Abstract
Purpose
To determine the relationship between posttraumatic growth (PTG), psychological flexibility, and psychological resilience of nursing students after the COVID‐19 alarm status.
Design and Methods
This descriptive cross‐sectional study was conducted with nursing students (N = 292) studying at a nursing school of a university. The data collection instruments included a form on descriptive variables, and the PTG, psychological flexibility, and psychological resilience scales. Descriptive statistics, independent‐samples t test, ANOVA, correlation, simple, and hierarchical linear regression analyses were used to analyze the data.
Findings
The mean scores regarding psychological flexibility, psychological resilience, and PTG were 27.56 ± 11.06, 18.10 ± 5.75, and 63.49 ± 20.64, respectively. While psychological flexibility explained 36.7% of the total variance in psychological resilience, the predictive effect of seven descriptive variables, including psychological flexibility and psychological resilience, on PTG was determined as 13.4%.
Practice Implications
PTG, psychological flexibility, and psychological resilience may help nursing students prepare for their transition to the profession.
Keywords: COVID‐19, education curriculum, nursing student, pandemic, psychological flexibility, psychological resilience
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) 1 pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) has become a public health problem concerning the whole world in a short time due to its rapid contamination characteristic).2, 3 According to the official website of the World Health Organization (WHO), it has been confirmed that more than 66,700,000 people worldwide had had COVID‐19 infection as of December 8, 2020. 4 The first case in Turkey was detected on March 10, 2020, and the number of confirmed cases exceeded 552,300 according to the data of December 8, 2020. 5 Although so many things such as virus information, clinical features, and diagnosis in COVID‐19 have been accomplished, there is no effective treatment yet. 6 Additionally, although there are vaccines recently developed for COVID‐19, there remain uncertainties about the effectiveness, supply, and how many people these vaccines will reach when it comes to stopping the pandemic.7, 8
The COVID‐19 pandemic continues to affect every segment of society in a different way. It is possible to state that some professions are more prominent than ever during the pandemic. The profession of nursing comes first among these professions. Indeed, 2020 is a year in which nursing services became the most talked about and visible due to the COVID‐19 pandemic. All nursing activities including nursing education have been dramatically affected by the current pandemic. Nursing education has been maintained through online classes in many parts of the world during the pandemic when protection of physical distance is essential. 9 All education programs at universities including nursing education were suspended on March 12, 2020, with the start of the COVID‐19 alarm status in Turkey. After a 1‐week recess, education was started to be provided on March 23, 2020, with digital and distance education opportunities to not interrupt education and training and with the idea of unity in practice. 10 Although it was stated by higher education institutions that students had the right to freeze the school during the period of the alarm process caused by COVID‐19, most nursing students continued their education. Theoretical lessons of nursing students could not be taught simultaneously due to the insufficiency of the distance education infrastructure in Turkey. Clinical practices have been postponed to the next training period, considering the pandemic process. To enable nursing students to capture the learning outcomes in clinical courses, care plans, case presentations, and other learning methods have been used. The final evaluation of students was carried out through online exams and homework.11, 12
It has been known that nursing students' transition to the workforce has always been stressful, and some newly graduated nurses quit the profession. 13 Moreover, COVID‐19 has become a new and serious stressor for nursing students. Nursing students witnessed the struggle (e.g., the shortage of needed materials including personal protective equipment and the disease caused by primary contact with individuals with infection) of their colleagues working in the field with the isolation measures and delays at universities across Turkey due to the COVID‐19 pandemic, and this may have caused them to be spiritually affected negatively.
2. BACKGROUND
COVID‐19 has caused not only the risk of death from viral infection globally, but also a serious psychological pressure,3, 14 Various studies that have been reported so for revealed that the COVID‐19 pandemic caused negative mental health issues such as anxiety, depression and posttraumatic stress disorder (PTSD) among individuals.15, 16, 17 When evaluated from the psychopathological perspective, the COVID‐19 pandemic may be interpreted as a new stress, psychological crisis, or trauma. 17 Although exposure to the negative consequences of trauma from COVID‐19 in the acute phase seems well documented, there is little information about some paradoxical, positive consequences of trauma experiences. 18
As positive psychology has become popular at the end of the 20th century, there is a need more than ever to conduct studies on positive changes even during a world‐threatening pandemic rather than negative aspects such as PTSD. 19 While a pathology‐based model was used to eliminate the cause of posttraumatic diseases and negative symptoms in the past, the focus of research has shifted to finding health sources and supporting and emphasizing the potentially positive aspects of the situation after the trauma in recent years.19, 20 According to this perspective, not all traumatic experiences turn into a source for negative psychological disorders. In fact, after serious traumatic experiences, a much larger part of people are able to continue to function normally and grow psychologically in the face of distress.20, 21 Positive psychological changes subjectively reported by individuals were observed in terms of self‐perception, interpersonal relations, and perspective on life after experiencing traumatic or crisis events, and this situation was conceptualized as posttraumatic growth (PTG). 20 This positive nature of PTG is generally referred to as psychological resilience.22, 23 The concept of psychological resilience that is important for personal welfare and public health is defined as successful compliance with environmental risks that are expected to bring negative psychological sequelae. 24 Psychological resilience includes not only resistance against psychological distress but also the capacity for positive experiences and growth in the face of trauma.22, 23 Individuals with a higher level of psychological resilience in the face of distress show fewer signs of anxiety, depression, and difficulty in rearrangement, and they tend to return to the predistress process more quickly. On the other hand, those with low psychological resilience levels tend to show more weakness. 25 Similar to psychological resilience, decreases in the psychological flexibility of individuals are associated with various forms of psychopathology. 26 Psychological flexibility is defined as the ability to flexibly adapt to situations by fully experiencing acceptance and all thoughts and emotions.27, 28 High psychological flexibility is associated with psychological development. People have the potential to better tolerate and effectively use emotions and opinions to obtain the best possible results in different situations. This wide dynamic spectrum of ability constitutes the basis of health. After all, a healthy person is someone who can manage themselves in the uncertain, unpredictable world around them where innovation and change are the norms rather than the exception. These flexibility processes are not present in various forms of psychopathology. 26
In light of the literature mentioned above, PTG, psychological resilience, and psychological flexibility are thought to be associated dynamics. Although PTG, psychological resilience, and psychological flexibility seem to have a strong place in positive psychology, there are no studies that have examined the correlation between these dynamics in the literature. While the COVID‐19 pandemic has brought a dynamic process in line with the changing characteristics of the virus, it has also changed the structure of nursing education. The literature which emerged within the scope of positive psychology during the COVID‐19 process revealed only one study examining the psychological resilience of nursing students. 18 However, uncertainty remains about examining the positive psychological dynamics of nursing students such as PTG, psychological resilience, and psychological resilience during the COVID‐19 process. Developing our understanding of the PTG, psychological resilience, and psychological flexibility of nursing students, who are the future of the nursing workforce, during the pandemic process is important in terms of helping students be prepared for their transition to the profession and cope with difficulties. In this context, the correlations between the psychological resilience, psychological flexibility, and PTG levels of nursing students after the first alarm period when severe psychological distress such as the COVID‐19 pandemic was experienced were aimed to be examined.
