Abstract
Coronavirus disease 2019 (COVID‐19) has hampered health care delivery globally. We evaluated the feasibility, outcomes, and safety of telehepatology in delivering quality care amid the pandemic. A telemedicine setup using smartphones by hepatologists was organized at our tertiary‐care center after pilot testing. Consecutive patients availing telehepatology services were recruited between March and July 2020. An adapted model for assessment of telemedicine was used after validity and reliability testing, to evaluate services 7‐21 days after index teleconsultation. Of the 1,419 registrations, 1,281 (90.3%) consultations were completed. From 245 randomly surveyed patients, 210 (85.7%) responded (age [years, interquartile range]: 46 [35‐56]; 32.3% females). Seventy percent of patients belonged to the middle or lower socio‐economic class, whereas 61% were from rural areas. Modes of teleconsultation were audio (54.3%) or hybrid video call (45.7%). Teleconsultation alone was deemed suitable in 88.6% of patients. Diagnosis and compliance rates were 94% and 82.4%, respectively. Patients’ convenience rate, satisfaction rate, improvement rate, success rate, and net promoter scores were 99.0%, 85.2%, 49.5%, 46.2% and 70, respectively. Physical and mental quality of life improved in 67.1% and 82.8% of patients, respectively, following index teleconsultation. Person‐hours and money spent by patients were significantly lower with teleconsultation (P < 0.001); however, person‐hours spent by hospital per teleconsultation were higher than in physical outpatient services (P < 0.001). Dissatisfied patients were more likely to have lower diagnosis rate, unsuitability for teleconsultation, noncompliance, poorer understanding, and uncomfortable conversation during teleconsultation. Connectivity issues (22.9%) were the most common barrier. Three patients, all of whom were advised emergency care during teleconsultation, succumbed to their illness. Conclusion: Telehepatology is a feasible and reasonably effective tool for rendering health care services using smartphones during the COVID‐19 pandemic. Systematic implementation, possible integration into routine health care delivery, and formal cost‐effectiveness of telehepatology services need further exploration.
Tele‐hepatology is a safe, feasible, and reasonably effective tool for rendering health‐care services using smartphones during the COVID‐19 pandemic.

Abbreviations
- CHC
chronic hepatitis C
- COVID‐19
coronavirus disease 2019
- HCC
hepatocellular carcinoma
- IQR
interquartile range
- MKS
modified Kuppuswamy scale
- NPS
net promoter score
- OPD
outpatient department
- QOL
quality of life
Chronic liver diseases affect 1.5 billion people globally and are the fourth and tenth most common ailments in males and females, respectively.( 1 ) Cirrhosis resulted in nearly 1.3 million deaths in 2017.( 1 ) Advanced cirrhosis requires multimodality care and liver transplantation as definitive treatment.( 2 ) Hepatology services are essential to provide quality care to such patients but are limited to the urban areas in most countries. There is an unmet need to deliver specialist care to all strata of patients with hepatobiliary diseases that is not restricted by distance and infrastructure.
The coronavirus disease 2019 (COVID‐19) pandemic has disrupted the health care services with maximum brunt on the outpatient department (OPD) services. Most patients with hepatobiliary diseases are either not getting treated or are being managed at local primary or secondary care centers with inadequate facilities and expertise. Technological evolution in telecommunication sector, including 4G services, can be used to provide telemedicine services to patients without any huge economic or geographic constraints. Importantly, it can avoid the spread of COVID‐19 in the community and exposure to health care workers. Moreover, telehealth services can empower physicians at primary/secondary‐care hospitals, enable telemonitoring of complex liver patients, and store‐forward health information for effective consultations.( 3 , 4 , 5 )
Telemedicine has been effective in managing patients with chronic hepatitis C (CHC) in communities using the Extension of Community Healthcare Outcomes (ECHO) model.( 3 , 6 ) We recently reported more than 90% cure rates in CHC using ECHO.( 7 ) Feasibility and efficacy of telemedicine have also been demonstrated in patients with cirrhosis,( 8 ) monitoring of liver transplant recipients,( 9 ) and other systemic diseases.( 10 , 11 , 12 , 13 , 14 , 15 , 16 )
Despite several encouraging reviews,( 5 ) objective data regarding the utility of telehepatology services remain scarce.( 4 , 17 , 18 ) Therefore, we conducted this study to evaluate the feasibility, efficacy, safety, and barriers of telehepatology services during the tempestuous COVID‐19 pandemic.
Materials and Methods
This was an observational study with analytic survey design conducted between March and July 2020 at a government‐run tertiary care teaching hospital. In the first phase, we organized telemedicine workflow in the department of hepatology followed by evaluation of telehepatology services in second phase. The protocol was approved by the institute’s ethics committee (Reference No. NK/6362/study/464) and adhered to the guidelines for reporting survey design,( 19 , 20 ) provisions of the 1975 Declaration of Helsinki, and Good Clinical Practice guidelines. All authors had access to the study data and approved the final manuscript.
