Abstract
Considering the recent COVID‐19 pandemic, we recognised a lack of synthesis amongst the available literature pertaining to the intersections of homelessness and pandemic response and planning. Therefore, the purpose of this review was to identify relevant peer‐reviewed literature in this area to thematically produce evidence‐based recommendations that would inform community planning and response amongst homeless populations. Although this review is inspired by the COVID‐19 pandemic, our intention was to produce relevant recommendations to for all current and future outbreaks and pandemics more generally. Our search criteria focused on pandemics and rapid‐spread illnesses such as contagious respiratory diseases with contact spread and with an emphasis on individuals experiencing homelessness. Content analysis methods were followed to extract and thematically synthesise key information amongst the 223 articles that matched our search criteria between the years of 1984 and 2020. Two reviewers were assigned to the screening process and used Covidence and undertook two rounds of discussion to identify and finalise themes for extraction. This review illustrates that the current breadth of academic literature on homeless populations has thus far focused on tuberculosis (TB) rather than diseases that are more recent and closely related to COVID‐19—such as Severe Acute Respiratory Syndrome (SARS) or H1N1. Our thematic content analysis revealed six themes that offer tangible and scalable recommendations which include (1) education and outreach, (2) adapting structure of services, (3) screening and contract tracing, (4) transmission and prevention strategies, (5) shelter protocols and (6) treatment, adherence and vaccination. The breadth and depth of reviews such as these are dependent on the quantity and quality of the available literature. Therefore, the limited existing literature outside of tuberculosis specific to homelessness in this review illustrates a need for more academic research into the intersections of pandemics and homelessness—particularly for evaluations of response and planning. Nonetheless, this review offers timely considerations for pandemic response and planning amongst homeless populations during the current COVID‐19 pandemic and can facilitate future research in this area.
Keywords: COVID‐19, emergency planning, homelessness, literature review, outbreak, pandemic, public health
What is known about this topic
The arrival of the COVID‐19 pandemic requires an assessment of outbreak response and planning amongst vulnerable groups.
Those experiencing homelessness do not fare well in terms of general health, providing them with compounded risks in the face of public health outbreaks.
The transient characteristics of homelessness provide unique challenges for planning, implementing and communicating any pandemic associated public health response.
What this paper adds
A synthesis of the available literature surrounding the intersections of homelessness and pandemic planning and response that include shelter protocols, preventative strategies, and education and outreach.
A range of best practices for the vaccination, treatment and adherence amongst homeless populations.
Recommendations for evaluation research into the implementation and success of the various homelessness outbreak responses, especially in relation to COVID‐19.
1. INTRODUCTION
At the time of writing this manuscript, there were over 60 million global cases of COVID‐19 with almost one and a half million deaths (World Health Organization, 2020a). The World Health Organization (2020b) recommends that all member nations need to administer a thorough public health response to COVID‐19 to control the spread and interpersonal transmission of the virus. Whilst various global measures have been essential to preventing COVID‐19, they do not account for the unique susceptibilities of vulnerable groups. In addition to the development of general guidance and public health measures, the Inter‐Agency Standing Committee (2020) suggests that ‘…extra care should be taken to assess their possible impact on the most vulnerable amongst populations to avoid disproportionate or discriminatory impacts’ (p. 4). Homeless populations are categorised as vulnerable groups (Inter‐Agency Standing Committee, 2020), and public health outbreaks create additional negative impacts and outcomes that are not addressed or easily solved by measures implemented for the general population (Tsai & Wilson, 2020). Furthermore, those experiencing homelessness are often neglected by public health policies and their health and societal inequalities become an ‘invisible burden’ for many developed countries (Banerjee & Bhattacharya, 2020).
Those experiencing homelessness do not fare well in terms of general health, providing them with the likelihood of compounded risks in the face of public health outbreaks. Research has shown that those under the age of 65 who are experiencing homelessness have a mortality rate 5–10 times higher for all causes in comparison to the overall population (Baggett et al., 2013). Those experiencing homelessness often live in low‐capacity shelters or transient locations that likely have no access to hygienic resources which places them at increased risk of obtaining and spreading viruses in comparison to the general population (Leung et al., 2008; Tsai & Wilson, 2020). The previous SARS (Severe Acute Respiratory Syndrome) outbreak has already illustrated this in how homeless populations are more likely to contract, spread and succumb to viruses and provide challenges for detection and tracing (Leung et al., 2008). Leung et al. (2008) suggest that shelter overcrowding, poor ventilation and an accumulation of clients with predispositions to infection increase the risk factors for virus outbreaks. These concerns provide extraordinary considerations for developing and implementing pandemic and outbreak response planning and protocols.
1.1. Rationale and objectives
The goal of this review was to identify the scope of literature at the intersection of homelessness and pandemic response and to synthesise available evidence in these areas to inform community planning and response. This is in line with the Inter‐Agency Standing Committee (2020) recommendation to develop pandemic planning that identifies and addresses the unique circumstances of vulnerable homeless populations. For the public health and homelessness sectors to formulate a pandemic response to the homelessness population, there needs to be accessible evidence to inform a reasonable emergency planning that can cover a variety of potential health threats. This outcome is accomplished by identifying and categorising disease responses and impacts specific to homeless populations through the examination of English language peer‐reviewed publications. Conclusively, this review can set up a baseline to structure future research on the COVID‐19 response and for subsequent efforts in emergency preparedness and planning updates in response to future pandemic crises.
2. METHODS
2.1. Protocol
This study followed a search protocol that was guided by the guidelines established by the PRISMA‐ScR (Tricco et al., 2018) and the ECLIPSE model of search development (Wildridge & Bell, 2002). Several analyses were conducted on data charted from the finalised collection of articles to provide both a quantitative overview of relevant authorship information, as well as a content analysis to identify themes. Both aspects followed the approach of prior reviews conducted by Bradshaw and Graham (2007) and Shier et al. (2011).
2.2. Search strategy
An extensive literature search took place on 18 June 2020 using seven electronic databases (refer to Table 1). The search strategy structure and database selection were advised by an experienced librarian and then further drafted and refined through team discussion.
TABLE 1.
Databases searched
| Databases | Provider |
|---|---|
| PubMed | National Library of Medicine |
| CINAHL Complete | EBSCO |
| Embase | Ovid |
| Social Work Abstracts | EBSCO |
| Sociology Collection | ProQuest |
| APA PsycInfo | EBSCO |
| Web of Science Core Collection—Emerging Sources Citation Index (ESCI) | Clarivate |
Our focus was pandemics and rapid‐spread illnesses such as contagious respiratory diseases, with contact spread [i.e. including tuberculosis (TB) but excluding human immunodeficiency virus (HIV)]. We did not seek out interventions for stable, endemic diseases, out of a desire to capture responses in face of increasing and/or emerging transmission. Search terms reflected a focus on individuals experiencing homelessness within communities and did not intentionally seek out literature on those at risk of homelessness or other unsheltered groups (e.g. refugees). Terms related to prison populations were considered but were removed for being too far afield but likely merit separate analysis and discussion. Search terms were also guided by prior reviews on environmental health conditions and hygiene behaviours in homeless shelters (Moffa et al., 2019), the effectiveness of interventions to reduce homelessness (Munthe‐Kaas et al., 2018), as well as a summary on respiratory infections with people experiencing homelessness (Wrezel, 2009). The resulting base search was as follows:
(‘coronavirus*’ OR ‘COVID’ OR ‘pandemic*’ OR ‘outbreak*’ OR ‘communicable disease*’ OR ‘wuhan virus’ OR ‘corona virus’ OR ‘H1N1’ OR ‘H3N2’ OR ‘H2N2’ OR ‘SARS’ OR ‘Severe acute respiratory syndrome’ OR ‘Zika’ OR ‘Ebola’ OR ‘MERS’ OR ‘Middle East respiratory syndrome’ OR ‘tuberculosis’ OR ‘TB’ OR ‘influenza’ OR ‘flu’ OR ‘pneumonia’).
AND
(‘homeless*’ OR ‘unhoused’ OR ‘unsheltered’ OR ‘roofless*’ OR ‘houseless*’ OR ‘sleeping on the street*’ OR ‘living on the street*’ OR ‘sleeping rough’ OR ‘living rough’ OR ‘addiction treatment*’ OR ‘domestic violence shelter*’ OR ‘women's shelter*’ OR ‘abuse shelter*’ OR ‘night shelter*’ OR ‘no fixed abode’ OR ‘no fixed address’ OR ‘couch surf*’ OR ‘transition hous*’ OR ‘halfway hous*’ OR ‘supported hous*’ OR ‘emergency hous*’ OR ‘emergency shelter*’ OR ‘adequate housing’ OR ‘inadequate housing’ OR ‘street dwell*’ OR ‘improvised dwell*’ OR ‘shelter dwell*’ OR ‘street liv*’ OR ‘marginally housed’ OR ‘precarious housing’ OR ‘precariously housed’ OR ‘without a roof’ OR ‘without shelter’ OR ‘temporary accommodation’ OR ‘emergency accommodation’ OR ‘insecure accommodation’ OR ‘overcrowded accommodation’ OR ‘street person’ OR ‘street people’ OR ‘sleeping out*’ OR ‘rough sleep*’).
The search parameters and limiters varied based on their availability within the searched databases. Our search terms applied to the abstract in each examined database. The timeframe of publication was defined as January 1984 to 2020. Language was limited to only include items in English. Limits of space precluded all genres from being analysed, and we therefore had peer review as an inclusion criterion. Therefore, conference papers, dissertations, manuscripts or additional grey literature were removed—and could be subject to a further analysis, beyond the scope of the present manuscript. See Supporting Information S1 for an example of a full search.
2.3. Inclusion and eligibility criteria
The database searches identified a total of 1,959 articles. These items were uploaded into Covidence for screening. This study took a linear process of reviewing articles. Two reviewers attended to the review process, and an experienced librarian was consulted and involved throughout the review. Initial steps were taken to electronically deduplicate, resulting in 1,001 removals. Reviewers discussed the screening criteria and amended the screening and data extraction process before screening for this review. Inclusion and exclusion criteria were developed iteratively as questions and conflicting decisions arose (see Table 2). The remaining 958 abstracts were reviewed in a linear process by two reviewers. In total, 684 items were excluded during screening for being out of scope. The remaining 274 articles were exported for synthesis and thematic coding following the screening process. During data extraction, an additional 50 items were removed, with 7 identified as additional duplicates and 43 deemed out of scope upon further discussion. A total of 223 articles were reviewed for the final trends and thematic summary presented below (for the full PRISMA flow diagram refer to Figure 1).
TABLE 2.
Inclusion and exclusion criteria
| Include if article: | Exclude if article: |
|---|---|
|
|
Abbreviation: HIV, human immunodeficiency virus.
FIGURE 1.
