As SARS‐CoV‐2 has spread across the globe, it has been difficult to ignore patterns suggesting that regions with poor air quality are witnessing disproportionate impacts in terms of the frequency and severity of COVID‐19 infection. Consequently, researchers have rightly recognized the importance of considering the role of air pollution in the COVID‐19 pandemic. Here, we discuss the pros and cons of air pollution as a contributing factor to COVID‐19, according to existing research questions (Table 1).
TABLE 1.
Research questions on air pollution as a contributing factor to COVID 19 infection
| Research question | Certainty vs. uncertainty |
|---|---|
| Is SARS‐CoV‐2 exhaled? | Yes |
| Is SARS‐CoV‐2 airborne? | Yes: evidence has accumulated that the majority of transmissions occur as a result of infected people spewing large droplets and small particles called aerosols when they cough, talk, sing, or breathe. |
| Is SARS‐CoV‐2 found in PM aerosols? | Potentially, as it can be carried by or mixed with secondary aerosols |
| Is SARS‐CoV‐2 viable once in suspension? | Yes, but needs to be confirmed |
| Is air pollution a co‐factor of SARS‐CoV‐2 infection? |
Yes, based on several mechanisms. Additionally, a link has already been observed in the cases of SARS, influenza, syncytial virus and measles. |
| Is COVID‐19 significantly related to air pollution? | Potentially yes, but additional ad hoc data are needed. In addition, the mechanisms are not understood. |
1. WHAT DATA EXIST ON THE RELATION OF AIR POLLUTION TO SARS‐COV‐2 OR COVID‐19?
At the general population level, COVID‐19 hospitalizations and deaths rates have skyrocketed in countries (eg, Iran, China, South Korea), regions (Lombardy), and towns (eg, New York, Madrid) most of which characterized by high levels of air pollution (eg, Lombardy, Iran, China, South Korea, New York, Madrid). Early in the pandemic, an Italian study positively related the proportion of daily exceedances of concentrations of particulate matter (PM) with 10 µm of diameter or less (PM10) with the number of COVID‐19admissions reported within the following 14 days. 1 Since then, various studies have confirmed the existence of a significant association between air pollution exposure and SARS‐CoV‐2 infection or COVID‐19 mortality. 2 A recent study that calculated the extent to which air pollution could be blamed for COVID‐19 deaths worldwide clearly showed that when both long‐term exposure to air pollution and infection with the COVID‐19 virus come together there is a significant adverse effect on health. 3 In East Asia, which has some of the highest levels of harmful pollution on the planet, it found that 27% of COVID‐19 deaths could be attributed to the health effects of poor air quality. The proportion was 19% in Europe, and 17% in North America. Not surprisingly, previous research has already shown the significant impact of air pollution on other respiratory viruses, such as SARS, influenza, syncytial virus and measles, also transmissible via the respiratory route. 2 However, no significant impact of air pollution on COVID‐19 was found in other zones also highly polluted (eg, Athens, London, Qatar). This may depend on fact that SARS‐CoV‐2 infection is multifactorial.
2. HOW CAN THIS BE EXPLAINED?
Two patterns seem possible 2 (Figure 1). On the one hand, air pollution may render people more susceptible to infection by SARS‐CoV‐2. It is well established that gases such as nitrogen dioxide (NO2) or ozone (O3) and respirable PM may modify airways permeability. In particular, exposure to either fine or ultrafine particles including black carbon may significantly damage lung epithelial cilia, the first line of defense against respiratory viruses including SARS‐CoV‐2, decrease the ability of macrophages to phagocytize the virus as well as prevent an effective immune response against the infection. Additionally, long‐term endemic exposure to air pollution is responsible through oxidative stress for chronic systemic inflammationat the origin of the comorbidities, such as cardiovascular and respiratory diseases, metabolic diseases, etc. that put COVID‐19 patients at higher risk of severe events and death. Specifically, the Angiotensin‐converting enzyme 2 (ACE‐2) receptor on lung cell surfaces, which is known to be involved in the way COVID‐19 infects patients 2 is over‐expressed under chronic exposure to air pollution. This has been described as a double hit: air pollution damages the lungs and increases the activity of ACE‐2, which in turn leads to enhanced uptake of the virus.
