Abstract
To quantify the impact of the COVID‐19 pandemic and public health interventions on parent and child mental health and family relationships, we examined change in individual and family functioning in a sample of parents enrolled in a prevention trial; we examined change before the pandemic (2017–2019) when children were an average of 7 years old to the first months after the imposition of widespread public health interventions in the United States (2020) with paired t tests and HLM models. We examined moderation by parent gender, education, family income, and coparenting conflict. We found large deteriorations from before the pandemic to the first months of the pandemic in child internalizing and externalizing problems and parent depression, and a moderate decline in coparenting quality. Smaller changes were found for parent anxiety and parenting quality. Mothers and families with lower levels of income were at particular risk for deterioration in well‐being. Results indicate a need for widespread family support and intervention to prevent potential family “scarring,” that is, prolonged, intertwined individual mental health and family relationship problems.
Keywords: Covid‐19, Family Relationships, Mental Health
Resumen
Para cuantificar el efecto de la pandemia de la COVID‐19 y de las intervenciones de salud pública en la salud mental de los padres y los niños y en las relaciones familiares, analizamos los cambios en el funcionamiento individual y familiar en una muestra de padres inscriptos en un ensayo de prevención; estudiamos el cambio antes de la pandemia (2017‐2019) cuando los niños tenían un promedio de 7 años hasta los primeros meses después de la imposición de las intervenciones generalizadas de salud pública en los Estados Unidos (2020) con pruebas t apareadas y modelos lineales jerárquicos. Analizamos la moderación por género, educación, ingresos familiares y conflicto de cocrianza de los padres. Hallamos grandes deterioros desde antes de la pandemia hasta los primeros meses de la pandemia en problemas de interiorización y exteriorización de los niños y depresión de los padres, y una disminución moderada de la calidad de la cocrianza. También encontramos cambios más pequeños en la ansiedad de los padres y la calidad de la crianza. Las madres y las familias con niveles más bajos de ingresos estuvieron en riesgo particular de deterioro del bienestar. Los resultados indican la necesidad de apoyo familiar generalizado y de intervenciones para prevenir posibles «secuelas» familiares, p. ej.: salud mental individual interconectada y prolongada y problemas en las relaciones familiares.
摘要
本文把COVID‐19和公共健康干预措施对父母和儿童的心理健康以及对家庭关系的影响进行量化,对参加一项预防试验的人群样本进行了研究,主要关于这些受试父母的个体功能和家庭功能产生了哪些变化; 我们采用配对t检验和HLM模型,研究了新冠肺炎(2017‐2019年)前的变化,即平均年龄为7岁的儿童至美国实施广泛公共健康干预措施(2020年)后的第一个月。我们通过父母性别、教育程度、家庭收入和养育子女的冲突来考察这些因素的调适作用。我们发现,儿童对很多问题以及父母的抑郁表现都进行内化和外化,从新冠肺炎流行发生前到新冠大流行的头几个月出现了严重恶化倾向,亲子教育的质量略有下降。父母的焦虑和培养孩子方面的质量也有较小的变化。收入水平较低的母亲和家庭的福祉尤其有恶化的风险。结果表明,需要给予广泛的家庭支持和干预,以防止潜在的家庭"伤疤",即长期错综搅合在一起的个人心理健康和家庭关系问题。
Although anecdotal reports and cross‐sectional surveys suggest that the COVID‐19 pandemic and public health interventions such as shelter‐in‐place orders have had a detrimental impact on the mental health of adults around the world (Alzueta et al., 2020), as well as on the well‐being of parents and children specifically (Cameron et al., 2020; de Miranda, da Silva Athanasio, de Sena Oliveira, & Silva, 2020; Patrick et al., 2020; Spinelli, Lionetti, Pastore, & Fasolo, 2020; Yeasmin et al., 2020). However, the magnitude of this impact remains unknown. In the past, economic crises have led to increased parent stress, mental health problems, and interparental conflict, leading to increased harsh and abusive parenting (Conger & Elder, 1994; Schneider, Waldfogel, & Brooks‐Gunn, 2017). In addition to work and financial disruptions, during the COVID‐19 pandemic, families have experienced enormous stress due to seclusion within households, social isolation, concern about the health of family and friends, disruptions to school and child care, and the need to make new health‐related decisions in a context of uncertainty.
Understanding the impact of the pandemic on these outcomes is critical for developing resources and interventions for families during and after the pandemic. Although cross‐sectional surveys point to significant declines in mental health and family relationships, studies comparing well‐being before and during the pandemic period have yielded mixed results. One study in the UK assessed adult mental distress two years before and again during the pandemic, finding a substantial increase in overall distress (Pierce et al., 2020). However, the questionnaire used was a brief, 12‐item screening measure assessing general mental distress, with items covering a range of topics such as anxiety, depression, self‐confidence, concentration, and social dysfunction. Psychometric analyses of the measure have yielded different sets of factor structures across studies. Thus, the degree of deterioration in mental health per se, and in particular dimensions of mental health, remains uncertain. Another study examined change in couples’ relationship functioning from shortly before to shortly after the onset of the pandemic, finding no change in relationship satisfaction or causal attributions, and small changes in responsibility attributions (Williamson, 2020). Two studies have compared the responses of one sample of adolescent respondents before the pandemic to a similar but different sample during the pandemic: In one study, adolescents during the pandemic reported lower levels of reported depression and loneliness, but higher levels of unhappiness and dissatisfaction with life, compared to other adolescents before the pandemic (Twenge, Coyne, Carroll, & Wilcox, 2020). In the second study, pregnant/parenting Latina adolescents reported somewhat better well‐being during the pandemic compared to counterparts from the same high schools before the pandemic (Astle et al., Under review).
Although intriguing in terms of potential adolescents’ response to the pandemic, this evidence may not bear on the experience of younger children who are more emotionally dependent on parents and require more daily adult supervision and guidance. We hypothesize that the pandemic‐related stressors experienced by parents mentioned above, along with increased emotional needs among children, have had negative implications for mental health and family relationships (Figure 1). Accordingly, we examine change in parent and child mental/behavioral health and family relationships in a single sample of families with children approximately 8‐ to 10‐year‐old. Leveraging existing research with a longitudinal sample, we assess the magnitude of change in well‐being from before the pandemic to the initial months of the pandemic.