3. AIMS AND RESEARCH QUESTIONS
This study aimed to determine the correlation between the PTG, psychological resilience, and psychological flexibility of nursing students after the COVID‐19 alarm status. The questions of the study determined in line with this general purpose were as follows.
What are the PTG, psychological resilience, and psychological flexibility levels of nursing students after the COVID‐19 alarm status?
Is there a relationship between PTG, psychological resilience, and psychological flexibility levels in nursing students after the COVID‐19 alarm status?
Are there relationships between the descriptive characteristics of nursing students after the COVID‐19 alarm status and PTG, psychological resilience, and psychological flexibility?
Do psychological resilience, psychological flexibility, and descriptive characteristics in nursing students after the COVID‐19 alarm status have decisive characteristics in terms of PTG?
4. METHOD
4.1. Design and setting
This descriptive cross‐sectional study was conducted with nursing students at the Inonu University School of Nursing that is located in eastern Turkey between June 1 and July 1, 2020, when the curfew restrictions due to COVID‐19 were terminated, and the return to normal life was initiated. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist was used to ensure the quality of this study (see Supplementary File 1).
4.2. Sample and participants
Official sample size was not determined based on the exploratory nature of this study. Additionally, this study followed the principle that the number of observations should be at least 10 times more than each independent variable in the analysis to provide a sufficient sample size for the effect size estimation used in multiple regression. 29
This study included 292 1st‐ and 4th‐year nursing students in the spring semester of the academic year of 2019–2020 (230 female students and 63 male students) (Figure 1). There were no inclusion criteria other than having the ability to read Turkish and being voluntary to participate.
Figure 1.
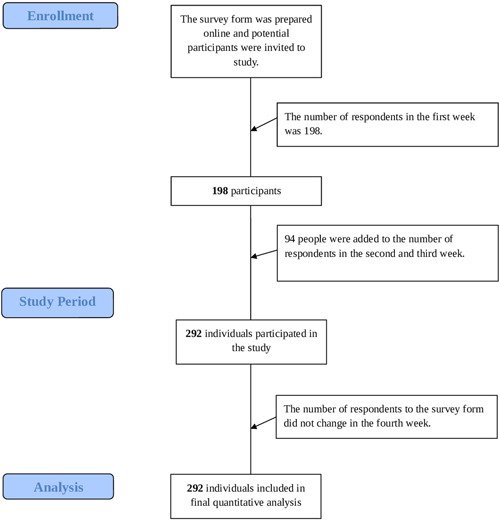
Flow diagram of participants inclusion [Color figure can be viewed at wileyonlinelibrary.com]
4.3. Variables and measurement
In this study, the use of measurement tools was provided by taking the necessary permissions from the researchers who conducted the validity and reliability studies of the instruments.
4.3.1. Introductory Characteristics Form
The form was developed by the researcher, and it included nine questions about the students' age, gender, marital status, grade, place of residence, perception of economic status, attitudes toward the profession before and after COVID‐19, and the society's attitude toward the profession of nursing during COVID‐19.
4.3.2. The Acceptance and Action Questionnaire‐II (AAQ‐II)
AAQ‐II is a seven‐point Likert‐type scale with seven items and aims to evaluate the psychological flexibility levels of individuals. High scores indicate psychological inflexibility, while low scores indicate psychological flexibility. 30 The Turkish adaptation, validity, and reliability studies of AAQ‐II were conducted by Yavuz et al. 31 The scale was used in this study due to its high internal consistency (e.g., Cronbach's alpha = 0.84), test–retest reliability, and discriminant validity in the Turkish society. 31
4.3.3. The Brief Resilience Scale (BRS)
BRS was developed by Smith et al. 32 to measure the psychological resilience of individuals. It is a self‐report‐style measurement tool and has six items as a five‐point Likert‐type scale. High scores indicate high levels of psychological resilience. The adaptation, validity, and reliability studies of BRS to Turkish were conducted by Doğan. 33 The Cronbach's alpha coefficient in the Turkish adaptation of BRS was reported as 0.83. 33 In this study, BRS was used as a measurement tool because it shows satisfactory psychometric properties.
4.3.4. Posttraumatic Growth Inventory (PTGI)
The scale was developed by Tedeschi and Calhoun 34 and adapted to the Turkish language by Kağan et al. 35 This is a five‐point Likert‐type scale with 21 items. Higher total scores indicate higher PTG levels. The scale consists of three subscales, including change in self‐perception, change in relationships with others, and change in philosophy of life. The Cronbach's alpha coefficient values obtained from the dimensions of change in self‐perception, change in relationships with others, and change in philosophy of life in the Turkish version of the scale were reported 0.88, 0.77, and 0.78, respectively. 35 In this study, PTGI was preferred because it preserves a valid and reliable construct with all its dimensions (Table 2).
Table 1.
Mean, standard deviation, and correlation values of variables (N = 292)
| α | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|---|
| Changes in self‐perception | 0.90 | 33.43 | 10.73 | – | |||||
| Changes in philosophy of life | 0.76 | 17.78 | 5.96 | 0.777** | – | ||||
| Changes in relationship | 0.83 | 12.28 | 5.99 | 0.727** | 0.649** | – | |||
| PTGI total score | 0.93 | 63.49 | 20.64 | 0.956** | 0.882** | 0.856** | – | ||
| AAQ‐II | 0.91 | 27.56 | 11.06 | −0.095 | 0.039 | −0.124* | −0.074 | – | |
| BRS | 0.88 | 18.10 | 5.75 | 0.196** | 0.063 | 0.190** | 0.175** | −0.608** | – |
Abbreviations: AAQ‐II, Acceptance and Action Questionnaire‐II; BRS, Brief Resilience Scale; PTGI, Posttraumatic Growth Inventory.
p < 0.05 (two‐tailed)
p < 0.01 (two‐tailed).
4.4. Data collection
Following the institutional and ethical authorizations, the researcher met with the advisor instructors of each class to explain the study's objective and engage with potentially suitable participants. The advisors invited the related nursing students to participate in the study by sharing the link of the information form prepared online by the researcher on WhatsApp and e‐mail groups including nursing students suitable for the study. The researcher collected the data by periodically following the data entry in the system.