Telemedicine Setup and Workflow
The liver clinic of our institute caters to nearly 50,000 outpatients from north India every year. Nearly two‐third of our patients reside in rural areas and come from more than five neighboring states (Supporting Fig. S1). With complete shutting down of OPD services and country‐wide lockdown, it was extremely important to devise a model to provide uninterrupted and adequate care to our new and follow‐up patients. Hence, in an already established telemedicine department at our institute, we incorporated our liver clinic services to provide teleconsultations. Initially, we provided telehepatology services only via audio consultations to patients who registered through two general telephone lines between 8 am and 9 am on hepatology OPD days. Considering the unlikelihood of the COVID‐19 pandemic waning in near future and encouraging feedback of initial setup (satisfaction rate, 80%), telehepatology services were expanded. Registration timing was extended from 1 hour to 2 hours (8 am to 10 am) and number of telephone lines for registrations increased to eight, which also catered to other department OPDs. Six 4G smartphones with WhatsApp (Facebook, Inc., Menlo Park, CA) and video‐calling capabilities were then procured and used specifically to provide telehepatology consultations. Hepatology teleconsultation cards, like physical OPD cards, were generated with all relevant patient particulars, including their central registration numbers, contact number, and other demographic details. Patients were called back for assessment after registration using 4G smartphones with WhatsApp by hepatologists on the same day following the country’s telemedicine guidelines.( 21 ) Further treatment plan was written on the teleconsultation cards, and a copy of the same was then sent back to patients over WhatsApp. Patients were called again to resolve any query(s). If the consulting hepatologist felt the need for inpatient care for a particular patient, they were directed to come for physical consultation or to emergency services at our institute. To maintain continuity, teleconsultation cards were catalogued with digital entry to ensure proper follow‐up of patients. Previous liver clinic files of follow‐up patients were also retrieved and attached with new teleconsultation cards. The same cards and files of the patients will be used in the future when physical OPDs open, to ameliorate any ambiguity and smooth transition back to normalcy (Fig. 1). All patient data were kept confidential, and communications were end‐to‐end encrypted and adhered to the Information Technology Act of India, 2000, and Personal Data Protection Bill, 2019, to maintain and protect patient privacy and details.
FIG. 1.
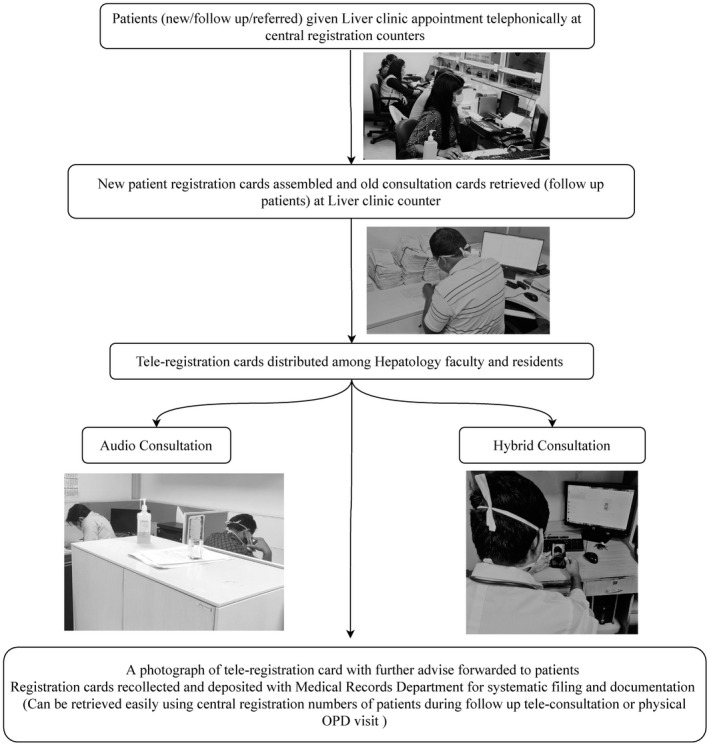
Telehepatology setup and execution.
Feasibility and Evaluation of Telehepatology Services
We first designed a suitable tool to assess the feasibility, impact, safety, and barriers of telehepatology services using an adapted model for assessment of telemedicine (MAST).( 22 ) The 34‐item tool was developed and validated for its face validity, item content validity index (I‐CVI), item impact score, and reliability (Supporting Tables S1 and S2).
Study Participants
Consecutive patients with hepatobiliary disorders aged 18 years or older, who availed telehepatology services, were enrolled prospectively after verbal and/or digital consent. Patients who did not consent or had non‐hepatobiliary ailments were excluded. The clinical details were noted by physicians during teleconsultation. A random sample of 245 patients was then selected from the whole cohort using a computer‐generated random‐number table; patients were then contacted telephonically by research fellows within 7‐21 days after the index consultation to inquire about their responses in the local language (Supporting Fig. S2). The intraperson and interperson reliability of the fellows was pretested and found to be satisfactory.
Feasibility Assessment Parameters of Telehepatology Services
Notification rate: Defined as the proportion of patients who were communicated back to their probable diagnosis and further management plan during the same teleconsultation.
Suitability rate: Defined as the proportion of patients who were deemed suitable for teleconsultation alone by the consulting physician during the index teleconsultation.
Unexpected return rate: Defined as the proportion of patients who had to register back for repeat teleconsultation before their next allotted appointment because of poor understanding or dissatisfaction or deterioration in health, needing emergent in‐patient care.
Productivity rate: Defined as a ratio of total completed teleconsultations and total person‐hours spent per tele‐OPD. This index was also calculated for physical OPD consults done before the pandemic using data from hospital records.
Patient‐Centered Outcomes and Impact Evaluation of Services
Convenience rate: Defined as the proportion of patients who found teleconsultations safer and more convenient during COVID‐19, regardless of improvement or satisfaction level.
Satisfaction rate: Patients were asked to rate their level of satisfaction on a 5‐point Likert scale from very dissatisfied to very satisfied. Somewhat satisfied and very satisfied responses were grouped as “satisfied,” and all other responses were grouped as “not satisfied” for subsequent analysis.
Improvement rate: Assessed as the proportion of patients responding “better” to the question about health issues after teleconsultation that concurred with physician assessment.
Successful teleconsultation: A composite index defined as when the patient complied with the treatment, was satisfied, and improved after the teleconsultation.
