Abstract
Aim
To evaluate the efficacy and safety of ultra rapid lispro (URLi) versus lispro (Humalog®) in people with type 1 diabetes on continuous subcutaneous insulin infusion (CSII).
Materials and Methods
This was a phase 3, 16‐week, treat‐to‐target study in patients randomized to double‐blind URLi (N = 215) or lispro (N = 217). The primary endpoint was change from baseline HbA1c (non‐inferiority margin 4.4 mmol/mol [0.4%]), with multiplicity‐adjusted objectives for postprandial glucose (PPG) levels during a meal test, and time spent in the target range 70–180 mg/dL (TIR).
Results
URLi was non‐inferior to lispro for change in HbA1c, with a least‐squares mean (LSM) difference of 0.3 mmol/mol (95% confidence interval [CI] –0.6, 1.2) or 0.02% (95% CI –0.06, 0.11). URLi was superior to lispro in controlling 1‐ and 2‐h PPG levels after the meal test: LSM difference −1.34 mmol/L (95% CI –2.00, −0.68) or −24.1 mg/dL (95% CI –36.0, −12.2) at 1 h and −1.54 mmol/L (95% CI –2.37, −0.72) or −27.8 mg/dL (95% CI –42.6, −13.0) at 2 h; both p < .001. TIR and time in hyperglycaemia were similar between groups but URLi resulted in significantly less time in hypoglycaemia (<3.0 mmol/L [54 mg/dL]) over the daytime, night‐time and 24‐h period: LSM difference −0.41%, −0.97% and −0.52%, respectively, all p < .05. The incidence of treatment‐emergent adverse events was higher with URLi (60.5% vs. 44.7%), driven by infusion‐site reaction and infusion‐site pain, which was mostly mild or moderate. Rates of severe hypoglycaemia and diabetic ketoacidosis were similar between groups.
Conclusions
URLi was efficacious, providing superior PPG control and less time in hypoglycaemia but with more frequent infusion‐site reactions compared with lispro when administered by CSII.
Keywords: continuous glucose monitoring, continuous subcutaneous insulin infusion, insulin analogues, type 1 diabetes
1. INTRODUCTION
Achieving glycaemic goals remains challenging for most people living with diabetes, despite advances in the therapies and technologies that manage and control hyperglycaemia. 1 , 2 , 3 , 4 Continuous subcutaneous insulin infusion (CSII) or insulin pump therapy is an advanced method of insulin administration that has the potential to improve glycaemic control compared with multiple daily injection (MDI) 5 , 6 regimens. Glycaemic control might be further enhanced by combining CSII with an insulin that has pharmacokinetic (PK) and pharmacodynamic (PD) profiles that more closely match physiological insulin secretion and therefore reduce postprandial glucose (PPG) excursions without increasing hypoglycaemia risk.
A number of ultrarapid‐acting insulins that demonstrate improved PK/PD profiles have been developed for both MDI and CSII use, including ultra rapid lispro (URLi). URLi is a novel ultrarapid formulation of insulin lispro that utilizes two enabling excipients, citrate and treprostinil, to accelerate insulin lispro absorption and the insulin time‐action profile. In a pooled analysis comparing PK/PD between URLi and lispro (Humalog) following subcutaneous injection, URLi showed a faster onset of appearance, greater early insulin exposure, and an earlier glucose‐lowering effect. 7 On glycaemic control, URLi was non‐inferior to lispro for change from baseline HbA1c and was superior in reducing 1‐ and 2‐h PPG excursions during a meal test in patients with type 1 diabetes (T1D) on MDI therapy (PRONTO‐T1D). 8 Accelerated absorption and improved PPG control were also demonstrated when URLi was administered via CSII in adults with T1D 9 and its compatibility with CSII use has also been shown. 10
The aim of this study was to show that URLi was non‐inferior to lispro (Humalog) on glycaemic control as measured by change from baseline to week 16 in HbA1c in people with T1D using CSII.
2. MATERIALS AND METHODS
2.1. Study design
In this phase 3, double‐blind, active‐controlled, treat‐to‐target trial, adults with T1D were randomized to URLi or lispro as both basal and bolus insulin delivered via CSII. The study included a screening (1 week) and lead‐in period (2 weeks) prior to randomization, followed by a 16‐week treatment phase and a 4‐week safety follow‐up (Figure S1 ).
The study was conducted at 83 sites in 10 countries and in accordance with the Declaration of Helsinki, the International Conference on Harmonization guidelines for Good Clinical Practice, and applicable laws and regulations in the respective countries. All procedures were approved by an independent ethics committee and all participants provided written, informed consent prior to participating in the study.
2.2. Participants
Adults (aged ≥18 years) with T1D, HbA1c 47.5–74.9 mmol/mol (6.5%–9.0%) and a body mass index (BMI) of 35.0 kg/m2 or less were eligible for inclusion if they had been using CSII therapy for 6 months or longer (specifically MiniMed 530G, Paradigm Revel, MiniMed 630G, MiniMed 640G or Paradigm Veo for ≥90 days) and had been treated for at least 30 days with less than 100 units/day of a rapid‐acting insulin analogue (insulin lispro, aspart or glulisine).
