Abstract
Aim
To explore the mediating role of post‐traumatic growth and perceived professional benefits between resilience and intent to stay among Chinese nurses to support Wuhan in managing COVID‐19.
Design
A cross‐sectional questionnaire survey.
Methods
In May 2020, the study recruited a convenience sample of 200 Chinese nurses to support Wuhan in managing COVID‐19. A set of self‐rating questionnaires was used to measure resilience, post‐traumatic growth, perceived professional benefits and intent to stay. Structural equation modelling was performed with 5,000 bootstrap samples using AMOS 23.0.
Results
The final model provided a good fit for the data. Resilience had the strongest direct effect on intent to stay. Perceived professional benefits partially mediated the association between resilience and intent to stay. Overall, the serial multiple mediations of post‐traumatic growth and perceived professional benefits in the relationship between resilience and intent to stay was statistically significant.
Keywords: Chinese nurses, COVID‐19, intent to stay, perceived professional benefits, post‐traumatic growth, resilience
1. INTRODUCTION
COVID‐19 was initially identified in Hubei province, in which the number of confirmed cases increased sharply in the early stage. As a significant public health emergency, 28,600 nurses were sent to Wuhan to fight against COVID‐19, accounting for nearly 68% of all frontline healthcare staff (Government of Hubei Province, 2020). These nurses risked their lives, undertook an enormous workload under high‐intensity pressure, and experienced long working hours, which cause serious negative emotions (Chen et al., 2020), professional burnout (Morgantini et al., 2020), job dissatisfaction (Zhang et al., 2020) and even a tendency to leave (Song et al., 2020). The COVID‐19 pandemic highlights the shortages of nurses that already exist, and widespread nursing shortages could lead to staff burnout and endanger patient safety.
2. BACKGROUND
COVID‐19, a major global public threat, severely affected frontline nurses' well‐being and the stability of the nursing team. Recent evidence has shown that nurses’ perceived threat of COVID‐19 would lead to negative behavioural outcomes, such as turnover intention (Irshad et al., 2020). Previous research confirmed that 24.8% of nurses intended to leave the field of nursing during the COVID‐19 pandemic in Egypt (Said & El‐Shafei, 2020). Thus, the retention of nurses is an essential concern for healthcare administrators. They need to consider effective measures to retain nurses and reduce their turnover intention.
Intent to stay is defined as the probability of nurses remaining in their profession and not looking for other job opportunities before retirement (Wang et al., 2012), which is the strongest predictor of nurses’ retention and a key to stabilizing the nursing team (Brown et al., 2013). Intent to stay and intent to leave are both relative concepts; research on intent to stay would focus on the positive impact that helps facilitate nurses’ retention. So far, very little attention has been paid to the intent to stay among the frontline nurses under COVID‐19 pandemic. The existing models of intent to stay (Cowden & Cummings, 2012; Ellenbecker, 2004; Tourangeau & Cranley, 2006) are not suitable for this group of people who experienced traumatic events. Therefore, we need to clarify the factors that influence the intent to stay among frontline nurses treating COVID‐19 patients and provide a theoretical basis for exploring measures to change these factors.
Existing research recognizes the critical role of positive psychology in nursing retention, which focuses more on personal strengths rather than weaknesses (Seligman & Csikszentmihalyi, 2014). Resilience is an essential concept in the field of positive psychology. It is defined as a human ability that adapts well in the face of tragedy, adversity, trauma, hardship or significant sources of stress (American Psychological Association, 2012). Resilience has high practical value in practice and could significantly enhance nurses’ intent to stay (Mills et al., 2017; Yu & Lee, 2018). Becoming more resilient helps individuals utilize available resources to cope, withstand and recover through difficult circumstances (American Psychological Association, 2012). Nurses with high levels of resilience can reduce emotional exhaustion, increase work engagement, identify or prevent potential problems and ultimately achieve personal and professional growth to promote retention. (Yu et al., 2019). The relationship between resilience and intent to stay has been initially confirmed by researchers, but the mechanism of how resilience affects intent to stay among nurses who manage COVID‐19 remains unclear. Thus, this study explores the direct and indirect effects of resilience and intent to stay among Chinese frontline nurses managing against the COVID‐19 epidemic.
Resilience, a positive resource, improves nurses’ perceived professional benefits, enhances job satisfaction, and shows less job burnout and job stress (Liu et al., 2019; Yu et al., 2019). Nurses’ perceived professional benefits are an important concept in positive psychology, which was proposed by Chinese scholar Hu (Hu & Liu, 2012). It is defined as nurses’ views on their gains and benefits during the process of employment, and their belief that the nursing profession can promote their overall growth and development (Hu & Liu, 2012). Hu et al. divided nurses’ perceived professional benefits into five dimensions: positive occupational perception, good nurse‐patient relationship, recognition from family, relatives, and friends, the sense of belonging to a team and self‐growth (Hu & Liu, 2012). Recent evidence suggests that nurses’ perceived professional benefits have a significantly positive effect on their intent to stay (Xiao et al., 2016). Overall, several studies support that resilience is a predictor of perceived professional benefits (Jin, 2019; Liu et al., 2019; Yu et al., 2019) and also affects intent to stay via the mediation of perceived professional benefits (Xiao et al., 2016). Consequently, we proposed a hypothesis that perceived professional benefits could be a potential mediating variable between resilience and intent to stay.
