Abstract
Several studies have demonstrated an association between individual zinc status and viral respiratory infections; however, evidence regarding COVID‐19 is still missing or insufficient. This study aimed to evaluate the correlation between the prevalence of zinc deficiency and COVID‐19 cases and deaths per million population in the Asian and European countries. The COVID‐19 data from two different time points, that is, May 30 and June 30, 2020 for the Asian population and May 15 and June 15, 2020 for the European population, were analyzed to determine the correlation with the estimated zinc deficiency for these two continents. The prevalence of zinc deficiency was about two times higher in the Asian population (mean 17.5%) than in the European population (mean 8.9%). A significant positive correlation (p < .05) was observed between the prevalence of zinc deficiency and COVID‐19 cases at both time periods for the Asian population. However, the correlation between zinc deficiency prevalence and COVID‐19 deaths was not significant in the Asian population. In contrast, a significant but negative correlation (p < .05 for all cases) was observed for zinc deficiency with both COVID‐19 cases and deaths per million population at both time periods in the European countries. Considering the direct antiviral properties of zinc, it can be suggested that zinc supplementation may be beneficial for most of the population, especially older people and those who are at risk of COVID‐19 infections. In conclusion, there is not enough evidence on the association between individual zinc status and COVID‐19 infections and mortality. Therefore, cohort studies and randomized controlled trials are required to test this hypothesis.
Keywords: COVID‐19, infections, deaths, population, zinc
1. INTRODUCTION
COVID‐19 pandemic is one of the greatest health burdens in the world. Physicians and health workers are struggling in reducing the severity and mortality of COVID‐19. 1 Across the globe, extensive research efforts are underway to identify specific treatment strategies. However, a reasonable time is required to develop a specific vaccine with its effective application against COVID‐19. Therefore, a cost‐effective, easily available, and safe option with little to no side effects and simple applications of therapeutic options are desperately needed. Zinc is an important trace element being involved in numerous biological processes due to its role as a cofactor, signaling molecule, and structural component. 2 Moreover, zinc exhibits potent immunoregulatory and antiviral properties. Several studies have demonstrated its importance in the development and functions of the immune system of all kinds of species. 3 , 4
Zinc deficiency is associated with altered numbers and impaired functions of all immune cells, and individuals with a suboptimal zinc status have an increased risk for infectious and autoimmune diseases. 4 , 5 Mild zinc deficiency is largely considered as subclinical and often unnoticed in a majority of people. However, according to the assumption of the World Health Organization (WHO), about one‐third of the global population is affected by zinc deficiency. 6 The fact that zinc deficiency is related to about 16% of all respiratory diseases worldwide 6 provides a hint of a possible link between zinc deficiency and the risk of infections and progression of the severity of COVID‐19 and suggests beneficial effects of zinc supplementation. 7
Previous studies have demonstrated that low zinc status is associated with the prevalence of respiratory tract infections in both children and adults. 2 , 8 The high prevalence of zinc deficiency with its impact on public health is considered as an important global health issue. 9 Moreover, certain groups of the population, especially children, preterm ones, and the elderly, are at higher risk of zinc deficiency and its adverse outcomes. 10 Although the antiviral properties of zinc have been investigated in different viral infections including hepatitis C virus, human immunodeficiency virus (HIV), and coronavirus, 11 the potential role of zinc in SARS‐CoV‐2 has not been well investigated yet. A recent study in India has reported zinc deficiency among a significant number of COVID‐19 patients. 12 Moreover, patients with zinc deficiency developed more health complications, and this deficiency was associated with extended hospital stay and deaths. 12 However, it remains unclear whether zinc deficiency is directly related to COVID‐19 infections and deaths, thereby requiring further investigations. This study aimed to evaluate the correlation between the prevalence of zinc deficiency and COVID‐19 incidence (cases) and adverse outcomes (deaths) in the Asian and European population.