Patients were excluded if they had experienced more than one episode of severe hypoglycaemia or more than one emergency room visit/hospitalization as a result of poor glucose control (hyperglycaemia or diabetic ketoacidosis) within the 6 months prior to screening, or if they received any oral or injectable medication for diabetes other than rapid‐acting insulin analogue via CSII in the 90 days prior to screening. Full inclusion and exclusion criteria are listed in Table S1.
2.3. Interventions and randomization
At the start of lead‐in, patients were switched from their rapid‐acting insulin analogue to lispro. After lead‐in, patients were randomized 1:1 to URLi or lispro, both 100 U/mL and administered via CSII, with bolus doses delivered 0 to 2 min prior to the start of each meal. Assignment to treatment groups was determined by a computer‐generated random sequence using an interactive web‐response system and stratified by country, HbA1c stratum (≤58.5 mmol/mol [7.5%], >58.5 mmol/mol at screening), and use of personal continuous glucose monitoring (CGM) or flash glucose monitoring (FGM) during the study (yes/no). Patients used their protocol‐allowed personal insulin pumps for the duration of the study but used study‐provided reservoirs and infusion sets. Routine/planned infusion‐set changes were required every 3 days, with the reasons for any unplanned changes being documented.
2.4. Self‐monitoring of blood glucose
Patients were supplied with a Contour Next Link (Ascensia Diabetes Care) blood glucose (BG) meter that was used to collect 10‐point self‐monitoring of blood glucose (SMBG) profiles on 3 consecutive days during the 2 weeks prior to randomization, week 4, and week 16. Additional BG values, including occasional recordings at 3:00 am, were collected to inform clinical management.
2.5. Dose titration
During the study, insulin doses were adjusted in a treat‐to‐target manner to SMBG levels of 4.4–6.1 mmol/L (80–110 mg/dL) fasting or premeal, 5.0–7.2 mmol/L (90–130 mg/dL) prebedtime, and less than 10.0 mmol/L (180 mg/dL) 1–2‐h postprandial. Adjustment of basal rates was based on BG values, hypoglycaemia data, and was determined by the investigator in discussion with the patient, in order to reach fasting BG targets and to optimize 24‐h basal rates. Premeal and PPG levels from 10‐ and 7‐point SMBG profiles were evaluated by the investigator for bolus dose titration. Bolus calculator settings (carbohydrate ratio [CR], insulin sensitivity factor [ISF] and active insulin time) were to be adjusted weekly to meet target glucose levels, and patients used the pump's bolus calculator to determine all meal and correction bolus doses. Full details regarding basal and bolus dose titration can be found in Table S2.
2.6. Continuous glucose monitoring
Patients were able to continue using their personal CGM/FGM during the study, but they were not allowed to initiate personal CGM/FGM after enrolment. Personal CGM/FGM could be used for the required glucose value entries into the pump bolus calculator for meal and correction boluses. If applicable, patients could use the ‘low glucose suspend’ pump feature, but not the ‘suspend before low’ feature.
The Dexcom G5 Mobile CGM System (DexCom Inc.; CA, USA) was used by all patients, in blinded mode, 14 days prior to randomization (week 0), week 8, and week 16. Patients were instructed to change the G5 sensor every 7 days as per the product label and to calibrate it every 12 h using the study‐provided BG meter.
2.7. Mixed meal tolerance test
A 4‐h standardized liquid mixed meal tolerance test ([MMTT] Ensure Plus; Abbott Nutrition, OH, USA) was performed at baseline (all patients on lispro) and at week 16 to assess PPG levels. Patients were required to have a fasting BG level of 4.0–10.0 mmol/L (71–180 mg/dL) prior to starting the MMTT and to consume the meal within 15 min. Serum glucose measurements were collected at time −15, 0, 15, 30, 60, 120, 180 and 240 min relative to meal start. Insulin dose during MMTT was individualized for each patient based on morning meal CR and ISF.
2.8. Assessments
The primary endpoint was non‐inferiority of URLi to lispro for HbA1c change from baseline to week 16.
Key secondary endpoints (multiplicity‐adjusted objectives) included superiority of URLi to lispro in: 1‐ and 2‐h PPG during MMTT; change from baseline to week 16 in HbA1c; duration of time with sensor glucose in target range 70–180 mg/dL (TIR) during the daytime (6:00 am to midnight) and 24‐h period with blinded CGM.
2.9. Statistical methods
A non‐inferiority margin of 4.4 mmol/mol (0.4%) was prespecified for the primary efficacy measure. Two analysis methods were employed: (a) the primary analysis model, a mixed‐effects model for repeated measures (MMRM) analysis in the efficacy estimand, which included all on‐investigational product (IP) data from randomization to week 16; and (b) a supportive ANCOVA analysis with multiple imputation using ‘return to baseline’ for missing data in the intention‐to‐treat (ITT) estimand including all data from randomization to week 16 regardless of IP use. Superiority of URLi to lispro for change in HbA1c was assessed using the same primary and supportive analysis models.
A graphical approach for multiple comparisons 11 , 12 (Figure S2) was used to strongly control the overall type I error (two‐sided alpha level of .05) for testing the treatment effect for the primary and multiplicity‐adjusted objectives.