4.5. Data analysis
The data, collected by the online survey method, were transferred to an Excel file and introduced into SPSS. The data were analyzed using the SPSS 25.0. Descriptive statistics (means, standard deviations, and percentages) were used to determine the factors related to the descriptive characteristics of the participants. Kolmogorov–Smirnov test was performed to examine data distribution, and Pearson's correlation analysis was used to measure the relationships between psychological resilience, psychological flexibility, and PTG. Independent‐samples t test and ANOVA were used to compare the scale mean scores of the participants based on their descriptive characteristics. Finally, multiple and hierarchical regression analyses were conducted to evaluate factors associated with PTG. Standardized coefficients (β) were computed to compare the relative significance of each variable in the model. The data were checked for multicollinearity, using tolerance, and the variance inflation factor (VIF). The statistical assumptions for the regression analysis were met when there was no multicollinearity. The variance inflation factors were between 1.000 and 1.639, which were below the 10.0 cut‐off, indicating the absence of multicollinearity. 36 The results were considered statistically significant at p < 0.05.
4.6. Validity and reliability
In this study, all scales had a Cronbach's alpha value of above 0.70 which corresponded to an acceptable internal consistency level (Table 2).
4.7. Ethical approval
For conducting the study, first, the institutional permission required for the ethical committee decision was obtained. Then, ethical approval was obtained from the Inonu University Scientific Research and Publication Ethics Committee (no: 2020/783‐10). Before starting to fill out the questionnaire, the participants were asked for informed consent explaining the topic and purpose of the study, assurance of keeping their information confidential, and the contact details of the researcher. The participants completed the study by making sure that their contribution to the study was entirely voluntary and anonymous and that they could be excluded at any time.
5. RESULTS
5.1. Descriptive characteristics
The distribution of the descriptive characteristics of the nursing students is summarized in Table 1. The mean age of the participants was 20.90 ± 2.16 (minimum: 18, maximum: 31). Among the participants, 78.8% were female, 99.3% were single, 32.9% were in the 1st year of their education, 59.6% lived in cities, and 83.6% stated to have a middle‐income level. This study showed that 59.6% of the participants remained strictly interested in the profession before the COVID‐19 pandemic, 48.6% had increased interest in the profession during the COVID‐19 pandemic, and 85.6% had a perception that the public interest in the profession increased during the COVID‐19 pandemic (Table 1).
Table 2.
Distribution of nursing students according to descriptive characteristics (N = 292)
| Descriptive Characteristics | n | Percent |
|---|---|---|
| Mean age | 20.90 ± 2.16 year | (min–max = 18–31) |
| Gender | ||
| Female | 230 | 78.8 |
| Male | 62 | 21.2 |
| Marital status | ||
| Married | 2 | 0.7 |
| Single | 290 | 99.3 |
| Year of education | ||
| 1 | 96 | 32.9 |
| 2 | 76 | 26.0 |
| 3 | 47 | 16.1 |
| 4 | 73 | 25.0 |
| Living place | ||
| Province | 174 | 59.6 |
| District | 80 | 27.4 |
| Village | 18 | 13.0 |
| How to perceive the economic situation | ||
| High | 30 | 10.3 |
| Middle | 244 | 83.6 |
| Low | 18 | 6.2 |
| Attitude toward the profession before COVID‐19 pandemic | ||
| Absolutely relevant | 174 | 59.6 |
| A little concerning | 60 | 20.5 |
| No change in interest | 42 | 14.4 |
| A little unconcerned | 16 | 5.5 |
| Attitude toward the profession during COVID‐19 pandemic | ||
| Interest definitely increased | 142 | 48.6 |
| There was some interest | 50 | 17.1 |
| No change in attitude | 74 | 25.3 |
| Unstable | 26 | 8.9 |
| Community's attitude toward the profession during the COVID‐19 pandemic | ||
| Changed positively | 250 | 85.6 |
| Changed negatively | 10 | 3.4 |
| Not changed | 32 | 11.0 |
5.2. Psychological flexibility, psychological resilience, and PTG levels and correlations
The mean scores of the participants on BRS, AAQ‐II, and PTGI were 18.10 ± 5.75, 27.56 ± 11.06, and 63.49 ± 20.64, respectively. A weak significant negative correlation was found between the AAQ‐II results obtained from the participants and the dimension of change in communication with others (r = −.124, p < 0.05). Similarly, a weak significant positive correlation was determined between BRS and PTGI total score (r = .175, p < 0.01). A strong significant negative correlation was revealed between AAQ‐II and BRS (r = −.608, p < 0.01). (Table 2).
5.3. Univariate analyses of the factors associated with PTG, psychological flexibility, and psychological resilience
The independent‐samples t test and ANOVA revealed that the nursing students who had a positive attitude toward the profession of nursing before and during the pandemic, those who were female, and those who had a higher level of income had higher PTG scores (p < 0.05). Although the PTG scores of students who had reached the last (4th) year of their education were higher, this difference was not statistically significant (p > 0.05). It was revealed that the nursing students who reported that there was no change in their attitudes toward the profession of nursing during the pandemic and that there was no change in society's attitudes toward the nursing profession had higher psychological flexibility levels. Finally, the nursing students with a middle‐income status and those whose attitudes toward the profession of nursing did not change during the pandemic period presented higher psychological resilience levels (p < 0.05) (Table 3).
Table 3.
