Abstract
Objectives
To explore factors associated with the impact of COVID‐19 on the Latinx population, a Scoping Review of literature was undertaken.
Design
A systematic review was conducted utilizing the Preferred Reporting Items for Systematic Reviews and Meta‐Analysis Scoping Review (PRISMA ScR) guidelines. A search of databases PubMed, CINAHL, and APA PsycINFO was conducted and included studies through November 23, 2020.
Sample
Selected articles were limited to English language, included population data from the US, were specific to the topic of COVID‐19, Latinx community findings significantly addressed, and added significant information to the developing narrative not covered elsewhere.
Results
Sixteen studies in the final selection included meta‐analyses, community‐based assessments, and electronic health records reviews of hospital systems and local/state/national public databases. This review describes the prevalence of COVID‐19 in the Latinx population, social factors related to disease burden, and the economic implications and disproportionality of COVID‐19.
Conclusions
The impact of COVID‐19 on the Latinx population is multi‐factorial. More research is needed to examine each of these factors in greater detail.
Keywords: COVID‐19, health disparities, Hispanic, Latinx
1. INTRODUCTION
The havoc visited upon the global community by COVID‐19 has brought the impact of infectious disease to the fore. The pandemic swiftly sickened over 125 million people and claimed the lives of 2.7 million worldwide (JHU, 2020). In the United States (US) alone over 30 million people have been sickened and more than 546,000 people have died (JHU, 2020). The increased impact of COVID‐19 on communities of color in the United States is of particular concern (Carethers, 2020; Chamie et al., 2020; Figueroa et al., 2020; Tai et al., 2020; Tirupathi et al., 2020).
The U.S. Latinx population includes people of Mexican, Puerto Rican, Cuban, Dominican, Guatemalan, Salvadoran, South American, Central American, and Caribbean descent (Velasco‐Mondragon et al., 2016). Persons identifying as Hispanic or Latino on census data in the United States have increased from 17.4% of the total population in 2014 (Velasco‐Mondragon et al., 2016) to an estimated 18.5% in 2019 (USCensusBureau, 2020), making Latinx the largest minority group within the United States. While research on COVID‐19 in the Latinx population is still developing, the purpose of this literature review is to describe the impact to date of COVID‐19 in the Latinx community in the United States when compared to the non‐Hispanic‐White (NHW) population.
2. BACKGROUND
Health disparities and inequity are foundational components to the discussion of disease distribution, morbidity, and mortality in populations, and this is especially true for U.S. Latinx. The impact of socioeconomic position (SEP) (Meier et al., 2016), poverty (Trepka et al., 2016), lack of availability of fresh, affordable, healthy food options termed “greengrocery deserts” (Carethers, 2020), insufficient housing (Velasco‐Mondragon et al., 2016), and lack of access to adequate healthcare (Soyemi et al., 2014; Truman et al., 2020) has long been associated with increased levels of infectious and non‐communicable disease (Meier et al., 2016; Soyemi et al., 2014; Sullivan et al., 2018; Trepka et al., 2016; Truman et al., 2020; Velasco‐Mondragon et al., 2016). Delays in treatment and lack of preventive care increase the risk of serious sequelae and disease burden for infections: for example, hepatitis, cancer, tuberculosis (Gudenkauf & Thrift, 2020; Pan et al., 2020; Velasco‐Mondragon et al., 2016), HIV (Sullivan et al., 2018; Trepka et al., 2016), and syphilis (Sullivan et al., 2018). For diseases of a communicable nature, delay can increase community spread and disease impact.
While Latinx persons are interwoven into communities across the United States, there are significant differences between their experiences compared to their NHW counterparts. On average, Latinx within the United States are four times less likely to have completed high school, twice as likely to live in poverty, with 9.6% of Latinx living in deep poverty defined as less than half of the poverty line when compared to NHW (Velasco‐Mondragon et al., 2016). Latinx are less likely to engage in preventive health care and less likely to report access to care for the prevention or treatment of health conditions (Carethers, 2020; Clarke et al., 2020; Cuellar et al., 2020; Velasco‐Mondragon et al., 2016). Latinx decreased access to preventative healthcare is multifactorial and includes lack of English fluency, discomfort with social services organizations including healthcare providers, unavailable or unacceptable choice of culturally sensitive healthcare providers, and lack of adequate health insurance (Clarke et al., 2020; Cuellar et al., 2020; Velasco‐Mondragon et al., 2016). Lack of employer‐based health coverage for working‐age Latinx is estimated at 30%, compared to their NHW counterparts at 11% uninsured or underinsured (Velasco‐Mondragon et al., 2016). Reduced access to routine healthcare services places Latinx at greater risk for health conditions associated with COVID‐19, such as hypertension, diabetes, obesity, and heart disease (Velasco‐Mondragon et al., 2016).
Issues of inequity and disproportionality were identified early in the COVID‐19 pandemic. The cause of the increased rate of COVID‐19 in Black, native‐American, and Latinx populations when compared to NHW has been theorized but no single answer emerged (Chamie et al., 2020; Cuellar et al., 2020; Figueroa et al., 2020; Izzy et al., 2020; Macias Gil et al., 2020; Selden & Berdahl, 2020; Tai et al., 2020; Tirupathi et al., 2020). This literature review compared only Latinx to NHW, so a focused exploration of the topics could be completed.
3. METHODS
A systematic scoping review of literature focused on the impact of COVID‐19 on the Latinx population was conducted utilizing the Preferred Reporting Items for Systematic Reviews and Meta‐Analysis Scoping Review (PRISMA ScR) guidelines with results summarized in Figure 1 (Moher et al., 2009). A search of databases PubMed, CINAHL, and APA PsycINFO was conducted and included studies since the pandemic began in late 2019 through November 23, 2020. All articles were limited to English language studies that included population data from the United States and were published within the last year. To determine the literature included in the final review, selected articles were examined and included if they were specific to the topic of COVID‐19 and added significant information to the developing narrative that was not covered elsewhere. Manuscripts covering prevention modalities, utilization of healthcare services, access to care, treatment approach, morbidity, mortality, and disparities were included. Inclusion criteria for the manuscripts had COVID‐19 as the primary focus with Latinx community findings significantly addressed. Manuscripts that did not have COVID‐19 as the primary focus and did not include the Latinx community prominently in the findings were excluded. The MeSH term of "Hispanic Americans" was utilized as it captures the terms Latina/Latino/Latinx/Hispanic and includes persons living in the United States of Mexican, Puerto Rican, Cuban, Central or South American as well as other Spanish Culture groups, but does not include Brazilian‐Americans or Portuguese‐ Americans. Table 1 describes each database searched and the specific search parameters, articles retrieved based upon the parameters searched, and articles selected for review. The final review contained 16 manuscripts that were selected for inclusion (Table 2).
FIGURE 1.