Figure 1.
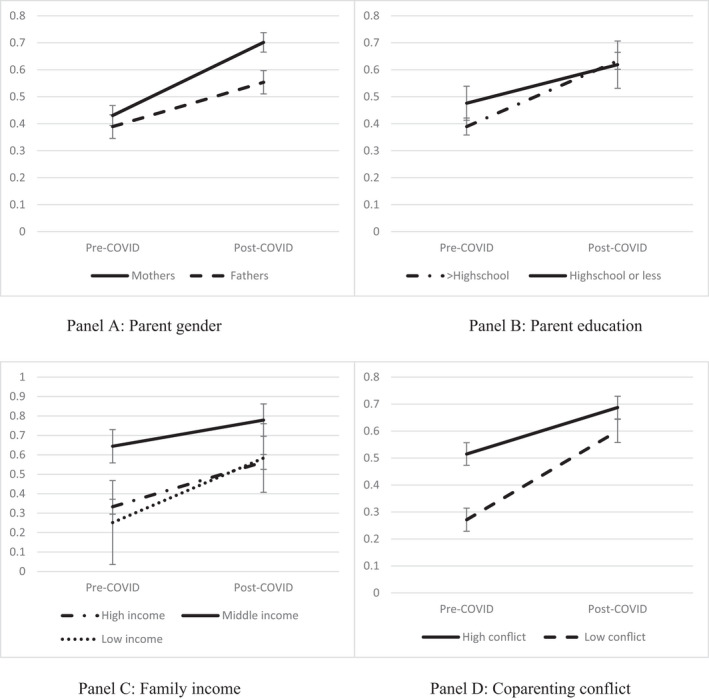
Change in Parent Depression as Moderated by Parent Gender (a), Education (b), Family Income (c), and Coparenting Conflict (d)
Finally, to understand which families are at greatest risk for declines in well‐being and thus where resources should be targeted, we examine whether several factors moderate the impact of the pandemic on family member and family well‐being. One key family factor we examine as a moderator of change in well‐being is the coparenting relationship—that is, parents’ ability to resolve disagreements, support each other in the parenting role, and coordinate family efforts in sustaining health protective behaviors are conceptualized as core dimensions of the coparenting relationship (Feinberg, 2003). Researchers have viewed coparenting as distinct from other interparental relationship dimensions such as romantic, sexual, companion‐like, legal, and financial relations. Prior research indicates that a mutually supportive coparenting relationship is a critical factor supporting parents’ own adjustment and mental health, and consequently parenting quality and children’s well‐being across diverse families and structures (Feinberg, 2003). Given the importance of coparenting quality for family functioning, we examine whether pre‐pandemic levels of coparenting conflict influence (moderate) the degree of deterioration of mental and behavioral health and family relationships.
We also assess whether decline in well‐being varies by pre‐pandemic levels of parent education or income—factors that may influence both the degree of pandemic‐related disruption (e.g., in work, housing, and health care) and families’ abilities to cope with these stressors. Although low parent education/income is linked to lower levels of family member well‐being in general, it is unclear how these risk factors would predict change in well‐being during a high‐stress period such as the pandemic. It is possible that well‐being among those with elevated levels of risk may already be so low that additional pandemic‐related stressors have little additional influence. It may also be possible that pandemic‐related stress is sufficiently severe such that it swamps the impact of pre‐existing risk factors, leading to generally similar, low levels of well‐being during the pandemic regardless of pre‐existing risk. We hypothesize, however, that both pre‐existing and pandemic‐period risk factors will be salient, and that lower parent education/income and higher pre‐pandemic coparenting conflict will exacerbate the negative impacts of the pandemic (i.e., leading to relatively greater declines in well‐being).
Methods
Participants in the current study were recruited primarily from central Pennsylvania, as well as Delaware and Texas, between 2008 and 2012 for a randomized trial of Family Foundations, a transition to parenthood prevention program (Feinberg et al., 2016, 2019; Feinberg, Roettger, Jones, Paul, & Kan, 2015; Jones et al., 2018). Parents were eligible for the trial if they were at least 18 years of age and resided together. 399 primiparous mother and father dyads enrolled; after four waves of data were collected between pregnancy and 4 years postpartum, 384 parents from 208 families participated in a final wave of pre‐pandemic data (2017–2020). In April and May 2020, we offered participants an opportunity to complete an online questionnaire regarding adjustment during the pandemic. Respondents to this online questionnaire included 122 mothers and 84 fathers from 129 families with an average 2.3 children (SD = 1.0; range = 1–5). The oldest child in each family (45.6% female) was an average of 9.9 years (SD = 1.0); mothers and fathers were 39.5 (SD = 4.4) and 41.2 years (SD = 4.7), respectively. Parents completed an average of 15.9 years of education (SD = 1.3). 95% of participants reported they continued to live with the partner with whom they enrolled in the study originally. Reflecting the original recruitment area, 94.7% of parents were non‐Hispanic white; thus, generalizations from this data should be made with caution. No significant differences were found in attrition from Time 1 (the last wave of data collected before the pandemic) to Time 2 (pandemic) by intervention condition, education, income, or race/ethnicity.
Measures
Depressive symptoms
Parents reported how often they had felt depressive symptoms during the last week using 20 items from the CES‐D Scale (Radloff, 1977). Example items include, “feel depressed” and “not feel like eating; your appetite was poor.” Each item was scored from 0 (rarely or none of the time; less than once a week) to 3 (most or all of the time; 5–7 days a week). Of 20 items, 4 items such as “Feel hopeful” and “Feel happy” were reverse coded so that higher scores indicate greater depressive symptoms. Given the repeated measures, we calculated reliability across time using appropriate methods (Hox, Moerbeek, & Van de Schoot, 2017), yielding a reliability estimate of 0.93. Based on the cutoff score of 16 (Weissman, Sholomskas, Pottenger, Prusoff, & Locke, 1977), 28 (13.6%) and 70 (34%) parents scored in the clinical range of depression before and during the pandemic, respectively.
