Abstract
Background
Economic crises during the coronavirus disease (COVID‐19) pandemic severely impacted mental health outcomes. However, there is limited evidence on this issue in Thailand. We aimed to evaluate the association of economic burden during the first phase of the pandemic and the risk of adverse mental health outcomes in the Thai population.
Methods
We recruited 2,303 participants aged 18 years or above with employment/full‐time jobs before the national lockdown in April–May 2020. The measures of economic burden were job loss, income loss, and financial problems related to the outbreak. The outcomes included depressive symptoms, anxiety, and perceived stress. The association between economic burden and adverse mental health outcomes was evaluated using multivariable logistic regression models.
Results
Individuals who lost their jobs during the COVID‐19 pandemic had a higher risk of perceived stress compared to those who maintained their job (adjusted odds ratio [OR], 2.40; 95% confidence interval [CI], 1.28–4.51; p = .006). A higher risk of anxiety was observed in individuals with a monthly income loss of 50% (adjusted OR, 1.42; 95% CI, 1.03–1.99; p = .035; individuals without income loss, reference group) or over. Self‐reported financial problems were significantly associated with adverse mental health outcomes (nonexperienced financial problems, reference group): Adjusted ORs of 1.84 (95% CI, 1.34–2.51; p < .001) for depressive symptoms, 2.00 (95% CI, 1.48–2.71; p < .001) for anxiety, and 2.12 (95% CI, 1.51–2.95; p < .001) for perceived stress.
Conclusions
Economic burden, especially self‐reported financial problems, was associated with adverse mental health outcomes. However, long‐term studies are needed to address the mental health consequences of COVID‐19 and economic downturns.
Keywords: COVID‐19, economic burden, financial problems, income loss, job loss, mental health
1. INTRODUCTION
The coronavirus disease‐2019 (COVID‐19) was declared a pandemic and a global emergency by the World Health Organisation on January 30, 2020. Since then, it has rapidly spread in 216 countries (Burki, 2020; Mahase, 2020). As of October 18, 2020, over 37 million COVID‐19 cases and 1 million deaths were reported globally (World Health Organization, 2020). The numbers are still rising as countries anticipate a second or third wave of infections. The pandemic has affected people from all walks of life; unprecedented measures, including lockdowns, movement restrictions, physical distancing rules, and schools and workplace closures, have been taken to contain the spread of the disease. The continued implementation of restrictions in the past few months may have helped delay the peaking of the epidemic. However, it has posed the largest economic shock the world has experienced in decades. The World Bank has forecasted the deepest economic recession for all countries (5.2% contraction in gross domestic product [GDP]) since World War II (World Bank, 2020).
Economic crises had greatly influenced the mental and psychological wellbeing of the population, especially those who are directly affected (World Health Organization: Regional Office for Europe, 2011). Generally, mental health problems are related to the determinants of population health, including inequality, poverty, deprivation, and other social and economic metrics. Although it is difficult to determine the causal relationship between these factors, existing evidence illustrates that poor mental health is linked with substantial financial strain, indebtedness, and unemployment (Drydakis, 2015; Fiori et al., 2016; Jenkins et al., 2008; Parmar et al., 2016; Silva et al., 2018; Urbanos‐Garrido & Lopez‐Valcarcel, 2015). Furthermore, the prevalence of mental health problems, such as common mental disorders, substance‐related disorders, and suicidal behavior, tends to be higher during the period of economic recession than during normal times (Frasquilho et al., 2016). Amid the COVID‐19 pandemic, certain groups of people may be particularly vulnerable to COVID‐19 related economic burden, for instance, those unemployed, in debt, or facing financial problems, which have detrimental effects on their mental wellbeing. As such, the current economic crisis brought about by the COVID‐19 pandemic may make people with or without preexisting mental illness more prone to poor mental health.
In Thailand, which effectively contained the COVID‐19 outbreak, 3–5 million people (8%–13% of the current workforce) are unemployed, the highest figure ever seen on record. The country's labor force started to weaken because of the economy even before the outbreak. The implementation of national health and government policies forced large‐scale businesses to shut down, resulting in job losses; indeed, the number of employees with irregular salaries, low‐paid workers, and those without a written contract are continually increasing. According to the latest projection of the International Monetary Fund in October 2020, Thailand's economy is projected to decline by 7.1% in 2020, its worst GDP report ever (International Monetary Fund, 2020). Before the pandemic, the Thai economic growth slowed in 2019, with Thailand's household debt being the highest in Asia. According to financial institutions, the ratio of household debt to GDP soared to 80% in the first quarter of 2020; however, it could increase to 90% of the GDP amid the economic downturn and COVID‐19 pandemic (Onthaworn, 2020).
Taken together, we postulated that the general Thai population, especially those facing economic burden, is at risk of developing mental health and psychosocial problems during the COVID‐19 pandemic. To our knowledge, the association between the general population's mental health issues and economic decline in Thailand due to the economic recession during the COVID‐19 pandemic has not been evaluated. Therefore, this nationwide cross‐sectional study aimed to evaluate the association of economic burden during the first phase of the COVID‐19 pandemic, including job loss, income loss, and financial problems, with the risk of adverse mental health outcomes in the general Thai population.
2. METHODS
2.1. Study design and participants
This study is a part of wave I (April 21–May 4, 2020) of The Health Outcomes and Mental Health Care Evaluation Survey: Under the Pandemic Situation of COVID‐19 (HOME‐COVID‐19). Details of the protocol are published elsewhere (Mongkhon et al., 2021; Nochaiwong et al., 2020). In brief, we conducted an open, online, voluntary, nationwide survey through convenient selection of the target population in Thailand. Participants who (i) were Thai citizens, permanent residents, or nonresidents with work permits aged 18 years or above at the date of the survey; (ii) had full‐time employment before the national lockdown owing to the COVID‐19 outbreak; (iii) can read and communicate in the Thai language; and (iv) can access the Internet were eligible for inclusion in this study. Those who did not complete the online survey, or spent less than 2 min or more than 60 min on the survey were excluded. We developed an online questionnaire via the SurveyMonkey® platform, which could limit one‐time participation per unique Internet Protocol address. Relevant links or QR codes were distributed to the eligible population using a convenience and snowball sampling strategy via social media networks, including public websites, Facebook, LINE, Twitter, and Instagram.
This study was performed in accordance with the Declaration of Helsinki. Ethics approval was granted by the Committee of Research Ethics of the Faculty of Public Health (ET010/2020) and Faculty of Pharmacy (23/2563), Chiang Mai University. A written consent form was obtained from all participants before completing the questionnaire. The study was reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology Statement (von Elm et al., 2007) and the Improving the Quality of Web Surveys: The Checklist for Reporting Results of Internet E‐Surveys (Eysenbach, 2004).