Net promoter score (NPS) ( 23 ) : Used to assess the overall satisfaction of patients and their likelihood of recommending telehepatology services to their friends/family on a scale of 0‐10 (10 being extremely likely) during the COVID‐19 pandemic. Patients with ratings of 0‐6, 7‐8, and 9‐10 were deemed as detractors, passives, and promoters, respectively. NPS was then determined by subtracting the percentage of detractors from the percentage of promoters. An NPS of ≥ 50 was considered excellent, and a score above 70 was deemed exceptional.
Clinical and Laboratory Assessment
All patients underwent a thorough clinical assessment, including history and physical examination (whenever possible) by teleconsultation, along with individualized biochemical and/or radiological evaluation. An appropriate diagnosis was made by hepatologists according to previous existing guidelines.( 2 )
Statistical Analysis
Data are presented as mean with SD or median with interquartile range (IQR) for quantitative variables and as proportions with percentages for qualitative variables as appropriate. Comparison between groups was done using chi‐square and Fisher’s exact tests for categorical variables, and Student t test and Mann‐Whitney U test for parametric and nonparametric variables, respectively. Paired t test and McNemar’s tests were done before and after teleconsultation‐related data. A P value of < 0.05 (two‐tailed) was considered significant. Statistical analysis was done using SPSS version 22.0 (SPSS Inc., Chicago, IL).
Results
Face validity and reliability (Cronbach‐alpha, 0.94; Kuder‐Richardson, 0.67) of the tool were good, with an overall I‐CVI and item‐impact score of 99.36% and 4.01, respectively (Supporting Tables S1 and S2).
Of the 1,419 registrations, 1,281 (90.3%) consultations were completed. Among the 245 randomly selected patients, 210 (85.7%) responded during the survey (median age [years, IQR]: 46 [35‐56]; 32.3% females). Most patients belonged to the upper‐lower and lower‐middle socio‐economic class, as per the modified Kuppuswamy scale (MKS)( 24 ) (Supporting Table S3), and 61% were from rural background. Seventy‐three (34.3%) patients had one or more comorbidities apart from hepatobiliary disease. Diabetes (n = 25, 11.9%), hypertension (n = 23, 10.9%), and chronic kidney disease (10, 4.8%) were the most frequent comorbidities. Cirrhosis (n = 78, 37.1%) was the most frequent diagnosis, followed by chronic viral hepatitis (n = 68, 32.4%). Twenty‐four (11.4%) patients with cirrhosis had concomitant hepatocellular carcinoma (HCC), whereas 64 (82.1%) had one or more decompensations.( 2 ) One‐hundred and nine (51.9%) patients were follow‐ups, whereas 101 (48.1%) consulted for the first time. The mode of teleconsultation was audio and hybrid (both audio and video) in 114 (54.3%) and 96 (45.7%) patients, respectively. Health care workers (n = 108, 51.4%) and patient relatives (n = 51, 24.3%) were the common sources of referral for teleconsultations (Table 1).
TABLE 1.
Baseline Demographic Parameters, Feasibility, Patient‐Centered Outcomes, and Impact of Telehepatology Services
| Parameter | All Surveyed Patients (n = 210) | Satisfied (n = 179) | Unsatisfied (n = 31) | P Value* |
|---|---|---|---|---|
| Age (years) | 46 (35‐56) | 46 (35‐56) | 46 (35‐50) | 0.751 |
| Male : female | 142:68 | 119:60 | 23:08 | 0.397 |
| Socioeconomic status (MKS) | ||||
| Upper class | 3 (1.4) | 2 (1.1) | 1 (3.2) | 0.597 |
| Upper middle class | 56 (26.7) | 50 (27.9) | 6 (19.4) | |
| Lower middle class | 75 (35.7) | 64 (35.8) | 11 (35.5) | |
| Upper lower class | 76 (36.2) | 63 (35.2) | 13 (41.9) | |
| Lower class | 0 | 0 | 0 | |
| Population (rural : urban) | 128:82 | 106:73 | 22:09 | 0.216 |
| Comorbidities present | 73 (34.8) | 59 (32.9) | 14 (45.2) | 0.467 |
| Diagnosis | ||||
| Cirrhosis | 78 (37.1) | 66 (36.9) | 12 (38.7) | |
| Compensated cirrhosis | 14 (17.9) | 13 (19.7) | 1 (8.30 | |
| Decompensated cirrhosis | 64 (82.1) | 53 (80.3) | 11 (91.7) | 0.787 |
| Cirrhosis with HCC | 24 (11.4) | 19 (10.6) | 5 (16.1) | |
| Chronic viral hepatitis | 68 (32.4) | 60 (33.5) | 8 (25.8) | |
| NAFLD | 16 (7.6) | 14 (7.8) | 2 (6.5) | |
| ALD | 4 (1.9) | 4 (2.2) | 0 (0.0) | |
| NCPH | 4 (1.9) | 3 (1.7) | 1 (3.2) | |
| Acute hepatitis | 10 (4.8) | 9 (5.0) | 1 (3.2) | |
| EHBO | 11(5.3) | 9 (5.0) | 2 (6.5) | |
| Others | 19 (9.0) | 14 (7.8) | 5 (16.1) | |
| Hepatology consultation | ||||
| First time | 101 (48.1) | 87 (48.4) | 14 (45.2) | 0.783 |
| Follow‐up | 109 (51.9) | 92 (51.4) | 17 (54.8) | |
| Mode of communication | ||||
