Abstract
Objective
This study aimed to test the effectiveness of the Whole of Systems Trial of Prevention Strategies for Childhood Obesity (WHO STOPS Childhood Obesity) for behavioral, health‐related quality of life (HRQoL), and BMI outcomes.
Methods
This was a cluster randomized trial of 10 communities randomly allocated (1:1) to start intervention in 2015 (step 1) or in 2019 (after 4 years) in South West Victoria, Australia. Data were collected from participating primary schools in April to June of 2015 (73% school participation rate), 2017 (69%), and 2019 (63%). Student participation rates were 80% in 2015 (1,792/2,516 invited), 81% in 2017 (2,411/2,963), and 79% in 2019 (2,177/2,720). Repeat cross‐sectional analyses of measured height and weight (grades two, four, and six [aged approximately 7 to 12 years]), self‐reported behavior, and HRQoL (grades four and six) were conducted.
Results
There was an intervention by time interaction in BMI z scores (P = 0.031) and obesity/overweight prevalence (P = 0.006). BMI z score and overweight/obesity prevalence decreased between 2015 and 2017 and increased between 2017 and 2019 in intervention communities. The intervention significantly reduced takeaway food consumption (P = 0.034) and improved physical (P = 0.019), psychosocial (P = 0.026), and global (P = 0.012) HRQoL. Water consumption increased among girls (P = 0.033) in the intervention communities, as did energy‐dense, nutrient‐poor snack consumption among boys (P = 0.006).
Conclusions
WHO STOPS had a positive impact on takeaway food intake and HRQoL.
Study Importance.
What is already known?
-
►
Community‐based interventions are seen as promising approaches to childhood obesity prevention.
-
►
New trials are needed that engage with the complex nature of community trials.
-
►
Long‐term sustainability (>2 years) of shorter‐term trial effects are as yet unstudied.
What does this study add?
-
►
This is a longer trial (4 years) than any previously of its type.
-
►
WHO STOPS initially reduced overweight/obesity in the intervention group in the first 2 years followed by increases in subsequent years.
-
►
Over 4 years, WHO STOPS helped intervention children keep their takeaway food intake low and sustain HRQoL compared with control children.
How might these results change the direction of research or the focus of clinical practice?
-
►
Prevention efforts need to be embedded in all aspects of community health, including education settings and clinical practice, to be sustainable and effective.
-
►
Sustained improvements in behaviors and HRQoL can be achieved if efforts are supported across multiple community systems.
-
►
Adaptive trial methodologies that allow for unforeseen impacts on trial design are needed for the next phase of childhood obesity prevention.
Introduction
Childhood obesity is a precursor to adult obesity, a major determinant of multiple diseases (1), and prevention of childhood obesity is a global priority (2, 3). The high prevalence of obesity, attendant diseases, and treatment costs are projected to rise (4). Childhood obesity (5) and associated behaviors track across the life‐span (6), making a compelling case for childhood obesity prevention.
Meta‐analyses of obesity prevention studies in children showed promising overall benefits of community‐based interventions among children (7, 8). Australian community‐based interventions among children under age 5 (9), primary school age (10), and adolescents (11) were among the first to demonstrate a reduction in the prevalence of obesity. These trials show that improving broader system determinants (e.g., community capacity for healthy change) strongly predicted the degree of reduction in childhood obesity (12) and encouraged diffusion of prevention action (13).
Several Lancet Commissions on obesity identified sustainability and scalability as challenges for community‐based childhood obesity prevention initiatives (14). The 2019 Lancet Commission (15) pointed to systems thinking as a way to enhance the reach, impact, and sustainability of such initiatives. Early examples of systems thinking being applied to obesity prevention include efforts in Australia (16), New Zealand (17), and England (18). These interventions fostered a shared understanding of the broader systemic determinants of obesity and engaged communities in asking how existing systems can be strengthened or new systems created (19). Building community capacity to understand and act to strengthen these systems is critical (12, 20).
Whole of Systems Trial of Prevention Strategies for Childhood Obesity (WHO STOPS Childhood Obesity) was a stepped wedge, cluster randomized trial of a whole of community systems‐based approach to preventing childhood obesity in the Great South Coast region of Victoria, Australia (21). The intervention helped community leaders and members identify and take actions to prevent childhood obesity in children aged 5 to 12 years (primary school age). The primary outcome was measured child BMI z score (BMIz) and overweight and obesity prevalence collected via an opt‐out monitoring system (22). Secondary outcomes were obesity‐related behaviors and perceived health‐related quality of life (HRQoL). Here, we answer the following questions for the WHO STOPS trial:
What were the 4‐year changes in BMIz and overweight and obesity prevalence (primary outcomes) among children attending primary schools in the intervention communities, compared with children in control communities?
What were the 4‐year changes in obesity‐related behaviors and HRQoL (secondary outcomes) among children attending primary schools in the intervention communities, compared with children in control communities?
Methods
Design
Following the baseline measurement of behaviors and height and weight in ten communities (April to June 2015), five communities were randomized to begin the intervention phase in late 2015. Under the original design (21), the remaining five communities were intended to begin the intervention in 2017. Delays occurred resulting from natural disasters (e.g., bushfire), staff turnover (in partner organizations), and shifting priorities of partners. As a result, the step 2 communities are treated here as “control communities.” The original step 1 communities were engaged as intended and maintained the intervention across the 4 years, and they are referred to as “intervention communities.” This paper reports the comparison of intervention versus control communities over 4 years (2015 to 2019). Full ethics clearances have been received from: Deakin University’s Human Research Ethics Committee (DU‐HREC) 2014‐279, DU‐HREC 2013‐095, Deakin University’s Human Ethics Advisory Group‐Health (HEAG‐H) 194_2014, HEAG‐H 17 2015, HEAG‐H 155_2014, the Victorian Department of Education and Training 2015_002622, 2013_002013, and the Catholic Archdiocese of Melbourne, Sale, Sandhurst, and Ballarat.
School and participant recruitment
All primary schools (government, independent, and Catholic) across 10 communities in six local government areas in South West Victoria, Australia, were invited. An opt‐out approach was used, whereby students were enrolled in data collection unless either the child or a parent or guardian actively declined participation. All children in grades two (mean age 7.8 years), four (mean age 9.8 years), and six (mean age 11.9 years) available on the day of data collection at their school who had not opted out were eligible. Repeat cross‐sectional measurement of these age groups provided a good representation across the school cohort without having to collect data from all children. Data were collected in Term 2 (April to June) of 2015, 2017 and 2019 on an electronic tablet (Samsung Galaxy; Samsung Group, Seoul, South Korea) using a specifically designed application.
WHO STOPS intervention description
The intervention comprised a multistage process (21).
The first phase involved the collection and sharing of baseline monitoring data to raise awareness of childhood obesity and to engage and recruit community leaders. Leaders included representatives of agencies (e.g., Departments of Health and Education, health services, business) and other community leaders with shared agendas or influence on childhood health, obesity prevention, healthy eating, or physical activity.
The second intervention phase involved identifying and working with community members and supporters who had authority to initiate action and who outlined the context for intervention and set the boundaries. This group included chief executive officers of health services and local council, business leaders, executives from the local water board, leaders of the local chamber of commerce, school principals, others in executive roles, and other informal and respected local community leaders. These leaders built a causal loop diagram of the causes of childhood obesity in their community (23) (e.g., Figure 1) using STICKE (Systems Thinking in Community Knowledge Exchange) version 1.7.1(Institute for Intelligent Systems Research and Innovation, Deakin University, Geelong, Australia) (24). The resultant diagram (known as a system map) captured drivers of childhood obesity in the community. Community leaders committed to advocating for the trial and providing resources (e.g., personnel) to support intervention implementation.
The third phase involved engaging a larger group of community representatives from organizations whose activities and agenda included remit and capacity to influence children's food and activity environments and choices, including retailers, schools, health organizations, leading community groups, and others.
The fourth phase involved this large group of engaged community representatives working together to design actions to prevent childhood obesity that they could carry out across the community, which were inspired by the systems map and informed by a prepared evidence brief on obesity prevention, including case studies from previous successful interventions.
Levels of community action implemented varied by the community. Action registers were recorded throughout the duration of the project. One community recorded 250 actions over 4 years, whereas another community recorded 11 actions in 2 years. Some key examples of actions were (1) a rural health service changing its beverage provision and cafe to be “green only,” in line with government healthy choices guidelines (25); (2) a local government area constructing a new footpath to allow schoolchildren to engage in active transport more easily to and from school; (3) implementing a junior sporting‐association‐wide water‐only policy; (4) a local primary school constructing signs encouraging children to be dropped off at set points away from the school gate to allow them to walk to school; and (5) implementing a healthy beverage policy at family day care.
The fifth and final phase involved ongoing data collection and updates of the systems map to enhance implementation and diffusion of the selected actions and stimulate new ideas in a constructive, capacity‐building cycle. The intervention design was deliberately adaptive so that communities moved through the intervention at their own pace.
At the 2017 data monitoring time point, step 1 communities were in the intervention phase (one had completed all five phases; the rest had completed phase two and were planning for phase three). At the 2019 data monitoring point, all step 1 communities in this analysis were ongoing in the fifth phase.
Demographic characteristics
A detailed description of the data collection procedures, psychometric properties of instruments used, and data management techniques has previously been published (22). Demographic data collected included gender, date of birth, country of birth, Aboriginal and/or Torres Strait Islander background, and language spoken at home, which was dichotomized as English or Other. Socioeconomic position was examined at the school level through the Index of Community Socio‐Educational Advantage (26).
Anthropometry measures
For all students, height and weight were measured by trained health professionals in private booths; the children wore light clothing and removed their shoes. A portable stadiometer (Charder HM‐200P Portstad, Charder Electronic Co. Ltd., Taichung City, Taiwan) was used to measure height to the nearest 0.1 cm, and an electronic weight scale (A&D Precision Scale UC‐321, A7D Medical, San Jose, California) was used to measure weight to the nearest 0.1 kg. Two measurements were taken for both height and weight, and a third measurement was taken if a discrepancy of >0.5 cm for height or >0.1 kg for weight was recorded between the two initial measures. Average height and weight were calculated for each child across these measures and used to generate age‐ and sex‐specific BMIz and overweight/obesity categories using the World Health Organization’s growth reference (27).
Physical activity and sedentary behavior
Grade‐four and ‐six students self‐reported time spent in moderate‐to‐vigorous physical activity (MVPA) and screen time for recreation (sedentary behavior) over the previous 7 days. Using the Core Indicators and Measures of Youth Health‐Physical Activity & Sedentary Behavior Module questionnaire (28), participants were asked to indicate the time they spent in MVPA (none, 1 to 14 minutes, 15 to 29 minutes, 30 to 59 minutes, 1 to 2 hours, or >2 hours) or screen time for recreation outside of school (none, <1 hour, 1 to 2 hours, 2 to 5 hours, and ≥5 hours) using these response options for each of the previous 7 days. These data were used to determine adherence to the physical activity (≥60 min/d of MVPA) and sedentary behavior (≤2 h/d of electronic media for entertainment) components of Australia’s 24‐hour movement and screen time guidelines (29). Contextual information was also collected (but not reported here) relating to physical activity and sedentary behaviors (e.g., having a TV in the bedroom, participation in active transportation to and from school) and perceived psychosocial influences on physical activity participation (e.g., social support, parental modeling) using the School Health Action, Planning and Evaluation System (SHAPES) questionnaire (30). Participants also reported the mode of transport they usually took to get to and from school in the past 7 days using response options (car, school bus, public bus, train or tram, cycling, other active, and other inactive) using the Core Indicators questionnaire (28). Students were classified as using active transport if they used one of these modes of transport to and/or from school.