2.2. Assessments
The main independent variables were job loss, income loss, and financial problems related to the COVID‐19 outbreak. We used dichotomous (yes/no) questions to assess job loss and self‐reported financial problems. Income loss was categorized as no, less than 50% of monthly income, or 50% or more of monthly income. The Thai versions of the Patient Health Questionnaire—9‐items (PHQ‐9), Generalised Anxiety Disorder Scale—7‐items (GAD‐7), and Perceived Stress Scale—10‐items (PSS‐10) were used to evaluate the mental health outcomes.
The PHQ‐9 was used for measuring depressive symptoms and comprises nine items rated on a 4‐point Likert scale. The total score ranges from 0 to 27, with higher scores reflecting greater depression severity within the past 2 weeks. The cut‐off score for the depressive symptom group was 9 or above. The PHQ‐9 Thai version showed good psychometric properties, with a Cronbach's α of .79 (Lotrakul et al., 2008).
The GAD‐7 was used for measuring worry and anxiety symptoms within the past 2 weeks and comprises seven items rated on a 4‐point Likert scale. The total score ranges from 0 to 21, with higher scores indicating more severe anxiety. A cut‐off point of 5 or above was used to identify the general population with anxiety symptoms. The psychometric properties of this tool were excellent, with a Cronbach's α of .92 (Spitzer et al., 2006).
The PSS‐10 was used to measure the perception of stress, and the items are rated on a 5‐point Likert scale; the questions are related to the participants' feelings and thoughts during the previous month. Scores range from 0 to 40; higher scores indicate a higher degree of stress. A cut‐off point of 14 or above was considered to indicate perceived stress. The PSS‐10 has good psychometric properties, with a Cronbach's α of .85 (Wongpakaran & Wongpakaran, 2010).
2.3. Covariates
Baseline sociodemographic characteristics included age, sex, educational level, marital status, religion, occupation/profession status, region of residence, living status, reimbursement schemes, history of mental illness, history of chronic noncommunicable diseases (NCDs), debt, media exposure, confirmed cases in the community, and quarantine/isolation information. The Brief Resilient Coping Scale, a four‐item questionnaire with each item rated on a 5‐point Likert scale, was also used to assess current resilience capability (Sinclair & Wallston, 2004).
2.4. Sample size calculation
According to a priori protocol, 3.3%–75.5% of the general population were selected, based on the results of previous studies reporting the prevalence of mental health problems (e.g., depression, anxiety, and stress) during the COVID‐19 outbreak (Nochaiwong et al., 2020). The sample was calculated using the compensation for a design effect of 2.0 and a response rate of 60%. To obtain statistical power of 80% and a type I error probability of 0.05, this study required 1,310 participants for the final analysis.
2.5. Statistical analyses
Descriptive statistics were used and expressed as frequency and percentage, mean ± standard deviation (SD), or median with a range (min–max) as appropriate. To test the differences in baseline characteristics between economic burden groups, an independent t test or Wilcoxon rank‐sum test was used for continuous data and Fisher's exact test for categorical data. The prevalence of adverse mental health outcomes in each economic burden group was assessed. For all models, we adjusted the weights for the national population and the rate of Internet use obtained from the National Statistic Office of the Thai Ministry of Information and Communication Technology.
The associations of job loss, income loss, and financial problems with the risk of adverse mental health outcomes were evaluated using multivariable logistic regression models to control for potential confounding factors (Kleinbaum & Klein, 2010). We reported the crude odds ratios (ORs) and the corresponding 95% confidence intervals (CIs). Multicollinearity was examined using a variance inflation factor (VIF) value of 4 or above as a cut‐off point for further investigation, and a VIF value of 10 or above indicated a serious multicollinearity, which required correction (O'brien, 2007). All three models were analyzed after adjusting for different confounders: (i) Model 1 adjusted for age and sex; (ii) model 2 for model 1 plus marital status, education level, religion, region, living status, reimbursement scheme, history of mental illness, history of NCDs, and debt; and (iii) model 3 for model 2 plus information exposure during the COVID‐19 outbreak, confirmed cases in the community, quarantine status, and resilient coping. Subsequently, missing data or incomplete responses were excluded from the analyses. All analyses were performed using Stata 14.0 (StataCorp, LP). The two‐tailed tests conducted had a type I error rate of .05.
3. RESULTS
3.1. Participants' characteristics
Among the 4,322 participants screened in the first wave of the HOME‐COVID‐19 survey, 318 who were unable to complete the questionnaire survey and 1,701 who were unemployed or with non‐full‐time jobs before the national lockdown were excluded (Figure 1). Therefore, 2,303 participants (mean age, 34.5 ± 10.2 years) were eligible for this study, of which, 60.0% were females, 67.5% were single, and 8.1% had a history of mental illness (Table 1). Of the 2,303 participants, 262 (11.4%) lost their jobs, whereas 374 (16.2%) and 755 (32.8%) reported monthly income losses of less than 50% and 50% or above, respectively. Additionally, 1,196 (51.9%) participants had self‐reported financial problems (Table 1).
Figure 1.
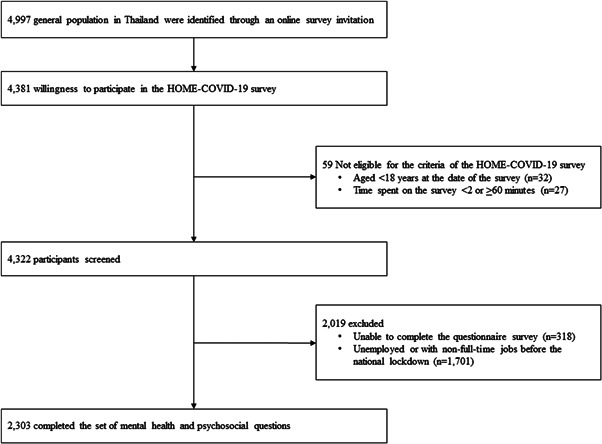
Flow diagram for study participants. HOME‐COVID‐19, The Health Outcomes and Mental Health Care Evaluation Survey Research Group‐Coronavirus disease 2019
Table 1.