Anxiety
Parents reported the inability to control worry during the past two weeks using four items from the Penn State Worry Questionnaire (Beck, Stanley, & Zebb, 1995). Parental worry items include “My worries overwhelm me” and “I worry all the time.” Each item was scored from 1 (not at all) to 5 (very typical), and the average score of these four items was constructed (reliability = 0.86).
Coparenting relationship quality
Parents reported the overall coparenting relationship quality over the past month using 14 items (reliability = 0.97) drawn from the Coparenting Relationship Scale (Feinberg, Brown, & Kan, 2012). Coparenting relationship items include “My partner and I have the same goals for our child” and “My partner makes me feel like I’m best possible parent for our child.” Each item was scored from 0 (not true) to 6 (very true). Seven items were reverse coded and higher scores indicate better coparenting. We created a subscale of coparenting conflict using two items (r = .58) at the pre‐pandemic wave for use as a moderator.
Externalizing and internalizing behavior problems
Parents reported on children’s externalizing and internalizing behavior problems during the past month using seven (reliability = 0.77) and six items (reliability = 0.72), respectively, from the Strengths and Difficulties Questionnaire (Goodman, Meltzer, & Bailey, 1998). An example of an externalizing behavior and internalizing problem item is “often loses his/her temper” and “is often unhappy, depressed or tearful,” respectively. The response scale of each item was ranged from 0 (not true) to 2 (certainly true). We also created binary variables representing clinically elevated levels of Externalizing and of Internalizing based on U.S. norms (Bourdon, Goodman, Rae, Simpson, & Koretz, 2005). The clinical range (i.e., upper 90% of the normative distribution) was coded as 1; scores below the clinical cutoff were coded as 0. Before the pandemic, the number of children in the clinical range was 25 (12.1%) and 11 (5.3%) for Externalizing and Internalizing, respectively. During the pandemic, those figures rose to 34 (16.5%) and 25 (12.1%).
Parenting quality
Parents reported on positive parenting behaviors toward children using three items from the Parental Behavior Inventory (Schaefer, 1965). Items include “I spoke to my oldest child in a warm and friendly voice” and “I tell or show my oldest child that I like him/her just the way he/she is.” Each item was scored from 1 (almost never) to 5 (almost always). The three items yielded a good internal consistency (reliability = 0.78).
Household income and education
We inquired about total pretax household income in the past year by providing 23 ranges from “$4,999 or less” to “over $150,000” and median annual household income was $112,500 (SD = 39,679; range = $12,500–$162,500). For analysis, we reclassified income intervals into five categories: (1) $34,999 or less, (2) $35,000–$49,999, (3) $50,000–$74,999, (4) $75,000–$99,999, and (5) $100,000 or more and used contrast coding by assigning the value of −2, −1, 0, 1, and 2, respectively, to the five groups. Education was asked as the “highest grade of school or year of college completed” and participants could select from 17 categories ranging from “Grade 1” to “5 or more years” of college. Education was contrast coded for analysis with individuals reporting 12 or fewer years of education coded as −1 and individuals with 13 or more years coded as 1.
Statistical Analysis
We examined disruption due to the pandemic in individual and family adjustment using hierarchical linear modeling (HLM), which included three levels: time, individual, and family. These models allowed us to examine changes across time while accounting for the dependencies in the data (i.e., persons nested in families) and potential covariates (intervention condition and parent gender). Models for continuous outcomes were fit using restricted maximum likelihood, the Satterthwaite degrees of freedom method, and allowed families and individuals to vary in their intercepts (SAS proc mixed). Models for the binary variables measuring clinical levels of parent depression, externalizing, and internalizing were fit using a binary distribution and a log link (SAS proc genmod). Time (pre‐pandemic = 0, pandemic = 1), parent gender (mothers = 0, fathers = 1) and intervention condition (control = 0, intervention = 1), and the parent gender by time interaction were included in all models. We assessed whether to include the time interval between assessments by examining correlations between time interval and absolute change in individual and family functioning. Results demonstrated that differences observed in most of the outcome variables between pre‐pandemic and pandemic waves were not significantly correlated with time interval (rs = −.10 to .07). The exception was externalizing behaviors where the correlation was significant but small (r = −.20, p = .05). Results of analyses for externalizing behaviors controlling for time interval were not different than when time interval was not included; therefore, we present the models without time interval as a control variable.
Moderators were tested in separate models. Categorical moderators (education and income) were contrast coded such that main effects of these variables represented the difference between the reference group and the other level (or levels) of the variable on the intercept. Moderation was tested as the interaction between the categorical variable and time which represented the difference in time slopes between the reference group and other levels of the variable. As a continuous moderator, coparenting conflict was grand mean centered to aid in interpretation.
Values for graphing are adjusted means obtained using estimate commands in SAS proc mixed to account for covariates and main effects of moderators. For coparenting conflict, higher and lower conflict were defined as one standard deviation above and below the sample mean, respectively. Cohen’s d quantified degree of change in continuous outcomes using the model‐estimated amount of change over time divided by the square root of the estimated within‐person variance (which served as an estimate of the corrected within‐person standard deviation). Odds ratios were estimated to capture change in likelihood of reporting clinically meaningful levels of parent depression, as well as externalizing and internalizing child behavior problems.
Results
Descriptive statistics for analytic variables are included in Table 1.
Table 1.
Descriptive Statistics and Correlations
| Time 1 | Time 2 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | M (SD) | A | B | C | D | E | M (SD) | |
| A Parent | ||||||||||||||
| Depression | 0.41 (0.34) | 0.64 (0.44) | ||||||||||||
| B Parent | ||||||||||||||
| Worry | .50 | 1.67 (0.87) | .66 | 1.83 (1.04) | ||||||||||
| C Coparent | ||||||||||||||
| Relation Q. | −.53 | −.32 | 5.23 (0.73) | −.35 | −.24 | 4.99 (0.84) | ||||||||
| D Child | ||||||||||||||
| Internalizing | .21 | .18 | −.20 | 1.38 (0.31) | .33 | .32 | −.23 | 1.39 (0.36) | ||||||
| E Child | ||||||||||||||
| Externalizing | .33 | .22 | −.33 | .35 | 1.62 (0.36) | .20 | .15 | −.32 | .34 | 1.63 (0.42) | ||||
| F Parenting | ||||||||||||||
| Quality | −.31 | −.07 | .21 | −.13 | −.39 | 4.37 (0.53) | −.25 | −.13 | .29 | −.23 | −.34 | 4.26 (0.62) | ||
| G Coparent | ||||||||||||||
| Conflict | .36 | .22 | −.58 | .08 | .14 | −.15 | 0.51 (0.76) | |||||||
| H Parent | ||||||||||||||
| Education | −.25 | −.01 | .23 | .04 | −.15 | .15 | −.06 | 15.84 (1.68) | ||||||
Bolded font indicates significant at p < .05.