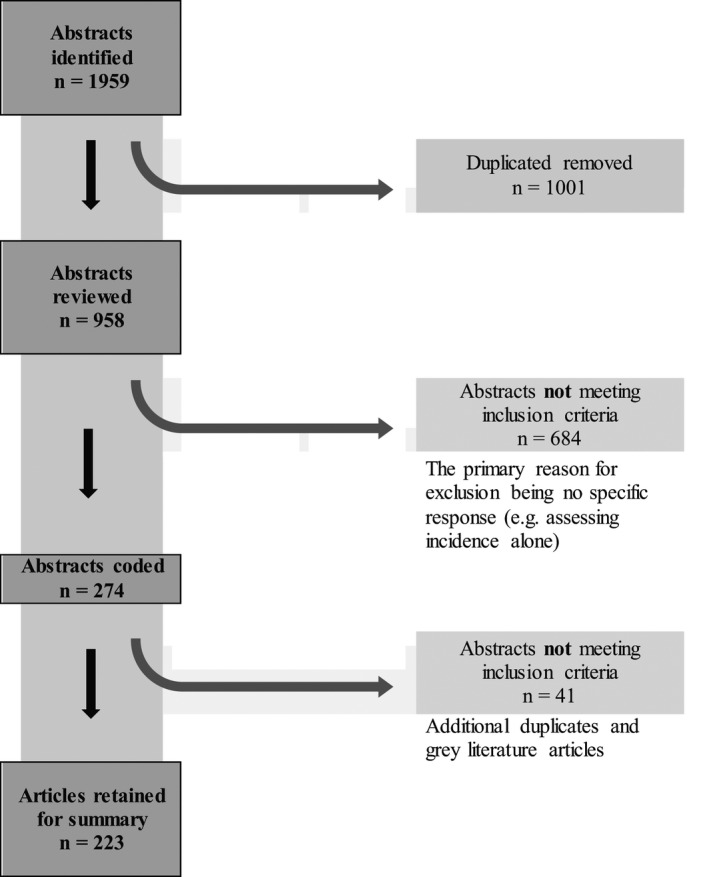
Flow chart of the abstract selection process
2.4. Data charting process
Content analysis methods were followed to extract and synthesise key information (Markoff et al., 1975; Neuendorf, 2002; Weber, 1990). All data were charted in Microsoft Excel. One reviewer independently charted the data for quantitative analysis. The general data items recorded included the following: first author (last name, first initials), year of publication, first author institution, first author country of study and journal of publication. During the charting and screening process, notes were taken on trends and potential themes within abstracts. An initial set of themes was discussed and finalised by reviewers. A similar charting process was then used for thematic coding, with individual charting in Microsoft Excel and subsequent discussion with a second reviewer to establish consensus. Articles coded to a particular theme were then reviewed and summarised in terms of trends and notable details.
3. RESULTS
Abstract screening identified that the overwhelming majority were related to TB, with 137 of the 223 included items mentioning ‘TB’ in the title or abstract and 178 mentioning ‘tuberculosis’. Only three mentioned ‘H1N1’ (subtype of Influenza A), four mentioned ‘SARS’ and 12 mentioned ‘COVID’. Excluded items frequently identified disease prevalence within homeless populations without analysis of a particular response or were discussions of screening or treatment options specific to tuberculosis. Many included items evaluated a particular response or set of responses, with some lengthier case studies such as Leung et al.'s (2008) overview of lessons from SARS. Some included items were themselves reviews on more specific intersections within this literature. See Supporting Information S2 for a full list of retained items.
3.1. Quantitative findings
Figure 2 shows a rise in 5‐year aggregated rates of article publication between 1986 and 2020. We additionally explored the countries of origin of the first authors (see Figure 3). It identified that contributors to English‐language research in this field are, unsurprisingly, typically based in English‐dominant developed countries, producing articles at a respective rate that is roughly proportionate to overall national scientific and technical publication trends available up until 2018 (World Bank, 2020), though Australian first authors were featured less than would be expected. However, first authors overall were based across a diverse mix of 28 nations.
FIGURE 2.
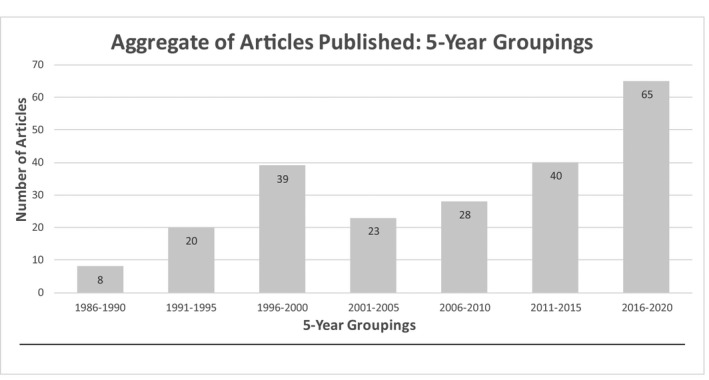
Aggregate of articles published: 5‐year groupings
FIGURE 3.
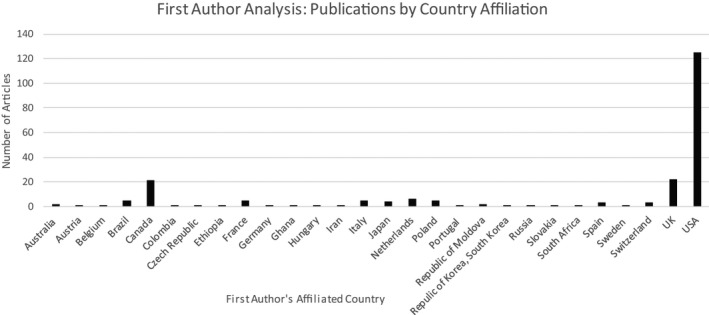
First author analysis: affiliated country
Journals were ranked according to their SCImago Journal Rank (SJR) indicator to broadly understand the value of this topic amongst the research community. The SCImago Journal and Country Rank is a publicly available portal developed from the Scopus® database (Elsevier B.V.) (SCImago, n.d.). Results from the portal are drawn from over 34,100 titles, from more than 5,000 international publishers and country performance metrics from 239 countries worldwide (Leydesdorff et al., 2009). The SJR measurement allows for a more robust understanding of the impact of where the literature is being published in terms of rank and reach (Guerrero‐Bote & Moya‐Anegón, 2012). A total of 124 journals appeared in our final list of retained items, with 37 journals having two or more articles fitting the search criteria, as can be seen in Table 3.
TABLE 3.
Journals with multiple included items, with associated SJR ranks
| Journals with multiple included items a | No. of Incl'd Items | Avg SJR indicator b | SJR quartile range (Avg) c |
|---|---|---|---|
| American Journal of Infection Control | 4 | 1.223 | 1.375 |
| American Journal of Preventive Medicine | 2 | 1.541 | 1.250 |
| American Journal of Public Health | 4 | 2.363 | 1.000 |
|
American Journal of Respiratory and Critical Care Medicine Formerly: American Review of Respiratory Diseases |
7 2 |
3.204 | 1.000 |
| Archives of Internal Medicine | 4 | 3.539 | 1.000 |
| Australian and New Zealand Journal of Public Health | 2 | / | / |
| BMC Infectious Diseases | 2 | 1.574 | 1.000 |
| BMC Public Health | 2 | 1.319 | 1.000 |
| British Medical Journal Open | 3 | 1.390 | 1.000 |
| Canadian Journal of Public Health | 4 | 0.537 | 2.000 |
| CHEST | 3 | 0.621 | 1.000 |
| Clinical Infectious Diseases | 2 | 4.396 | 1.000 |
| Clinical Social Work and Health Intervention | 3 | / | / |
| Emergent Infectious Diseases | 4 | 2.798 | 1.000 |
| Epidemiology and Infection | 2 | 1.349 | 1.500 |
| European Journal of Public Health | 2 | 1.078 | 1.000 |
| International Journal of Infectious Diseases | 2 | 1.354 | 1.333 |
| International Journal of Tuberculosis and Lung Disease | 23 | 1.314 | 1.076 |
| Journal of the American Medical Association | 3 | 5.290 | 1.000 |
| Journal of Addiction Medicine | 2 | / | / |
| Journal of Advanced Nursing | 2 | 0.959 | 1.000 |
| Journal of Community Health Nursing | 3 | 0.334 | 2.500 |
| Journal of Health Care for the Poor and Underserved | 5 | 0.578 | 1.750 |
| Journal of Public Health | 2 | 0.905 | 1.500 |
| Journal of Public Health Management and Practice | 2 | 0.714 | 1.000 |
| Journal of Urban Health | 3 | 1.175 | 1.000 |
| Lancet Infectious Diseases | 2 | 9.963 | 1.000 |
| Morbidity and Mortality Weekly Report (MMWR—CDC) | 6 | 4.996 | 1.000 |
| MMWR—Recommendations and Reports (CDC) | 2 | 9.861 | 1.000 |
| New England Journal of Medicine | 3 | 11.976 | 1.000 |
| PLoS One | 7 | 1.643 | 1.000 |
| Pneumonologia i Alergologia Polska | 2 | / | / |
| Public Health Action | 2 | 0.743 | 2.000 |
| Public Health Nursing | 5 | 0.462 | 1.500 |
| Public Health Reports | 5 | 1.120 | 1.000 |
| Seminars in Respiratory Infections | 3 | / | / |
| Thorax | 2 | 1.010 | 1.000 |
| AVERAGE | 1.778 | 1.378 | |
Abbreviation: SJR, SCImago Journal Rank.
Journals with only one included article have been omitted.
For available years with included items (SJR scores can vary over time).
For available years with included items (ranks can vary over time and differ across associated categories).
Overall, articles were published in journals primarily related to the SJR category of ‘Medicine’ (n = 64), followed by ‘Infectious Disease’ (n = 40) and ‘Public Health, Environmental and Occupational Health’ (n = 40). As can be seen in Table 3 journals frequently publishing on this topic tend to be in the top quartile of their respective categories. There was no obvious trend in rankings over time.
3.2. Qualitative findings
Six major themes were identified within the 223 retained items. Through summation, we sought to circulate relevant information that can inform planning for outbreak‐style diseases, such as the ongoing COVID‐19 crisis. Whilst many interventions were designed specifically for TB or other individual diseases, our focus was to present scalable and generalizable sectoral responses. Themes are presented within distinctive summarised categories, although all individual interventions are best conceived as intersectional and corresponding.
3.2.1. Theme 1: Education and outreach
The Outreach and Education theme served to collect information about how previous efforts were successful in reaching and educating individuals in the homeless sector about COVID‐19 and relay pertinent information about procedures and safety with previous success (Falchook et al., 2000). Articles recommended electronic (e.g. notification systems and emergency numbers), hard copy (e.g. pamphlets, leaflets and letters; Roy et al., 2008) and media (Kitazawa, 1995; Ohtsu et al., 2011) methods of delivering information or a mixture of methods (Filler et al., 2006). With the help of social outreach, another viable method of delivering information was through word of mouth from service providers to clients who are homeless (Craig et al., 2007, 2014). It may also be worthwhile to provide information via newspapers or magazines as these are prominent avenues by which information is accessed by individuals who are homeless (Ohtsu et al., 2011).
Urban TB control may benefit from ‘a coordinated programme of education and training to raise and sustain awareness amongst affected risk groups and communities, front‐line professionals working with high‐risk groups and health and social care professionals’ (van Hest et al., 2014, p. 4) that involves the impacted community in the design and delivery (Joint Tuberculosis Committee of the British Thoracic Society, 2000; van Hest et al., 2014). Education programs can be supported by community health workers (Heuvelings, de Vries, Greve, et al., 2017) or by a peer educator with homelessness experience (Croft et al., 2013). There are suggestions for information to be delivered in a simple, clear and targeted fashion (Roy et al., 2008) and for public health agencies to provide explicit guidelines for service providers to follow (Leung et al., 2008; Mayo et al., 1996). Furthermore, there were recommendations for information and programs to be delivered in a variety of languages to decrease stigma and improve access to services (Hernández Sarmiento et al., 2013; Murti et al., 2015).
At the provider level, detection and management of diagnosed cases of disease can be improved by providing staff with adequate knowledge and education about what to do and who to contact if a case has been diagnosed or suspected (Joint Tuberculosis Committee of the British Thoracic Society, 2000; Leung et al., 2008). Education programs informing case management and care protocols are recommended for front‐line professional working with the homeless sectors and related health and social care professionals (Cousineau, 1997; Hutchison & Quartaro, 1993; Uchimura et al., 2013; van Hest et al., 2014). Specifically, programs should educate providers on how to encourage treatment and immunisation and how to improve patient‐provider alliances (Kong et al., 2020; Metcalfe & Sexton, 2014; Moreau et al., 2012; Peterson Tulsky et al., 1999; Tankimovich, 2013; Vlahov et al., 2007).