Univariate analyses of the factors associated with PTG, psychological flexibility, and psychological resilience (N = 292)
| Variables | PTG | AAQ‐II | BRS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | t/F | p | Mean (SD) | t/F | p | Mean (SD) | t/F | p | |
| Gender | |||||||||
| Female | 62.24 (21.30) | 27.46 (11.30) | 18.02 (5.98) | ||||||
| Male | 57.00 (16.56) | 2.824 | 0.005 a | 27.90 (10.20) | 0.143 | 0.785a | 18.41 (4.81) | −0.477 | 0.634a |
| Year of education | |||||||||
| 1 | 61.89 (19.83) | 28.89 (11.71) | 17.09 (5.75) | ||||||
| 2 | 62.47 (19.59) | 0.604 | 0.613b | 25.72 (10.24) | 1.518 | 0.210b | 19.13 (5.75) | 1.846 | 0.139b |
| 3 | 65.10 (21.22) | 28.93 (11.26) | 18.29 (5.97) | ||||||
| 4 | 65.61 (22.47) | 26.83 (10.77) | 18.26 (5.50) | ||||||
| Living place | |||||||||
| Province | 61.88 (21.20) | 28.44 (11.18) | 17.75 (5.67) | ||||||
| District | 67.47 (18.32) | 2.077 | 0.127b | 26.17 (10.64) | 1.392 | 0.250b | 19.02 (5.98) | 1.398 | 0.249b |
| Village | 62.47 (22.01) | 26.42 (11.30) | 17.78 (5.55) | ||||||
| How to perceive the economic situation | |||||||||
| High | 65.93 (19.73) | 24.90 (13.52) | 17.53 (6.65) | ||||||
| Middle | 64.51 (19.79) | 7.636 | 0.001 b | 27.34 (10.68) | 0.460 | 0.632b | 18.44 (5.64) | 4.076 | 0.018 b |
| Low | 45.55 (25.80) | 27.44 (12.05) | 14.55 (4.47) | ||||||
| Attitude toward the profession before COVID‐19 pandemic | , | ||||||||
| Absolutely relevant | 67.67 (20.66) | 27.36 (11.16) | 18.34 (5.72) | ||||||
| A little concerning | 61.03 (17.47) | 8.076 | 0.001 b | 28.73 (11.12) | 1.013 | 0.387b | 17.63 (5.83) | 0.471 | 0.703b |
| No change in interest | 51.85 (19.78) | 28.23 (10.95) | 17.52 (5.83) | ||||||
| A little unconcerned | 57.75 (20.75) | 23.50 (9.95) | 18.87 (5.87) | ||||||
| Attitude toward the profession during COVID‐19 pandemic | , | ||||||||
| Interest definitely increased | 67.85 (21.77) | 27.11 (11.09) | 18.23 (5.66) | ||||||
| There was some interest | 62.56 (16.32) | 4.999 | 0.002 b | 30.00 (10.02) | 4.327 | 0.005 b | 17.28 (5.37) | 2.669 | 0.048 b |
| No change in attitude | 57.16 (20.23) | 24.94 (10.49) | 19.21 (5.72) | ||||||
| Unstable | 59.46 (18.01) | 32.76 (12.31) | 15.84 (6.46) | ||||||
| Community's attitude toward the profession during the COVID‐19 pandemic | |||||||||
| Changed positively | 64.22 (19.93) | 27.73 (11.09) | 18.12 (5.96) | ||||||
| Changed negatively | 76.60 (22.79) | 5.979 | 0.003 b | 35.40 (9.78) | 4.544 | 0.011 b | 16.80 (4.18) | 0.310 | 0.734b |
| Not changed | 53.68 (22.31) | 23.75 (9.90) | 18.43 (4.36) | ||||||
Note: Values with p < 0.05 were in bold.
Abbreviations: AAQ‐II, Acceptance and Action Questionnaire‐II; BRS, Brief Resilience Scale; PTGI, Posttraumatic Growth Inventory; SD, standard deviation.
Independent samples t test.
One‐way ANOVA.
5.4. Psychological flexibility as a determinant of psychological resilience
The results of the simple regression analysis for the determinant psychological flexibility of psychological resilience revealed that psychological flexibility was a negative factor for psychological resilience, and psychological resilience explained 36.7% of the total variance (Table 4).
Table 4.
Simple regression analysis for psychological flexibility as a determinant of psychological resilience (N = 292)
| Variable | ß | t | p | VIF | F | Model (p) | Adjusted R 2 | DW |
|---|---|---|---|---|---|---|---|---|
| Constant | 26.822 | 37.262 | 0.001 | |||||
| AAQ‐II | −0.316 | −13.040 | 0.001 | 1.000 | 170.030 | 0.001 | 0.367 | 2.064 |
Abbreviations: AAQ‐II, Acceptance and Action Questionnaire‐II; VIF, variance inflation factor.
5.5. Determinants of PTG
Hierarchical regression analysis was performed to determine the variables predicting PTG. Seven basic variables in the study were included in the model. Psychological resilience was included in the analysis in the first model, in which PTG was considered as the explained variable, and psychological flexibility was included in the second model. In the third, fourth, and fifth models, some descriptive characteristics of the participants (age, gender, economic status, attitude toward profession before and during COVID‐19) were analyzed. The VIF values were checked for multicollinearity between the variables, and no problem of multicollinearity was found since the VIF values were less than 5. This situation met the assumptions of the regression analysis. As seen in Table 4, the total mean score of the participants in PTGI could be explained by psychological resilience, gender, economic status, and students' attitudes toward the profession of nursing before and during COVID‐19 pandemic. These five variables explained 13.4% of total variance observed in PTGI. This study indicated that psychological flexibility and age did not significantly determine the PTGI scores (Table 5).
Table 5.
Hierarchical regression analysis results regarding determinants of posttraumatic growth (N = 292)
| Variables | ß | t | p | VIF | F | Model (p) | Adjusted R 2 | |
|---|---|---|---|---|---|---|---|---|
| Model 1 | Constant | 52.108 | 13.223 | 0.001 | ||||
| BRS | 0.062 | 3.031 | 0.003 | 1.000 | 9.187 | 0.003 | 0.027 | |
| Model 2 | Constant | 47.404 | 6.148 | 0.001 | ||||
| BRS | 0.742 | 2.836 | 0.005 | 1.586 | 4.838 | 0.009 | 0.026 | |
| AAQ‐II | 0.097 | 0.710 | 0.478 | 1.586 | ||||
| Model 3 | Constant | 51.021 | 3.862 | 0.001 | ||||
| BRS | 0.764 | 2.943 | 0.004 | 1.615 | ||||
| AAQ‐II | 0.104 | 0.764 | 0.445 | 1.616 | 4.777 | 0.001 | 0.049 | |
| Age | 0.304 | 0.550 | 0.583 | 1.025 | ||||
| Gender | −8.878 | ‐3.016 | 0.003 | 1.009 | ||||
| Model 4 | Constant | 71.664 | 4.779 | 0.001 | ||||
| BRS | 0.683 | 2.643 | 0.009 | 1.625 | ||||
| AAQ‐II | 0.066 | 0.492 | 0.623 | 1.632 | ||||
| Age | 0.231 | 0.423 | 0.673 | 1.028 | 5.479 | 0.001 | 0.071 | |
| Gender | −9.224 | −3.219 | 0.001 | 1.013 | ||||
| Economic situation | −8.173 | −2.799 | 0.005 | 1.024 | ||||
| Model 5 | Constant | 81.753 | 5.574 | 0.001 | ||||
| BRS | 0.621 | 2.484 | 0.014 | 1.631 | ||||
| AAQ‐II | 0.046 | 0.354 | 0.724 | 1.639 | ||||
| Age | 0.287 | 0.540 | 0.590 | 1.043 | ||||
| Gender | −7.464 | −2.671 | 0.008 | 1.034 | 7.443 | 0.001 | 0.134 | |
| Economic situation | −7.797 | −2.761 | 0.006 | 1.027 | ||||
| Attitude toward the profession before COVID‐19 | −3.826 | −3.137 | 0.002 | 1.082 | ||||
| Attitude toward the profession during COVID‐19 | −3.113 | −2.798 | 0.005 | 1.070 |
Abbreviations: AAQ‐II, Acceptance and Action Questionnaire‐II; BRS, Brief Resilience Scale.
