Abstract
Objective
Network theory considers mental disorders as the product of symptom interaction. A growing number of studies employing this methodology has been conducted in eating disorders (EDs). We aimed to review those studies to provide evidence and limitations for a novel conceptualisation of EDs.
Methods
According to PRISMA guidelines and PICOS criteria, studies eligible for inclusion were those employing network analysis in people with a clinically defined diagnosis of ED. Twenty‐five studies were included and were analysed in relation to diagnosis, comorbidity, and treatment outcome.
Results
Despite the central role of overvaluation of body shape and weight and cognitive restraint across ED diagnoses, ineffectiveness, interoceptive awareness and affective problems appear central symptoms. Ineffectiveness and interoceptive awareness emerge as bridge symptoms promoting comorbidity in people with anorexia nervosa and in mixed ED samples. Although few studies assessed treatment outcome, there is evidence supporting the predictive role of central network nodes.
Conclusions
Ineffectiveness, interoceptive ability and affective problems may be included in the core ED psychopathology, in addition to ED‐specific symptoms. Network analysis is a promising method to reconceptualize comorbidity. Future studies are recommended to include general psychopathology in ED networks, to assess connections with the external field and clinical meaning of network connectivity.
Keywords: comorbidity, eating disorders, network analysis, psychopathology, systematic review
Highlights
Overvaluation of body shape and weight and cognitive restraint appear as central nodes across eating disorder diagnoses and ages.
In addition to specific symptoms, ineffectiveness, low interoceptive ability and affective problems also emerge as central nodes in eating disorders.
There is some evidence to point to ineffectiveness and low interoceptive ability as bridge nodes promoting psychiatric comorbidity.
Only few studies assessed treatment outcome through the network analysis approach
Abbreviations
- AN
anorexia nervosa
- BED
binge eating disorder
- BN
bulimia nervosa
- CBT
cognitive behavioural therapy
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- ED
Eating Disorder
- EDE‐Q
Eating Disorders Examination Questionnaire
- EDI
Eating Disorder Inventory
- MANTRA
Maudsley Model of Anorexia Nervosa Treatment for Adults
- OSFED
other specified feeding or eating disorders
- PICOS
population intervention control, and outcomes
- PRISMA
Preferred reporting items for systematic reviews and meta-analyses
- PTSD
Post‐Traumatic Stress Disorder
- RDoC
Research Domain Criteria
1. INTRODUCTION
Network models have been proposed as an alternative framework for the analysis of mental disorders (Borsboom, 2017; Borsboom et al., 2019; McNally, 2016) conceptualising psychiatric problems as the result of interplay among symptoms. This theory assumes that symptoms arise from factors internal (i.e., neurobiological dysfunctions) or external (i.e., stressful life events) to the person and directly activate other symptoms. Thus, symptoms influence one another and, once their connections become enough strong, these relations lead the network to sustain its own activation.
Clinical implications of network approach to mental disorders span diagnosis and classification, comorbidity, prognosis and treatment. Networks are composed of nodes, the observed variables, and connections among them, the ‘edges’. Within the networks, it is possible to identify the most central nodes, which are the nodes with the strongest connections in the network and thus with higher probability to promote the development of other network symptoms with respect to the activation of peripheral nodes. The centrality of each node can be estimated through the following indexes: the strength, the betweenness, and the closeness. The strength metric is the most reliable parameter in psychopathology networks (Epskamp et al., 2018). When assessing the centrality estimates and the strength of their edges, Epskamp et al. (2018) recommended to ascertain the reliability of the network calculating the accuracy of edge weights, by computing bootstrapped confidence intervals, and the stability of centrality indexes. Two networks can be compared in terms of network structure, edge strength and global strength by employing the network comparison test (van Borkulo et al., 2019). Within the network, it is also possible to identify particular groups of symptoms that are very closely related and influence each other to a greater degree (Borsboom et al., 2011; Borsboom & Cramer, 2013). Although these ‘clusters’ of symptoms may be associated with a specific diagnostic and statistical manual of mental disorders (DSM)‐defined mental disorder, their activation does not stop at the border of a DSM diagnosis and may promote the activation of symptoms belonging to a cluster associated with another DSM‐conceptualised disorder (Borsboom, 2017; Boschloo et al., 2015). This new conceptualisation of psychiatric disorders and comorbidity is in accordance with innovative research frameworks for investigating mental disorders, that is, the research domain criteria (RDoC) initiative (Insel et al., 2010). This system describes psychopathology as the product of the interplay between six domains of human functioning highlighting the importance to integrate classes of variables coming from different levels of analysis (from genetic to self‐report assessments). The network clusters may be a priori theoretically defined or identified through a network analytic procedure (Blanken et al., 2018). In this line, it is possible to identify the ‘bridge’ nodes shared by different clusters whose activation promotes comorbidity between two disorders (Fried et al., 2017). Two main estimates are used to assess the bridge centrality of each node, the bridge strength and the bridge expected influence, which are the sum of the absolute values and the sum of positive and negative values of the edges that connect a node to all nodes that are not part of the same community (Jones et al., 2019). Network studies also allow to investigate the connection of symptoms in the network with conditions that are external to the network but not outside of the person (the ‘external field’). Furthermore, the density of connections between symptoms has been hypothesised to reflect the probability of other symptoms activation, thus representing an important prognostic factor (Fried et al., 2017). The most central symptoms and their connections may represent the most important variables contributing to the maintenance of psychopathology and, thus, potential targets to disrupt the network and prevent further activation of symptoms (Borsboom, 2017; Fried et al., 2017).
Network approach offers a new perspective to conceptualise eating disorder (ED) psychopathology. Indeed, in the last few years a growing number of studies has employed the network approach in the ED field. This is highly reasonable in the light of studies (Treasure et al, 2020a; 2020b) describing ED psychopathology as the product of several vicious cycles, which is consistent with the network approach. In addition, treatment effectiveness in EDs is modest and there is a great need for treatment innovation in order to specifically target maintaining factors of the ED psychopathology (Kan et al., 2019; Murray et al., 2018; Murray et al., 2018, 2019; Pennesi & Wade, 2016). Two published papers (Levinson et al., 2018; Smith et al., 2018) have reviewed literature studies conceptualizing EDs from a network approach. However, they included a low number of studies and focused on the description of network analysis as a possible innovative tool to understand ED psychopathology. To this purpose, these review studies provided methodological considerations as well as a description of new methods and directions for network research in EDs. Given the number of network studies published in the recent years, there is a need to update the knowledge deriving from network theory application in EDs and to provide further directions for future studies. Thus, we aimed to systematically review studies exploring ED psychopathology and treatment through the use of network analysis. This systematic review attempts to provide evidence and limitations for a novel conceptualisation of EDs, as indicated by the network theory, analysing network data related to diagnosis, comorbidity, and treatment outcome in these psychiatric disorders. According to the network theory (Borsboom, 2017), we expected to observe high centrality not only of ED‐specific nodes, but also of those relative to internalising symptoms, with a predictive role of central nodes on treatment outcomes.
2. METHODS
2.1. Information sources and searches
The PRISMA guidelines were followed to select and assess published articles (Moher et al., 2010).
In order to perform a systematic review of the literature, the following search keys were used in PubMed and Scopus: ‘network analysis’ AND ‘anorexia nervosa’ OR ‘bing*’ OR ‘bulimi*’ OR ‘eating disord*’. Bibliographies from relevant papers were inspected to identify studies not yielded by the initial search.
