Abstract
As the coronavirus disease 2019 (COVID‐19) pandemic forced universities to switch to distance online education, there was an urgent need to find some virtual/digital alternatives in order to continue teaching. Opportunities such as watching pre‐recorded autopsy videos or creating and analyzing post‐mortem computed tomography or magnetic resonance imaging with various 3D surface imaging techniques are usually time‐consuming and cost‐intensive. Photogrammetry, which allows the creation of 3D textured surface models from a series of overlapping photographs taken from varying viewpoints, is a less common approach compared with post‐mortem imaging. We created 3D autopsy case models for a special online forensic pathology course in which students could try the models. Then, formal feedback was requested regarding the possible application of this method in education. Most of the students were satisfied with the new method and ranked photogrammetry higher than the other available methods. Our results indicate that photogrammetry has a high potential in undergraduate education, especially in the case of distance education or in those countries where declining autopsy rates have resulted in a decline in the use of the autopsy as an educational tool. Photogrammetry can also be used as a supplementary tool in traditional autopsy‐based education and has potential applications in various fields of medical education.
Keywords: autopsy, COVID‐19, 3D documentation, forensic pathology, medical school education, photogrammetry
Highlights.
Documentation by photogrammetry is easy, fast, and compatible with the routine autopsy algorithm.
Photogrammetry does not need special equipment; even a mid‐range smartphone camera can produce suitable results.
3D models produced by photogrammetry are useful for autopsy and forensic pathology education.
Photogrammetry has high educational potential for medical students and medical education.
1. INTRODUCTION
On January 30, 2020, following the recommendations of the Emergency Committee, the World Health Organization (WHO) declared the 2019 novel coronavirus outbreak a global public health emergency [1]. Apart from the many medical, social, and economic effects to deal with after the outbreak of the virus, the coronavirus disease 2019 (COVID‐19) pandemic forced universities to switch to online distance education, as classical contact education with medical students was impossible. Educators had to quickly adapt to an unpredictable duration of social distancing, and there was an urgent need to identify virtual/digital alternatives to in‐person teaching.
The use of digital imaging in medical education has increased in recent years, becoming popular and commonly accepted [2], especially in the case of basic medical subjects such as human anatomy [3]. In the case of pre‐clinical or clinical subjects, it is more challenging to create quality online education providing useful knowledge and practical skills. During the traditional Hungarian forensic pathology curriculum, theoretical lectures/seminars are usually combined with a relatively high number of autopsy demonstrations, where students are present and observing an autopsy being performed, with explanation by the performing forensic pathologist. The COVID‐19 era has made it necessary for us to replace conventional autopsy instruction with alternatives. Opportunities such as watching pre‐recorded autopsy videos [4, 5, 6] or creating and analyzing post‐mortem computed tomography (CT) or magnetic resonance (MR) imaging with various 3D surface imaging techniques are usually time‐consuming, cost‐intensive [7] and require extensive training to obtain acceptable results [8].
Photogrammetry is a technology that allows the creation of 3D textured surface models from a series of overlapping photographs taken from varying viewpoints [9]. Every aspect of the created model can be examined by rotating in 3D and zooming in and out. Although it is a less common approach for digital 3D reconstruction compared with the aforementioned post‐mortem imaging techniques, its ease of use and cost‐effectiveness [10] make it an interesting alternative for distance education of medical students. In recent years, there has been an increase in the use of single‐camera photogrammetry in several fields of science, including medicine, driven by the spread of relatively cheap high‐resolution digital cameras and easily accessible freeware, open‐source, and commercial photogrammetry and 3D modeling programs. A recent study described a basic, practical workflow regarding autopsy room photogrammetry [11], while two other publications proposed the possible utilization of similar methods in the field of education [12, 13].
During the first wave of the pandemic, we developed a practical, user‐friendly, low‐cost, and fast single‐camera photogrammetry workflow. Based on our initial results, we propose that this method has educational potential and, among available options, provides an experience most similar to a traditional autopsy.
2. MATERIALS AND METHODS
2.1. Photograph recording procedure
Photographs were taken during the forensic autopsies using Canon EOS 600D (18 megapixel) with EF‐S 18‐55mm kit lens. Camera setup included aperture priority (AV) f stops set around 16–22 with ISO between 1600 and 3200 and white balance adjusted to the room light temperature. We also used a smartphone camera (Samsung Galaxy S7 Edge) using automatic settings (12 megapixel) in case of the femur. Natural window light and light fixtures above the autopsy table were able to illuminate the entire surface of the body or organs/bones. Photographs were taken handheld from different points of view and with an overlap area of about 60%–70%. Generally, three sets of pictures were taken of each objects: one round from a low perspective, one round at around 45°, and one from above. Additional pictures of important details (e.g., injuries) were also taken. Camera positions are presented on Figure 1A. The total number of photographs for the reconstruction of total bodies varied between 55 and 100, and between 30 and 60 for the imaging of organs. We did not use special backgrounds.