6. DISCUSSION
This study is the first study that evaluated the positive psychologies of nursing students after the COVID‐19 alarm status in the scientific literature. Since nursing students are the future of the nursing workforce, it is important to improve our understanding about PTG, psychological resilience, and psychological flexibility in this population. It is also more important than ever to refresh our knowledge about positive psychology while it is clear that other pandemics will potentially occur in the future. 17 This study aimed to determine the correlation between the PTG, psychological resilience, and psychological flexibility of nursing students after the current pandemic alarm status.
Psychological resilience is regarded as a feature or capacity that allows individuals to cope with distress and adapt positively especially in the face of traumatic experiences.22, 23 An exploratory study that examined resilience in nursing students reported that only 33.3% of the students were resilient. The results of the study emphasized the importance of resilience among nursing students and advised nursing instructors to help nursing students develop resilience to better prepare for academic success and experience a smooth transition to professional nursing roles. 37 There are limited numbers of studies that examined the psychological resilience in different samples during the current pandemic. Only one study examining the psychological resilience of nursing students during the COVID‐19 process was found, and 38% of the students in the aforementioned study were found to have poor resilience scores. 18 There are studies that found mean psychological resilience scores as 21.22 ± 4.68 in university students, 38 as 20.47 ± 3.95 adult individuals 39 and as 18.13 ± 5.42 in young adults. 40 The findings of this study indicated that the mean psychological resilience score of the nursing students was 18.10 ± 5.75. In this context, the psychological resilience score of the nursing students in this study presents similar data to other studies conducted during the COVID‐19 pandemic process. It seems that the nursing students could demonstrate the ability to successfully overcome the psychological distress experienced after the COVID‐19 alarm status and adapt to the new situation. In the literature, supportive learning environments, integration of reflective exercises, 41 peer support or peer programs, 42 and mindfulness programs 43 have been stated to be important methods to support resilience. In this context, nursing educators may play an important role by taking advantage of these methods to help students maintain or develop resilience during these challenging times in the COVID‐19 pandemic period. This is because the role of nursing educators is very valuable in terms of developing learning activities or programs to increase resilience, supporting nursing students, providing protection during stressful events, and increasing future employability. 18
The self‐management of the individual in the face of vague and unpredictable situations such as the COVID‐19 pandemic is closely related to psychological flexibility. 26 A study that examined the psychological flexibility levels of university students found that the mean psychological flexibility score of the participants was 24.11 ± 9.42. 44 This study determined that the mean psychological flexibility score of the participants was 27.56 ± 11.06. Although the result obtained in this study was a bit higher compared to a study conducted before the COVID‐19 pandemic, it represents lower psychological flexibility. This result indicates that the students were unable to manage the uncertainty caused by COVID‐19 functionally. Additionally, the fact that the study was carried out in the first 4 weeks after the COVID‐19 alarm status ended may have affected the psychological flexibility of the students. This is because, in this process, as in many European countries, although the epidemic followed a horizontal course in Turkey, new cases and deaths continued.
Positive changes that emerge as a result of the struggle against difficult life crises express PTG. Positive psychological changes may be observed in individuals in terms of subjectively reported self‐perception, interpersonal relations, and perspective on life after experiencing traumatic events such as the COVID‐19 pandemic.19, 45 Although there is no study examining the PTG of nursing students in any epidemic process, the mean PTG score of the participants was determined as 70.53 ± 17.26 in a study conducted to determine the PTG of nurses during the COVID‐19 pandemic process. 45 It may be stated that other studies on PTG in the literature cover various conditions and populations. The PTG scores of the individuals exposed to disasters such as earthquakes and individuals diagnosed with breast cancer and HIV in the literature were 58.08 ± 23.33, 46 48.23 ± 23.96, 47 and 61.26 ± 25.34, 48 respectively. The mean PTG score of the participants in this study was 63.49 ± 20.64, and it pointed out a higher result in comparison to other studies. This proves that the participants experienced positive changes in terms of subjective self‐perception, interpersonal relations, and perspective on life during the COVID‐19 pandemic).19, 20, 21 Additionally, the fact that the nursing students witnessed the difficulties experienced by their colleagues working in the field, being aware of the high risk, may have caused them to analyze the current situation and possible problems in a rational manner. This, in turn, may have created positive emotions in their rational responses to the experience and increased their preparedness for such situations in the future. This study showed that nursing students who were female and had a high economic level had higher PTG levels. In several clinical trials examining PTG in parallel with this finding, it has been reported that women 49 and individuals with higher household incomes 50 have higher PTG levels. Although there was no statistical difference between the PTG levels of the students according to their education years in this study, it was revealed that senior nursing students had a higher PTG score. This may be evidence that senior nursing students have learned to take care of themselves and are better able to cope with crisis situations as a result of their theoretical training as well as their clinical experience.
Psychological flexibility which contributes to psychological resilience is defined as the ability to accept events and situations without experiencing emotional avoidance, and it is closely related to the individual's continuation of their life in line with their values despite negative experiences. 51 This study showed that psychological flexibility explained 36.7% of the total variance observed in psychological resilience. Researchers report that targeting psychological flexibility following a trauma may provide improvement by increasing resilience. 52 The results of a study that examined psychological resilience and flexibility among university students revealed that the participants' behaviors consistent with the values related to psychological flexibility explained 20% of the total variance observed in endurance. 53 A study conducted with nursing students reported that resilience had a significant effect on the correlation between awareness, self‐efficacy, and coping, which are compounds of psychological flexibility, and psychological compliance. 54 Another study conducted with nursing students determined that awareness which is one of the components of psychological flexibility explained 23% of the variance in resilience. 55 This study found that the nursing students had strong psychological flexibility with a higher rate than other studies on the background of their psychological resilience after the alarm period during which the psychological crisis caused by the COVID‐19 pandemic was intense. This finding can be explained by the fact that nursing students stay in a flexible psychology by accepting the dynamic process of the pandemic and analyzing potential problems rationally. Additionally, nursing students were exempted from all practice areas, including the clinical field, since the time period in which the study was conducted corresponded to the period when the school lessons ended. Since this situation kept nursing students away from the risk of disease, even if a little, they may have brought them closer to positive psychology and affected the results.