FIGURE 1.
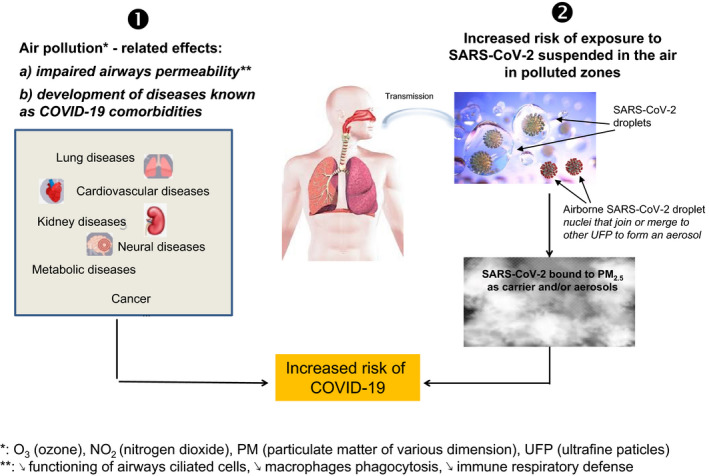
Patterns of air pollutants and SARS‐CoV‐2 interaction. Air pollution may contribute to COVID‐19 pandemic by 1) rendering people more susceptible to SARS‐CoV‐2 infection through impaired mucosal permeability and/or in the long term increased individual susceptibility to develop chronic diseases putting COVID‐19 patients at higher risk of severe COVID‐19 events and death; 2) augmenting the risk of exposure to SARS‐CoV‐2. Once in the air, SARS‐CoV‐2 can either be carried by fine particles or mix with secondary ultrafine aerosols. O3, Ozone; NO2, Nitrogen dioxide; PM: Particulate matter; ↘, diminution
On the other hand, there is now growing evidence that SARS‐CoV‐2 is exhaled as a result of regular breathing of an individual, becoming airborne and hence inhalable by others. 4 Once in the air, the virus can either be carried by fine particles or mix with secondary ultrafine aerosols. 2 Experimentally, it has been observed that SARS‐CoV‐2 remains viable in aerosols for up to 3 h, with rate of decrease of SARS‐CoV‐2 infectious titer comparable to that found for SARS‐CoV‐1, which supports another possible route of infection transmission other than respiratory droplets and contact via contaminated surfaces. 5
The viability and long‐range transport of respiratory viruses in open air, and thus their potential to infect individuals, have also been observed under real life conditions, 2 and for SARS‐CoV‐2 both indoors 4 and outdoors. 2 A recent study observed that the overburdening of the health services and hospitals, as well as the high over‐mortality due to COVID‐19 observed in various regions of Europe in the Spring of 2020 may be linked to peaks of PM2.5and likely particular weather situations that have favored the spread and enhanced the virulence of the virus. 6 Ergo, air pollution may be an important factor in viral disease transmission and further investigations into the interaction of SARS‐CoV‐2 and air pollution are warranted. Interestingly, recent data showed the ability of pollen to suppress innate antiviral immunity, independent of allergy. 7
3. IN WHICH MATTERS SHOULD WE BE CAUTIOUS?
The role of airborne SARS‐CoV‐2 transmission due to small respiratory droplets of diameter <5 µm emitted by symptomatic as well as asymptomatic, but infected, individuals at the origin of droplet nuclei remaining suspended in the air is, however, still challenged by a lack of studies. A major drawback in this respect is that the minimum infectious dose, as expressed in viral RNA copies necessary to promote the infection, is not yet defined. In addition, very few studies so far have assessed RNA copies in outdoor air and they are not conclusive. In a Chinese study, the observed RNA concentrations were above the detection limits only in crowded areas. 8 In Italy, a study also observed detectable SARS‐CoV‐2 RNA in congested zones, but not in less polluted zones (below 10 µg/m3 in mean). 9 A previous Italian study had similarly found traces of SARS‐CoV‐2 RNA in 23% of the sampled PM10 in a polluted zone but without assessing RNA copies. 10 However, sampling the virulence of the sampled virus has proved challenging so far.