COVID‐19 severely affects frontline nurses' well‐being. Therefore, supporting Wuhan in treating COVID‐19 patients can be regarded as a traumatic experience by nurses. When faced with traumatic events, difficult losses or great pain, people will experience a variety of highly painful psychological reactions. They endure psychological struggles in dealing with those crises and can often see positive growth afterwards. In the mid‐1990s, psychologists Tedeschi and Calhoun first proposed the term “post‐traumatic growth,” which was an explanation of transformation following trauma (Tedeschi & Calhoun, 1996). Traumatic experiences do not directly lead to post‐traumatic growth. They are catalysts for creation of meaning, a necessary step in transforming an old (negative) schema into a more positive view (Xu et al., 2016). Some scholars believe that resilience can significantly predict post‐traumatic growth (Li et al., 2018; Zhang et al., 2019). In addition, existing studies have shown that people with post‐traumatic growth have a positive attitude towards their careers and show a strong willingness to stay in their current jobs (Hyatt‐Burkhart, 2014; Vough & Caza, 2017). A study pointed out that resilience was found to positively affect post‐traumatic growth and intent to stay (Çam, 2017). Therefore, we hypothesized that post‐traumatic growth is the mediating variable between resilience and intent to stay. Post‐traumatic growth has also been shown to have a positive impact on perceived professional benefits (Shao et al., 2019). The perceived professional benefits was in turn found to have a significant positive impact on intent to stay (Xiao et al., 2016). Recent evidence also shows that people's personal and professional post‐traumatic growth has a positive effect on their perceived professional benefits, and they gain a better understanding and appreciation of work, which indirectly or directly affects their intent to stay (Brooks et al., 2020; Hyatt‐Burkhart, 2014; Maitlis, 2020). Based on these findings, we also hypothesized that the positive effects of resilience on intent to stay would be mediated by post‐traumatic growth and perceived professional benefits.
The present study was designed to target Chinese nurses who support Wuhan in treating COVID‐19 patients and aimed to address the following questions: (a) What is the status of resilience, post‐traumatic growth, perceived professional benefits and intent to stay? (b) What is the mediating effect of post‐traumatic growth and perceived professional benefits between resilience and intent to stay among frontline nurses in China? The relationships hypothesized in the study are shown in Figure 1. We hypothesized that: (a) resilience would have a positive effect on intent to stay, post‐traumatic growth and perceived professional benefits; (b) resilience impacts intent to stay, mediated by post‐traumatic growth and perceived professional benefits.
FIGURE 1.
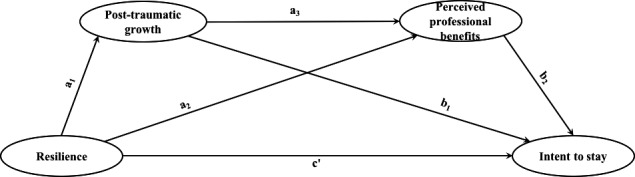
Hypothesized relationships among resilience, post‐traumatic growth, perceived professional benefits, and intent to stay
3. METHODS
3.1. Study design and participants
We conducted a cross‐sectional study from 30 April 2020 to 25 May 2020. Participants were nurses who came to Wuhan Mountain and Thor Mountain Square Cabin Hospital to treat COVID‐19 patients from January to April 2020 and had returned to their home hospitals during the survey period. Through convenience sampling, nurses supporting Wuhan were selected to complete the questionnaires. The inclusion criteria were as follows: (a) nurses who treated COVID‐19 patients in Wuhan; (b) those who have obtained a nurse professional qualification certificate; and (c) those who volunteered to participate in this study. The nurses who worked part‐time were excluded. The frontline nurses established WeChat groups during the COVID‐19 outbreak in Wuhan. Through the WeChat groups, the investigators, who received full training, sent the questionnaire link to the nurses who met the inclusion criteria. They were asked to complete the questionnaires independently and anonymously on the website https://www.wj.qq.com. The nurses needed to check "Agree" in an informed consent form before filling out the questionnaire. To prevent filling errors, researchers used unified filling guidelines to explain the questionnaires and set mandatory questions to ensure the integrity of the questionnaire. Using computerized calculations (Preacher & Coffman, 2006), we set the degree of freedom as 49, α = 0.05, 1‐β = 0.85, RMSEA (H0) = 0, and RMSEA (H1) was set as 0.06 for reasonable model fit (Bentler & Yuan, 1999), showing that the minimum sample size is at least 188 (MacCallum et al., 1996). We obtained 200 usable responses, with an effective response rate of 96.2%. The time taken by the nurses to fill out the questionnaire was 8 min and 48 s.
3.2. Instruments
3.2.1. Demographic information data
The demographic information consisted of 11 variables, including five of personal data (gender, age, marital status, education level and children‘s situation), four of working information (department, position, professional title and nursing experience) and two related to the experience of treating COVID‐19 patients (ever previously been involved in public health emergencies and rescue time).
3.2.2. Measurement of resilience
The 10‐Item Connor‐Davidson Resilience Scale (CD‐RISC‐10) was developed by Campbell‐Sills and Stein (2007) and was designed to measure resilience. The Chinese version of CD‐RISC‐10 is a translation by Ye et al. (2016). The CD‐RISC‐10 is a unidimensional scale that consists of 10 items. Each item was rated by the respondents on a 5‐point Likert scale, ranging from 0 (not true at all) to 4 (true nearly all the time). The scale score was calculated by summing all the items that ranged from 0 to 40, a higher score on the CD‐RISC‐10 reflecting higher resilience. The CD‐RISC‐10 has been found suitable for Chinese nurses and has good validity and reliability (Kong et al., 2016). In this study, the Cronbach's coefficient was 0.955.
3.2.3. Measurement of post‐traumatic growth
Tedeschi et al. initially developed the Posttraumatic Growth Inventory in 1996 (Tedeschi & Calhoun, 1996), and Wang et al. translated it to a Chinese version (Wang et al., 2011). This scale includes 20 items and five dimensions: appreciation of life, new possibilities, relating to others, personal strength and self‐transformation. This scale is also a self‐report scale. Each item is scored on a 6‐point Likert scale, ranging from 0 (I did not experience this change as a result of my crisis) to 5 (I experienced this change to a very great degree as a result of my crisis). The total score ranged from 0 to 100, with higher scores reflecting more post‐traumatic growth. In our study, the Cronbach's coefficient for the total scale was 0.968, and each dimension was 0.869–0.925.