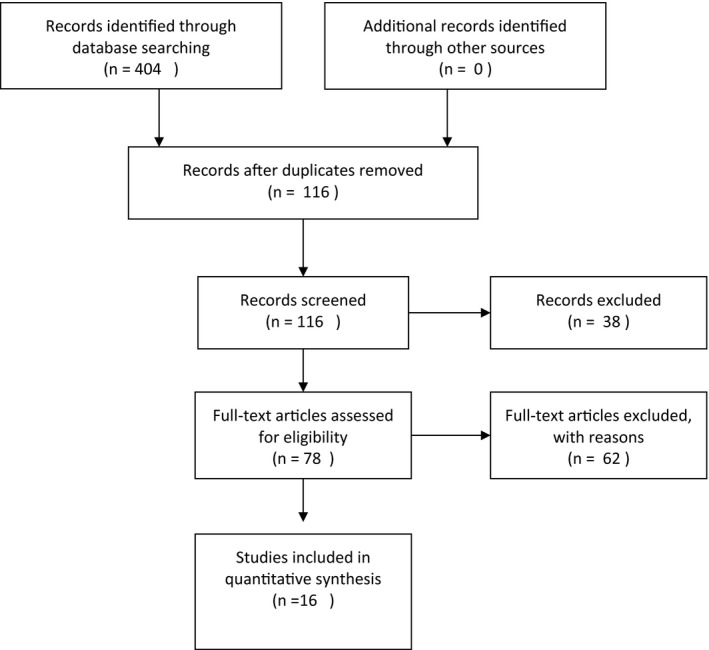
PRISMA ScR flow of literature search results (Moher et al., 2009)
TABLE 1.
Keywords and terms for systematic scoping literature review conducted November 2020
| Terms/MeSH terms | Number Returned | Number selected for review |
|---|---|---|
| PubMed Searches | ||
| Hispanic Americans AND COVID | 111 | 60 |
| Hispanic Americans AND Communicable Disease | 61 | 8 |
| Hispanic Americans AND Infectious Disease | 71 | 5 |
| Hispanic Americans AND COVID AND HIV | 8 | 0* |
| Latinx AND COVID | 53 | 0* |
| Latinx AND Communicable Disease | 21 | 0* |
| Latinx AND Infectious Disease | 34 | 0* |
| Latinx AND COVID AND HIV | 9 | 0* |
| CINAHL Search | ||
| Hispanic Americans AND COVID AND English AND Academic Journals | 36 | 5 |
| APA PsycInfo Search | ||
| Hispanic Americans AND COVID | 0 | 0 |
None selected related to all potential manuscripts identified during prior searches.
TABLE 2.
Literature review table
| Author/Date Title | Purpose | Sample/Study Description | Methods/Design | Limitations | Results |
|---|---|---|---|---|---|
| Carethers (2020) | Identify reasons and risk factors for disparities in morbidity and mortality from COVID19 | Review of existing literature at the time of authorship directed at the exploration of issues that might explain the distribution of COVID‐19 infection in the United States and risk of serious illness from COVID‐19. | Review | Date of review as publications and information is rapidly evolving. |
4 major risk factors: Age, comorbidities, male gender, race/ethnicity Increased risk: greengrocery deserts, Medicaid as health insurance, medical disability, SES, education level, race, "essential workers", size of home, # in household, multigenerational households, public transportation. No identified genetic, ABO, or immunologic predisposition. |
| Cates et al. (2020) | Compare the risk of death from all causes in hospitalized patients with COVID19 versus Influenza. |
VHA and Corporate Data Warehouse 3,948 hospitalized patients with COVID‐19 5,453 hospitalized patients with influenza Data collected: age, sex, race/ethnicity, ICD10 diagnosis codes, hospital admission, discharge dates, problem list records from at least 14 days prior to specimen collection date, ICU care admission, and death date if applicable. |
Retrospective EHR Records Review | ICD Codes may lack sensitivity and misclassify chronic as acute, obesity was based on ICD‐10 codes and not BMI, clinician ordered testing could potentially underestimate complications, small sample size of “non‐Hispanic other” race, influenza vaccinations, and treatment for COVID‐19 were not examined, generalizability may be limited by circulating influenza strain. |
33 acute complications identified. Hospitalized patients with COVID19: > 5 times higher risk of in‐hospital death and increased risk for 17 respiratory and non‐respiratory complications than did hospitalized patients with influenza. Risks of sepsis and respiratory, neurologic, and renal complications of COVID‐19: higher among Hispanic/Latinx patients than among NHW patients. |
| Chamie et al. (2020) | Identify transmission rate and risk factors for transmission |
Conducted over 4 days in a largely Latinx census tract (022,901) in San Francisco Convenience sample of 3,953 persons with tests performed (out of 5,174 possible residents) 40% Latinx; 41% white; 9% Asian/Pacific Islander; 2% Black |
Community‐Based Assessment Cross‐Sectional Design |
PCR and antibody testing sensitivity and reliability, selection bias is possible, self‐reported symptoms, and survey responses. |
40% Latinx; 41% white; 9% Asian/Pacific Islander; 2% Black Overall 2.1% of the total sample were PCR positive ‐ 95% of the positive results were Latinx. Risk factors for recent infections: Latinx ethnicity, inability to shelter in place and maintain income, frontline service work, unemployment, household income <$50,000/year. Five SARS‐CoV‐2 phylogenetic lineages were detected. |
| Figueroa et al. (2020) | To determine the demographic, economic, and occupational factors contributed to disparities in COVID‐19 incidence rates | 351 Massachusetts cities and towns from January 1‐May 6, 2020. | Cross‐sectional study | Discrepancies in how race/ethnicity, occupation, COVID‐19 cases, death rates are recorded in datasets. Done in a single state. Underlying comorbidities not explored. |
10 percentage point increase in Hispanic/Latinx population was associated with an increase of 258.2 cases per 100,000 population. Independent predictors of higher COVID‐19 rates: proportion of foreign‐born non‐citizens living in a community, mean household size, and prevalence of food service workers in the population. |
| Galanis et al. (2020) | Determine seroprevalence of SARS‐CoV‐2 in HCWs and determine factors associated with seropositivity | 49 studies which included 127,480 healthcare workers (HCWs) |
Systematic Review Meta‐analysis |
14 of 49 studies were published as pre‐prints, heterogeneity between results was very high, seroprevalence in the studies could be impacted by the type of testing completed, factors associated with seroprevalence required a qualitative approach to assess factors. |
Antibodies among HCWs overall were considered high at 8.7%. Seroprevalence higher in North American studies (12.7%), versus studies in Europe (8.5%), Africa (8.2%), and Asia (4%). Factors associated with seropositivity: male gender, race (Black, Asian, Hispanic), work in a COVID‐19 unit, patient‐related work, frontline HCWs, health care assistant role, PPE shortage, self‐reported previous SARS‐CoV‐2 infection, previous positive PCR test, household contact with suspected or confirmed COVID‐19 patient. |
| Holtgrave et al. (2020) | To determine the most impactful area for intervention to decrease disparities for NHW, AA/Black non‐Hispanic, and Hispanic/Latinx adults in NY state. |
Hospitalized NY COVID‐19 patients, NY State COVID‐19 hospitalization and death record archives Described each continuum using overall percentages, fatality rates, and relative changes between stages, with comparisons between race and ethnicity using risk ratios |
Retrospective Cohort Study Creation of an Outcomes Continuum utilizing data from: CDC, NY State Dept of Health, NYC Depart of Health |
Race/ethnicity categorizations are limited in some datasets. Continuum developed in a single state, at one point in time, with available data. Findings are not age‐adjusted. Pandemic is rapidly evolving. |
COVID‐19 fatality rates estimated per population: 0.03% white, 0.18% AA/Black, 0.12% Hispanic/Latinx. Community variance between: NHW and Hispanic/Latinx 3.48 fold disparity difference in infection experience. |
| Izzy et al. (2020) |
To determine the factors associated with a disparity in COVID‐19 |
5,190 COVID‐19 positive patients evaluated at 12 hospitals within Mass General Brigham Hospital System Hospitalized patients: 29% Required ICU: 33% Deceased: 4.3% Race of COVID‐19 positive patients: NHW 2,404 (46%) Latinx 1,309 (25%) AA/Black 719 (14%) Asian 177 (3%) |