Safety analyses were conducted on all randomized patients who received one or more doses of IP. Patient‐reported adverse events (including serious adverse events [SAEs] and treatment‐emergent adverse events [TEAEs]) were summarized by preferred term and/or system organ class using the Medical Dictionary for Drug Regulatory Activities (MedDRA) version 21.0. Severe hypoglycaemia, defined as an episode requiring assistance because of neurological impairment as confirmed by the investigator, was reported as an SAE.
It was estimated that 420 randomized patients would provide 99% statistical power to show non‐inferiority of URLi to lispro for change in HbA1c with assumptions of no difference between treatments, a standard deviation of 0.88%, at two‐sided α‐level .05, and 12% dropout rate.
3. RESULTS
A total of 432 patients were randomized to URLi (n = 215) and lispro (n = 217) with 94.7% of patients completing the 16‐week study and 92.6% completing 16 weeks of study treatment (Figure S3). Demographic and baseline characteristics were similar between groups (Table 1).
TABLE 1.
Baseline characteristics
| Lispro N = 217 | URLi N = 215 | Overall N = 432 | |
|---|---|---|---|
| Age (years), mean (SD) | 44.7 (14.9) | 48.2 (15.4) | 46.4 (15.3) |
| Men, % | 45.2 | 44.2 | 44.7 |
| Race, n (%) | |||
| American Indian or Alaska Native | 0 (0.0) | 2 (0.9) | 2 (0.5) |
| Asian | 0 (0.0) | 2 (0.9) | 2 (0.5) |
| Black or African American | 6 (2.8) | 7 (3.3) | 13 (3.0) |
| Multiple | 1 (0.5) | 0 (0.0) | 1 (0.2) |
| Native Hawaiian or other Pacific Islander | 1 (0.5) | 0 (0.0) | 1 (0.2) |
| Not reported | 2 (0.9) | 2 (0.9) | 4 (0.9) |
| White | 207 (95.4) | 202 (94.0) | 409 (94.7) |
| Hispanic or Latino, n (%) | 17 (7.8) | 18 (8.4) | 35 (8.1) |
| Weight (kg), mean (SD) | 79.3 (15.1) | 78.5 (15.1) | 78.9 (15.1) |
| BMI (kg/m2), mean (SD) | 27.2 (4.1) | 27.0 (4.0) | 27.1 (4.0) |
| Duration of diabetes (years), mean (SD) | 25.4 (13.2) | 25.9 (12.6) | 25.6 (12.9) |
| Duration of CSII use (years), mean (SD) | 8.7 (7.9) | 10.2 (9.0) | 9.5 (8.5) |
| Prandial insulin at study entry, n (%) | |||
| Insulin aspart | 126 (58.1) | 108 (50.2) | 234 (54.2) |
| Insulin glulisine | 0 (0.0) | 5 (2.3) | 5 (1.2) |
| Insulin lispro | 91 (41.9) | 102 (47.4) | 193 (44.7) |
| Total daily insulin dose, mean (SD) | |||
| Units | 47.2 (20.5) | 46.7 (20.0) | 47.0 (20.2) |
| Units/kg | 0.59 (0.20) | 0.59 (0.21) | 0.59 (0.20) |
| Personal CGM/FGM use, n (%) | 124 (57.1) | 125 (58.1) | 249 (57.6) |
| Use of low glucose suspend, n (%) | 35 (16.3) | 38 (17.7) | 73 (17.0) |
| HbA1c at study entry, mean (SD) | |||
| % | 7.71 (0.63) | 7.69 (0.62) | 7.70 (0.63) |
| Mmol/mol | 60.7 (6.9) | 60.5 (6.8) | 60.6 (6.8) |
| HbA1c at baseline, mean (SD) | |||
| % | 7.54 (0.58) | 7.56 (0.59) | 7.55 (0.58) |
| Mmol/mol | 58.9 (6.3) | 59.1 (6.5) | 59.0 (6.4) |
Abbreviations: BMI, body mass index; CGM, continuous glucose monitoring; CSII, continuous subcutaneous insulin infusion; FGM, flash glucose monitoring; SD, standard deviation.
3.1. Efficacy
3.1.1. HbA1c
Mean HbA1c improved in both groups during the 2‐week lead‐in period from 60.6 mmol/mol (7.70%) to 59.1 mmol/mol (7.56%) in the URLi group and 58.9 mmol/mol (7.54%) in the lispro group. There was a further improvement in the first 8 weeks after randomization, after which HbA1c increased slightly in both groups before stabilizing to 58.3 mmol/mol (7.48%) for URLi and 58.0 mmol/mol (7.46%) for lispro by week 16 (Figure 1). Non‐inferiority of URLi to lispro was confirmed with a least‐squares mean (LSM) difference of 0.3 mmol/mol (95% CI –0.6; 1.2) or 0.02% (95% CI –0.06; 0.11) (Figure 1). Similar results were observed in the supportive analysis using the ITT estimand. Superiority of URLi to lispro for change in HbA1c was not achieved with either analysis.
FIGURE 1.