2.2. Eligibility criteria
Articles were selected according to the following inclusion criteria: the paper (1) was a peer reviewed research article published in English; (2) included at least one network analysis as statistical method; (3) included samples of people with a current or lifetime diagnosis of any ED according to the DSM5 criteria and diagnosed through face‐to‐face clinical interviews or through validated diagnostic questionnaires; (4) was published between 1 January 2016 and 15 November 2020. Review papers, meta‐analyses and case reports were excluded.
2.3. Study selection and data collection process
The literature search identified 971 papers. GC identified literature papers through database searching. AMM and GC independently screened the identified full‐text articles for eligibility. This resulted in the inclusion of 25 studies in the qualitative synthesis. Figure 1 reports the flow diagram of study inclusion.
FIGURE 1.
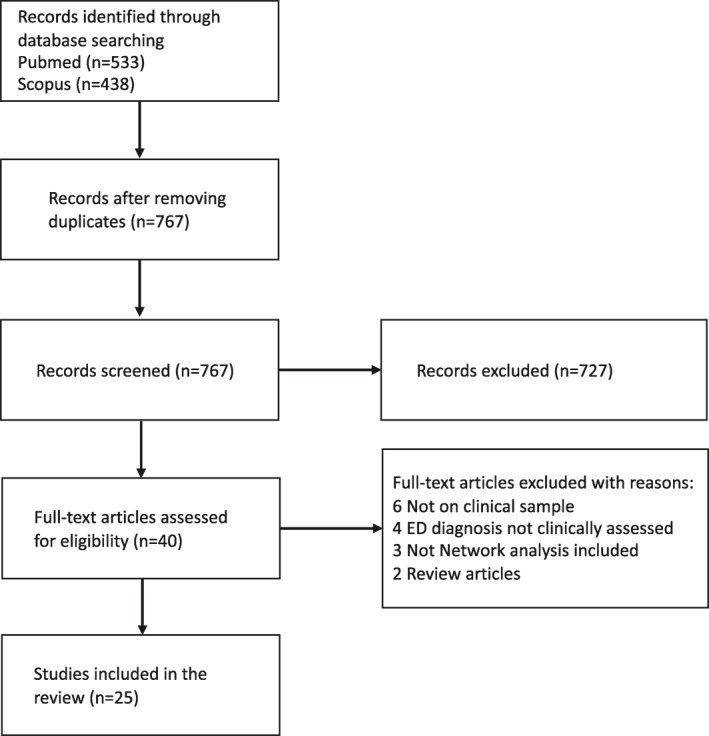
Flow chart of the study selection process
3. RESULTS
3.1. General characteristics of selected studies
The main characteristics (diagnosis, sample size of each patients' groups and psychometric assessment tools), the assessed outcomes and the main findings of each study are reported in Table 1
TABLE 1.
Description of included studies
| Study | Sample | Age (years): mean (SD) | Scales | Nodes | Outcome | Findings |
|---|---|---|---|---|---|---|
| Brown et al. (2020) | 428 male/female adolescents and male/female adults with AN; BN, BED and OSFED | 21.7 (8.8) | EDE‐Q, MAIA | Items | Centrality | Desire to lose weight, feeling guilty, listening for information from the body about emotional state |
| Outcome centrality | Stronger desire to lose weight at admission was associated with lower likelihood of achieving remission at discharge | |||||
| Bridge | Not feeling safe in one's body, mistrust in body sensations, ignoring physical tension | |||||
| Calugi et al. (2020) | 547 male/female adolescents and 724 male/female adults with AN |
|
EDE‐Q | Items | Centrality | Shape overvaluation and desiring weight loss both in adolescents and adults |
| Cascino et al. (2019) | 84 female adults with AN | 27.0 (8.8) | EDI‐2, IDEA | Subscores | Centrality | Feeling extraneous from one's own body, feeling oneself through objective measures, interoceptive awareness, social insecurity |
| Du Bois et al. (2017) | 194 male/female adolescents and adults with AN, BN, BED and OSFED | 25.5 (11.7) | EPSI, EDE‐Q | Subscores, 2 items from EDE‐Q | Centrality | Overvaluation of weight and shape |
| Elliott et al. (2020) | 142 female/male adults with AN | EDE, DASS | Items |
|
|
|
| Forbush et al. (2016) | 143 female/male adults with AN, BN, BED and OSFED | 25.0 (7.7) | EPSI | Items | Centrality | Trying on different outfits because one did not like how one looked, excessive exercise, eating when not physically hungry, being disgusted by the sight of obese people and not liking how one's body looked |
| Forrest et al. (2018) | 604 female adolescents and adults with AN and 477 with BN |
|
EDE‐Q | Items | Centrality | AN, BN: desiring weight loss, restraint, shape and weight preoccupation and shape overvaluation |
| Forrest et al. (2019) | 296 male/female adolescents and adults with AN, BN, BED, OSFED | Adolescents: 17.2 (1.3) | EDE‐Q, STAI‐T | Items | Centrality | Dietary restraint, overvaluation of and dissatisfaction with shape and weight, low feelings of satisfaction, steadiness and security |
| Adults: 27.1 (10.0) | Bridge | The strongest eating disorder bridge node was avoidance of social eating, while the strongest trait anxiety bridge node was low self‐confidence. | ||||
| Goldschmidt et al. (2018) | 636 male/female children and adolescents with AN, BN, OSFED | 15.4 (2.2) | EDE | Items | Centrality | Dissatisfaction with shape/weight, feelings of fatness, restraint over eating, fear of weight gain, and empty stomach |
| Hilbert et al. (2020) | 178 adults with BED | EDE, DEBQ, CIA, BDI, RSES, BIS‐BAS, BMI | Subscores | Centrality | Eating disorder‐related impairment and self‐esteem | |
| Outcome centrality | Central symptoms did not predict treatment outcome | |||||
| Outcome connectivity (NCT) |
|
|||||
| Kerr‐Gaffney et al. (2020) | 101 male/female adults with current of lifetime AN | 26.9 (8.3) | EDE‐Q, SRS‐2 | Items | Centrality | Isolation, difficulties with relating to others, and feelings of tension |
| Bridge | Concerning about other people seeing you eat, low self‐confidence | |||||
| Levinson et al. (2017) | 196 female/male adults with BN | 28.2 (9.2) | EDE, BDI, BAI | Items | Centrality | Fear of weight gain, desire to lose weight, feelings of fatness and worthlessness, sadness, concentration difficulties, feeling shaky/unsteady/choking or dizzy |
| Meier et al. (2020) | 303 female/male adults with AN, BN, BED, OSFED | 30.3 (11.8) | EDE‐Q, Y‐BOCS‐SR | Items | Centrality | Fear of weight gain, restrained eating, interference due to obsessions, weight overvaluation and preoccupation with shape and weight |
| Bridge | Difficulty controlling obsessions and compulsions, time spent on obsessions | |||||
| Monteleone et al. (2019) | 405 female/male children and adolescents with AN | 14.9 (1.8) | EDI‐2, MASC, CDI, YSR | Subscores | Centrality | Depression and personal alienation |
| Bridge | Depression, personal alienation, low self‐esteem, and interoceptive awareness | |||||
| Monteleone et al. (2019) | 94 female adults with AN‐restricting subtype and 134 with binge‐purging AN or BN |
|
EDI‐2, CTQ, STAI | Subscores | Shortest pathways |
|
| Monteleone et al. (2020b) | 77 female adults with AN and BN |
|
EDE‐Q, MASC (task), EAT‐R (task) | Subscores |
|
|
| Olatunji et al. (2018) | 5193 female adolescents and adults with AN, BN, OSFED | 22.61 (8.26) | EDI‐2, BDI, BAI | Subscores | Centrality |
|
| Outcome centrality | Ineffectiveness at admission predicted discharge BMI and discharge depression | |||||
| Rodgers et al. (2019) | EDE‐Q, BDI | Bayesian network in not‐abused ED people, symptom importance | Overvaluation of shape and weight, depressed mood, energy in behaviours (eating large amount of food) | |||