HLM models simultaneously tested change across time while accounting for parent gender, intervention condition, and the gender by time interaction (where appropriate). Results indicated that all measures demonstrated significant change toward worse individual and family well‐being from pre‐pandemic to the pandemic (Table 2). Effect sizes indicated large changes for parent Depression (d = 0.82), child Externalizing (d = 1.59), and Internalizing problems (d = 1.31). Smaller but substantial changes were observed for parent Anxiety (d = 0.25), Coparenting quality (d = −0.40), and Parenting Quality (d = −0.24).
Table 2.
Results of Models Assessing Change and Moderation of Change
| Depression | Worry | |||||
|---|---|---|---|---|---|---|
| Estimate (SE) | p | 95% CI | Estimate (S.E.) | p | 95% CI | |
| Intercept | 0.41 (0.04) | <.001 | 0.33, 0.50 | 1.95 (0.1) | <.001 | 1.76, 2.15 |
| Change over time | 0.27 (0.04) | <.001 | 0.20, 0.34 | 0.16 (0.08) | .044 | 0.005, 0.32 |
| Parent gender | −0.04 (0.05) | .443 | −0.15, 0.06 | −0.6 (0.13) | <.001 | −0.85, −0.34 |
| Condition | 0.03 (0.05) | .515 | −0.07, 0.14 | −0.09 (0.12) | .481 | −0.32, 0.15 |
| Gender × time | −0.11 (0.06) | .060 | −0.22, 0.005 | −0.03 (0.12) | .818 | −0.27, 0.21 |
| Coparenting quality | Parenting quality | |||||
|---|---|---|---|---|---|---|
| Estimate (SE) | p | 95% CI | Estimate (SE) | p | 95% CI | |
| Intercept | 5.10 (0.09) | <.001 | 4.92, 5.29 | 4.51 (0.06) | <.001 | 4.39, 4.63 |
| Change over time | −0.23 (0.06) | <.001 | −0.35, −0.11 | −0.10 (0.05) | .054 | −0.20, 0.002 |
| Parent gender | 0.11 (0.09) | .223 | −0.07, 0.28 | −0.17 (0.08) | .027 | −0.32, −0.02 |
| Condition | −0.04 (0.13) | .729 | −0.3, 0.21 | −0.23 (0.08) | .003 | −0.39, −0.08 |
| Gender × time | 0.12 (0.1) | .227 | −0.07, 0.30 | 0.02 (0.08) | .847 | −0.14, 0.17 |
| Internalizing | Externalizing | |||||
|---|---|---|---|---|---|---|
| Estimate (SE) | p | 95% CI | Estimate (SE) | p | 95% CI | |
| Intercept | 0.11 (0.03) | .002 | 0.04, 0.17 | 0.23 (0.04) | <.001 | 0.14, 0.31 |
| Change over time | 0.28 (0.03) | <.001 | 0.23, 0.34 | 0.36 (0.03) | <.001 | 0.29, 0.42 |
| Parent gender | −0.002 (0.03) | .956 | −0.07, 0.07 | 0.03 (0.04) | .489 | −0.05, 0.11 |
| Condition | 0.05 (0.04) | .309 | −0.04, 0.13 | 0.02 (0.06) | .683 | −0.09, 0.14 |
| Gender × time | −0.05 (0.04) | .265 | −0.13, 0.04 | 0.06 (0.05) | .211 | −0.04, 0.16 |
“Change over time” refers to change from pre‐pandemic to the first months of the pandemic.
The large effect size for parent Depression was confirmed examining those parents with clinically meaningful levels of Depression. Parents were 2.4 times (95% CI: 1.70–3.40) more likely to report high levels of Depression during the pandemic compared to pre‐pandemic levels. The large effect sizes for change in child behavior problems are consistent with results from our analysis of change in the proportion of children rated in the clinical problem range: Parents were 2.5 times (95% CI: 1.61–4.02) and 4.0 times (95% CI: 2.14–7.49) more likely to report clinical levels of Externalizing problems and Internalizing problems, respectively, during the pandemic compared to pre‐pandemic levels.
We then tested parent gender and parent pre‐pandemic reports of income, education, and Coparenting Conflict as moderators of change in separate HLM models to determine whether specific subgroups were more or less impacted by the onset of the pandemic (full results available from the first author). Significant interaction effects for Depression are depicted in Figure 1. We found that parent Depression was significantly modulated by three moderators: Depression increased more for parents with more vs. fewer years of education, for lower‐income vs. higher‐income parents, and for lower vs. higher levels of Coparenting Conflict. For education and Coparenting Conflict, parents at lower risk before the pandemic demonstrated lower levels of pre‐pandemic Depression. Thus, although less educated and higher Coparenting Conflict parents did experience increases in Depression with the onset of the pandemic, their elevated levels of Depression before the pandemic may have limited the size of increases in Depression with the onset of the pandemic. There was also a trend toward a significant gender by time interaction (p = .06). Mothers, relative to fathers, reported somewhat larger increases in Depression.
In the only other significant moderation result (Figure 2), pre‐pandemic income moderated change in Parenting Quality. Plots indicated that middle‐income parents reported that their Parenting Quality declined substantially more than was reported by lower‐ and upper‐income parents.
Figure 2.
