Abstract
Objectives
The aim of this study was to explore factors that influence individuals' attitudes towards mandatory vaccination in Greece.
Methods
A nationally representative cross‐sectional telephone survey was conducted via a random multistage selection process in October 2019 in Greece. The survey was designed to obtain information about whether vaccination should be mandated or not among adults 18 years of age or older. A multivariable logistic regression model was used to estimate the association between individuals' sociodemographic, contextual and clinical characteristics, utilization, satisfaction, and trust in the healthcare system and providers and their preference over mandatory vaccination.
Results
A total of 901 participants fully completed the survey (response rate 90%‐901/1001). About 85% of the respondents supported mandatory vaccination. Individuals who used preventive services more often compared to those who never or rarely used such, those who reported increased trust in official healthcare authorities' guidelines and recommendations compared to those who reported no trust and those who had underage children living in the household were significantly more likely to support mandatory vaccination. No differences were observed for sociodemographic factors and mandatory vaccination support.
Conclusion
This survey revealed that most Greek citizens support mandatory vaccination, which was critically affected by the utilization of preventive services and trust in healthcare authorities. Our results suggest that healthcare policy interventions should promote mandatory vaccination through multi‐level initiatives to improve healthcare providers' and the general public's understanding of the value of vaccination.
Keywords: disease prevention, hesitancy, infectious diseases, patient preferences, public health, vaccination
1. INTRODUCTION
Vaccination is widely recognized as one of the most cost‐effective medical interventions that has historically reduced and even eradicated the incidence of many preventable infectious diseases protecting millions of people. 1 , 2 , 3 Despite the wide recognition of the health, economic, and societal benefits of mass vaccination, large variation and gaps continue to exist in vaccination policies and uptake rates across countries, thus raising the risk of exposure and transmission of preventable infections. 4
Efficacious vaccination requires high‐rates of acceptance and adherence to guidelines and recommendations by healthcare professionals and by the general population in particular. 5 Globally, only a small share of individuals perceives vaccines as not safe. 6 However, trust in vaccines varies across different countries. In France, Switzerland, Belgium, Gabon, Togo, Russia, and Austria more than 20% of the general population were sceptical about vaccination safety. 6
Vaccination rates in Greece are among the highest globally and only a small share of Greek citizens questioned the effectiveness of vaccination. 6 , 7 , 8 Most vaccines for preventable diseases are covered by the national health insurance system at no cost, thus enhancing access to such services by eliminating financial barriers. As of March 2020, vaccination for transmittable diseases is legally mandated in Greece, however, some vaccines such as those for meningitis‐B are still in the discretion of individuals and are not reimbursed. 9 Despite the high vaccination uptake, evidence in Greece has revealed differential attitudes and suboptimal completed vaccination rates even among healthcare professionals. 10 , 11 , 12 , 13 In addition, a large share of Greek citizens perceives that vaccination is necessary only for children, thus increasing the susceptibility of adults. 14
The existing variability in vaccination even within countries implies that there is a complex interplay of systemic and individual factors influencing uptake. 15 , 16 In recent years, vaccine hesitancy, the refusal, delay or uncertainty about vaccines, has emerged as a term and has received significant attention, with arguments about the safety of vaccines focusing on the perceived risks of vaccines instead of their well‐documented benefits. 15 , 17 , 18 Several factors influence and have been associated with vaccine‐hesitant behaviours, ranging from socioeconomic characteristics, perceived susceptibility, cultural, behavioural and emotional factors, to trust to healthcare systems, governments and information sources. 16 , 19 , 20 , 21 , 22 , 23
The most common source of vaccine information are healthcare providers, and health information credibility stemming from trustworthy providers as well as frequent interaction with the healthcare system was found to positively influence vaccination uptake. 16 , 20 , 21 , 24 , 25 In recent years the Internet has emerged as an important source of information on vaccines as well. However, most of the available online vaccine information contains antivaccine content, and vaccine myths and harms are especially prevalent on the Internet and social networking sites. 26 , 27 , 28 , 29 In fact, the use of the Internet as the primary source of healthcare information was associated with questioning the information accuracy and credibility of healthcare providers, professional organizations, and governmental health departments and in turn with decreased vaccination acceptance. 5
The purpose of this study was to explore factors associated with individuals' perspectives on mandatory vaccination in Greece. To our knowledge, this is the first study to estimate how individuals' attitudes towards the healthcare system and authorities influence mandatory vaccination preference using the most recent data available for the Greek population, beyond their sociodemographic, contextual and clinical characteristics. As such, our findings can contribute to public health planning in Greece.