FIGURE 1.
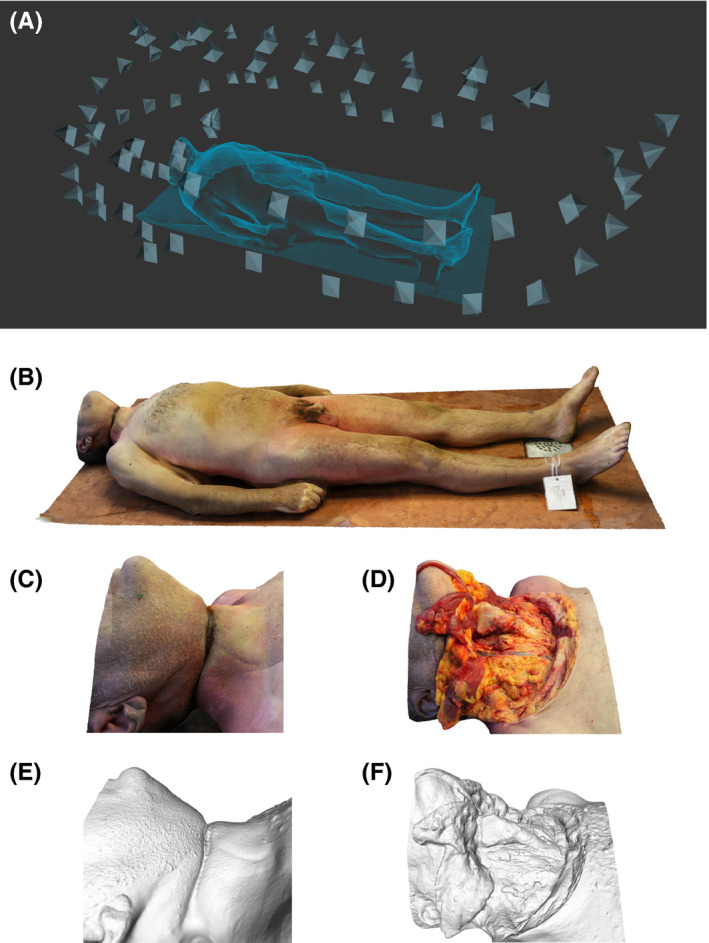
Photogrammetric reconstruction of a forensic autopsy of a case of suicidal hanging. Camera positions (A). Model of the whole body (B). Hanging mark on the neck: model with texture (C) and solid model of the same area (D). Layer‐by‐layer preparation of neck structures: model with texture (E) and solid model of the same segment (F) [Colour figure can be viewed at wileyonlinelibrary.com]
A detailed guide and reference sheet about the photography process can be found at Appendix S1.
2.2. Post‐processing of data
Images were transferred to a computer, and any blurred or out of focus ones were erased. The remaining image sets were uploaded to Autodesk ReCap Photo. A detailed guide to the use of the software can be found in the Appendix S2. The constructed 3D models were cropped and remeshed to decrease polygon count and converted into .obj file format. This ensures compatibility with viewing various software. The photographs were de‐identified during the process, and the use of these anonymized pictures for scientific and educational purposes is allowed by the 40. § (3) of the Hungarian act of Forensic Experts (2016.XXIX).
2.3. The online course test
Twenty volunteer medical students attended a special online forensic pathology seminar focusing on the usability of 3D models in education only. Previously, each student successfully completed the original, in‐person version of the forensic pathology course involving multiple autopsy room and forensic post‐mortem CT/MR demonstrations.
The online demonstration contained (1) a post‐mortem external examination and neck dissection in a case of suicidal hanging (Figure 1B–D); (2) an external post‐mortem examination in a case of a suicidal wrist cut; (3) the external examination of the lungs and liver in a case of polytrauma (Figure 2); and (4) one anthropology‐oriented case, consisting of skull, humerus, and femur (Figure 3). The seminar was held on Microsoft Teams, while the 3D models were presented by screen sharing. After the seminar, the students had the opportunity to use some of the models in Microsoft Teams without downloading the files, or they could download the 3D models and attempt to use them on their own computer/tablet or mobile phone. Microsoft 3D Viewer, a free application in Windows 10, or Emb3D, a free application in iOS/Android, was used by the students. A video showing one of the 3D models can be accessed from https://youtu.be/TB9pUIogxiQ
FIGURE 2.
