates, 2015).
Why don't we invest in medical weapons? As we present in this paper, it is very difficult for each country individually to maintain a significant surplus in modern medical equipment in the long run. The needs are enormous when a pandemic breaks out and it is not easy to ramp up production of medical equipment and PPE or modify production lines at short notice. As a result, precious time is lost. A surplus of MAPPE would make it easier to ensure equitable distribution of supplies and help curb the spread of a virus, thus minimizing the impact of a pandemic. The cost for this surplus may be huge for a single country to bear and the suggested design for a global MAPPE reserve does not involve increased cost.
If global leaders decide to build a global organization, which stores medical equipment and renews this equipment using the “first in, first out” approach, the cost for the global economy will be significantly low relative to the global GDP. However, the benefits will be major: a crucial surplus of MAPPE to help fight a future pandemic and minimize an international health risk, as well as messages of solidarity among the nations of the world. Such an organization could contribute to a more stable economic environment because it will reduce the economic risk caused by health risk, but most importantly it will save lives.
CONFLICTS OF INTEREST
The author declares that there are no conflicts of interest.
Biography
Evangelos Vasileiou, Ph.D, is an Assistant Professor at the University of the Aegean, School of Engineering, Department of Financial and Management Engineering, Chios, Greece.
Vasileiou, E. (2021). Fighting a war without weapons? Lessons from the COVID‐19 outbreak. World Medical & Health Policy. 13, 383–390. 10.1002/wmh3.431
ENDNOTES
According to Johns Hopkins Coronavirus Resource Center: https://coronavirus.jhu.edu/map.html.
Some highlights from the Novel Coronavirus (2019‐nCoV) SITUATION REPORT—1 (World Health Organization): https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf.
https://www.euronews.com/2020/04/21/a-mostly-virtual-westminster-reopens-amidst-ppe-shortage-debacle
The death toll from COVID‐19 is very high in the countries we mentioned as you can see in several COVID‐19 databases.
https://www.nytimes.com/2020/03/07/business/eu-exports-medical-equipment.html, https://abcnews.go.com/Health/wireStory/scramble-virus-supplies-strains-global-solidarity-69958117
A pandemic is global and hence a global response is needed. This is a matter of values that reflects concerns about the world and society we want to live in. For example, if COVID‐19 emerged in a poor country and this county did not have enough MAPPE reserves due to economic issues, would it be an acceptable solution to let the death toll increase because of lack of protective measures?
Many organizations have been established after crisis periods, for example, International Monetary Fund and World Bank after World War II.
Member countries will review the quality of the equipment.
REFERENCES
- Almond, D. , & Mazumder, B. (2005). The 1918 influenza pandemic and subsequent health outcomes: An analysis of SIPP data. American Economic Review, 95(2), 258–262. 10.1257/000282805774669943 [DOI] [PubMed] [Google Scholar]
- Bonaccorsi, G. , Pierri, F. , Cinelli, M. , Flori, A. , Galeazzi, A. , Porcelli, F. , Schmidt, A. L. , Valensise, C. M. , Scala, A. , Quattrociocchi, W. , & Pammolli, F. (2020). Economic and social consequences of human mobility restrictions under COVID‐19. Proceedings of the National Academy of Sciences of the United States of America, 117(27), 15530–15535. 10.1073/pnas.2007658117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates, B. (2015). The next outbreak? We're not ready. TED. https://www.ted.com/talks/bill_gates_the_next_outbreak_we_re_not_ready?language=en
- Jonas, O. (2013). Pandemic risk. World Bank. ; https://openknowledge.worldbank.org/handle/10986/16343 [Google Scholar]
- Keogh‐Brown, M. R. , Wren‐Lewis, S. , Edmunds, W. J. , Beutels, P. , & Smith, R. D. (2010). The possible macroeconomic impact on the UK of an influenza pandemic. Health Economics, 19(11), 1345–1360. 10.1002/hec.1554 [DOI] [PubMed] [Google Scholar]
- Kumar, A. , & Nayar, K. R. (2020). COVID 19 and its mental health consequences. Journal of Mental Health, 1–2, 817–818. 10.1080/09638237.2020.1757052 [DOI] [PubMed] [Google Scholar]
- Ming, X. , Ray, C. , & Bandari, M. (2020). Beyond the PPE shortage: Improperly fitting personal protective equipment and COVID‐19 transmission among health care professionals. Hospital Practice, 48(5), 246–247. 10.1080/21548331.2020.1802172 [DOI] [PubMed] [Google Scholar]
- Nie, J.‐B. (2020). In the shadow of biological warfare: Conspiracy theories on the origins of COVID‐19 and enhancing global governance of biosafety as a matter of urgency. Journal of Bioethical Inquiry, 17(4), 567–574. 10.1007/s11673-020-10025-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy, M. , Moreau, N. , Rousseau, C. , Mercier, A. , Wilson, A. , & Atlani‐Duault, L. (2020). Ebola and localized blame on social media: Analysis of Twitter and Facebook conversations during the 2014–2015 Ebola epidemic. Culture, Medicine and Psychiatry, 44(1), 56–79. 10.1007/s11013-019-09635-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasileiou, E. (2020). Behavioral finance and market efficiency in the time of the COVID‐19 pandemic: Does fear drive the market? International Review of Applied Economics, 35(2), 224–241. 10.1080/02692171.2020.1864301 [DOI] [Google Scholar]
- Vasileiou, E. , Samitas, A. , Karagiannaki, M. , & Dandu, J. (2020). Health risk and the efficient market hypothesis in the time of COVID‐19. International Review of Applied Economics, 35(2), 210–223. 10.1080/02692171.2020.1864299 [DOI] [Google Scholar]