3.2.4. Measurement of perceived professional benefits
The Nurses’ Perceived Professional Benefits Questionnaire compiled by Hu and Liu (2012) was used to measure nurses' perceived professional benefits. This questionnaire consists of 33 items and five dimensions: positive occupational perception, good nurse‐patient relationship, recognition from family, relatives, and friends, the sense of belonging to a team and self‐growth (Hu & Liu, 2014). Each item was rated on a 5‐point Likert scale from 1 (strongly disagree) to 5 (strongly agree). The total score ranged from 33 to 165; the higher the score, the higher the level of professional benefits perceived by nurses. In our study, the Cronbach's coefficient for the total questionnaire was 0.967, and each dimension was 0.838–0.919.
3.2.5. Measurement of intent to stay
Nurse Intent to Stay Questionnaire was developed by Tao and Wang (2010). It has six items and uses a 5‐point Likert scale. Among them, items 2, 3 and 6 were reverse scoring questions, and the results were adjusted to opposite scoring during statistics. The total score on the questionnaire ranged from 6 to 30. The higher the score, the stronger the intention for nurses to retain. In this study, the Cronbach's coefficient was 0.770, which indicates excellent reliability and validity in the nurse population (Tao & Wang, 2010).
3.3. Data analysis
Data coding, cleaning and analysis were performed using SPSS Statistics 25.0 and Amos 23.0 for Mac. We used descriptive analysis to present demographic data and then conducted a Pearson's correlation analysis to discover the relationships between resilience, intent to stay, post‐traumatic growth and perceived professional benefits. Third, according to previous studies of these four variables, we established a mediating structural equation model using serial multivariable mediation analysis. Finally, the serial mediation effect of post‐traumatic growth and perceived professional benefits was tested based on bootstrap results. The indirect effect could be statistically significant if the 95% confidence interval (CI) with 5,000 bootstrapping re‐samples did not include zero.
3.4. Ethical consideration
This study was approved by the Ethics Committee of Shanghai Chest Hospital, and the approval number was KS2038.
4. RESULTS
4.1. Demographic characteristic
The demographic data of the 200 participants are summarized in Table 1. The participants’ average age was 32.28 ± 6.21, and the average rescue time was 51.57 ± 12.64 days. Descriptive statistics of resilience, post‐traumatic growth, perceived professional benefits and intent to stay are shown in Table 2. There were no missing values in any of the data.
TABLE 1.
The demographic characteristics of the study participants (N = 200)
| Demographic variable | N | % |
|---|---|---|
| Gender | ||
| Female | 166 | 83.0 |
| Male | 34 | 17.0 |
| Age (years) | ||
| ≤30 | 89 | 44.5 |
| 31–40 | 93 | 46.5 |
| >40 | 18 | 9.0 |
| Marital status | ||
| Married/divorced | 126 | 63.0 |
| Single | 74 | 37.0 |
| Children's situation | ||
| One or more children | 109 | 54.5 |
| N/A | 91 | 45.5 |
| Education level | ||
| Technical secondary school | 4 | 2.0 |
| Junior college | 42 | 21.0 |
| College or above | 154 | 77.0 |
| Nursing experience (years) | ||
| ≤10 | 105 | 52.5 |
| 11–20 | 73 | 36.5 |
| >20 | 22 | 11.0 |
| Professional title | ||
| Nurse | 49 | 24.5 |
| Senior nurse | 92 | 46.0 |
| Primary nurse | 53 | 26.5 |
| Chief nurse | 6 | 3.0 |
| Position | ||
| General nurse | 150 | 75.0 |
| Clinical nursing teacher | 17 | 8.5 |
| Head nurse | 32 | 16.0 |
| Assistant nursing director | 1 | 0.5 |
| Department | ||
| Medicine department | 74 | 37.0 |
| Surgery department | 34 | 17.0 |
| Emergency department | 13 | 6.5 |
| ICU | 70 | 35.0 |
| Others | 9 | 4.5 |
| Ever previously been involved in public health emergencies | ||
| N/A | 190 | 95.0 |
| Yes | 10 | 5.0 |
| Rescue time (days) | ||
| ≤40 | 23 | 11.5 |
| 41–60 | 124 | 62.0 |
| >60 | 53 | 26.5 |
TABLE 2.
Description analysis and correlations of resilience, nurses’ perceived professional benefits, post‐traumatic growth and intent to stay
| Variable | Mean ± SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nurses’ perceived professional benefits | 4.33 ± 0.49 | |||||||||||||
| Positive occupational perception | 4.27 ± 0.55 | 0.919** | ||||||||||||
| Good nurse‐patient relationship | 4.36 ± 0.54 | 0.940** | 0.851** | |||||||||||
| Recognition from family, relatives, and friends | 4.40 ± 0.52 | 0.923** | 0.804** | 0.872** | ||||||||||
| Sense of belonging to a team | 4.32 ± 0.53 | 0.944** | 0.827** | 0.839** | 0.834** | |||||||||
| Self‐growth | 4.30 ± 0.49 | 0.946** | 0.807** | 0.845** | 0.828** | 0.913** | ||||||||
| Post‐traumatic growth | 3.18 ± 1.06 | 0.529** | 0.460** | 0.487** | 0.473** | 0.490** | 0.548** | |||||||
| Appreciation of life | 3.60 ± 1.08 | 0.500** | 0.426** | 0.465** | 0.476** | 0.457** | 0.509** | 0.930** | ||||||
| Personal strength | 3.50 ± 1.13 | 0.551** | 0.501** | 0.510** | 0.488** | 0.509** | 0.556** | 0.920** | 0.877** | |||||
| Relating to others | 3.01 ± 1.23 | 0.460** | 0.395** | 0.413** | 0.405** | 0.431** | 0.492** | 0.923** | 0.791** | 0.814** | ||||
| New possibilities | 2.95 ± 1.25 | 0.501** | 0.442** | 0.475** | 0.432** | 0.465** | 0.514** | 0.935** | 0.792** | 0.830** | 0.878** | |||
| Self‐transformation | 2.83 ± 1.21 | 0.445** | 0.384** | 0.399** | 0.385** | 0.420** | 0.478** | 0.917** | 0.787** | 0.771** | 0.833** | 0.847** | ||
| Intent to stay | 3.84 ± 0.6 | 0.689** | 0.644** | 0.629** | 0.633** | 0.659** | 0.653** | 0.434** | 0.412** | 0.473** | 0.363** | 0.397** | 0.374** | |
| Resilience | 3.13 ± 0.631 | 0.553** | 0.506** | 0.460** | 0.494** | 0.558** | 0.556** | 0.569** | 0.551** | 0.627** | 0.490** | 0.504** | 0.479** | 0.596** |
p < .05.