3.2.2. Theme 2: Adapting structure of services
Some articles advanced recommendations on shifting the ingrained structures at different levels of societal constructs to facilitate collaboration between institutions, organisations, government and service providers. Literature indicates that communication and collaboration between common goal‐oriented organisations resulted in improved service delivery, access for individuals in the homeless sector (de Queiroga et al., 2018; Brickner et al., 1986; O'Connell, 1991) and that ‘planning for future outbreaks should take into account the need to develop systems that enable rapid two‐way communication between public health officials and homeless service providers’ (Leung et al., 2008, p. 402). An investigation by Dohoo et al. (2020) in one shelter demonstrated the need for a comprehensive, integrated electronic information system. Lashley (2007) discussed the expansion of clinic hours to include evenings and weekends but also touched on a partnership between faith, academic, and governmental institutions: ‘in an environment of scarce resources, such creative and innovative partnerships can improve access to care, remove barriers to treatment, meet the needs of underserved populations and have a positive impact on promoting community health and well‐being’ (p. 38).
Existing infrastructure and systems can be modified to improve continuity of care for homeless individuals, from toll‐free numbers for outreach workers to report and triage people in need (Barbieri, 2020). Barbieri also advocates for an ‘agile referral system’ and a ‘safe transportation system (i.e. equipped vehicle, trained staff with personal protective equipment)’ (p. 296). Harris et al. (2020) and Samuels et al. (2020) both noted a transition of many substance use disorder treatment programs to telemedicine. A frequently raised alternative (or supplement) was mobile services, typically in reference to mobile x‐rays for TB detections, and also mobile health units (Lau & Ferson, 1997; Silva et al., 2018). Badiaga et al. (2008) further posit that ‘street‐ or shelter‐based interventions for targeted populations are the most efficient methods’ (p. 1353), offering specific options that are further discussed in Theme 5: Shelter Protocols.
3.2.3. Theme 3: Screening and contact tracing
Numerous articles identified successful practices in screening and contact tracing for individuals in the homelessness sector, which often adapted to the needs and challenges of a transient and hard to reach population (Janssens et al., 2017; Kong et al., 2002; Li et al., 2003; Macnee et al., 1996; Schieffelbein & Snider, 1988; Southern et al., 1999; Tobolowsky et al., 2020). Unfortunately, those who are most likely to test positive for a disease are those who are least likely to be screened (Hamilton et al., 2018), and screening questionnaires may not be useful for this population (Forman & Kinney, 2003). Symptom screening through a verbal questionnaire has not shown to be promising in the homelessness sector; rather, active screening methods (Barbieri, 2020) such as temperature and other objective measures of screening may be recommended (Baggett et al., 2020; Forman & Kinney, 2003). Baggett et al. (2020) and Kong et al. (2002) recommend screening for all members of shelters and homelessness service organisations for outbreaks where expedited testing and results are encouraged. Offering incentives for screening is also encouraged (Heuvelings, de Vries, Greve, et al., 2017; Heuvelings, de Vries, Grobusch, 2017; Schluger et al., 1995; Southern et al.,1999; Tankimovich, 2013) whilst cooperation between service providers such as street teams and drugs and outreach services improves screening uptake (Alecrim et al., 2016; Badiaga et al., 2008; Heuvelings, de Vries, Greve, et al., 2017). However, an important consideration of screening procedure is confidentiality of the results. One study of TB testing indicated that young women with children did not want to be seen accessing services out of fear that it could impact their custody (Swigart & Kolb, 2004). It has further been outlined that geographically‐informed mobile screening units (Janssens et al., 2017) and screening of homeless individuals presenting to emergency rooms and primary care (Bothamley et al., 2002) may be functional avenues by which to access this hard to reach population (Asch et al., 1998; Goswami et al., 2012; Potter et al., 2016). Similar adaptation may be considered for contact tracing, specifically contact tracing in small group in which many typically reside (Althomsons et al., 2012). Furthermore, contact tracing in the homeless sector may be better served focusing on the locations of the homeless individual, rather than specific names of contacts (Barnes et al., 1997; Li et al., 2003).
3.2.4. Theme 4: Transmission prevention strategies
Transmission can be a result of both environmental and behavioural factors and includes the occupational exposure of staff (Schieffelbein & Snider, 1988; Wurtz et al., 1996), due to its congregate nature (Munn et al., 2015). Bodkin et al. (2020) note the necessity during COVID‐19 for shelter restructuring to allow physical distancing, testing and isolation—items further discussed in Theme 5. Prevention of spread may also be benefitted through directly observed treatment, the use of masks, hygienic bedding (Badiaga et al., 2008; Moffa et al., 2019), improved ventilation in crowded spaces and engineering control strategies for airborne infectious diseases (Babatsikou & Zavitsanou, 2009; Barbieri, 2020; Brickner & McAdam, 1995; Doshani et al., 2019; Nardell, 1989).
Engineering strategies include the use of ultraviolet light germicidal irradiation and ultraviolet light germicidal irradiation of upper room air, filters and consideration of factors including aerosol generation, particle size and concentration, organism viability, infectivity and virulence, airflow and climate (Azevedo et al., 2015; Centers for Disease Control, 1992; Coffey et al., 2009; Cole & Cook, 1998; McMillan Jackson, 1996; Moffa et al., 2019; Moreau et al., 2012; Nardell, 1989; Schieffelbein & Snider, 1988). The mobility of the homeless populations creates conditions that are conducive to the spread of TB and all other easily communicable diseases, related to both the dynamic and changing nature of contacts as well as one's control over contact (Ali, 2010).
Existing health disparities may also be linked to risk, and collaboration between health services and shelter is encouraged (Schieffelbein & Snider, 1988). Accordingly, both Amiri et al. (2018) and Torres (1990) advocate for special programs to improve the healthy behaviour of the homeless population, such as where Uchimura et al. (2013) observed that programs to enhance health and nutrition status may benefit TB prevention amongst the elderly. However, another identified factor was personal responsibility, with Rayner (2000) noting that ‘healthcare professionals are becoming more prescriptive in their approach which is relinquishing the homeless population from taking responsibility for their own health care’ (p. 871). The need for ‘prompt and adequate treatment’ is balanced with a need for adherence when it comes to issues of drug resistance (Carnie et al., 1998)—both aspects are discussed in Theme 6: Treatment, adherence and vaccination.
3.2.5. Theme 5: Shelter protocols
The included items relayed pertinent, detailed recommendations for maintaining health and safety in shelters related to both patrons and staff. The main tangible recommendations relevant to shelters included topics such as service provision, environment, education, staff and planning (Please refer to Supporting Information S3). Bodkin et al. (2020) offer a case review of the actions taken in Hamilton, Canada, where collaboration actually increased the number of beds during COVID‐19 (i.e. across pre‐existing shelters, an additional temporary shelter and three hotel sites), as well as using existing space for short‐term isolation during testing and testing on‐site for everyone who failed the symptom screener. Shelters should have plans in place for staff surveillance (Di Renzi et al., 2012), staff shortages (Leung et al., 2008), screening and preventive therapy for eligible persons (Curtis, 2016).
Hwang et al. (2008) advocate that policies be implemented following an outbreak to ‘strongly encourage’ individuals to remain at their current shelter until the situation has been managed. Further recommendations are for public health agencies to work with shelters to ensure that clients' attendance records contain the necessary information to facilitate contact tracing during public health investigations (Munn et al., 2015). Badiaga et al. (2008) advocate for a variety of street or shelter based interventions, including, as needed and relevant, ‘education, free condom distribution, syringe and needle prescription programs, chest radiography screening for tuberculosis, directly observed therapy for tuberculosis treatment, improvement of personal clothing and bedding hygiene and widespread use of ivermectin for scabies and body louse infestation’ (p. 1353). Moreover, the authors support an inclusion of a holistic vaccination program and encourage systematic vaccination against hepatitis B virus, hepatitis A virus, influenza, streptococcus pneumoniae and diphtheria (Badiaga et al., 2008). However, such efforts must be mindful of health‐seeking behaviors and the possibility of minimal engagement amongst target populations (see Connors et al., 2017 for one example and associated recommendations).
3.2.6. Theme 6: Treatment, adherence, and vaccination
A key goal of this review was to highlight protocols to inform best practices surrounding access to treatment, treatment itself and adherence to treatment of pandemic‐related diseases. Often, individuals who are homeless will wait till the disease is in advanced stages prior to seeking treatment (Moreau et al., 2012). Incentives are understood to be beneficial for treatment (Ciobanu et al., 2014; Nyamathi et al., 2008) and management (i.e. screening and follow up appointments) of pandemic‐related disease in the homeless population, which could include monetary (Heuvelings, de Vries, Greve, et al., 2017; Hwang et al., 2005) and simple low‐cost incentives or compensation such as food, lodging (Kim et al., 2019; Lo Bue et al., 1999; Tulsky et al., 2000) and care (Diez et al., 1996; Gärden et al., 2013; Kim et al., 2019; Pilote et al., 1996; Riquelme‐Miralles et al., 2019; Tankimovich, 2013; Tulsky et al., 2004). Directly observed treatment short‐course (DOTS) could be a useful program that has been successfully implemented in the homeless sectors, particularly noncompliant individuals (Barclay et al., 1995; Gasner et al., 1999; Gupta et al., 2015; Kawatsu et al., 2013; Onwubiko et al., 2019). Rendleman's (1999) study examined a community program requiring users of public facilities to carry cards certifying their compliance with a tuberculosis program, resulting in a large reduction in both TB as well as in cost.
The competing demands in the day to day life of a homeless individual can be exacerbated by additional issues concerning money, immigration and the law and substance use (Onwubiko et al., 2019; Potter et al., 2016). Mandated treatment in past pandemic‐related illness has only been possible when the individual is actively infectious and will repeatedly not abide by social policy, health care directives or authority (Miller et al., 2006; Rendleman, 1999). Evidently, the denial of personal freedom is not to be taken lightly (Joint Tuberculosis Committee of the British Thoracic Society, 2000), and mandated treatment should only be enforced if it is absolutely necessary (Lerner, 1996).
A collaborative, multi‐agency approach (Buechler et al., 2020), including authorities and public health officials, community partners (Doroshenko et al., 2012) and peer mentors (Heuvelings et al., 2018; Pilote et al., 1996), could facilitate treatment uptake and adherence and enhance the crucial continuity of care (de Vries et al., 2017; Heuvelings, de Vries, Greve, et al., 2017; Joint Tuberculosis Committee of the British Thoracic Society, 2000; Potter et al., 2016). Brainard et al. (1997) comment that ‘raising therapy completion rates to acceptable levels may require additional social services … and enforceable legal remedies for noncompliance’ (p. 381). Recent literature has highlighted the success and need for a shift to a holistic model which takes into consideration not only the imminent threat of the diagnosed pandemic‐related disease but also of comorbid factors such as substance misuse (Brudney & Dobkin, 1992; Lesnic et al., 2016), mental health (Lau & Ferson, 1997) or HIV (Auer et al., 2020; Berg et al., 2005; Craig et al., 2007; Herdics et al., 2017; Hirsch‐Moverman et al., 2010). This may promote compliance and can serve to decrease the risk of transmission or reinfection and improve treatment outcomes overall. Tankimovich (2013) further comments on targeting cultural values for homeless and immigrant populations.