Diet quality
For grade‐four and ‐six students, a modified version of the psychometrically tested Simple Dietary Questionnaire (31) was used to collect self‐reported “usual” intake of core foods and beverages (e.g., fruit, vegetables, water, unsweetened dairy products) and noncore foods and beverages (e.g., takeaway foods, packaged snacks, sugar‐sweetened beverages [SSBs]).
These data were used to determine adherence to the Australian Dietary Guidelines, which recommend daily consumption of 2 servings of fruit for children aged 9 to 18 years, 5 servings of vegetables for girls aged 9 to 18 years and boys aged 9 to 11 years, and 5.5 servings of vegetables for older boys (12 to 18 years) (32). Water servings were measured in cups (1 cup to approximately 250 mL), and students reported how many cups they consumed each day. Water data were dichotomized into <5 and ≥5 cups per day, based on the adequate intake level recommended for children 9 to 13 years old (33). There is no recommendation for SSB consumption in Australian children. An arbitrary cut point of ≤1 SSB per day was used. Takeaway food consumption was dichotomized as ≤2 times per week or above.
HRQoL
For grade‐four and ‐six students, version four of the 23‐item Pediatric Quality of Life Inventory 4.0 generic core scale (34) was used to measure children’s perceived HRQoL. It consists of four domains: physical, emotional, social, and school functioning. Questions were reverse scored, and domain scores were summed to provide an overall HRQoL score with potential ranges of 0 to 100. We report on the physical subscore, psychosocial subscore, and global, which combines emotional, social, and school functioning scores. The minimal clinically important difference of the Pediatric Quality of Life Inventory summary score is 4.5 points (35).
Statistical analyses
The sample size calculation was conducted under the original stepped wedge design (10 clusters, three steps, three measurement points, average of 300 children per cluster at each measurement time, α=0.05), assuming BMIz standard deviation (1.2) and intracluster correlation (0.027) estimated from a previous study of >2,500 Victorian schoolchildren (2013 to 2014) (36). Under these assumptions the study had 80% power to detect a difference of 0.13 BMIz score between groups. Because the second step of the stepped wedge design did not occur (see “Design” subsection) the study was analyzed as a parallel cluster randomized trial. When considering a cluster randomized trial with a baseline measure, the proposed sample size (10 clusters, average of 300 children per cluster at each measurement time) had 80% power to detect a 0.17 BMIz difference between arms (37).
The trial was analyzed as a parallel design with all statistical analyses conducted on an intention‐to‐treat basis.
The effect of the WHO STOPS intervention on BMIz was estimated using linear mixed models with school as a random effect to adjust for clustering. Community was not incorporated as a clustering factor because its contribution to variance was negligible after school was considered. Further, additional sensitivity analyses are reported in the online Supporting Information. The effect of the intervention on binary variables was estimated using generalized estimating equations (logit link and binomial distribution, compound symmetry correlation). The models included group (intervention, control), wave (2015, 2017, 2019), the interaction group × wave, the schools’ Index of Community Socio‐Educational Advantage tertile, and type of school (government, independent, Catholic). These last two factors were incorporated to adjust for potential imbalances in the type/socioeconomic level of schools participating at different waves. The same models were fitted for gender and grade level separately. For completeness, we report two prespecified contrasts for each outcome: mean difference (BMIz) and prevalence difference (binary outcomes) between study arms in (1) change between 2017 and baseline and (2) change between 2019 and baseline. We did not adjust for multiplicity of outcomes. All analyses were performed using SAS (version 9.4; SAS Institute, Cary, North Carolina).
Results
Of the primary schools invited in each study year, 40/55 (73%) participated in 2015, 48/70 (69%) participated in 2017, and 44/70 (63%) participated in 2019 (Table 1). The number of schools increased in 2017 and 2019 because of the inclusion of Catholic schools. Student participation rates were 80% in 2015 (1,792/2,251), 81% (2,411/2,963) in 2017, and 79% (2,137/2,720) in 2019. The average age of children ranged between 9.6 years and 9.9 years over the study waves, and between 93% and 96% reported speaking English at home.
TABLE 1.
School and student participation rate for 2015, 2017, and 2019
| School | Student | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2017 | 2019 | 2015 | 2017 | 2019 | |||||||||||||
| INV | CONS | RR | INV | CONS | RR | INV | CONS | RR | INV | CONS | RR | INV | CONS | RR | INV | CONS | RR | |
| Intervention | 34 | 25 | 73.5 | 41 | 25 | 61.0 | 41 | 23 | 56.1 | 1,202 | 972 | 80.9 | 1,260 | 1,041 | 82.6 | 1,127 | 878 | 77.9 |
| Control | 21 | 15 | 71.4 | 29 | 23 | 79.3 | 29 | 21 | 72.4 | 1,049 | 820 | 78.2 | 1,703 | 1,370 | 80.4 | 1,593 | 1,259 | 79.0 |
| Total | 55 | 40 | 72.7 | 70 | 48 | 68.6 | 70 | 44 | 62.9 | 2,251 | 1,792 | 79.6 | 2,963 | 2,411 | 81.4 | 2,720 | 2,137 | 78.6 |
This table includes values for all government, Catholic, and independent schools (excluding Catholic schools in 2015).
CONS, consent; INV, invited; RR, response rate.
BMIz
Overall
A significant trial arm by study wave interaction effect on BMIz was observed (P = 0.031), although no significant difference was observed between intervention and control groups in change in BMIz between 2015 and 2017 or between 2015 and 2019. Reductions in BMIz within the intervention group were observed from 2015 to 2017 followed by an increase to 2019. Conversely, BMIz remained stable within the control group across the study period (Table 2).
TABLE 2.
Demographic, anthropometric, and behavioral outcomes by wave and trial arm
| Intervention communities | Control communities | Difference in change (Int. vs. Control) | Difference in change (Int. vs. Control) | Wave × group interaction P | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2017 | 2019 | 2015 | 2017 | 2019 | 2017 vs. 2015 | 2019 vs. 2015 | ||||||||||
| N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | Estimate (95% CI) | P | Estimate (95% CI) | P | ||
| Demographic data | |||||||||||||||||
| Age, y (mean) | 970 | 9.6 (9.5 to 9.8) | 1,030 | 9.9 (9.7 to 10.0) | 878 | 9.8 (9.7 to 10.0) | 820 | 9.8 (9.6 to 9.9) | 1,370 | 9.9 (9.7 to 10.0) | 1,259 | 9.8 (9.7 to 10.0) | 0.15 (−0.06to 0.37) | 0.169 | 0.13 (−0.09to 0.36) | 0.236 | 0.345 |
| English language at home (%) | 568 | 93.4 (89.9 to 96.9) | 696 | 93.8 (91.5 to 96.1) | 583 | 96.3 (94.8 to 97.7) | 541 | 94.6 (93.1 to 96.0) | 928 | 92.5 (90.6 to 94.3) | 830 | 93.9 (92.2‐95.6) | 2.5 (−1.4 to 6.5) | 0.207 | 3.5 (−0.2 to 7.3) | 0.065 | 0.178 |
| Student SEIFA score (grade 4 & grade 6) (mean) | 588 | 972 (962 to 983) | 1,026 | 972 (962 to 983) | 872 | 973 (962 to 983) | 540 | 984 (972 to 995) | 1,363 | 982 (970 to 994) | 1,249 | 982 (971‐994) | 1.7 (−1.6 to 5.0) | 0.319 | 1.4 (−2.1 to 4.6) | 0.471 | 0.607 |
| Anthropometric outcomes | |||||||||||||||||
| BMIz (WHO) | 966 | 0.64 (0.52 to 0.76) | 993 | 0.55 (0.44 to 0.67) | 868 | 0.74 (0.62 to 0.86) | 815 | 0.60 (0.46 to 0.73) | 1,329 | 0.60 (0.48 to 0.73) | 1,228 | 0.60 (0.48‐0.72) | ‐0.09 (−0.24 to 0.06) | 0.217 | 0.10 (−0.06 to 0.25) | 0.219 | 0.031 |