2. MATERIALS AND METHODS
2.1. Data collection and study population
This study was a cross‐sectional telephone survey conducted in October 2019 in Greece to obtain information on attitudes towards mandatory vaccination among Greek citizens, as part of a larger‐scale project on preferences for healthcare policy reforms. Criteria for participation included being 18 years of age or older, residing permanently in Greece and fluency in the Greek language since the survey was conducted in Greek. The sample was randomly selected from the National Telephone Company Directory, categorized based on the National Census by region, municipality, and urbanization level and stratified proportionately according to the 13 administrative regions in the country. The survey was carried out by a commercial company working in the field of demographic surveys and the process was supported by the specialized software computer‐assisted telephone interviewing (CATI). Calls were made during both weekdays and weekends, during morning and evening hours. In cases where individuals did not pick up, at least 6 callbacks were made.
2.2. Study variables
The outcome of interest was whether individuals supported mandatory vaccination or not, defined as a dichotomous indicator (0 = No, 1 = Yes). The question was phrased as “Do you believe that vaccination should be mandatory or in the discretion of each individual?”.
Multiple independent variables were obtained to explore their association with the outcome variable of the study. These included: (a) sociodemographic and contextual characteristics, namely age, gender, education, occupation, income, area of residence, and insurance status, (b) health‐related characteristics, namely self‐reported health and whether the respondent had any chronic condition, (c) whether underage children resided currently in the household, (d) information regarding trust and satisfaction with the healthcare system and utilization of preventive healthcare services, which were obtained by asking participants to respond to the three Likert‐scale questions. All variables were measured as categorical or dichotomous.
2.3. Statistical analysis
Descriptive analysis was initially conducted to present characteristics of all study participants and preferences over mandatory vaccination using percentage points. We then conducted bivariate analyses on all independent variables stratified on whether respondents supported mandatory vaccination or not. We tested for statistical differences in the stratified mandatory vaccination preference using Pearson χ2 test. Finally, to estimate the association between respondents' characteristics, their healthcare system attitudes and utilization patterns and their opinion on whether vaccination should be mandated or not, a multivariable logistic regression was used. We controlled for unobserved time‐invariant regional characteristics using geographic‐level fixed effects. Standard errors were clustered at the geographical region of residence. A P‐value <.05 was considered as statistically significant. All statistical analyses were conducted using Stata (version 16.1; StataCorp, College Station, TX). The study was approved by the Ethics Committee of the University of Peloponnese.
3. RESULTS
A total of 1001 individuals were approached and participated in the survey. Of those, 44 participants (4.4%) did not respond to the question regarding mandatory vaccination while 56 (5.6%) did not fully complete the survey. This resulted in 901 respondents, who comprised the final analytic sample for this study (response rate 90.0%).
3.1. Sociodemographic, contextual and health‐related characteristics of participants
About half of the respondents were 25 to 54 years of age (52.3%), employed full‐time (50.6%) and reported average incomes (41.7%), while gender was balanced (Table 1). About 42% had high‐school level education, while a similar share had university‐level education. Underage children resided in about one‐quarter (24.1%) of the respondents' households. The majority had compulsory health insurance coverage (95.3%), while 14.0% had additional private insurance coverage. Most participants reported having good health status (46.2%), while 5.2% perceived their health status as bad or very bad. Overall, 43.1% had at least one existing chronic condition.
TABLE 1.
Descriptive characteristics and information of all participants overall and stratified by mandatory vaccination support
| Should vaccination be mandated? | All (n = 901) | No (n = 148) | Yes (n = 753) | P‐value |
|---|---|---|---|---|