Other major criticisms to the population‐based data are methodological. Studies of air pollution and SARS‐CoV‐2 or COVID‐19 are cross‐sectional or more rarely temporal series, have relied mainly on ecological measures of exposures and outcomes, and are susceptible to important sources of bias: selection bias, underreporting of health data, exposure misclassification, no taking into account of the infection dynamics, and poor adjustment for confounders. 11 Most of the studies published so far have only considered the one factor under study and usually without following strict methodological protocols for data harmonization for epidemiological studies. Only in the UK biobank dataset, data on the SARS‐CoV‐2 infection and some characteristics for adjustment were available at the individual level. 2 Additional co‐factors that could interact with air pollution and/or viral infections and that have to be taken into account in the models include among others air temperature (negative effect), UV radiation (negative association), and comorbidity. 2 Furthermore, longitudinal studies with individual‐level data are needed to adequately address this topic. In addition, careful peer review is necessary.
Though more studies are imperative, collectively the data existing so far suggest that air pollution—regardless of origin—should be considered as a contributing factor to the dynamics of COVID‐19 epidemics in terms of both viral transmission as well as pre‐existing susceptibility to viral infection, and advocate the need to diminish air pollution emissions in the interest of public health.
CONFLICT OF INTEREST
The authors have nothing to disclose.
REFERENCES
- 1. Setti L, Passarini F, De Gennaro G, et al. Potential role of particulate matter in the spreading of COVID‐19 in Northern Italy: first observational study based on initial epidemic diffusion. BMJ Open. 2020;10(9):e039338. 10.1136/bmjopen-2020-039338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bourdrel T, Annesi‐Maesano I, Alahmad B, Maesano C, Bind MA. The impact of outdoor air pollution on COVID‐19: a review of evidence from in vitro, animal, and human studies. Eur Respir Rev. 2021;30(159):200242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pozzer A, Dominici F, Haines A, Witt C, Münzel T, Lelieveld J. Regional and global contributions of air pollution to risk of death from COVID‐19. Cardiovasc Res. 2020;116(14):2247‐2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Morawska L, Milton DK. It is time to address airborne transmission of coronavirus disease 2019 (COVID‐19). Clin Infect Dis. 2020;71(9):2311‐2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS‐CoV‐2 as compared with SARS‐CoV‐1. N Engl J Med. 2020;382:1564–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rohrer M, Flahault A, Stoffel M. Peaks of fine particulate matter may modulate the spreading and virulence of COVID‐19. Earth Syst Environ. 2020;4(4):789‐796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gilles S, Blume C, Wimmer M, et al. Pollen exposure weakens innate defense against respiratory viruses. Allergy. 2020;75(3):576‐587. [DOI] [PubMed] [Google Scholar]
- 8. Liu Y, Ning Z, Chen Y, Guo M, Liu Y, Gali NK. Aerodynamic analysis of SARS‐CoV‐2 in two Wuhan hospitals. Nature. 2020;582:557‐560. [DOI] [PubMed] [Google Scholar]
- 9. Chirizzi D, Conte M, Feltracco M, et al. SARS‐CoV‐2 concentrations and virus‐laden aerosol size distributions in outdoor air in north and south of Italy. Environ Int. 2020;146:106255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Setti L, Passarini F, De Gennaro G, et al. SARS‐Cov‐2RNA found on particulate matter of Bergamo in Northern Italy: First evidence. Environ Res. 2020;188:109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Villeneuve PJ, Goldberg MS. Methodological considerations for epidemiological studies of air pollution and the SARS and COVID‐19 coronavirus outbreaks. Environ Health Perspect. 2020;128(9):95001. [DOI] [PMC free article] [PubMed] [Google Scholar]