2. METHODS
The data for COVID‐19 cases and deaths per one million populations were collected for 45 Asian countries at two different time points (May 30, 2020, most countries at peak, and June 30, 2020, most countries after peak) using data from the coronavirus pandemic data portal https://www.worldometers.info/coronavirus/. Similarly, COVID‐19 cases and deaths per million population were collected for 39 European countries at two different time points (May 15, 2020, most countries at peak, and June 15, 2020, most countries after peak) using data from this pandemic data portal. 13 Zinc deficiency can be defined either as insufficient zinc to meet the needs of the body or as the zinc level in serum below the normal range. In the present study, the zinc deficiency estimate data for different countries based on the Food and Agriculture Organization's (FAO's) food balance datasheet and the prevalence of stunting in the countries were obtained from the previous estimate reported by Wessells and Brown 14 and data from the global prevalence of zinc deficiency 2005 (https://ourworldindata.org/grapher/global-prevalence-of-zinc-deficiency?time=2005). Pearson's correlation coefficient test (two‐tailed) was used to determine the correlation of zinc deficiency with COVID‐19 cases and deaths per million population in the Asian and European countries.
3. RESULTS
The prevalence of zinc deficiency was about two times higher in the Asian population (mean, 17.5%) than in the European population (mean, 8.9%). The number of COVID‐19 cases and deaths per million populations varied from one country to another country at both periods. A significant positive correlation (p < .05) between the prevalence of zinc deficiency estimate for the Asian countries and COVID‐19 cases per million population was consistently observed at two time points analyzed, covering infection peak time (May 30, 2020) and post‐infection peak time (June 30, 2020) (Table 1 and Figure 1). However, the correlation between the prevalence of zinc deficiency and COVID‐19 deaths per million populations in the Asian countries was not significant at any time point (Table 1 and Figure 1). However, a significant but negative correlation (p < .05 at least for all cases) was observed between the prevalence of zinc deficiency estimate for the European countries and COVID‐19 cases and deaths per million population at both time points analyzed, covering infection peak time (May 15, 2020) and post‐infection peak time (June 15, 2020) (Table 2 and Figure 2).
Table 1.
The number of COVID‐19 cases and deaths per million population at two different time periods in 45 Asian countries
| May 30, 2020 | June 30, 2020 | ||||
|---|---|---|---|---|---|
| Countries | Zinc deficiency (%) | Cases/1 M Pop. | Deaths/1 M Pop. | Cases/1 M Pop. | Deaths/1 M Pop. |
| Afghanistan | 20.2 | 373.3 | 6.4 | 809.9 | 19.2 |
| Armenia | 16.3 | 3012.6 | 42.9 | 8619.7 | 149.5 |
| Azerbaijan | 22.4 | 517.4 | 6.0 | 1728.5 | 21.0 |
| Bahrain | 24.8 | 6828.1 | 10.0 | 15,738.4 | 51.2 |
| Bangladesh | 29.7 | 270.9 | 3.7 | 883.5 | 11.2 |
