Abbreviations
- BPO
benign prostate obstruction
- COVID‐19
coronavirus disease 2019
- IRR
incidence rate ratio
Healthcare lockdown involving the cancellation or postponement of non‐urgent examinations and treatments during the coronavirus disease 2019 (COVID‐19) pandemic has reduced the number of emergency department visits by urological patients [1, 2]. As most urological conditions are treated non‐urgently, a major result of the lockdown may be an accumulating treatment backlog in elective urological surgery. Indeed, the predicted global urological surgery backlog has been estimated to be 2.5 million procedures [3].
We gathered data from the discharge registers of three Finnish public hospitals (Central Finland Hospital, Mikkeli Central Hospital, and Tampere University Hospital), which serve a combined catchment population of 900 000 citizens. Data on referrals to a urologist and elective urological procedures (Nordic Medico‐Statistical Committee [NOMESCO] procedure codes K*) were collected for the years 2017–2020. Population data were obtained from Statistics Finland [4].
Monthly and annual incidences with 95% CIs of referrals and elective surgical procedures were calculated by Poisson exact method. The year 2020 was compared to the reference years 2017–2019 by incidence rate ratios (IRRs), focussing on the changes in incidences during the nationwide lockdown period (16 March to 1 June 2020; including the cancelling or postponing of non‐acute public healthcare visits) and during the period of regional restrictions (September onwards; more restrained stepwise restrictions). Annual and monthly mean waiting times for elective urological surgery were calculated along with 95% CIs in days. The incidences of the most common urological procedures were examined separately. These procedures included: benign prostate obstruction (BPO) procedures, major surgery for urological cancers (radical prostatectomy, radical cystectomy, radical nephrectomy, and partial nephrectomy), urinary stone removal procedures, and circumcision and other foreskin procedures. Ethical committee approval was not required owing to the register‐based study design.
During 2017–2020, the urological units of the study hospitals received 44 752 referrals overall, and a total of 12 832 urological procedures were performed. In 2020, the annual referral incidence was slightly below the reference level (IRR 0.97, 95% CI 0.96–0.98; Figure 1). The monthly incidence decreased from the beginning of lockdown in March. After recovering during the summer, the referral incidence followed the reference levels without any rebound effect. A similar trend was observed in the overall incidence of urological surgery. In addition, the surgery incidence slightly decreased again during the period of regional restrictions (September onwards), resulting in 9% fewer procedures in 2020 when compared to the reference years (IRR 0.91, 95% CI 0.89–0.93). After a slight occasional decrease during the lockdown, surgery waiting times increased in summer 2020. Although a recovery of waiting times was seen in October and thereafter, the mean surgery waiting time was 10% higher in 2020 when compared to the reference years.
Fig. 1.
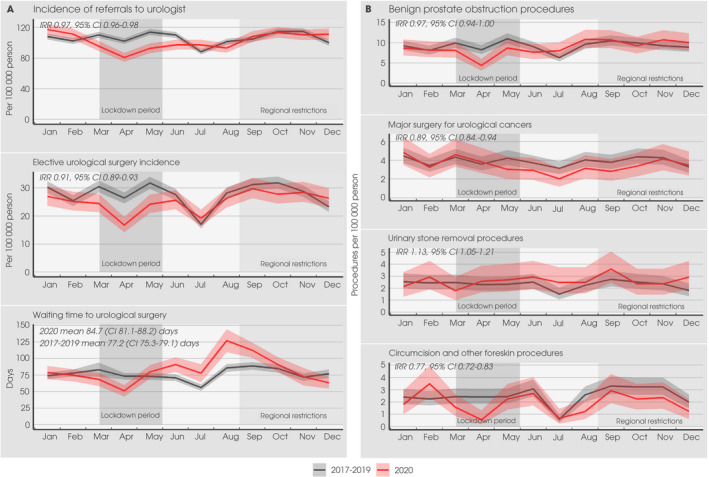
(A) Monthly incidences and 95% CIs of referrals to urological units and elective urological surgeries, and the mean monthly waiting times for urological surgery in 2020 and in the reference years. (B) Monthly incidences and 95% CIs of most common elective urological procedures in 2020 and in the reference years.