| % | 14.8 | 85.2 | ||
| Gender (%) | .020 | |||
| Male | 50.7 | 59.5 | 49.0 | |
| Female | 49.3 | 40.5 | 51.0 | |
| Age groups (%) | <.001 | |||
| 18 to 24 | 11.8 | 3.4 | 13.4 | |
| 25 to 39 | 26.5 | 29.7 | 25.9 | |
| 40 to 54 | 25.8 | 37.2 | 23.5 | |
| 55 to 64 | 15.4 | 10.1 | 16.5 | |
| ≥65 | 20.5 | 19.6 | 20.7 | |
| Education (%) | .685 | |||
| Elementary | 7.9 | 8.8 | 7.7 | |
| High School | 42.3 | 39.2 | 42.9 | |
| University | 41.7 | 41.9 | 41.7 | |
| MSc/PhD | 8.1 | 10.1 | 7.7 | |
| Occupation (%) | <.001 | |||
| Full‐time | 50.6 | 65.5 | 47.8 | |
| Retired | 26.9 | 23.6 | 27.5 | |
| Other (student, housewife) | 15.3 | 6.8 | 17.0 | |
| Unemployed | 7.2 | 4.1 | 7.7 | |
| Underage children living in the household (%) | .443 | |||
| No | 75.9 | 78.4 | 75.4 | |
| Yes | 24.1 | 21.6 | 24.6 | |
| Chronic conditions (at least one) (%) | .033 | |||
| No | 56.9 | 64.9 | 55.4 | |
| Yes | 43.1 | 35.1 | 44.6 | |
| Rural residence (%) | .126 | |||
| No | 76.9 | 81.8 | 76.0 | |
| Yes | 23.1 | 18.2 | 24.0 | |
| Income (%) | .950 | |||
| Very low | 27.9 | 27.0 | 28.0 | |
| Low to average | 18.5 | 19.6 | 18.3 | |
| Average | 41.7 | 42.6 | 41.6 | |
| Higher than average | 11.9 | 10.8 | 12.1 | |
| Uninsured (%) | .216 | |||
| No | 95.3 | 97.3 | 95.0 | |
| Yes | 4.7 | 2.7 | 5.0 | |
| Do you have private insurance coverage? (%) | .484 | |||
| No | 86.0 | 87.8 | 85.7 | |
| Yes | 14.0 | 12.2 | 14.3 | |
| Self‐reported health (%) | .528 | |||
| Average | 21.2 | 25.0 | 20.5 | |
| Bad/very bad | 5.2 | 5.4 | 5.2 | |
| Good | 46.2 | 41.2 | 47.1 | |
| Very good | 27.4 | 28.4 | 27.2 | |
| Trust in official healthcare authorities' guidelines and recommendations on healthcare issues (ie, vaccination) (%) | <.001 | |||
| No trust | 9.1 | 20.3 | 6.9 | |
| Somewhat | 19.3 | 31.8 | 16.9 | |
| Quite | 42.2 | 31.0 | 44.3 | |
| A lot | 29.4 | 16.9 | 31.9 | |
| How often do you use healthcare preventive services (ie, checkup)? (%) | .002 | |||
| Never/Rarely | 26.5 | 38.5 | 24.2 | |
| Few times | 33.3 | 32.4 | 33.4 | |
| Often | 33.4 | 24.3 | 35.2 | |
| Very often | 6.8 | 4.7 | 7.2 | |
| How satisfied are you with the healthcare system? (%) | .011 | |||
| Not at all | 22.0 | 26.7 | 21.3 | |
| Somewhat | 47.4 | 54.0 | 46.0 | |
| Quite/Very satisfied | 30.6 | 20.3 | 32.7 |
3.2. Healthcare system satisfaction, trust to authorities and utilization of preventive healthcare services
Among all respondents, 47.4% were somewhat satisfied with the healthcare system, 30.6% were satisfied or very satisfied, while 22.0% were not satisfied at all. In terms of trust in official healthcare authorities' guidelines and recommendations on healthcare issues such as vaccination, 42.2% quite trusted authorities, 29.4% placed a lot of trust in them, while 9.1% did not trust healthcare authorities at all. About one‐third (33.3%) utilized preventive healthcare services (ie, check‐ups) a few times every year and a similar proportion (33.4%) reported that they used such services often. In contrast, 26.5% indicated that they rarely or never used preventive services.
3.3. Mandatory vaccination support
Table 1 also presents results of the stratified analysis by the difference in mandatory vaccination responses (Table 1). Overall, 85.2% of participants supported mandatory vaccination. Individuals who supported mandatory vaccination had higher shares of those who trusted official healthcare authorities' guidelines and recommendations on healthcare issues such as vaccination (P < .001) (Figure 1A) and those who used preventive healthcare services more often (P = .002) (Figure 1B). Participants who were more satisfied with the healthcare system were disproportionately higher represented in the mandatory vaccination supporting group (P = .011) (Figure 1C). Similarly, the mandatory vaccination supporters had higher percentages of individuals with at least one chronic condition (P = .033), females (P = .020), and those who were 18 to 24 years of age (P < .001), while the opposite was observed for those employed full‐time (P < .001).
FIGURE 1.
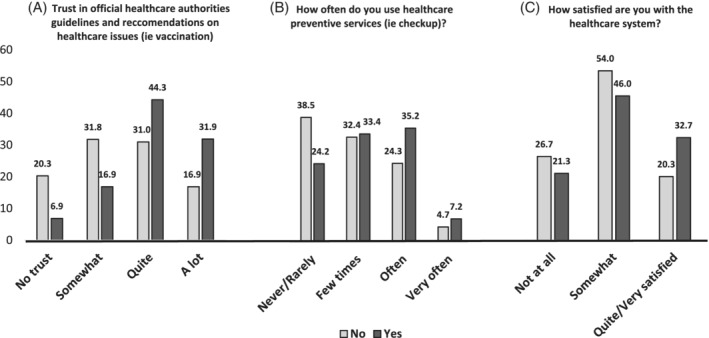
Percentages of participants by mandatory vaccination support (yes) or not (no) related to trust in official healthcare authorities' guidelines and recommendations on healthcare issues, frequency of preventive services utilization, and satisfaction with the healthcare system. A, Trust in official healthcare authorities guidelines and recommendations on healthcare issues (ie vaccination). B, How often do you use healthcare preventive services (ie checkup)? C, How satisfied are you with the healthcare system?