| Bhutan | 31.7 | 42.8 | 0.0 | 99.8 | 0.0 |
| Brunei | 10.6 | 322.3 | 2.3 | 322.3 | 6.9 |
| Cambodia | 16.4 | 7.5 | 0.0 | 8.4 | 0.0 |
| China | 7.5 | 57.7 | 3.2 | 58.0 | 3.2 |
| Cyprus | 6.1 | 781.1 | 14.1 | 826.7 | 15.7 |
| Georgia | 23.6 | 189.8 | 3.0 | 232.6 | 3.8 |
| India | 31.2 | 131.8 | 3.8 | 424.5 | 12.6 |
| Indonesia | 31.2 | 94.2 | 5.8 | 206.2 | 10.5 |
| Iran | 23.2 | 1773.6 | 92.1 | 2710.9 | 128.8 |
| Iraq | 13.1 | 153.7 | 4.8 | 1172.7 | 48.3 |
| Israel | 5.5 | 1849.6 | 30.9 | 2744.6 | 34.8 |
| Japan | 16.4 | 132.9 | 7.0 | 147.0 | 7.7 |
| Jordan | 16.3 | 71.9 | 0.9 | 111.0 | 0.9 |
| Kazakhstan | 4.9 | 553.0 | 2.0 | 1162.2 | 10.0 |
| Kuwait | 15.4 | 6134.3 | 48.0 | 10,819.1 | 82.9 |
| Kyrgyzstan | 6 | 264.0 | 2.5 | 811.9 | 8.7 |
| Laos | 14.8 | 2.6 | 0.0 | 2.6 | 0.0 |
| Lebanon | 14.3 | 174.5 | 3.8 | 260.5 | 5.0 |
| Malaysia | 11.3 | 239.9 | 3.6 | 267.0 | 3.7 |
| Maldives | 14.4 | 3094.0 | 9.3 | 4368.9 | 16.7 |
| Mongolia | 4.1 | 54.6 | 0.0 | 67.1 | 0.0 |
| Myanmar | 19.5 | 4.1 | 0.1 | 5.5 | 0.1 |
| Nepal | 23.7 | 48.1 | 0.2 | 465.7 | 1.0 |
| Oman | 21.2 | 2042.0 | 8.2 | 7850.4 | 34.5 |
| Pakistan | 20.4 | 300.9 | 6.3 | 948.0 | 19.5 |
| Philippines | 9.9 | 157.2 | 8.7 | 342.4 | 11.6 |
| Qatar | 33.4 | 19,681.6 | 12.8 | 34,221.7 | 40.2 |
| South Korea | 13 | 223.2 | 5.2 | 249.7 | 5.5 |
| Saudi Arabia | 19.2 | 2395.6 | 13.8 | 5482.4 | 47.4 |
| Singapore | 15.4 | 5874.6 | 3.9 | 7505.6 | 4.4 |
| Syria | 15.2 | 7.0 | 0.2 | 15.9 | 0.5 |
| Taiwan | 21.7 | 18.6 | 0.3 | 18.8 | 0.3 |
| Tajikistan | 18.9 | 399.3 | 4.9 | 618.8 | 5.5 |
| Thailand | 20.4 | 44.1 | 0.8 | 45.4 | 0.8 |
| Timor‐Leste | 16.9 | 18.2 | 0.0 | 18.2 | 0.0 |
| Turkey | 21.7 | 1736.7 | 48.1 | 2132.5 | 57.2 |
| UAE | 20.8 | 3427.6 | 26.5 | 4921.3 | 31.9 |
| Uzbekistan | 8.8 | 106.0 | 0.4 | 254.1 | 0.8 |
| Vietnam | 10.7 | 3.4 | 0.0 | 3.6 | 0.0 |
| Yemen | 23.4 | 10.4 | 2.6 | 38.8 | 10.5 |
| Average | 17.5 ± 7.5 | 1413.9 ± 3261.9 | 10.0 ± 17.4 | 2661.0 ± 5886.2 | 20.5 ± 32.0 |
| Correlation (r) | .306 | .081 | .328 | .133 | |
| p value | .041 | .595 | .028 | .384 | |
Note: Pearson's correlation coefficient test (two‐tailed) was applied to determine the correlation of zinc deficiency with COVID‐19 cases and deaths per one million population.
Source: Global prevalence of zinc deficiency 2005 (https://ourworldindata.org/grapher/global-prevalence-of-zinc-deficiency?time=2005), and COVID‐19 cases and deaths from worldwide COVID‐19 pandemic data portal at https://www.worldometers.info/coronavirus/.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Figure 1.
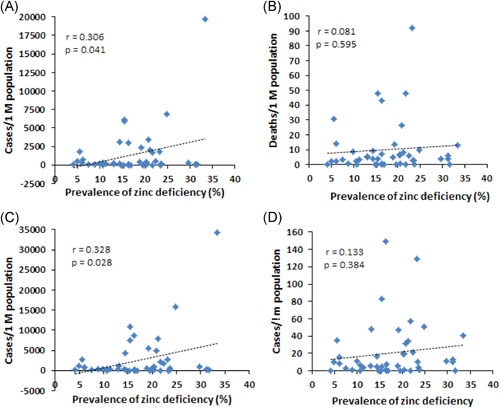
Correlation between zinc deficiency and the number of COVID‐19 cases and deaths/1 M population in 45 Asian countries. Source: Global prevalence of zinc deficiency 2005 (https://ourworldindata.org/grapher/global-prevalence-of-zinc-deficiency?time=2005), and COVID‐19 cases and mortality as of May 30, 2020 (A and B) and June 30, 2020 (C and D) from worldwide COVID‐19 pandemic data portal at https://www.worldometers.info/coronavirus/
Table 2.