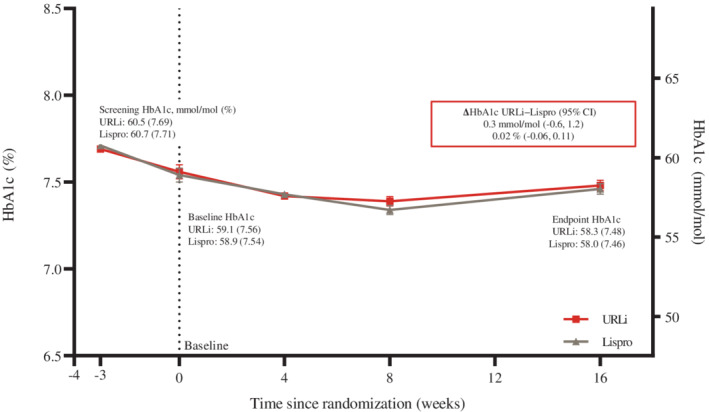
Mean HbA1c from study entry to week 16. Data are mean at study entry and LSM ± SE at all other time points and based on the MMRM analysis. LSM difference between URLi and lispro (URLi−lispro) was 0.3 mmol/mol (95% CI –0.6, 1.2) or 0.02% (−0.06, 0.11) with the MMRM analysis and 0.3 mmol/mol (95% CI –0.6, 1.2) or 0.03% (95% CI –0.05, 0.11) with the supportive ANCOVA analysis. Both analysis models included treatment, strata (pooled country and patient's personal CGM/FGM use during the study [yes/no]) and the fixed covariate of baseline HbA1c. The MMRM model also included visit, treatment‐by‐visit interaction and an unstructured covariance structure. ANCOVA, analysis of covariance; CGM, continuous glucose monitoring; CI, confidence interval; FGM, flash glucose monitoring; LSM, least squares mean; MMRM, mixed‐effects model for repeated measures; SE, standard error
At week 16, 18.9% of patients in the URLi group and 20.8% in the lispro group reached target HbA1c of less than 53.0 mmol/mol (7.0%), and 4.2% and 4.4% achieved an HbA1c of 47.5 mmol/mol (6.5%) or less, respectively.
3.1.2. MMTT at week 16
URLi showed superiority to lispro in controlling 1‐ and 2‐h PPG levels during the 4‐h MMTT (Figure 2A): LSM difference −1.34 mmol/L (−24.1 mg/dL) and −1.54 mmol/L (−27.8 mg/dL) (both p < .001) at 1‐ and 2‐h postmeal, respectively. Treatment with URLi resulted in significantly lower PPG levels at all time points from 30 min to 3 h and excursions from 15 min to 3 h (Figure 2A,B).
FIGURE 1.
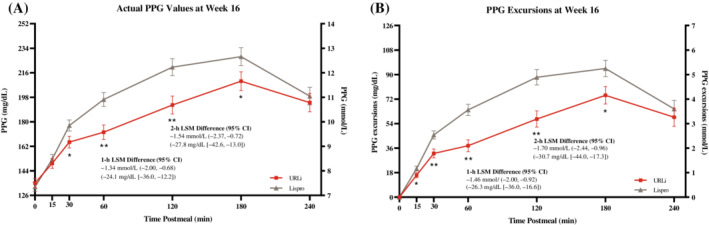
A, Postprandial glucose levels and B, postprandial glucose excursions following MMTT at week 16. Data are LSM ± SE. *p < .05; **p < .001.Note: a standardized liquid test meal consisting of approximately 700 kcal and approximately 100 g carbohydrate was used for the MMTT. An ANCOVA model was used in the analysis of superiority of URLi to lispro on 1‐ and 2‐h PPG. The analysis model included treatment and strata (pooled country, patient's personal CGM/FGM use during the study [yes/no] and HbA1c stratum at baseline [≤58.5 and >58.5 mmol/mol]) as fixed effects and baseline as a covariate. ANCOVA, analysis of covariance; CGM, continuous glucose monitoring; CI, confidence interval; FGM, flash glucose monitoring; LSM, least‐squares mean; MMTT, mixed meal tolerance test; PPG, postprandial glucose; SE, standard error
Fasting glucose prior to MMTT was similar between groups (URLi, 7.5 mmol/L [135.1 mg/dL]; lispro, 7.3 mmol/L [132.2 mg/dL]), while maximum glucose after the meal was lower with URLi compared with lispro (13.3 vs. 14.2 mmol/L [239.4 vs. 255.2 mg/dL]; p = .022). Incremental area under the serum glucose concentration‐time curve (iAUC) and above the glucose level at the start of MMTT was also significantly lower with URLi at all time intervals during the MMTT, with URLi resulting in a 25% reduction in iAUC0‐4h (Table S3). Mean insulin dose for the MMTT was similar between groups (URLi, 0.17 U/kg; lispro, 0.16 U/kg).
3.1.3. Blinded CGM at week 16
There was no difference between groups in the mean duration of TIR during the daytime (URLi, 640 min; lispro, 633 min) and 24‐h periods (URLi, 834 min; lispro, 828 min). URLi did not meet superiority to lispro in change from baseline TIR for either time period.