Participants characteristics according to the economic burden during the COVID‐19 pandemic in Thailand (n = 2,303)
| Characteristics | Overall (n = 2,303) | Job loss | Income loss | Self‐reported financial problems | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No (n = 2,041) | Yes (n = 262) | p Value | No (n = 1,174) | Monthly income loss of <50% (n = 374) | Monthly income loss of ≥ 50% (n = 755) | p Value | No (n = 1,107) | Yes (n = 1,196) | p Value | ||
| Age, year (mean ± SD) | 34.5 ± 10.2 | 35.0 ± 10.3 | 30.5 ± 8.9 | <.001 | 34.9 ± 10.2 | 35.5 ± 11.0 | 33.2 ± 9.6 | .009 | 35.6 ± 10.8 | 33.4 ± 9.5 | <.001 |
| ≤30 | 1,009 (43.8) | 845 (41.4) | 164 (62.6) | <.001 | 484 (41.2) | 158 (42.3) | 367 (48.6) | .003 | 444 (40.1) | 565 (47.2) | <.001 |
| 31‐50 | 1,072 (46.6) | 986 (48.3) | 86 (32.8) | 572 (48.7) | 168 (44.9) | 332 (44.0) | 525 (47.4) | 547 (45.7) | |||
| ≥51 | 222 (9.6) | 210 (10.3) | 12 (4.6) | 118 (10.1) | 48 (12.8) | 56 (7.4) | 138 (12.5) | 84 (7.0) | |||
| Sexual identity | |||||||||||
| Male | 851 (37.0) | 774 (37.9) | 77 (23.4) | .020 | 443 (37.7) | 143 (38.2) | 265 (35.1) | .371 | 430 (38.8) | 421 (35.2) | .127 |
| Female | 1,384 (60.0) | 1,206 (59.1) | 178 (67.9) | 703 (59.9) | 218 (58.3) | 463 (61.3) | 649 (58.6) | 735 (61.5) | |||
| Other | 68 (3.0) | 61 (3.0) | 7 (2.7) | 28 (2.4) | 13 (3.5) | 27 (3.6) | 28 (2.5) | 40 (3.3) | |||
| Marital status | |||||||||||
| Single | 1,554 (67.5) | 1,349 (66.1) | 205 (78.2) | <.001 | 778 (66.3) | 257 (68.7) | 519 (68.7) | .097 | 746 (67.4) | 808 (67.6) | .331 |
| Married/domestic partnership | 654 (28.4) | 608 (29.8) | 46 (17.6) | 357 (30.4) | 98 (26.2) | 199 (26.4) | 322 (29.1) | 332 (27.8) | |||
| Divorced/widowed/separated | 95 (4.1) | 84 (4.1) | 11 (4.2) | 39 (3.3) | 19 (5.1) | 37 (4.9) | 39 (3.5) | 56 (4.7) | |||
| Education level | |||||||||||
| Illiterate/primary school/junior high school | 110 (4.8) | 84 (4.1) | 26 (9.9) | <.001 | 33 (2.8) | 10 (2.7) | 67 (8.9) | <.001 | 18 (1.6) | 92 (7.7) | <.001 |
| Senior high school/diploma/high vocational | 354 (15.4) | 298 (14.6) | 56 (21.4) | 113 (9.6) | 55 (14.7) | 186 (24.6) | 88 (8.0) | 266 (22.2) | |||
| Bachelor's degree/higher education | 1,839 (79.8) | 1,659 (81.3) | 180 (68.7) | 1,028 (87.6) | 309 (82.6) | 502 (66.5) | 1,001 (90.4) | 838 (70.1) | |||
| Religion | |||||||||||
| No | 174 (7.6) | 147 (7.2) | 27 (10.3) | .082 | 78 (6.6) | 25 (6.7) | 71 (9.4) | .070 | 81 (7.3) | 93 (7.8) | .694 |
| Region | |||||||||||
| Capital and vicinity | 877 (38.1) | 802 (39.3) | 187 (71.4) | .001 | 510 (43.4) | 163 (43.6) | 204 (27.0) | <.001 | 528 (47.7) | 349 (29.2) | <.001 |
| Provincial | 1,426 (61.9) | 1,239 (60.7) | 75 (28.6) | 664 (56.6) | 211 (56.4) | 551 (73.0) | 579 (52.3) | 847 (70.8) | |||
| Living status | |||||||||||
| Alone | 402 (17.5) | 361 (17.7) | 41 (15.6) | .727 | 221 (18.8) | 71 (19.0) | 110 (14.6) | .069 | 226 (20.4) | 176 (14.7) | .001 |
| With family | 1,730 (75.1) | 1529 (74.9) | 201 (76.7) | 876 (74.6) | 273 (73.0) | 581 (76.9) | 806 (72.8) | 924 (77.3) | |||
| With others | 171 (7.4) | 151 (7.4) | 20 (7.6) | 77 (6.6) | 30 (8.0) | 64 (8.5) | 75 (6.8) | 96 (8.0) | |||
| Reimbursement scheme | |||||||||||
| Government/state enterprises | 388 (16.9) | 388 (19.0) | 0 (0.0) | <.001 | 325 (27.7) | 36 (9.6) | 27 (3.6) | <.001 | 302 (27.3) | 86 (7.2) | <.001 |
| Universal coverage scheme | 468 (20.3) | 363 (17.8) | 105 (40.1) | 129 (11.0) | 69 (18.5) | 270 (35.8) | 106 (9.6) | 362 (30.3) | |||
| Social security scheme | 1,044 (45.3) | 952 (46.6) | 92 (35.1) | 544 (46.3) | 193 (51.6) | 307 (40.7) | 502 (45.3) | 542 (45.3) | |||
| Self‐payment/others | 403 (17.5) | 338 (16.6) | 65 (24.8) | 176 (15.0) | 76 (20.3) | 151 (20.0) | 197 (17.8) | 206 (17.2) | |||
| History of mental illness | |||||||||||
| Yes | 187 (8.1) | 149 (7.3) | 38 (14.5) | <.001 | 78 (6.6) | 29 (7.8) | 80 (10.6) | .009 | 70 (6.3) | 117 (9.8) | .003 |
| History of chronic NCDa | |||||||||||
| Yes | 451 (19.6) | 398 (19.5) | 53 (20.2) | .804 | 224 (19.1) | 66 (17.6) | 161 (21.3) | .287 | 212 (19.2) | 239 (20.0) | .636 |
| Debt | |||||||||||
| Yes | 1,591 (69.1) | 1,430 (70.1) | 161 (61.4) | .006 | 790 (67.3) | 272 (72.7) | 529 (70.1) | .109 | 684 (61.8) | 907 (75.8) | <.001 |
| Information exposure during the COVID‐19 outbreak | |||||||||||
| <1 h/day | 774 (33.6) | 705 (34.5) | 69 (26.3) | <.001 | 437 (37.2) | 108 (28.9) | 229 (30.3) | <.001 | 378 (34.2) | 396 (33.1) | <.001 |
| 1–2 h/day | 945 (41.0) | 846 (41.5) | 99 (37.8) | 505 (43.0) | 165 (44.1) | 275 (36.4) | 506 (45.7) | 439 (36.7) | |||
| ≥3 h/day | 584 (25.4) | 490 (24.0) | 94 (35.9) | 232 (19.8) | 101 (27.0) | 251 (33.3) | 223 (20.1) | 361 (30.2) | |||
| Confirmed cases in the community | |||||||||||
| No | 1,521 (66.0) | 1,353 (66.3) | 168 (64.1) | .354 | 749 (63.8) | 264 (70.6) | 508 (67.3) | .042 | 751 (67.8) | 770 (64.4) | .033 |