3.4. Determinants of mandatory vaccination support
The results of the multivariable logistic regression analysis are presented in Table 2. Compared to those who did not trust official healthcare authorities' recommendation and guidelines on healthcare issues, individuals who reported a lot or quite some trust in authorities were significantly more likely to support mandatory vaccination (a lot: adjusted Odds Ratio ‐ OR = 5.72, 95% Confidence Intervals ‐ CI = 2.82‐11.62, P < .001; quite: OR = 4.57, 95% CI = 2.40‐8.67, P < .001). Participants who reported more frequent use of preventive services were also more likely to support mandatory vaccination compared to those who never or rarely used such services, particularly those who indicated that they utilize preventive services often (OR = 2.24, 95% CI = 1.29‐3.89, P = .004) or very often (OR = 2.42, 95% CI = 1.02‐5.78, P = .046). A similar association was also observed for individuals who indicated that an underage child resided in the household (OR = 1.84, 95% CI = 1.07‐3.16, P = .028) and for those who reported that their health status was very good or good, although statistical significance was found only for those with good self‐reported health (OR = 1.89, 95% CI = 1.14‐3.14, P = .014). In contrast, participants who were 25 years of age or older were less likely to support mandatory vaccination, compared to those who 18 to 24 years old. We did not observe any significant association between other independent variables and mandatory vaccination in the multivariable analysis.
TABLE 2.
Multivariable logistic regression for mandatory vaccination support
| Trust in official healthcare authorities' guidelines and recommendations on healthcare issues (ie, vaccination) (Ref.: No trust) | OR | 95% CI | P‐value | |
|---|---|---|---|---|
| Somewhat | 1.65 | 0.88 | ‐ 3.12 | .120 |
| Quite | 4.57 | 2.40 | ‐ 8.67 | <.001 |
| A lot | 5.72 | 2.82 | ‐ 11.62 | <.001 |
|
How often do you use healthcare preventive services (ie, checkup)? (Ref.: Never/Rarely) |
||||
| Few times | 1.38 | 0.87 | ‐ 2.19 | .170 |
| Often | 2.24 | 1.29 | ‐ 3.89 | .004 |
| Very often | 2.42 | 1.02 | ‐ 5.78 | .046 |
| How satisfied are you with the healthcare system? (Ref.: Somewhat) | ||||
| Not at all | 1.13 | 0.70 | ‐ 1.83 | .626 |
| Quite/Very satisfied | 1.61 | 0.95 | ‐ 2.75 | .077 |
| Underage children living in the household (Ref.: No) | ||||
| Yes | 1.84 | 1.07 | ‐ 3.16 | .028 |
| Age groups (Ref.: 18 to 24) | ||||
| 25 to 39 | 0.23 | 0.08 | ‐ 0.67 | .007 |
| 40 to 54 | 0.14 | 0.05 | ‐ 0.38 | <.001 |
| 55 to 64 | 0.44 | 0.14 | ‐ 1.42 | .169 |
| ≥65 | 0.22 | 0.06 | ‐ 0.73 | .014 |
| Self‐reported health (Ref.: Average) | ||||
| Bad/very bad | 1.17 | 0.43 | ‐ 3.19 | .755 |
| Good | 1.89 | 1.14 | ‐ 3.14 | .014 |
| Very good | 1.61 | 0.86 | ‐ 3.01 | .136 |
| Occupation (Ref.: Full‐time) | ||||
| Unemployed | 2.67 | 0.98 | ‐ 7.26 | .055 |
| Retired | 1.42 | 0.65 | ‐ 3.10 | .377 |
| Other (student, housewife) | 2.15 | 0.85 | ‐ 5.41 | .104 |
| Gender (Ref.: Male) | ||||
| Female | 1.35 | 0.90 | ‐ 2.00 | .143 |
| Income (Ref.: Very low) | ||||
| Low to average | 0.85 | 0.47 | ‐ 1.51 | .570 |
| Average | 0.83 | 0.50 | ‐ 1.37 | .464 |
| Higher than average | 0.74 | 0.36 | ‐ 1.53 | .419 |
| Chronic conditions (Ref.: No) | ||||
| Yes | 1.43 | 0.90 | ‐ 2.28 | .135 |
| Uninsured (Ref.: No) | ||||
| Yes | 1.69 | 0.53 | ‐ 5.36 | .371 |
| Do you have private insurance coverage? (Ref.: No) | ||||
| Yes | 1.20 | 0.65 | ‐ 2.25 | .559 |
| Rural residence (Ref.: No) | ||||
| Yes | 1.36 | 0.76 | ‐ 2.46 | .301 |
| Education (Ref.: University) | ||||
| Elementary | 0.58 | 0.26 | ‐ 1.28 | .177 |
| High School | 1.30 | 0.80 | ‐ 2.12 | .284 |
| MSc/PhD | 1.06 | 0.50 | ‐ 2.26 | .874 |
Note: The regression model controls for geographic‐level fixed effects.