p < .01.
4.2. Correlation of measured variables
The correlations among resilience, post‐traumatic growth, perceived professional benefits and intent to stay are shown in Table 2. Results showed that intent to stay was positively related to resilience (r = 0.596, p < .001), post‐traumatic growth (r = 0.434, p < .001) and perceived professional benefits (r = 0.689, p < .001).
4.3. Testing the proposed model
According to the theoretical framework, we first tested the mediating effects of post‐traumatic growth and perceived professional benefits, both of which are significant (Figures 2 and 3). We then established a structural model for the relationship between resilience, post‐traumatic growth, perceived professional benefits and intent to stay among Chinese nurses to support Wuhan in managing COVID‐19. For our participants, except for the relationship of post‐traumatic growth to intent to stay, the rest of the relationships were statistically significant. We then evaluated the goodness of fit for this model; because the fitness index of the modified model was better than that of the initial model, we chose it as the final model of this study. Model graphics and goodness of fit indices of this study are shown in Figure 4 and Table 3.
FIGURE 2.
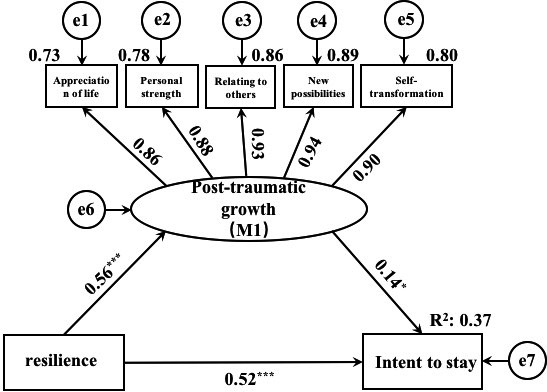
Mediating effect of post‐traumatic growth
FIGURE 3.
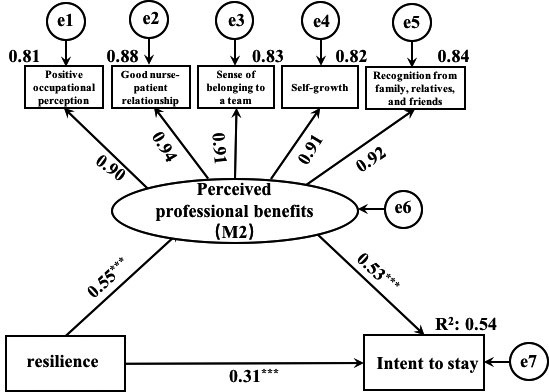
Mediating effect of perceived professional benefits
FIGURE 4.
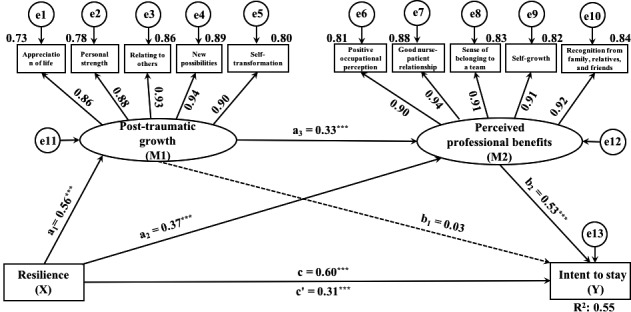
Structural equation model of intent to stay
TABLE 3.
Structural equation model fitting index
| Model | χ2/df | PMSEA | SRMR | GFI | NFI | IFI | CFI | RFI | TLI | PNFI | PCFI | PFGI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Recommended value | ≤5 | ≤0.08 | ≤0.08 | ≥0.90 | ≥0.90 | ≥0.90 | ≥0.92 | ≥0.90 | ≥0.90 | >0.50 | >0.50 | >0.50 |
| Initial model | 1.960 | 0.070 | 0.041 | 0.928 | 0.966 | 0.983 | 0.983 | 0.953 | 0.977 | 0.703 | 0.715 | 0.571 |
| Structural model | 1.927 | 0.068 | 0.041 | 0.928 | 0.966 | 0.983 | 0.983 | 0.954 | 0.977 | 0.717 | 0.730 | 0.583 |
Abbreviations: CFI, comparative fit index; GFI, goodness of fit index; IFI, incremental fit index; NFI, normed fit index; PCFI, parsimony comparative fit index; PGFI, parsimony goodness fit index; PNFI, parsimony normed fit index; RESEA, root mean square error of approximation; RFI, relative fit index; SRMR, standardized residual mean root; TLI, Tucker‐Lewis index.