| Bayesian network in abused ED people, symptom importance | Depressed mood, energy out behaviours (purging and driven exercise), dietary restriction | |||||
| Smith et al. (2019) | 446 female/male adolescents and adults with AN, BN, OSFED | 26.12 (10.1) | EDE‐Q, QIDS‐SR, | Items | Centrality | Desire to lose weight, guilt about eating, shape overvaluation and wanting an empty stomach |
| STAI‐T | Outcome connectivity (NCT) |
|
||||
| Smith et al. (2020) | 238 female/male adolescents and adults with AN, BN, BED and OSFED | 17.61 (10.91) | EDI‐3, DSI‐SS, FAD | Subscores and items | Centrality | Thoughts of killing oneself, feeling inadequate, body dissatisfaction, and drive for thinness |
| Bridge | Pain tolerance connected suicidality and eating disorder symptoms | |||||
| Solmi et al. (2018) | 2068 female/male adolescents and adults with AN, BN, BED | AN: 23.13 (7.58) BN: 26.06 (8.23) BED: 35.31 (11.48) | EDI, SCL‐90, TPQ | Subscores | Centrality |
|
| Solmi et al. (2019) | 955 female adolescents and adults with AN |
|
EDI, SCL‐90, TPQ | Subscores | Centrality |
|
| Vanzhula et al. (2019) | 158 female/male adolescents and adults with AN, BN, BED, OSFED recently discharged | 25.77 (8.95) | EDE‐Q, PCL‐C | Items | Centrality | Binge eating, fear of weight gain, disturbing dreams and being upset at reminders of trauma |
| Bridge | Binge eating, irritability, desire for a flat stomach and concentration problems | |||||
| Vervaet et al. (2020) | 1969 female/male adolescents and adults with AN, BN, BED and OSFED | 23.93 (8.85) | EDI‐2 TCI, YSQ, FMPS, BDI‐II, STAI, RS | Subscores | Centrality | Overvigilance and inhibition of emotions, perfectionism, interoceptive awareness, ineffectiveness and impaired autonomy and performance |
| Wang et al. (2019) | 788 female/male adults with BED | 45.6 (9.9) | EDE | Items | Centrality | Overvaluation of shape and weight, dissatisfaction with weight |
Abbreviations: AN, Anorexia Nervosa; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; BED, Binge Eating Disorder; BIS‐BAS, Behavioral Inhibition System/Behavioral Activation System Scales; BMI, Body Mass Index; BN, Bulimia Nervosa; CIA, Clinical Impairment Assessment; CDI, Children's Depression Inventory; CTQ, Childhood Trauma Questionnaire; DASS, Depression, Anxiety and Stress Scale; DEBQ, Dutch Eating Behavior Questionnaire; DSI‐SS, Depressive Symptom Inventory‐ Suicidality Subscale; EAT‐R, Empathic Accuracy Task‐Revised; EDs, Eating Disorders; EDE‐Q, Eating Disorder Examination Questionnaire; EDI, Eating Disorder Inventory; EPSI, Eating Pathology Symptom Inventory; FAD, Fearlessness About Death (scale); FMPS, Frost Multidimensional Perfectionism Scale; IDEA, Identity and Eating Disorders; MAIA, Multidimensional Assessment of Interoceptive Awareness; MASC, Multidimensional Anxiety Scale for Children; MASC (task), Movie for the Assessment of Social Cognition; OSFED, Other Specified Feeding or Eating Disorder; QIDS‐SR, Quick Inventory of Depressive Symptomatology–Self‐Report; RS, Resilience Scale; RSES, Rosenberg Self‐Esteem Scale; SCL‐90, Symptom Check‐List 90; SRS, Social Responsiveness Scale; STAI, State and Trait Anxiety Inventory; TCI; Temperament and Character Inventory; TPQ, Tridimensional Personality Questionnaire; Y‐BOCS‐SR, Yale–Brown Obsessive Compulsive Scale–Self‐Report; YSQ, Young Schema Questionnaire; YSR, Youth Self Report.
Nine studies included samples with diagnosis of AN; 3 studies samples with diagnosis of BN and 3 studies samples with diagnosis of BED; 8 studies included mixed samples with AN, BN, BED and OSFED diagnoses; 3 studies mixed samples with AN, BN and OSFED diagnoses; one study a mixed sample with AN and BN diagnoses and one study a mixed sample with AN, BN and BED diagnoses. Thirteen studies were conducted on outpatients, 8 studies on inpatients, including one on recently discharged patients, and 3 studies included both inpatients and outpatients.
Thirteen studies presented networks with questionnaire single item scores as nodes; 8 networks with questionnaire subscale scores as nodes; 2 studies networks with both questionnaire single item scores and subscale scores as nodes and only one study presented a network composed of questionnaire subscale scores and task scores as nodes. Six studies included only eating related symptomatology in the networks, while 18 studies included general psychopathology measures in addition to the ED ones; 9 of the latter studies used the bridge function to identify the nodes connecting symptom clusters. No study assessed differences between men and women with EDs.
All studies performed concentration networks (consisting of undirected and weighted edges signified by partial correlations) with cross‐sectional data. Only one study (Rodgers et al., 2019) employed a Bayesian network (consisting of directed and unweighted edges).
Studies using the same outcome measure or outcome measures tapping into the same process were clustered together. This resulted in: (1) a group of studies assessing diagnosis and classification through the identification of the nodes with the highest centrality in the network; (2) a group of studies assessing psychiatric comorbidity through the bridge function analysis, which identifies the nodes connecting ED‐specific with general symptoms or with variables belonging to the external field; (3) a group of studies assessing treatment outcome in terms of the predictive role of central nodes, of changes in network connectivity between before and after treatment or through the use of the network intervention analysis. This last group of papers encompassed studies assessing the predicting value of network central nodes, studies evaluating the predictive value of network density and studies investigating treatment‐induced changes in the network structure.
The most central nodes reported in the present systematic review were those indicated by the authors in each selected article. Furthermore, when more networks were performed in the same study, we reported only results from the network including the highest number of nodes. Indeed, these more inclusive networks allow a better description of psychopathology (Fried & Cramer, 2017).