Abbreviations: OR, Adjusted odds ratio; CI, confidence intervals; Ref., reference.
4. DISCUSSION
The results of our study based on a random and nationally representative sample extend the current literature on preferences over mandatory vaccination in Greece and highlight the importance of understanding the factors that influence individuals' attitudes towards vaccination. These findings are critical to guide and tailor health‐policy interventions to address concerns, inform and support the rationale for vaccination and improve uptake. However, it is imperative for policymakers and authorities to first understand and identify population subgroups that are more sceptical and hesitant towards vaccines.
Our study reveals that almost 85% of participants supported mandatory vaccination. This finding is consistent and within the range of previous studies in Greece about acceptance of mandatory vaccination (65% to 97%) and similar to the proportion of Greek citizens who perceived vaccines as being effective and safe (87%). 6 , 10 , 30 The strongest predictors of mandatory vaccination support in our study were increased trust in official healthcare authorities' guidelines and recommendations (such as information on vaccines) and more frequent use of preventive services. Our findings are supported by previous work which found that interaction with healthcare providers and credible health information by trustworthy and reliable sources were commonly associated with acceptance and uptake of recommended vaccinations. 16 , 18 , 20 , 21 , 24 , 26 , 31 , 32 In fact, a review of the literature highlighted that the credibility of institutions might influence vaccination attitudes more than information. 32
Despite, there are still people who are uncertain and/or oppose a mandate to vaccinate. Mandating vaccination or coercive actions against such individuals restrict their liberty and autonomy and might not be ethically justifiable. However, even when public health threats are serious and the expected societal welfare and utility gains are high, multifaceted, least restrictive to individuals' liberties, and ethically justifiable approaches and interventions should be adopted that aim to balance between individuals' rights and the greater good. 33 , 34
Given the current vaccine developments for the coronavirus disease 2019 (COVID‐19) prevention, the importance of vaccination has received particular attention in the public context and has raised heated debates over mandating vaccines. Early evidence suggests that messages emphasizing the personal and collective health risks and consequences of not vaccinating increased individuals' intentions to vaccinate in the United States, while another study in the United Kingdom found that mistrust and concerns about vaccination benefits and poor adherence to preventive recommendations were associated with unwillingness to vaccinate against COVID‐19. 35 , 36 These findings are in‐line with the results of our study and shed light on the influential role of healthcare professionals and authorities to address and mitigate both long‐lasting and pandemic‐induced vaccine‐related public concerns through effective community outreach efforts and information dissemination.
Health professionals are the most influential and trusted source of information on vaccination. 20 Our findings highlight the need to support and educate healthcare professionals through coordinated efforts led by the national healthcare authorities, which have already been proven to improve vaccination uptake. 32 , 37 , 38 As vaccine scepticism and hesitancy increase, efforts to improve vaccination rates should focus on training health professionals not only on the benefits of vaccination but also on the provision of consistent and homogenous information in line with national guidelines. 39 , 40
Evidence from previous studies among healthcare professionals in Greece, and in other countries, has identified major knowledge deficits, with only 12.9% of healthcare workers correctly naming recommended vaccines, while almost half were not concerned about influenza infection and believed that they were not at risk of contracting such diseases. 10 , 11 , 13 , 30 , 41 Moreover, about one‐fifth questioned the effectiveness of vaccines. 13 Further, time limitations to counsel patients as well as some patients' overconfidence about their knowledge may also hinder efforts to build a patient‐provider relationship that is based on trust. 32 , 42 In particular, confidence about vaccines' knowledge was found to be highest among patients with lower levels of knowledge and was also associated with increased support for the involvement of non‐experts in policymaking processes. 42 Recent efforts by the Greek government to create a national vaccination registry will allow real‐time monitoring of compliance with vaccination schedule, which would, in turn, assist with targeted reminders and information provision.