Retrospective EHR Review | From a single health system, may underrepresent non‐hospitalized COVID‐19 positive patients. |
Hospitalized patients (1,489% –28.6%) were likely to be male 56% (versus. female 42%); Older (median 62 versus. 47 not hospt); Obese; More CV and pulmonary risk factors. Most common were HTN, hyperlipidemia, DM, COPD. Mortality higher in hospitalized than non‐hospitalized Race: 2,404 (46%) NHW, 1,309 (25%) Latinx, 719 (14%) AA/Black,177 Asian Latinx were more likely to be admitted, were hospitalized younger, disproportionally required ICU admission compared to NHW patients. SES correlated to hospitalization rates. Disparity is multifactorial (less healthcare insurance, access, presenting later in dz, higher comorbidity, lower SES.) |
| Macias Gil et al. (2020) | Describe the emerging disproportionate impact of COVID‐19 on the Hispanic/Latinx community in the United States. |
Identify potential antecedents. Consider strategies to address the disparate impact of COVID‐19 on this population. |
Review | Completed early in the U.S. pandemic (May, 2020). |
19.8% of Hispanics uninsured as of 2018 compared to 5.4% of NHW. Lowest rates of medical health insurance coverage of all racial/ethnic groups in the United States. Issues identified: Immigration status – mistrust of health and social institutions, language barriers, work conditions, financial burden, living conditions. |
| Mahajan et al. (2020) | Describe seroprevalence of SARS‐CoV‐2 IgG antibodies in a representative sample of CT residents to determine the need for continued adherence to risk mitigation strategies. |
567 respondents/ participants, Connecticut residents,> 18 years of age, residing in non‐congregant settings Intentional oversampling of Hispanic and Black residents related to weighted seroprevalence concerns. |
Representative Sample Study | Single state utilized, early in the pandemic, seroprevalence could be impacted by the type of testing completed |
567 respondents; 53% women; 75% NHW; 23 positive for SARS‐CoV‐2‐specific antibodies resulted in seroprevalence of 4.0% (90% confidence interval). The vast majority of CT residents lack SARS‐CoV‐2 antibodies. Weighted seroprevalence for oversampled non‐Hispanic Black 6.4% (90% CI0.9–11–9) and Hispanic 19.9% (90% CI 13.2–26.6). Majority of participants reported the following risk mitigation strategies: 73% avoided public places, 75% avoided gatherings of families and friends, 97% wore a facemask at least part of the time. |
| Meyerowitz et al. (2020) | To evaluate risk factors, clinical manifestations, and outcomes in a large cohort of PLWH with COVID‐19. |
Systematically identified all persons living with HIV (PLWH) who were diagnosed with COVID‐19 at a large hospital system from March 3‐April 26, 2020. Sample: 47 PLWH ‐ 36 PLWH with confirmed COVID‐19 and 11 with probable COVID‐19 |
Retrospective EHR Review Analyzed demographics, medical comorbidities, clinical presentation, illness course after COVID‐19 diagnosis |
From a single health system in one state, seroprevalence could be impacted by testing limitations. |
85% of PLWH with confirmed COVID‐19 had comorbidity associated with severe disease, including obesity, CVD, HTN. 77% of PLWH with COVID‐19 were non‐Hispanic Black or Latinx, whereas only 40% of PLWH in the clinic were Black or Latinx. Nearly half of PLWH with COVID‐19 had exposure to congregate settings. |
| Mithal et al. (2020) | To evaluate characteristics and risks of infants as it relates to COVID‐19 infection. |
171 infants less than 90 days of age who had positive nasopharyngeal PCR testing for SARS‐CoV‐2 at a Children's Hospital in Chicago, IL, between April 11 and May 12, 2020. 18 Infants aged 10–88 days tested COVID‐19 positive (15 in ED and 3 outpatient). |
Retrospective EHR Review | Single hospital system, early in the pandemic. |
171 infants tested, 18 infants aged 10–88 days tested positive (15 in ED and 3 outpatient). 78% of infants who tested positive were Latinx. 50% (9/18) were admitted to the inpatient, none required ICU. None required respiratory support. |
| Rentsch et al. (2020) | Evaluate the association between race/ethnicity and COVID‐19 testing/results |
5,834,543 persons receiving care through the VHA nationwide Total Tested: 254,595 COVID Positive: 16,317 Deaths: 1,057 |
Retrospective EHR cohort study | Conducted in the VHA – patients generally older and male. Unable to explore social determinants by race/ethnicity due to EHR limitations. Conducted during the early timeframe of pandemic when testing was less readily available. |
Results: 254,595 tests; 16,317 tested positive; 1,057 deaths. No difference in mortality by ethnicity. Likelihood of testing: Black 60.0/1000 Hispanic/Latinx 52.7/1000 NHW 38.6/1000 Positive tests (odds ratio compared to NHW): Black1.93 Hispanic/Latinx 1.84 Increased positivity rates for Hispanic/Latinx were stable over region, time, and outbreak pattern. |
| Sachdev et al. (2020) | To determine if PLWH are more susceptible to and experience more severe disease/outcomes of COVID‐19. |
SF Department of Public Health (SFDPH) testing database and SFDPH HIV surveillance Sample: 4,252 COVID‐19 tests performed among PLWH |
Retrospective review | Single city utilized and completed within the first six months of the pandemic. |
4.5% (N = 193) of PLWH were positive for COVID‐19 compared to 3.5%(N = 9,626) positivity rate among 272,555 people without HIV. Mean age of those co‐infected with both HIV and COVID‐19 was 48 years (20–76); 38.9% NHW, 38.3% Latinx, 11.9% Black; 91.2% male. 54.6% of PLWH and COVID‐19 were housed, with the remainder marginally housed. Housing status significant factor for co‐infection. The rate of severe illness with COVID‐19 in PLWH was not increased. |
| Selden and Berdahl (2020) | To determine explanations for racial/ethnic disparities in COVID‐19 hospitalizations and mortality. | Pooled data from 2014–2017 yielding 100,064 persons year observations on adults aged 18 yrs and older. |
Review of Medical Expenditure Panel Survey (MEPS) Augmented with American Time Use Survey (2017–2018) to determine work behaviors/industries |
Examined only community housed non‐institutionalized populations. Health risks were based upon self‐report. Employment data reflect occupation before COVID‐19. Did not address outcomes, overall hospital course of illness, overall quality of care. |
Disparities seen with COVID‐19 multifactorial: Income, education, health insurance, access to medical care, access to food, health status, job characteristics, living conditions. Risk for infection: Work exposure Household transmission Community contact Differences in Illness severity: Comorbidities Large racial/ethnic differences in employment and household composition that might contribute to infection. AA/Black more likely than NHW to work in healthcare, public safety, and public utility jobs. Hispanic more likely than NHW to work in food‐related jobs, and Black and Hispanic less likely to be able to work from home than NHW. |