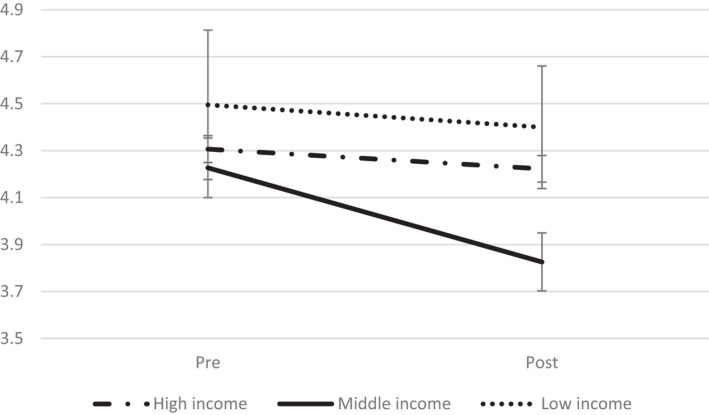
Change in Parenting Quality Moderated by Family Income
Discussion
This is the first study of which we are aware that examined the magnitude of change in parent, child, and family mental health and adjustment from before to the pandemic period. By examining within‐individual change, our approach overcomes major methodological weaknesses in other reports that have examined cross‐sectional survey data (Alzueta et al., 2020), compared different sets of respondents before and after the pandemic (Twenge et al., 2020), or utilized a non‐specific measure of mental distress (Pierce et al., 2020). Our results provide evidence of a large deterioration in parent and child mental and behavioral health during the first months of the pandemic.
The magnitude of increases in parent depression and children’s internalizing and externalizing problems from before the pandemic was striking. Changes of this magnitude are rarely seen in developmental and family studies. It is instructive to note that the magnitude of change in parent depression that we found in this study (d = 0.87) is over twice as much as the average effect size of common anti‐depressants (0.38) (Leucht, Helfer, Gartlehner, & Davis, 2015). Although comparisons across measures and samples are fraught, this comparison indicates that the clinical implications of the pandemic on parent depression were severe. In terms of clinical relevance, parents were 2.4 times more likely to score in the clinical range on depression during the pandemic compared to before. The effect sizes for increases in children’s internalizing and externalizing problems are even larger than that for depression; and the proportion of children rated in the clinical range increased by 2.5 and four times in internalizing and externalizing problems, respectively, from pre‐pandemic levels.
Our results are consistent with impressions of elevated parent and child stress and mental health difficulties experienced during the pandemic derived from recent cross‐sectional research (Brown, Doom, Lechuga‐Peña, Watamura, & Koppels, 2020; Cameron et al., 2020; Spinelli et al., 2020; Yeasmin et al., 2020). However, these results for families with children in middle‐childhood stand in contrast to findings of two studies of adolescents that suggest the possibility of better adjustment during the pandemic compared to before the pandemic (Astle et al., Under review; Twenge et al., 2020). Although it is possible that adolescents may have experienced some improvements in mental health and well‐being during the pandemic not experienced by younger children and their parents, we point out that the results in one study were mixed, and the respondents in the other study reflected a fairly small, circumscribed subset of adolescents (pregnant/parenting Latinx adolescents).
In comparison with these large increases in parent depression and child adjustment, we found that overall deterioration in parent anxiety and the quality of family relationships (coparenting and parenting quality) were smaller but nonetheless substantial. In future longitudinal analyses with several more waves of data collected from this sample across the pandemic, we will examine whether deteriorations in family relationships triggered changes in parent and child adjustment, or the reverse.
We found evidence that three factors significantly moderated the increase in parent depression. Our findings for two of these factors were consistent: Parents with lower levels of risk before the pandemic—as defined by higher levels of education or lower levels of coparenting conflict—reported relatively greater increases in depression during the pandemic. These lower‐risk parents, as one might expect, had lower levels of depression before the pandemic relative to higher‐risk parents. Thus, whereas both lower‐ and higher‐risk parents experienced increases in depression with the pandemic, the increases for lower‐risk parents were larger and brought their levels of depression closer to the levels reported by higher‐risk parents. In this case, the acute stress of the pandemic partly or wholly “swamped” the effect of pre‐existing risk (i.e., lower education or higher coparenting conflict) on depression. Although in many ways the pandemic has highlighted disparities in health and vulnerability in our population, in this sample at least, the pandemic may have reduced disparities in parent depression.
Apart from parent depression, we found only one case of significant moderation—family income qualified the degree of decline in parenting quality. The plot of this interaction indicates that middle‐income parents reported the lowest levels of parenting quality before the pandemic, and also reported the largest decreases in parenting quality with the pandemic. A speculative interpretation of these income moderation findings is that, at least in this sample, middle‐income parents may have experienced high levels of stress and consequently depression before the pandemic due to a parenting style in which they feel compelled to invest considerable time, energy, and financial resources to promote children’s well‐being through numerous enrichment activities and high levels of parent involvement (Vincent & Ball, 2007). These middle‐income parents, who do not have the financial resources of wealthy parents that allow one to hire others to perform household or childcare duties, may expend considerable internal resources in maintaining positive, supportive parenting toward their child despite their own elevated levels of stress. With the additional strains brought on by the pandemic, these middle‐income parents’ ability to self‐regulate and maintain positive parenting in the face of their already higher levels of depression may have been most compromised.
With regard to the pandemic itself, we suggest that future research examine the implications of deterioration in parent and child psychological well‐being for physical health, especially regarding susceptibility to COVID‐19. There are two pathways through which mental health and family relationship problems may affect susceptibility to the virus. In order to provide guidance for future investigations, we depict these pathways in a conceptual model (Figure 3), including the pathways representing the impact of the pandemic on mental health and family relationships reported on in this paper. First, mental health problems and family conflict may compromise parents’ abilities to implement and sustain family member protective health actions recommended by public health authorities (such as social distancing, seclusion in households, hand‐washing, and mask‐wearing (Feinberg et al., Under review). As there is considerable variation in opinions about and deployment of protective health behaviors in the United States (Gollwitzer et al., 2020; Simonov, Sacher, Dubé, & Biswas, 2020), it is likely that many parents do not completely agree with each other about the necessity of such practices. Evidence in other contexts indicates that monitoring and guiding children’s behavior are compromised when parents are unable to resolve coparenting conflict (Feinberg, 2003). In addition to influencing exposure to the virus, psychosocial stress, depression, and interpersonal conflict may increase susceptibility to infection and the severity of the resulting illness upon exposure. Evidence indicates that stress, depression, and conflict reduce the healthy immune response to virus infections—likely mediated by dysregulation of inflammatory responses to virus exposure (Cohen, 2020). This pathway is of particular note given that recent research has documented the influence of immune functioning and “cytokine storms” on severity of the COVID‐19 illness (Ragab, Eldin, Taeimah, Khattab, & Salem, 2020).