| Yes | 346 (15.0) | 310 (15.2) | 36 (13.7) | 200 (17.0) | 42 (11.2) | 104 (13.8) | 171 (15.5) | 175 (14.6) | |||
| Not known | 436 (18.9) | 378 (18.5) | 58 (22.1) | 225 (19.2) | 68 (18.2) | 143 (18.9) | 185 (16.7) | 251 (21.0) | |||
| Quarantine status | |||||||||||
| Never | 1,336 (58.0) | 1,223 (59.9) | 113 (43.1) | <.001 | 738 (62.9) | 228 (61.0) | 370 (49.0) | <.001 | 727 (65.7) | 609 (50.9) | <.001 |
| Past | 724 (31.4) | 625 (30.6) | 99 (37.8) | 343 (29.2) | 105 (28.1) | 276 (36.6) | 280 (25.3) | 444 (37.1) | |||
| Current | 243 (10.6) | 193 (9.5) | 50 (10.1) | 93 (7.9) | 41 (11.0) | 109 (14.4) | 100 (9.0) | 143 (12.0) | |||
| Resilient copingb | |||||||||||
| Low resilient copers | 988 (42.9) | 860 (42.1) | 128 (48.8) | .089 | 485 (41.3) | 163 (43.6) | 340 (45.0) | .029 | 412 (37.2) | 576 (48.2) | <.001 |
| Medium resilient copers | 890 (38.7) | 795 (39.0) | 95 (36.3) | 475 (40.5) | 125 (33.4) | 290 (38.4) | 467 (42.2) | 423 (35.4) | |||
| High resilient copers | 425 (18.4) | 386 (18.9) | 39 (14.9) | 214 (18.2) | 86 (23.0) | 125 (16.6) | 228 (20.6) | 197 (16.5) | |||
Abbreviations: COVID‐19, coronavirus disease‐2019; NCD, noncommunicable disease.
To include diabetes mellitus, hypertension, dyslipidemia, stroke and heart disease, chronic kidney disease, chronic lung disease, and cancer.
Defined according to the brief resilient coping scale: 4–13 points, low resilient copers; 14–16 points, moderate resilient copers; and 17–20, high resilient copers.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
3.2. Job loss and mental health status
Our results revealed that participants who reported losing their job had 51.9%, 56.9%, and 84.7% prevalence rates of depressive symptoms, anxiety symptoms, and perceived stress, respectively (Tables 2, 3, 4). Using a cut‐off PHQ‐9 value of 9 or above, job loss was a significant risk factor for depression compared to participants who maintained their job; however, the significance was diluted in model 3 (fully adjusted model), (adjusted OR, 1.51; 95% CI, 0.97–2.34; p = .070) (Table 2). Job loss was a significant risk factor for anxiety symptoms, with models 1 and 2 revealing adjusted ORs of 1.76 and 1.58, respectively (Table 3). However, when more covariates were incorporated in model 3, we only found a statistically nonsignificant trend of higher anxiety symptoms (adjusted OR, 1.39; 95% CI, 0.89–2.18; p = .146). According to the risk of perceived stress, job loss was a statistically significant risk factor for perceived stress in all models, with adjusted ORs of 2.19 (95% CI, 1.28–3.76; p = .004), 2.18 (95% CI, 1.24–3.83; p = .007), and 2.40 (95% CI, 1.28–4.51; p = .006) for models 1, 2, and 3, respectively (Table 4).
Table 2.
Economic burden during the COVID‐19 outbreak and the risk of depressive symptoms
| Economic burden | No. of cases/no. of total (%) | PHQ‐9 score, mean ± SD (median, min–max) | Depression (PHQ‐9 value of ≥9 points) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | |||||||
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | ||||
| Job loss | |||||||||
| No | 705/2,041 (34.5) | 6.9 ± 5.8 (6, 0 – 27) | Reference (1.00) | Reference (1.00) | Reference (1.00) | ||||
| Yes | 136/262 (51.9) | 9.8 ± 6.2 (9, 0–27) | 1.68 (1.13–2.49) | .010 | 1.51 (1.00–2.28) | .048 | 1.51 (0.97–2.34) | .070 | |
| Income loss | |||||||||
| No | 378/1,174 (32.2) | 6.4 ± 5.5 (5, 0–27) | Reference (1.00) | Reference (1.00) | Reference (1.00) | ||||
| Monthly income loss of <50% | 137/374 (36.6) | 7.3 ± 5.8 (6, 0–27) | 1.26 (0.87–1.82) | .230 | 1.31 (0.87–1.96) | .199 | 1.43 (0.94–2.16) | .090 | |
| Monthly income loss of ≥50% | 326/755 (43.2) | 8.4 ± 6.3 (7, 0–27) | 1.38 (1.05–1.80) | .020 | 1.23 (0.91–1.68) | .182 | 1.36 (0.98–1.88) | .063 | |
| Self‐reported financial problems | |||||||||
| No | 321/1,107 (29.0) | 6.1 ± 5.3 (5, 0–27) | Reference (1.00) | Reference (1.00) | Reference (1.00) | ||||
| Yes | 520/1,196 (43.5) | 8.3 ± 6.2 (7, 0–27) | 1.80 (1.40–2.30) | <.001 | 1.78 (1.33–2.38) | <.001 | 1.84 (1.34–2.51) | <.001 | |
Note: The ORs corresponding to 95% CIs are presented weighted according to the national population and the rate of internet use in Thailand.
Abbreviations: CI, confidence interval; COVID‐19, coronavirus disease‐2019; OR, odds ratio; PHQ‐9, Patient Health Questionnaire—9‐items.
Model 1 adjusted for age and sexual identity.
Model 2 adjusted for model plus marital status, education level, religion, region, living status, reimbursement scheme, history of mental illness, history of chronic non‐communicable diseases, and debt.
Model 3 adjusted for model 2 plus information exposure during the COVID‐19 outbreak, confirmed cases in the community, quarantine status, and resilient coping.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Table 3.