| Audio call | 114 (54.3) | 99 (55.3) | 15 (48.4) | 0.559 |
| Hybrid (audio and video) call | 96 (45.7) | 80 (44.7) | 16 (51.6) | |
| Source of information for teleconsultation | ||||
| Health care worker | ||||
| Relatives/friends | 108 (51.4) | 90 (50.3) | 18 (58.1) | 0.679 |
| Internet | 51 (24.3) | 46 (25.7) | 5 (16.1) | |
| Newspaper | 27 (12.9) | 22 (12.3) | 5(16.1) | |
| 24 (11.4) | 21 (11.7) | 3 (9.7) | ||
| Notification rate | 205 (97.6) | 176 (98.3) | 29 (93.5) | 0.759 |
| Compliance to treatment | 173 (82.4) | 151 (84.4) | 22 (71.1) | 0.071 |
| Suitability rate | 173 (82.4) | 163 (91.1) | 23 (74.2) | 0.006 |
| Unexpected return rate | 41 (19.6) | 14 (7.8) | 27 (87.1) | <0.001 |
| Patient preference during COVID‐19 | ||||
| Telemedicine | 176 (83.8) | 153 (85.5) | 23 (74.2) | 0.115 |
| Physical OPD | 34 (16.2) | 26 (14.5) | 8 (25.8) | |
| Patient preference if no COVID‐19 | ||||
| Telemedicine | 56 (26.7) | 54 (30.2) | 2 (6.5) | |
| Physical OPD | 133 (63.3) | 107 (59.8) | 26 (83.9) | 0.018 |
| Both | 21 (10) | 18 (10.1) | 3(9.7) | |
| Patient comfort level | ||||
| Very uncomfortable | 12 (5.7) | 0 (0.0 | 12 (38.7) | |
| Somewhat uncomfortable | 2 (0.9) | 0 (0.0) | 2 (6.5) | <0.001 |
| Neither | 18 (8.6) | 6 (3.4) | 12 (38.7) | |
| Somewhat comfortable | 49 (23.3) | 46 (25.7) | 3 (9.7) | |
| Very comfortable | 129 (61.4) | 127 (70.9) | 2 (6.5) | |
| Acceptability/satisfaction rate | ||||
| Very dissatisfied | 13 (6.2) | 0 (0.0) | 13 (41.9) | |
| Somewhat dissatisfied | 1 (0.5) | 0 (0.0) | 1 (3.2) | |
| Neither | 17 (8.1) | 0 (0.0) | 17 (54.8) | <0.001 |
| Somewhat satisfied | 52 (24.8) | 52 (29.1) | 0 (0.0) | |
| Very satisfied | 127 (60.5) | 127 (70.9) | 0 (0.0) | |
| Level of understanding | ||||
| Very poor | 8 (3.8) | 0 (0.0) | 8 (25.8) | |
| Somewhat poor | 1 (0.5) | 0 (0.0) | 1 (3.2) | |
| Neither | 24 (11.4) | 7 (3.9) | 17 (54.8) | <0.001 |
| Somewhat good | 41 (19.5) | 38 (21.2) | 3 (9.7) | |
| Very good | 139 (66.2) | 134 (74.9) | 2 (6.5) | |
| Improvement rate | 104 (49.5) | 97 (54.2) | 7 (22.6) | 0.001 |
| Diagnosis rate | 197 (94.0) | 170 (95.0) | 27 (87.1) | 0.093 |
| Success rate | 97 (46.2) | 97 (54.2) | 0 (0.0) | <0.001 |
| QOL improvement | ||||
| Physical | 141 (67.1%) | 125 (69.8) | 16 (51.6) | 0.046 |
| Mental | 174 (82.8%) | 168 (93.9) | 6 (19.4) | <0.001 |
Data are presented as median (IQR), n (%).
*P < 0.05 was regarded as significant.
Abbreviations: ALD, alcohol‐associated liver disease; EHBO, extrahepatic biliary obstruction; NAFLD, nonalcoholic fatty liver disease; NCPH, noncirrhotic portal hypertension.
On feasibility analysis, among the 210 responders, 205 were notified of their diagnosis and treatment (notification rate: 97.6%). A total of 186 (88.6%) consultations were deemed suitable with teleconsultation alone; however, there was an unexpected return rate of 19.6%. The productivity rate with teleconsultation and physical OPD was compared. Total person‐hours used and patients attended per day were noted in tele‐OPD prospectively and in physical OPD by retrospective record review. The mean (SD) person‐hours used per OPD was significantly higher in physical OPD as compared with tele‐OPD (165 [12] vs. 30 [8]; P < 0.001); however, the productivity rate of physical OPD was higher as compared with tele‐OPD (3.3 [0.5] vs. 2.7 [0.4]; P = 0.008). The time spent (in minutes) per consult was more in teleconsultation than physical OPD (22.2 [4.9] vs. 18.0 [4.0]; P < 0.001) (Table 2).
TABLE 2.
Productivity of Health Care Facility and Patient Expenditure (Time and Money) in Teleconsultation and Physical Consultation
| Parameter | Teleconsultation (n = 1,281) | Physical Consultation (n = 4,500) |
|---|---|---|
| Productivity rate (average consults per person‐hour used by hospital) | 2.7 (0.4) | 3.3 (0.5) |
| Total (mean [SD]) person‐hours spent by hospital per consultation* | 30.0 (8.0) | 165.0 (12.0) |
| Mean (SD) person‐hours spent by hospital per patient per consultation | 0.37 (0.08) | 0.30 (0.06) |
| Mean (SD) person‐hours spent by patients/family per consultation* | 1.4 (0.15) | 12.0 (4.0) |
| Mean (SD) expenditure (INR) by patients/family per consultation* | 1.00 (0.25) | 700.00 (500.00) |
*P < 0.05.
Abbreviation: INR, Indian National Rupee.
Patients were likely to recommend telehepatology services to their near ones in the prevailing situation with an NPS of 70%. Overall, 208 (99.0%) and 178 (84.8%) of patients reported teleconsultation as convenient and comfortable, respectively. During the pandemic, 176 (83.8%) preferred teleconsultations, whereas 133 (63.3%) would prefer physical OPD after the pandemic.