Figure 3.
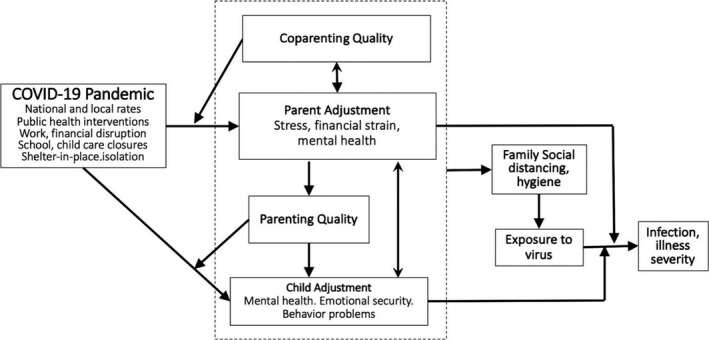
Illustration of Pathways from Pandemic Stressors to Family Functioning to Infection/Disease Severity
A major limitation of this study is that the longitudinal sample was not representative of the U.S. population. The sample was predominantly white, whereas the pandemic has had more severe impacts on Latinx, Native American, and African‐American populations (Abedi et al., 2020; Tai, Shah, Doubeni, Sia, & Wieland, 2020). Although there was a wide range of income and we found moderation of change in well‐being by income, median income was at the 69th percentile of the U.S. distribution—toward the higher end of the middle‐income range spanning from the 30th to 81st percentiles (Kochhar, 2018). 95% of respondents were in two‐parent families (the focus of the original study was on couples at the transition to parenthood), and these results are not generalizable to single‐parent families. An additional limitation of this study is that we examined change across time, but we were unable to compare change in these families to a sample of families who did not experience the pandemic. However, there is little evidence that mental health and the quality of family relationships deteriorate to a substantial degree over the period of family development (in terms of the age of the oldest child) examined here. With the data presented in this report, we are unable to assess whether family member adjustment recovered in the following months of the pandemic; this is a question we plan to investigate in the future. Finally, our measure of child adjustment was reported on by parents, and thus may be subject to reporter bias; however, most measures of child adjustment in the literature are based on the report of an informant (e.g., teacher or parent vs. direct observation or archival records of school suspensions or arrests). Increasing the reliability typically requires triangulation across informants; but with schools and activities operating remotely during the time when the data were collected, there were no other informants capable of rating child adjustment across families.
Implications
These results indicate a need for widespread family intervention to reduce parent and child mental health and behavior problems during crises such as the current pandemic (Fontanesi et al., 2020). One intervention strategy would be to promote individual and family resilience before a crisis period. For example, recent findings from a randomized trial suggest that a universal, couple‐focused, preventive intervention at the transition to parenthood resulted in better parent, child, and family well‐being during the pandemic, 10 years after program implementation (Feinberg, Under review; Feinberg, Jones, Roettger, Solmeyer, & Hostetler, 2014). A second strategy would be to provide support to families after the onset of a crisis. Such intervention should promote better coping skills, mood management, family relationship quality, and accessing of social support. An efficient strategy for supporting families in a period of acute stress would focus on positive coparenting (Feinberg, 2002)—that is, parents’ mutual support and childrearing coordination. Empirical and experimental evidence demonstrates that coparenting quality plays a critical role in supporting parent mental health, positive parenting quality (Prime, Wade, & Browne, 2020), and children’s adjustment (Feinberg & Jones, 2018; Figure 1). An evaluation of a coparenting‐focused, telehealth intervention delivered in Australia during the pandemic suggests that this approach is acceptable to and beneficial for parents and families (Giallo, Seymour, & Feinberg, Under review).
Conclusion
Based on our findings of large negative impacts of the pandemic on parent and child well‐being, we believe it is important to consider the possibility of these negative impacts persisting after the pandemic. This is analogous to the possibility raised by economists that severe disruption in businesses and financial markets might “scar” the economy that make it hard for recovery to take hold. We suggest that similar scarring may take place within families; after a decline in inter‐related factors such as parent mental health, child adjustment, coparenting, and parenting quality, initial increases in well‐being in one area may be undermined by persisting problems in another. For example, research suggests that parent depression and coparenting quality are in particular reciprocally linked (Feinberg, 2003; Tissot, Favez, Frascarolo, & Despland, 2016), and indeed these two factors were substantially linked (r’s = .39–.58) in our data. The inter‐relatedness of depression and coparenting creates the potential for a vicious cycle of increasing depression leading to coparenting conflict leading to more severe depression. If one parent began to experience reduced depression after the pandemic, it is possible that a dynamic of coparenting conflict would persist and undermine such gains. Likewise, the alleviation of child‐related stressors (e.g., opening of schools and extracurricular activities) may not lead to improved coparenting quality if one or both parents remain depressed and parenting quality remains compromised.
As ongoing, intertwined family conflict and mental health problems are difficult to interrupt (Harold & Sellers, 2018; Parry, Davies, Sturge‐Apple, & Coe, 2020), a “scarring” phenomenon could lead to entrenched, long‐term psychological and family relationship difficulties. Assisting families in recovering from the pandemic period may require multi‐component, inter‐disciplinary approaches by schools, counselors, mental health clinicians, pediatricians, family service agencies, faith‐based congregations, and youth‐serving recreational and athletic organizations. Thus, it will be important to follow families’ as the pandemic and screen for persistence of disruptions in parent and child well‐being.
This research was supported by a grant from the National Institute of Child Health and Development (NICHD; HD058529), Mark Feinberg, Principal Investigator. Data collection during the pandemic was supported by a grant from The Huck Institutes of the Life Sciences, Pennsylvania State University.