The mean percentage (and duration) of TIR during the night‐time, and time above range for daytime, night‐time and 24‐h periods, was also similar between groups (Table S4).
On average, mean glucose was numerically higher for URLi starting at around 03:00 pm until 8:00 am the following morning (Figure S4).
Consistent with MMTT findings, postmeal iAUC0‐1h and iAUC0‐2h from CGM were significantly lower with URLi treatment for breakfast, lunch and dinner (Figure 3). Overall (across all meals combined), URLi resulted in a significant reduction in postmeal iAUC0‐1h and iAUC0‐2h of 45% and 37%, respectively. Lower iAUCs were also observed with URLi between 0–3 and 0–4 h after meals, although these differences did not reach statistical significance. Postmeal glucose excursions across all meals were lower with URLi treatment at 0–1 h postmeal (LSM difference −0.24 mmol/L [−4.3 mg/dL]; p < .001) and at 0–2 h postmeal (LSM difference −0.29 mmol/L [−5.3 mg/dL]; p = .001).
FIGURE 3.
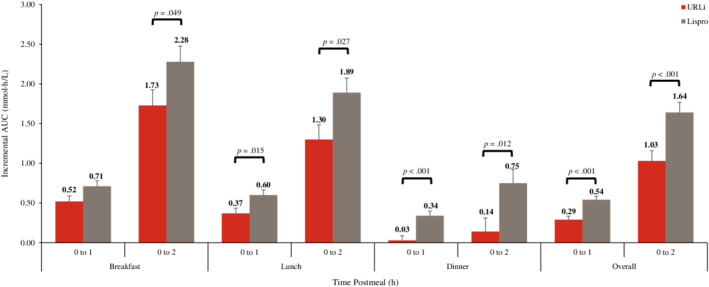
Postmeal incremental AUC from blinded CGM at week 16. Data are LSM ± SE. AUC, area under the curve; CGM, continuous glucose monitoring; LSM, least‐squares mean; SE, standard error
For both treatments, glucose control was generally maintained across all 3 days of infusion‐set wear as reflected by similar times above, below and in range, and iAUC after meals (Table S4).
3.1.4. 10‐point SMBG at week 16
Mean BG values were lower with URLi at morning 1‐h postmeal (URLi, 9.3 mmol/L [166.6 mg/dL]; lispro 9.8 mmol/L [176.5 mg/dL]; p = .032) and higher at evening premeal (URLi, 9.2 mmol/L [165.7 mg/dL]; lispro, 8.4 mmol/L [152.0 mg/dL]; p = .004) (Figure S5). There were no significant differences between groups at other time points.
Overall daily mean glucose values were similar between groups: URLi, 9.1 mmol/L (163.3 mg/dL); lispro, 8.9 mmol/L (159.8 mg/dL). Premeal daily mean, and 1‐ and 2‐h postmeal daily mean values, were also similar between groups. However, PPG excursions from midday premeal to 1‐h postmeal and from the daily mean premeal to 1‐h postmeal were significantly lower with URLi: LSM difference −0.50 mmol/L (−8.8 mg/dL; p = .045) and −0.42 mmol/L (−7.6 mg/dL; p = .011), respectively.
3.1.5. Insulin dose
Mean total daily insulin dose decreased with URLi from 0.62 units/kg at baseline to 0.59 units/kg at week 16 and increased minimally for lispro from 0.60 to 0.61 units/kg, with no significant difference between groups. Basal insulin doses (units/kg) were similar between groups at baseline and at week 16. While bolus insulin doses and bolus: total dose ratios were similar between groups at baseline, at week 16 both were significantly lower with URLi compared with lispro: the mean bolus insulin dose was 0.28 versus 0.31 units/kg (p = .036) and mean bolus: total dose ratio was 46.9% versus 48.8% (p = .049), respectively.
Pump basal rates and bolus calculator settings at week 16 were similar between groups (Table S5).
3.2. Safety
3.2.1. Adverse events
No deaths occurred in this study and the incidence of SAEs was similar between groups (Table S6). The most frequently reported SAEs were hypoglycaemia (URLi, 3 [1.4%]; lispro, 2 [0.9%]) and diabetic ketoacidosis (URLi, 3 [1.4%]; lispro, 3 [1.4%]).
The incidence of TEAEs was higher with URLi compared with lispro: URLi, 60.5% (n = 130); lispro, 44.7% (n = 97). This was primarily driven by an increase in infusion‐site reaction (URLi, 41 [19.1%]; lispro, 15 [6.9%]) and infusion‐site pain (URLi, 34 [15.8%]; lispro, 6 [2.8%]). The majority of these events (94%) were of mild or moderate severity; however, seven (3.3%) patients on URLi treatment discontinued IP as a result of infusion‐site reactions, six within the first 4 weeks of treatment and one between weeks 4 and 6 after starting treatment. Subgroup analyses for incidence of infusion‐site reaction by gender, BMI, infusion‐set model, bolus speed, total daily dose, age, duration of diabetes and duration of CSII showed no significant treatment‐by‐subgroup interaction. However, a statistically significant difference was seen in the treatment‐by‐infusion‐set‐cannula‐length (6 mm vs. greater than 6 mm; p = .070) and treatment‐by‐region analysis (US vs. non‐US patients; p = .046). The incidence of infusion site reaction with cannula length greater than 6 mm was similar between treatments (URLi, 15.3% vs. lispro, 8.8%; p = .149), but higher with URLi compared with lispro when the cannula length was 6 mm (24.5% vs. 4.9%; p < .001). Similarly, for US patients, the incidence of infusion‐site reaction was similar between URLi and lispro (8.0% vs. 6.8%; p = .765), while for non‐US patients the incidence was significantly higher with URLi compared with lispro (26.6% vs. 7.0%; p < .001).