Economic burden during the COVID‐19 outbreak and the risk of anxiety symptoms
| Economic burden | No. of cases/no. of total (%) | GAD‐7 score, mean ± SD (median, min–max) | Anxiety (GAD‐7 value of ≥5 points) | |||||
|---|---|---|---|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | ||||||
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |||
| Job loss | ||||||||
| No | 795/2,041 (39.0) | 4.2 ± 4.5 (3, 0–21) | Reference (1.00) | Reference (1.00) | Reference (1.00) | |||
| Yes | 149/262 (56.9) | 6.1 ± 5.0 (5, 0–21) | 1.76 (1.18–2.60) | .005 | 1.58 (1.05–2.38) | .028 | 1.39 (0.89–2.18) | .146 |
| Income loss | ||||||||
| No | 428/1,174 (36.4) | 3.8 ± 4.1 (3. 0–21) | Reference (1.00) | Reference (1.00) | Reference (1.00) | |||
| Monthly income loss of <50% | 143/374 (38.2) | 4.5 ± 4.6 (3, 0–21) | 0.94 (0.65–1.34) | .719 | 0.94 (0.64–1.38) | .739 | 0.99 (0.67–1.47) | .960 |
| Monthly income loss of ≥50% | 373/755 (49.4) | 5.3 ± 5.1 (4, 0–21) | 1.50 (1.15–1.95) | .003 | 1.34 (0.99–1.81) | .057 | 1.42 (1.03–1.99) | .035 |
| Self‐reported financial problems | ||||||||
| No | 341/1,107 (30.8) | 3.5 ± 4.1 (2, 0–21) | Reference (1.00) | Reference (1.00) | Reference (1.00) | |||
| Yes | 603/1,196 (50.4) | 5.3 ± 4.8 (5, 0–21) | 2.14 (1.68–2.72) | <.001 | 2.09 (1.58–2.77) | <.001 | 2.00 (1.48–2.71) | <.001 |
Note: The ORs corresponding to 95% CIs are presented weighted according to the national population and the rate of internet use in Thailand.
Abbreviations: CIs, confidence intervals; COVID‐19, coronavirus disease‐2019; GAD‐7, Generalized Anxiety Disorder—7‐items; OR, odds ratio.
Model 1 adjusted for age and sexual identity.
Model 2 adjusted for model plus marital status, education level, religion, region, living status, reimbursement scheme, history of mental illness, history of chronic noncommunicable diseases, and debt.
Model 3 adjusted for model 2 plus information exposure during the COVID‐19 outbreak, confirmed cases in the community, quarantine status, and resilient coping.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Table 4.
Economic burden during the COVID‐19 outbreak and the risk of perceived stress
| Economic burden | No. of cases/no. of total (%) | PSS‐10 score, mean ± SD (median, min–max) | Stress (PSS‐10 value of ≥14 points) | |||||
|---|---|---|---|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | ||||||
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |||
| Job loss | ||||||||
| No | 1,422/2,041 (69.7) | 16.5 ± 6.6 (17, 0–40) | Reference (1.00) | Reference (1.00) | Reference (1.00) | |||
| Yes | 222/262 (84.7) | 19.6 ± 6.4 (19, 4–37) | 2.19 (1.28–3.76) | .004 | 2.18 (1.24–3.83) | .007 | 2.40 (1.28–4.51) | .006 |
| Income loss | ||||||||
| No | 793/1,174 (67.5) | 15.8 ± 6.4 (16, 0–38) | Reference (1.00) | Reference (1.00) | Reference (1.00) | |||
| Monthly income loss of <50% | 259/374 (69.2) | 16.8 ± 6.9 (17, 0–40) | 1.23 (0.84–1.80) | .282 | 1.26 (0.85–1.86) | .254 | 1.37 (0.89–2.09) | .148 |
| Monthly income loss of ≥50% | 592/755 (78.4) | 18. 4 ± 6.5 (19, 3–38) | 1.30 (0.95–1.78) | .099 | 1.17 (0.83–1.66) | .372 | 1.44 (0.98–2.13) | .066 |
| Self‐reported financial problems | ||||||||
| No | 685/1,107 (61.9) | 15.1 ± 6.5 (16, 0 – 40) | Reference (1.00) | Reference (1.00) | Reference (1.00) | |||
| Yes | 959/1,196 (80.2) | 18.4 ± 6.3 (18, 0 – 38) | 2.20 (1.66–2.89) | <.001 | 1.97 (1.46–2.66) | <.001 | 2.12 (1.51–2.95) | <.001 |
Note: The ORs corresponding to 95% CIs are presented weighted according to the national population and the rate of internet use in Thailand.
Abbreviations: CIs, confidence intervals; COVID‐19, coronavirus disease‐2019; OR, odds ratio; PSS‐10, Perceived Stress Scale—10‐items.
Model 1 adjusted for age and sexual identity.
Model 2 adjusted for model plus marital status, education level, religion, region, living status, reimbursement scheme, history of mental illness, history of chronic noncommunicable diseases, and debt.
Model 3 adjusted for model 2 plus information exposure during the COVID‐19 outbreak, confirmed cases in the community, quarantine status, and resilient coping.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
3.3. Income loss and mental health status
We grouped the participants into those with or without income loss with 50% of lost income as the cut‐off point. Participants with a monthly income loss of less than 50% and 50% or above had the following prevalence rates: 36.6% and 43.2%, for depressive symptoms; 38.2% and 49.4%, for anxiety symptoms; and 69.2% and 78.4%, for perceived stress, respectively (Tables 2, 3, 4). Income loss showed a slight association with depressive symptoms when no income loss was used as a reference group. Among the three models in Table 2, only the group reporting a monthly income loss of 50% or lesser had a significant association with depression (adjusted OR, 1.38; 95% CI, 1.05–1.80; p = .020 (model 1). This significant association was lost in models 2 and 3. Compared with no income loss, participants with a monthly income loss of 50% or more had a significant association with anxiety symptoms: adjusted ORs of 1.50 (95% CI; 1.15–1.95, p = .003) in model 1 and 1.42 (95% CI; 1.03–1.99, p = .035) in model 3. After dividing the participants into two groups according to PSS‐10 scores, income loss was not a statistically significant risk factor for perceived stress in any of the models (Table 4).