| Tai et al. (2020) |
To explore the disparities seen in COVID‐19 through social determinants of health lens. |
Creation of a model to assist with understanding disparities seen in COVID‐19: Social determinants of health, social injustice, environmental factors, host factors | Review and Theoretical Construct | Completed early in pandemic |
Poverty in United States prior to COVID 24% Native Americans 22% AA/Black 19% Latinx 9% whites COVID‐19 disparities through social determinants of health lens 33.8% of COVID in U.S. Latinx (18% of the population), 21.8% AA/Black (13% of the population) Contributing factors: Comorbidities (access to prevention, healthcare) Housing (Redlining, overcrowding) Mistrust of health institutions (delay in care) |
| Tirupathi et al. (2020) | To analyze racial disparities in COVID‐19 cases in the United States and discuss possible reasons behind the inequities. | Sample drawn from Dept of Health website, Publicly available data from NYC and 16 states, and case counts. | Cross‐sectional analysis records review | Race/ethnicity data limited for some datasets including death case counts. Datasets from 16 states and NYC. Data is from early in the pandemic. | Incidence rates were higher among Hispanic/Latinx disproportionately when compared to their representation in the total population. |
4. RESULTS
The articles selected for review were all peer‐reviewed and utilized a variety of research methodologies: cross‐sectional design, retrospective records reviews, systematic reviews of existing literature, community‐based assessment, and representative sampling. As the selected articles were examined and synthesized, themes were identified that illuminated the impact of COVID‐19 on the Latinx community: prevalence, economics, and social variables.
5. PREVALENCE
Infectious disease prevalence within a population provides a snapshot of community health. For COVID‐19, prevalence is viewed through the prism of seroprevalence for active and prior infections, as well as overall morbidity and mortality. To determine seroprevalence, polymerase chain reaction (PCR), and antigen testing demonstrating current infection as well as antibody testing demonstrating prior infection were utilized (Chamie et al., 2020; Galanis et al., 2020; Mahajan et al., 2020).
5.1. Seroprevalence
In community‐based convenience sampling conducted in a largely Latinx census tract, Latinx persons represented only 41% of the 3,953 samples collected, but over 95% of the positive results (Chamie et al., 2020). Similarly, a community‐based random‐sampling survey of non‐congregant adults found seroprevalence for the overall population was 4.0% compared to 19.9% for Hispanic/Latinx (Mahajan et al., 2020). A Veterans Health Administration (VHA) nationwide retrospective records review of over 5 million persons found Hispanic patients had a higher likelihood of testing positive for COVID‐19 (1.84) compared to NHW (Rentsch et al., 2020). A meta‐analysis of 49 studies of 127,480 global healthcare workers (HCW) revealed that HCW from North America had higher seroconversion rates (12.7%) compared to all others (Europe 8.5%, Africa 8.2%, Asia 4%), with Latinx HCW at higher risk compared to NHW (Galanis et al., 2020).
Increased seroprevalence was noted regardless of study type (meta‐analysis, community‐based surveys) or geographic location (California, Massachusetts, nationwide, global) (Chamie et al., 2020; Galanis et al., 2020; Mahajan et al., 2020; Rentsch et al., 2020), suggesting a pattern of increased disease in the Latinx community requiring further exploration.
5.2. Morbidity and Mortality
COVID‐19 disease disparity in the Latinx community is further borne out with increased illness and death observed regardless of age, healthcare setting, and comorbidities. (Carethers, 2020; Cates et al., 2020; Figueroa et al., 2020; Holtgrave et al., 2020; Izzy et al., 2020; Meyerowitz et al., 2020; Mithal et al., 2020; Sachdev et al., 2020; Tai et al., 2020; Tirupathi et al., 2020). To examine disparities in morbidity and mortality, studies utilizing retrospective electronic health records reviews of public local, state, and national level databases (Holtgrave et al., 2020; Sachdev et al., 2020; Tirupathi et al., 2020), Veterans Administration (Cates et al., 2020), and private health institutions (Holtgrave et al., 2020; Izzy et al., 2020; Meyerowitz et al., 2020; Mithal et al., 2020), a cross‐sectional analysis (Figueroa et al., 2020), and a meta‐analysis (Tirupathi et al., 2020) were reviewed.
Although Latinx in the United States comprises approximately 18% of the total population (US Census Bureau, 2020), they account for nearly 33.8% of COVID‐19 cases where race is reported (Tai et al., 2020). Latinx patients with COVID‐19 are more likely to be admitted to the hospital regardless of age, more likely to require hospitalization and intensive care unit (ICU) admission, and disproportionally more likely to die from COVID‐19 than their NHW counterparts (Figueroa et al., 2020; Holtgrave et al., 2020; Izzy et al., 2020; Tirupathi et al., 2020).
A meta‐analysis of public health data from 16 states and New York City (NYC) demonstrated that Latinx persons are at a substantially higher risk of serious illness and death from COVID‐19 when compared to NHW (Tirupathi et al., 2020). A cross‐sectional analysis in Massachusetts found a similar disparity with a 10‐percentage point increase in the Latinx population associated with an increased case rate of 258.2 cases per 100,000 persons (Figueroa et al., 2020). Estimated COVID‐19 fatality rates for Latinx patients in New York state were 0.12% compared to 0.03% for NHW (Holtgrave et al., 2020). Latinx patients of all ages are 3.2 times more likely to die of COVID‐19 than NHW and 4.3 times higher in the 25–34‐year‐old age range (Carethers, 2020).
Izzy et al. (2020) found that of 5,190 patients of all ethnicities diagnosed with COVID‐19, a total of 29% required hospital admission, with an ICU admission rate of 33% and a fatality rate of 4.3%. For Latinx patients, they were more likely to be admitted to the hospital (35.9% compared to 25.8% NHW) and more likely to require ICU admission (39% compared to 30% NHW). When analyses of comorbidities’ impact on admission rates were controlled, Latinx were noted to require admission at twice the rate of NHW regardless of pre‐existing conditions. Age is noted to be a significant risk factor for serious sequela of COVID‐19, with those over the age of 65 years recognized to be at five times greater risk than young adults (Centers for Disease Control & Prevention, 2020a). For Latinx patients in this study, the average age of hospital admission was noted at 52 years compared to 72 years for NHW, suggesting a more serious course of illness for younger patients in the Latinx community. In patients aged 18–40 years old, this disparity continues, with young Latinx patients admitted at a rate of 22% compared to 6% for NHW (Izzy et al., 2020).