3.2. Diagnosis
Strength centrality is the most used (17 out of 25 studies) index to assess the centrality of nodes in the ED networks. It refers to the sum of the absolute edge weights between a focal node and all the other connected nodes in the network, quantifying how well a node is directly connected to other nodes (Epskamp et al., 2018). Another index (‘expected influence’), which accounts for negative edges referring to the sum of the values (+or ‐), has also been widely used (9 out of 25 studies). The accuracy of these estimates has been provided in terms of stability‐coefficient in 22 out of 23 studies. Considering these parameters, overvaluation of body shape and weight, dissatisfaction with body shape and weight and desire to lose weight were the most central nodes in ED networks. This finding has been largely replied across studies in all ED diagnoses, thus supporting the transdiagnostic theory of EDs (Fairburn et al., 2003). Indeed, these nodes appeared to be central in adult people with AN restricting type as well in those with AN binge‐purging type and in those with BN (Forrest et al., 2018). The same finding was detected in studies with mixed ED diagnostic groups (DuBois et al., 2017; Forbush et al., 2016), in that exploring differences among the main ED groups in adolescents (Goldschmidt et al., 2018) and in those comparing adolescents and adults with EDs (Calugi et al., 2020). These results highlight the central role of cognitive symptoms while behavioural symptoms (i.e., binging or purging) appear to be peripheral nodes in the ED networks. The transdiagnostic high centrality of overvaluation and dissatisfaction with body shape and weight was also confirmed in a large population with BED (Wang et al., 2019). The high replicability of these centrality data in people with EDs may be questioned in the light of the use of the Eating Disorders Examination Questionnaire (EDE‐Q) or interview, which was specifically developed from the cognitive behavioural model of EDs, in the majority of those studies. However, most of the networks including other psychometric assessment tools together with the EDE‐Q scores showed high centrality of overvaluation of body shape and weight (Forrest et al., 2019; Levinson et al., 2017; Meier et al., 2020; Smith et al., 2019, 2020) and high centrality of anxiety, depressive, obsessive‐compulsive or post‐traumatic stress disorder symptoms too. On the other hand, one study (Kerr‐Gaffney et al., 2020) showed that difficulties in social communications and isolation were core psychopathological symptoms in people with a current or past diagnosis of AN over and above shape and weight concerns. The high centrality of interpersonal difficulties has been highlighted also in other studies conducted in people with AN (Monteleone et al., 2019; Solmi et al., 2019) or in a mixed ED diagnostic group (Solmi et al., 2018). Furthermore, some studies identified also ineffectiveness feelings (Hilbert et al., 2020; Olatunji et al., 2018; Solmi et al., 2018; 2019; Vervaet et al., 2020), interoceptive awareness (Cascino et al., 2019; Olatunji et al., 2018; Solmi et al., 2018, 2019; Vervaet et al., 2020) or emotional regulation/internalising difficulties (Forrest et al., 2019; Levinson et al., 2017; Monteleone et al., 2019; Solmi et al., 2018, 2019; Vervaet et al., 2020) as central symptoms in ED networks. In most of these latter studies, drive to thinness as opposed to body dissatisfaction showed moderate‐high centrality and the Eating Disorder Inventory (EDI) instead of the EDE‐Q was employed. Thus, the inclusion of nodes representing the general psychopathology and not only the ED core psychopathology affects the centrality results of ED networks pointing to a high relevance of non ED‐specific core symptoms.
3.3. Comorbidity
Bridge centrality indicates a node's total connectivity with other communities (groups of symptoms that are very closely related). Therefore, the nodes with high bridge centrality are spreading activation of symptoms from one disorder to another and, thus, promote psychiatric comorbidity (Fried et al., 2017). The assessment of bridge symptoms in ED network studies has been conducted in 9 out of 15 studies, with the remaining ones exploring comorbidity in terms of the strongest edges between different cluster of symptoms or by visually inspecting the network structure. In people with AN, low self‐esteem was a node with high bridge centrality in several studies (Elliott et al., 2020; Forrest et al., 2019; Kerr‐Gaffney et al., 2020; Monteleone et al., 2019), while avoidance of social eating was a bridge symptom between anxiety and eating psychopathology (Elliott et al., 2020; Forrest et al., 2019; Kerr‐Gaffney et al., 2020). In samples with mixed ED diagnoses the replicability of the bridge centrality is highly affected by the type of nodes included in the network, which differed across studies. Indeed, Vanzhula et al. (2019) found that irritability, concentration problems, binge eating and desire for a flat stomach were the highest bridge nodes connecting Post‐Traumatic Stress Disorder (PTSD) and ED core symptoms, while Brown et al. (2020) identified body mistrust as the bridge symptom between ED psychopathology and variables describing the interoceptive function. Consistent with the latter study, another interoceptive symptom, pain tolerance, was found to bridge ED‐specific and suicidality symptoms (Smith et al., 2020). Studies assessing comorbidity without the bridge function analysis corroborated the role of low ability to discriminate physical sensation as the node connecting ED and general symptoms in networks conducted in people with BN (Levinson et al., 2017), AN (Cascino et al., 2019) or with mixed ED diagnoses (Smith et al., 2019). No study has investigated bridge symptoms in sample composed only of people with BN or BED.
3.4. External field
The external field is composed of conditions ‘that can influence symptoms from outside the network’ and that are ‘external relative to the psychopathology network, but not relative to the physical boundaries of the person’ (Borsboom, 2017). According to this definition, only few studies have been conducted in EDs exploring this dimension. One of these study (Monteleone et al., 2019) included in the network the five dimensions of maltreatment experienced in childhood, as assessed by the Childhood Trauma Questionnaire (Bernstein et al., 2003), and ED‐specific and anxiety symptoms. Emotional abuse was identified as the node connecting all types of early adverse experiences and psychopathology. Moreover, ineffectiveness and interoceptive awareness were identified in the shortest pathway between emotional abuse and drive to thinness or bulimic symptoms in people with AN restricting type and with AN purging type or BN, respectively. In accordance with this study, early maladaptive schema (over‐vigilance and inhibition of emotions and impaired autonomy and performance) were external field nodes resulting highly central in samples with mixed EDs (Vervaet et al., 2020), although their possible bridge role was not assessed. Another study (Monteleone, Corsi, et al., 2020) explored the connections of ED‐specific and affective symptoms with mentalizing and empathy, assessed through experimental tasks, and displayed emotional mental state inference and restraint as the bridge nodes between psychopathology and socio‐cognitive processes. This was the only study including data from multiple levels of assessment in an ED network. Finally, personality and identity variables were included in ED networks: trait characteristics resulted peripheral nodes in people with different ED diagnoses (Solmi et al., 2018, 2019; Vervaet et al., 2020) while feeling oneself through objective measures was a central node in people with AN (Cascino et al., 2019).
3.5. Outcome: central nodes, network connectivity, network intervention analysis
Four studies assessed treatment outcome in people with EDs by exploring the ability of the most central symptoms to predict the course of psychopathology (Borsboom, 2017). In a sample with mixed ED diagnoses, Olatunji et al. (2018) found that baseline ineffectiveness predicted BMI and depressed symptoms at discharge, while Brown et al. (2020) displayed that baseline stronger desire to lose weight was associated with lower likelihood to achieve remission at discharge. In people with AN, higher levels of the most central nodes (items related to the overvaluation of shape and weight) were related to poorer recovery and higher clinical impairment at 12 months follow‐up. Only one study (Hilbert et al., 2020) failed to identify a predictive role of the most central symptoms in people with BED undergoing an internet‐based CBT intervention.