3.4. Financial problems and mental health status
Results revealed that 43.5%, 50.4%, and 80.2% of the participants with self‐reported financial problems developed depressive symptoms, anxiety symptoms, and perceived stress, respectively (Tables 2, 3, 4). Further analyses of the relationship between self‐reported financial problems and depressive symptoms, anxiety symptoms, and perceived stress showed statistically significant differences in all aspects after adjusting for various confounders (all models). The adjusted ORs for depressive symptoms were 1.80 (95% CI, 1.40–2.30; p < .001), 1.78 (95% CI, 1.33–2.38; p < .001), and 1.84 (95% CI, 1.34–2.51; p < .001) in models 1, 2, and 3, respectively (Table 2). The adjusted ORs for anxiety symptoms were 2.14 (95% CI, 1.68–2.72; p < .001), 2.09 (95% CI, 1.58–2.77; p < .001), and 2.00 (95% CI, 1.48–2.71; p < .001) in models 1, 2, and 3, respectively (Table 3). Finally, the risk of perceived stress had a positive association with self‐reported financial problems, with adjusted ORs of 2.20 (95% CI, 1.66–2.89; p < .001), 1.97 (95% CI, 1.46–2.66; p < .001), and 2.12 (95% CI, 1.51–2.95; p < .001) in models 1, 2, and 3, respectively (Table 4).
4. DISCUSSION
To our knowledge, this study was the first to conduct a nationwide online survey to address the early effects of the economic burden caused by the COVID‐19 pandemic and the risk for adverse mental health outcomes among the general population in Thailand. Our findings showed that among the general population who were employed before the national lockdown, 11.4% ended up losing their jobs, whereas 16.2% and 32.8% reported monthly income losses of less than 50% and 50% or above, respectively. Moreover, 51.9% of the participants' self‐reported financial problems related to the COVID‐19 outbreak.
Before the COVID‐19 pandemic, a population‐based longitudinal study in the United States found that drops in household incomes were substantially associated with an increased risk for incident mood, anxiety, or substance use disorders (adjusted OR, 1.30; 95% CI, 1.06–1.60) (Sareen et al., 2011). Longitudinal studies have also revealed that housing payment problems and indebtedness have significant detrimental effects on mental wellbeing (Taylor et al., 2007) and increase the risk of depression (incidence density ratio [IDR], 2.4; 95% CI, 1.6–3.6) and anxiety (IDR, 1.9; 95% CI, 1.4–2.6) (McLaughlin et al., 2012). A cross‐sectional study based on the national working population sample in the United Kingdom showed that job insecurity (OR, 1.86; 95% CI, 1.47–2.35) and being in debt (OR, 2.17; 95% CI, 1.58–2.98) are significantly associated with depression (Meltzer et al., 2010). Furthermore, during the recession in Greece, people under stressful economic situations had a 1.33‐fold increased risk of developing a major depressive episode (Madianos et al., 2011).
During the COVID‐19 pandemic, several cross‐sectional studies have reported the effects of economic burden and mental health and psychosocial issues. A study of active members of the labor force of six European nations showed that individuals with an instant loss of income have a higher probability of reporting feelings of depression than those who maintained their income (33.2% vs. 21.5%; p < .001) (Witteveen & Velthorst, 2020). Furthermore, Wilson et al. (2020) found that job insecurity due to the COVID‐19 outbreak and financial concern among employed individuals in the United States are associated with greater depressive and anxiety symptoms. With regard to young adults in the United States who recently experienced employment loss, the estimated risk ratios for depression and anxiety were 1.22 (95% CI, 1.12–1.32; p < .001) and 1.25 (95% CI, 1.13–1.37; p < .001), respectively (Ganson et al., 2021).
In a particular population, a survey among 735 Italian dentists during the lockdown indicated that perceived job insecurity was positively associated with depressive symptoms (β coefficient, .58; 95% CI, 0.35–0.70; p < .001) (Gasparro et al., 2020). Thayer & Gildner, 2020 also found that individuals who experienced financial stress in relation to the COVID‐19 pandemic had a twofold increased risk of having clinically depressive symptoms (OR, 2.23; 95% CI, 1.80–2.77; p < .001).
Collectively, our findings expanded the literature on economic burden and mental health during the COVID‐19 pandemic. Individuals who lost their job had 2.40‐fold odds of higher perceived stress, whereas those who had a monthly income loss of 50% or above had a 1.42‐fold higher risk of developing anxiety symptoms. Self‐reported financial problems were substantially associated with adverse mental health outcomes: 1.84‐, 2.00‐, and 2.12‐fold higher levels of depressive symptoms, anxiety symptoms, and perceived stress, respectively. Our findings unsurprisingly showed the different impact of the three measures of economic burden on mental health, losing jobs or income loss had a lesser effect on mental health outcomes. This factor had the highest impact among participants with self‐reported financial problems related to the COVID‐19 outbreak. With regard to the economic burden, self‐reported financial problems are the subjective indicator that reflects the perception of financial strain, a powerful factor of onset and duration of mental health episodes, more than the objective indicators (i.e., loss of job and income) (Weich & Lewis, 1998).
We postulated that individuals with economic burden may experience widespread social inequality and financial exclusion in terms of socioeconomic status, education, employment, public health coverage (reimbursement scheme or health insurance), housing, and access to recognized financial services (i.e., resorting to loan sharking, or illegal loans). Thus, inequalities and poverty levels may mediate the temporal link between economic stress and unemployment and adverse mental health outcomes contingent on the economic burden during the COVID‐19 outbreak.
Our findings show the early effects of the COVID‐19 pandemic and provide important insights into the economic burden indices—job loss, income loss, and financial problems. The study was conducted considering the public mental health response in Thailand, which is characterized by a high economic vulnerability in terms of the estimated percent change in real GDP growth below the world average (world GDP: −5.2; Thailand GDP: −7.1) (International Monetary Fund, 2020; World Bank, 2020), a high household debt‐to‐GDP ratio (Onthaworn, 2020), and high inbound tourism expenditure (% of GDP) (Kovacevic & Jahic, 2020).
Nonetheless, our study had several limitations. First, the evidence indicates the association between the consequences of the economic burden brought by the COVID‐19 pandemic and the risk of adverse mental health outcomes at the national level. As this study used cross‐sectional online survey data, we could not establish a causal relationship between economic burden and consequences of adverse mental health outcomes. Second, to prevent breaking physical distancing protocols, our findings were based on an open online survey, which can be prone to information bias and limit participants to only those who can access the Internet. Consequently, the effect estimates of our findings should be interpreted with caution. Additionally, as non‐Thai, part‐time employees were excluded from this study, the results may only generalize to the native Thai people's experiences who are/were fully employed and had access to the Internet. Lastly, this study focused on the period of the national lockdown and collected data on short‐term public responses to the COVID‐19 outbreak during the 1st phase of the pandemic in Thailand. As such, the findings only reflected the short‐term effects. Hence, further studies are warranted to examine the long‐term effect through a panel of Wave II, III, and IV data collection.