The findings of this study showed that psychological resilience was a predictive factor affecting PTG. Resilience is conceptualized as an individual's ability to resist behavioral and emotional problems despite the risk of stress, distress or change. 56 An individual with a high level of psychological resilience tries to find a meaning in every situation and tends to adapt in a positive direction to face problems as a challenge instead of avoiding various negativities.57, 58 Considering that PTG has an established conceptual basis for a positive change in the process of challenging and coping after experiencing distress just like psychological resilience,19, 20 the strong correlation between PTG and psychological resilience among the participants in this study might not be surprising. Studies conducted with nursing students,59, 60 university students, 58 and healthcare specialists 61 have revealed a positive correlation between PTG and psychological resilience. However, no significant correlations were found between psychological flexibility and PTG in this study. In other words, psychological flexibility was not a significant parameter that determined PTG. This result may be explained with the possibility that the psychological flexibility levels of the participants were not sufficient due to their young age. In this context, it does not seem surprising that psychological flexibility was not a determinant for PTG.
7. LIMITATIONS
This study is the first study to report the positive psychological dynamics of nursing students in Turkey after a 12‐week period of alarm, when the acute effects of the outbreak were felt extensively on the national level. However, the study had limitations that need to be addressed. First, the generalizability of the obtained findings is low since the study was conducted with nursing students at one institution. Second, these data are cross sectional, and the nature of the analyses is correlational. Causality cannot be directly deducted. Finally, the data were collected shortly after the alarm status of the pandemic, and although the search for psychological experience was important during this study period, the scores obtained from the scales could not be obtained from a longitudinal perspective.
8. CONCLUSION
The current findings reveal that psychological flexibility is important to support the psychological resilience of nursing students after the primary acute period of the COVID‐19 pandemic, and psychological resilience is of great importance to support their PTG. The results may provide clues to helping implement target strategies to support students' positive psychology in nursing education.
8.1. Implications for nursing practice
Tragedy, suffering, and losses are an integral part of nurses' daily lives just like during the COVID‐19 pandemic. Considering that other pandemics will potentially emerge in the future, 17 psychological flexibility, psychological resilience, and PTG seem important to help nursing students be prepared for their transition to the profession, and to support them to cope with difficulties. Considering the importance of these dynamics, incorporating psychological resilience and psychological flexibility into nursing education may help smoothing the transition of students to professional nursing roles. Psychosocial approaches using acceptance and awareness strategies such as acceptance and commitment therapy to support psychological flexibility and resilience are preferred.62, 63 In a recent review study, five basic methods such as adoption of peer activities, reflective practice, guided work, problem‐based learning/inquiry‐based learning, and experiential learning were determined as learning and teaching approaches that support resilience in nursing students. 41 Strategies such as awareness training, conflict management skills, stress management skills, biofeedback, communication skills, and development of emotional intelligence may be included in the nursing curriculum to support resilience considering that they are effective.64, 65, 66, 67
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Supporting information
Supporting information.
Yıldız E. Posttraumatic growth and positive determinants in nursing students after COVID‐19 alarm status: A descriptive cross‐sectional study. Perspect Psychiatr Care. 2021;57:1876‐1887. 10.1111/ppc.12761
DATA AVAILABILITY STATEMENT
The data used to support the findings of this study are available from the corresponding author upon request.
REFERENCES
- 1. World Health Organization . (2020). WHO characterizes COVID‐19 as a pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed July 8, 2020.
- 2. Day M. Covid‐19: surge in cases in Italy and South Korea makes pandemic look more likely. BMJ. 2020;368:m751. 10.1136/bmj.m751 [DOI] [PubMed] [Google Scholar]
- 3. Zhang W, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID‐19 epidemic in China. Psychother Psychosom. 2020;89:242‐250. 10.1159/000507639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization . (2020). Coronavirus Disease (COVID‐19) Situation Dashboard. https://covid19.who.int/
- 5. Republic of Turkey Ministry of Health . (2020). Türkiye günlük koronavirüs tablosu erişim (Daily Turkey coronavirus table access). https://covid19.saglik.gov.tr/. Accessed December 8, 2020.
- 6. Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID‐19. J Crit Care. 2020;57:279‐283. 10.1016/j.jcrc.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization . (2021). Coronavirus disease (COVID‐19): vaccines. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-(covid-19)-vaccines. Accessed February 19, 2021.
- 8. Centers for Disease Control and Prevention . (2021). Ensuring the safety of COVID‐19 vaccines in the United States. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety.html. Accessed February 15, 2021.
- 9. Jackson D, Bradbury‐Jones C, Baptiste D, et al. Life in the pandemic: Some reflections on nursing in the context of COVID‐19. J Clin Nurs. 2020;29:2041‐2043. 10.1111/jocn.15257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Republic of Turkey Higher Education Council . (2020). Statements by the council of higher education on education and training processes in the new epidemic of coronary disease. https://www.yok.gov.tr/Sayfalar/Haberler/2020/universitelerde-uygulanacak-uzaktan-egitime-iliskin-aciklama.aspx. Accessed March 18, 2020.