To better understand the hospitalization path for a patient admitted with COVID‐19, a review of VHA records comparing patients' hospital experience admitted for COVID‐19 versus influenza was completed (Cates et al., 2020). COVID‐19 patients had a higher risk of severe multi‐system complications such as respiratory failure, kidney failure, and sepsis with Latinx patients' rates of these sequelae noted to be significantly higher than NHW (Cates et al., 2020).
Mithal et al. (2020) found that although the pediatric emergency department usage for Latinx patients was 52%, Latinx infants represented 78% of positive COVID‐19 results. This trend of overrepresentation of COVID‐19 seropositive Latinx patients also held true for persons living with HIV (PLWH) who were co‐infected (Meyerowitz et al., 2020; Sachdev et al., 2020).
6. ECONOMICS
Over 70% of Latinx are estimated to have insufficient funds to cover three months of living expenses, placing their financial situation during a mandatory shelter‐in‐place or job loss at grave risk (Carethers, 2020). Latinx persons are more likely to live in poverty, have a lower education level, and be uninsured or have Medicaid for their insurance (Carethers, 2020). Identified factors associated with a recent diagnosis of COVID‐19 included household income less than $50,000 per year, employment as a frontline service worker, and an inability to shelter‐in‐place related to potential loss of employment or income (Chamie et al., 2020).
6.1. Workplace
Of late, workplace has often meant working remotely to limit our exposure to this respiratory contagion; however, for many in the Latinx community, working from home is a luxury they cannot afford (Baquero et al., 2020; Carethers, 2020; Figueroa et al., 2020; Selden & Berdahl, 2020). Latinx persons are more likely than NHW to fill "essential" jobs (e.g., food service, building maintenance, and housekeeping) which are more likely to be impacted by COVID‐19 through a reduction in pay or unemployment (Carethers, 2020; Figueroa et al., 2020; Selden & Berdahl, 2020). In a meta‐analysis of HCWs, factors commonly associated with seropositivity included: frontline patient care duties, healthcare‐assistant role, and shortage of personal protective equipment (PPE) (Galanis et al., 2020). While overall compliance rates with risk mitigation efforts such as avoiding public places (73%), avoiding in‐home gatherings (75%), and wearing a mask when outside the home (97%), were relatively comparable across groups (e.g., NHW, Black, Hispanic), a noticeable difference was in the ability to work from home: Hispanics/Latinx at (11.8%) compared to all respondents (39.3%) (Mahajan et al., 2020).
6.2. Policies
Issues of access to health insurance, access to healthcare, sick leave, childcare, and historic wage disparities are particularly consequential for the Latinx community (Carethers, 2020; Figueroa et al., 2020; Izzy et al., 2020; Macias Gil et al., 2020; Meyerowitz et al., 2020; Sachdev et al., 2020; Selden & Berdahl, 2020; Tai et al., 2020). For an "essential worker" the prospect of missing work to care for a child who is sick or learning remotely is a precarious situation with financial consequences (Carethers, 2020; Selden & Berdahl, 2020).
Policies that cause communities of color to experience economic disparities, including redlining of housing (Millett et al., 2020; Tai et al., 2020), have a significant impact on overall family wealth creation and lessen the ability of those in poverty to move up into the middle class. For those Latinx who are recent immigrants, less favorable immigration policies, and fear of public institutions related to deportation risk are significant deterrents to seeking care for health‐related issues (Figueroa et al., 2020; Izzy et al., 2020; Macias Gil et al., 2020).
In addition to the aforementioned issues experienced by Latinx persons in the United States, the lack of insurance and lack of access to culturally sensitive healthcare providers is a significant barrier to care which can exacerbate underlying health conditions seen in COVID‐19 (Carethers, 2020; Izzy et al., 2020; Macias Gil et al., 2020; Selden & Berdahl, 2020). Latinx have the lowest rate of medical health insurance in the United States, with 19.8% of Latinx uninsured compared to 5.4% of NHW (Macias Gil et al., 2020). Lack of insurance leads to a reticence to seek care for fear of additional financial burden (Izzy et al., 2020; Macias Gil et al., 2020), leading to a delayed presentation for health concerns and more advanced disease at the time of presentation (Carethers, 2020; Izzy et al., 2020; Macias Gil et al., 2020; Selden & Berdahl, 2020). Reduced access to routine healthcare services places Latinx at greater risk for health conditions associated with COVID‐19, such as hypertension, diabetes, obesity, and heart disease (Carethers, 2020).
7. SOCIAL FACTORS
Complex social factors compound the already troubling landscape of COVID‐19 in the Latinx community. Greengrocery deserts (Carethers, 2020; Selden & Berdahl, 2020) and household overcrowding (Figueroa et al., 2020; Izzy et al., 2020; Selden & Berdahl, 2020) significantly impact U.S. Latinx and increase their risk of contracting COVID‐19.
Ready access to adequate food, water, housing, and sanitary needs are the basic requirements of a developed society, but for the U.S. Latinx community too often these basic needs go unmet. Latinx households in the United States are less likely to possess functional indoor plumbing, access to basic sanitation, and electricity than NHW (Tirupathi et al., 2020). The time, energy, and percentage of income spent to acquire basic needs are substantial for Latinx and unlike the experience of their NHW counterparts (Carethers, 2020; Tai et al., 2020). In the United States, socioeconomic inequities place Latinx at a distinct disadvantage, with an estimated 19% living below the poverty line compared to 9% for NHW (Tai et al., 2020). With shelter‐in‐place orders requiring children to be out of public schools, the loss of subsidized daytime meals worsens food insecurity (Carethers, 2020).
Living in a community with a high concentration of foreign‐born non‐citizens, high levels of food service workers, and larger mean household sizes were independent predictors for increased rates of COVID‐19 (Figueroa et al., 2020). Multigenerational households are common in the Latinx community, which further increases the risk of experiencing a household contact who is positive for COVID‐19 (Carethers, 2020; Figueroa et al., 2020; Galanis et al., 2020; Selden & Berdahl, 2020; Tai et al., 2020; Tirupathi et al., 2020). In the Medical Expenditure Panel Survey (MEPS) database, Latinx average household size is 3.8 people compared to NHW of 2.8 people (Selden & Berdahl, 2020). For PLWH who are Latinx, the issue of insufficient housing is even more significant, with greater than 50% reporting being unhoused or experiencing congregant living (Meyerowitz et al., 2020; Sachdev et al., 2020).
The impact of language barriers within the Latinx community cannot be overstated. Inability to speak, read, or understand English, significantly diminishes the ability to apply for work, follow health instructions, access healthcare services, and engage in higher education in the United States, thus limiting economic opportunities and flowing into the cascade of disparity that informs the other risks for poverty and COVID‐19 (Izzy et al., 2020; Macias Gil et al., 2020; Selden & Berdahl, 2020; Velasco‐Mondragon et al., 2016). For Latinx, the high school dropout rate is nearly three times higher than NHW, with only 15% going on to achieve a bachelor's degree from a university compared to 40% NHW (Velasco‐Mondragon et al., 2016).