Overall, 179 (85.2%) patients were satisfied with the teleconsultation, and 104 (49.5%) patients reported improvement in their overall health. Diagnosis was achieved in 197 (94%) patients, and 173 (82.4%) patients complied with the treatment with an overall success rate of 46.2%. Physical and mental quality of life (QOL) improved in 141 (67.1%) and 174 (82.8%) patients, respectively. The mean (SD) person‐hours and money spent (in Indian National Rupee) by patient for consultation were less with teleconsultation than physical OPD (1.4 [0.15] vs. 12 [4.0]; P < 0.001) and (1 [0.25] vs. 700 [500]; P < 0.001), respectively (Table 2).
The demographic characteristics were not different between the satisfied/unsatisfied (Table 1) and improved/not improved groups (Table 3). Suitability for teleconsultation, acceptability rate, preference to teleconsultation in the post‐COVID period, comfortable conversation during teleconsult, success rate, improvement rate, level of understanding, compliance to treatment, and improvement in physical and mental QOL were significantly higher in the satisfied group as compared with the unsatisfied group after teleconsultation. Although a higher number of patients in the satisfied group preferred teleconsultation at present, most of them (n = 107, 59.8%) would prefer physical OPD after the COVID‐19 pandemic (Table 1).
TABLE 3.
Baseline Demographic Parameters, Feasibility, Patient‐Centered Outcomes, and Impact of Telehepatology Services Among the Improved and Non‐improved Groups
| Parameter | Improved (n = 104) | Non‐improved (n = 106) | P Value* |
|---|---|---|---|
| Age (years) | 46.5 (35.2‐50) | 45.5 (35‐55) | 0.698 |
| Male : female | 70:34 | 72:34 | 0.924 |
| Socioeconomic status (MKS) | |||
| Upper class | 1 (1) | 2 (1.9) | |
| Upper middle class | 30 (28.8) | 26 (24.5) | 0.844 |
| Lower middle class | 37 (35.6) | 38 (35.8) | |
| Upper lower class | 36 (34.6) | 40 (37.7) | |
| Lower class | 0 | 0 | |
| Population (rural : urban) | 65:39 | 63:43 | 0.649 |
| Comorbidity present | 27 (26) | 30 (28.3) | 0.703 |
| Diagnosis | |||
| Cirrhosis | 41 (39.4) | 37 (34.9) | |
| Compensated cirrhosis | 7 (17.1) | 7 (18.9) | |
| Decompensated Cirrhosis | 34 (82.9) | 30 (81.1) | |
| Cirrhosis with HCC | 10 (9.6) | 14 (13.2) | |
| Chronic viral hepatitis | 33 (31.7) | 35 (33) | 0.205 |
| NAFLD | 9 (8.7) | 7 (6.6) | |
| ALD | 4 (3.8) | 0 | |
| NCPH | 1 (1) | 3 (2.8) | |
| Acute hepatitis | 6 (5.8) | 4 (3.8) | |
| EHBO | 4 (3.8) | 7 (6.6) | |
| Others | 6 (5.8) | 13 (12.3) | |
| Hepatology consultation | |||
| First time | 45 (43.3) | 56 (52.8) | 0.166 |
| Follow‐up | 59 (57.7) | 50 (48.2) | |
| Mode of communication | |||
| Audio call | 57 (54.8) | 57 (53.8) | 0.88 |
| Hybrid (audio and video) call | 47 (45.2) | 49 (46.2) | |
| Source of information for teleconsultation | |||
| Health care worker | 52 (50) | 56 (52.8) | |
| Relatives/friends | 29 (27.9) | 22 (20.8) | 0.75 |
| Internet | 13 (12.5) | 14 (13.2) | |
| Newspaper | 10 (9.6) | 14 (13.2) | |
| Compliance to treatment | 104 (100) | 69 (65.1) | <0.001 |
| Suitability rate | 94 (90.4) | 92 (86.8) | 0.413 |
| Confidence rate | 91 (87.5) | 85 (80.2) | 0.15 |
| Patient preference if no COVID | |||
| Telemedicine | 34 (32.7) | 22 (20.8) | |
| Physical OPD | 58 (55.8) | 75 (70.8) | 0.076 |
| Both | 12 (11.5) | 9 (8.5) | |
| Patient comfort level | |||
| Very uncomfortable | 0 | 12 (11.3) | |
| Somewhat uncomfortable | 1 (1) | 1 (0.9) | <0.001 |
| Neither | 8 (7.7) | 10 (9.4) | |
| Somewhat comfortable | 17(16.3) | 32(30.2) | |
| Very comfortable | 78 (75) | 51 (48.1) | |
| Acceptability/satisfaction rate | |||
| Very dissatisfied | 0 (0.0) | 13 (12.3) | |
| Somewhat dissatisfied | 0 (0.0) | 1 (0.9) | |
| Neither | 7 (6.7) | 10 (9.4) | <0.001 |
| Somewhat satisfied | 21 (20) | 31 (29.2) | |
| Very satisfied | 76 (73.1) | 51 (41.8) | |
| Level of understanding | |||
| Very poor | 0 (0.0) | 8 (7.5) | |
| Somewhat poor | 1 (1.0) | 0 (0.0) | |
| Neither | 8 (7.7) | 16 (15.1) | 0.006 |
| Somewhat good | 18 (17.3) | 23 (21.7) | |
| Very good | 77 (74.0) | 59 (55.7) | |
| Satisfaction rate | 97 (93.3) | 82 (77.4) | 0.002 |
| Diagnosis rate | 98 (94.2) | 99 (93.4) | 0.81 |
| Success rate | 97 (93.3) | 0 (0.0) | <0.001 |
| QOL improvement | |||
| Physical | 104 (100) | 37 (34.9) | <0.001 |
| Mental | 94 (90.4) | 80 (75.5) | 0.004 |
Data are presented as median (IQR), n (%).
