Dear Editor,
A recent paper 1 suggested the absence of epidemiologic association between COVID‐19 and Guillain‐Barré syndrome (GBS). Previously, we had published the lack of national increase in GBS hospitalizations during Dengue 2 and Zika virus 3 outbreaks in Singapore. Using similar methodology, we asked if GBS hospitalizations have changed in 2020 during the COVID‐19 outbreak. All hospitalization episodes coded with discharge diagnosis of GBS (ICD‐10: G61.0) from January 2019 to October 2020 were extracted from the Singapore Ministry of Health's inpatient administrative database, taking into account patients who were recorded more than once because they were transferred from another hospital. COVID‐19 notification data were obtained from the Ministry's surveillance system on infectious diseases. Like Zika and Dengue, COVID‐19 is a legally notifiable disease under Singapore law. Association between monthly GBS hospitalization episodes and monthly number of COVID‐19 notifications was examined by calculating Spearman's correlation coefficient, after adjusting the time series data for stationarity. 57 985 COVID‐19 infections were notified from January 2020 to October 2020. Compared to 2019, there was a significant decrease in the number of GBS hospitalization (figure 1), from an average of 9 per month in 2019 to 4 per month in 2020 (P < .005). There was no association between GBS hospitalizations and COVID‐19 (Spearman's correlation coefficient = −.03). To date, we have had only one patient with probable COVID‐19‐related GBS, as defined by Ellul et al. 4 It was a case of acute motor sensory axonal neuropathy, diagnosed in a patient approximately 1 month after admission for critical COVID‐19 infection that required prolonged ventilation. 5 Spinal fluid SARSCoV2 real‐time polymerase chain reaction was negative.
FIGURE 1.
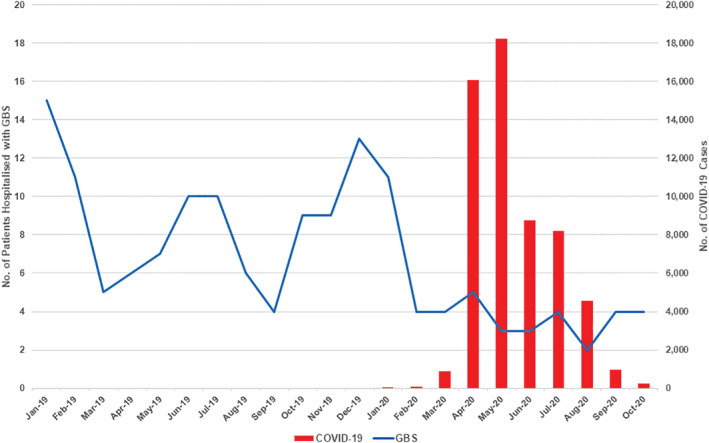
Number of Guillain‐Barré syndrome (GBS) hospitalizations and COVID‐19 notifications, January 2019 to October 2020
Our data suggest that COVID‐19 may not be a significant antecedent infection of GBS. The decrease in GBS hospitalizations may be partly related to mild cases not being hospitalized during the pandemic. A few Singapore hospitals also restricted non COVID‐19 admissions during the second and third quarter of 2020. However, these cases would likely have been admitted to other hospitals and therefore captured in the national data. Overall, we believe the period of national lockdown, the social and physical isolation, emphasis on hygiene measures and mandatory mask‐wearing were the main factors behind the general decrease in GBS cases.
AUTHOR CONTRIBUTIONS
Thirugnanam Umapathi: conceptualization and writing. Benjamin Er, Lily Chua, Jasmine Shimin Koh, Yi Hui Goh: data analysis and revision of draft.
Thirugnanam Umapathi and Benjamin Er contributed equally to the study as joint first authors.
Abstract based on this data has been submitted for presentation at the 2021 Peripheral Nerve Society Annual Meeting.
REFERENCES
- 1. Keddie S, Pakpoor J, Mousele C, et al. Epidemiological and cohort study finds no association between COVID‐19 and Guillain‐Barré syndrome. Brain. 2021;144(2):682–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Umapathi T, Lim CS, Ooi EE, et al. Asymptomatic dengue infection may trigger Guillain‐Barré syndrome. J Peripher Nerv Syst. 2016;21:375‐377. [DOI] [PubMed] [Google Scholar]
- 3. Umapathi T, Kam YW, Ohnmar O, et al. The 2016 Singapore Zika virus outbreak did not cause a surge in Guillain‐Barré syndrome. J Peripher Nerv Syst. 2018;23:197‐201. [DOI] [PubMed] [Google Scholar]
- 4. Ellul MA, Benjamin L, Singh B, et al. Neurological associations of COVID‐19. Lancet Neurol. 2020;9:767‐783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Koh JS, De Silva DA, Quek AML, et al. Neurology of COVID‐19 in Singapore. J Neurol Sci. 2020;418:117118. [DOI] [PMC free article] [PubMed] [Google Scholar]