4.4. Direct and indirect effects
Overall, the results of our study revealed that serial mediation had occurred, as shown in Table 4. Resilience has a direct impact on intent to stay (p < .001) after controlling for post‐traumatic growth and perceived professional benefits. Also, resilience had a total effect on intent to stay when the variables of post‐traumatic growth and perceived professional benefits were uncontrolled, which means post‐traumatic growth and perceived professional benefits mediated the effects of resilience on intent to stay. Moreover, the analysis revealed that resilience significantly influenced post‐traumatic growth (β = 0.56, p < .001) and perceived professional benefits (β = 0.37, p < .001). Post‐traumatic growth was significantly associated with perceived professional benefits (β = 0.33, p < .001). The direct effect of perceived professional benefits on intent to stay (β = 0.53, p < .001) was significant. There are two significant indirect paths. One was resilience through perceived professional benefits to intent to stay (95% CI = 0.122 to 0.273); the other was resilience affects post‐traumatic growth first, followed by perceived professional benefits and finally has an impact on intent to stay (95% CI = 0.056 to 0.154). However, the mediation effect of post‐traumatic growth between intent to stay and resilience was not significant (95% CI = −0.010 to 0.198).
TABLE 4.
Direct and indirect effects of resilience on intent to stay
| Effect | Point estimate | Boot SE | Bias‐corrected 95% CI | ||
|---|---|---|---|---|---|
| Lower | Upper | p | |||
| Indirect effect 1: X→M2→Y | 0.194 | 0.038 | 0.122 | 0.273 | <.001 |
| Indirect effect 2: X→M1→M2→Y | 0.097 | 0.025 | 0.056 | 0.154 | <.001 |
| Indirect effect 1 versus Indirect effect 2 | 0.097 | 0.053 | −0.010 | 0.198 | .075 |
| Total indirect effect of X on Y | 0.290 | 0.036 | 0.226 | 0.368 | <.001 |
| Total direct effect of X on Y | 0.306 | 0.050 | 0.207 | 0.404 | <.001 |
| Total effect | 0.596 | 0.044 | 0.495 | 0.676 | <.001 |
N = 200. Number of bootstrap samples for bias‐corrected bootstrap confidence intervals: 5,000.
X, resilience; M1, post‐traumatic growth; M2, perceived professional benefits; Y, intent to stay.
5. DISCUSSION
In this research, we explored a serial mediation model of the association between resilience, post‐traumatic growth, perceived professional benefits and intent to stay among Chinese nurses who support Wuhan in managing COVID‐19. Our study showed that the intent to stay of target nurses was 3.84, which was at a medium level. This finding is contrary to previous studies of nurses for the Middle East Respiratory Syndrome (MERS; Jung et al., 2020), which may be explained by the fact that MERS and COVID‐19 are different in mortality rate, morbidity and control challenge. Also, as each country copes in different ways, such differences may contribute to differences in intent to stay. COVID‐19 has relatively high morbidity and low mortality rates (Peeri et al., 2020). The results suggested that nurses had a medium level of intent to stay. However, the intent to stay is easily affected by external factors and may be weakened at any time (Lin et al., 2019). The long‐term intent to stay of frontline nurses treating COVID‐19 patients needs to be further explored. In addition, this study indicates that nursing managers should formulate a postepidemic recovery plan from the perspective of positive psychology and provide targeted support measures to stabilize the nursing team.
Further, post‐traumatic growth and perceived professional benefits had serial mediation effects on resilience to intent to stay. Only the separate mediation of perceived professional benefits was statistically significant among resilience and intent to stay in nurses. According to the transactional theory of stress and coping, an individual appraises a stressor that determines how he or she copes with or responds to the stressor (Lazarus, 1966). Thus, nurses' negative emotions and turnover intention caused by the experience of treating COVID‐19 patients also depend on their cognitive evaluation. This study showed that the higher the nurse's resilience, the easier it is to perceive professional benefits, which results in stronger intent to stay. Perceived professional benefits as a positive evaluation of nurses' professions, which have a significant influence on their decision to stay in the job, improve professional identity and the job psychograph, and increase their intent to stay (Xiao et al., 2016). The frontline experience of treating COVID‐19 patients has enabled nurses to perceive professional benefits, including improved nursing image, confidence, social support, financial rewards and reputation certificates (Wu et al., 2020). They had a deeper understanding of the value of the nursing profession, and this may increase their intent to stay. To increase job retention for frontline nurses under COVID‐19, improving the sense of perceived professional benefits, providing financial rewards and paid sick leave for nursing staff are effective methods (Wu et al., 2020).
Another mediation effect of post‐traumatic growth between resilience and intent to stay was not significant. Nearly half of the participants were post‐90s nurses, and 52.5% of nurses’ working experience was below ten years; thus, caring for COVID‐19 patients is a highly stressful and difficult job for nurses. This finding is consistent with that of Loft and Jensen (Loft & Jensen, 2020) which indicates that nurses may feel uneasy about career challenges, so they may consider whether or not to stay in their job. Interestingly, recent evidence has shown that employees were using the experience of post‐traumatic growth to rebuild their self‐concept and raising a sense of openness and optimism about what they can do, which may prompt them to pursue new roles and vocations (Vogel & Bolino, 2020). In summary, this study found that post‐traumatic growth may not promote the intent to stay.
Our research results supported the concept that positive resilience was sequentially linked with increased post‐traumatic growth first and then promoted perceived professional benefits, which increased intent to stay. A resilient person can respond flexibly to the challenges of life and get out of the dilemma of trauma, so is more likely to develop post‐traumatic growth (Ogińska‐Bulik & Zadworna‐Cieślak, 2018). For frontline nurses, after COVID‐19, post‐traumatic growth is a positive adaptation process through deliberate reflection and re‐evaluation of their rescue experience (Tamiolaki & Kalaitzaki, 2020). Growth after trauma can bring positive aspects and meanings to this experience and enhance their sense of professional benefits (Cui et al., 2020). The more professional benefits nurses perceive, the stronger their intrinsic motivation. As a result, these nurses see nursing as a unique profession rather than a job, because it offers immersion and development opportunities, so that they would persist in their careers (Loft & Jensen, 2020; Wu et al., 2019). What leads to growth is not the rescue experience, but how the frontline nurses interpret and respond to this experience. Therefore, hospital administrators should organize postepidemic recovery programmes to guide nurses to evaluate and adapt to their rescue experience in positive ways, and sharing lessons learned can help overcome growth barriers. Frontline nurses will find their own professional value when they receive all‐round personal growth and social support, leading to increased intent to stay.