Despite the abovementioned limitations, our findings suggest the magnitude of the impacts of the economic burden on public mental health outcomes amid the COVID‐19 pandemic and global economic recession. In promoting public mental wellbeing, we underscore that early identification and effective assessment in individuals who are facing unemployment, debts and economic strain, and financial problems, particularly those who have a preexisting mental illness, may help optimize the planning of financial counseling, debt relief programs, family support programs, and interventions to enhance access to effective health coverage, financial organization, and utility companies.
As the study only focused on investigating the effects of the economic crisis on depressive symptoms, anxiety symptoms, and perceived stress, we were unable to examine its impact on substance use disorders as well as suicidal ideation and suicide attempts. Studies conducted before the COVID‐19 pandemic have revealed negative trends in these aspects during economic recessions (Frasquilho et al., 2016; Meltzer et al., 2011; Sareen et al., 2011). Hence, future public health surveys should pay attention to these issues. As the global economy can be expected to continue contracting, longitudinal studies are needed to explore the effects of economic stress and downturn and the subsequent risk of adverse mental health outcomes during and after an epidemic or a pandemic. In addition, such longitudinal surveys could also be supported by governments and public health officials to increase awareness and ensure the timely implementation of both financial and nonfinancial strategies.
5. CONCLUSION
Economic burden, especially self‐reported financial problems, was associated with all adverse mental outcomes, namely, depression symptoms, anxiety symptoms, and perceived stress in the first phase of the pandemic. Countries' policies for addressing the recession should focus on supporting people facing economic stress and unemployment. Compensation and reimbursement should be provided to individuals who are badly in need of these types of support and in a timely manner. Further studies are needed to determine effective strategies to manage the impacts of the COVID‐19 pandemic and economic turndown on mental health issues during and after such crises.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests. All the researchers involved performed this study in the context of their research.
AUTHOR CONTRIBUTIONS
Study concept/design study and study supervision, statistical analysis, drafting of the manuscript: Chidchanok Ruengorn and Surapon Nochaiwong. Administrative, technical, or material support: Chidchanok Ruengorn and Ratanaporn Awiphan. Critical revision of the manuscript for important intellectual content: Ratanaporn Awiphan, Nahathai Wongpakaran, and Tinakon Wongpakaran. All authors contributed acquisition, interpretation of data, and take responsibility for the integrity of the data and the accuracy of the data analysis.
ACKNOWLEDGMENTS
The authors thank the research assistances and all staff of Pharmacoepidemiology and Statistics Research Center (PESRC), Chiang Mai, Thailand. Particular thanks are given to the study participants for their contribution to the project. This study reported in this manuscript was partially supported by a grant from the Chiang Mai University, Thailand. The funder of the study had no role in the study design, data collection, analysis, and data interpretation, nor in the writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit it for publication. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the funders.
Ruengorn, C. , Awiphan, R. , Wongpakaran, N. , Wongpakaran, T. , & Nochaiwong, S . (2021). Association of job loss, income loss, and financial burden with adverse mental health outcomes during coronavirus disease 2019 pandemic in Thailand: A nationwide cross‐sectional study. Depression Anxiety. 38, 648–660. 10.1002/da.23155
Chidchanok Ruengorn and Surapon Nochaiwong contributed equally to this study.
DATA AVAILABILITY STATEMENT
Data will be shared upon reasonable request and with permission according to the Health Outcomes and Mental Health Care Evaluation Survey Research Group (HOME‐Survey) data release policy.
REFERENCES
- Burki, T. K. (2020). Coronavirus in China. Lancet Respiriratory Medicine, 8(3), 238. 10.1016/s2213-2600(20)30056-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drydakis, N. (2015). The effect of unemployment on self‐reported health and mental health in Greece from 2008 to 2013: A longitudinal study before and during the financial crisis. Social Science and Medicine, 128, 43–51. 10.1016/j.socscimed.2014.12.025 [DOI] [PubMed] [Google Scholar]
- Eysenbach, G. (2004). Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E‐Surveys (CHERRIES). Journal of Medical Internet Research, 6(3), e34. 10.2196/jmir.6.3.e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiori, F. , Rinesi, F. , Spizzichino, D. , & Di Giorgio, G. (2016). Employment insecurity and mental health during the economic recession: An analysis of the young adult labour force in Italy. Social Science and Medicine, 153, 90–98. 10.1016/j.socscimed.2016.02.010 [DOI] [PubMed] [Google Scholar]
- Frasquilho, D. , Matos, M. G. , Salonna, F. , Guerreiro, D. , Storti, C. C. , Gaspar, T. , & Caldas‐de‐Almeida, J. M. (2016). Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health, 16, 115. 10.1186/s12889-016-2720-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganson, K. T. , Tsai, A. C. , Weiser, S. D. , Benabou, S. E. , & Nagata, J. M. (2021). Job insecurity and symptoms of anxiety and depression among U.S. young adults during COVID‐19. Journal of Adolescent Health, 68(1), 53–56. 10.1016/j.jadohealth.2020.10.008 [DOI] [PubMed] [Google Scholar]
- Gasparro, R. , Scandurra, C. , Maldonato, N. M. , Dolce, P. , Bochicchio, V. , Valletta, A. , Sammartino, G. , Sammartino, P. , Mariniello, M. , di Lauro, A. E. , & Marenzi, G. (2020). Perceived job insecurity and depressive symptoms among Italian dentists: The moderating role of fear of COVID‐19. International Journal of Environmental Research and Public Health, 17(15), 5338. 10.3390/ijerph17155338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Monetary Fund . (2020). World economic outlook: A long and difficult ascent. International Monetary Fund. [Google Scholar]
- Jenkins, R. , Bhugra, D. , Bebbington, P. , Brugha, T. , Farrell, M. , Coid, J. , Fryers, T. , Weich, S. , Singleton, N. , & Meltzer, H. (2008). Debt, income and mental disorder in the general population. Psychological Medicine, 38(10), 1485–1493. 10.1017/s0033291707002516 [DOI] [PubMed] [Google Scholar]
- Kleinbaum, D. G. , & Klein, M. (2010). Chapter 6: Modeling strategy guidelines. In Kleinbaum D. G., & Klein M. (Eds.), Logistic regression: A self‐learning text (3rd ed., pp. 165–202). Springer Science+Business Media LLC. [Google Scholar]