We also found that healthier and younger individuals were more likely to support mandatory vaccination. Health status is a critical factor that affects the demand for health and medical care. Our finding is consistent with the human capital framework and implies that, in Greece, healthier individuals might be future‐oriented and acknowledge the benefits of vaccination and thus invest in preventive care to maintain their health status. 43 The presence of underage children in the household was also associated with increased mandatory vaccination preference. This could be related to the parental perception of their children's increased susceptibility to infectious diseases and, coupled with the existing pre‐school mandate for vaccination in Greece, might shape vaccination supporting attitudes. 44
We note that we did not observe any significant association between other socioeconomic factors such as gender, income, education and health insurance coverage and mandatory vaccination support. Similar results were also found by Coniglio and colleagues in Italy. 25 This finding might be related to the fact that the sample population in our study was random and representative of the overall Greek population, hence yielding different results compared to previous work among parents with young children in Greece. 19 Finally, the free‐of‐charge access to most vaccines in the country might also eliminate disparities and barriers to receive vaccinations among heterogeneous sociodemographic population subgroups.
This study is not without limitations. First, participants were recruited from the telephone household bank and recruitment was based on landline phones rather than mobile phones which might lead to sampling bias. However, more than 80% of Greek households have fixed telephone lines and our study sample was similar to national estimates, and thus representative of the Greek population. 45 Second, due to the study design, we cannot rule out some other sources of bias inherent in surveys, such as social desirability bias, and response bias. In addition, since the data used in this study were part of a larger‐scale project on public attitudes for healthcare policy reforms, we were not able to include other information and variables that might influence vaccinating decisions, such as receiving physician advice and past experiences with vaccines (ie, side effects), due to the absence of those in our data. We also highlight that the findings are relevant only to the Greek population and thus cannot be extrapolated to other countries. Finally, we highlight that our results are based on data collected in 2019 and thus might not fully generalizable to the current situation given the ongoing pandemic. Despite these limitations, our study results are supported by previous literature on mandatory vaccination preferences and thus present timely and critical evidence for healthcare authorities.
In conclusion, our study provides novel evidence on factors that critically affect the support of mandatory vaccination in Greece. The results indicate that despite the high support for mandatory vaccination, trust in official healthcare authorities and utilization of preventive services in general primarily shape the general public's decisions on vaccination. Provision of univocal and accurate evidence‐based information on the risks and benefits of vaccination by healthcare providers, which have to be consistent with national guidelines and recommendations, is crucial to maintain and improve vaccination uptake and rates. It is, therefore, increasingly important for national public health authorities to integrate holistic approaches and strategies targeting both health professionals and the general population and to ensure that community outreach efforts and information dissemination are consistent, scientifically driven, and tailored to the needs of different populations with respect to individuals' autonomy.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Theodoros V. Giannouchos: Conceived and designed the study, conducted data and statistical analyses and wrote the first draft of the manuscript. Kyriakos Souliotis: Collected the data and contributed to the study design. Evaggelia Steletou, Maria Saridi, Kyriakos Souliotis: Critically reviewed the manuscript for important intellectual content and contributed to the editing and writing of the final manuscript. All authors read and approved the final manuscript.
Giannouchos TV, Steletou E, Saridi M, Souliotis K. Should vaccination be mandated? Individuals' perceptions on mandatory vaccination in Greece. J Eval Clin Pract. 2021;27:1104–1111. 10.1111/jep.13568
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Xu L, Chen J, Zhan Z, et al. Evaluating the effectiveness of national measles elimination action in mainland China during 2004–2016: a multi‐site interrupted time‐series study. Vaccine. 2020;38(28):4440‐4447. [DOI] [PubMed] [Google Scholar]
- 2. Doherty M, Buchy P, Standaert B, Giaquinto C, Prado‐Cohrs D. Vaccine impact: benefits for human health. Vaccine. 2016;34(52):6707‐6714. [DOI] [PubMed] [Google Scholar]
- 3. Andre FE, Booy R, Bock HL, et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. 2008;86:140‐146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Maltezou HC, Botelho‐Nevers E, Brantsæter AB, et al. Vaccination of healthcare personnel in Europe: update to current policies. Vaccine. 2019;37(52):7576‐7584. [DOI] [PubMed] [Google Scholar]
- 5. Jones AM, Omer SB, Bednarczyk RA, Halsey NA, Moulton LH, Salmon DA. Parents' source of vaccine information and impact on vaccine attitudes, beliefs, and nonmedical exemptions. Adv Prev Med. 2012;1:2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wellcome Trust . Wellcome global monitor 2018. Chapter 5: Attitudes to vaccine. https://wellcome.ac.uk/reports/wellcome-global-monitor/2018/chapter-5-attitudes-vaccines. Accessed July 19, 2020.