*P < 0.05 was regarded as significant.
Abbreviations: ALD, alcohol‐associated liver disease; EHBO, extrahepatic biliary obstruction; NAFLD: nonalcoholic fatty liver disease; NCPH, noncirrhotic portal hypertension.
On analyzing improved and not‐improved subgroups, compliance rate was significantly higher in the improved group. Lower level of satisfaction, an uncomfortable conversation during teleconsult, poor level of understanding, and non‐improvement in physical and mental QOL were significantly higher in the not‐improved group as compared with the improved group after the teleconsult. Suitability rate, confidence rate, and diagnosis were not different, with a trend to prefer physical OPD among the not‐improved patients (Table 3).
Thirty‐two patients were hospitalized, and 3 patients died during follow‐up. All 3 patients who died were considered unsuitable for teleconsultation alone and had been advised emergency care. Patient and physician‐reported barriers to teleconsultation are shown in Supporting Fig. S3. Among the 58 patients who suggested measures to improve patient care via teleconsultation, 34 (58.6%) asked for an increase in registration time, 12 (20.7%) desired re‐opening of physical OPDs, 9 (15.5%) wanted more consultation time per patient, and 3 (5.2%) requested better scheduling with respect to the call‐back time.
Discussion
The potential of telehepatology has remained underutilized due to concerns regarding patient safety, overall acceptance, connectivity, unclear reimbursement policies, and legislative restrictions.( 4 , 11 ) There has been a rapid improvisation and extension of the 4G network globally with dramatic cost reduction. More than 80% of our country’s population now use 4G smartphones.( 25 ) Our study showed that telehepatology is feasible using 4G smartphones with a limited setup without exposing health care staff to the deadly virus. Institutes with pre‐existing telemedicine facilities may not need extensive and costly infrastructure to initiate telehepatology services, and other institutes may extend this model with improvisation, minimal training of health care professionals, and patient education.( 26 )
The tool used in the study was adapted using the MAST model( 22 ) and tested for validity and reliability in our setting. Teleconsultation was found to be feasible with excellent completion and notification rates (>90%). Most patients belonged to lower and middle socio‐economic strata and rural locations. Even the poor and relatively illiterate patients adopting telehepatology as a mode of first consultation appears reassuring and alleviates, to some extent, the concerns regarding potential telemedicine barriers like digital literacy, availability, and affordability of telecommunication services.( 27 ) Partner acceptability was also good, as health care workers and patient relatives, apart from internet and print media, were the major source of information for telemedicine services to the general population.
We achieved a satisfaction rate of 85% and an overall success rate of 46%. Less than 50% success rate in our study can be attributed to a low improvement rate (49.5%). Although satisfaction rate and improvement rate did not differ significantly among the various underlying etiologies, there was a trend toward poorer improvement rate in patients with cirrhosis (52.1%), HCC (58.3%), and chronic viral hepatitis (51.4%). The primary reason for this trend in patients with chronic viral hepatitis was a delay in the initiation of antiviral medications due to the nonavailability of required investigations at index teleconsult. Apart from the nature of underlying disease, discordance between satisfaction and improvement rate can also be explained by the timing of the survey following index teleconsultation. Response to treatment such as mobilization of ascites, improvement in jaundice, pruritis, and appetite may take more than 4 weeks. We believe a repeat survey after a longer period and more teleconsults may show higher improvement and success rate.
Treating physicians deemed 88% patients suitable for tele‐evaluation alone; unfortunately, nearly 20% made an unscheduled appointment due to improper understanding or persistence or worsening of symptoms. The fluctuating nature of decompensated cirrhosis may have led to such unexpected returns. A significantly greater proportion of patients with decompensated cirrhosis, HCC, and biliary obstruction were deemed unsuitable for teleconsultation alone, given the need for detailed examination, imaging evaluation, and possible invasive procedure (Supporting Table S4). Previously, Serper et al.( 18 ) reported a 94% scheduling rate with 85% video consultations in their pilot telehepatology services before COVID‐19, and suggested good feasibility and exceptional NPS of 94%. There can be two reasons for a relatively lower, although an excellent, NPS of 70% in our study. First, more than half of their patients( 18 ) were referred for a second opinion with prior personal evaluation at the referring center. Second, availability of a medical assistant to explain to patients about their disease and management plan at the referring institutes would definitely have led to better understanding. However, our study was done in the sudden aftermath of the COVID‐19 pandemic, and half of the patients were not seen at any hospital physically and did not have immediate availability of a medical assistant. Despite these shortcomings, 99% and 84.8% of our patients found telehepatology to be convenient and comfortable, respectively, with good confidence rate (83.8%), diagnosis rate (94%), and acceptable understanding (85.7%). Similar high satisfaction rates with telehealth services during the COVID‐19 pandemic were reported by both patients and gastroenterologists in a recent e‐mail‐based online satisfaction survey of 1,492 patients( 28 ); however, only 66 (4.4%) of patients had primary hepatobiliary ailments, and the questionnaire was quite restricted.