6. LIMITATIONS
Our study is a cross‐sectional design that cannot identify the causal relationship between resilience, post‐traumatic growth, intent to stay and perceived professional benefits. Thus, longitudinal studies are needed. In addition, convenience sampling is not well representative of frontline nurses treating COVID‐19 patients in Wuhan. Also, the short time for which nurses take care of COVID‐19 patients may impact the results of this study. Furthermore, the time of data collection was for about two months after the nurses returned to their hospitals. Post‐traumatic growth usually takes a long time to develop, and the time of 2 months may not be long enough to generate post‐traumatic growth, which may have an unclear risk of bias on the results. The long‐term post‐traumatic growth of frontline nurses needs to be further explored.
7. CONCLUSION
From a positive psychology perspective, the present findings show a serial mediation model in which positive resilience sequentially increased post‐traumatic growth first and then promoted perceived professional benefits, which also enhanced the intent to stay of Chinese nurses treating COVID‐19 patients. To stabilize nursing manpower, nursing managers need to develop postepidemic recovery plans that help frontline nurses balance the pros and cons of rescue experience, and identify the benefits of the nursing profession by providing targeted education and organizational support.
CONFLICT OF INTEREST
The authors declare that no conflict of interest exists.
AUTHOR CONTRIBUTION
X.H.L conceived and designed the study; X.X.L managed the conduct of the study, with supervision by X.H.L; X.X.J analysed the data; X.X.L and X.X.J drafted the paper; all authors reviewed and contributed to finalization of the paper.
ETHICAL STATEMENTS
This study was approved by permission from the Shanghai chest hospital (No. KS2038).
ACKNOWLEDGEMENTS
We would like to thank all the nurses who participated in this study.
Liu X, Ju X, Liu X. The relationship between resilience and intent to stay among Chinese nurses to support Wuhan in managing COVID‐19: The serial mediation effect of post‐traumatic growth and perceived professional benefits. Nurs Open. 2021;8:2866–2876. 10.1002/nop2.874
Xiaoxin Liu and Xinxing Ju should be considered joint first author.
Funding information
The Gaoyuan Nursing Grant Support of Shanghai Municipal Education
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- American Psychological Association . (2012). Building your resilience. https://www.apa.org/topics/resilience
- Bentler, P. M., & Yuan, K. H. (1999). Structural equation modeling with small samples: Test statistics. Multivariate Behavioral Research, 34(2), 181–197. 10.1207/S15327906Mb340203 [DOI] [PubMed] [Google Scholar]
- Brooks, S., Amlôt, R., Rubin, G. J., & Greenberg, N. (2020). Psychological resilience and post‐traumatic growth in disaster‐exposed organisations: Overview of the literature. BMJ Military Health, 166(1), 52–56. 10.1136/jramc-2017-000876 [DOI] [PubMed] [Google Scholar]
- Brown, P., Fraser, K., Wong, C. A., Muise, M., & Cummings, G. (2013). Factors influencing intentions to stay and retention of nurse managers: A systematic review. Journal of Nursing Management, 21(3), 459–472. 10.1111/j.1365-2834.2012.01352.x [DOI] [PubMed] [Google Scholar]
- Çam, O. (2017). Nurses’ resilience and effective factors. Journal of Psychiatric Nursing, 8(2), 118–126. 10.14744/PHD.2017.75436 [DOI] [Google Scholar]
- Campbell‐Sills, L., & Stein, M. B. (2007). Psychometric analysis and refinement of the Connor‐Davidson Resilience Scale (CD‐RISC): Validation of a 10‐item measure of resilience. Journal of Traumatic Stress, 20(6), 1019–1028. 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- Chen, Q., Liang, M., Li, Y., Guo, J., Fei, D., Wang, L., He, L., Sheng, C., Cai, Y., Li, X., Wang, J., & Zhang, Z. (2020). Mental health care for medical staff in China during the COVID‐19 outbreak. Lancet Psychiatry, 7(4), e15–e16. 10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowden, T. L., & Cummings, G. G. (2012). Nursing theory and concept development: A theoretical model of clinical nurses’ intentions to stay in their current positions. Journal of Advanced Nursing, 68(7), 1646–1657. 10.1111/j.1365-2648.2011.05927.x [DOI] [PubMed] [Google Scholar]
- Cui, P. P., Wang, P. P., Wang, K., Ping, Z., Wang, P., & Chen, C. (2020). Post‐traumatic growth and influencing factors among frontline nurses fighting against COVID‐19. Occupational and Environmental Medicine, 78(2), 129–135. 10.1136/oemed-2020-106540 [DOI] [PubMed] [Google Scholar]
- Ellenbecker, C. H. (2004). A theoretical model of job retention for home health care nurses. Journal of Advanced Nursing, 47(3), 303–310. 10.1111/j.1365-2648.2004.03094.x [DOI] [PubMed] [Google Scholar]
- Government of Hubei Province, C . (2020). Transcript of the press conference on. http://www.nhc.gov.cn/xcs/s3574/202004/35b23a66a5cd4ee2a643c2719811081e.shtml
- Hu, J., & Liu, X. H. (2012). Research and thinking on nurses’ perceived professional benefits. Chinese Journal of Nursing, 47(5), 470–472. 10.3761/j.issn.0254-1769.2012.05.033 [DOI] [Google Scholar]