- 7. Jorgensen P, Mereckiene J, Cotter S, Johansen K, Tsolova S, Brown C. How close are countries of the WHO European Region to achieving the goal of vaccinating 75% of key risk groups against influenza? Results from national surveys on seasonal influenza vaccination programmes, 2008/2009 to 2014/2015. Vaccine. 2018;36(4):442‐452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization (WHO). Regional Office for Europe. Routine immunization profile: Greece, 2017. https://www.euro.who.int/data/assets/pdf_file/0006/420657/GRC.pdf. Accessed July 20, 2020.
- 9. President of Greek Democracy – FEK A 54/11.03.2020 . Prevention, protection and promotion of health. Chapter B: Prevention program for health risks “ΣΠϒPΟΣ ΔΟΞΙΑΔHΣ”. https://www.e-nomothesia.gr/kat-ygeia/nomos-4675-2020-phek-54a-11-3-2020.html. Accessed July 21, 2020.
- 10. Maltezou HC, Katerelos P, Poufta S, Pavli A, Maragos A, Theodoridou M. Attitudes toward mandatory occupational vaccinations and vaccination coverage against vaccine‐preventable diseases of health care workers in primary health care centers. Am J Infect Control. 2013;41(1):66‐70. [DOI] [PubMed] [Google Scholar]
- 11. Toska A, Saridi M, Wozniak G, Souliotis K, Korovesis K, Apostolopoulou E. Influenza vaccination among nurses in Greece. Am J Infect Control. 2012;40(3):276‐278. [DOI] [PubMed] [Google Scholar]
- 12. Psarrou A, Moisoglou I, Meimeti E, et al. Hepatitis B vaccination coverage of healthcare professionals in Greece. FARMACIA. 2018;66(4):581‐586. [Google Scholar]
- 13. Dedoukou X, Nikolopoulos G, Maragos A, Giannoulidou S, Maltezou HC. Attitudes towards vaccination against seasonal influenza of health‐care workers in primary health‐care settings in Greece. Vaccine. 2010;28(37):5931‐5933. [DOI] [PubMed] [Google Scholar]
- 14. Hellenic National Public Health Organization . Satisfactory levels of vaccination rates among children in Greece. https://www.iefimerida.gr/news/445209/keelpno-se-ikanopoiitika-epipeda-i-emvoliastiki-kalypsi-ton-paidion-stin-ellada. Accessed July 26, 2020.
- 15. Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150‐2159. [DOI] [PubMed] [Google Scholar]
- 16. Smith LE, Amlôt R, Weinman J, Yiend J, Rubin GJ. A systematic review of factors affecting vaccine uptake in young children. Vaccine. 2017;35(45):6059‐6069. [DOI] [PubMed] [Google Scholar]
- 17. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161‐4164. [DOI] [PubMed] [Google Scholar]
- 18. Habersaat KB, Pistol A, Stanescu A, et al. Measles outbreak in Romania: understanding factors related to suboptimal vaccination uptake. Eur J Public Health. 2020;30(5):986‐992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Danis K, Georgakopoulou T, Stavrou T, Laggas D, Panagiotopoulos T. Socioeconomic factors play a more important role in childhood vaccination coverage than parental perceptions: a cross‐sectional study in Greece. Vaccine. 2010;28(7):1861‐1869. [DOI] [PubMed] [Google Scholar]
- 20. Stefanoff P, Mamelund SE, Robinson M, et al. VACSATC Working Group on Standardization of Attitudinal Studies in Europe. Tracking parental attitudes on vaccination across European countries: the Vaccine Safety, Attitudes, Training and Communication Project (VACSATC). Vaccine. 2010;28(35):5731‐5737. [DOI] [PubMed] [Google Scholar]
- 21. Güvenç IA, Parıldar H, Şahin MK, Erbek SS. Better knowledge and regular vaccination practices correlate well with higher seasonal influenza vaccine uptake in people at risk: promising survey results from a university outpatient clinic. Am J Infect Control. 2017;45(7):740‐745. [DOI] [PubMed] [Google Scholar]
- 22. Santorelli G, West J, Mason D, et al. Factors associated with the uptake of the UKroutine childhood immunization schedule in a bi‐ethnic population. Eur J Public Health. 2020;30(4):697‐702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ding X, Tian C, Wang H, Wang W, Luo X. Characteristics associated with human papillomavirus vaccination initiation and completion among young adults. Am J Infect Control. 2019;47(9):1096‐1101. [DOI] [PubMed] [Google Scholar]
- 24. Bert F, Olivero E, Rossello P, et al. Knowledge and beliefs on vaccines among a sample of Italian pregnant women: results from the NAVIDAD study. Eur J Public Health. 2020;30(2):286‐292. [DOI] [PubMed] [Google Scholar]