| Overweight and obesity (%) | 966 | 35.5 (31.6 to 39.4) | 993 | 31.5 (27.4 to 35.6) b | 868 | 40.4 (35.8 to 45.0) b | 815 | 34.3 (29.5 to 39.2) | 1,329 | 32.9 (29.0 to 36.7) | 1,228 | 34.7 (30.8‐38.7) | ‐2.5 (−7.2 to 2.2) | 0.297 | 4.5 (−0.5 to 9.4) | 0.079 | 0.006 |
| Behavioral outcomes | |||||||||||||||||
| Met PA guideline, 5 days (%) | 594 | 32.1 (24.8 to 39.4) | 700 | 36.7 (30.2 to 43.3) | 587 | 40.3 (32.2 to 48.4) a | 544 | 33.4 (25.3 to 41.6) | 930 | 33.7 (26.3 to 41.1) | 831 | 37.0 (30.1‐43.9) | 4.4 (−5.7 to 14.4) | 0.396 | 4.6 (−5.5 to 14.8) | 0.371 | 0.632 |
| Met sedentary guideline, 5 days (%) | 564 | 82.9 (77.5 to 88.4) | 661 | 81.4 (76.9 to 85.9) | 584 | 79.7 (74.7 to 84.6) | 539 | 83.1 (77.6 to 88.6) | 893 | 82.9 (78.6 to 87.2) | 829 | 78.4 (73.6 to 83.2) | ‐1.3 (−8.2 to 5.5) | 0.701 | 1.4 (−6.5 to 9.4) | 0.722 | 0.658 |
| Active transport to or from school (%) | 593 | 25.3 (17.0 to 33.5) | 699 | 27.9 (22.9 to 32.8) | 587 | 23.0 (17.3 to 28.7) | 544 | 28.1 (19.2 to 37.0) | 931 | 30.3 (21.5 to 39.1) | 831 | 25.8 (18.4 to 33.3) | 0.4 (−6.5 to 7.4) | 0.903 | 0.0 (−9.0 to 9.0) | 0.999 | 0.987 |
| Met vegetable guideline (%) | 588 | 19.2 (15.2‐ 23.2) | 695 | 18.9 (15.8 to 22.1) | 585 | 17.4 (14.4 to 20.4) | 541 | 19.8 (15.3 to 24.4) | 921 | 18.6 (14.1 to 23.2) | 824 | 18.9 (15.1 to 22.7) | 0.9 (−5.1 to 7.0) | 0.764 | −1.0 (−6.4 to 4.5) | 0.730 | 0.733 |
| Met fruit guideline (%) | 580 | 72.9 (68.8 to 77.0) | 675 | 77.5 (74.3 to 80.8) a | 588 | 73.2 (69.0 to 77.4) | 538 | 76.4 (71.3 to 81.5) | 909 | 76.9 (72.4 to 81.4) | 831 | 80.0 (76.2 to 83.9) | 4.2 (−3.5 to 11.9) | 0.290 | ‐3.3 (−11.3 to 4.7) | 0.415 | 0.038 |
| Takeaway (less than once a week) (%) | 593 | 87.9 (84.1 to 91.7) | 696 | 87.6 (84.7 to 90.5) | 588 | 88.8 (85.9 to 91.8) | 545 | 91.1 (87.5 to 94.6) | 930 | 91.0 (88.0 to 94.0) | 830 | 86.0 (82.6 to 89.4) a | ‐0.2 (−5.2 to 4.8) | 0.942 | 6.0 (0.5 to 11.6) | 0.034 | 0.006 |
| Packaged snacks (≤1 times/d) (%) | 582 | 69.9 (65.5 to 74.3) | 655 | 73.2 (69.9 to 76.6) | 588 | 74.1 (70.1 to 78.1) | 530 | 76.2 (71.3 to 81.1) | 861 | 75.1 (70.0 to 80.2) | 831 | 73.6 (69.4 to 77.9) | 4.4 (−3.7 to 12.5) | 0.290 | 6.7 (−0.9 to 14.4) | 0.085 | 0.227 |
| Water ≥ 5 glasses/d (%) | 538 | 56.6 (50.6 to 62.6) | 625 | 61.7 (56.2 to 67.2) | 590 | 55.7 (50.4 to 61.0) | 486 | 60.6 (53.9 to 67.3) | 803 | 56.8 (50.1 to 63.4) | 831 | 53.7 (48.2 to 59.1) | 8.9 (−0.1 to 18.0) | 0.054 | 6.1 (−3.3 to 15.4) | 0.204 | 0.140 |
| SSB ≤ 1/d (%) | 593 | 82.8 (78.8 to 86.8) | 693 | 86.2 (81.9 to 90.6) | 588 | 84.2 (79.9 to 88.6) | 542 | 83.7 (78.7 to 88.6) | 927 | 85.6 (81.2 to 90.1) | 829 | 88.6 (84.6 to 92.6) | 1.4 (−4.3 to 7.1) | 0.619 | −3.5 (−10.5 to 3.4) | 0.318 | 0.189 |
| HRQoL | |||||||||||||||||
| HRQoL psychosocial score | 565 | 75.6 (73.4 to 77.9) | 677 | 74.7 (72.7 to 76.7) | 578 | 73.8 (71.7 to 76.0) | 530 | 78.4 (76.0 to 80.8) | 903 | 75.4 (73.2 to 77.6) b | 821 | 73.6 (71.5 to 75.8) c | 2.0 (−0.53 to 4.53) | 0.122 | 2.9 (0.4 to 5.5) | 0.026 | 0.079 |
| HRQoL physical score | 576 | 83.0 (81.0 to 84.9) | 687 | 84.0 (82.3 to 85.8) | 586 | 82.6 (80.7 to 84.5) | 537 | 86.2 (84.1 to 88.4) | 913 | 84.4 (82.5 to 86.3) b | 830 | 82.7 (80.8 to 84.6) c | 2.87 (0.34 to 5.39) | 0.026 | 3.1 (0.5 to 5.7) | 0.019 | 0.036 |
| HRQoL global score | 564 | 78.3 (76.4 to 80.3) | 673 | 78.0 (76.2 to 79.8) | 576 | 76.9 (75.0 to 78.8) | 530 | 81.3 (79.1 to 83.4) | 901 | 78.7 (76.7 to 80.6) b | 821 | 76.9 (74.9 to 78.8) c | 2.28 (0.00 to 4.57) | 0.050 | 3.0 (0.6 to 5.3) | 0.012 | 0.036 |
P < 0.05.
P < 0.01.
P < 0.001.
Boldface indicates significant difference within trial group between 2015 and 2017 or 2015 and 2019. Estimates are based on generalized mixed models (logit link, binary distribution, compound symmetry covariance matrix) or linear mixed models with school as a random effect. All models included time, group, and their interaction. Models for outcomes additionally included school type and Index of Community Socio‐Educational Advantage tertile. Behavioral and HRQoL outcomes only collected in grade‐four and grade‐six children.
HRQoL, Health‐Related Quality of Life; Int., intervention; PA, physical activity; SEIFA, Socio‐Economic Indexes For Areas; SSB, sugar‐sweetened beverage; WHO, World Health Organization.
By gender
No significant changes were observed in girls’ BMIz within groups or between groups. However, in the intervention group, girls’ BMIz initially reduced from 2015 to 2017 followed by an increase to 2019, whereas control girls experienced a steady increase from 2015 to 2019. A similar pattern was observed within boys in the intervention group in which BMIz initially reduced (but not significantly) from 0.59 in 2015 to 0.54 in 2017 but significantly increased between 2015 and 2019 to 0.77 (P = 0.047). Among control group boys, BMIz was stable from 2015 to 2019 (Table 3).
TABLE 3.
Demographic, anthropometric, and outcomes by gender, wave, and trial arm
| Intervention communities | Control communities | Difference in change (Int. vs. Control | Difference in change (Int. vs. Control) | Wave × group interaction P | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2017 | 2019 | 2015 | 2017 | 2019 | 2017 vs. 2015 | 2019 vs. 2015 | ||||||||||
| N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | Estimate (95% CI) | P | Estimate (95% CI) | P | ||
| Girls | |||||||||||||||||
| Demographic data | |||||||||||||||||
| Age, y (mean) | 470 | 9.6 (9.4 to 9.8) | 493 | 9.8 (9.6 to 10.0) a | 421 | 9.8 (9.6 to 10.0) | 409 | 9.9 (9.7 to 10.1) | 680 | 9.9 (9.7 to 10.1) | 579 | 9.8 (9.7 to 10.0) | 0.20 (−0.11 to 0.51) | 0.206 | 0.23 (−0.08 to 0.55) | 0.149 | 0.305 |
| English language at home (%) | 279 | 93.5 (90.3 to 96.8) | 332 | 93.3 (90.3 to 96.4) | 277 | 97.7 (95.9 to 99.5) a | 288 | 95.6 (93.9 to 97.3) | 463 | 93.3 (90.8 to 95.8) a | 388 | 96.5 (95.2 to 97.9) | 2.1 (−2.3 to 6.5) | 0.351 | 3.3 (−1.1 to 7.6) | 0.142 | 0.339 |
| Student ICSEA score (grade four and grade six) (mean) | 288 | 974 (963 to 984) | 487 | 974 (963 to 984) | 420 | 973 (963 to 984) | 285 | 986 (974 to 998) | 674 | 983 (971 to 995) | 575 | 984 (972 to 996) | 2.4 (−2.2 to 7.0) | 0.299 | 1.8 (−3.0 to 6.5) | 0.467 | 0.582 |
| Anthropometric outcomes | |||||||||||||||||
| BMIz (WHO) | 470 | 0.69 (0.54 to 0.84) | 477 | 0.57 (0.43 to 0.71) | 416 | 0.72 (0.58 to 0.86) | 405 | 0.59 (0.43 to 0.75) | 660 | 0.64 (0.50 to 0.78) | 571 | 0.63 (0.49 to 0.78) | −0.16 (−0.36 to 0.04) | 0.118 | −0.01 (−0.22 to 0.20) | 0.930 | 0.190 |
| Overweight and obesity (%) | 470 | 39.2 (34.5 to 43.8) | 477 | 35.3 (30.1 to 40.4) | 416 | 41.7 (36.5 to 47.0) | 405 | 37.7 (31.9 to 43.5) | 660 | 37.0 (33.0 to 41.1) | 571 | 37.9 (32.5 to 43.3) | −3.2 (−11.3 to 4.8) | 0.432 | 2.4 (−6.1 to 10.8) | 0.582 | 0.420 |
| Behavioral outcomes | |||||||||||||||||
| Met PA guideline, 5 days (%) | 291 | 23.7 (14.1 to 33.2) | 335 | 31.7 (24.3 to 39.2) | 279 | 31.5 (21.8 to 41.1) | 287 | 23.2 (14.2 to 32.2) | 464 | 29.5 (19.9 to 39.0) | 388 | 31.0 (22.9 to 39.2) | 1.8 (−12.8 to 16.4) | 0.809 | −0.1 (−13.1 to 13.0) | 0.993 | 0.953 |
| Met sedentary guideline, 5 days (%) | 282 | 86.5 (82.1 to 90.8) | 320 | 86.4 (82.2 to 90.6) | 277 | 82.2 (77.6 to 86.9) | 285 | 87.0 (82.3 to 91.7) | 439 | 87.9 (83.7 to 92.0) | 388 | 83.2 (78.7 to 87.7) | −0.9 (−8.5 to 6.8) | 0.824 | −0.4 (−8.5 to 7.7) | 0.922 | 0.973 |
| Active transport to or from school (%) | 292 | 24.8 (14.8 to 34.8) | 335 | 27.8 (21.5 to 34.1) | 279 | 20.5 (16.0 to 25.0) | 288 | 32.4 (22.3 to 42.5) | 464 | 37.0 (27.6 to 46.4) | 388 | 28.0 (19.2 to 36.8) | −1.6 (−10.7 to 7.6) | 0.739 | 0.1 (−10.3 to 10.5) | 0.983 | 0.872 |