- Hu, J., & Liu, X. H. (2014). Qualitative research on the conceptual framework of “nurses’ perceived professional benefits”. Journal of Nurses Training, 8, 732–735. 10.3761/j.issn.0254-1769.2012.05.033 [DOI] [Google Scholar]
- Hyatt‐Burkhart, D. (2014). The experience of vicarious posttraumatic growth in mental health workers. Journal of Loss and Trauma, 19(5), 452–461. 10.1080/15325024.2013.797268 [DOI] [Google Scholar]
- Irshad, M., Khattak, S. A., Hassan, M. M., Majeed, M., & Bashir, S. (2020). How perceived threat of Covid‐19 causes turnover intention among Pakistani nurses: A moderation and mediation analysis. International Journal of Mental Health Nursing, 10.1111/inm.12775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin, L. A. H. F. S. (2019). Mediating effect of resilience between perceived professional benefits and intention to stay among nurses. Modern Nursing, 25(11), 1375–1380. 10.3760/cma.j.issn.1674-2907.2019.11.013 [DOI] [Google Scholar]
- Jung, H., Jung, S. Y., Lee, M. H., & Kim, M. S. (2020). Assessing the presence of post‐traumatic stress and turnover intention among nurses post‐middle east respiratory syndrome outbreak: The importance of supervisor support. Workplace Health and Safety, 68(7), 337–345. 10.1177/2165079919897693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong, L., Liu, Y., Li, G., Fang, Y., Kang, X., & Li, P. (2016). Resilience moderates the relationship between emotional intelligence and clinical communication ability among Chinese practice nursing students: A structural equation model analysis. Nurse Education Today, 46, 64–68. 10.1016/j.nedt.2016.08.028 [DOI] [PubMed] [Google Scholar]
- Lazarus, R. S. (1966). Psychological stress and the coping process. McGraw‐Hill. [Google Scholar]
- Li, T., Liu, T., Han, J., Zhang, M., Li, Z., Zhu, Q., & Wang, A. (2018). The relationship among resilience, rumination and posttraumatic growth in hemodialysis patients in North China. Psychology, Health and Medicine, 23(4), 442–453. 10.1080/13548506.2017.1384553 [DOI] [PubMed] [Google Scholar]
- Lin, Y. Y., Lee, Y. H., Chang, S. C., Lee, D. C., Lu, K. Y., Hung, Y. M., & Chang, Y. P. (2019). Individual resilience, intention to stay, and work frustration among postgraduate two‐year programme nurses. Collegian, 26(4), 435–440. 10.1016/j.colegn.2018.12.001 [DOI] [Google Scholar]
- Liu, Y., Yu, Y. T., Jiang, T. T., & Shi, T. Y. (2019). Correlation between perceived professional benefits, resilience and emotional intelligence of nursing students. Chinese Nursing Research, 33(22), 3858–3862. 10.12102/j.issn.1009-6493.2019.22.007 [DOI] [Google Scholar]
- Loft, M. I., & Jensen, C. S. (2020). What makes experienced nurses stay in their position? A qualitative interview study. Journal of Nursing Management, 28(6), 1305–1316. 10.1111/jonm.13082 [DOI] [PubMed] [Google Scholar]
- MacCallum, R. C., Browne, M. W., & Sugawara, H. M. (1996). Power analysis and determination of sample size for covariance structure modeling. Psychological Methods, 1(2), 130–149. 10.1037/1082-989X.1.2.130 [DOI] [Google Scholar]
- Maitlis, S. (2020). Posttraumatic growth at work. Annual Review of Organizational Psychology and Organizational Behavior, 7(1), 395–419. 10.1146/annurev-orgpsych-012119-044932 [DOI] [Google Scholar]
- Mills, J., Woods, C., Harrison, H., Chamberlain‐Salaun, J., & Spencer, B. (2017). Retention of early career registered nurses: The influence of self‐concept, practice environment and resilience in the first five years post‐graduation. Journal of Research in Nursing, 22(5), 372–385. 10.1177/1744987117709515 [DOI] [Google Scholar]
- Morgantini, L. A., Naha, U., Wang, H., Francavilla, S., Acar, Ö., Flores, J. M., Crivellaro, S. M., Moreira, D., Abern, M., Eklund, M., Vigneswaran, H. T., & Weine, S. M. (2020). Factors contributing to healthcare professional burnout during the COVID‐19 pandemic: A rapid turnaround global survey. medRxiv: the Preprint Server for Health Sciences, 2020.2005.2017.20101915. 10.1101/2020.05.17.20101915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogińska‐Bulik, N., & Zadworna‐Cieślak, M. (2018). The role of resiliency and coping strategies in occurrence of positive changes in medical rescue workers. International Emergency Nursing, 39, 40–45. 10.1016/j.ienj.2018.02.004 [DOI] [PubMed] [Google Scholar]
- Peeri, N. C., Shrestha, N., Rahman, M. S., Zaki, R., Tan, Z., Bibi, S., Baghbanzadeh, M., Aghamohammadi, N., Zhang, W., & Haque, U. (2020). The SARS, MERS and novel coronavirus (COVID‐19) epidemics, the newest and biggest global health threats: What lessons have we learned? International Journal of Epidemiology, 49(3), 717–726. 10.1093/ije/dyaa033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher, K. J., & Coffman, D. L. (2006). Computing power and minimum sample size for RMSEA. http://quantpsy.org/
- Said, R. M., & El‐Shafei, D. A. (2020). Occupational stress, job satisfaction, and intent to leave: Nurses working on front lines during COVID‐19 pandemic in Zagazig City, Egypt. Environmental Science and Pollution Research International, 28(7), 8791–8801. 10.1007/s11356-020-11235-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman, M. E. P., & Csikszentmihalyi, M. (2014). Positive psychology: An introduction. In Flow and the foundations of positive psychology: The collected works of Mihaly Csikszentmihalyi. (pp. 279–297). Springer. 10.1007/978-94-017-9088-8_18 [DOI] [Google Scholar]