Teleconsultation led to an improvement in physical QOL in nearly two‐thirds of patients, with an even higher rate (82.8%) of mental QOL improvement. Undoubtedly, objective improvement is an important surrogate in assessing patient progress, as the reassuring effect of a doctor’s consult on patient mental health is underrepresented and is a significant contributor to patient’s overall well‐being, especially during such difficult times. Feasibility, acceptability, and cost‐effectiveness of telemedicine have also been previously demonstrated in teleneurology,( 15 , 29 ) diabetes management,( 13 ) teleradiology,( 16 ) and telepsychiatry,( 12 ) apart from patients with CHC,( 6 , 7 ) cirrhosis,( 4 , 30 ) and liver transplant recipients.( 9 )
The total mean (SD) person‐hours spent per teleconsultation OPD were significantly lower. However, time spent per patient was higher with teleconsultation (22.2 vs. 18 minutes), which accounted for a higher productivity rate of physical OPD. A much higher number of patients (552) was seen in our liver clinic during 2019, as compared with 128 patients per tele‐OPD now, and needed significantly more doctors, nurses, and support staff simultaneously. Not surprisingly, time taken per patient was lower in physical OPD because of more effective face‐to‐face communication, judicious use of clinical acumen, and better building of the doctor–patient relationship. As per the patient’s perspective, teleconsultation was more economical with respect to both time and money spent due to the savings on travel and accommodation.
We found that satisfied patients were more likely to be comfortable with teleconsultation and compliant to treatment with a better understanding of the information given. They were also more likely to report improvement in overall health, physical QOL, and mental QOL. Satisfied patients were also adjudged more suitable for teleconsultation alone, suggesting that a subset of patients who may not be satisfied with teleconsultation can be identified at index consultation and remedial steps can be taken. A similar assessment among the improved and non‐improved groups showed that compliance and comfortability rates were significantly higher among the improved patients. Non‐improved patients reported poorer understanding, lower satisfaction rate, and lesser improvement in both physical and mental QOL. Interestingly, diagnosis rate and suitability rate were not significantly different between the two groups.
It was surprising to note that despite high convenience and satisfaction rates with teleconsultation, most patients preferred in‐person visits after the pandemic. On evaluation, there was a trend toward preference for physical visits among patients with HCC, patients requiring interventions, and those uncomfortable during teleconsults. Furthermore, this may be looked upon as a sudden cultural change during the COVID‐19 pandemic, during which patients had none or few choices but to opt for telemedicine for their care. We believe with the evolution of telemedicine in our country, the patient preferences would change, and a hybrid consultation will gain more acceptance and preference from both patients and physicians.
Connectivity, data exchange, and language issues, the potential conventional barriers to teleconsultation,( 27 ) were reported by less than 10% patients, whereas more than 70% did not report barriers. Reimbursement, one of the main limiting factors for telemedicine in the Western and European countries, was considered an impediment by less than 1% of our patients, likely due to the free cost government health services in our country and posttreatment reimbursement by local state governments. The primary connectivity issue faced by patients was the inability to register, sometimes due to busy telephone lines because of a relatively narrow time period of 2 hours for registration. This can be improved by increasing the number of telephone lines and registration time, increasing the number of OPD days per week, and staggering the registration time for different specialties. These measures have been subsequently implemented in our setup in a phased manner, with improvement in these barriers.
The strengths of this study include the illustration of a simple and feasible telemedicine model, to continue care of hepatobiliary diseases during the COVID‐19 pandemic. This model can be extrapolated to provide care for other illnesses too. The tool used to assess the utility of telehepatology services was comprehensive, valid, and reliable. The patient’s convenience, confidence, and satisfaction without major safety concerns for this model was motivating. Limitations of the study include relative immaturity of telehepatology setup, which may have led to some inaccurate assessment of parameters like level of understanding, connectivity rate, improvement rate, and success rate. There was a lack of data for patient‐centered outcomes, safety, and success rates from physical OPD consults.
In the future, we must explore the utility of stratifying patients suitable for telemedicine during physical OPD visits. Telemedicine can be used to triage patients referred to hepatology services at the outset. Some subsets of patients like those with inactive chronic hepatitis B, treated CHC, and simple steatosis may be seen in physical OPD initially and then put on telehepatology follow‐up after discussion with the patient. Such hybrid of telehepatology in combination with physical consultation beyond this pandemic may reduce appointment times for patients requiring immediate attention, prevent overcrowding in PDS (especially in resource‐limited countries), and also reduce costs to both patients and health care facilities. Nonetheless, patients with cirrhosis and its complications will still need physical OPD assessment. Telemedicine may be used to empower medical physicians to provide follow‐up care to such patients in the community and remote areas. The physician‐reported barriers need further exploration in telehepatology. Telemedicine appears to be a wild stallion raring to go, and its integration into routine health care services after the COVID‐19 pandemic is over may be one of the silver linings in an otherwise dismal 2020. Further experience and refining of protocols with government approval may help us realize the true potential of telehepatology beyond the pandemic.
In conclusion, in this study we found that telehepatology was a feasible, acceptable, and reasonably effective tool to provide quality care to patients with hepatobiliary diseases during the COVID‐19 pandemic. Telehepatology has the potential to bridge the rural–urban divide of superspecialist hepatology services. It saved patients’ time and money and avoided exposure of health care professionals to COVID‐19. The impact of telehepatology services on patients’ mental QOL and satisfaction level was remarkable. Systematic implementation and formal cost‐effectiveness of telemedicine should be explored further in hepatology services beyond the COVID‐19 pandemic.
Supporting information
Supplementary Material
Acknowledgment
The authors acknowledge the services of Mr. Shiv and Mr. Sunny in arranging and digital entry of teleconsultation cards for the smooth functioning of telehepatology services.
Potential conflict of interest: Nothing to report.