The number of COVID‐19 cases and deaths per million population at two different time periods in 39 European countries
| May 15, 2020 | June 15, 2020 | ||||
|---|---|---|---|---|---|
| Countries | Zinc deficiency (%) | Cases/1 M Pop. | Deaths/1 M Pop. | Cases/1 M Pop. | Deaths/1 M Pop. |
| Albania | 5.3 | 318.3 | 10.8 | 552.5 | 12.5 |
| Austria | 7.3 | 1788.7 | 69.7 | 1902.6 | 75.3 |
| Belarus | 9 | 2934.6 | 16.5 | 5786.6 | 33.0 |
| Belgium | 6.8 | 4715.1 | 773.0 | 5185.8 | 833.6 |
| Bosnia and Herzegovina | 16.7 | 681.5 | 39.0 | 926.3 | 50.0 |
| Bulgaria | 15.3 | 307.7 | 14.7 | 480.8 | 25.3 |
| Croatia | 12.4 | 541.2 | 23.1 | 549.0 | 26.1 |
| Czechia | 11 | 784.4 | 27.5 | 939.8 | 30.8 |
| Denmark | 6.2 | 1863.1 | 92.7 | 2109.3 | 103.2 |
| Estonia | 10.5 | 1331.3 | 47.5 | 1488.1 | 52.0 |
| Finland | 4.6 | 1124.1 | 52.9 | 1282.9 | 58.8 |
| France | 3.9 | 2174.3 | 421.8 | 2411.0 | 451.0 |
| Germany | 9 | 2097.1 | 95.5 | 2244.4 | 106.0 |
| Greece | 7.2 | 269.6 | 15.4 | 300.7 | 17.7 |
| Hungary | 8.4 | 353.7 | 45.8 | 421.9 | 58.3 |
| Iceland | 3.1 | 5281.0 | 29.3 | 5304.4 | 29.3 |
| Ireland | 4 | 4852.2 | 307.5 | 5128.6 | 345.5 |
| Italy | 5.8 | 3702.4 | 521.8 | 3924.4 | 567.5 |
| Latvia | 11.6 | 514.3 | 10.1 | 581.6 | 14.8 |
| Lithuania | 7.5 | 563.5 | 19.8 | 651.3 | 27.9 |
| Malta | 8.1 | 1204.9 | 13.6 | 1472.1 | 20.4 |
| Moldova | 20 | 1424.1 | 50.1 | 2944.7 | 101.9 |
| Montenegro | 7.5 | 515.9 | 14.3 | 519.1 | 14.3 |
| Netherlands | 5 | 2549.3 | 329.3 | 2856.7 | 354.0 |
| North Macedonia | 14.1 | 835.2 | 46.6 | 1995.3 | 92.6 |
| Norway | 6.2 | 1516.2 | 42.8 | 1595.1 | 44.6 |
| Poland | 10.3 | 476.0 | 24.0 | 787.1 | 33.2 |
| Portugal | 6.3 | 2803.1 | 116.7 | 3632.1 | 149.1 |
| Romania | 7.5 | 854.4 | 55.6 | 1152.1 | 74.2 |
| Russia | 8.3 | 1801.1 | 16.6 | 3681.2 | 48.6 |
| Serbia | 7 | 1194.6 | 25.8 | 1415.4 | 29.2 |
| Slovakia | 16.3 | 271.1 | 4.9 | 284.3 | 5.1 |
| Slovenia | 9.8 | 704.7 | 49.5 | 719.6 | 52.4 |
| Spain | 5.4 | 5868.2 | 581.6 | 6228.0 | 605.3 |
| Sweden | 6.1 | 3015.0 | 385.2 | 5261.3 | 507.9 |
| Switzerland | 4.9 | 3526.0 | 217.0 | 3597.3 | 224.1 |
| UK | 4.6 | 3487.0 | 500.8 | 4373.1 | 614.8 |
| Ukraine | 11.4 | 396.3 | 10.9 | 727.3 | 20.6 |
| Turkey | 21.7 | 1736.7 | 48.1 | 2132.5 | 57.2 |
| Average | 8.9 ± 4.4 | 1804.6 ± 1528.3 | 132.5 ± 193.0 | 2224.8 ± 1782.8 | 153.0 ± 212.1 |
| Correlation (r) | −.484 | −.414 | −.383 | −.396 | |
| p value | .002 | .009 | .016 | .013 | |
Note: Pearson's correlation coefficient test (two‐tailed) was applied to determine the correlation of zinc deficiency with COVID‐19 cases and deaths per one million population.