No between‐treatment differences were observed from baseline to week 16 regarding systolic blood pressure, diastolic blood pressure or pulse rate. Mean body weight increased similarly in each treatment group during the 16‐week treatment phase (0.6 kg with URLi, 0.4 kg with lispro).
3.2.2. Hypoglycaemia
The incidence and rate of severe hypoglycaemia and nocturnal hypoglycaemia (BG < 3.0 mmol/L [54 mg/dL]) were low and similar between groups. However, the rates of documented and non‐nocturnal hypoglycaemia were significantly lower with URLi compared with lispro (Figure 4A). The incidence and rate of postmeal hypoglycaemia from 2–4 h and up to 4 h after the start of the meal were also significantly lower with URLi (Figure 4B).
FIGURE 4.
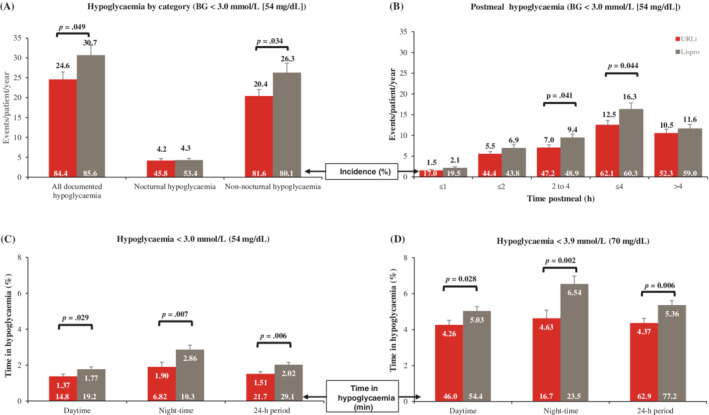
A, Rate and incidence of hypoglycaemia by category from SMBG, B, rate and incidence of postmeal hypoglycaemia from SMBG, C, percentage and duration of time in hypoglycaemia less than 3.0 mmol/L from CGM and, D, percentage and duration of time in hypoglycaemia less than 3.9 mmol/L from CGM. Data are LSM ± SE. Note: Daytime was defined as 6:00 am to 11:59 pm; and night‐time as 0:00 am to 5:59 am. Rate and incidence of hypoglycaemia in A and B were analysed using a negative binomial regression model and a logistic regression model, respectively. All time in range, time above range, and time below range data (including C and D above) were analysed using an MMRM analysis model with treatment and strata (pooled country, patient's personal CGM/FGM use during the study [yes/no] and HbA1c stratum at baseline [≤58.5 and >58.5 mmol/mol]) as fixed effects and baseline as a covariate. BG, blood glucose; CGM, continuous glucose monitoring; FGM, flash glucose monitoring; LSM, least‐squares mean; MMRM, mixed‐effects model for repeated measures; SE, standard error
CGM analysis also showed significantly less time (percentage and duration) in hypoglycaemic ranges of less than 3.0 mmol/L and less than 3.9 mmol/L (70 mg/dL) with URLi during the daytime, night‐time and 24‐h periods compared with lispro (Figure 4C,D).
3.2.3. Infusion‐set changes
Mean time interval to infusion‐set change was similar between groups for planned (URLi, 73.9 h; lispro, 73.5 h) and unplanned infusion‐set changes (URLi, 37.6 h; lispro, 34.9 h).
No between‐treatment differences were noted for the rate of planned infusion‐set changes. However, the rate of unplanned infusion‐set changes was higher with URLi compared with lispro: 0.86 versus 0.61 events/patient/30 days (p = .019). This difference was primarily driven by a higher rate of unplanned infusion‐set changes because of infusion‐site reactions with URLi compared with lispro (0.28 vs. 0.04 events/patient/30 days, p = .000; Table S7). Unplanned infusion‐set changes as a result of an infusion‐set problem, occlusion alarm or unexplained hyperglycaemia were similar between groups. Similar trends in the rates of unplanned infusion‐set change by reason were observed across the 3 days of infusion‐set wear (Table S7).