References
- Abedi, V. , Olulana, O. , Avula, V. , Chaudhary, D. , Khan, A. , Shahjouei, S. et al. (2020). Racial, economic, and health inequality and COVID‐19 infection in the United States. Journal of Racial and Ethnic Health Disparities, 1–11. 10.1007/s40615-020-00833-4. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzueta, E. , Perrin, P. , Baker, F. C. , Caffarra, S. , Ramos‐Usuga, D. , Yuksel, D. et al. (2020). How the COVID‐19 pandemic has changed our lives: A study of psychological correlates across 59 countries. Journal of Clinical Psychology, 77, 556–570. 10.1002/jclp.23082. [DOI] [PubMed] [Google Scholar]
- Astle, S. , Duncan, J. C. , Toews, M. , McAllister, P. , Maddy, M. , Perez‐Brena, N. et al. (Under review). “A Little Bit Closer”: A mixed method analysis of the effect of the covid‐19 pandemic on the lives of adolescent parents. [Google Scholar]
- Beck, J. G. , Stanley, M. A. , & Zebb, B. J. (1995). Psychometric properties of the Penn State Worry Questionnaire. Journal of Clinical Geropsychology, 1, 33–42. [Google Scholar]
- Bourdon, K. H. , Goodman, R. , Rae, D. S. , Simpson, G. , & Koretz, D. S. (2005). The Strengths and Difficulties Questionnaire: US normative data and psychometric properties. Journal of the American Academy of Child & Adolescent Psychiatry, 44, 557–564. 10.1097/01.chi.0000159157.57075.c8. [DOI] [PubMed] [Google Scholar]
- Brown, S. M. , Doom, J. R. , Lechuga‐Peña, S. , Watamura, S. E. , & Koppels, T. (2020). Stress and parenting during the global COVID‐19 pandemic. PsyArXiv, 1–43. 10.31234/osf.io/ucezm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron, E. E. , Joyce, K. M. , Delaquis, C. P. , Reynolds, K. , Protudjer, J. L. P. , & Roos, L. E. (2020). Maternal psychological distress & mental health service use during the COVID‐19 pandemic. Journal of Affective Disorders, 276, 765–774. 10.1016/j.jad.2020.07.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. (2020). Psychosocial vulnerabilities to upper respiratory infectious illness: Implications for susceptibility to Coronavirus disease 2019 (COVID‐19). Perspectives on Psychological Science, 16, 161–174. 10.1177/1745691620942516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger, R. D. , & Elder, G. H. (1994). Families in troubles times: Adapting to change in rural America. Hawthorne, NY: Aldine de Gruyter. [Google Scholar]
- de Miranda, D. M. , da Silva Athanasio, B. , de Sena Oliveira, A. C. , & Silva, A. C. S. (2020). How is COVID‐19 pandemic impacting mental health of children and adolescents? International Journal of Disaster Risk Reduction, 51, 101845. 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg, M. E. (Under review). The effects of early family prevention on resilience during the COVID‐19 pandemic 10 years later. [Google Scholar]
- Feinberg, M. E. (2002). Coparenting and the transition to parenthood: A framework for prevention. Clinical Child & Family Psychology Review, 5, 173–195. 10.1023/A:1019695015110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg, M. E. (2003). The internal structure and ecological context of coparenting: A framework for research and intervention. Parenting: Science and Practice, 3, 95–132. 10.1207/S15327922PAR0302_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg, M. E. , Boring, J. , Le, Y. , Hostetler, M. L. , Karre, J. , Irvin, J. et al. (2019). Supporting military family resilience at the transition to parenthood: A randomized pilot trial of an online version of Family Foundations. Journal of Family Psychology, 69, 109–124. 10.1111/fare.12415. [DOI] [Google Scholar]
- Feinberg, M. E. , Brown, L. D. , & Kan, M. L. (2012). A multi‐domain self‐report measure of coparenting. Parenting: Science & Practice, 12, 1–21. 10.1080/15295192.2012.638870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg, M. E. , & Jones, D. E. (2018). Experimental support for a family systems approach to child development: Multiple mediators of intervention effects across the transition to parenthood. Couple & Family Psychology: Research & Practice, 7, 63–75. 10.1037/cfp0000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg, M. E. , Jones, D. E. , Hostetler, M. L. , Roettger, M. E. , Paul, I. M. , & Ehrenthal, D. B. (2016). Couple‐focused prevention at the transition to parenthood, a randomized trial: Effects on coparenting, parenting, family violence, and parent and child adjustment. Prevention Science, 17, 751–764. 10.1007/s11121-016-0674-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg, M. E. , Jones, D. E. , Roettger, M. E. , Solmeyer, A. , & Hostetler, M. L. (2014). Long‐term follow‐up of a randomized trial of family foundations: Effects on children’s emotional, behavioral, and school adjustment. Journal of Family Psychology, 28, 821–831. [DOI] [PubMed] [Google Scholar]
- Feinberg, M. E. , Mogle, J. , Lee, J. , Tornello, S. L. , Cifelli, J. A. , & Hostetler, M. L. (Under review). Social distancing, stress, and family conflict. [Google Scholar]
- Feinberg, M. E. , Roettger, M. E. , Jones, D. E. , Paul, I. , & Kan, M. L. (2015). Effects of a psychosocial couple‐based prevention program on adverse birth outcomes. Maternal & Child Health Journal, 19, 102–111. 10.1007/s10995-014-1500-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontanesi, L. , Marchetti, D. , Mazza, C. , Di Giandomenico, S. , Roma, P. , & Verrocchio, M. C. (2020). The effect of the COVID‐19 lockdown on parents: A call to adopt urgent measures. Psychological Trauma: Theory, Research, Practice, & Policy, 12(S1), S79–S81. 10.1037/tra0000672. [DOI] [PubMed] [Google Scholar]
- Giallo, R. , Seymour, M. , & Feinberg, M. E. (Under review). Supporting families during the pandemic via telehealth. [Google Scholar]
- Gollwitzer, A. , Martel, C. , Brady, W. J. , Pärnamets, P. , Freedman, I. G. , Knowles, E. D. et al. (2020). Partisan differences in physical distancing are linked to health outcomes during the COVID‐19 pandemic. Nature Human Behaviour, 4, 1186–1197. 10.1038/s41562-020-00977-7. [DOI] [PubMed] [Google Scholar]