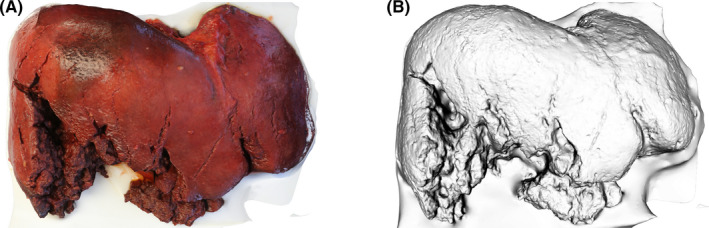
Model of a polytraumatic liver with texture (A) and as a solid model (B) [Colour figure can be viewed at wileyonlinelibrary.com]
FIGURE 3.
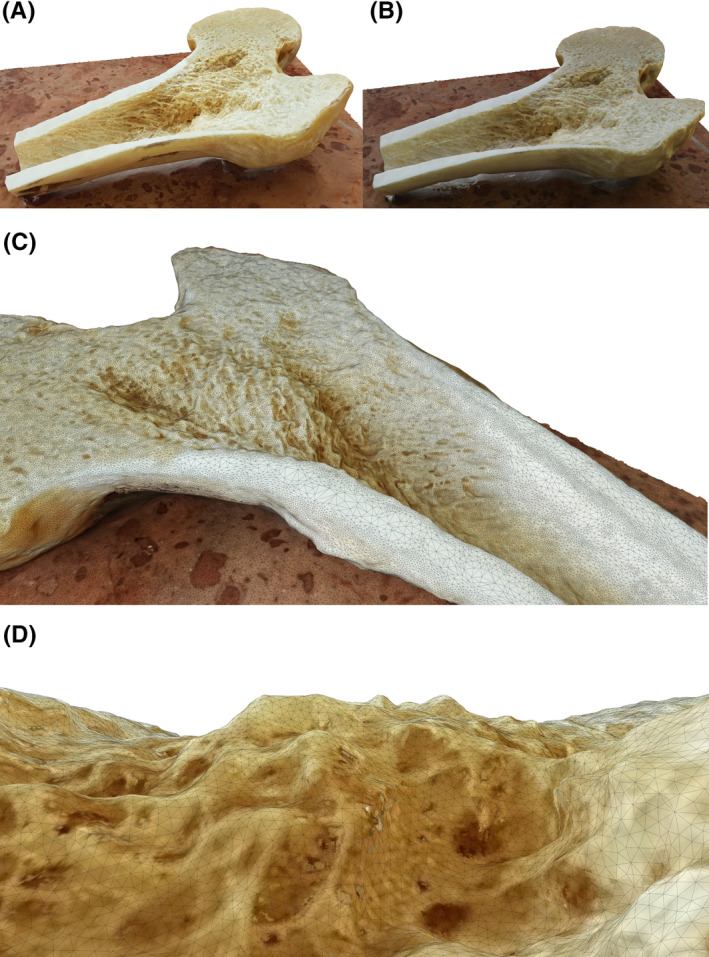
Femur models created with photogrammetry. Model created with a smartphone (Samsung S7 Edge (A) and a DSLR (Canon EOS 1300D) (B). Wireframe of the model superimposed on a part of the model (C). Virtual view from the medullary cavity with superimposed wireframe (D) [Colour figure can be viewed at wileyonlinelibrary.com]
All participants were requested to give formal feedback, answering eight questions regarding the usefulness of the method. The first part of the anonymous questionnaire consisted of three questions, in which photogrammetry was compared to other “conventional” methods. The students had to respond according to a 5‐point Likert scale to express their satisfaction with 3D photogrammetry models compared with current in‐person autopsy room experiences, watching pre‐recorded autopsy videos, or viewing post‐mortem images. The second segment consisted of three questions about the possible future role of photogrammetry in forensic pathology education. In this part, the participants had to respond using a 3‐point Likert scale to indicate whether they would like to learn with this modality only in the setting of required distance education, or whether it could be used in the setting of in‐person education as an additional educational modality or as a replacement for the current conventional in‐person autopsy room experience. The last part of the questionnaire contained two open‐ended questions. One related to the quality of the 3D models, asking the students which of three bone models was created using a smartphone camera, and the other asked for the student’s personal opinions, suggestions, and technical notes.