Source: Global prevalence of zinc deficiency 2005 (https://ourworldindata.org/grapher/global-prevalence-of-zinc-deficiency?time=2005), and COVID‐19 cases and deaths from worldwide COVID‐19 pandemic data portal at https://www.worldometers.info/coronavirus/.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Figure 2.
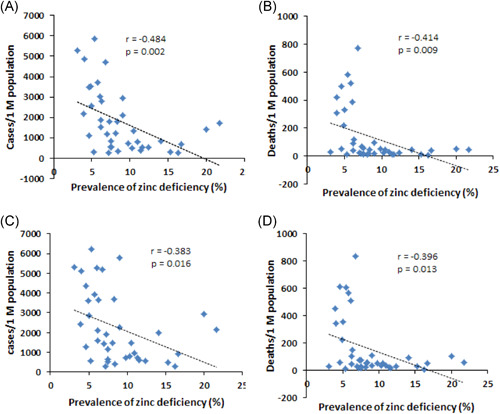
Correlation between zinc deficiency and the number of COVID‐19 cases and deaths/1 M population in 39 European countries. Source: Global prevalence of zinc deficiency 2005 (https://ourworldindata.org/grapher/global-prevalence-of-zinc-deficiency?time=2005), and COVID‐19 cases and mortality as of May 15, 2020 (A and B) and June 15, 2020 (C and D) from worldwide COVID‐19 pandemic data portal at https://www.worldometers.info/coronavirus/
4. DISCUSSION
This study showed a significant positive correlation between zinc deficiency prevalence and COVID‐19 cases per million population in Asian countries. However, the correlation between zinc deficiency and COVID‐19 deaths was not significant for the Asian population. In contrast, a significant but negative correlation was observed for zinc deficiency prevalence with both COVID‐19 cases and deaths in the European population. At present, it is not clear whether the correlation between zinc deficiency and COVID‐19 cases and deaths is causal or an epiphenomenon. Moreover, the negative correlation of zinc deficiency prevalence with COVID‐19 impact in terms of cases and deaths raises the question whether individual zinc status plays a positive role in preventing COVID‐19. Other potential factors could affect the correlation of zinc with COVID‐19 infections and mortality.
It is important to mention that the prevalence of zinc deficiency was about twofold higher in Asian countries than in European countries. In the European and North American countries, zinc deficiency prevalence is lower as compared with other parts of the world. 14 , 15 Rather, there exist possibilities of adequate zinc intake from diet and supplements. 16 , 17 Countries with less variation in diet, lower animal protein intake, and high ingestion of phytate (impairs zinc absorption) through diet may tend to have increased zinc deficiency levels. From our analysis, it seems that the spectrum of zinc deficiency is an important factor that may influence its correlation with COVID‐19 infections and deaths. The lower prevalence of zinc deficiency and the high COVID‐19 cases and mortality rates in most of the European countries might be a reason for the negative correlation in this continent. The underlying differences in the population composition, sex, age distribution, comorbidities, and variation in drugs used in the treatment may be possible confounding factors that could also affect the correlation. It has been demonstrated that pre‐existing medical conditions including diabetes, hypertension, chronic liver, and kidney diseases can worsen the COVID‐19 disease. 18 , 19 , 20 , 21 , 22 Therefore, the subject's history of pre‐existing diseases should also be considered during such correlations analysis.
A prospective observational study conducted in India between May 17 and May 27, 2020 reported a significant (p < .001) low level of zinc in COVID‐19 patients (74.5 mg/dl) when compared with healthy controls (105.8 mg/dl). 12 Among COVID‐19 patients, 57.4% of the subjects were zinc‐deficient. The authors observed that COVID‐19 patients with a low zinc status developed more health complications, and zinc deficiency was related to the prolonged hospitalization and increased deaths. 12 However, that study was a single‐center analysis with a small number of COVID‐19 patients (n = 47). 12 Therefore, multicenter studies including both symptomatic and asymptomatic COVID‐19 patients with no comorbid conditions would be worthwhile in evaluating the role of zinc in preventing COVID‐19.