Of the most common urological procedure types, the lockdown had a clear negative effect on the incidence of BPO, as well as foreskin excision, procedures (Fig. 1). However, the annual incidence of BPO procedures remained at the reference level, whereas the annual incidence of foreskin procedures was 23% below the reference level in 2020 (IRR 0.77, 95% CI 0.72–0.83). The incidence of major urological cancer surgery decreased after the lockdown and remained lower than the reference level until November, with a total annual decrease of 11% (IRR 0.84–0.94). In urinary stone procedures, the incidence increased during the lockdown and remained slightly over the reference level until October, with a total annual increase of 13% (IRR 1.13, 95% CI 1.05–1.21).
The results of the present study confirm the concerns that the COVID‐19 pandemic has had a considerable impact on specialised urological care in Finland. The lockdown decreased the referral and urological surgery incidences. Furthermore, surgery waiting times increased after the lockdown.
The lockdown had the most prominent impact on those procedures related to BOO and foreskin diseases, which is consistent with results reported in a previous study [5]. Patients with these diseases are usually referred to a urologist via primary healthcare units with non‐urgent referrals.
The incidence of major urological surgery, in turn, decreased in the last third of the lockdown and remained lower until November. These procedures are performed due to cancer or, in rare cases, other severe diseases, and are therefore performed urgently after diagnosis. Thus, the decrease may be related to primary care lockdown that likely resulted in delays in the examination and treatment of patients with urinary symptoms. This, in the worst case, may be observed as increased mortality or incidence of metastatic cancers in future.
Finally, in contrast to the other procedures, the number of urinary stone removal procedures increased during the COVID‐19 pandemic. Due to the intense pain experienced during a urinary stone attack, patients are usually diagnosed in the emergency department, and thereby avoided the delays caused by the primary care lockdown. However, the increased incidence of urinary stone removals was still somewhat unexpected considering the findings of two previous studies, which reported that emergency department visit incidence remained similar both before and during the first COVID‐19 wave [6, 7]. Urinary stone disease is relatively prevalent in the younger population with a lower risk of severe COVID‐19 [8]. Due to the effects of the lockdown, free space was available in the operation capacity of urological units. Therefore, to fill the gap after the lockdown, patients at low risk of COVID‐19 were the first to be invited to elective operations, probably involving a higher‐than‐average proportion of patients with urinary stones.
The strength of the present study is that the data used in the study were gathered from three large Finnish hospitals that are representative of the Finnish public healthcare system. The main limitation of the present study was the lack of data on indications of referrals to a urologist that prevented us from further assessing the relationship between the referrals and the surgical procedures for specific diseases. However, it is unlikely that this (i.e. the presentation of different diseases) would have changed during the study period.
In conclusion, the healthcare lockdown due to COVID‐19 in Finland decreased the availability of non‐urgent specialised urological care. Although the incidence of surgery recovered after lockdown, there may still be a substantial underlying backlog that may result in more patients presenting at specialised urological units with severe urological conditions after the pandemic.
Disclosure of Interest
The authors declare no conflicts of interest.
Funding
None.
References
- 1. Gallioli A, Albo G, Lievore E et al. How the COVID‐19 wave changed emergency urology: results from an academic tertiary referral hospital in the epicentre of the Italian red zone. Urology 2021; 147: 43–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grasso AA, Massa G, Castelnuovo M. The impact of COVID‐19 pandemic on urological emergencies: a multicenter experience on over 3,000 patients. Urol Int 2021; 105: 17–20 [DOI] [PubMed] [Google Scholar]
- 3. Negopdiev D, Collaborative C, Hoste E. Elective surgery cancellations due to the COVID‐19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg 2020; 107: 1440–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Statistics Finland . Population data. 2021; Available at: www.stat.fi/index_en.html. (day cited 12 March 2021)
- 5. Teoh JC, Ong WL, Gonzalez‐Padilla D et al. A global survey on the impact of COVID‐19 on urological services. Eur Urol 2020; 78: 265–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Anderson S, McNicholas D, Murphy C et al. The impact of COVID‐19 on acute urinary stone presentations: a single‐centre experience. Ir J Med Sci 2021. 10.1007/s11845-021-02562-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Flammia S, Salciccia S, Tufano A, Busetto GM, Ricciuti GP, Sciarra A. How urinary stone emergencies changed in the time of COVID‐19? Urolithiasis 2020; 48: 467–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Scales CD Jr, Smith AC, Hanley JM, Saigal CS, Project UDiA . Prevalence of kidney stones in the United States. Eur Urol 2012; 62: 160–5 [DOI] [PMC free article] [PubMed] [Google Scholar]