| Met vegetable guideline (%) | 291 | 23.1 (17.9 to 28.4) | 334 | 20.1 (15.5 to 24.6) | 279 | 19.9 (15.6 to 24.2) | 287 | 20.4 (14.0 to 26.8) | 463 | 19.3 (13.3 to 25.2) | 388 | 18.8 (13.8 to 23.8) | −2.0 (−9.4 to 5.4) | 0.601 | −1.6 (−10 to 6.7) | 0.701 | 0.870 |
| Met fruit guideline (%) | 287 | 77.8 (72.0 to 83.5) | 323 | 85.9 (81.1 to 90.8) a | 279 | 76.6 (71.8 to 81.5) | 284 | 82.4 (75.2 to 89.7) | 453 | 82.1 (76.6 to 87.5) | 388 | 84.0 (79.2 to 88.8) | 8.6 (−2.4 to 19.6) | 0.127 | −2.7 (−12.7 to 7.4) | 0.600 | 0.001 |
| Takeaway (less than once a week) (%) | 292 | 90.7 (86.7 to 94.6) | 333 | 91.1 (87.8 to 94.3) | 279 | 91.7 (87.7 to 95.6) | 288 | 93.6 (89.4 to 97.7) | 463 | 93.9 (90.5 to 97.2) | 388 | 90.5 (86.8 to 94.3) | 0.1 (−5.4 to 5.5) | 0.978 | 4.1 (−2.7 to 10.8) | 0.238 | 0.311 |
| Packaged snacks (≤1 times/d) (%) | 288 | 71.9 (67.0 to 76.9) | 313 | 74.3 (69.0 to 79.7) | 279 | 75.1 (69.7 to 80.4) | 283 | 75.8 (69.0 to 82.5) | 429 | 80.8 (74.7 to 86.9) | 388 | 78.7 (73.2 to 84.2) | −2.6 (−12.5 to 7.2) | 0.603 | 0.2 (−9.7 to 10.0) | 0.975 | 0.820 |
| Water ≥5 glasses/d (%) | 269 | 52.9 (45.5 to 60.3) | 299 | 67.4 (60.4 to 74.4) a | 281 | 59.1 (52.7 to 65.4) | 255 | 60.7 (51.3 to 70.1) | 391 | 57.1 (47.4 to 66.9) | 388 | 55.0 (48.8 to 61.3) | 18.1 (4.3 to 31.8) | 0.010 | 11.8 (1.0 to 22.7) | 0.033 | 0.019 |
| SSB ≤1/d (%) | 291 | 83.1 (77.6 to 88.5) | 331 | 87.9 (83.8 to 92.0) a | 279 | 86.0 (81.1 to 90.9) | 285 | 87.7 (82.3 to 93.1) | 463 | 89.9 (85.8 to 94.1) | 386 | 90.5 (86.4 to 94.7) | 2.7 (−3.5 to 8.8) | 0.394 | 0.1 (−8.6 to 8.8) | 0.980 | 0.561 |
| HRQoL | |||||||||||||||||
| HRQoL psychosocial score | 275 | 77.4 (74.7 to 80.1) | 329 | 77.2 (74.7 to 79.6) | 274 | 75.0 (72.4 to 77.6) | 285 | 80.9 (78.0 to 83.7) | 454 | 77.3 (74.7 to 79.9) b | 383 | 75.8 (73.2 to 78.4) c | 3.4 (−0.1 to 6.8) | 0.055 | 2.6 (−0.9 to 6.2) | 0.148 | 0.144 |
| HRQoL physical score | 281 | 85.5 (83.0 to 88.0) | 333 | 85.8 (83.5 to 88.1) | 279 | 83.1 (80.7 to 85.5) | 288 | 88.0 (85.3 to 90.6) | 457 | 85.8 (83.4 to 88.2) | 388 | 83.6 (81.2 to 86.0) c | 2.5 (−0.9 to 5.8) | 0.154 | 2.0 (−1.5 to 5.4) | 0.272 | 0.340 |
| HRQoL global score | 274 | 80.3 (77.9 to 82.7) | 329 | 80.3 (78.1 to 82.4) | 272 | 77.9 (75.6 to 80.2) a | 285 | 83.5 (81.0 to 86.0) | 453 | 80.3 (78.0 to 82.6) b | 383 | 78.6 (76.3 to 80.9) c | 3.1 (0.0 to 6.2) | 0.049 | 2.4 (−0.8 to 5.7) | 0.136 | 0.129 |
| Boys | |||||||||||||||||
| Demographic data | |||||||||||||||||
| Age, y (mean) | 499 | 9.7 (9.5 to 9.8) | 540 | 9.9 (9.8 to 10.1) a | 454 | 9.9 (9.7 to 10.0) | 411 | 9.7 (9.5 to 9.9) | 690 | 9.9 (9.7 to 10.0) | 673 | 9.9 (9.7 to 10.0) | 0.09 (−0.21 to 0.38) | 0.565 | 0.05 (−0.25 to 0.35) | 0.738 | 0.848 |
| English language at home (%) | 289 | 93.3 (88.6 to 98.1) | 364 | 94.3 (91.8 to 96.8) | 303 | 95.5 (93.7 to 97.3) | 253 | 93.4 (90.9 to 95.9) | 465 | 91.6 (88.4 to 94.9) | 435 | 91.3 (88.0 to 94.7) | 2.8 (−3.0 to 8.6) | 0.344 | 4.3 (−1.5 to 10.1) | 0.148 | 0.350 |
| Student SEIFA score (grade four and grade six) (mean) | 300 | 972 (961 to 982) | 542 | 972 (961 to 982) | 449 | 972 (962 to 983) | 255 | 981 (969 to 994) | 689 | 981 (969 to 993) | 667 | 982 (970 to 994) | 0.5 (−4.2 to 5.3) | 0.831 | 0.1 (−4.7 to 5.0) | 0.959 | 0.970 |
| Anthropometric outcomes | |||||||||||||||||
| BMIz (WHO) | 496 | 0.59 (0.42 to 0.77) | 516 | 0.54 (0.38 to 0.70) | 452 | 0.77 (0.60 to 0.94) a | 410 | 0.60 (0.40 to 0.79) | 669 | 0.58 (0.40 to 0.75) | 657 | 0.58 (0.40 to 0.75) | −0.03 (−0.25 to 0.19) | 0.782 | 0.2 (−0.02 to 0.42) | 0.077 | 0.062 |
| Overweight and obesity (%) | 496 | 32.7 (27.4 to 38.0) | 516 | 28.9 (23.7 to 34.2) | 452 | 40.1 (33.8 to 46.4) b | 410 | 31.1 (24.9 to 37.3) | 669 | 29.2 (24.1 to 34.3) | 657 | 32.1 (27.1 to 37.1) | −1.9 (−8.1 to 4.3) | 0.546 | 6.4 (−0.9 to 13.7) | 0.088 | 0.045 |
| Behavioral outcomes | |||||||||||||||||
| Met PA guideline, 5 days (%) | 303 | 41.1 (32.9 to 49.3) | 365 | 41.6 (33.7 to 49.6) | 305 | 49.2 (41.1 to 57.3) a | 257 | 45.7 (33.9 to 57.5) | 466 | 38.7 (29 to 48.4) | 436 | 42.8 (34.5 to 51.2) | 7.5 (−6.0 to 20.9) | 0.276 | 10.9 (−3.6 to 25.4) | 0.142 | 0.340 |
| Met sedentary guideline, 5 days (%) | 282 | 79.0 (70.7 to 87.2) | 341 | 77.0 (70.3 to 83.7) | 304 | 76.9 (70.5 to 83.4) | 254 | 78.0 (69.7 to 86.3) | 454 | 78.4 (72 to 84.8) | 435 | 74.5 (67.6 to 81.4) | −2.4 (−11.4 to 6.7) | 0.607 | 1.4 (−9.2 to 12.1) | 0.793 | 0.637 |
| Active transport to or from school (%) | 301 | 26.7 (18.2 to 35.1) | 364 | 28.0 (21.7 to 34.3) | 305 | 26.2 (18.2 to 34.1) | 256 | 25.2 (14.3 to 36.1) | 467 | 26.4 (15.9 to 36.8) | 436 | 25.0 (16.8 to 33.2) | 0.2 (−9.1 to 9.5) | 0.972 | −0.3 (−10.0 to 9.4) | 0.953 | 0.996 |
| Met vegetable guideline (%) | 297 | 16.5 (11.7 to 21.3) | 361 | 18.1 (13.7 to 22.5) | 303 | 15.5 (12.0 to 19.0) | 254 | 21.2 (17.6 to 24.8) | 458 | 20.0 (15.5 to 24.5) | 429 | 21.4 (17.6 to 25.2) | 2.8 (−4.7 to 10.4) | 0.464 | −1.2 (−7.0 to 4.6) | 0.677 | 0.503 |
| Met fruit guideline (%) | 293 | 69.6 (64.1 to 75.0) | 352 | 70.0 (66.3 to 73.7) | 306 | 70.1 (63.4 to 76.8) | 254 | 71.5 (65.5 to 77.5) | 456 | 74.1 (69.5 to 78.8) | 436 | 78.8 (73.8 to 83.8) a | −2.2 (−10.7 to 6.4) | 0.617 | −6.8 (−18.8 to 5.2) | 0.264 | 0.503 |
| Takeaway (less than once a week) (%) | 301 | 85.0 (79.8 to 90.2) | 363 | 85.1 (82.0 to 88.1) | 306 | 87.3 (83.8 to 90.7) | 257 | 88.8 (84.3 to 93.3) | 467 | 88.7 (85.8 to 91.5) | 435 | 82.7 (78.8 to 86.6) a | 0.2 (−6.2 to 6.6) | 0.951 | 8.4 (0.1 to 16.7) | 0.047 | 0.012 |
| Packaged snacks (≤1 times/d) (%) | 294 | 67.9 (61.4 to 74.3) | 342 | 72.6 (67.9 to 77.2) a | 306 | 73.1 (67.7 to 78.4) b | 247 | 76.4 (71.5 to 81.4) | 432 | 69.7 (64.2 to 75.3) a | 436 | 69.4 (64.2 to 74.7) a | 11.4 (1.3 to 21.5) | 0.027 | 12.2 (3.5 to 20.9) | 0.006 | 0.015 |
| Water ≥5 glasses/d (%) | 269 | 60.1 (52.2 to 68.0) | 326 | 56.3 (49.6 to 63.0) | 306 | 52.1 (45.4 to 58.8) | 231 | 60.3 (52.0 to 68.5) | 412 | 56.2 (50.2 to 62.3) | 436 | 52.4 (45.3 to 59.5) | 0.2 (−10.3 to 10.8) | 0.966 | −0.1 (−13.8 to 13.6) | 0.987 | 0.997 |
| SSB ≤1/d (%) | 302 | 82.5 (77.3 to 87.7) | 362 | 85.2 (79.1 to 91.3) | 306 | 82.5 (77.6 to 87.3) | 257 | 79.5 (72.4 to 86.6) | 464 | 81.7 (76.4 to 87.0) | 436 | 87.2 (82.4 to 92) a | 0.5 (−8.7 to 9.7) | 0.915 | −7.7 (−17.0 to 1.6) | 0.105 | 0.087 |
| HRQoL | |||||||||||||||||
| HRQoL psychosocial score | 290 | 74.2 (71.4 to 77.0) | 348 | 72.8 (70.3 to 75.3) | 301 | 73.2 (70.6 to 75.9) | 245 | 76.5 (73.3 to 79.7) | 449 | 74.1 (71.3 to 76.8) | 431 | 72.4 (69.6 to 75.1) a | 1.0 (−2.6 to 4.6) | 0.587 | 3.1 (−0.6 to 6.8) | 0.096 | 0.214 |
| HRQoL physical score | 295 | 80.8 (78.0 to 83.6) | 354 | 82.6 (80.1 to 85.2) | 304 | 82.4 (79.7 to 85.1) | 249 | 84.6 (81.5 to 87.8) | 456 | 83.2 (80.4 to 85.9) | 435 | 82.0 (79.2 to 84.7) a | 3.3 (−0.5 to 7.0) | 0.085 | 4.3 (0.4 to 8.1) | 0.029 | 0.080 |
| HRQoL global score | 290 | 76.7 (74.0 to 79.3) | 344 | 76.3 (73.9 to 78.6) | 301 | 76.4 (73.9 to 78.9) | 245 | 79.4 (76.5 to 82.4) | 448 | 77.4 (74.8 to 80.0) | 431 | 75.7 (73.1 to 78.3) a | 1.7 (−1.6 to 5.0) | 0.319 | 3.5 (0.2 to 6.9) | 0.040 | 0.117 |
P < 0.05.
P < 0.01.
P < 0.001.
Boldface indicates significant difference within trial group between 2015 and 2017 or 2015 and 2019. Estimates are based on generalized mixed models (logit link, binary distribution, compound symmetry covariance matrix) or linear mixed models with school as a random effect. All models included time, group, and their interaction. Models for outcomes additionally included school type and Index of Community Socio‐Educational Advantage tertile. Behavioral and HRQoL outcomes only collected in grade‐four and grade‐six children.