- Kovacevic, M. , & Jahic, A. (2020). COVID‐19 and human development: Exploring global preparedness and vulnerability. Human Development Report Office, UNDP. [Google Scholar]
- Lotrakul, M. , Sumrithe, S. , & Saipanish, R. (2008). Reliability and validity of the Thai version of the PHQ‐9. BMC Psychiatry, 8, 46. 10.1186/1471-244x-8-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madianos, M. , Economou, M. , Alexiou, T. , & Stefanis, C. (2011). Depression and economic hardship across Greece in 2008 and 2009: Two cross‐sectional surveys nationwide. Social Psychiatry and Psychiatric Epidemiology, 46(10), 943–952. 10.1007/s00127-010-0265-4 [DOI] [PubMed] [Google Scholar]
- Mahase, E. (2020). Covid‐19: WHO declares pandemic because of "alarming levels" of spread, severity, and inaction. British Medical Journal, 368, m1036. 10.1136/bmj.m1036 [DOI] [PubMed] [Google Scholar]
- McLaughlin, K. A. , Nandi, A. , Keyes, K. M. , Uddin, M. , Aiello, A. E. , Galea, S. , & Koenen, K. C. (2012). Home foreclosure and risk of psychiatric morbidity during the recent financial crisis. Psychological Medicine, 42(7), 1441–1448. 10.1017/s0033291711002613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer, H. , Bebbington, P. , Brugha, T. , Jenkins, R. , McManus, S. , & Dennis, M. S. (2011). Personal debt and suicidal ideation. Psychological Medicine, 41(4), 771–778. 10.1017/s0033291710001261 [DOI] [PubMed] [Google Scholar]
- Meltzer, H. , Bebbington, P. , Brugha, T. , Jenkins, R. , McManus, S. , & Stansfeld, S. (2010). Job insecurity, socio‐economic circumstances and depression. Psychological Medicine, 40(8), 1401–1407. 10.1017/s0033291709991802 [DOI] [PubMed] [Google Scholar]
- Mongkhon, P. , Ruengorn, C. , Awiphan, R. , Thavorn, K. , Hutton, B. , Wongpakaran, N. , Wongpakaran, T. , & Nochaiwong, S. (2021). Exposure to COVID‐19‐related information and its association with mental health problems in Thailand: Nationwide, cross‐sectional survey study. Journal of Medical Internet Research, 23(2), e25363. 10.2196/25363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nochaiwong, S. , Ruengorn, C. , Awiphan, R. , Ruanta, Y. , Boonchieng, W. , Nanta, S. , Kowatcharakul, W. , Pumpaisalchai, W. , Kanjanarat, P. , Mongkhon, P. , Thavorn, K. , Hutton, B. , Wongpakaran, N. , & Wongpakaran, T. (2020). Mental health circumstances among health care workers and general public under the pandemic situation of COVID‐19 (HOME‐COVID‐19). Medicine (Baltimore), 99(26), e20751. 10.1097/md.0000000000020751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'brien, R. M. (2007). A caution regarding rules of thumb for variance inflation factors. Quality & Quantity, 41(5), 673–690. 10.1007/s11135-006-9018-6 [DOI] [Google Scholar]
- Onthaworn, P. (2020). Kasikorn predicts household debt to GDP could rise to 90 percent. https://www.thaienquirer.com/15601/kasikorn-predicts-household-debt-to-gdp-could-rise-to-90-per-cent/
- Parmar, D. , Stavropoulou, C. , & Ioannidis, J. P. (2016). Health outcomes during the 2008 financial crisis in Europe: Systematic literature review. British Medical Journal, 354, i4588. 10.1136/bmj.i4588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sareen, J. , Afifi, T. O. , McMillan, K. A. , & Asmundson, G. J. (2011). Relationship between household income and mental disorders: Findings from a population‐based longitudinal study. Archives of General Psychiatry, 68(4), 419–427. 10.1001/archgenpsychiatry.2011.15 [DOI] [PubMed] [Google Scholar]
- Silva, M. , Resurrección, D. M. , Antunes, A. , Frasquilho, D. , & Cardoso, G. (2018). Impact of economic crises on mental health care: A systematic review. Epidemiology and Psychiatric Sciences, 29, e7. 10.1017/s2045796018000641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair, V. G. , & Wallston, K. A. (2004). The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment, 11(1), 94–101. 10.1177/1073191103258144 [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L. , Kroenke, K. , Williams, J. B. , & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD‐7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Taylor, M. P. , Pevalin, D. J. , & Todd, J. (2007). The psychological costs of unsustainable housing commitments. Psychological Medicine, 37(7), 1027–1036. 10.1017/s0033291706009767 [DOI] [PubMed] [Google Scholar]
- Thayer, Z. M. , & Gildner, T. E. (2020). COVID‐19‐related financial stress associated with higher likelihood of depression among pregnant women living in the United States. American Journal of Human Biology. Advance online publication. e23508. 10.1002/ajhb.23508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbanos‐Garrido, R. M. , & Lopez‐Valcarcel, B. G. (2015). The influence of the economic crisis on the association between unemployment and health: An empirical analysis for Spain. The European Journal of Health Economics, 16(2), 175–184. 10.1007/s10198-014-0563-y [DOI] [PubMed] [Google Scholar]
- von Elm, E. , Altman, D. G. , Egger, M. , Pocock, S. J. , Gøtzsche, P. C. , & Vandenbroucke, J. P. (2007). Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. British Medical Journal, 335(7624), 806–808. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weich, S. , & Lewis, G. (1998). Poverty, unemployment, and common mental disorders: Population‐based cohort study. British Medical Journal, 317(7151), 115–119. 10.1136/bmj.317.7151.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson, J. M. , Lee, J. , Fitzgerald, H. N. , Oosterhoff, B. , Sevi, B. , & Shook, N. J. (2020). Job insecurity and financial concern during the COVID‐19 pandemic are associated with worse mental health. Journal of Occupational and Environmental Medicine, 62(9), 686–691. 10.1097/jom.0000000000001962 [DOI] [PubMed] [Google Scholar]
- Witteveen, D. , & Velthorst, E. (2020). Economic hardship and mental health complaints during COVID‐19. Proceedings of the National Academy of Sciences of the United States of America, 117, 27277–27284. 10.1073/pnas.2009609117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wongpakaran, N. , & Wongpakaran, T. (2010). The Thai version of the PSS‐10: An investigation of its psychometric properties. BioPsychoSocial Medicine, 4, 6. 10.1186/1751-0759-4-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank . (2020). Global economic prospects, June 2020. World Bank. [Google Scholar]
- World Health Organization . (2020). WHO Coronavirus Disease (COVID‐19) Dashboard. https://covid19.who.int/
- World Health Organization: Regional Office for Europe . (2011). Impact of economic crises on mental health. World Health Organization: Regional Office for Europe. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be shared upon reasonable request and with permission according to the Health Outcomes and Mental Health Care Evaluation Survey Research Group (HOME‐Survey) data release policy.