In vitro studies reveal that the spike protein of SARS‐CoV‐2 directly interacts with the host cell surface ACE2 (angiotensin‐converting enzyme 2) and the cellular protease TMPRSS2 (transmembrane protease serine 2), permitting its entry and replication. 23 Recent studies suggested that a lower zinc level favors the interaction of ACE2 with the viral spike protein, whereas a high level of zinc inhibits the expression of ACE2, resulting in a decreased viral interaction with its receptor. 24 , 25
Zinc has been shown to exhibit antiviral effects by inhibition of RNA synthesis, DNA polymerase, viral application, and reverse transcriptase. 26 , 27 , 28 Several studies have demonstrated the direct antiviral effects of zinc against viruses such as herpes simplex virus, papillomavirus, picornavirus, respiratory syncytial virus, hepatitis C virus, and HIV reviewed by Wessels et al. 7 It has been suggested that zinc can prevent fusion with the host cell membrane, reduce the viral polymerase activity, impair the protein translation process, block releasing viral particles, and destabilize the viral envelope. 27 , 29 However, the evidence is limited regarding the effects of zinc on SARS‐CoV‐2. More research on the zinc effect on SARS‐CoV‐2 is highly required.
Zinc plays an important role in immune system development and serves as an immunomodulator. 7 Zinc deficiency is associated with underdevelopment of lymphoid tissue and decreased NK cell (natural killer cell) function, which causes poor innate immune responses. 30 Zinc deficiency is also associated with decreased cytokine production and macrophage activation. Zinc plays a significant role in B‐ and T‐cell function. 30 Moreover, zinc deficiency is associated with increased levels of proinflammatory molecules, higher levels of reactive oxygen species (ROS), and predisposing for rapid progression of some inflammatory diseases, especially those impairing lung functions, and can be reversible with zinc supplementation. 7 Several studies suggested that prophylactic zinc supplementation can be an effective approach than therapeutic proceedings. 31 , 32 It has been shown that zinc administration can reduce symptom severity and duration of the common cold. 33 , 34 , 35 A recent review highlighted the potential benefits of zinc supplementation for COVID‐19 severity. 7 The authors indicated that zinc supplementation can help to preserve antiviral immunity and support antioxidative effects, thus reducing lung injury and minimizing secondary infections. 7 Older people and those who are at risk of COVID‐19 infections would be benefited most from zinc supplementation. It has also been hypothesized that zinc supplementation might be beneficial for prophylaxis and treatment of COVID‐19. 36
There are some limitations to the present study. First, the retrospective design of the study used the global prevalence of zinc deficiency data as reported in 2005. At present, the zinc status at the population level in both continents may be improved or changed that could affect such correlation level. Second, the extracted data are heterogeneous, that is, the sample has not been drawn from a single population but rather from a mixture. Third, the potential confounding variables like, age, sex, ethnicity, and pre‐existing diseases were not included in the analysis, which could affect the correlation between zinc and the risk of COVID‐19 infections. Therefore, these confounding variables should be considered during the evaluation of the role of zinc in respiratory diseases including COVID‐19. Overall, it remains unclear whether the observed relationship is coincidental or causal, which can be revealed by further research only. Extensive research is needed before using zinc as a therapeutic option for COVID‐19.