HRQoL, Health‐Related Quality of Life; Int., intervention; PA, physical activity; SEIFA, Socio‐Economic Indexes For Areas; SSB, Sugar Sweetened Beverages; WHO, World Health Organization.
By year level
Over the study period, BMIz of the grade‐two cohort increased with each wave, although nonsignificantly. Among intervention communities, BMIz was significantly lower in the 2017 grade‐four intervention cohort compared with 2015 (P = 0.01 for grade four), although this was not sustained at 2019, whereas BMIz in the grade‐four control group remained stable over the same period, with a significant interaction effect (P = 0.033) (Table 4).
TABLE 4.
Demographic, anthropometric, and outcomes by year level, wave, and trial arm
| Intervention communities | Control communities | Difference in change (Int. vs. Control) | Difference in change (Int. vs. Control) | Wave × group interacton P | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2017 | 2019 | 2015 | 2017 | 2019 | 2017 vs. 2015 | 2019 vs. 2015 | ||||||||||
| N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | N | Estimate (95% CI) | Estimate (95% CI) | P | Estimate (95% CI) | P | ||
| YEAR 2 | |||||||||||||||||
| Demographic data | |||||||||||||||||
| Age, y (mean) | 374 | 7.8 (7.8 to 7.9) | 327 | 7.8 (7.8 to 7.9) | 281 | 7.8 (7.8 to 7.9) | 275 | 7.9 (7.9 to 8.0) | 436 | 7.9 (7.8 to 7.9) | 421 | 7.9 (7.8 to 7.9) | 0.09 (0.01 to 0.17) | 0.036 | 0.04 (−0.05 to 0.12) | 0.409 | 0.102 |
| Anthropometric outcomes | |||||||||||||||||
| BMIz (WHO) | 373 | 0.63 (0.47 to 0.80) | 325 | 0.66 (0.50 to 0.82) | 280 | 0.8 (0.64 to 0.96) | 275 | 0.57 (0.39 to 0.76) | 431 | 0.61 (0.45 to 0.78) | 420 | 0.69 (0.53 to 0.86) | −0.01 (−0.25 to 0.22) | 0.908 | 0.04 (−0.2 to 0.28) | 0.722 | 0.879 |
| Overweight and obesity (%) | 373 | 30.8 (24.4 to 37.1) | 325 | 32 (26.2 to 37.7) | 280 | 40.5 (33.6 to 47.4) a | 275 | 32.0 (25.7 to 38.3) | 431 | 30.0 (25.3 to 34.6) | 420 | 36.1 (30.8 to 41.4) | 3.2 (−8.4 to 14.9) | 0.586 | 5.7 (−6.1 to 17.4) | 0.346 | 0.641 |
| YEAR FOUR | |||||||||||||||||
| Demographic data | |||||||||||||||||
| Age, y (mean) | 316 | 9.8 (9.8 to 9.9) | 364 | 9.9 (9.8 to 9.9) | 303 | 9.8 (9.8 to 9.9) | 306 | 9.9 (9.9 to 10.0) | 477 | 9.9 (9.9 to 9.9) | 437 | 9.9 (9.9 to 10.0) | 0.08 (−0.01 to 0.16) | 0.073 | 0.03 (−0.06 to 0.12) | 0.530 | 0.179 |
| English language at home (%) | 297 | 92.8 (88.7 to 97) | 361 | 94.1 (91.3 to 97.0) | 295 | 96.4 (94.3 to 98.6) | 302 | 92.3 (89.8 to 94.9) | 473 | 94.2 (91.8 to 96.5) | 431 | 93 (90.9 to 95) | −0.5 (−5.9 to 4.9) | 0.858 | 3.0 (−2.3 to 8.3) | 0.266 | 0.216 |
| Student SEIFA score (grade four and grade six) (mean) | 309 | 973 (962 to 984) | 359 | 973 (963 to 984) | 300 | 973 (962 to 984) | 303 | 983 (971 to 995) | 476 | 981 (969 to 993) | 434 | 982 (970 to 995) | 2.5 (−2.4 to 7.3) | 0.320 | 0.7 (−4.3 to 5.7) | 0.788 | 0.569 |
| Anthropometric outcomes | |||||||||||||||||
| BMIz (WHO) | 315 | 0.76 (0.59 to 0.94) | 350 | 0.52 (0.36 to 0.69) a | 300 | 0.83 (0.66 to 1.00) | 306 | 0.69 (0.50 to 0.88) | 460 | 0.66 (0.49 to 0.84) | 418 | 0.66 (0.49 to 0.83) | −0.22 (−0.47 to 0.04) | 0.092 | 0.10 (−0.16 to 0.35) | 0.466 | 0.033 |
| Overweight and obesity (%) | 315 | 41.7 (35.3 to 48.1) | 350 | 30.3 (24.2 to 36.5) b | 300 | 42.9 (36.6 to 49.2) | 306 | 38.6 (32.0 to 45.1) | 460 | 36.4 (31.8 to 41.1) | 418 | 37.9 (32.2 to 43.6) | −9.3 (−18.7 to 0.1) | 0.053 | 1.9 (−8.2 to 12.0) | 0.715 | 0.038 |
| Behavioral outcomes | |||||||||||||||||
| Met PA guideline, 5 days (%) | 314 | 26.7 (18.3 to 35.0) | 362 | 30.3 (23.5 to 37.1) | 297 | 33.5 (23.8 to 43.1) | 305 | 30.6 (21.7 to 39.5) | 475 | 25.4 (17.2 to 33.6) | 431 | 28.0 (20.0 to 35.9) | 8.8 (−3.3 to 21.0) | 0.154 | 9.5 (−4.9 to 23.8) | 0.195 | 0.328 |
| Met sedentary guideline, 5 days (%) | 289 | 78.7 (73.0 to 84.4) | 334 | 82.6 (77.3 to 87.8) | 296 | 81.9 (77.3 to 86.5) | 303 | 81.2 (74.8 to 87.6) | 451 | 81.1 (76.6 to 85.7) | 430 | 79.4 (74.9 to 83.9) | 4.0 (−5.6 to 13.6) | 0.419 | 5.0 (−4.8 to 14.8) | 0.319 | 0.592 |
| Active transport to or from school (%) | 313 | 20.7 (13.1 to 28.3) | 362 | 20.2 (15.2 to 25.1) | 297 | 16.0 (10.1 to 21.8) | 305 | 23.0 (13.0 to 33.0) | 476 | 24.2 (15.5 to 32.9) | 431 | 23.9 (15.9 to 31.8) | −1.7 (−10.2 to 6.8) | 0.695 | −5.6 (−15.7 to 4.6) | 0.284 | 0.555 |
| Met vegetable guideline (%) | 311 | 18.6 (13.8 to 23.4) | 361 | 21.8 (18.4 to 25.1) | 297 | 19.4 (15.7 to 23.1) | 305 | 21.9 (16.0 to 27.8) | 473 | 17.2 (12.3 to 22.0) | 431 | 21.0 (17.0 to 25.1) | 8.0 (−0.4 to 16.3) | 0.061 | 1.7 (−5.5 to 8.9) | 0.644 | 0.081 |
| Met fruit guideline (%) | 304 | 71.1 (65.7 to 76.5) | 351 | 75.1 (70.7 to 79.5) | 297 | 74.1 (68.2 to 80.0) | 301 | 74.4 (68.0 to 80.7) | 462 | 75.4 (70.7 to 80.1) | 431 | 82.9 (77.9 to 88) a | 3.0 (−5.8 to 11.8) | 0.499 | −5.5 (−15.7 to 4.6) | 0.286 | 0.092 |
| Takeaway (less than once a week) (%) | 312 | 85.4 (80.3 to 90.4) | 361 | 83.6 (79.8 to 87.3) | 297 | 87.7 (83.7 to 91.7) | 306 | 87.6 (83.2 to 91.9) | 476 | 87.3 (84.3 to 90.4) | 430 | 81.5 (77.2 to 85.8) a | −1.5 (−8.5 to 5.4) | 0.667 | 8.4 (0.3 to 16.5) | 0.041 | 0.006 |
| Packaged snacks (≤1 times/d) (%) | 304 | 66.2 (60.5 to 72.0) | 339 | 72.9 (67.2 to 78.7) | 297 | 71.8 (66.6 to 77.0) | 295 | 77.5 (72.6 to 82.5) | 442 | 74.0 (68.2 to 79.7) | 431 | 73.0 (67.3 to 78.7) | 10.3 (−0.2 to 20.8) | 0.054 | 10.1 (0.3 to 20.0) | 0.044 | 0.050 |
| Water ≥5 glasses/d (%) | 286 | 56.5 (52.4 to 60.5) | 327 | 64.7 (59.2 to 70.2) b | 298 | 55.7 (49.8 to 61.6) | 279 | 63.1 (57.1 to 69.2) | 419 | 59.8 (53.3 to 66.3) | 431 | 57.0 (52.5 to 61.5) | 11.6 (1.9 to 21.3) | 0.019 | 5.4 (−4.5 to 15.2) | 0.288 | 0.061 |
| SSB ≤1/d (%) | 312 | 81.3 (75.8 to 86.9) | 358 | 86.2 (82.5 to 89.9) | 297 | 83.4 (78.0 to 88.9) | 304 | 86.2 (80.6 to 91.7) | 473 | 83.7 (78.9 to 88.5) | 430 | 86.7 (82.1 to 91.4) | 7.3 (−0.3 to 14.9) | 0.060 | 1.5 (−7.5 to 10.6) | 0.738 | 0.054 |
| HRQoL | |||||||||||||||||
| HRQoL psychosocial score | 292 | 73.5 (71.2 to 75.8) | 343 | 73.8 (71.7 to 75.8) | 291 | 73.2 (71.0 to 75.3) | 297 | 76.6 (74.2 to 79.0) | 455 | 75.1 (73.1 to 77.2) | 425 | 71.9 (69.9 to 74.0) c | 1.8 (−1.7 to 5.2) | 0.313 | 4.3 (0.8 to 7.9) | 0.016 | 0.050 |
| HRQoL physical score | 300 | 80.8 (78.4 to 83.2) | 353 | 83.0 (80.8 to 85.2) | 295 | 81.1 (78.8 to 83.4) | 301 | 85.0 (82.4 to 87.5) | 462 | 82.9 (80.8 to 85.1) | 430 | 80.8 (78.6 to 83.0) b | 4.2 (0.6 to 7.9) | 0.023 | 4.5 (0.7 to 8.2) | 0.019 | 0.032 |
| HRQoL global score | 291 | 76.3 (74.2 to 78.5) | 341 | 77.1 (75.2 to 79.0) | 289 | 76.0 (74.1 to 78.0) | 297 | 79.8 (77.6 to 82.0) | 453 | 78.1 (76.2 to 80.0) | 425 | 75.2 (73.4 to 77.1) c | 2.4(−0.7 to 5.6) | 0.128 | 4.39 (1.1 to 7.5) | 0.009 | 0.034 |
| Grade six | |||||||||||||||||
| Demographic data | |||||||||||||||||
| Age, y (mean) | 280 | 11.9 (11.8 to 11.9) | 344 | 11.9 (11.8 to 11.9) | 294 | 11.9 (11.8 to 11.9) | 239 | 11.9 (11.8 to 11.9) | 457 | 11.9 (11.8 to 11.9) | 401 | 11.9 (11.9 to 11.9) | −0.01 (−0.10 to 0.08) | 0.769 | −0.05 (−0.14 to 0.04) | 0.306 | 0.546 |
| English language at home (%) | 270 | 94.3 (90.7 to 98.0) | 340 | 93.5 (90.8 to 96.3) | 288 | 96.4 (94.5 to 98.4) | 239 | 97.5 (96.0 to 99.0) | 455 | 90.9 (88.4 to 93.4) | 399 | 95.2 (92.4 to 98.0) | 5.8 (1.0 to 10.6) | 0.018 | 4.4 (−0.3 to 9.1) | 0.067 | 0.041 |
| Student SEIFA score (grade four and grade six) (mean) | 278 | 974 (963 to 984) | 339 | 972 (961 to 982) | 292 | 973 (962 to 983) | 237 | 985 (973 to 997) | 454 | 985 (973 to 997) | 397 | 985 (973 to 997) | −1.9 (−7.5 to 3.6) | 0.500 | −1.0 (−6.7 to 4.7) | 0.734 | 0.793 |