Changes in the density (the sum of absolute values of all connections in the network) of the network before and after treatment have been suggested as a further method to employ network analysis to predict treatment outcome. A more dense network should predict higher vulnerability to the spread of symptom activation (Borsboom, 2017): in line with this hypothesis, a stronger connectivity has been found in an ED patients' network compared to a network of healthy students (Vanzhula et al., 2019). A comparison between pre‐ and post‐treatment network connectivity has been done through the network comparison test in two studies and revealed mixed results. Indeed, Smith et al. (2019) did not find significant differences between pre‐ and post‐treatment network connectivity in a population with mixed ED diagnoses, although patients with higher clinical improvement at the end of the treatment were those with lower density of the network at admission and at discharge. Contrary, Hilbert et al. (2020) identified a significant increase of network connectivity at the end of the treatment, without significant differences between the admission network and that computed at 6 months follow‐up.
Only one study has employed the network intervention analysis method. This is a novel procedure, which includes a dichotomous treatment variable in the network in order to investigate the sequential development and the order of treatment‐induced changes of specific symptoms and to highlight possible pathways through which the effects of treatment evolve (Blanken et al., 2019). A specific direct positive effect of the Recovery MANTRA intervention, in comparison to treatment as usual, has been found in people with AN on anxiety, shape concern and restraint at the end of the treatment but it did not persist at the follow‐up (Monteleone et al., 2020a).
4. DISCUSSION
This systematic review aimed to update the current knowledge of ED psychopathology and treatment deriving from the use of network analysis method in this field. The selected studies support the central role of overvaluation and concerns about body shape and weight and desire to lose weight across ages and ED diagnoses, in accordance with the transdiagnostic theory of EDs. In accordance with our hypothesis, non‐specific ED symptoms such as low self‐esteem, reduced interoceptive awareness and affective problems may also be suggested as central symptoms in ED psychopathology. Literature also provides evidence of a putative role of ineffectiveness as a psychopathological dimension promoting comorbidity between specific and general psychopathology in people with AN, while there is some evidence for a similar role also for interoceptive awareness in people with EDs as a unique diagnostic group. Despite the low number of studies using the network approach to assess treatment outcome, the hypothesised role of central nodes of the network as those predicting recovery may be suggested.
The network approach describes the nodes with high centrality as those maintaining psychopathology (Borsboom, 2017). The main and novel feature emerging from our review is that, although many network studies support the transdiagnostic theory of EDs (Fairburn, 2003), the centrality of overvaluation of body shape and weight and cognitive restraint should be accepted with caution. Indeed, this evidence arises from studies employing the EDEQ, a questionnaire designed on the cognitive‐behavioural model of EDs and including items that may overlap, as ascertained by the use of a network technique measuring the proportion of correlations shared by two items, the goldbricker function (Brown et al., 2020; Calugi et al., 2020; Elliott et al., 2020; Forrest et al., 2019; Kerr‐Gaffney et al., 2020; Meier et al., 2020). Studies exploring ED psychopathology through the EDI and those assessing non–ED‐specific psychopathological features highlight the centrality of other symptoms too, spanning ineffectiveness feelings, low interoceptive abilities and emotion regulation difficulties. Thus, network results are highly dependent on which variables are evaluated. This assumption is exemplified by the case of Vanzhula et al. (2019), who showed that binging had high centrality and bridge strength, given its specific connection with traumatic symptoms included in their network model, while in all the other ED networks it was a peripheral node. This limitation of network analyses is common to other statistical methods but may have contributed to the low reproducibility of network findings (Forbes et al., 2019). Only a few studies (Monteleone et al., 2019; Solmi et al., 2018; Vervaet et al., 2020) have included in their networks a broad range of general and ED‐specific symptoms, thus allowing to evaluate the centrality of each symptom taking into account the possible effect of all the internalizing symptoms which have been found associated to ED psychopathology (Marzola et al., 2020; Spindler & Milos, 2007). Therefore, this systematic review highlights the need in future studies for a theoretically driven selection of nodes, thus including general psychopathology and employing the suggested method (the goldbricker function) to ascertain the lack of overlapping between the network items and to inform their selection. In addition to these methodological issues, the results of our review highlight the likelihood to consider ineffectiveness, interoceptive awareness and affective problems as central symptoms together with overvaluation of body shape and weight.
The second major finding of this review is related to the evaluation of psychiatric comorbidity in EDs through the network approach, even if results cannot be considered conclusive because of the low number of studies employing the bridge function analysis to assess comorbidity. In people with AN, there is evidence to indicate ineffectiveness as the bridge node between specific and general psychopathology and avoidance of social eating as the bridge node between specific and anxiety symptoms. Furthermore, low interoceptive ability also seems to contribute to comorbidity, although this evidence was only partially drawn through bridge analysis. Ineffectiveness and interoceptive awareness were also nodes with high centrality in the ED networks: thus, they could be implicated in the maintenance of both ED and comorbid psychopathology and may be considered possible treatment targets, especially in the presence of psychiatric comorbidity. Future studies are recommended to evaluate the possible bridge role of affective regulation problems, which have shown high centrality in ED networks. More studies are also needed to explore the connections between psychopathology and the external field through network analysis, an area of investigation that has been already emphasised in EDs (Levinson et al., 2018; Smith et al., 2018). The findings of our review demonstrate that, so far, this area of investigation includes only two studies (Monteleone et al., 2019, 2020b) assessing the connection of ED psychopathology with childhood traumatic experiences or socio‐cognitive deficits and few studies investigating in terms of centrality the connection with personality dimensions (Solmi et al., 2018; Vervaet et al., 2020) and identity (Cascino et al., 2019).
This systematic review also aimed to assess the role of the network approach to predict treatment outcome in EDs. Of the three main approaches proposed to measure treatment outcome through network analysis (assessing the predictive role of central nodes on outcome, comparing network structure and connectivity before and after treatment, evaluating mechanisms of treatment‐induced changes) the reviewed literature supports the validity of the first one only. Indeed, three out of four studies (Brown et al., 2020; Elliott et al., 2020; Hilbert et al., 2020; Olatunji et al., 2018) identified a predictive role of the most central nodes on the treatment outcome. This result is consistent with the findings in a population of obese people, including individuals with BED, undergoing bariatric surgery (Monteleone et al., 2019b) and those in a mixed population composed of people with EDs and healthy peers (Levinson & Williams, 2020). Instead, more research is needed to clarify whether a high network connectivity at the end of treatment points to a treatment not sufficiently targeting the relationships between symptoms and, thus, may represent an index of vulnerability to relapse, or points to the result of a better understanding of the relationships between symptoms promoted by the treatment itself. Similarly, the network intervention approach showed a promising role of this technique to assess mechanisms of treatment‐induced changes (Monteleone et al., 2020a), but this evidence is far from being conclusive. This seems a missed opportunity given that this is a research area with high priority in EDs (Glashouwer et al., 2020; Pennesi & Wade, 2016).
Further limitations of the reviewed network analysis studies need also to be considered. First, none of the selected studies employed a directed network and used longitudinal data (as those deriving from the multiple ecological assessment): this has been done only in a recent study including participants at risk for ED onset (Levinson et al., 2020). In addition, the use of cross‐sectional data in concentration networks (consisting of undirected partial correlations) limits the possibility to draw definitive conclusions. Second, the mixed inclusion of psychometric items or sub‐item scores in the networks and the use of different psychometric assessment tools represent possible confounding factors to produce conclusive inferences.