- 25. Coniglio MA, Platania M, Privitera D, Giammanco G, Pignato S. Parents' attitudes and behaviours towards recommended vaccinations in Sicily, Italy. BMC Public Health. 2011;11(1):305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lahouati M, De Coucy A, Sarlangue J, Cazanave C. Spread of vaccine hesitancy in France: what about YouTube™? Vaccine. 2020;38(36):5779‐5782. [DOI] [PubMed] [Google Scholar]
- 27. Yiannakoulias N, Slavik CE, Chase M. Expressions of pro‐and anti‐vaccine sentiment on YouTube. Vaccine. 2019;37(15):2057‐2064. [DOI] [PubMed] [Google Scholar]
- 28. Gandhi CK, Patel J, Zhan X. Trend of influenza vaccine Facebook posts in last 4years: a content analysis. Am J Infect Control. 2020;48(4):361‐367. [DOI] [PubMed] [Google Scholar]
- 29. Meadows CZ, Tang L, Liu W. Twitter message types, health beliefs, and vaccine attitudes during the 2015 measles outbreak in California. Am J Infect Control. 2019;47(11):1314‐1318. [DOI] [PubMed] [Google Scholar]
- 30. Karageorgou K, Katerelos P, Efstathiou A, Theodoridou M, Maltezou HC. Vaccination coverage and susceptibility against vaccine‐preventable diseases of healthcare students in Athens, Greece. Vaccine. 2014;32(39):5083‐5086. [DOI] [PubMed] [Google Scholar]
- 31. Cates JR, Shafer A, Carpentier FD, et al. How parents hear about human papillomavirus vaccine: implications for uptake. J Adolescent Health. 2010;47(3):305‐308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yaqub O, Castle‐Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med. 2014;112:1‐11. [DOI] [PubMed] [Google Scholar]
- 33. Hendrix KS, Sturm LA, Zimet GD, Meslin EM. Ethics and childhood vaccination policy in the United States. Am J Public Health. 2016;106(2):273‐278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Navin MC, Attwell K. Vaccine mandates, value pluralism, and policy diversity. Bioethics. 2019;33(9):1042‐1049. [DOI] [PubMed] [Google Scholar]
- 35. Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID‐19: implications for public health communications. Lancet Regional Health‐Europe. 2021;1:100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Motta M, Sylvester S, Callaghan T, Trujillo KL. Encouraging COVID‐19 vaccine uptake through effective health communication. Front Polit Sci. 2021;3:630133. [Google Scholar]
- 37. Saitoh A, Nagata S, Saitoh A, et al. Perinatal immunization education improves immunization rates and knowledge: a randomized controlled trial. Prev Med. 2013;56(6):398‐405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Betsch C, Wicker S. E‐health use, vaccination knowledge and perception of own risk: drivers of vaccination uptake in medical students. Vaccine. 2012;30(6):1143‐1148. [DOI] [PubMed] [Google Scholar]
- 39. Fu LY, Bonhomme LA, Cooper SC, Joseph JG, Zimet GD. Educational interventions to increase HPV vaccination acceptance: a systematic review. Vaccine. 2014;32(17):1901‐1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jung Y, Kwon M, Song J. Stepwise intervention including 1‐on‐1 counseling is highly effective in increasing influenza vaccination among health care workers. Am J Infect Control. 2017;45(6):635‐641. [DOI] [PubMed] [Google Scholar]
- 41. Kadi Z, Atif ML, Brenet A, Izoard S, Astagneau P. Barriers of influenza vaccination in health care personnel in France. Am J Infect Control. 2016;44(3):361‐362. [DOI] [PubMed] [Google Scholar]
- 42. Motta M, Callaghan T, Sylvester S. Knowing less but presuming more: Dunning‐Kruger effects and the endorsement of anti‐vaccine policy attitudes. Soc Sci Med. 2018;211:274‐281. [DOI] [PubMed] [Google Scholar]
- 43. Grossman M. On the concept of health capital and the demand for health. J Polit Econ. 1972;80:223‐255. [Google Scholar]
- 44. Pavlopoulou ID, Michail KA, Samoli E, Tsiftis G, Tsoumakas K. Immunization coverage and predictive factors for complete and age‐appropriate vaccination among preschoolers in Athens, Greece: a cross‐sectional study. BMC Public Health. 2013;13(1):908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hellenic Statistical Authority . Greece in Figures: October‐December 2019. https://www.statistics.gr/documents/20181/1515741/GreeceInFigures_2019Q4_EN.pdf.pdf/d0149260-0983-9d80-e5c1-4368dc87fda3. Accessed March 1, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