- Goodman, R. , Meltzer, H. , & Bailey, V. (1998). The Strengths and Difficulties Questionnaire: A pilot study on the validity of the self‐report version. European Child & Adolescent Psychiatry, 7, 125–130. 10.1007/s007870050057. [DOI] [PubMed] [Google Scholar]
- Harold, G. T. , & Sellers, R. (2018). Annual research review: Interparental conflict and youth psychopathology: An evidence review and practice focused update. Journal of Child Psychology & Psychiatry, 59, 374–402. 10.1111/jcpp.12893. [DOI] [PubMed] [Google Scholar]
- Hox, J. J. , Moerbeek M., & Van de Schoot R. (Eds.) (2017). Multilevel analysis: Techniques and applications. New York: Routledge. [Google Scholar]
- Jones, D. E. , Feinberg, M. E. , Hostetler, M. L. , Roettger, M. E. , Paul, I. M. , & Ehrenthal, D. B. (2018). Family and child outcomes 2 years after a transition to parenthood intervention. Family Relations, 67, 270–286. 10.1111/fare.12309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochhar, R. (2018). The American middle class is stable in size, but losing ground financially to upper‐income families. Retrieved from https://www.pewresearch.org/fact‐tank/2018/09/06/the‐american‐middle‐class‐is‐stable‐in‐size‐but‐losing‐ground‐financially‐to‐upper‐income‐families/. [Google Scholar]
- Leucht, S. , Helfer, B. , Gartlehner, G. , & Davis, J. M. (2015). How effective are common medications: A perspective based on meta‐analyses of major drugs. BMC Medicine, 13, 1–5. 10.1186/s12916-015-0494-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry, L. Q. , Davies, P. T. , Sturge‐Apple, M. L. , & Coe, J. L. (2020). Coparental discord and children’s behavior problems: Children’s negative family representations as an explanatory mechanism. Journal of Family Psychology, 34, 523–533. 10.1037/fam0000638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick, S. W. , Henkhaus, L. E. , Zickafoose, J. S. , Lovell, K. , Halvorson, A. , Loch, S. et al. (2020). Well‐being of parents and children during the COVID‐19 pandemic: A national survey. Pediatrics, 146, e2020016824. 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- Pierce, M. , Hope, H. , Ford, T. , Hatch, S. , Hotopf, M. , John, A. et al. (2020). Mental health before and during the COVID‐19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 7, 883–892. 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime, H. , Wade, M. , & Browne, D. T. (2020). Risk and resilience in family well‐being during the COVID‐19 pandemic. American Psychologist, 75, 631–643. 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Radloff, L. S. (1977). The CES‐D scale: A self‐report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. 10.1177/014662167700100306. [DOI] [Google Scholar]
- Ragab, D. , Eldin, H. S. , Taeimah, M. , Khattab, R. , & Salem, R. (2020). The COVID‐19 cytokine storm; what we know so far. Frontiers in Immunology, 11, 1446. 10.3389/fimmu.2020.01446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer, E. S. (1965). Children's report of parental behaviour: An inventory. Child Development, 36, 413–424. 10.2307/1126465. [DOI] [PubMed] [Google Scholar]
- Schneider, W. , Waldfogel, J. , & Brooks‐Gunn, J. (2017). The great recession and risk for child abuse and neglect. Children & Youth Services Review, 72, 71–81. 10.1016/j.childyouth.2016.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonov, A. , Sacher, S. K. , Dubé, J.‐P.‐H. , & Biswas, S. (2020). The persuasive effect of fox news: Non‐compliance with social distancing during the covid‐19 pandemic (0898‐2937). Retrieved from National Bureau of Economic Research: https://www.nber.org/papers/w27237. [Google Scholar]
- Spinelli, M. , Lionetti, F. , Pastore, M. , & Fasolo, M. (2020). Parents' stress and children's psychological problems in families facing the COVID‐19 outbreak in Italy. Frontiers in Psychology, 11, 1713. 10.3389/fpsyg.2020.01713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai, D. B. G. , Shah, A. , Doubeni, C. A. , Sia, I. G. , & Wieland, M. L. (2020). The disproportionate impact of COVID‐19 on racial and ethnic minorities in the United States. Clinical Infectious Diseases, 72, 703–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tissot, H. , Favez, N. , Frascarolo, F. , & Despland, J.‐N. (2016). Coparenting behaviors as mediators between postpartum parental depressive symptoms and toddler’s symptoms. Frontiers in Psychology, 7, 1912. 10.3389/fpsyg.2016.01912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge, J. M. , Coyne, S. M. , Carroll, J. S. , & Wilcox, W. B. (2020). Teens in quarantine: Mental health, screen time, and family connection. Retrieved from The Wheatley Institution: https://ifstudies.org/ifs‐admin/resources/final‐teenquarantine2020.pdf. [Google Scholar]
- Vincent, C. , & Ball, S. J. (2007). Making up' the middle‐class child: Families, activities and class dispositions. Sociology, 41, 1061–1077. 10.1177/0038038507082315. [DOI] [Google Scholar]
- Weissman, M. M. , Sholomskas, D. , Pottenger, M. , Prusoff, B. A. , & Locke, B. Z. (1977). Assessing depressive symptoms in five psychiatric populations: A validation study. American Journal of Epidemiology, 106, 203–214. 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- Williamson, H. C. (2020). Early effects of the COVID‐19 pandemic on relationship satisfaction and attributions. Psychological Science, 31, 1479–1487. 10.1177/0956797620972688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeasmin, S. , Banik, R. , Hossain, S. , Hossain, M. N. , Mahumud, R. , Salma, N. et al. (2020). Impact of COVID‐19 pandemic on the mental health of children in Bangladesh: A cross‐sectional study. Children & Youth Services Review, 117, 105277. 10.1016/j.childyouth.2020.105277. [DOI] [PMC free article] [PubMed] [Google Scholar]


