Dear Editor,
The COVID‐19 pandemic continues its impact worldwide. Estimated prevalence of skin findings in patients with COVID‐19 is estimated to be 5%, but the prevalence and clinical presentation varies greatly among series (0.1–60%). 1 National registries have become an important tool to understand this highly contagious and potentially mortal infection. In this report, we aimed to describe the results of the Mexican Academy of Dermatology nationwide survey of dermatological manifestations of COVID‐19 infection in Mexico.
On July 1, 2020, we established a national registry to collect demographic and clinical information of patients with COVID‐19 cutaneous manifestations. Mexican dermatologists were invited to fill out an electronic survey. The survey was shared via the official social media accounts and the official website of the Mexican Academy of Dermatology. No protected health information was collected, and all data were deidentified. The survey collected demographic data, COVID‐19 diagnosis type (PCR, serum antibodies, clinical, or otherwise unspecified), and dermatological manifestations related to the infection. Subjects with laboratory confirmation of COVID‐19 or clinical suspicion of the infection were included in the study. Each physician was responsible for obtaining informed consent regarding clinical pictures uploaded to the survey webpage. The analysis was performed blindly by two of the authors with SPSS v. 23 (Armonk, NY, USA).
Cases uploaded to the survey from July 9, 2020, to December 7, 2020, were included. A total of 164 cases were included in the final analysis. A total of 120 subjects (73.3%) were women. The most common age range was 31–40 with 23.8% of the total followed by 21–30 (18.3%) and 41–50 (17.1%). A total of 86 (52.4%) subjects had a confirmed diagnostic test by PCR. An additional nine (5.5%) has a positive test for serum antibodies. The rest of the subjects had a clinical COVID‐19 diagnosis (29, 17.7%), or the information was unspecified (40, 24.4%). Demographic and clinical information of the cases are shown in Table 1.
Table 1.
COVID‐19 dermatological manifestations in Mexico
| Characteristic | Value (%) |
|---|---|
| Total | 164 |
| Sex | |
| Female | 120 (73.3) |
| Male | 44 (26.8) |
| Age (range) | |
| 31–40 | 39 (23.8) |
| 21–30 | 30 (18.3) |
| 41–50 | 28 (17.1) |
| 51–60 | 22 (13.4) |
| 11–20 | 14 (8.5) |
| 0–10 | 22 (13.4) |
| 61–70 | 6 (3.7) |
| 71–80 | 3 (1.8) |
| Anatomical site a | |
| Trunk | 49 (29.9) |
| Lower extremities | 43 (26.2) |
| Upper extremities | 33 (20.1) |
| Face | 17 (10.4) |
| Oral mucosa | 14 (8.5) |
| Palms/Soles | 14 (8.5) |
| Scalp | 10 (6.1) |
| Extensor surfaces | 9 (5.5) |
| Flexor surfaces | 7 (4.3) |
| Skin manifestation a | |
| Urticaria | 40 (24.4) |
| Maculopapular eruption | 28 (23.2) |
| Varicelliform eruption | 25 (15.2) |
| Enanthema | 13 (7.9) |
| Pernio‐like eruption | 11 (6.7) |
| Petechiae/Purpura | 10 (6.1) |
| Palmar erythema | 10 (6.1) |
| Pityriasis rosea‐like eruption | 7 (4.3) |
| Alopecia (unspecified) | 6 (3.7) |
| Elbow/knee erythema | 6 (3.7) |
| Erythema multiforme‐like eruption | 5 (3) |
| Livedo racemosa | 2 (1.2) |
| COVID‐19 diagnosis/testing | |
| PCR positive | 86 (52.4) |
| Positive antibodies | 9 (5.5) |
| Clinical diagnosis | 29 (17.7) |
| Unspecified diagnostic test | 40 (24.4) |
Patients may fall into more than one category.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
The dermatological manifestations of COVID‐19 are shown in Table 1 and Figure 1. The most common manifestations were urticaria in 40 (24.4%), maculopapular eruption in 28 (23.2%), varicella‐like eruption in 25 (15.2%), enanthema in 13 (7.9%), and a pernio‐like eruption in 11 (6.7%). Of interest 10 (6.1%) patients presented palmar erythema and six (3.7%) elbow/knee erythema, manifestations seldom associated with COVID‐19.
Figure 1.