4.1. Clinical implications and future directions
This is the first systematic review selecting a large number of studies employing network analysis in EDs. Following on from previous reviews of network analysis in EDs (Levinson et al., 2018; Smith et al., 2018), this systematic review highlights the possibility to include ineffectiveness, interoceptive ability and affective problems in addition to ED‐specific symptoms in the core psychopathology of AN, BN and, possibly, BED. This hypothesis should be verified in future network studies that are advised to include general psychopathology, in addition to eating‐specific psychopathology, and to exclude overlapping symptoms. Remarkably, the lack of network evaluation of other emerging EDs, such as the avoidant restrictive food intake disorder, as well as of network assessment of gender differences in EDs are missed opportunities. Furthermore, in the light of the possibility to conceptualise comorbidity in terms of bridge symptoms (Fried et al., 2017), our systematic review suggests that ineffectiveness and avoidance of social eating may respectively promote activation of general and anxiety symptom clusters in people with AN. Low interoceptive ability may also be hypothesised as a bridge symptom between general and ED‐specific psychopathology, while no studies exploring bridge nodes have been conducted separately in people with BN or with BED. These variables may represent novel treatment targets for comorbidity in EDs. Nonetheless, the findings of this work validate the use of therapeutic adjuncts to target not only ED‐specific symptoms, as occurring in effective ED treatments (i.e., the enhanced cognitive behavioural therapy (Fairburn et al., 2013) or the psychodynamic focal therapy for EDs (Zipfel et al., 2014)). However, in order to confirm the validity of the network approach in EDs, there is urgent need for studies exploring the effectiveness of treatments targeting central symptoms and their connections. Finally, future network research in EDs is recommended to fill in the revealed literature gap through the assessment of psychopathology connections with the external field, in particular in terms of the multilevel assessment data, considering other constructs and measures which have proved a significant impact on the clinical and behavioural profile of people with ED, such as personality traits, emotion regulation processes, quality of life, neuropsychological functioning and biological variables (such as genetics). Further fields worthy of investigation are the assessment of the longitudinal course of psychopathology in both group and individual networks in order to identify subgroups with more homogeneous network structures, the exploration of changes in network connectivity occurring after treatment and of its clinical meaning, and the study of mechanisms of treatment‐induced changes. All these areas may contribute to the advance of psychopathology and treatment knowledge in EDs.
REFERENCES
- Bernstein, D. P. , Stein, J. A. , Newcomb, M. D. , Walker, E. , Pogge, D. , Ahluvalia, T. , Stokes, J. , Handelsman, L. , Medrano, M. , Desmond, D. , & Zule, W. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27(2), 169–190. 10.1016/S0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- Blanken, T. F. , Deserno, M. K. , Dalege, J. , Borsboom, D. , Blanken, P. , Kerkhof, G. A. , & Cramer, A. O. (2018). The role of stabilizing and communicating symptoms given overlapping communities in psychopathology networks. Scientific Reports, 8(1), 1–8. 10.1038/s41598-018-24224-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanken, T. F. , Van Der Zweerde, T. , Van Straten, A. , Van Someren, E. J. W. , Borsboom, D. , & Lancee, J. (2019). Introducing network intervention analysis to investigate sequential, symptom‐specific treatment effects: A demonstration in Co‐occurring Insomnia and depression. Psychotherapy and Psychosomatics, 88(1), 55–57. 10.1159/000495045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom, D. (2017). A network theory of mental disorders. World Psychiatry, 16(1), 5–13. 10.1002/wps.20375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom, D. , & Cramer, A. O. J. (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9(1), 91–121. 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- Borsboom, D. , Cramer, A. O. J. , & Kalis, A. (2019). Brain disorders? Not really: Why network structures block reductionism in psychopathology research. Behavioral and Brain Sciences, 42, e2. 10.1017/S0140525X17002266 [DOI] [PubMed] [Google Scholar]
- Borsboom, D. , Cramer, A. O. J. , Schmittmann, V. D. , Epskamp, S. , & Waldorp, L. J. (2011). The small world of psychopathology. PloS One, 6(11), e27407. 10.1371/journal.pone.0027407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boschloo, L. , van Borkulo, C. D. , Rhemtulla, M. , Keyes, K. M. , Borsboom, D. , & Schoevers, R. A. (2015). The network structure of symptoms of the diagnostic and statistical manual of mental disorders. PloS One, 10(9), e0137621. 10.1371/journal.pone.0137621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, T. A. , Vanzhula, I. A. , Reilly, E. E. , Levinson, C. A. , Berner, L. A. , Krueger, A. , Lavender, J. M. , Kaye, W. H. , & Wierenga, C. E. (2020). Body mistrust bridges interoceptive awareness and eating disorder symptoms. Journal of Abnormal Psychology, 129(5), 445–456. 10.1037/abn0000516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calugi, S. , Sartirana, M. , Misconel, A. , Boglioli, C. , & Dalle Grave, R. (2020). Eating disorder psychopathology in adults and adolescents with anorexia nervosa: A network approach. International Journal of Eating Disorders, 53(5), 690–701. 10.1002/eat.23270 [DOI] [PubMed] [Google Scholar]
- Cascino, G. , Castellini, G. , Stanghellini, G. , Ricca, V. , Cassioli, E. , Ruzzi, V. , Monteleone, P. , & Monteleone, A. M. (2019). The role of the embodiment disturbance in the anorexia nervosa psychopathology: A network analysis study. Brain Sciences, 9(10), 276. 10.3390/brainsci9100276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuBois, R. H. , Rodgers, R. F. , Franko, D. L. , Eddy, K. T. , & Thomas, J. J. (2017). A network analysis investigation of the cognitive‐behavioral theory of eating disorders. Behaviour Research and Therapy, 97, 213–221. 10.1016/j.brat.2017.08.004 [DOI] [PubMed] [Google Scholar]
- Elliott, H. , Jones, P. J. , & Schmidt, U. (2020). Central symptoms predict posttreatment outcomes and clinical impairment in anorexia nervosa: A network analysis. Clinical Psychological Science, 8, 139–154. 10.1177/2167702619865958 [DOI] [Google Scholar]
- Epskamp, S. , Borsboom, D. , & Fried, E. I. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behaviour Research Methods, 50(1), 195–212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn, C. G. , Cooper, Z. , Doll, H. A. , O'Connor, M. E. , Palmer, R. L. , & Dalle Grave, R. (2013). Enhanced cognitive behaviour therapy for adults with anorexia nervosa: A UK‐Italy study. Behaviour Research and Therapy, 51, R2–R8. 10.1016/j.brat.2012.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn, C. G. , Cooper, Z. , & Shafran, R. (2003). Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behaviour Research and Therapy, 41(5), 509–528. 10.1016/S0005-7967(02)00088-8 [DOI] [PubMed] [Google Scholar]