| Anthropometric outcomes | |||||||||||||||||
| BMIz (WHO) | 278 | 0.56 (0.37 to 0.75) | 323 | 0.48 (0.32 to 0.65) | 288 | 0.61 (0.44 to 0.79) | 234 | 0.52 (0.31 to 0.73) | 438 | 0.56 (0.39 to 0.74) | 390 | 0.46 (0.28 to 0.63) | −0.11 (−0.39 to 0.16) | 0.416 | 0.12 (−0.16 to 0.40) | 0.400 | 0.189 |
| Overweight and obesity (%) | 278 | 35.5 (28.4 to 42.7) | 323 | 31.3 (24.9 to 37.7) | 288 | 38.2 (30.1 to 46.3) | 234 | 32.1 (25.1 to 39.2) | 438 | 32.1 (26.9 to 37.3) | 390 | 29.6 (24.1 to 35.1) | −4.2 (−14.0 to 5.5) | 0.398 | 5.3 (−5.8 to 16.3) | 0.350 | 0.163 |
| Behavioral outcomes | |||||||||||||||||
| Met PA guideline, 5 days (%) | 279 | 37.9 (31.4 to 44.3) | 343 | 43.7 (37.2 to 50.2) | 290 | 47.5 (40.3 to 54.7) b | 239 | 38.3 (29.0 to 47.5) | 455 | 44.0 (36.8 to 51.2) | 400 | 48.3 (39.8 to 56.8) | 0.1 (−9.7 to 9.8) | 0.991 | −0.5 (−12.8 to 11.9) | 0.942 | 0.996 |
| Met sedentary guideline, 5 days (%) | 274 | 87.5 (80.4 to 94.7) | 332 | 80.5 (73.9 to 87.2) a | 288 | 77.6 (70.6 to 84.5) b | 236 | 85.6 (78.3 to 92.8) | 442 | 84.8 (77.4 to 92.1) | 399 | 77.5 (70.8 to 84.2) a | −6.2 (−14.0 to 1.7) | 0.123 | −1.9 (−11.6 to 7.9) | 0.706 | 0.287 |
| Active transport to or from school (%) | 279 | 30.2 (18.8 to 41.5) | 342 | 36.2 (29.7 to 42.8) | 290 | 31.6 (24.6 to 38.7) | 239 | 35.0 (24.1 to 45.9) | 455 | 38.5 (27.2 to 49.7) | 400 | 29.3 (19.2 to 39.3) | 2.6 (−6.8 to 12.1) | 0.583 | 7.2 (−4.0 to 18.5) | 0.209 | 0.374 |
| Met vegetable guideline (%) | 276 | 21.9 (16.3 to 27.6) | 339 | 17.1 (12.7 to 21.5) | 288 | 16.6 (12.9 to 20.4) | 236 | 19.5 (12.4 to 26.6) | 448 | 22.7 (16.3 to 29.1) | 393 | 18.7 (13.7 to 23.7) | −8.0 (−18.6 to 2.5) | 0.136 | −4.5 (−13.1 to 4.0) | 0.300 | 0.327 |
| Met fruit guideline (%) | 275 | 75.6 (70.7 to 80.5) | 329 | 80.3 (77.1 to 83.4) | 291 | 72.0 (66.5 to 77.5) | 237 | 80.4 (70.8 to 90.0) | 447 | 80.0 (74.4 to 85.6) | 400 | 78.1 (73.7 to 82.6) | 5.1 (−7.9 to 18.0) | 0.445 | −1.3 (−13.6 to 10.9) | 0.830 | 0.333 |
| Takeaway (less than once a week) (%) | 280 | 90.8 (87.1 to 94.4) | 340 | 92.0 (89.6 to 94.5) | 291 | 90.1 (87.1 to 93.1) | 239 | 95.6 (92.7 to 98.5) | 454 | 95.2 (92.2 to 98.2) | 400 | 91 (87.4 to 94.6) a | 1.6 (−2.7 to 6.0) | 0.463 | 3.9 (−1.8 to 9.5) | 0.179 | 0.404 |
| Packaged snacks (≤1 times/d) (%) | 277 | 73.7 (67.5 to 80.0) | 320 | 72.9 (66.3 to 79.5) | 291 | 75.8 (71.3 to 80.3) | 235 | 74.1 (67.6 to 80.6) | 419 | 76.0 (70.1 to 81.8) | 400 | 73.9 (67.6 to 80.2) | −2.7 (−13.9 to 8.5) | 0.638 | 2.2 (−7.9 to 12.4) | 0.666 | 0.687 |
| Water ≥5 glasses/d (%) | 251 | 57.3 (47.6 to 67.0) | 303 | 58.6 (51.0 to 66.2) | 292 | 56.2 (48.7 to 63.8) | 207 | 59.7 (48.0 to 71.3) | 384 | 55.3 (46.6 to 63.9) | 400 | 51.3 (43.4 to 59.1) | 5.7 (−8.4 to 19.8) | 0.427 | 7.3 (−6.6 to 21.3) | 0.302 | 0.564 |
| SSB ≤1/d (%) | 280 | 84.3 (80.5 to 88.1) | 340 | 87.1 (82.0 to 92.2) | 291 | 85.2 (81.1 to 89.4) | 238 | 81.3 (76.6 to 86.0) | 454 | 88.3 (84.1 to 92.5) a | 399 | 90.9 (86.9 to 94.9) b | −4.2 (−11.0 to 2.7) | 0.232 | −8.7 (−15.9 to −1.4) | 0.019 | 0.062 |
| HRQoL | |||||||||||||||||
| HRQoL psychosocial score | 272 | 77.3 (74.2 to 80.4) | 339 | 75.4 (72.6 to 78.1) | 287 | 73.8 (70.9 to 76.7) b | 233 | 81.0 (77.6 to 84.5) | 448 | 75.6 (72.5 to 78.7) c | 396 | 75.6 (72.6 to 78.7) c | 3.6 (0.2 to 7.0) | 0.045 | 1.9 (−1.6 to 5.5) | 0.283 | 0.133 |
| HRQoL physical score | 275 | 84.6 (81.9 to 87.4) | 339 | 84.5 (82.1 to 86.9) | 291 | 83.5 (80.9 to 86.1) | 236 | 87.3 (84.3 to 90.4) | 451 | 85.5 (82.8 to 88.2) | 400 | 84.5 (81.8 to 87.2) a | 1.7 (−1.6 to 4.9) | 0.312 | 1.7 (−1.6 to 5.0) | 0.320 | 0.533 |
| HRQoL global score | 272 | 79.8 (77.0 to 82.5) | 337 | 78.6 (76.1 to 81.1) | 287 | 77.1 (74.5 to 79.7) a | 233 | 83.3 (80.2 to 86.4) | 448 | 79 (76.3 to 81.8) c | 396 | 78.7 (75.9 to 81.4) c | 3.1 (0.0 to 6.2) | 0.048 | 1.95 (−1.2 to 5.1) | 0.226 | 0.140 |
P < 0.05.
P < 0.01.
P < 0.001.
Boldface indicates significant difference within trial group between 2015 and 2017 or 2015 and 2019. Estimates are based on generalized mixed models (logit link, binary distribution, compound symmetry covariance matrix) or linear mixed models with school as a random effect. All models included time, group, and their interaction. Models for outcomes additionally included school type and Index of Community Socio‐Educational Advantage tertile. Behavioral and HRQoL outcomes only collected in grade‐four and grade‐six children.
HRQoL, Health‐Related Quality of Life; Int., intervention; PA, physical activity; SEIFA, Socio‐Economic Indexes For Areas; SSB, Sugar Sweetened Beverages; WHO, World Health Organization.
Proportion with overweight and obesity in 2015, 2017, and 2019
Overall
There was a significant interaction effect between trial group and time (P = 0.006) (Table 2). Within intervention communities, the prevalence of combined overweight and obesity was 35.5% in 2015, 31.5% in 2017, and 40.4% in 2019. This represented a significant reduction in prevalence of −4.0% (95% CI: −6.77% to −1.24%, P = 0.005) between 2015 and 2017 and a significant increase between 2015 and 2019 (+4.9% [95% CI: 1.8% to 8.0%, P = 0.002]). Prevalence within the control group remained stable at 34.3% in 2015 and 34.7% in 2019.
By gender
For both girls and boys (Table 3), a similar pattern of nonsignificant initial reduction in prevalence of overweight and obesity in intervention communities followed by an increase in prevalence was observed, whereas in the control communities the prevalence remained stable. A significant interaction effect was observed among boys (P = 0.045).
By year level
Differential effects were observed within grade levels. The prevalence of overweight and obesity within intervention communities changed −11.4% (95% CI: −18.9% to −3.8%, P = 0.003) among grade‐four students between 2015 and 2017 (significant group by wave P = 0.038). Over the 4‐year period, prevalence significantly increased by + 9.7% (95% CI: 0.9% to 18.6%) in grade‐two intervention communities (Table 4). Among control communities, prevalence within year levels remained relatively stable. No interaction effects were observed for wave and trial arm within grade‐two and grade‐six levels.
Behavioral outcomes
Overall
The number of children reporting meeting the physical activity guidelines increased by 8.2% (95% CI: 0.7%‐15.7%, P = 0.032) between 2015 and 2019 within intervention communities but not in control communities. However, control communities. However, the group by time interaction was not significant (Table 2). An interaction effect (P = 0.038) was observed for fruit consumption. In intervention communities, fruit consumption increased between 2015 and 2017 (+4.2%) and decreased again in 2019, whereas in control communities, fruit consumption gradually increased between 2017 and 2019.
Intake of takeaway food significantly improved in the intervention communities by 2019 relative to 2015 compared with control (6.0%; 95% CI: 0.5% to 11.6%, interaction, P = 0.006) (Table 2). Among intervention communities, the proportion of children consuming takeaway food less than once a week (i.e., the lowest intake category) did not change across the study period, whereas among control communities, this percentage significantly decreased between 2015 and 2019 (−5.1%; 95% CI: −9.1% to −1.1%, P = 0.013), indicating that takeaway food consumption increased for children in control communities.