2.4. Statistical analysis
Chi‐square test was calculated with GraphPad (GraphPad Software) to determine statistical significance between answers. Level of significance was p < 0.05.
3. RESULTS
Each participant completed the questionnaire. The responses are presented in Tables 1 and 2 and show that 3D models are a promising educational modality in forensic pathology. While 100% of the students recommended the use of photogrammetry in distance education and as a supplement to traditional in‐person autopsy experiences, only 40% indicated that it should be used instead of the in‐person demonstration.
TABLE 1.
Questionnaire: Comparison of photogrammetry to other means of autopsy demonstrations
| How satisfied are you with the photogrammetry models compared to… | Completely satisfied | Very satisfied | Moderately satisfied | Slightly satisfied | Not at all satisfied |
|---|---|---|---|---|---|
| Traditional autopsy room demonstrations | 10 (50%) | 9 (45%) | 1 (5%) | 0 (0%) | 0 (0%) |
| Watching an autopsy video | 16 (80%) | 3 (15%) | 1 (5%) | 0 (0%) | 0 (0%) |
| Post‐mortem CT/MR imaging | 14 (70%) | 6 (30%) | 0 (0%) | 0 (0%) | 0 (0%) |
TABLE 2.
Demonstration questionnaire: Preference of photogrammetric demonstration in different educational scenarios
| Would you recommend the use of photogrammetry… | Would recommend | Would not recommend | Do not know |
|---|---|---|---|
| In distance education | 20* (100%) | 0 (0%) | 0 (0%) |
| In addition to autopsy demonstrations in contact education | 20* (100%) | 0 (0%) | 0 (0%) |
| Instead of autopsy demonstrations in contact education | 8 (40%) | 7 (35%) | 5 (25%) |
p < 0.000.1 vs. would not recommend
According to the last part of the questionnaire, only one (5%) student correctly selected the image of the bone model which had been digitized using a smartphone camera.
The last question was about personal opinions. The students felt that photogrammetry would be a practical and potent tool in education: “I would use the method during the exam period and even after my forensic classes…”. Regarding technical handling of the models, and compatibility with different media tools and operating systems, only one student gave negative feedback, citing difficulties rotating the models using touchscreen device.
4. DISCUSSION
With the improvement of algorithms, photogrammetry has become widely available but is not yet a commonly used tool in forensic pathology and in medical education.
Documentation by photogrammetry was easy, fast, and fitted completely into our routine autopsy algorithm. The extra time needed to take the required photographs varied from 3 to 4 min per object, so it did not interrupt the process of autopsy. Basic knowledge in photography was sufficient to obtain images of good quality.
To increase depth of field, small aperture (f: 16 or 22) was used. This resulted in decreased light reaching the sensor, which increased shutter time and the likelihood of blurred pictures. To counter this, high sensitivity (ISO 1600‐3200) was set. In traditional photograph documentation, this should be avoided, because elevated sensitivity increases background “noise” levels. However, because of the use the overlapping pictures, noise is eliminated during the data processing.
Unlike post‐mortem imaging and 3D surface scanning, photogrammetry does not need special equipment. If there is homogenous lighting, even a mid‐range smartphone camera can produce suitable results. To demonstrate this, one of the bones (femur) was also photographed with a mobile phone. The resulting 3D model was presented to the students along with two other models made with the DSLR camera. Based on the result of the questionnaires, the vast majority of students could not detect which model was made by a professional camera and which one with a smartphone (Figure 3).
Among academic users, one of the most popular software products for photogrammetry is Meshroom, a free and open‐source 3D reconstruction software based on the AliceVision framework. For optimal results, it needs a computer with relatively strong CPU and a CUDA enabled GPU. Models can be produced with a slower computer as well, but the reconstruction can be very time‐consuming. We have used Autodesk ReCap Photo suite; one advantage is that the computation‐intensive tasks are handed server‐side, so the user does not need a powerful computer. For teachers, students, and academic institutions, AutoCAD offers a free educational license with some limitations.
Our study focused on the online forensic pathology teaching experience of medical students in Hungary during the first wave of the COVID‐19 pandemic. The results of our study indicate that photogrammetry has a high educational potential in forensic pathology, both in the setting of required distance education when in‐person autopsy experiences cannot be provided and providing a useful educational modality to enhance accompanying conventional in‐person autopsy education. By using the photogrammetric models, the students were able to visualize each dimension (including depth) of the wound and injury patterns, resulting in a similar experience to autopsy demonstration. In addition, they were able to study and review these models.