There are some recommendations for the successful administration of vaccination to homeless populations. First, and foremost, vaccinations should be free of charge, as this has been noted as one of the biggest barriers to uptake in the homeless sector and facilitated by improved access to care (Rendleman, 1999), drop‐in clinics in shelters (Buccieri & Gaetz, 2013; Kaplan‐Weisman et al., 2018) and good case management (Haddad et al., 2005). It is important to note that some individuals may be resistant to vaccination (Nwana et al., 2019); thus, incentives and education program for both service providers and patrons are encouraged to facilitate alliance (Kaplan‐Weisman et al., 2018; Kawatsu et al., 2013). Vaccination strategies such as ‘blitzing’ or offering a large cohort of homeless individuals the vaccination have been successful in decreasing diseases incidence such as influenza (Weatherill et al., 2004). Systematic vaccination against hepatitis B, hepatitis A, influenza, pneumococcus and diphtheria is strongly recommended for homeless individuals who are receiving outbreak related vaccinations (Badiaga et al., 2008). The Advisory Committee on Immunisation Practices Hepatitis Vaccines Work Group likewise recommends routine immunisation for all persons experiencing homelessness aged 1 year and older (Doshani et al., 2019). Partnerships to administer vaccinations have shown to be successful, such as in Metcalfe and Sexton's (2014) study of a social marketing education program developed by nursing students, and Lashley (2007) on a joint program between faith‐based organisation, an academic institution and local government. The latter, however, highlighted the importance of sharing proper documentation and records to accurately track health progress.
4. DISCUSSION
This review illustrates that the current breadth of academic literature on homeless populations has thus far focused on TB rather than diseases that are more recent and closely related to COVID‐19—such as SARS or H1N1. However, the similarities within the mode of transmission from TB and susceptibility of outbreak amongst homelessness populations make it a viable health crisis to learn from. As the World Health Organization (2020c) explains, ‘people ill with COVID‐19 and TB show similar symptoms such as cough, fever and difficulty breathing. Both diseases attack primarily the lungs and although both biological agents transmit mainly via close contact’ (p. 2). Certainly, as further publications on COVID‐19 pandemic response become available, future reviews of this nature may shift or find further support for the themes addressed here. Additionally, whilst many of the articles reviewed here outline possible routes for pandemic response amongst homeless populations, we only uncovered a few that formally evaluated the implementation and success of such practices (e.g. Leung et al., 2008). In which case, this review provides further guidance in relation to the existing broad suggestions from global agencies such as the World Health Organization (2020b) or the Inter‐Agency Standing Committee (2020), although further research would be required to evaluate best practices and planning.
4.1. Outbreak and pandemic response and planning
The Inter‐Agency Standing Committee (2020) suggests that special attention needs to be paid for communicating pandemic guidelines and response to vulnerable populations and that clear and continued two‐way communication is key. The Inter‐Agency Standing Committee (IASC) nonetheless provides this recommendation without any particular strategies to accomplish this task amongst homeless populations. This review supports the IASC's suggestion for communication and begins to expand on it by offering some tangible routes to accomplish this. Authors have identified that there is a need to extend outreach to identify, educate and communicate with hard‐to‐reach groups (Craig et al., 2014; Vlahov et al., 2007), which can possibly be accomplished through community posters and public announcement at homeless shelters (Filler et al., 2006), small educational groups using a combination of video and written learning tools (Kitazawa, 1995) and the creation of simple language leaflets (Samuels et al., 2020). However, to establish the best routes of communication amongst various communities, there needs to be some knowledge of, and collaboration with, the local homeless populations. In principle, all communication should consider cultural, language and literacy issues (van Hest et al., 2014) and should be directed in a clear and targeted manner (Roy et al., 2008).
Outbreak planning and response cannot ignore issues with comorbidity amongst the homeless. There were quite a few articles that discussed the issue of comorbidities during an outbreak and often included HIV or diabetes intersections with tuberculosis. Whilst articles that had a primary focus on HIV outbreaks were excluded from this review, we found that several articles concerned with tuberculosis also discussed HIV (Amiri et al., 2018; Azevedo et al., 2015; Bernardo, 1991; Tulsky et al., 2000). For example, both Tulsky et al. (2000) and Bernardo (1991) discuss HIV and tuberculosis in relation to comorbidity and found that comorbidity is much higher for those experiencing homelessness in comparison to the general population. It is not unusual for homeless individuals to maintain an underlying myriad of illnesses, which could leave them more susceptible to virus obtainment, transmission and mortality (Leung et al., 2008). This only further supports the recommendation from Tulsky et al. (2000) that homeless populations should be screened for comorbidities when treated concurrently. Additionally, because people experiencing homelessness are at increased risk of infection, there needs to adequate plans for tracing, prevention and intervention that are specific for these populations.
Prevention, intervention and tracing becomes difficult for transient groups, as there is no easy route to contact them and their lack of permanent housing creates barriers for public health strategies that would more readily apply to the general population. Therefore, pandemic planning considerations for such groups need to include flexible methods for screening, communication and intervention. Harris et al. (2020) identify telemedicine as a valuable route to providing health and addiction services to homeless groups during a pandemic; Badiaga et al. (2008) suggest that interventions and services should be street or shelter based, whilst Brickner et al. (1986) showed support for the use of healthcare outreach teams made up of physicians and nurses that provide on‐site services. These forms on site healthcare have the potential to address other health issues and comorbidities, especially in relation to mental health and addictions as found by Harris et al. (2020). Our position supports Lashley (2007), in that successful pandemic planning and services will require great collaboration amongst healthcare workers, government and service agencies.
The World Health Organization (2003) early on pointed to the difficulty with treatment adherence generally, although especially amongst those experiencing homelessness. This problem is still appropriate since a current lack of understanding for successful treatment delivery and adherence strategies amongst homeless populations still exists (Johnson et al., 2020). The suggestions for adherence outlined in this review further contribute to mitigating the current lack of understanding in this area, particularly the support for the use of monetary or housing incentives to encourage and improve public health program adherence (Pilote et al., 1996; Tulsky et al., 2000) and the offering of peer health advisors, which showed promise in supporting treatment obedience within homelessness groups (Pilote et al., 1996).
Whilst policy considerations were not the express focus of this review, they did come up and represent a key enabling and/or inhibiting factor at regional (Bartels et al., 2020; Harris et al., 1994; Mayo et al., 1996), national (Bloch et al., 1996; Gupta et al., 2015; Miller et al., 2006; Ohkado et al., 2005) and international (Campbell et al., 2019; Corburn et al., 2020; Rimawi et al., 2014) levels. A policy shift allowing the integration of drug, alcohol and HIV services within existing homelessness services may address complex and the co‐morbid needs that can impact treatment (Craig & Zumla, 2015). Furthermore, housing and relevant support services may not only impact therapy completion rates but may also reduce hospital utilisation (Marks et al., 2000). Overall, Alberti et al. (2020) argue for a health equity framework to pandemic preparedness, grounded in meaningful community engagement that, whilst recognising the fundamental causes of social and health inequity, has a clear focus on upstream and midstream preparedness and downstream rapid response efforts that put social and health equity at the forefront (p. 4).
4.2. Brief considerations for COVID‐19
Whilst the goal of this study was to focus on uncovering useful practices and guidance for pandemics and outbreaks, in general, this review does contain relevant considerations for COVID‐19. Canadian governments at all levels have been using hotels as temporary emergency shelters for people experiencing homelessness, which has seen some great success (Lupton, 2020). Not only could other national government implement similar practices, but we would also stress that this continues to be offered until the pandemic is settled. As vaccines become available, continual monitoring, testing and vaccination of homeless groups will become difficult if they face housing instability and associated increases in transience. Furthermore, housing has shown to be an effective incentive for health program and vaccination adherence (Pilote et al., 1996; Tulsky et al., 2000), and as such, continuous offering of temporary hotel housing likely offers increased success for tracing, vaccination and public health adherence.
The continued use of hotels would also free up much needed space for shelters to adapt to public health guidelines set out by the World Health Organization (2020b), such as creating space for safe social distancing and the isolation of positive or suspected cases. More specifically to shelter space, engineered controls also need to be considered. Shelters are often crowded spaces with poor ventilation, with residents that often hold poor hygienic practices. Therefore, COVID‐19 planning should include provisions for the unique characteristics of shelters and its users. Some methods identified within this review include the installation of adequate ventilation and ultraviolet light (Moffa et al., 2019), providing clean cloths, hygienic bedding (Badiaga et al., 2009) and masks (Brickner & McAdam, 1995). Public health planning and pandemic response need to consider the barriers to implantation amongst shelters and the homeless population. Furthermore, as many of these changes and considerations are costly, there needs to be consistent and accessible funding available to those who need it.
This review presents a need for future studies to evaluate the implementation and success of current pandemic response practices in relation to people experiencing homelessness. As governments and organisations plan for the current and future pandemics, they will need social scientists to engage in these facets to provide evidence‐based policy and best practices. The scope of the current literature offers plenty of methods for pandemic response and planning, although there are insufficient evaluative and assessment studies that identify the effectiveness of such suggestions. Therefore, research to address this gap is both paramount and opportune considering the future developments and policies to come.
4.3. Limitations and delimitations
This review was designed to provide a snapshot of academic literature pertaining to the intersections of people experiencing homelessness and pandemic response and planning. This was accomplished through the use of terms specific to homelessness, pandemics and rapid‐spread illnesses such as contagious respiratory diseases with contact spread. Abstract‐based reviews carry potential limitations in their capacity to fully capture concepts as well as the capacity to synthesise knowledge into a cohesive and usable format. The inclusion of other terms may alter the identified literature and reshape implications for practice and research (i.e. policy, intervention, HIV/AIDS and vulnerable groups). There is also the possibility that expanding the search fields to include titles, keywords and/or full text would provide additional context, but we believe the abstract‐level search was enough to identify our high‐level themes. Additionally, an inclusion of other forms of literature (e.g., government documents and NGO reports) would provide supporting information pertaining to the discussions offered in this review. In terms of methodology, we also realise that qualitative thematic analysis is subjective, which leaves room for bias, missed areas of importance or differences of interpretation. Lastly, a broader—or narrower—range of databases may be considered for future systematic reviews, depending on the scope and intent. Furthermore, since our search was initiated in June 2020, additional articles related to COVID‐19 will continue to be produced and may offer additional support or new avenues for pandemic response as it relates to the homelessness response literature outlined in this review. This may warrant a review of its own, particularly on the current, and largest, vaccination campaign in history. We invite researchers to replicate or advance the findings presented in this review.
5. CONCLUSION
Generally, past outbreaks and the current COVID‐19 pandemic illustrate the various public health response challenges—especially amongst vulnerable groups. Whilst this review engages with the Inter‐Agency Standing Committee (2020) recommendation to develop pandemic planning that identifies and addresses the unique circumstances of vulnerable homeless populations, the breadth and depth of reviews such as this are dependent on the quantity and quality of the available literature. Therefore, the limited existing literature specific to homelessness in this review illustrates a need for more academic research into the intersections of pandemics and homelessness—specifically a call to social scientists to conduct studies that evaluate pandemic response and planning. Nonetheless, this review offers timely considerations for pandemic response and planning amongst homeless populations during the current COVID‐19 pandemic and can facilitate future research in this area. Furthermore, as COVID‐19 vaccinations become available, the included discussions of treatment delivery and adherence will become more relevant.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
Supporting information
Supplementary Material
Supplementary Material
Supplementary Material
Babando J, Quesnel DA, Woodmass K, Lomness A, Graham JR. Responding to pandemics and other disease outbreaks in homeless populations: A review of the literature and content analysis. Health Soc Care Community. 2022;30:11–26. 10.1111/hsc.13380
Jordan Babando and Danika A. Quesnel contributed equally to this study.
Funding information
This paper was funded by the University of British Columbia Eminence programme and the Social Sciences and Humanities Research Council. Funders played no role in any aspect of study design, data collection and analysis, nor decision to publish and where to publish, nor preparation of any manuscript.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analysed in this study. For further data inquiry, please contact the corresponding author.