The risks associated with these social factors do not end with contracting COVID‐19; rather, they extend into higher death rates as well. Higher rates of mortality attributed to COVID‐19 are seen in areas with greengrocery deserts (Carethers, 2020; Selden & Berdahl, 2020), higher levels of poverty (Izzy et al., 2020; Macias Gil et al., 2020; Selden & Berdahl, 2020), and lower levels of education (Izzy et al., 2020; Macias Gil et al., 2020; Selden & Berdahl, 2020).
8. DISCUSSION
Prevalence of COVID‐19 in the Latinx community is seen in community‐based sampling of antigen and antibody testing, retrospective reviews, and morbidity and mortality data regardless of study type or geographic location (Chamie et al., 2020; Galanis et al., 2020; Mahajan et al., 2020; Rentsch et al., 2020). The disparity of COVID‐19 disease distribution in the Latinx community is borne out with increased illness and death observed regardless of age, healthcare setting, and comorbidities. (Carethers, 2020; Cates et al., 2020; Figueroa et al., 2020; Holtgrave et al., 2020; Izzy et al., 2020; Meyerowitz et al., 2020; Mithal et al., 2020; Sachdev et al., 2020; Tai et al., 2020; Tirupathi et al., 2020). Latinx patients with COVID‐19 are more likely to require hospitalization and ICU admission, and disproportionally more likely to die from COVID‐19 than their NHW counterparts (Figueroa et al., 2020; Holtgrave et al., 2020; Izzy et al., 2020; Tirupathi et al., 2020).
Economic frailty and social disparities are also disproportionately seen in the Latinx community and contribute to this complex disease state. Latinx persons are more likely to live in poverty, experience insufficient housing and green‐grocery deserts, have lower education levels, and be uninsured or underinsured (Carethers, 2020; Izzy et al., 2020; Macias Gil et al., 2020; Selden & Berdahl, 2020). For Latinx workers, an inability to shelter‐in‐place, and employment as a frontline service‐worker or healthcare assistant, places them at increased risk of exposure to COVID‐19 outside the home (Carethers, 2020; Figueroa et al., 2020; Galanis et al., 2020; Selden & Berdahl, 2020). Policies that may contribute to the experience of COVID‐19 in the Latinx community and influence the ability to seek care include issues of immigration, access to health insurance, access to culturally competent healthcare, childcare, and paid sick leave for workers (Carethers, 2020; Figueroa et al., 2020; Izzy et al., 2020; Macias Gil et al., 2020; Meyerowitz et al., 2020; Sachdev et al., 2020; Selden & Berdahl, 2020; Tai et al., 2020).
The impact of COVID‐19 on the Latinx community in the United States is concerning. This potentially fatal, highly contagious infectious disease is causing infection, and death at a disproportionate rate within the Latinx community. The suffering caused by loss of income, instability in education, and childcare for Latinx children, and increased fragility of this community's socioeconomic fabric caused by increased morbidity and mortality of wage earners is significant.
9. GAPS AND LIMITATIONS
The most significant limitation of this review is COVID‐19 itself. The disease has been recognized for one year, yet we are still learning about transmission, prevention, treatment, and future impact of the disease. The long‐term sequela for patients who survived COVID‐19 infection is still unknown (Mahase, 2020). For some survivors, ongoing severe health issues have been identified, while others appear to have few sequelae. The degree to which disparities are borne out in the later phase of COVID‐19 remains to be studied.
Other unknowns that may impact the Latinx community will be shaped by the policies of our political leaders and their global counterparts. The inauguration of a new U.S. President is anticipated to change policies on issues of immigration, the economy, healthcare, and global engagement from the previous administration's approach (Alvarez, 2020; Frumkin & Myers, 2020; McInturff & Lewis, 2020; Ries, 2020). The rate and overall degree of financial recovery for United States and global economies remain uncertain (Atkeson, 2020; Bartsch et al., 2020, McKibbin & Fernando, 2020). The long‐term economic consequences of COVID‐19 on changes in the job sector with business closures, movement from an in‐person economy to one that is more heavily reliant on technology, resumption of travel, and its effect on the hospitality industry, all are quite impactful for the Latinx community. Some businesses and industries may permanently close, precipitating increased unemployment, which could lead to a worsening financial situation for marginalized communities. Access to healthcare resources may also be altered by the closure of some primary care institutions but conversely aided by the potential expansion of public options for healthcare insurance and access to care (King, 2020). Additionally, the global consequences to our relationships abroad and impact on international trade may be significant (Baldwin & Tomiura, 2020; Fernandes, 2020). Future studies on the impact of these policies on the Latinx community will be warranted.
In the near future, events will occur that can potentially reshape the battle against COVID‐19. Immunizations that are estimated to have a high rate of effectiveness in the prevention of COVID‐19 infection are slated for widespread release (Centers for Disease Control & Prevention, 2020b). The overall uptake of the U.S. immunization campaign, especially within the Latinx community, will require an individualized, culturally sensitive approach (Hughes et al., 2018; Salgado de Snyder et al., 2020). It is unclear what percentage of the population will agree to receive the immunizations or barriers to vaccination acceptance, but the issues raised and barriers presented will require further study.
10. CONCLUSION
Issues of healthcare access and increased rates of disease have been raised when discussing the prevalence of other infectious diseases in the Latinx community (Soyemi et al., 2014; Trepka et al., 2016; Truman et al., 2020); however, COVID‐19 illuminated the factors associated with the disproportionality of disease burden within the Latinx population. The disparities, social injustice, and suffering we have seen during the COVID‐19 pandemic should give us pause and force us to face the consequence of continuing down this path of inequity without attempting to change the factors that contributed to its rise. Only through the deliberate, contemplative, and steadfast actions of a motivated populace will we become "a more perfect union" (U.S. Const.,pmbl).
11. DATA SHARING AVAILABILITY STATEMENT
No datasets were generated during the current study.