5. CONCLUSION
This retrospective study shows a positive correlation between the high prevalence of zinc deficiency and the COVID‐19 cases per million population in Asian countries. Although zinc supplementation has been suggested as beneficial against respiratory tract infections, it is not clear yet whether its supplementation after hospital admission can reduce the severity of COVID‐19. To date, little information exists on the relationship between zinc levels and COVID‐19 infections and mortality. Therefore, multicenter cohort studies and randomized clinical trials are needed to test this hypothesis.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Conceptualization: Nurshad Ali. Data acquisition and analysis: Khandaker A. Fariha, Farjana Islam, Nayan C. Mohanto, Iftekhar Ahmad. Drafting of the manuscript: Nurshad Ali. Critical review of the manuscript: Nurshad Ali, Mohammad J. Hosen, Shamim Ahmed. Statistical analysis: Nurshad Ali, Farjana Islam, Nayan C. Mohanto. Supervision: Nurshad Ali.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/jmv.26932
Ali N, Fariha KA, Islam F, et al. Assessment of the role of zinc in the prevention of COVID‐19 infections and mortality: a retrospective study in the Asian and European population. J Med Virol. 2021;93:4326‐4333. 10.1002/jmv.26932
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Ali N. Elevated level of C‐reactive protein may be an early marker to predict risk for severity of COVID‐19. J Med Virol. 2020;92(11):2409‐2411. 10.1002/jmv.26097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Skalny AV, Rink L, Ajsuvakova OP, et al. Zinc and respiratory tract infections: perspectives for COVID‐19. Int J Mol Med. 2020;46(1):17‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wessels I, Maywald M, Rink L. Zinc as a gatekeeper of immune function. Nutrients. 2017;9(12):1286. 10.3390/nu9121286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Roohani N, Hurrell R, Kelishadi R, Schulin R. Zinc and its importance for human health: an integrative review. J Res Med Sci. 2013;18(2):144. [PMC free article] [PubMed] [Google Scholar]
- 5. Wessels I, Rink L. Micronutrients in autoimmune diseases: possible therapeutic benefits of zinc and vitamin D. J Nutr Biochem. 2020;77:108240. 10.1016/j.jnutbio.2019.108240 [DOI] [PubMed] [Google Scholar]
- 6. WHO . The World Health report 2002. Midwifery. 2003;19:72‐73. 10.1054/midw.2002.0343 [DOI] [PubMed] [Google Scholar]
- 7. Wessels I, Rolles B, Rink L. The potential impact of zinc supplementation on COVID‐19 pathogenesis. Front Immunol. 2020;11:1712. 10.3389/fimmu.2020.01712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Walker CLF, Rudan I, Liu L, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381(9875):1405‐1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bailey RL, West Jr, KP , Black RE. The epidemiology of global micronutrient deficiencies. Ann Nutr Metab. 2015;66(suppl 2):22‐33. [DOI] [PubMed] [Google Scholar]
- 10. Yasuda H, Tsutsui T. Infants and elderlies are susceptible to zinc deficiency. Sci Rep. 2016;6:21850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Barocas JA, So‐Armah K, Cheng DM, et al. Zinc deficiency and advanced liver fibrosis among HIV and hepatitis C co‐infected anti‐retroviral naïve persons with alcohol use in Russia. PLOS One. 2019;14(6):e0218852. 10.1371/journal.pone.0218852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jothimani D, Kailasam E, Danielraj S, et al. COVID‐19: poor outcomes in patients with zinc deficiency. Int J Infect Dis. 2020;100:343‐349. 10.1016/j.ijid.2020.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Coronavirus pandemic data portal . https://www.worldometers.info/coronavirus/. Accessed June 3, 2020.
- 14. Wessells KR, Brown KH. Estimating the global prevalence of zinc deficiency: results based on zinc availability in national food supplies and the prevalence of stunting. PLOS One. 2012;7(11):e50568. 10.1371/journal.pone.0050568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hess SY. National risk of zinc deficiency as estimated by national surveys. Food Nutr Bull. 2017;38(1):3‐17. [DOI] [PubMed] [Google Scholar]
- 16. European Food Safety Authority . Tolerable upper intake levels for vitamins and minerals; 2006. http://www.efsa.europa.eu/en/ndatopics/docs/ndatolerableuil.pdf. Accessed May 30, 2020.
- 17. National Institute of Health Office of Dietary Supplements . Zinc: Fact sheet for health professionals; 2020. https://ods.od.nih.gov/factsheets/Zinc-HealthProfessional/. Accessed May 27, 2020.