REFERENCES
- Alberti, P. M. , Lantz, P. M. , & Wilkins, C. H. (2020). Equitable pandemic preparedness and rapid response: Lessons from COVID‐19 for pandemic health equity. Journal of Health Politics, Policy and Law, 45(6), 921–935. 10.1215/03616878-8641469 [DOI] [PubMed] [Google Scholar]
- Alecrim, T. F. D. A. , Mitano, F. , Reis, A. A. D. , Roos, C. M. , Palha, P. F. , & Protti‐Zanatta, S. T. (2016). Experience of health professionals in care of the homeless population with tuberculosis. Revista Da Escola De Enfermagem Da USP, 50(5), 808–815. 10.1590/s0080-623420160000600014 [DOI] [PubMed] [Google Scholar]
- Ali, S. H. (2010). Tuberculosis, homelessness, and the politics of mobility. Canadian Journal of Urban Research, 19(2), 80–107. [Google Scholar]
- Althomsons, S. P. , Kammerer, J. S. , Shang, N. , & Navin, T. R. (2012). Using routinely reported tuberculosis genotyping and surveillance data to predict tuberculosis outbreaks. PLoS One, 7(11), e48754. 10.1371/journal.pone.0048754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amiri, F. B. , Doosti‐Irani, A. , Sedaghat, A. , Fahimfar, N. , & Mostafavi, E. (2018). Knowledge, attitude, and practices regarding HIV and TB among homeless people in Tehran, Iran. International Journal of Health Policy and Management, 7(6), 549–555. 10.15171/ijhpm.2017.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asch, S. , Leake, B. , Knowles, L. , & Gelberg, L. (1998). Tuberculosis in homeless patients: Potential for case finding in public emergency departments. Annals of Emergency Medicine, 32(2), 144–147. 10.1016/S0196-0644(98)70128-3 [DOI] [PubMed] [Google Scholar]
- Auer, C. , Mazitov, R. , Makhmudov, A. , Pirmahmadzoda, B. , Skrahina, A. , Dobre, A. , Sécula, F. , Bosch‐Capblanch, X. , Van den Boom, M. , Migliori, G. B. , Mdivani, N. , & Yassin, M. A. (2020). Factors contributing to drug‐resistant tuberculosis treatment outcome in five countries in the Eastern Europe and Central Asia region. Monaldi Archives for Chest Disease, 90(1), 10.4081/monaldi.2020.1235 [DOI] [PubMed] [Google Scholar]
- Azevedo, M. J. , Conwill, D. E. , Lawrence, S. , Jackson, A. , Bhuiyan, A. R. , Hall, D. , Anderson, B. , Franklin, D. , Brown, D. , Wilkerson, P. , & Beckett, G. (2015). Tuberculosis containment among the homeless in metropolitan Jackson, Mississippi. Journal of the Mississippi State Medical Association, 56(8), 243–248. [PubMed] [Google Scholar]
- Babatsikou, F. , & Zavitsanou, A. (2009). Homeless: A high risk group for ectoparasites infestation and arthropod‐borne diseases. Review of Clinical Pharmacology and Pharmacokinetics, International Edition, 23(2), 93–98. [Google Scholar]
- Badiaga, S. , Raoult, D. , & Brouqui, P. (2008). Preventing and controlling emerging and reemerging transmissible diseases in the homeless. Emerging Infectious Diseases, 14(9), 1353–1359. 10.3201/eid1409.082042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badiaga, S. , Richet, H. , Azas, P. , Zandotti, C. , Rey, F. , Charrel, R. , Benabdelkader, E. , Drancourt, M. , Raoult, D. , & Brouqui, P. (2009). Contribution of a shelter‐based survey for screening respiratory diseases in the homeless. European Journal of Public Health, 19(2), 157–160. 10.1093/eurpub/ckn142 [DOI] [PubMed] [Google Scholar]
- Baggett, T. P. , Hwang, S. W. , O'Connell, J. J. , Porneala, B. C. , Stringfellow, E. J. , Orav, E. J. , Singer, D. E. , & Rigotti, N. A. (2013). Mortality among homeless adults in Boston: Shifts in causes of death over a 15‐year period. JAMA Internal Medicine, 173(3), 189–195. 10.1001/jamainternmed.2013.1604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baggett, T. P. , Racine, M. W. , Lewis, E. , De Las Nueces, D. , O'Connell, J. J. , Bock, B. , & Gaeta, J. M. (2020). Addressing COVID‐19 among people experiencing homelessness: Description, adaptation, and early findings of a multiagency response in Boston. Public Health Reports, 135(4), 435–441. 10.1177/0033354920936227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee, D. , & Bhattacharya, P. (2020). The hidden vulnerability of homelessness in the COVID‐19 pandemic: Perspectives from India. International Journal of Social Psychiatry. Advance online publication. 10.1177/0020764020922890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbieri, A. (2020). CoViD‐19 in Italy: Homeless population needs protection. Recenti Progressi in Medicina, 111(5), 295–296. 10.1701/3366.33409 [DOI] [PubMed] [Google Scholar]
- Barclay, D. M. , Richardson, J. P. , & Fredman, L. (1995). Tuberculosis in the homeless. Archives of Family Medicine, 4(6), 541–546. 10.1001/archfami.4.6.541 [DOI] [PubMed] [Google Scholar]
- Barnes, P. F. , Yang, Z. , Preston‐Martin, S. , Pogoda, J. M. , Jones, B. E. , Otaya, M. , Eisenach, K. D. , Knowles, L. , Harvey, S. , & Cave, M. D. (1997). Patterns of tuberculosis transmission in Central Los Angeles. JAMA, 278(14), 1159–1163. 10.1001/jama.1997.03550140051039 [DOI] [PubMed] [Google Scholar]
- Bartels, S. J. , Baggett, T. P. , Freudenreich, O. , & Bird, B. L. (2020). COVID‐19 emergency reforms in Massachusetts to support behavioral health care and reduce mortality of people with serious mental illness. Psychiatric Services, 71(10), 1078–1081. 10.1176/appi.ps.202000244 [DOI] [PubMed] [Google Scholar]
- Berg, J. , Nyamathi, A. , Christiani, A. , Morisky, D. , & Leake, B. (2005). Predictors of screening results for depressive symptoms among homeless adults in Los Angeles with latent tuberculosis. Research in Nursing & Health, 28(3), 220–229. 10.1002/nur.20074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardo, J. (1991). Tuberculosis: A disease of the 1990s. Hospital Practice, 26(10), 195–222. 10.1080/21548331.1991.11705315 [DOI] [PubMed] [Google Scholar]
- Bloch, A. B. , Onorato, I. M. , Ihle, W. W. , Hadler, J. L. , Hayden, C. H. , & Snider, D. E. (1996). The need for epidemic intelligence. Public Health Reports, 111(1), 26–31. [PMC free article] [PubMed] [Google Scholar]
- Bodkin, C. , Mokashi, V. , Beal, K. , Wiwcharuk, J. , Lennox, R. , Guenter, D. , Smieja, M. , Bulir, D. , Chong, S. , & O'Shea, T. (2020). Pandemic planning in homeless shelters: A pilot study of a coronavirus disease 2019 (COVID‐19) testing and support program to mitigate the risk of COVID‐19 outbreaks in congregate settings. Clinical Infectious Diseases. Advance online publication. 10.1093/cid/ciaa743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bothamley, G. H. , Rowan, J. P. , Griffiths, C. J. , Beeks, M. , McDonald, M. , Beasley, E. , van den Bosch, C. , & Feder, G. (2002). Screening for tuberculosis: The port of arrival scheme compared with screening in general practice and the homeless. Thorax, 57(1), 45–49. 10.1136/thorax.57.1.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradshaw, C. , & Graham, J. (2007). Localization of social work practice, education, and research: A content analysis. Social Development Issues, 29(2), 92–111. [Google Scholar]
- Brainard, D. , Hyslop, N. E. , Mera, R. , & Churchill, J. (1997). Long‐term outcome of inpatients with tuberculosis assigned to outpatient therapy at a local clinic in New Orleans. Journal of Investigative Medicine, 45(6), 381–387. [PubMed] [Google Scholar]
- Brickner, P. W. , & McAdam, J. M. (1995). Tuberculosis, HIV disease, and directly observed therapy. Journal of Public Health Management and Practice, 1(4), 52–54. 10.1097/00124784-199500140-00012 [DOI] [PubMed] [Google Scholar]
- Brickner, P. W. , Scanlan, B. C. , Conanan, B. , Elvy, A. , McAdam, J. , Scharer, L. K. , & Vicic, W. J. (1986). Homeless persons and health care. Annals of Internal Medicine, 104(3), 405–409. 10.7326/0003-4819-104-3-405 [DOI] [PubMed] [Google Scholar]
- Brudney, K. , & Dobkin, J. (1992). Resurgent tuberculosis in New York City: Human immunodeficiency virus, homelessness, and the decline of tuberculosis control programs. Journal of Public Health Policy, 13(4), 435–450. 10.2307/3342533 [DOI] [PubMed] [Google Scholar]
- Buccieri, K. , & Gaetz, S. (2013). Ethical vaccine distribution planning for pandemic influenza: Prioritizing homeless and hard‐to‐reach populations. Public Health Ethics, 6(2), 185–196. 10.1093/phe/pht005 [DOI] [Google Scholar]
- Buechler, C. R. , Ukani, A. , Elsharawi, R. , Gable, J. , Petersen, A. , Franklin, M. , Chung, R. , Bell, J. , Manly, A. , Hefzi, N. , Carpenter, D. , & Bryce, R. (2020). Barriers, beliefs, and practices regarding hygiene and vaccination among the homeless during a hepatitis A outbreak in Detroit, MI. Heliyon, 6(3), e03474. 10.1016/j.heliyon.2020.e03474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, J. R. , Dowdy, D. , & Schwartzman, K. (2019). Treatment of latent infection to achieve tuberculosis elimination in low‐incidence countries. PLoS Med, 16(6), e1002824. 10.1371/journal.pmed.1002824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnie, J. , Randall, M. , & Ng, M. M. (1998). Tuberculosis. The old and the new. Australian Family Physician, 27(7), 615–618. [PubMed] [Google Scholar]
- Centers for Disease Control . (1992). Prevention and control of tuberculosis among homeless persons: Recommendations of the Advisory Council for the Elimination of Tuberculosis. Morbidity and Mortality Weekly Report, 41(RR‐5). Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/00019922.htm [PubMed]
- Ciobanu, A. , Domente, L. , Soltan, V. , Bivol, S. , Severin, L. , Plesca, V. , Van den Bergh, R. , Kumar, A. M. V. , & de Colombani, P. (2014). Do incentives improve tuberculosis treatment outcomes in the Republic of Moldova? Public Health Action, 4(Suppl 2), S59–63. 10.5588/pha.14.0047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey, C. C. , Hudnall, J. B. , & Martin, S. B. (2009). Improving the environmental controls at a homeless shelter to assist in reducing the probability of airborne transmission of mycobacterium tuberculosis: A case study. Indoor and Built Environment, 18(2), 168–182. 10.1177/1420326X09103008 [DOI] [Google Scholar]
- Cole, E. C. , & Cook, C. E. (1998). Characterization of infectious aerosols in health care facilities: An aid to effective engineering controls and preventive strategies. American Journal of Infection Control, 26(4), 453–464. 10.1016/S0196-6553(98)70046-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connors, W. J. , Hussen, S. A. , Holland, D. P. , Mohamed, O. , Andes, K. L. , & Goswami, N. D. (2017). Homeless shelter context and tuberculosis illness experiences during a large outbreak in Atlanta, Georgia. Public Health Action, 7(3), 224–230. 10.5588/pha.17.0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corburn, J. , Vlahov, D. , Mberu, B. , Riley, L. , Caiaffa, W. T. , Rashid, S. F. , Ko, A. , Patel, S. , Jukur, S. , Martínez‐Herrera, E. , Jayasinghe, S. , Agarwal, S. , Nguendo‐Yongsi, B. , Weru, J. , Ouma, S. , Edmundo, K. , Oni, T. , & Ayad, H. (2020). Slum health: Arresting COVID‐19 and improving well‐being in urban informal settlements. Journal of Urban Health, 97(3), 348–357. 10.1007/s11524-020-00438-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cousineau, M. R. (1997). Health status of and access to health services by residents of urban encampments in Los Angeles. Journal of Health Care for the Poor and Underserved, 8(1), 70–82. 10.1353/hpu.2010.0378 [DOI] [PubMed] [Google Scholar]