- 11. Kürtüncü M, Aylin K. COVID‐19 pandemisi döneminde hemşirelik öğrencilerinin uzaktan eğitim konusunda yaşadiklari sorunlar (Problems experienced by nursing students on distance education during the COVID‐19 pandemic period). Avrasya Sosyal ve Ekonomi Araştırmaları Dergisi. 2020;7(5):66‐77. [Google Scholar]
- 12. Vatan F, Avdal EÜ, Yağcan H, Şanlı D. COVID‐19 pandemisi ve hemşirelik eğitimi derneği faaliyetleri (COVID‐19 pandemic and nursing education association activities). Koç Üniversitesi Hemşirelikte Eğitim ve Araştırma Dergisi. 2020;17(4):369‐373. 10.5222/KUHEAD.2020.32858 [DOI] [Google Scholar]
- 13. Chang E, Daly J. Transitions in nursing‐e‐book: preparing for professional practice. Elsevier Health Sciences; 2012. [Google Scholar]
- 14. Zandifar A, Badrfam R. Iranian mental health during the COVID‐19 epidemic. Asian J Psychiatry. 2020;51:101990. 10.1016/j.ajp.2020.101990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dan Z. China adopts non‐contact free consultation to help the public cope with the psychological pressure caused by new coronavirus pneumonia. Asian J Psychiatry. 2020;52:102093. 10.1016/j.ajp.2020.102093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. González‐Sanguino C, Ausín B, Castellanos MÁ, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID‐19) in Spain. Brain Behav Immun. 2020;87:172‐176. 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yıldız E. What can be said about lifestyle and psychosocial issues during the coronavirus disease pandemic? first impressions. Perspect Psychiatr Care. 2021;57(1):413‐415. 10.1111/ppc.12560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Keener TA, Hall K, Wang K, Hulsey T, Piamjariyakul U. Quality of Life, Resilience, and Related Factors of Nursing Students During the COVID‐19 Pandemic [published online ahead of print December 29, 2020]. Nurse Educator. 10.1097/nne.0000000000000969 [DOI] [PubMed] [Google Scholar]
- 19. Tedeschi R, Shakespeare‐Finch J, Taku K, Calhoun L. Posttraumatic growth. Routledge; 2018. [Google Scholar]
- 20. Calhoun LG, Tedeschi RG. Handbook of posttraumatic growth: research and practice. Routledge; 2014. [Google Scholar]
- 21. Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health. 2014;35(1):169‐183. 10.1146/annurev-publhealth-032013-182435 [DOI] [PubMed] [Google Scholar]
- 22. Ewert A, Tessneer S. Psychological resilience and posttraumatic growth: an exploratory analysis. J Exp Educ. 2019;42(3):280‐296. 10.1177/1053825919859027 [DOI] [Google Scholar]
- 23. Brooks S, Amlôt R, Rubin GJ, Greenberg N. Psychological resilience and post‐traumatic growth in disaster‐exposed organisations: overview of the literature. BMJ Mil Health. 2020;166(1):52‐56. 10.1136/jramc-2017-000876 [DOI] [PubMed] [Google Scholar]
- 24. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet. 2020;395(10227):912‐920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tan S‐Y. Resilience and posttraumatic growth: empirical evidence and clinical applications from a Christian perspective. J Psychol Christianity. 2013;32(4):358‐364. [Google Scholar]
- 26. Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clin Psychol Rev. 2010;30(7):865‐878. 10.1016/j.cpr.2010.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Harris R. ACT made simple: an easy‐to‐read primer on acceptance and commitment therapy. New Harbinger Publications; 2019. [Google Scholar]
- 28. Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: the process and practice of mindful change. Guilford Press; 2011. [Google Scholar]
- 29. Afifi A, May S, Donatello R, Clark VA. Practical multivariate analysis. 6th ed. CRC Press; 2019. [Google Scholar]
- 30. Bond FW, Hayes SC, Baer RA, et al. Preliminary psychometric properties of the Acceptance and Action Questionnaire–II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther. 2011;42(4):676‐688. 10.1016/j.beth.2011.03.007 [DOI] [PubMed] [Google Scholar]
- 31. Yavuz F, Ulusoy S, Iskin M, et al. Turkish version of Acceptance and Action Questionnaire‐II (AAQ‐II): a reliability and validity analysis in clinical and non‐clinical samples. Bull Clin Psychopharmacol. 2016;26(4):397‐408. 10.5455/bcp.20160223124107 [DOI] [Google Scholar]
- 32.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. (2008). The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194‐200. 10.1080/10705500802222972 [DOI] [PubMed]
- 33. Doğan T. Kısa psikolojik sağlamlık ölçeği'nin Türkçe uyarlaması: geçerlik ve güvenirlik çalışması [Adaptation of the Brief Resilience Scale into Turkish: a validity and reliability study]. J Happiness Well‐Being. 2015;3(1):93‐102. [Google Scholar]
- 34. Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: Measuring the positive legacy of trauma. J Trauma Stress. 1996;9(3):455‐471. 10.1002/jts.2490090305 [DOI] [PubMed] [Google Scholar]
- 35. Kağan M, Güleç M, Boysan M, Çavuş H. Travma sonrasi büyüme envanteri'nin Türkçe versiyonunun normal toplumda hiyerarşik faktör yapısı [Hierarchical factor structure of the Turkish version of the posttraumatic growth inventory in a normal population]. TAF Prev Med Bull. 2012;11(5):617‐624. 10.5455/pmb.1323620200 [DOI] [Google Scholar]
- 36. Fox J, Weisberg S. An R companion to applied regression. 3rd ed. Sage Publications; 2019. [Google Scholar]
- 37. Lekan DA, Ward TD, Elliott AA. Resilience in baccalaureate nursing students: An exploration. J Psychosoc Nurs Ment Health Serv. 2018;56(7):46‐55. 10.3928/02793695-20180619-06 [DOI] [PubMed] [Google Scholar]
- 38. Çetin C, Özlem A. COVID‐19 Pandemi sürecinde yalnizlik ve psikolojik dayaniklilik: bir kamu üniversitesi öğrencileri örneklemi [COVID‐19 pandemic process and psychological resilience: sample of students from a public universıty]. Avrasya Sosyal ve Ekonomi Araştırmaları Dergisi. 2020;7(5):170‐189. [Google Scholar]
- 39. Yıldırım M, Arslan, G . Exploring the associations between resilience, dispositional hope, preventive behaviours, subjective well‐being, and psychological health among adults during early stage of COVID‐19. Curr Psychol. 2020. 10.1007/s12144-020-01177-2 [DOI] [PMC free article] [PubMed]
- 40. Yıldırım M, Arslan G, Wong PTP. Meaningful living, resilience, affective balance, and psychological health problems among Turkish young adults during coronavirus pandemic. Curr Psychol. 2021. 10.1007/s12144-020-01244-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Walsh P, Owen PA, Mustafa N, Beech R. Learning and teaching approaches promoting resilience in student nurses: an integrated review of the literature. Nurse Educ Pract. 2020;45:102748. 10.1016/j.nepr.2020.102748 [DOI] [PubMed] [Google Scholar]