- Forbes, M. K. , Wright, A. G. C. , Markon, K. E. , & Krueger, R. F. (2019). The network approach to psychopathology: Promise versus reality. World Psychiatry, 18(3), 272–273. 10.1002/wps.20659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbush, K. T. , Siew, C. S. Q. , & Vitevitch, M. S. (2016). Application of network analysis to identify interactive systems of eating disorder psychopathology. Psychological Medicine, 46(12), 2667–2677. 10.1017/S003329171600012X [DOI] [PubMed] [Google Scholar]
- Forrest, L. N. , Jones, P. J. , Ortiz, S. N. , & Smith, A. R. (2018). Core psychopathology in anorexia nervosa and bulimia nervosa: A network analysis. International Journal of Eating Disorders, 51(7), 668–679. 10.1002/eat.22871 [DOI] [PubMed] [Google Scholar]
- Forrest, L. N. , Sarfan, L. D. , Ortiz, S. N. , Brown, T. A. , & Smith, A. R. (2019). Bridging eating disorder symptoms and trait anxiety in patients with eating disorders: A network approach. International Journal of Eating Disorders, 52(6), eat.23070. 10.1002/eat.23070 [DOI] [PubMed] [Google Scholar]
- Fried, E. I. , & Cramer, A. O. J. (2017). Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science, 12(6), 999–1020. 10.1177/1745691617705892 [DOI] [PubMed] [Google Scholar]
- Fried, E. I. , van Borkulo, C. D. , Cramer, A. O. J. , Boschloo, L. , Schoevers, R. A. , & Borsboom, D. (2017). Mental disorders as networks of problems: A review of recent insights. Social Psychiatry and Psychiatric Epidemiology, 52(1), 1–10. 10.1007/s00127-016-1319-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glashouwer, K. A. , Brockmeyer, T. , Cardi, V. , Jansen, A. , Murray, S. B. , Blechert, J. , Levinson, C. A. , Schmidt, U. , Tchanturia, K. , Wade, T. D. , Svaldi, J. , Giel, K. E. , Favaro, A. , Fernández‐Aranda, F. , Friederich, H. C. , Naumann, E. , Treasure, J. L. , Tuschen‐Caffier, B. , Vocks, S. , & Werthmann, J. (2020). Time to make a change: A call for more experimental research on key mechanisms in anorexia nervosa. European Eating Disorders Review, 28(4), 361–367. 10.1002/erv.2754 [DOI] [PubMed] [Google Scholar]
- Goldschmidt, A. B. , Crosby, R. D. , Cao, L. , Moessner, M. , Forbush, K. T. , Accurso, E. C. , & Le Grange, D. (2018). Network analysis of pediatric eating disorder symptoms in a treatment‐seeking, transdiagnostic sample. Journal of Abnormal Psychology, 127(2), 251–264. 10.1037/abn0000327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbert, A. , Herpertz, S. , Zipfel, S. , Tuschen‐Caffier, B. , Friederich, H.‐C. , Mayr, A. , & de Zwaan, M. (2020). Psychopathological networks in cognitive‐behavioral treatments for binge‐eating disorder. Psychotherapy and Psychosomatics, 89(6), 1–7. 10.1159/000509458 [DOI] [PubMed] [Google Scholar]
- Insel, T. , Cuthbert, B. , Garvey, M. , Heinssen, R. , Pine, D. S. , Quinn, K. , Sanislow, C. , & Wang, P. (2010). Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. The American Journal of Psychiatry, 167(7), 748–751. 10.1176/appi.ajp.2010.09091379 [DOI] [PubMed] [Google Scholar]
- Jones, P. J. , Ma, R. , & McNally, R. J. (2019). Bridge centrality: A network approach to understanding comorbidity. Multivariate Behavioral Research, 1–15. 10.1080/00273171.2019.1614898 [DOI] [PubMed] [Google Scholar]
- Kan, C. , Cardi, V. , Stahl, D. , & Treasure, J. (2019). Precision psychiatry‐What it means for eating disorders? European Eating Disorders Review, 27(1), 3–7. 10.1002/erv.2651 [DOI] [PubMed] [Google Scholar]
- Kerr‐Gaffney, J. , Halls, D. , Harrison, A. , & Tchanturia, K. (2020). Exploring relationships between autism spectrum disorder symptoms and eating disorder symptoms in adults with anorexia nervosa: A network approach. Frontiers in Psychiatry, 11, 401. 10.3389/fpsyt.2020.00401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson, C. A. , Vanzhula, I. A. , Brosof, L. C. , & Forbush, K. (2018). Network analysis as an alternative approach to conceptualizing eating disorders: Implications for research and treatment. Current Psychiatry Reports, 20(9), 67. 10.1007/s11920-018-0930-y [DOI] [PubMed] [Google Scholar]
- Levinson, C. A. , Vanzhula, I. A. , Smith, T. W. , & Stice, E. (2020). Group and longitudinal intra‐individual networks of eating disorder symptoms in adolescents and young adults at‐risk for an eating disorder. Behaviour Research and Therapy, 135, 103731. 10.1016/j.brat.2020.103731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson, C. A. , & Williams, B. M. (2020). Eating disorder fear networks: Identification of central eating disorder fears. International Journal of Eating Disorders, 52(12), eat.23382. 10.1002/eat.23382 [DOI] [PubMed] [Google Scholar]
- Levinson, C. A. , Zerwas, S. , Calebs, B. , Forbush, K. , Kordy, H. , Watson, H. , Hofmeier, S. , Levine, M. , Crosby, R. D. , Peat, C. , Runfola, C. D. , Zimmer, B. , Moesner, M. , Marcus, M. D. , & Bulik, C. M. (2017). The core symptoms of bulimia nervosa, anxiety, and depression: A network analysis. Journal of Abnormal Psychology, 126(3), 340–354. 10.1037/abn0000254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzola, E. , Porliod, A. , Panero, M. , De‐Bacco, C. , & Abbate‐Daga, G. (2020). Affective temperaments and eating psychopathology in anorexia nervosa: Which role for anxious and depressive traits? Journal of Affective Disorders, 266, 374–380. 10.1016/j.jad.2020.01.142 [DOI] [PubMed] [Google Scholar]
- McNally, R. J. (2016). Can network analysis transform psychopathology? Behaviour Research and Therapy, 86, 95–104. 10.1016/j.brat.2016.06.006 [DOI] [PubMed] [Google Scholar]
- Meier, M. , Kossakowski, J. J. , Jones, P. J. , Kay, B. , Riemann, B. C. , & McNally, R. J. (2020). Obsessive‐compulsive symptoms in eating disorders: A network investigation. International Journal of Eating Disorders, 53(3), 362–371. 10.1002/eat.23196 [DOI] [PubMed] [Google Scholar]
- Moher, D. , Hopewell, S. , Schulz, K. F. , Montori, V. , Gøtzsche, P. C. , Devereaux, P. J. , Elbourne, D. , Egger, M. , & Altman, D. G. (2010). CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. InternationalJournal of Surgery, 10(1), 340. 10.1136/bmj.c869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteleone, A. M. , Cardi, V. , Ambwani, S. , Cascino, G. , Albano, G. , Pellegrino, F. , & Treasure, J. (2020). Network intervention analysis to assess the trajectory of change and treatment effects associated with the use of online guided self‐help for anorexia nervosa. Early Intervention in Psychiatry, eip.13064. 10.1111/eip.13064 [DOI] [PubMed] [Google Scholar]
- Monteleone, A. M. , Cascino, G. , Pellegrino, F. , Ruzzi, V. , Patriciello, G. , Marone, L. , De Felice, G. , Monteleone, P. , & Maj, M. (2019). The association between childhood maltreatment and eating disorder psychopathology: A mixed‐model investigation. European Psychiatry, 61, 111–118. 10.1016/j.eurpsy.2019.08.002 [DOI] [PubMed] [Google Scholar]