By gender
Among girls, there was a significant interaction of group by time (P = 0.001) for prevalence of meeting fruit guidelines, with an increased prevalence in 2017 in the intervention communities, and a decrease by 2019, but a stable prevalence in the control communities (Table 3). There was a significant intervention effect on water consumption (interaction, P = 0.019) with an increased percentage of girls consuming more than five glasses of water per day in intervention communities between 2015 and 2017 (18.1% increase) and 2015 to 2019 (11.8% increase) compared with control communities (Table 3).
Among boys, there was a significant intervention effect on takeaway food (interaction, P = 0.012) and packaged snack consumption (interaction, P = 0.015) (Table 3). Prevalence of takeaway food less than once a week (i.e., the lowest intake category) was significantly higher in intervention than control communities in 2019 relative to 2015 (8.4%) (Table 3). Prevalence of boys reporting consumption of packaged snacks less than once a day relative to 2015 was significantly higher in the intervention group in 2017 (11.4%) and 2019 (12.2%) relative to the control group (Table 3).
By year level
Among grade‐four students, there were significant behavioral changes favoring intervention for low takeaway food consumption (8.4%; interaction, P = 0.006) and low packaged snack consumption (10.1%; interaction, P = 0.050) between 2015 and 2019 (Table 4). Among grade‐six students, the proportion of students reporting low SSB consumption significantly increased in the control communities, whereas in the intervention communities, SSB consumption remained relatively stable.
HRQoL
Overall
Significant intervention effects were observed for the physical and global HRQoL scores (interaction, P = 0.036 for both). Compared with control, and relative to 2015, the intervention significantly improved the psychosocial score in 2019 (2.9 points), the physical score in 2017 and 2019 (2.9 and 3.1 points, respectively), and the global score in both 2017 and 2019 (2.3 and 3.0 points, respectively) (Table 2).
By gender
Significant intervention effects favoring intervention communities for physical HRQoL (+4.3; P = 0.029) and global health (+3.5; P = 0.040) were observed over the 4‐year intervention period among boys; for girls, there was an intervention effect for the global HRQoL score between 2015 and 2017 (Table 3).
Discussion
Statement of principal findings
No intervention effect for the primary outcome BMIz or overweight or obesity was observed for intervention communities compared with control communities over the 4 years of the trial. Although we observed a statistically significant (4%) reduction in the prevalence of overweight and obesity in intervention communities in the first 2 years (2015 to 2017), this was followed by a large increase in the final 2‐year period against a backdrop of no change in control communities. Positive effects of the intervention were observed for takeaway consumption, water consumption among girls, and packaged snacks among boys. Positive intervention effects were reported for physical, psychosocial, and global HRQoL scores driven by reductions in all HRQoL outcomes among control communities relative to stable levels among intervention children.
Comparison with other studies
High‐quality community‐based obesity prevention studies are limited; a recent review (32) of contemporary studies (2013 to 2017) identified only seven studies that presented a quality design with a minimum follow‐up duration of 12 months and measured anthropometric outcomes. Of these studies, one was a randomized controlled trial (RCT) with 2 years’ follow‐up, and the remainder were quasi‐experimental (32). The RCT (33) targeted children aged 5 to 8 years recruited via recreation centers in San Diego, California. Unlike our study, no intervention effects on BMIz or behaviors were identified after 2 years, although significant intervention effects for reduction in BMIz were observed for girls.
A meta‐analysis (7) of eight community‐based interventions (1990 to 2011) found that seven had a positive impact on weight status in which BMIz was reduced by 0.16 among girls and 0.03 among boys, in line with the first 2 years of the WHO STOPS trial. For WHO STOPS, these improvements were reversed in the following 2 years, whereas control communities’ BMIz remained unchanged. The longest intervention period reported in this review was 3 years (38). Tarro et al. observed lower BMIz and obesity prevalence among intervention children (5 to 7 years old at baseline) compared with control children 2 years after intervention from their healthy lifestyle education program (39). Economos et al. observed a significant reduction in BMIz 1 year after intervention for Shape Up Somerville, a reduction that persisted after 20 months before dissipating as intervention intensity dropped (40).
The initial reductions followed by increase in prevalence and BMIz in WHO STOPS may be related to intervention length. A systematic review (41) of 26 prevention studies in the same age group as WHO STOPS found that interventions of 12 months or less were the most effective in preventing obesity.
The drop and subsequent increase in intervention communities remains a question for further investigation but our initial explanations are as follows: Firstly, at the 2‐year time point, the research team reduced their implementation support to step 1 communities to begin recruiting step 2 communities. Although this was planned, the impact of bushfires and other natural disasters resulted in the control communities delaying uptake of intervention for a further 2 years, and resources were reduced to what was planned for the second 2‐year period. These disasters were not uniformly distributed across the study region, and subsequent subanalyses should examine whether there may have been some impact on children’s health and behavior. Secondly, the data collection methods meant that monitoring data were available and presented back to communities in close to real time. One possible unintended consequence of the early signs of positive change in the intervention communities may have led to some complacency or shifting of priorities as the initial reduction suggested that “the job was done” and reductions in obesity were being observed. Thirdly, it is possible that as actions accumulated over time, they overwhelmed implementation capacity. It is generally agreed that multicomponent interventions targeting both physical activity and nutrition are most likely to be effective (42). In this trial, this was successful over the first 2 years, but as actions continued to be rolled out, a peak in capacity and or engagement may have been reached. Improvements in behaviors in the intervention communities between 2015 and 2017 (e.g., fruit guideline [all], SSB [girls]) that diminished thereafter, and the absence of change in targeted behaviors are consistent with this explanation. Finally, changes in the control communities suggest that, in the absence of intervention, regional Victorian environments were becoming more obesogenic for children (e.g., increased takeaway [all], reduced water [all], increased SSB [boys], increased packaged snacks [boys]) and negatively impacting HRQoL.
The Chirpy Dragon cluster RCT (43) of primary‐school‐based obesity prevention efforts was similar to WHO STOPS. Chirpy Dragon targeted physical activity and dietary behaviors using a complex intervention framework (44). A mean difference in BMIz between intervention and control was observed (−0.13), and positive intervention effects were observed for fruit and vegetables, SSBs, snacking, screen time behavior, and physical activity. We do not know whether these changes persisted, however, as the trial was conducted over a 12‐month period.
This intervention design is comparable to capacity‐building trials, such as those by Economos (40) and Sanigorski et al. (10), which have reported significantly lower BMIz. The similarities between these and the current trial was the focus on building the capacity of communities to design and implement prevention activities tailored to their local context.
Strengths
Our study represents the longest follow‐up (4 years) of any contemporary community‐based intervention. Until now, the longest was 3 years, with 1 to 2 years being most common (45). The trial used a cluster randomized design and electronic tablets for data collection saving time compared with paper‐based surveys. Local, high‐quality data were recognized by community partners as a key aspect of the community engagement and ongoing intervention adaptation. Student participation rates were higher than 80% using an opt‐out approach, which compares favorably to other active (opt‐in) school‐based data collection in which participation rates typically range between 30% and 60%. Participation bias has been observed in regard to differing student response rates and resulting estimates of BMIz and overweight/obesity prevalence (36).
Weaknesses
Communities were considered to be “active” once they had completed the third phase of the five‐phase intervention design process. This gave a clear “start point” adapted to community readiness but meant, for each community, the intervention period varied. This variation in intervention period likely impacted our primary outcome. One community had completed all phases as described in the WHO STOPS intervention description section by 2017, whereas the other four communities had completed the second phase. All communities in this analysis had completed all phases by 2019. Intention‐to‐treat analysis is likely to overlook the nuance of early or late adoption.
This trial was designed to engage community leaders in making changes that were feasible, realistic, and more likely to be sustained. Thus, interventions differ by community and vary depending on community resources, priorities, and capacity to engage. Levels of community action varied and showed some promise; one community recorded 400 intervention actions involving >20 community leaders and >150 community members.
Our study did not achieve the proposed sample size of 1,500 in each trial arm at each wave (21), so our analyses are underpowered for detection of BMIz change of an estimated −0.13. The observed changes that were shown to be significant and the intervention effects in secondary outcomes are therefore highly relevant because to detect a significant change in a percentage variable (e.g., percentage physical activity guide) requires large changes.
Meaning of the study: possible mechanisms and implications for clinicians or policy makers
WHO STOPS reduced obesity prevalence over 2 years and over 4 years helped a majority of children keep their takeaway intake low and sustained HRQoL in a context in which this was declining. Results varied with gender and age group, indicating that single‐behavior, single‐setting interventions are unlikely to generate the level of change required to improve child health or prevent obesity across the spectrum of childhood. Rather, interventions need to adapt to children’s needs considering age, gender, and the capacity or limitations of the surrounding systems. These were not “greenfield” communities (with no previous or existing prevention efforts), and any interpretation of overall study effect needs to consider that a range of efforts was already in place to address childhood obesity.
Childhood obesity is demonstrably preventable, and community‐based interventions are effective, feasible, and acceptable to government, industry, and the public (8). These interventions should plan to mitigate unforeseen social and economic shocks that may distract community efforts. For WHO STOPS, bushfire brought this issue into stark relief. To be more effective community interventions should be supported by larger auspice organizations, such as health services or local government, and they should be considered a priority across community leadership (39).
Funding agencies
This study was supported by an Australian National Health and Medical Research Council Partnership Project titled “Whole of Systems Trial of Prevention Strategies for childhood obesity: WHO STOPS Childhood Obesity” (APP1114118). During this time, SA was partly supported by funding from an Australian National Health and Medical Research Council/Australian National Heart Foundation Career Development Fellowship (GNT1045836). SA, NC, KAB, PF, ADB, HL, MM, BS, CB, and CS were researchers within a National Health and Medical Research Council Centre for Research Excellence in Obesity Policy and Food Systems (GNT1041020/APP1041020) at the time the study was conducted. Community partners also providing support to the research include Portland District Health, Western Alliance, Southern Grampians and Glenelg Primary Care Partnership, Colac Area Health, Southwest Primary Care Partnership, Portland Hamilton Principal Network of Schools, Colac Corangamite Network of Schools, The Glenelg Shire Council, Southern Grampians Shire Council, Warrnambool and District Network of Schools, Western District Health Service, and Victorian Department of Health and Human Services. The opinion and analysis in this article are those of the authors and are not those of the Department of Health and Human Services, the Victorian Government, the Secretary of the Department of Health and Human Services, or the Victorian Minister for Health.
Disclosure
The authors declared no conflict of interest.
Author contributions
SA, CS, KdLH, JL, LM, MM, BS, and CB conceived the trial design and data collection for the whole trial. LO, CS, NC, PF, and HL monitored data collection for the whole trial, wrote the statistical analysis plan, and cleaned and analyzed the data. SA, NC, KAB, PF, ADB, JL, and CS supported communities to implement the trial. SA, NC, KAB, KdLH, LM, MM, BS, CB, and CS designed data collection tools. All authors contributed to interpretation of results and drafting and revision of the paper.
Clinical trial registration
Australian New Zealand Clinical Trials Registry (ANZCTR.org.au) identifier 12616000980437.
Figure 1.