- Craig, G. M. , Booth, H. , Story, A. , Hayward, A. , Hall, J. , Goodburn, A. , & Zumla, A. (2007). The impact of social factors on tuberculosis management. Journal of Advanced Nursing, 58(5), 418–424. 10.1111/j.1365-2648.2007.04257.x [DOI] [PubMed] [Google Scholar]
- Craig, G. M. , Joly, L. M. , & Zumla, A. (2014). ‘Complex’ but coping: Experience of symptoms of tuberculosis and health care seeking behaviours – A qualitative interview study of urban risk groups, London, UK. BMC Public Health, 14(1), 618. 10.1186/1471-2458-14-618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig, G. M. , & Zumla, A. (2015). The social context of tuberculosis treatment in urban risk groups in the United Kingdom: A qualitative interview study. International Journal of Infectious Diseases, 32, 105–110. 10.1016/j.ijid.2015.01.007 [DOI] [PubMed] [Google Scholar]
- Croft, L. A. , Hayward, A. C. , & Story, A. (2013). Tuberculosis peer educators: Personal experiences of working with socially excluded communities in London. The International Journal of Tuberculosis and Lung Disease, 17(10), 36–40. 10.5588/ijtld.13.0309 [DOI] [PubMed] [Google Scholar]
- Curtis, J. (2016). Impact of x‐ray screening programmes for active tuberculosis in homeless populations: A systematic review of original studies. Journal of Public Health, 38(1), 106–114. 10.1093/pubmed/fdv014 [DOI] [PubMed] [Google Scholar]
- de Queiroga, R. P. F. , de Sá, L. D. , & Gazzinelli, A. (2018). A tuberculose na população em situação de rua: Desempenho de profissionais da atenção primária. Revista Da Rede De Enfermagem do Nordeste, 19, e32463. 10.15253/2175-6783.20181932463 [DOI] [Google Scholar]
- de Vries, S. G. , Cremers, A. L. , Heuvelings, C. C. , Greve, P. F. , Visser, B. J. , Bélard, S. , Janssen, S. , Spijker, R. , Shaw, B. , Hill, R. A. , Zumla, A. , van der Werf, M. J. , Sandgren, A. , & Grobusch, M. P. (2017). Barriers and facilitators to the uptake of tuberculosis diagnostic and treatment services by hard‐to‐reach populations in countries of low and medium tuberculosis incidence: A systematic review of qualitative literature. The Lancet Infectious Diseases, 17(5), e128–e143. 10.1016/S1473-3099(16)30531-X [DOI] [PubMed] [Google Scholar]
- Di Renzi, S. , Tomao, P. , Martini, A. , Capanna, S. , Rubino, L. , D'Amico, W. , Tomei, F. , Visca, P. , & Vonesch, N. (2012). Screening for tuberculosis among homeless shelter staff. American Journal of Infection Control, 40(5), 459–461. 10.1016/j.ajic.2011.07.002 [DOI] [PubMed] [Google Scholar]
- Diez, E. , Claveria, J. , Serra, T. , Caylà, J. A. , Jansà, J. M. , Pedro, R. , & Villalbi, J. R. (1996). Evalution of a social health intervention among homeless tuberculosis patients. Tubercle and Lung Disease, 77(5), 420–424. 10.1016/S0962-8479(96)90114-8 [DOI] [PubMed] [Google Scholar]
- Dohoo, C. , Stuart, R. , Finkelstein, M. , Bradley, K. , & Gournis, E. (2020). Risk factors associated with group A streptococcus acquisition in a large, urban homeless shelter outbreak. Canadian Journal of Public Health, 111(1), 117–124. 10.17269/s41997-019-00258-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doroshenko, A. , Hatchette, J. , Halperin, S. A. , MacDonald, N. E. , & Graham, J. E. (2012). Challenges to immunization: The experiences of homeless youth. BMC Public Health, 12(1), 338–348. 10.1186/1471-2458-12-338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doshani, M. , Weng, M. , Moore, K. L. , Romero, J. R. , & Nelson, N. P. (2019). Recommendations of the Advisory Committee on Immunization Practices for use of hepatitis A vaccine for persons experiencing homelessness. Morbidity and Mortality Weekly Report, 68(6), 153–156. 10.15585/mmwr.mm6806a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falchook, G. , Gaffga, C. , Eve, S. , & Ali, J. (2000). Tuberculosis screening, referral, and treatment in an inner city homeless shelter in Orleans parish. The Journal of the Louisiana State Medical Society, 152(8), 398–404. [PubMed] [Google Scholar]
- Filler, S. J. , MacArthur, J. R. , Parise, M. , Wirtz, R. , Eliades, M. J. , Dasilva, A. , & Steketee, R. W. (2006). Locally acquired mosquito‐transmitted malaria: A guide for investigations in the United States. Morbidity and Mortality Weekly Report, 55(RR‐13). Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5513a1.htm [PubMed]
- Forman, P. D. , & Kinney, C. (2003). Evaluation of a tuberculosis screening questionnaire for use in an Alaskan homeless population. Alaska Medicine, 45(4), 94–101. [PubMed] [Google Scholar]
- Gärden, B. , Samarina, A. , Stavchanskaya, I. , Alsterlund, R. , Övregaard, A. , Taganova, O. , Shpakovskaya, L. , Zjemkov, V. , Ridell, M. , & Larsson, L.‐O. (2013). Food incentives improve adherence to tuberculosis drug treatment among homeless patients in Russia. Scandinavian Journal of Caring Sciences, 27(1), 117–122. 10.1111/j.1471-6712.2012.01009.x [DOI] [PubMed] [Google Scholar]
- Gasner, M. R. , Maw, K. L. , Feldman, G. E. , Fujiwara, P. I. , & Frieden, T. R. (1999). The use of legal action in New York City to ensure treatment of tuberculosis. The New England Journal of Medicine, 340(5), 359–366. 10.1056/nejm199902043400506 [DOI] [PubMed] [Google Scholar]
- Goswami, N. D. , Hecker, E. J. , Vickery, C. , Ahearn, M. A. , Cox, G. M. , Holland, D. P. , Naggie, S. , Piedrahita, C. , Mosher, A. , Torres, Y. , Norton, B. L. , Suchindran, S. , Park, P. H. , Turner, D. , & Stout, J. E. (2012). Geographic information system‐based screening for TB, HIV, and syphilis (GIS‐THIS): A cross‐sectional study. PLoS One, 7(10), e46029. 10.1371/journal.pone.0046029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero‐Bote, V. P. , & Moya‐Anegón, F. (2012). A further step forward in measuring journals' scientific prestige: The SJR2 indicator. Journal of Informetrics, 6(4), 674–688. 10.1016/j.joi.2012.07.001 [DOI] [Google Scholar]
- Gupta, V. , Sugg, N. , Butners, M. , Allen‐White, G. , & Molnar, A. (2015). Tuberculosis among the homeless: Preventing another outbreak through community action. The New England Journal of Medicine, 372(16), 1483–1485. 10.1056/nejmp1501316 [DOI] [PubMed] [Google Scholar]
- Haddad, M. B. , Wilson, T. W. , Ijaz, K. , Marks, S. M. , & Moore, M. (2005). Tuberculosis and homelessness in the United States, 1994–2003. JAMA, 293(22), 2762–2766. 10.1001/jama.293.22.2762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton, K. , Tolfree, R. , & Mytton, J. (2018). A systematic review of active case‐finding strategies for tuberculosis in homeless populations. The International Journal of Tuberculosis and Lung Disease, 22(10), 1135–1144. 10.5588/ijtld.17.0784 [DOI] [PubMed] [Google Scholar]
- Harris, M. , Johnson, S. , Mackin, S. , Saitz, R. , Walley, A. Y. , & Taylor, J. L. (2020). Low barrier tele‐buprenorphine in the time of COVID‐19: A case report. Journal of Addiction Medicine, 14(4), e136–e138. 10.1097/ADM.0000000000000682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, S. N. , Mowbray, C. T. , & Solarz, A. (1994). Physical health, mental health, and substance abuse problems of shelter users. Health & Social Work, 19(1), 37–45. 10.1093/hsw/19.1.37 [DOI] [PubMed] [Google Scholar]
- Herdics, G. , Prochazkova, K. , Mikloskova, M. , Mikolasova, G. , Olah, M. , Kovac, R. , Tordova, S. , Gliganic, M. , Novak, V. , Matuschek, C. , Bucko, L. , Karvaj, M. , Benca, J. , Jankechova, M. , Mrazova, M. , Radkova, L. , Tomanek, P. , Thimm, D. , Ondrejkova, A. , … Kara, S. (2017). A daily low‐threshold integration center for the homeless. Model of social and healthcare for excluded populations. Clinical Social Work and Health Intervention, 8(1), 19–22. 10.22359/cswhi_8_1_04 [DOI] [Google Scholar]
- Hernández Sarmiento, J. M. , Correa, N. , Correa, M. , Franco, J. G. , Alvarez, M. , Ramírez, C. , Gómez, L. M. , Toro, A. C. , Londoño, N. H. , Martínez, M. , Restrepo, M. A. , Zapata, E. , Mejía, G. I. , & Robledo, J. (2013). Tuberculosis among homeless population from Medellín, Colombia: Associated mental disorders and socio‐demographic characteristics. Journal of Immigrant and Minority Health, 15(4), 693–699. 10.1007/s10903-013-9776-x [DOI] [PubMed] [Google Scholar]
- Heuvelings, C. C. , de Vries, S. G. , Greve, P. F. , Visser, B. J. , Bélard, S. , Janssen, S. , Cremers, A. L. , Spijker, R. , Shaw, B. , Hill, R. A. , Zumla, A. , Sandgren, A. , van der Werf, M. J. , & Grobusch, M. P. (2017). Effectiveness of interventions for diagnosis and treatment of tuberculosis in hard‐to‐reach populations in countries of low and medium tuberculosis incidence: A systematic review. The Lancet Infectious Diseases, 17(5), e144–e158. 10.1016/S1473-3099(16)30532-1 [DOI] [PubMed] [Google Scholar]
- Heuvelings, C. C. , de Vries, S. G. , & Grobusch, M. P. (2017). Tackling TB in low‐incidence countries: Improving diagnosis and management in vulnerable populations. International Journal of Infectious Diseases, 56, 77–80. 10.1016/j.ijid.2016.12.025 [DOI] [PubMed] [Google Scholar]
- Heuvelings, C. C. , Greve, P. F. , de Vries, S. G. , Jelle Visser, B. , Bélard, S. , Janssen, S. , Cremers, A. L. , Spijker, R. , Shaw, E. , Hill, R. A. , Zumla, A. , Sandgren, A. , van der Werf, M. J. , & Grobusch, M. P. (2018). Effectiveness of service models and organisational structures supporting tuberculosis identification and management in hard‐to‐reach populations in countries of low and medium tuberculosis incidence: A systematic review. British Medical Journal Open, 8(9), e019642. 10.1136/bmjopen-2017-019642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch‐Moverman, Y. , Bethel, J. , Colson, P. W. , Franks, J. , & El‐Sadr, W. (2010). Predictors of latent tuberculosis infection treatment completion in the United States: An inner city experience. The International Journal of Tuberculosis and Lung Disease, 14(9), 1104–1111. [PMC free article] [PubMed] [Google Scholar]
- Hutchison, R. R. , & Quartaro, E. G. (1993). Training imperatives for volunteers caring for high‐risk, vulnerable populations. Journal of Community Health Nursing, 10(2), 87–96. 10.1207/s15327655jchn1002_3 [DOI] [PubMed] [Google Scholar]