- Monteleone, A. M. , Cascino, G. , Solmi, M. , Pirozzi, R. , Tolone, S. , Terracciano, G. , Parisi, S. , Cimino, M. , Monteleone, P. , Maj, M. , & Docimo, L. (2019). A network analysis of psychological, personality and eating characteristics of people seeking bariatric surgery: Identification of key variables and their prognostic value. Journal of Psychosomatic Research, 120, 81–89. 10.1016/j.jpsychores.2019.03.010 [DOI] [PubMed] [Google Scholar]
- Monteleone, A. M. , Corsi, E. , Cascino, G. , Ruzzi, V. , Ricca, V. , Ashworth, R. , Bird, G. , & Cardi, V. (2020). The interaction between mentalizing, empathy and symptoms in people with eating disorders: A network analysis integrating experimentally induced and self‐report measures. Cognitive Therapy and Research, 44(6), 1140–1149. 10.1007/s10608-020-10126-z [DOI] [Google Scholar]
- Monteleone, A. M. , Mereu, A. , Cascino, G. , Criscuolo, M. , Castiglioni, M. C. , Pellegrino, F. , Patriciello, G. , Ruzzi, V. , Monteleone, P. , Vicari, S. , & Zanna, V. (2019). Re‐conceptualization of anorexia nervosa psychopathology: A network analysis study in adolescents with short duration of the illness. International Journal of Eating Disorders, 52(11), 1263–1273. 10.1002/eat.23137 [DOI] [PubMed] [Google Scholar]
- Murray, S. B. , Loeb, K. L. , & Le Grange, D. (2018). Treatment outcome reporting in anorexia nervosa: Time for a paradigm shift? Journal of Eating Disorders 6(1), 10. 10.1186/s40337-018-0195-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray, S. B. , Quintana, D. S. , Loeb, K. L. , Griffiths, S. , & Le Grange, D. (2019). Treatment outcomes for anorexia nervosa: A systematic review and meta‐analysis of randomized controlled trials. Psychological medicine, 49(4), 535–544. 10.1017/S0033291718002088 [DOI] [PubMed] [Google Scholar]
- Olatunji, B. O. , Levinson, C. , & Calebs, B. (2018). A network analysis of eating disorder symptoms and characteristics in an inpatient sample. Psychiatry Research, 262, 270–281. 10.1016/J.PSYCHRES.2018.02.027 [DOI] [PubMed] [Google Scholar]
- Pennesi, J.‐L. , & Wade, T. D. (2016). A systematic review of the existing models of disordered eating: Do they inform the development of effective interventions? Clinical psychology review, 43, 175–192, 10.1016/j.cpr.2015.12.004 [DOI] [PubMed] [Google Scholar]
- Rodgers, R. F. , DuBois, R. , Thiebaut, S. , Jaussent, I. , Maimoun, L. , Seneque, M. , Lefebvre, P. , Renard, E. , Courtet, P. , & Guillaume, S. (2019). Structural differences in eating disorder psychopathology after history of childhood abuse: Insights from a Bayesian network analysis. Journal of Abnormal Psychology. 128(8), 795–805. 10.1037/abn0000470 [DOI] [PubMed] [Google Scholar]
- Smith, A. R. , Forrest, L. N. , Duffy, M. E. , Jones, P. J. , Joiner, T. E. , & Pisetsky, E. M. (2020). Identifying bridge pathways between eating disorder symptoms and suicidal ideation across three samples. Journal of Abnormal Psychology, 129(7), 724–736. 10.1037/abn0000553 [DOI] [PubMed] [Google Scholar]
- Smith, K. E. , Crosby, R. D. , Wonderlich, S. A. , Forbush, K. T. , Mason, T. B. , & Moessner, M. (2018). Network analysis: An innovative framework for understanding eating disorder psychopathology. International Journal of Eating Disorders, 51(3), 214–222. 10.1002/eat.22836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, K. E. , Mason, T. B. , Crosby, R. D. , Cao, L. , Leonard, R. C. , Wetterneck, C. T. , Smith, B. E. R. , Farrell, N. R. , Riemann, B. C. , Wonderlich, S. A. , & Moessner, M. (2019). A comparative network analysis of eating disorder psychopathology and co‐occurring depression and anxiety symptoms before and after treatment. Psychological Medicine, 49(2), 314–324. 10.1017/S0033291718000867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solmi, M. , Collantoni, E. , Meneguzzo, P. , Degortes, D. , Tenconi, E. , & Favaro, A. (2018). Network analysis of specific psychopathology and psychiatric symptoms in patients with eating disorders. International Journal of Eating Disorders, 51(7), 680–692. 10.1002/eat.22884 [DOI] [PubMed] [Google Scholar]
- Solmi, M. , Collantoni, E. , Meneguzzo, P. , Tenconi, E. , & Favaro, A. (2019). Network analysis of specific psychopathology and psychiatric symptoms in patients with anorexia nervosa. European Eating Disorders Review, 27(1), 24–33. 10.1002/erv.2633 [DOI] [PubMed] [Google Scholar]
- Spindler, A. , & Milos, G. (2007). Links between eating disorder symptom severity and psychiatric comorbidity. Eating Behaviors, 8(3), 364–373. 10.1016/j.eatbeh.2006.11.012 [DOI] [PubMed] [Google Scholar]
- Treasure, J. , Duarte, T. A. , & Schmidt, U. (2020).Eating disorders. The Lancet, 395(10227), 899–911, 10.1016/S0140-6736(20)30059-3 [DOI] [PubMed] [Google Scholar]
- Treasure, J. , Willmott, D. , Ambwani, S. , Cardi, V. , Clark Bryan, D. , Rowlands, K. , & Schmidt, U. (2020). Cognitive interpersonal model for anorexia nervosa revisited: The perpetuating factors that contribute to the development of the severe and enduring illness. Journal of Clinical Medicine, 9(3), 630. 10.3390/jcm9030630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Borkulo, C. , Epskamp, S. , Jones, P. A. , Haslbeck, J. , & Millner, A. J. (2019). Package 'NetworkComparisonTest': Statistical comparison of two networks based on three invariance measures. R package. Version 2.2.1. Retrieved from https://cran.r‐project.org/web/packages/NetworkComparisonTest/NetworkComparisonTest.pdf [Google Scholar]
- Vanzhula, I. A. , Calebs, B. , Fewell, L. , & Levinson, C. A. (2019). Illness pathways between eating disorder and post‐traumatic stress disorder symptoms: Understanding comorbidity with network analysis. European Eating Disorders Review, 27(2), 147–160. 10.1002/erv.2634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vervaet, M. , Puttevils, L. , Hoekstra, R. , Fried, E. , & Vanderhasselt, M. A. (2020). Transdiagnostic vulnerability factors in eating disorders: A network analysis. European eating disorders review. 29(1), 86–100. 10.1002/erv.2805 [DOI] [PubMed] [Google Scholar]
- Wang, S. B. , Jones, P. J. , Dreier, M. , Elliott, H. , & Grilo, C. M. (2019). Core psychopathology of treatment‐seeking patients with binge‐eating disorder: A network analysis investigation. Psychological Medicine, 49(11), 1923–1928. 10.1017/S0033291718002702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zipfel, S. , Wild, B. , Groß, G. , Friederich, H.‐C. , Teufel, M. , Schellberg, D. , Giel, K. E. , de Zwaan, M. , Dinkel, A. , Herpertz, S. , Burgmer, M. , Löwe, B. , Tagay, S. , von Wietersheim, J. , Zeeck, A. , Schade‐Brittinger, C. , Schauenburg, H. , & Herzog, W. , & ANTOP study group. (2014). Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): Randomised controlled trial. The Lancet, 383(9912), 127–137. 10.1016/S0140-6736(13)61746-8 [DOI] [PubMed] [Google Scholar]