- Shao, B. S., Zheng, X. Q., Zhou, X. L., & Chen, X. Y. (2019). The correlation of post‐traumatic growth and sense of coherence with perceived professional benefits among nurses in ICU. Zhejiang Medical Education, 18(6), 25–27. [Google Scholar]
- Song, L., Wang, Y., Li, Z., Yang, Y., & Li, H. (2020). Mental health and work attitudes among people resuming work during the COVID‐19 pandemic: A cross‐sectional study in China. International Journal of Environmental Research and Public Health, 17(14). 10.3390/ijerph17145059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamiolaki, A., & Kalaitzaki, A. E. (2020). “That which does not kill us, makes us stronger”: COVID‐19 and Posttraumatic Growth. Psychiatry Research, 289, 113044. 10.1016/j.psychres.2020.113044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao, H., & Wang, L. (2010). Establishment of questionnaire for nurse intention to remain employed: The Chinese version. Academic Journal of Second Military Medical University, 30(8), 925–927. 10.3724/SP.J.1008.2010.00925 [DOI] [Google Scholar]
- Tedeschi, R. G., & Calhoun, L. G. (1996). The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. 10.1007/BF02103658 [DOI] [PubMed] [Google Scholar]
- Tourangeau, A. E., & Cranley, L. A. (2006). Nurse intention to remain employed: Understanding and strengthening determinants. Journal of Advanced Nursing, 55(4), 497–509. 10.1111/j.1365-2648.2006.03934.x [DOI] [PubMed] [Google Scholar]
- Vogel, R. M., & Bolino, M. C. (2020). Recurring nightmares and silver linings: Understanding how past abusive supervision may lead to posttraumatic stress and posttraumatic growth. Academy of Management Review, 45(3), 549–569. 10.5465/amr.2017.0350 [DOI] [Google Scholar]
- Vough, H. C., & Caza, B. B. (2017). Where do I Go from here? Sensemaking and the construction of growth‐based stories in the wake of denied promotions. Academy of Management Review, 42(1), 103–128. 10.5465/amr.2013.0177 [DOI] [Google Scholar]
- Wang, J., Yao, C., Wang, Y. B., & Liu, X. H. (2011). Revision of the Posttraumatic Growth Inventory and testing its reliability and validity. Journal of Nursing Science, 26(14), 26–28. 10.3870/hlxzz.2011.14.026 [DOI] [Google Scholar]
- Wang, L., Tao, H., Ellenbecker, C. H., & Liu, X. H. (2012). Predictors of hospital nurses’ intent to stay: A cross‐sectional questionnaire survey in Shanghai. China. International Nursing Review, 59(4), 547–554. 10.1111/j.1466-7657.2012.01009.x [DOI] [PubMed] [Google Scholar]
- Wu, B., Zhao, Y., Xu, D., Wang, Y., Niu, N., Zhang, M., Zhi, X., Zhu, P., & Meng, A. (2020). Factors associated with nurses’ willingness to participate in care of patients with COVID‐19: A survey in China. Journal of Nursing Management, 28(7), 1704–1712. 10.1111/jonm.13126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, C. C., Lin, C. C., Chang, S. C., & Chou, H. L. (2019). Identifying the positive energy for retention in clinical nurses: A focus group study. Journal of Nursing Management, 27(6), 1200–1207. 10.1111/jonm.12792 [DOI] [PubMed] [Google Scholar]
- Xiao, X. L., Zhang, D. H., Xiong, L. P., & Zeng, Y. Z. (2016). A survey study of nurses’ perceived benefits and intent to stay. Chinese Nursing Management, 16(4), 468–472. 10.3969/j.issn.1672-1756.2016.04.010 [DOI] [Google Scholar]
- Xu, X., Hu, M. L., Song, Y., Lu, Z. X., Chen, Y. Q., Wu, D. X., & Xiao, T. (2016). Effect of positive psychological intervention on posttraumatic growth among primary healthcare workers in China: A preliminary prospective study. Scientific Reports, 6, 39189. 10.1038/srep39189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye, Z. J., Ruan, X. L., Zeng, Z. N., Xie, Q. B., Cheng, M. H., Peng, C. H., & Qiu, H. Z. (2016). Psychometric properties of 10‐item Connor‐Davidson resilience scale among nursing students. Journal of Nursing (China), 23(21), 9–13. 10.16460/j.issn1008-9969.2016.21.009 [DOI] [Google Scholar]
- Yu, F., Raphael, D., Mackay, L., Smith, M., & King, A. (2019). Personal and work‐related factors associated with nurse resilience: A systematic review. International Journal of Nursing Studies, 93, 129–140. 10.1016/j.ijnurstu.2019.02.014 [DOI] [PubMed] [Google Scholar]
- Yu, M., & Lee, H. (2018). Impact of resilience and job involvement on turnover intention of new graduate nurses using structural equation modeling. Japan Journal of Nursing Science, 15(4), 351–362. 10.1111/jjns.12210 [DOI] [PubMed] [Google Scholar]
- Zhang, C., Gao, R., Tai, J., Li, Y., Chen, S., Chen, L., Cao, X., Wang, L., Jia, M., & Li, F. (2019). The relationship between self‐perceived burden and posttraumatic growth among colorectal cancer patients: The mediating effects of resilience. BioMed Research International, 2019, 1–8. 10.1155/2019/6840743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, S. X., Liu, J., Afshar Jahanshahi, A., Nawaser, K., Yousefi, A., Li, J., & Sun, S. (2020). At the height of the storm: Healthcare staff’s health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID‐19. Brain, Behavior, and Immunity, 87, 144–146. 10.1016/j.bbi.2020.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