Moore KS. The Impact of COVID‐19 on the Latinx Population: A Scoping Literature Review. Public Health Nurs. 2021;38:789–800. 10.1111/phn.12912
REFERENCES
- Alvarez, J. (2020). This is how President‐elect Biden’s policies could affect Hispanics in America. CNBC. Retrieved December 24,2020 from https://www.cnbc.com/2020/11/13/this‐is‐how‐president‐elect‐bidens‐policies‐could‐affect‐hispanics.html [Google Scholar]
- Atkeson, A. (2020). What will be the economic impact of covid‐19 in the US? Rough estimates of disease scenarios (0898‐2937). [Google Scholar]
- Baldwin, R. , & Tomiura, E. (2020). Thinking ahead about the trade impact of COVID‐19. In Economics in the Time of COVID‐19 (pp. 59–71). Centre for Economic Policy Research. [Google Scholar]
- Baquero, B. , Gonzalez, C. , Ramirez, M. , Chavez Santos, E. , & Ornelas, I. J. (2020). Understanding and addressing Latinx COVID‐19 disparities in Washington State. Health Education & Behavior, 47(6), 845–849. 10.1177/1090198120963099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartsch, S. M. , Ferguson, M. C. , McKinnell, J. A. , O'Shea, K. J. , Wedlock, P. T. , Siegmund, S. S. , & Lee, B. Y. (2020). The potential health care costs and resource use associated with COVID‐19 in The United States. Health Affairs (Millwood), 39(6), 927–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carethers, J. M. (2020). Insights into disparities observed with COVID‐19. Journal of Internal Medicine, 289(4), 463–473. 10.1111/joim.13199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cates, J. , Lucero‐Obusan, C. , Dahl, R. M. , Schirmer, P. , Garg, S. , Oda, G. , Hall, A. J. , Langley, G. , Havers, F. P. , Holodniy, M. , & Cardemil, C. V. (2020). Risk for in‐hospital complications associated with COVID‐19 and influenza—Veterans Health Administration, United States. MMWR. Morbidity and Mortality Weekly Report, 69(42), 1528–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2020). Older adults at greater risk of requiring hospitalization or dying if diagnosed with COVID‐19. https://www.cdc.gov/coronavirus/2019‐ncov/need‐extra‐precautions/older‐adults.html .
- Centers for Disease Control and Prevention . (2020). COVID‐19 Vaccines. https://www.cdc.gov/coronavirus/2019‐ncov/vaccines/index.html [PubMed] [Google Scholar]
- Chamie, G. , Marquez, C. , Crawford, E. , Peng, J. , Petersen, M. , Schwab, D. , Schwab, J. , Martinez, J. , Es, D. J. , Black, D. , Gandhi, M. , Kerkhoff, A. D. , Jain, V. , Sergi, F. , Jacobo, J. , Rojas, S. , Tulier‐Laiwa, V. , Gallardo‐Brown, T. , Appa, A. , … Havlir, D. V. (2020). SARS‐CoV‐2 community transmission disproportionately affects Latinx population during shelter‐in‐place in San Francisco. Clinical Infectious Diseases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke, S. K. , Kumar, G. S. , Sutton, J. , Atem, J. , Banerji, A. , Brindamour, M. , Geltman, P. , & Zaaeed, N. (2020). Potential impact of COVID‐19 on Recently resettled refugee populations in the United States and Canada: Perspectives of Refugee Healthcare Providers. Journal of Immigrant and Minority Health, 23(1), 184–189. 10.1007/s10903-020-01104-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuellar, N. G. , Aquino, E. , Dawson, M. A. , Garcia‐Dia, M. , Im, E. , Jurado, L. M. , Lee, Y. S. , Littlejohn, S. , Tom‐Orme, L. , & Toney, D. (2020). Culturally Congruent Health Care of COVID‐19 in minorities in the United States: A clinical practice paper from the National Coalition of Ethnic Minority Nurse Associations. Journal of Transcultural Nursing, 31(5), 434–443. 10.1177/1043659620941578 [DOI] [PubMed] [Google Scholar]
- Fernandes, N. (2020). Economic effects of coronavirus outbreak (COVID‐19) on the world economy. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3557504
- Figueroa, J. F. , Wadhera, R. K. , Lee, D. , Yeh, R. W. , & Sommers, B. D. (2020). Community‐level factors associated with racial and ethnic disparities in COVID‐19 rates in Massachusetts. Health Affairs, 39(11), 1984–1992. 10.1377/hlthaff.2020.01040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frumkin, H. & Myers, S. (2020). Planetary health and the 2020 US election. The Lancet, 396(10257), 1048–1050. 10.1016/S0140-6736(20)32038-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanis, P. , Vraka, I. , Fragkou, D. , Bilali, A. , & Kaitelidou, D. (2020). Seroprevalence of SARS‐CoV‐2 antibodies and associated factors in health care workers: A systematic review and meta‐analysis. Journal of Hospital Infection, 108, 120–134. 10.1016/j.jhin.2020.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudenkauf, F. J. , & Thrift, A. P. (2020). Racial/Ethnic differences in cancers attributable to preventable infectious agents in Texas, 2015. Public Health Reports, 135(6), 805–812. 10.1177/0033354920954497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtgrave, D. R. , Barranco, M. A. , Tesoriero, J. M. , Blog, D. S. , & Rosenberg, E. S. (2020). Assessing racial and ethnic disparities using a COVID‐19 outcomes continuum for New York State. Annals of Epidemiology, 48, 9–14. 10.1016/j.annepidem.2020.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes, M. M. , Saiyed, N. S. , & Chen, T. S. (2018). Local‐level adult influenza and pneumococcal vaccination disparities: Chicago, Illinois, 2015–2016. American Journal of Public Health, 108(4), 517–523. 10.2105/AJPH.2017.304257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izzy, S. , Tahir, Z. , Cote, D. J. , Al Jarrah, A. , Roberts, M. B. , Turbett, S. , Kadar, A. , Smirnakis, S. M. , Feske, S. K. , Zafonte, R. , Fishman, J. A. , & El Khoury, J. (2020). Characteristics and outcomes of Latinx patients with COVID‐19 in comparison with other ethnic and racial groups. Open Forum Infectious Diseases, 7(10), ofaa401. 10.1093/ofid/ofaa401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns Hopkins University (JHU) . (2020). COVID‐19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
- King, J. S. (2020). COVID‐19 and the need for healthcare reform. New England Journal of Medicine, 382(26), e104. 10.1056/NEJMp2000821 [DOI] [PubMed] [Google Scholar]
- Macias Gil, R. , Marcelin, J. R. , Zuniga‐Blanco, B. , Marquez, C. , Mathew, T. , & Piggott, D. A. (2020). Pandemic: Disparate health impact on the Hispanic/Latinx population in the United States. Journal of Infectious Diseases, 222(10), 1592–1595. 10.1093/infdis/jiaa474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahajan, S. , Srinivasan, R. , Redlich, C. A. , Huston, S. K. , Anastasio, K. M. , Cashman, L. , Massey, D. S. , Dugan, A. , Witters, D. , Marlar, J. , Li, S. X. , Lin, Z. , Hodge, D. , Chattopadhyay, M. , Adams, M. D. , Lee, C. , Rao, L. V. , Stewart, C. , Kuppusamy, K. , … Krumholz, H. M. (2020). Seroprevalence of SARS‐CoV‐2‐specific IgG antibodies among adults living in Connecticut: Post‐Infection Prevalence (PIP) Study. American Journal of Medicine. 10.1016/j.amjmed.2020.09.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahase, E. (2020). Covid‐19: What do we know about “long covid”? BMJ, 370, m2815. [DOI] [PubMed] [Google Scholar]