- Hwang, S. W. , Kiss, A. , Ho, M. M. , Leung, C. S. , & Gundlapalli, A. (2008). Infectious disease exposures and contact tracing in homeless shelters. Journal of Health Care for the Poor and Underserved, 19(4), 1163–1167. 10.1353/hpu.0.0070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang, S. , Tolomiczenko, G. , Kouyoumdjian, F. , & Garner, R. (2005). Interventions to improve the health of the homeless: A systematic review. American Journal of Preventive Medicine, 29(4), 311e1–311e75. 10.1016/j.amepre.2005.06.017 [DOI] [PubMed] [Google Scholar]
- Inter‐Agency Standing Committee . (2020). Public health and social measures for COVID‐19 preparedness and response in low capacity and humanitarian settings. Retrieved from https://www.who.int/publications/m/item/public‐health‐and‐social‐measures‐for‐covid‐19‐preparedness‐and‐response‐in‐low‐capacity‐and‐humanitarian‐settings [Google Scholar]
- Janssens, J.‐P. , Wuillemin, T. , Adler, D. , & Jackson, Y. (2017). Screening for tuberculosis in an urban shelter for homeless in Switzerland: A prospective study. BMC Infectious Diseases, 17(1), 347. 10.1186/s12879-017-2449-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, L. , Lewer, D. , Aldridge, R. W. , Hayward, A. C. , & Story, A. (2020). Protocol for a systematic review of treatment adherence for HIV, hepatitis C and tuberculosis among homeless populations. Systematic Reviews, 9(1), 211. 10.1186/s13643-020-01470-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint Tuberculosis Committee of the British Thoracic Society . (2000). Control and prevention of tuberculosis in the United Kingdom: Code of practice 2000. Thorax, 55(11), 887–901. 10.1136/thorax.55.11.887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan‐Weisman, L. , Waltermaurer, E. , & Crump, C. (2018). Assessing and improving zoster vaccine uptake in a homeless population. Journal of Community Health, 43(6), 1019–1027. 10.1007/s10900-018-0517-x [DOI] [PubMed] [Google Scholar]
- Kawatsu, L. , Sato, N. , Ngamvithayapong‐Yanai, J. , & Ishikawa, N. (2013). Leaving the street and reconstructing lives: Impact of DOTS in empowering homeless people in Tokyo, Japan. The International Journal of Tuberculosis and Lung Disease, 17(7), 940–946. 10.5588/ijtld.12.0503 [DOI] [PubMed] [Google Scholar]
- Kim, H. , Choi, H. , Yu, S. , Lee, A.‐Y. , Kim, H.‐O. , Joh, J.‐S. , Heo, E. Y. , Oh, K.‐H. , Kim, H. J. , & Chung, H. (2019). Impact of housing provision package on treatment outcome among homeless tuberculosis patients in South Korea. Asia Pacific Journal of Public Health, 31(7), 603–611. 10.1177/1010539519871779 [DOI] [PubMed] [Google Scholar]
- Kitazawa, S. (1995). Tuberculosis health education needs in homeless shelters. Public Health Nursing, 12(6), 409–416. 10.1111/j.1525-1446.1995.tb00170.x [DOI] [PubMed] [Google Scholar]
- Kong, K. L. , Chu, S. , & Giles, M. L. (2020). Factors influencing the uptake of influenza vaccine vary among different groups in the hard‐to‐reach population. Australian and New Zealand Journal of Public Health, 44(2), 163–168. 10.1111/1753-6405.12964 [DOI] [PubMed] [Google Scholar]
- Kong, P.‐M. , Tapy, J. , Calixto, P. , Burman, W. J. , Reves, R. R. , Yang, Z. , & Cave, M. D. (2002). Skin‐test screening and tuberculosis transmission among the homeless. Emerging Infectious Diseases, 8(11), 1280–1284. 10.3201/eid0811.020306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lashley, M. (2007). A targeted testing program for tuberculosis control and prevention among Baltimore City's homeless population. Public Health Nursing, 24(1), 34–39. 10.1111/j.1525-1446.2006.00605.x [DOI] [PubMed] [Google Scholar]
- Lau, E. A. , & Ferson, M. J. (1997). Surveillance for tuberculosis among residents of hostels for homeless men. Australian and New Zealand Journal of Public Health, 21(5), 447–450. 10.1111/j.1467-842X.1997.tb01733.x [DOI] [PubMed] [Google Scholar]
- Lerner, B. H. (1996). Temporarily detained: Tuberculous alcoholics in Seattle, 1949 through 1960. American Journal of Public Health, 86(2), 257–265. 10.2105/AJPH.86.2.257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesnic, E. , Ustian, A. , & Pop, C. M. (2016). The role of exogenous risk factors of antituberculosis treatment failure. Clujul Medical, 89(3), 396–401. 10.15386/cjmed-608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung, C. S. , Ho, M. M. , Kiss, A. , Gundlapalli, A. V. , & Hwang, S. W. (2008). Homelessness and the response to emerging infectious disease outbreaks: Lessons from SARS. Journal of Urban Health, 85(3), 402–410. 10.1007/s11524-008-9270-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leydesdorff, L. , de Moya‐Anegón, F. , & Guerrero‐Bote, V. P. (2009). Journal maps on the basis of Scopus data: A comparison with the journal citation reports of the ISI. Journal of the American Society for Information Science and Technology, 61(2), 352–369. 10.1002/asi.21250 [DOI] [Google Scholar]
- Li, J. , Driver, C. R. , Munsiff, S. S. , & Fujiwara, P. I. (2003). Finding contacts of homeless tuberculosis patients in New York City. The International Journal of Tuberculosis and Lung Disease, 7(12 Suppl 3), S397–S404. [PubMed] [Google Scholar]
- Lo Bue, P. A. , Cass, R. , Lobo, D. , Moser, K. , & Catanzaro, A. (1999). Development of housing programs to aid in the treatment of tuberculosis in homeless individuals: A pilot study. Chest, 115(1), 218–223. 10.1378/chest.115.1.218 [DOI] [PubMed] [Google Scholar]
- Lupton, A. (2020). Housing homeless in hotels has proven effective against COVID‐19. CBC. Retrieved from https://www.cbc.ca/news/canada/london/housing‐homeless‐in‐hotels‐has‐proven‐effective‐against‐covid‐19‐1.5555879 [Google Scholar]
- Macnee, C. L. , Hemphill, J. C. , & Letran, J. (1996). Screening clinics for the homeless: Evaluating outcomes. Journal of Community Health Nursing, 13(3), 167–177. 10.1207/s15327655jchn1303_4 [DOI] [PubMed] [Google Scholar]
- Markoff, J. , Shapiro, G. , & Weitman, S. R. (1975). Toward the integration of content analysis and general methodology. Sociological Methodology, 6, 1–58. 10.2307/270893 [DOI] [Google Scholar]
- Marks, S. M. , Taylor, Z. , Burrows, N. R. , Qayad, M. G. , & Miller, B. (2000). Hospitalization of homeless persons with tuberculosis in the United States. American Journal of Public Health, 90(3), 435–438. 10.2105/AJPH.90.3.435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayo, K. , White, S. , Oates, S. K. , & Franklin, F. (1996). Community collaboration: Prevention and control of tuberculosis in a homeless shelter. Public Health Nursing, 13(2), 120–127. 10.1111/j.1525-1446.1996.tb00229.x [DOI] [PubMed] [Google Scholar]
- McMillan Jackson, M. (1996). Pulmonary tuberculosis in a homeless person. American Journal of Infection Control, 24(4), 294–298. 10.1016/S0196-6553(96)90060-7 [DOI] [PubMed] [Google Scholar]
- Metcalfe, S. E. , & Sexton, E. H. (2014). An academic‐community partnership to address the flu vaccination rates of the homeless. Public Health Nursing, 31(2), 175–182. 10.1111/phn.12088 [DOI] [PubMed] [Google Scholar]
- Miller, T. , Hilsenrath, P. , Lykens, K. , Mcnabb, S. , Moonan, P. , & Weis, S. (2006). Using cost and health impacts to prioritize the targeted testing of tuberculosis in the United States. Annals of Epidemiology, 16(4), 305–312. 10.1016/j.annepidem.2005.07.053 [DOI] [PubMed] [Google Scholar]
- Moffa, M. , Cronk, R. , Fejfar, D. , Dancausse, S. , Padilla, L. A. , & Bartram, J. (2019). A systematic scoping review of environmental health conditions and hygiene behaviors in homeless shelters. International Journal of Hygiene and Environmental Health, 222(3), 335–346. 10.1016/j.ijheh.2018.12.004 [DOI] [PubMed] [Google Scholar]
- Moreau, D. , Gratrix, J. , Kunimoto, D. , Beckon, A. , Der, E. , Hansen, E. , Chui, L. , & Ahmed, R. (2012). A shelter‐associated tuberculosis outbreak: A novel strain introduced through foreign‐born populations. Canadian Journal of Public Health, 103(6), e408–e412. 10.1007/BF03405627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munn, M. S. , Duchin, J. S. , Kay, M. , Pecha, M. , Thibault, C. S. , & Narita, M. (2015). Analysis of risk factors for tuberculous infection following exposure at a homeless shelter. The International Journal of Tuberculosis and Lung Disease, 19(5), 570–575. 10.5588/ijtld.14.0648 [DOI] [PubMed] [Google Scholar]
- Munthe‐Kaas, H. M. , Berg, R. C. , & Blaasvær, N. (2018). Effectiveness of interventions to reduce homelessness: A systematic review and meta‐analysis. Campbell Systematic Reviews, 14(1), 1–281. 10.4073/csr.2018.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murti, M. , Louie, K. , Bigham, M. , & Hoang, L. M. N. (2015). Outbreak of shigellosis in a homeless shelter with healthcare worker transmission—British Columbia, April 2015. Infection Control & Hospital Epidemiology, 36(11), 1372–1373. 10.1017/ice.2015.211 [DOI] [PubMed] [Google Scholar]
- Nardell, E. A. (1989). Tuberculosis in homeless, residential care facilities, prisons, nursing homes, and other close communities. Seminars in Respiratory Infections, 4(3), 206–215. [PubMed] [Google Scholar]
- Neuendorf, K. A. (2002). The content analysis guidebook. Sage Publications. [Google Scholar]
- Nwana, N. , Marks, S. M. , Lan, E. , Chang, A. H. , Holcombe, M. , & Morris, S. B. (2019). Treatment of latent Mycobacterium tuberculosis infection with 12 once weekly directly‐observed doses of isoniazid and rifapentine among persons experiencing homelessness. PLoS One, 14(3), e0213524. 10.1371/journal.pone.0213524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi, A. , Nahid, P. , Berg, J. , Burrage, J. , Christiani, A. , Aqtash, S. , Morisky, D. , & Leake, B. (2008). Efficacy of nurse case‐managed intervention for latent tuberculosis among homeless subsamples. Nursing Research, 57(1), 33–39. 10.1097/01.NNR.0000280660.26879.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connell, J. J. (1991). Nontuberculous respiratory infections among the homeless. Seminars in Respiratory Infections, 6(4), 247–253. [PubMed] [Google Scholar]
- Ohkado, A. , Williams, G. , Ishikawa, N. , Shimouchi, A. , & Simon, C. (2005). The management for tuberculosis control in Greater London in comparison with that in Osaka City: Lessons for improvement of TB control management in Osaka City urban setting. Health Policy, 73(1), 104–123. 10.1016/j.healthpol.2004.11.006 [DOI] [PubMed] [Google Scholar]