- 42. Cleary M, Visentin D, West S, Lopez V, Kornhaber R. Promoting emotional intelligence and resilience in undergraduate nursing students: an integrative review. Nurse Educ Today. 2018;68:112‐120. 10.1016/j.nedt.2018.05.018 [DOI] [PubMed] [Google Scholar]
- 43. Chamberlain D, Williams A, Stanley D, Mellor P, Cross W, Siegloff L. Dispositional mindfulness and employment status as predictors of resilience in third year nursing students: a quantitative study. Nurs Open. 2016;3(4):212‐221. 10.1002/nop2.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Uygur SS. Üniversite öğrencilerinin psikolojik esneklik düzeylerinin yordanmasinda duygusal şemalarin rolü: Buca eğitim fakültesi örneği (The role of emotional schemes in predicting psychological flexibility levels of university students: the example of faculty of Buca educatıon). Jass Stud–– J Acad Social Sci Stud. 2018;70(1):135‐151. 10.9761/JASSS7641 [DOI] [Google Scholar]
- 45. Cui Pp, Wang Pp, Wang K, Ping Z, Wang P, Chen C. Post‐traumatic growth and influencing factors among frontline nurses fighting against COVID‐19. Occup Environ Med. 2020;78:129‐135. 10.1136/oemed-2020-106540 [DOI] [PubMed] [Google Scholar]
- 46. Wang W, Wu X, Lan X. Rumination mediates the relationships of fear and guilt to posttraumatic stress disorder and posttraumatic growth among adolescents after the Ya'an earthquake. Eur J Psychotraumatol. 2020;11(1):1704993. 10.1080/20008198.2019.1704993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Liu X, Wang L, Zhang Q, Wang R, Xu W. Less mindful, more struggle and growth: mindfulness, posttraumatic stress symptoms, and posttraumatic growth of breast cancer survivors. J Nerv Ment Dis. 2018;206(8):621‐627. [DOI] [PubMed] [Google Scholar]
- 48. Murphy PJ, Hevey D. The relationship between internalised HIV‐related stigma and posttraumatic growth. AIDS Behav. 2013;17(5):1809‐1818. 10.1007/s10461-013-0482-4 [DOI] [PubMed] [Google Scholar]
- 49. Koutná V, Jelínek M, Blatný M, Kepák T. Predictors of posttraumatic stress and posttraumatic growth in childhood cancer survivors. Cancers. 2017;9(26):1‐11. 10.3390/cancers9030026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Zhang L, Lu Y, Qin Y, Xue J, Chen Y. Post‐traumatic growth and related factors among 1221 Chinese cancer survivors. Psycho‐Oncology. 2020;29(2):413‐422. 10.1002/pon.5279 [DOI] [PubMed] [Google Scholar]
- 51. Bryan CJ, Ray‐Sannerud B, Heron EA. Psychological flexibility as a dimension of resilience for posttraumatic stress, depression, and risk for suicidal ideation among Air Force personnel. J Contextual Behav Sci. 2015;4(4):263‐268. 10.1016/j.jcbs.2015.10.002 [DOI] [Google Scholar]
- 52. Meyer EC, Kotte A, Kimbrel NA, et al. Predictors of lower‐than‐expected posttraumatic symptom severity in war veterans: The influence of personality, self‐reported trait resilience, and psychological flexibility. Behav Res Ther. 2019;113:1‐8. 10.1016/j.brat.2018.12.005 [DOI] [PubMed] [Google Scholar]
- 53. Murrell AR, Jackson R, Lester EG, Hulsey T. Psychological flexibility and resilience in parentally bereaved college students. OMEGA––J Death Dying. 2018;76(3):207‐226. 10.1177/0030222817693154 [DOI] [PubMed] [Google Scholar]
- 54. Rees CS, Heritage B, Osseiran‐Moisson R, et al. Can we predict burnout among student nurses? An exploration of the ICWR‐1 model of individual psychological resilience. Front Psychol. 2016;7:1072. 10.3389/fpsyg.2016.01072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mathad MD, Pradhan B, Rajesh SK. Correlates and predictors of resilience among baccalaureate nursing students. J Clin Diag Res. 2017;11(2):JC05‐JC08. 10.7860/JCDR/2017/24442.9352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zeidner M, Kampler S. Memory traces of childhood exposure to terror attack and resilience and post‐traumatic growth in adulthood. Pers Individ Dif. 2020;155:109719. 10.1016/j.paid.2019.109719 [DOI] [Google Scholar]
- 57. Goldstein S, Brooks RB. Why study resilience? In: Goldstein S, Brooks RB, eds. Handbook of Resilience in Children. Springer US; 2013:3‐14. [Google Scholar]
- 58. Kim I, Oh W‐O. Predictors of posttraumatic growth among university students who experienced a recent earthquake. Issues Ment Health Nurs. 2019;40(2):176‐184. 10.1080/01612840.2018.1471759 [DOI] [PubMed] [Google Scholar]
- 59. Kim M‐J. Effects of emotional intelligence, resilience, and post‐traumatic growth on communication skills of nursing students. J Ind Converg. 2018;16(3):23‐32. 10.22678/JIC.2018.16.3.023 [DOI] [Google Scholar]
- 60. Li Y, Cao F, Cao D, Liu J. Nursing students' post‐traumatic growth, emotional intelligence and psychological resilience. J Psychiatr Ment Health Nurs. 2015;22(5):326‐332. 10.1111/jpm.12192 [DOI] [PubMed] [Google Scholar]
- 61. Nishi D, Kawashima Y, Noguchi H, et al. Resilience, post‐traumatic growth, and work engagement among health care professionals after the Great East Japan Earthquake: a 4‐year prospective follow‐up study. J Occup Health. 2016;58(4):347‐353. 10.1539/joh.16-0002-OA [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Yıldız E. The effects of acceptance and commitment therapy in psychosis treatment: a systematic review of randomized controlled trials. Perspect Psychiatr Care. 2020a;56(1):149‐167. 10.1111/ppc.12396 [DOI] [PubMed] [Google Scholar]
- 63. Yıldız E. The effects of acceptance and commitment therapy on lifestyle and behavioral changes: a systematic review of randomized controlled trials. Perspect Psychiatr Care. 2020b;56(3):657‐690. 10.1111/ppc.12482 [DOI] [PubMed] [Google Scholar]
- 64. Mealer M, Hodapp R, Conrad D, Dimidjian S, Rothbaum BO, Moss M. Designing a resilience program for critical care nurses. AACN Adv Crit Care. 2017;28(4):359‐365. 10.4037/aacnacc2017252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Sigalit W, Sivia B, Michal I. Factors associated with nursing students' resilience: communication skills course, use of social media and satisfaction with clinical placement. J Prof Nurs. 2017;33(2):153‐161. 10.1016/j.profnurs.2016.08.006 [DOI] [PubMed] [Google Scholar]
- 66. Stacey G, Aubeeluck A, Cook G, Dutta S. A case study exploring the experience of resilience‐based clinical supervision and its influence on care towards self and others among student nurses. Int Pract Develop J. 2017;7(2):1‐16. 10.19043/ipdj.72.005 [DOI] [Google Scholar]
- 67. van der Riet P, Levett‐Jones T, Aquino‐Russell C. The effectiveness of mindfulness meditation for nurses and nursing students: an integrated literature review. Nurse Educ Today. 2018;65:201‐211. 10.1016/j.nedt.2018.03.018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.