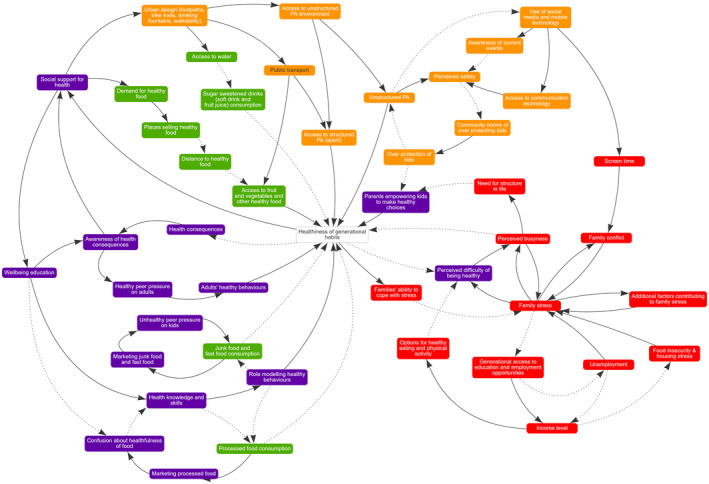
Community causal loop diagram of causes of obesity. PA, physical activity.
Supporting information
Acknowledgments
Because of ethical constraints on data sharing (e.g., participants did not consent for data to be shared with third parties), there are no data that can be shared.
References
- 1. Australian Institute of Health and Welfare . Impact of overweight and obesity as a risk factor for chronic conditions: Australian Burden of Disease Study. Australian Burden of Disease Study series no. 11. Cat. no. BOD 12. AIHW; 2017. [Google Scholar]
- 2. Chan M. WHO Director‐General Opens a Meeting of the Childhood Obesity Commission. World Health Organization website. Published July 17, 2014. https://www.who.int/director-general/speeches/detail/who-director-general-opens-a-meeting-of-the-childhood-obesity-commission 2014:1.
- 3. World Health Organization . Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013‐2020. WHO; 2013. [Google Scholar]
- 4. Ward ZJ, Long MW, Resch SC, et al. Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med 2017;377:2145‐2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Singh AS, Mulder C, Twisk JWR, et al. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008;9:474‐488. [DOI] [PubMed] [Google Scholar]
- 6. Craigie AM, Lake AA, Kelly SA, et al. Tracking of obesity‐related behaviours from childhood to adulthood: a systematic review. Maturitas 2011;70:266‐284. [DOI] [PubMed] [Google Scholar]
- 7. Wolfenden L, Wyse R, Nichols M, et al. A systematic review and meta‐analysis of whole of community interventions to prevent excessive population weight gain. Prev Med 2014;62:193‐200. [DOI] [PubMed] [Google Scholar]
- 8. Ananthapavan J, Nguyen PK, Bowe SJ, et al. Cost‐effectiveness of community‐based childhood obesity prevention interventions in Australia. Int J Obes 2019;43:1102‐1112. [DOI] [PubMed] [Google Scholar]
- 9. de Silva‐Sanigorski AM, Bell AC, Kremer P, et al. Reducing obesity in early childhood: results from Romp & Chomp, an Australian community‐wide intervention program. Am J Clin Nutr 2010;91:831‐840. [DOI] [PubMed] [Google Scholar]
- 10. Sanigorski AM, Bell AC, Kremer PJ, et al. Reducing unhealthy weight gain in children through community capacity‐building: results of a quasi‐experimental intervention program, Be Active Eat Well. Int J Obes 2008;32:1060‐1067. [DOI] [PubMed] [Google Scholar]
- 11. Millar L, Kremer P, de Silva‐Sanigorski A, et al. Reduction in overweight and obesity from a 3‐year community‐based intervention in Australia: The 'It's Your Move!' project. Obes Rev 2011;12:20‐28. [DOI] [PubMed] [Google Scholar]
- 12. Millar L, Robertson N, Allender S, et al. Increasing community capacity and decreasing prevalence of overweight and obesity in a community based intervention among Australian adolescents. Prev Med 2013;56:379‐384. [DOI] [PubMed] [Google Scholar]
- 13. Swinburn B, Malakellis M, Moodie M, et al. Large reductions in child overweight and obesity in intervention and comparison communities 3 years after a community project. Pediatr Obes 2014;9:455‐462. [DOI] [PubMed] [Google Scholar]
- 14. Gortmaker SL, Swinburn BA, Levy D, et al. Changing the future of obesity: science, policy, and action. Lancet 2011;378:838‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Swinburn BA, Kraak VI, Allender S, et al. The global syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. Lancet 2019;393 791‐846. [DOI] [PubMed] [Google Scholar]
- 16. Victorian Department of Health . Healthy Together Victoria ‐ Frequently Asked Questions. In: Department of Health , ed. State Government of Victoria; 2013. [Google Scholar]
- 17. Ministry of Health . Healthy Families New Zealand. Wellington: New Zealand Government; 2015. Accessed May 8, 2018. https://www.health.govt.nz/our‐work/preventative‐health‐wellness/healthy‐families‐nz
- 18. Public Health England . Whole Systems Approach to Obesity ‐ Invitation to Participate in National Programme. Public Health England; 2015. [Google Scholar]
- 19. Hovmand PS. Community Based System Dynamics. Springer; 2014. [Google Scholar]
- 20. Owen B, Brown AD, Kuhlberg J, et al. Understanding a successful obesity prevention initiative in children under 5 from a systems perspective. PLoS One 2018;13:e0195141. doi: 10.1371/journal.pone.0195141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Allender S, Millar L, Hovmand P, et al. Whole of systems trial of prevention strategies for childhood obesity: WHO STOPS Childhood Obesity. Int J Environ Res Public Health 2016;13:1143.doi:10.3390/ijerph13111143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Crooks N, Strugnell C, Bell C, et al. Establishing a sustainable childhood obesity monitoring system in regional Victoria. Health Promot J Austr 2017;28:96‐102. [DOI] [PubMed] [Google Scholar]
- 23. Allender S, Owen B, Kuhlberg J, et al. A community based systems diagram of obesity causes. PLoS One 2015;10:e0129683. doi: 10.1371/journal.pone.0129683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hayward J, Morton S, Johnstone M, et al. Tools and analytic techniques to synthesise community knowledge in CBPR using computer‐mediated participatory system modelling. NPJ Digit Med 2020;3:22.doi:10.1038/s41746-020-0230-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Department of Health and Human Services . Healthy Choices: Food and Drink Classification Guide: A System for Classifying Foods and Drinks Services. State Government of Victoria; 2016. [Google Scholar]
- 26. Australian Curriculum, Assessment and Reporting Authority . Index of Community Socio‐Educational Advantage (ICSEA). Accessed January 16, 2020. http://docs.acara.edu.au/resources/About_icsea_2014.pdf
- 27. de Onis M, Onyango AW, Borghi E, et al. Development of a WHO growth reference for school‐aged children and adolescents. Bull World Health Organ 2007;85:660‐667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Card A, Manske S, Mammen G, King M, Gleddie D, Schwartz M. Core indicators and measures of youth health physical activity & sedentary behaviour module: indicators and questions to use with youth respondents and/or school setting assessments. Memorial University of Newfoundland; 2012. [Google Scholar]
- 29. Australian Department of Health . Australian 24‐hour movement guidelines for children and young people (5–17) ‐ an integration of physical activity, sedentary behaviour and sleep. Updated April 12, 2019. Accessed April 23, 2020. https://www1.health.gov.au/internet/main/publishing.nsf/Content/health‐24‐hours‐phys‐act‐guidelines [Google Scholar]
- 30. Wong SL, Leatherdale ST, Manske SR. Reliability and validity of a school‐based physical activity questionnaire. Med Sci Sports Exerc 2006;38:1593‐1600. [DOI] [PubMed] [Google Scholar]
- 31. Parletta N, Cooper P, Gent DN, et al. Effects of fish oil supplementation on learning and behaviour of children from Australian Indigenous remote community schools: a randomised controlled trial. Prostaglandins Leukot Essent Fatty Acids 2013;89:71‐79. [DOI] [PubMed] [Google Scholar]
- 32. Bleich SN, Vercammen KA, Zatz LY, et al. Interventions to prevent global childhood overweight and obesity: a systematic review. Lancet Diabetes Endocrinol 2018;6:332‐346. [DOI] [PubMed] [Google Scholar]
- 33. Elder JP, Crespo NC, Corder K, et al. Childhood obesity prevention and control in city recreation centres and family homes: The MOVE/me Muevo Project. Pediatr Obes 2014;9:218‐231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the pediatric quality of life inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39: 800‐812. doi: 10.1097/00005650-200108000-00006 [DOI] [PubMed] [Google Scholar]
- 35. Varni JW, Burwinkle TM, Seid M, et al. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 2003;3:329‐341. [DOI] [PubMed] [Google Scholar]
- 36. Strugnell C, Orellana L, Hayward J, et al. Active (Opt‐In) consent underestimates mean BMI‐z and the prevalence of overweight and obesity compared to passive (Opt‐Out) consent. Evidence from the Healthy Together Victoria and Childhood Obesity Study. Int J Environ Res Public Health 2018;15:747. doi: 10.3390/ijerph15040747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hemming K, Kasza J, Hooper R, Forbes A, Taljaard M. A tutorial on sample size calculation for multiple-period cluster randomized parallel, cross-over and stepped-wedge trials using the Shiny CRT Calculator. Int J Epidemiol 2020;49:979‐995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Müller MJ, Asbeck I, Mast M, et al. Prevention of obesity–more than an intention. Concept and first results of the Kiel Obesity Prevention Study (KOPS). Int J Obes Relat Metab Disord 2001;25(suppl 1):S66‐S74. [DOI] [PubMed] [Google Scholar]
- 39. Tarro L, Llaurado E, Morina D, et al. Follow‐up of a healthy lifestyle education program (the Educacio en Alimentacio Study): 2 years after cessation of intervention. J Adolesc Health 2014;55:782‐789. [DOI] [PubMed] [Google Scholar]
- 40. Economos CD, Hyatt RR, Must A, et al. Shape Up Somerville two‐year results: a community‐based environmental change intervention sustains weight reduction in children. Prev Med 2013;57:322‐327. [DOI] [PubMed] [Google Scholar]
- 41. Gori D, Guaraldi F, Cinocca S, et al. Effectiveness of educational and lifestyle interventions to prevent paediatric obesity: systematic review and meta‐analyses of randomized and non‐randomized controlled trials. Obes Sci Pract 2017;3:235‐248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Brown T, Moore TH, Hooper L, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2019;7:CD001871. doi: 10.1002/14651858.CD001871.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Li B, Pallan M, Liu WJ, et al. The CHIRPY DRAGON intervention in preventing obesity in Chinese primary‐school–aged children: a cluster‐randomised controlled trial. PLoS Med 2019;16:e1002971. doi: 10.1371/journal.pmed.1002971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Campbell NC, Murray E, Darbyshire J, et al. Designing and evaluating complex interventions to improve health care. BMJ 2007;334:455‐459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bleich SN, Segal J, Wu Y, et al. Systematic review of community‐based childhood obesity prevention studies. Pediatrics 2013;132:e201‐e210. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