On the other hand, the application of this fast, easy, and cheap method could be a promising addition in pathology education, as it would allow the teacher to show more types of cases to students. 3D modeling of organs or organ systems affected with specific diseases could provide better visualization and understanding to students. The questionnaires showed that most students would see this technique as a supplementary method, but not a substitute, as one of the students commented: “I would not replace the autopsy demonstrations, because I really liked them, but this would help studying and practicing at home…”. Furthermore, this method also has much potential for use in routine forensic pathology as a way of documentation [11]. In courtroom testimony, the rotatable, zoomable 3D models have higher demonstrative value and help better understand certain situations than the standard static photograph documentation [14]. It is important to note that during the educational use of photogrammetric models of autopsy cases, the local legal regulations must always considered, and all 3D models should be de‐identified.
Supporting information
Appendix S1
Appendix S2
Acknowledgments
The authors thank Edit Anna Szegedi for the linguistic help.
References
- 1. World Health Organization . Novel Coronavirus(2019‐nCoV): Situation Report‐11. Geneva, Switzerland: WHO. https://apps.who.int/iris/bitstream/handle/10665/330776/nCoVsitrep31Jan2020‐eng.pdf?sequence=1&isAllowed=y. Accessed 24 Jan 2021. [Google Scholar]
- 2. Harden RM. Trends and the future of postgraduate medical education. Emerg Med J. 2006;23(10):798–802. 10.1136/emj.2005.033738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Trelease RB. From chalkboard, slides, and paper to e‐learning: How computing technologies have transformed anatomical sciences education. Anat Sci Educ. 2016;9(6):583–602. 10.1002/ase.1620. [DOI] [PubMed] [Google Scholar]
- 4. Charlton R. Autopsy and medical education: a review. J R Soc Med. 1994;87(4):232–6. [PMC free article] [PubMed] [Google Scholar]
- 5. Burton JL, Diercks‐O’Brien G, Rutty GN. Videos have a role in postgraduate necropsy education. J Clin Pathol. 2004;57(8):877–81. 10.1136/jcp.2003.010637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hunt NCA, James DS, Bull AD. The still video camera: a suitable and convenient method of demonstrating post mortem findings. Med Educ. 1997;31(5):386–9. 10.1046/j.1365-2923.1997.00677.x. [DOI] [PubMed] [Google Scholar]
- 7. Bolliger SA, Thali MJ. Imaging and virtual autopsy: looking back and forward. Philos Trans R Soc Lond B Biol Sci. 2015;370(1674):20140253. 10.1098/rstb.2014.0253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grabherr S, Baumann P, Costin M, Fahrni S, Mangin P. Post‐mortem imaging in forensic investigations: current utility, limitations, and ongoing developments. Res Reports Forensic Med Sci. 2016;6:25–37. 10.2147/rrfms.s93974. [DOI] [Google Scholar]
- 9. Urbanová P, Hejna P, Jurda M. Testing photogrammetry‐based techniques for three‐dimensional surface documentation in forensic pathology. Forensic Sci Int. 2015;250:77–86. 10.1016/j.forsciint.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 10. Struck R, Cordoni S, Aliotta S, Pérez‐Pachón L, Flora GF. Application of photogrammetry in biomedical science. In: Rea PM, editor. Biomedical visualisation. Advances in experimental medicine and biology. Vol. 1120. Cham, Switzerland: Springer; 2002. p. 121–30. [DOI] [PubMed] [Google Scholar]
- 11. Gitto L, Donato L, Di Luca A, Bryant SM, Serinelli S. The application of photogrammetry in the autopsy room: a basic, practical workflow. J Forensic Sci. 2020;65(6):2146–54. 10.1111/1556-4029.14493. [DOI] [PubMed] [Google Scholar]
- 12. Villa C. Forensic 3D documentation of skin injuries. Int J Legal Med. 2017;131(3):751–9. 10.1007/s00414-016-1499-9. [DOI] [PubMed] [Google Scholar]
- 13. Thompson TJU, Collings AJ, Earwaker H, Horsman G, Nakhaeizadeh PU. Forensic undergraduate education during and after the COVID‐19 imposed lockdown: Strategies and reflections from India and the UK. Forensic Sci Int. 2020;316(110500): 10.1016/j.forsciint.2020.110500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Blau S, Phillips E, O’Donnell C, Markowsky G. Evaluating the impact of different formats in the presentation of trauma evidence in court: a pilot study. Aust J Forensic Sci. 2019;51(6):695–704. 10.1080/00450618.2018.1457717. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Appendix S2