- 18. Ali N. Is SARS‐CoV‐2 associated with liver dysfunction in COVID‐19 patients? Clin Res Hepatol Gastroenterol. 2020;44(4):e84‐e86. 10.1016/j.clinre.2020.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ali N. Relationship between COVID‐19 infection and liver injury: a review of recent data. Front Med (Lausanne). 2020;7:458. 10.3389/fmed.2020.00458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ali N, Hossain K. Liver injury in severe COVID‐19 infection: current insights and challenges. Expert Rev Gastroenterol Hepatol. 2020;14(10):879‐884. 10.1080/17474124.2020.1794812 [DOI] [PubMed] [Google Scholar]
- 21. Ali N, Mahmood S. Kidney injury in COVID‐19: an emerging concern to the clinician. SN Compr Clin Med. 2020:1808‐1809. 10.1007/s42399-020-00482-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Khan MMA, Khan MN, Mustagir MG, Rana J, Islam MS, Kabir MI. Effects of underlying morbidities on the occurrence of deaths in COVID‐19 patients: a systematic review and meta‐analysis. J Glob Health. 2020;10(2):020503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hoffmann M, Kleine‐Weber H, Krüger N, Müller M, Drosten C, Pöhlmann S. The novel coronavirus 2019 (2019‐NCoV) uses the SARS‐coronavirus receptor ACE2 and the cellular protease TMPRSS2 for entry into target cells. Mol Biol. 2020. 10.1101/2020.01.31.929042 [DOI] [Google Scholar]
- 24. Devaux CA, Rolain J‐M, Raoult D. ACE2 receptor polymorphism: susceptibility to SARS‐CoV‐2, hypertension, multi‐organ failure, and COVID‐19 disease outcome. J Microbiol Immunol Infect. 2020;53(3):425‐435. 10.1016/j.jmii.2020.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Li M‐Y, Li L, Zhang Y, Wang X‐S. Expression of the SARS‐CoV‐2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020;9(1):45. 10.1186/s40249-020-00662-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ko Y‐L, Morihara D, Shibata K, et al. Factors attenuating zinc deficiency improvement in direct‐acting antiviral agent‐treated chronic hepatitis C virus infection. Nutrients. 2018;10(11):1620. 10.3390/nu10111620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Read SA, Obeid S, Ahlenstiel C, Ahlenstiel G. The role of zinc in antiviral immunity. Adv Nutr. 2019;10(4):696‐710. 10.1093/advances/nmz013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Xue J, Moyer A, Peng B, Wu J, Hannafon BN, Ding W‐Q. Chloroquine is a zinc ionophore. PLOS One. 2014;9(10):e109180. 10.1371/journal.pone.0109180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Suara RO, Crowe JE. Effect of zinc salts on respiratory syncytial virus replication. Antimicrob Agents Chemother. 2004;48(3):783‐790. 10.1128/AAC.48.3.783-790.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shankar AH, Prasad AS. Zinc and immune function: the biological basis of altered resistance to infection. Am J Clin Nutr. 1998;68(2):447S‐463S. 10.1093/ajcn/68.2.447S [DOI] [PubMed] [Google Scholar]
- 31. Meydani SN, Barnett JB, Dallal GE, et al. Serum zinc and pneumonia in nursing home elderly. Am J Clin Nutr. 2007;86(4):1167‐1173. 10.1093/ajcn/86.4.1167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Roth DE, Richard SA, Black RE. Zinc supplementation for the prevention of acute lower respiratory infection in children in developing countries: meta‐analysis and meta‐regression of randomized trials. Int J Epidemiol. 2010;39(3):795‐808. 10.1093/ije/dyp391 [DOI] [PubMed] [Google Scholar]
- 33. Eby GA, Davis DR, Halcomb WW. Reduction in duration of common colds by zinc gluconate lozenges in a double‐blind study. Antimicrob Agents Chemother. 1984;25(1):20‐24. 10.1128/AAC.25.1.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hemilä H. Zinc lozenges and the common cold: a meta‐analysis comparing zinc acetate and zinc gluconate, and the role of zinc dosage. JRSM Open. 2017;8(5):205427041769429. 10.1177/2054270417694291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hulisz D. Efficacy of zinc against common cold viruses: an overview. J Am Pharm Assoc. 2004;44(5):594‐603. 10.1331/1544-3191.44.5.594.Hulisz [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kumar A, Kubota Y, Chernov M, Kasuya H. Potential role of zinc supplementation in prophylaxis and treatment of COVID‐19. Med Hypotheses. 2020;144:109848. 10.1016/j.mehy.2020.109848 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