4. DISCUSSION
In this double‐blind, treat‐to‐target study, the primary endpoint was met, with non‐inferiority of URLi to lispro confirmed for change in HbA1c following 16 weeks of treatment in patients with T1D using CSII therapy. Patients entering this study had generally good glycaemic control, with on average an HbA1c of 60.6 mmol/mol (7.70%). However, improvement in HbA1c was observed during the lead‐in and first half of the treatment phase in both treatment groups, resulting in an average endpoint HbA1c of 58.2 mmol/mol (7.47%). These findings are similar to results from the ONSET 5 study, where similar improvements in HbA1c were observed between fast‐acting insulin aspart and insulin aspart, with non‐inferiority confirmed following 16 weeks of treatment in patients with T1D on CSII therapy. 13
URLi showed superiority to lispro in controlling both 1‐ and 2‐h PPG levels and significantly reduced PPG levels at all time points between 30 min and 3 h after the start of the MMTT, with a corresponding 25% decrease in the iAUC0‐4h. Supportive of the MMTT findings, CGM analyses showed that URLi resulted in significant reductions in iAUC 0–1 and 0–2 h after meals of 45% and 37%, respectively. These results are consistent with findings from the PRONTO‐T1D study in patients with T1D on MDI therapy and its subsequent CGM substudy, where URLi was superior to lispro on PPG control, showing significant reductions in PPG levels following an MMTT 8 and in iAUC0–2h following breakfast and for all meals combined. 14 Finally, while the average 1‐ and 2‐h postmeal daily mean values from 10‐point SMBG data were similar between groups in the current study, PPG excursions were significantly lower with URLi from premeal to 1‐h postmeal for the daily average and at midday, confirming the improved PPG control observed with URLi treatment.
It is worth noting that improved PPG control was achieved with URLi with a reduction in the rate of hypoglycaemia. URLi treatment resulted in significantly lower rates of documented hypoglycaemia and non‐nocturnal hypoglycaemia compared with lispro. Postmeal hypoglycaemia was also consistently lower with URLi, with differences reaching statistical significance at 2–4 h and up to 4 h postmeal. Similarly, with CGM analyses, URLi showed reduced time in hypoglycaemia at both glucose thresholds of less than 3.0 and less than 3.9 mmol/L during the daytime, night‐time and 24‐h period. Lower rates of postmeal hypoglycaemia and decreased time below range were also observed with URLi in the PRONTO‐T1D study and PRONTO‐T1D CGM substudy. 8 , 14 These lower rates of hypoglycaemia are reflective of the shorter duration of action observed with URLi in clinical pharmacology studies, 15 , 16 which allows for improved PPG control without causing late postmeal hypoglycaemia.
In this study, superiority of URLi to lispro in HbA1c reduction and TIR was not achieved. The reason for this is unclear but could be attributable to the higher glucose levels seen with URLi between late afternoon and early morning and the significantly lower bolus insulin doses. Similar hyperglycaemia in the late postevening period to early morning was seen in the ONSET 5 trial with fast‐acting insulin aspart. 13 These higher glucose values with URLi suggest that bolus doses were inadequate and/or correction factors were not aggressive enough. It is possible that upon seeing lower PPG values with URLi treatment, patients randomized to URLi reduced their mealtime bolus doses to avoid a perceived risk of hypoglycaemia. This would be most apparent with the evening meal, which is often larger and higher in fat and protein content. Given URLi's shorter duration of action, it is possible that patients would have benefitted from more aggressive bolus dosing without increasing the risk of late postmeal hypoglycaemia. However, a limitation of this study was that instructions for titration of basal rates and bolus doses provided in the study protocol were not enforced or monitored during the study, which may have negatively affected efficacy findings. For comparison, in PRONTO‐T1D, the 8‐week lead‐in and first 12 weeks of the treatment phase were dedicated to basal and bolus dose optimization, respectively. 8 At endpoint, basal, bolus and total insulin doses (U/kg) were similar between the URLi and lispro groups. While superior PPG control 8 and increased daytime TIR 14 were shown with mealtime URLi treatment, URLi was non‐inferior to lispro for HbA1c reduction. Elevated overnight BG levels were apparent with mealtime URLi in patients enrolled in the CGM substudy and the authors speculated that treatment with URLi may have warranted further basal dose optimization or use of a closed‐loop system in order to further improve glycaemic outcomes. 14 Taking URLi's enhanced PK/PD profile into consideration, it is probable that different insulin pump settings will be required, which allow for the most ideal distribution of basal and bolus insulin doses throughout the day to avoid periods of elevated BG levels. For future studies, a longer dose optimization period in conjunction with enforced titration protocols is recommended. Strategies such as using an extended bolus dose to mitigate hyperglycaemia in the late postmeal period following the larger, high protein/fat meals should be implemented where possible. In addition, patients using URLi with CSII therapy will need further education on the effects of URLi's unique pharmacological profile and how to best leverage these properties to attain more favourable glycaemic outcomes.
A higher incidence of TEAEs was noted with URLi in this study, driven by infusion‐site pain and infusion‐site reaction. Although a causal statistical analysis was not conducted to establish the reason for the increased infusion‐site reactions with URLi, we found that they were more common in non‐US regions or when a shorter infusion‐set cannula length was used. While the reason for the differential treatment effect in non‐US regions was not immediately apparent, the higher incidence of infusion‐site reaction with URLi using a shorter cannula length could be linked to delivering the insulin more superficially in the subcutaneous tissue. Infusion‐site reactions resulted in an imbalance in treatment discontinuations, with slightly more patients discontinuing URLi treatment. Although the majority of the infusion‐site–related events were of mild or moderate severity, they resulted in higher rates of premature infusion‐set changes with URLi treatment; but the difference was small, corresponding to one additional change approximately every 4 months with URLi, assuming routine changes every 3 days. Incidences of SAEs were similar between groups, including a small number of events of severe hypoglycaemia and diabetic ketoacidosis with both treatments.