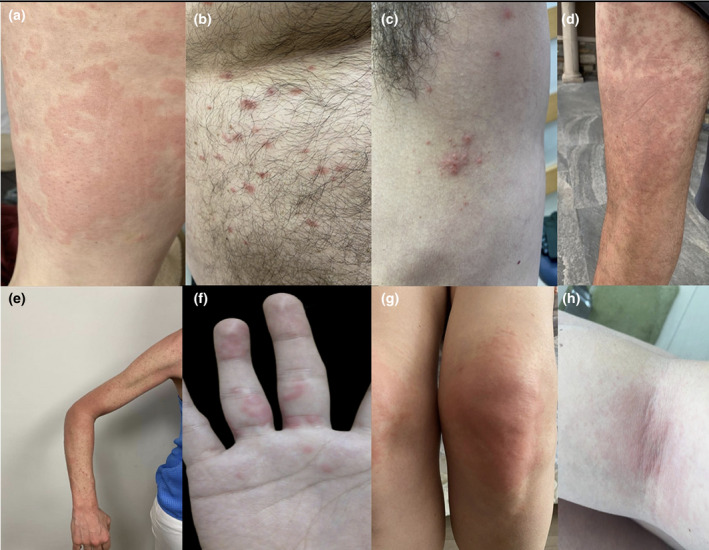
Dermatologic manifestations of COVID‐19 infection. (a) Urticarial rash; (b) Pityriasis rosea‐like eruption; (c) Varicelliform rash; (d and e) Maculopapular rash; (f) Pernio‐like lesions; (g) Extensor surface rash involving the knees; (h) Flexor surface rash involving the antecubital fossa
In accordance with other COVID‐19 dermatologic registries, the most common skin manifestations were urticaria and maculopapular eruptions. 2 We highlight an unusually high number of cases with varicella‐like eruptions, flexural rash similar to the one presented in symmetrical drug‐related intertriginous and flexural exanthema (SDRIFE), extensor surface rash, alopecia, and enanthem. Around 1.6% of patients with COVID‐19, skin manifestations may present with vesiculobullous lesions reminiscent of chickenpox. 1 Flexural or extensor surface rash in COVID‐19 patients has been rarely reported previously but seems more prevalent in our series compared to other registries. 3 , 4 Enanthem and alopecia (including telogen effluvium and alopecia areata) have been increasingly associated with COVID‐19 as reflected in our results. 1 , 5 The specific alopecia type was not specified in our survey and warrants further study. Interestingly, pernio‐like lesions were uncommon in our study, reaching only 6.7%. Other registries have reported a much higher prevalence. 1 Age and anatomical site of involvement were similar to previous reports with more subjects. 2
Considering the lack of racial and ethnic diversity in COVID‐19 dermatology registries, this study may increase awareness of the most common skin manifestations in Hispanic populations from North America. Limitations to our study include the ratio of cases with unspecified diagnostic test, lack of temporality, and skin symptom datum. A subanalysis of skin manifestations by region morphology or temporality morphology surpasses the objective of this short report.
Acknowledgments
The authors thank Ana Isabel Alvarez, Anayantzin Cruz Victor, Blanca Carlos Ortega, Cynthia Guadalupe Gonzalez Villalobos, Diana Carolina Perez Salinas, Josefina Navarrete Solis, Laura Ramos Gomez, Lilia Rizo Topete, Liza Aymes Garcia, Mercedes Fernandez Reyes, Orieta Herbas Rocha, Pilar Hernandez Elizondo, Rocio de la Rosa, Shelley Ashley Rodriguez, Veronica Ramirez Cisneros, Carlos Cruz Palacios, Daniel Asz Sigall, Dario Martinez Villarreal, Ismael Cheng Flores, Francisco Lozano Lee, Juan Carlos Garcia Rodriguez, Mario Amaya Guerra, Vicente Sustaita Villagomez, Maria Isabel Lemus Gómez, and Gabriel Gojon Zorrilla for contributing with cases for the study.
Conflict of interest: None.
Funding source: None.
References
- 1. Bandhala Rajan M, Kumar MP, Bhardwaj A. The trend of cutaneous lesions during COVID‐19 pandemic: lessons from a meta‐analysis and systematic review. Int J Dermatol 2020; 59: 1358–1370. [DOI] [PubMed] [Google Scholar]
- 2. Freeman EE, McMahon DE, Lipoff JB, et al. The spectrum of COVID‐19‐associated dermatologic manifestations: an international registry of 716 patients from 31 countries. J Am Acad Dermatol 2020; 83: 1118–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wollina U, Karadağ AS, Rowland‐Payne C, et al. Cutaneous signs in COVID‐19 patients: a review. Dermatol Ther 2020; 33: e13549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Potekaev NN, Zhukova OV, Protsenko DN, et al. Clinical characteristics of dermatologic manifestations of COVID‐19 infection: case series of 15 patients, review of literature, and proposed etiological classification. Int J Dermatol 2020; 59: 1000–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rizzetto G, Diotallevi F, Campanati A, et al. Telogen effluvium related to post severe Sars‐Cov‐2 infection: clinical aspects and our management experience. Dermatol Ther. 2020; 34: e14547. [DOI] [PMC free article] [PubMed] [Google Scholar]