References
- 1. James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1789‐1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Angeli P, Bernardi M, Villanueva C, Francoz C, Mookerjee RP, Trebicka J, et al. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol 2018;69:406‐460. [DOI] [PubMed] [Google Scholar]
- 3. Kirsh S, Su GL, Sales A, Jain R. Access to outpatient specialty care: solutions from an integrated health care system. Am J Med Qual 2015;30:88‐90. [DOI] [PubMed] [Google Scholar]
- 4. Serper M, Volk ML. Current and future applications of telemedicine to optimize the delivery of care in chronic liver disease. Clin Gastroenterol Hepatol 2018;16:157‐161.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Piao C, Terrault NA, Sarkar S. Telemedicine: an evolving field in hepatology. Hepatol Commun 2019;3:716‐721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arora S, Kalishman S, Thornton K, Dion D, Murata G, Deming P, et al. Expanding access to hepatitis C virus treatment—Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology 2010;52:1124‐1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dhiman RK, Grover GS, Premkumar M, Taneja S, Duseja A, Arora S, et al. Decentralized care with generic direct‐acting antivirals in the management of chronic hepatitis C in a public health care setting. J Hepatol 2019;71:1076‐1085. [DOI] [PubMed] [Google Scholar]
- 8. Mauro E, Marciano S, Torres MC, Roca JD, Novillo AL, Gadano A. Telemedicine improves access to hepatology consultation with high patient satisfaction. J Clin Exp Hepatol 2020;10:555‐562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ertel AE, Kaiser TE, Abbott DE, Shah SA. Use of video‐based education and tele‐health home monitoring after liver transplantation: results of a novel pilot study. In: Surgery (United States). St. Louis, MO: Mosby, Inc.; 2016:869‐876. [DOI] [PubMed] [Google Scholar]
- 10. Der‐Martirosian C, Griffin AR, Chu K, Dobalian A. Telehealth at the US department of Veterans Affairs after Hurricane Sandy. J Telemed Telecare 2019;25:310‐317. [DOI] [PubMed] [Google Scholar]
- 11. Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Informatics 2010;79:736‐771. [DOI] [PubMed] [Google Scholar]
- 12. Olthuis JV, Watt MC, Bailey K, Hayden JA, Stewart SH. Therapist‐supported Internet cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database Syst Rev 2015;3:CD011565. [DOI] [PubMed] [Google Scholar]
- 13. Kesavadev J, Shankar A, Pillai PBS, Krishnan G, Jothydev S. Cost‐effective use of telemedicine and self‐monitoring of blood glucose via Diabetes Tele Management System (DTMS) to achieve target glycosylated hemoglobin values without serious symptomatic hypoglycemia in 1,000 subjects with type 2 diabetes mellitus—a retrospective study. Diabetes Technol Ther 2012;14:772‐776. [DOI] [PubMed] [Google Scholar]
- 14. Caffery LJ, Farjian M, Smith AC. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: a scoping review. J Telemed Telecare 2016;22:504‐512. [DOI] [PubMed] [Google Scholar]
- 15. Müller KI, Alstadhaug KB, Bekkelund SI. Acceptability, feasibility, and cost of telemedicine for nonacute headaches: a randomized study comparing video and traditional consultations. J Med Internet Res 2016;18:e140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kalyanpur A, Neklesa VP, Pham DT, Forman HP, Stein ST, Brink JA. Implementation of an international teleradiology staffing model. Radiology 2004;232:415‐419. [DOI] [PubMed] [Google Scholar]
- 17. Currell R, Urquhart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Nurs Times 2001;97:35. [PubMed] [Google Scholar]
- 18. Serper M, Cubell AW, Deleener ME, Casher TK, Rosenberg DJ, Whitebloom D, et al. Telemedicine in liver disease and beyond: can the COVID‐19 crisis lead to action? Hepatology 2020;72:723‐728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Burns KE, Duffett M, Kho ME, Meade MO, Adhikari NK, Sinuff T, et al. A guide for the design and conduct of self‐administered surveys of clinicians. CMAJ 2008;179:245‐252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zamanzadeh V, Ghahramanian A, Rassouli M, Abbaszadeh A, Alavi‐Majd H, Nikanfar A‐R. Design and implementation content validity study: development of an instrument for measuring patient‐centered communication. J Caring Sci 2015;4:165‐178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Telemedicine Practice Guidelines . https://www.mohfw.gov.in/pdf/Telemedicine.pdf. Accessed August 2020.
- 22. Kidholm K, Ekeland AG, Jensen LK, Rasmussen J, Pedersen CD, Bowes A, et al. A model for assessment of telemedicine applications: MAST. Int J Technol Assess Health Care 2012;28:44‐51. [DOI] [PubMed] [Google Scholar]
- 23. Net Promoter Score | Medallia . https://www.medallia.com/net‐promoter‐score/. Accessed August 2020.
- 24. Mohd SS. Modified Kuppuswamy socioeconomic scale updated for the year 2019. Indian J Forensic Community Med 2019;6:1‐3. [Google Scholar]
- 25. Annual Report | Department of Telecommunications | Ministry of Communication | Government of India . https://dot.gov.in/reports‐statistic/2471. Accessed January 2021.
- 26. Schulz T, Long K, Kanhutu K, Bayrak I, Johnson D, Fazio T. Telehealth during the coronavirus disease 2019 pandemic: rapid expansion of telehealth outpatient use during a pandemic is possible if the programme is previously established. J Telemed Telecare 2020;1357633X2094204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare 2018;24:4‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dobrusin A, Hawa F, Gladshteyn M, Corsello P, Harlen K, Walsh CX, et al. Gastroenterologists and patients report high satisfaction rates with telehealth services during the novel coronavirus 2019 pandemic. Clin Gastroenterol Hepatol 2020;18:2393‐2397.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wechsler LR. Advantages and limitations of teleneurology. JAMA Neurol 2015;72:349‐354. [DOI] [PubMed] [Google Scholar]
- 30. Thomson M, Volk M, Kim HM, Piette JD. An automated telephone monitoring system to identify patients with cirrhosis at risk of re‐hospitalization. Dig Dis Sci 2015;60:3563‐3569. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