- Ohtsu, T. , Toda, R. , Shiraishi, T. , Toyoda, H. , Toyozawa, H. , Kamioka, Y. , Ochiai, H. , Shimada, N. , Shirasawa, T. , Hoshino, H. , & Kokaze, A. (2011). Living conditions, ability to seek medical treatment, and awareness of health conditions and healthcare options among homeless persons in Tokyo, Japan. Acta Medica Okayama, 65(6), 387–393. 10.18926/AMO/47264 [DOI] [PubMed] [Google Scholar]
- Onwubiko, U. , Wall, K. , Sales, R.‐M. , & Holland, D. P. (2019). Using Directly Observed Therapy (DOT) for latent tuberculosis treatment – A hit or a miss? A propensity score analysis of treatment completion among 274 homeless adults in Fulton County, GA. PLoS One, 14(6), e0218373. 10.1371/journal.pone.0218373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson Tulsky, J. , Castle White, M. , Young, J. A. , Meakin, R. , & Moss, A. R. (1999). Street talk: Knowledge and attitudes about tuberculosis and tuberculosis control among homeless adults. The International Journal of Tuberculosis and Lung Disease, 3(6), 528–533. [PubMed] [Google Scholar]
- Pilote, L. , Tulsky, J. P. , Zolopa, A. R. , Hahn, J. A. , Schecter, G. F. , & Moss, A. R. (1996). Tuberculosis prophylaxis in the homeless: A trial to improve adherence to referral. Archives of Internal Medicine, 156(2), 161–165. 10.1001/archinte.1996.00440020063008 [DOI] [PubMed] [Google Scholar]
- Potter, J. L. , Inamdar, L. , Okereke, E. , Collinson, S. , Dukes, R. , & Mandelbaum, M. (2016). Support of vulnerable patients throughout TB treatment in the UK. Journal of Public Health, 38(2), 391–395. 10.1093/pubmed/fdv052 [DOI] [PubMed] [Google Scholar]
- Rayner, D. (2000). Reducing the spread of tuberculosis in the homeless population. British Journal of Nursing, 9(13), 871–875. 10.12968/bjon.2000.9.13.5516 [DOI] [PubMed] [Google Scholar]
- Rendleman, N. J. (1999). Mandated tuberculosis screening in a community of homeless people. American Journal of Preventive Medicine, 17(2), 108–113. 10.1016/S0749-3797(99)00052-5 [DOI] [PubMed] [Google Scholar]
- Rimawi, B. H. , Mirdamadi, M. , & John, J. F. (2014). Infections and homelessness: Risks of increased infectious diseases in displaced women: Infections and homelessness. World Medical and Health Policy, 6(2), 118–132. 10.1002/wmh3.95 [DOI] [Google Scholar]
- Riquelme‐Miralles, D. , Palazón‐Bru, A. , Sepehri, A. , & Gil‐Guillén, V. F. (2019). A systematic review of non‐pharmacological interventions to improve therapeutic adherence in tuberculosis. Heart & Lung, 48(5), 452–461. 10.1016/j.hrtlng.2019.05.001 [DOI] [PubMed] [Google Scholar]
- Roy, A. , Abubakar, I. , Yates, S. , Chapman, A. , Lipman, M. , Monk, P. , & Catchpole, M. ; on behalf of the National Knowledge Service TB Project Board . (2008). Evaluating knowledge gain from TB leaflets for prison and homeless sector staff: The National Knowledge Service TB pilot. The European Journal of Public Health, 18(6), 600–603. 10.1093/eurpub/ckn096 [DOI] [PubMed] [Google Scholar]
- Samuels, E. A. , Clark, S. A. , Wunsch, C. , Jordison Keeler, L. A. , Reddy, N. , Vanjani, R. , & Wightman, R. S. (2020). Innovation during COVID‐19: Improving addiction treatment access. Journal of Addiction Medicine, 14(4), e8–e9. 10.1097/ADM.0000000000000685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schieffelbein, C. W. , & Snider, D. E. (1988). Tuberculosis control among homeless populations. Archives of Internal Medicine, 148(8), 1843–1846. 10.1001/archinte.1988.00380080109029 [DOI] [PubMed] [Google Scholar]
- Schluger, N. , Ciotoli, C. , Cohen, D. , Johnson, H. , & Rom, W. N. (1995). Comprehensive tuberculosis control for patients at high risk for noncompliance. American Journal of Respiratory and Critical Care Medicine, 151(5), 1486–1490. 10.1164/ajrccm.151.5.7735604 [DOI] [PubMed] [Google Scholar]
- SCImago . (n.d.). About us. Retrieved from https://www.scimagojr.com/aboutus.php [Google Scholar]
- Shier, M. L. , Engstrom, S. , & Graham, J. R. (2011). International migration and social work: A review of the literature. Journal of Immigrant & Refugee Studies, 9(1), 38–56. 10.1080/15562948.2011.547825 [DOI] [Google Scholar]
- Silva, E. , Pereira, A. C. , Araújo, W. , & Elias, F. (2018). A systematic review of economic evaluations of interventions to tackle tuberculosis in homeless people. Revista Panamericana De Salud Pública, 42, 1–8. 10.26633/RPSP.2018.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southern, A. , Premaratne, N. , English, M. , Balazs, J. , & O’Sullivan, D. (1999). Tuberculosis among homeless people in London: An effective model of screening and treatment. The International Journal of Tuberculosis and Lung Disease, 3(11), 1001–1008. [PubMed] [Google Scholar]
- Swigart, V. , & Kolb, R. (2004). Homeless persons' decisions to accept or reject public health disease‐detection services. Public Health Nursing, 21(2), 162–170. 10.1111/j.0737-1209.2004.021210.x [DOI] [PubMed] [Google Scholar]
- Tankimovich, M. (2013). Barriers to and interventions for improved tuberculosis detection and treatment among homeless and immigrant populations: A literature review. Journal of Community Health Nursing, 30(2), 83–95. 10.1080/07370016.2013.778723 [DOI] [PubMed] [Google Scholar]
- Tobolowsky, F. A. , Gonzales, E. , Self, J. L. , Rao, C. Y. , Keating, R. , Marx, G. E. , McMichael, T. M. , Lukoff, M. D. , Duchin, J. S. , Huster, K. , Rauch, J. , McLendon, H. , Hanson, M. , Nichols, D. , Pogosjans, S. , Fagalde, M. , Lenahan, J. , Maier, E. , Whitney, H. , … Kay, M. (2020). COVID‐19 outbreak among three affiliated homeless service sites—King County, Washington, 2020. Morbidity and Mortality Weekly Report, 69(17), 523–526. 10.15585/mmwr.mm6917e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres, R. A. (1990). Human immunodeficiency virus infection among homeless men in a New York City shelter. Association with Mycobacterium tuberculosis infection. Archives of Internal Medicine, 150(10), 2030–2036. 10.1001/archinte.150.10.2030 [DOI] [PubMed] [Google Scholar]
- Tricco, A. C. , Lillie, E. , Zarin, W. , O'Brien, K. K. , Colquhoun, H. , Levac, D. , Moher, D. , Peters, M. D. J. , Horsley, T. , Weeks, L. , Hempel, S. , Akl, E. A. , Chang, C. , McGowan, J. , Stewart, L. , Hartling, L. , Aldcroft, A. , Wilson, M. G. , Garritty, C. , … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA‐ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- Tsai, J. , & Wilson, M. (2020). COVID‐19: A potential public health problem for homeless populations. The Lancet Public Health, 5(4), e186–e187. 10.1016/S2468-2667(20)30053-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tulsky, J. P. , Hahn, J. A. , Long, H. L. , Chambers, D. B. , Robertson, M. J. , Chesney, M. A. , & Moss, A. R. (2004). Can the poor adhere? Incentives for adherence to TB prevention in homeless adults. The International Journal of Tuberculosis and Lung Disease, 8(1), 83–91. [PubMed] [Google Scholar]
- Tulsky, J. P. , Pilote, L. , Hahn, J. A. , Zolopa, A. J. , Burke, M. , Chesney, M. , & Moss, A. R. (2000). Adherence to isoniazid prophylaxis in the homeless: A randomized controlled trial. Archives of Internal Medicine, 160(5), 697–702. 10.1001/archinte.160.5.697 [DOI] [PubMed] [Google Scholar]
- Uchimura, K. , Ngamvithayapong‐Yanai, J. , Kawatsu, L. , Ohkado, A. , Yoshiyama, T. , Shimouchi, A. , Ito, K. , & Ishikawa, N. (2013). Characteristics and treatment outcomes of tuberculosis cases by risk groups, Japan, 2007–2010. Western Pacific Surveillance and Response Journal, 4(1), 11–18. 10.5365/wpsar.2012.3.4.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hest, N. A. , Aldridge, R. W. , de Vries, G. , Sandgren, A. , Hauer, B. , Hayward, A. , Arrazola de Oñate, W. , Haas, W. , Codecasa, L. R. , Caylà, J. A. , Story, A. , Antoine, D. , Gori, A. , Quabeck, L. , Jonsson, J. , Wanlin, M. , Orcau, À. , Rodes, A. , Dedicoat, M. , & Abubakar, I. (2014). Tuberculosis control in big cities and urban risk groups in the European Union: A consensus statement. Eurosurveillance, 19(9), 1–13. 10.2807/1560-7917.ES2014.19.9.20728 [DOI] [PubMed] [Google Scholar]
- Vlahov, D. , Coady, M. H. , Ompad, D. C. , & Galea, S. (2007). Strategies for improving influenza immunization rates among hard‐to‐reach populations. Journal of Urban Health, 84(4), 615–631. 10.1007/s11524-007-9197-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weatherill, S. A. , Buxton, J. A. , & Daly, P. C. (2004). Immunization programs in non‐traditional settings. Canadian Journal of Public Health, 95(2), 133–137. 10.1007/BF03405781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber, R. P. (1990). Basic content analysis (2nd ed.). Sage Publications. 10.4135/9781412983488 [DOI] [Google Scholar]
- Wildridge, V. , & Bell, L. (2002). How CLIP became ECLIPSE: A mnemonic to assist in searching for health policy/management information. Health Information and Libraries Journal, 19(2), 113–115. 10.1046/j.1471-1842.2002.00378.x [DOI] [PubMed] [Google Scholar]
- World Bank . (2020). Scientific and technical journal articles. Retrieved from https://data.worldbank.org/indicator/IP.JRN.ARTC.SC?most_recent_value_desc=true&year_low_desc=true
- World Health Organization . (2003). Adherence to long‐term therapies: Evidence for action. Retrieved from https://www.who.int/chp/knowledge/publications/adherence_report/en/ [Google Scholar]
- World Health Organization . (2020). WHO coronavirus disease (COVID‐19) dashboard. Retrieved from https://covid19.who.int [Google Scholar]
- World Health Organization . (2020). Considerations for implementing and adjusting public health and social measures in the context of COVID‐19. Retrieved from https://www.who.int/publications/i/item/considerations‐in‐adjusting‐public‐health‐and‐social‐measures‐in‐the‐context‐of‐covid‐19‐interim‐guidance [Google Scholar]
- World Health Organization . (2020). World Health Organization (WHO) information note: Tuberculosis and COVID‐19. Retrieved from https://www.who.int/docs/default‐source/documents/tuberculosis/infonote‐tb‐covid‐19.pdf [Google Scholar]
- Wrezel, O. (2009). Respiratory infections in the homeless. UWO Medical Journal, 78(2), 61–65. [Google Scholar]
- Wurtz, R. , Lee, C. , Lama, J. , & Kuharik, J. (1996). A new class of close contacts: Home health care workers and occupational exposure to tuberculosis. Journal of Home Health Care Practice, 8(2), 28–31. 10.1177/108482239600800209 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- World Bank . (2020). Scientific and technical journal articles. Retrieved from https://data.worldbank.org/indicator/IP.JRN.ARTC.SC?most_recent_value_desc=true&year_low_desc=true
Supplementary Materials
Supplementary Material
Supplementary Material
Supplementary Material
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analysed in this study. For further data inquiry, please contact the corresponding author.