- McInturff, W. , & Lewis, J. (2020). What COVID‐19 and the nomination of Joe Biden mean for health care in the 2020 presidential election. JAMA Health Forum, 1(7), e200825. 10.1001/jamahealthforum.2020.0825 [DOI] [PubMed] [Google Scholar]
- McKibbin, W. , & Fernando, R. (2020). The economic impact of COVID‐19. In Economics in the Time of COVID‐19 (pp. 45–51). Centre for Economic Policy. Researchhttp://www.sensiblepolicy.com/download/2020/2020_CEPR_McKibbin_Fernando_COVD‐19.pdf [Google Scholar]
- Meier, H. S. , Haan, M. N. , Mendes de Leon, C. F. , Simanek, A. M. , Dowd, J. B. , & Aiello, A. E. (2016). Early life socioeconomic position and immune response to persistent infections among elderly Latinos. Social Science & Medicine, 166, 77–85. 10.1016/j.socscimed.2016.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyerowitz, E. A. , Kim, A. Y. , Ard, K. L. , Basgoz, N. , Chu, J. T. , Hurtado, R. M. , Lee, C. K. , He, W. , Minukas, T. , Nelson, S. , Ojikutu, B. O. , Robbins, G. , Sanchez, S. , Triant, V. A. , Zachary, K. , Gandhi, R. T. (2020). Disproportionate burden of coronavirus disease 2019 among racial minorities and those in congregate settings among a large cohort of people with HIV. AIDS, 34(12), 1781–1787. 10.1097/QAD.0000000000002607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett, G. A. , Honermann, B. , Jones, A. , Lankiewicz, E. , Sherwood, J. , Blumenthal, S. , & Sayas, A. (2020). White Counties stand apart: The primacy of residential segregation in COVID‐19 and HIV diagnoses. AIDS Patient Care & STDs, 34(10), 417–424. 10.1089/apc.2020.0155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mithal, L. B. , Machut, K. Z. , Muller, W. J. , & Kociolek, L. K. (2020). SARS‐CoV‐2 infection in infants less than 90 days old. Journal of Pediatrics, 224, 150–152. 10.1016/j.jpeds.2020.06.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , Altman, D. , & The PRISMA Group . (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. PLoS Med, 6(7), e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan, C. Q. , Rabinovich, C. , Gayam, V. , Normatov, M. , Fidman, B. , & Wang, D. (2020). Late presenters among minority patients with chronic hepatitis C infection in the USA. International Journal of Public Health, 65(7), 1181–1191. 10.1007/s00038-020-01467-3 [DOI] [PubMed] [Google Scholar]
- Rentsch, C. T. , Kidwai‐Khan, F. , Tate, J. P. , Park, L. S. , King, J. T. , Skanderson, M. , Hauser, R. G. , Schultze, A. , Jarvis, C. I. , Holodniy, M. , Lo Re, V. , Akgün, K. M. , Crothers, K. , Taddei, T. H. , Freiberg, M. S. , & Justice, A. C. (2020). Patterns of COVID‐19 testing and mortality by race and ethnicity among United States veterans: A nationwide cohort study. PLoS Med, 17(9), e1003379. 10.1371/journal.pmed.1003379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ries, L. (2020). President Trump and Joe Biden: Comparing Immigration Policies. The Heritage Foundation. https://www.heritage.org/sites/default/files/2020‐10/BG3547.pdf. [Google Scholar]
- Sachdev, D. , Mara, E. , Hsu, L. , Scheer, S. , Rutherford, G. , Enanoria, W. , & Gandhi, M. (2020). COVID‐19 susceptibility and outcomes among people living with HIV in San Francisco. Journal of Acquired Immune Deficiency Syndromes, 86(1), 19–21. 10.1097/QAI.0000000000002531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salgado de Snyder, V. N. , Garcia, D. , Pineda, R. , Calderon, J. , Diaz, D. , Morales, A. , & Perez, B. (2020). Exploring why adult Mexican males do not get vaccinated: Implications for COVID‐19 preventive actions. Hispanic Journal of Behavioral Sciences, 42(4), 515–527. 10.1177/0739986320956913 [DOI] [Google Scholar]
- Selden, T. M. , & Berdahl, T. A. (2020). COVID‐19 and racial/ethnic disparities in health risk, employment, and household composition. Health Affairs (Millwood), 39(9), 1624–1632. 10.1377/hlthaff.2020.00897 [DOI] [PubMed] [Google Scholar]
- Soyemi, K. , Medina‐Marino, A. , Sinkowitz‐Cochran, R. , Schneider, A. , Njai, R. , McDonald, M. , Glover, M. , Garcia, J. , & Aiello, A. E. (2014). Disparities among 2009 pandemic influenza A (H1N1) hospital admissions: A mixed methods analysis–Illinois, April‐December 2009. PLoS One, 9(4), e84380. 10.1371/journal.pone.0084380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan, P. S. , Purcell, D. W. , Grey, J. A. , Bernstein, K. T. , Gift, T. L. , Wimbly, T. A. , Hall, E. , & Rosenberg, E. S. (2018). Patterns of racial/ethnic disparities and prevalence in HIV and Syphilis diagnoses among men who have sex with men, 2016: A Novel data visualization. American Journal of Public Health, 108(S4), S266–S273. 10.2105/AJPH.2018.304762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai, D. B. G. , Shah, A. , Doubeni, C. A. , Sia, I. G. , & Wieland, M. L. (2020). The disproportionate impact of COVID‐19 on racial and ethnic minorities in the United States. Clinical Infectious Diseases, 72(4), 703–706. 10.1093/cid/ciaa815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirupathi, R. , Muradova, V. , Shekhar, R. , Salim, S. A. , Al‐Tawfiq, J. A. , & Palabindala, V. (2020). COVID‐19 disparity among racial and ethnic minorities in the US: A cross sectional analysis. Travel Medicine and Infectious Disease, 38, 101904. 10.1016/j.tmaid.2020.101904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trepka, M. J. , Fennie, K. P. , Sheehan, D. M. , Niyonsenga, T. , Lieb, S. , & Maddox, L. M. (2016). Racial‐ethnic differences in all‐cause and HIV mortality, Florida, 2000–2011. Annals of Epidemiology, 26(3), 176–182.e171. 10.1016/j.annepidem.2016.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truman, B. I. , Moonesinghe, R. , Brown, Y. T. , Chang, M.‐H. , Mermin, J. H. , & Dean, H. D. (2020). Differential association of HIV funding with HIV mortality by race/ethnicity, United States, 1999–2017. Public Health Reports, 135(1_suppl), 149S–157S. 10.1177/0033354920912716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- USCensusBureau . (2020). Quick Facts United States. https://www.census.gov/quickfacts/fact/table/US/RHI725219
- USConstitution . (1776). U.S. Const. U.S. Const, pmbl. https://www.uscourts.gov/about‐federal‐courts/educational‐resources/about‐educational‐outreach/activity‐resources/us
- Velasco‐Mondragon, E. , Jimenez, A. , Palladino‐Davis, A. G. , Davis, D. , & Escamilla‐Cejudo, J. A. (2016). Hispanic health in the USA: A scoping review of the literature. Public Health Reviews, 37, 31. 10.1186/s40985-016-0043-2 [DOI] [PMC free article] [PubMed] [Google Scholar]