Regarding pump compatibility, there was no evidence of an increased risk of infusion‐set occlusions with URLi, confirming long‐term pump compatibility with URLi treatment.
A strength of this study was the use of blinded CGM sessions in all participants, which provided insight into the extent of improved PPG control with URLi in an ad libitum feeding state. While these sessions were conducted a number of times during the study, access to this real‐time CGM data in all patients during the entire treatment period could have helped inform dosing decisions and might also have further improved glycaemic control.
In summary, this 16‐week, treat‐to‐target study in patients with T1D showed that when administered via CSII, URLi provided good glycaemic control and an acceptable safety profile with a reduced risk of hypoglycaemia but more frequent infusion‐site reactions. Furthermore, URLi provided superior PPG control over lispro treatment in patients with T1D on CSII.
CONFLICT OF INTEREST
MW received research support from Allergan, Astra Zeneca, Eli Lilly and Company, Gan and Lee, Idorsia, Novo Nordisk, Radius, Sanofi and Takeda; has been on the speaker's bureau for Amgen, Astra Zeneca, Eli Lilly and Company, Novo Nordisk and Sanofi; and has participated on advisory boards for Eli Lilly and Company, Novo Nordisk and Sanofi. BB is a shareholder of Aseko, Inc. and has received consultant fees from Eli Lilly and Company, Lexicon, Medtronic, Novo Nordisk and Pfizer; speaker honoraria from Astra Zeneca, Boehringer Ingelheim, Eli Lilly and Company, Janssen, Mannkind, Medtronic, Novo Nordisk, Sanofi, Senseonics and Xeris; and is an employee of Atlanta Diabetes Associates, which has received research grants and support from Boehringer Ingelheim, Dexcom, Diasome, Eli Lilly and Company, Insulet, Janssen, Lexicon, Mannkind, Medtronic, National Institutes of Health (NIH), Nova Biomedical, Novo Nordisk, Provention Bio, Sanofi, Senseonics, REMD Biotherapeutics, vTv Therapeutics LLC and Xeris. JIC, RL, JT, TH, FC and DI are employees and shareholders of Eli Lilly and Company. MP is the director of the Institute for Endocrinology and Diabetes National Center at Schneider Children's Medical Center. His institution has received grants from AstraZeneca, Dexcom, DreaMed Diabetes, Eli Lilly and Company, Insulet, Lexicon, Medtronic, NG Solutions, Novo Nordisk, Nutriteen Professionals, OPKO Health, Pfizer, Roche and Sanofi; he received honorarium and/or speaker fees from Eli Lilly and Company, Insulet, Medtronic, Novo Nordisk, Pfizer and Sanofi; consultation fees from Qulab Medical and RSP Systems; he is the Chief Scientific Officer and owns stock and options in NG Solutions; he is the Chairman and Chief Science Officer and owns stock and options in DreaMed Diabetes. BH reports no conflicts of interest. No other potential conflicts of interest relevant to this article were reported.
AUTHOR CONTRIBUTIONS
MW, BB, MP and BH participated as trial investigators and reviewed and edited the manuscript. JIC and RL contributed to the study design, the statistical analyses, the interpretation of the research and writing the manuscript. JT and TH contributed to the study design, medical oversight, interpretation of the research and writing of the manuscript. FC contributed to the interpretation of the research and writing of the manuscript. DI was responsible for medical oversight during the trial and contributed to the study design, the data analysis, interpretation of the research and writing the manuscript. All authors approved the final manuscript to be published. DI is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/dom.14368.
Supporting information
Table S1. Study inclusion and exclusion criteria.
Table S2. Insulin dose titration.
Table S3. Fasting and postprandial glucose levels, postprandial glucose excursions, and incremental AUC with meal test at week 16.
Table S4. Duration and percentage of time in ranges overall and by infusion set wear day at week 16.
Table S5. Pump factors.
Table S6. Adverse events from randomisation to week 16.
Table S7. Unplanned infusion set changes by reason and by infusion set wear day.
Figure S1. Study design.
Figure S2. Graphical approach to testing for multiplicity objectives.
Figure S3. Patient disposition from enrollment to week 16.
Figure S4. Mean glucose profiles over the 24‐hour period at week 16.
Figure S5. 10‐Point SMBG profile at week 16.
ACKNOWLEDGEMENTS
The authors thank the study participants, and the investigators and study coordinators who cared for them. The authors also thank Dr Annette M. Chang and Mary Anne Dellva (Eli Lilly and Company, Indianapolis, IN, USA) for critically reviewing the manuscript.
Warren M, Bode B, Cho JI, et al. Improved postprandial glucose control with ultra rapid lispro versus lispro with continuous subcutaneous insulin infusion in type 1 diabetes: PRONTO‐Pump‐2. Diabetes Obes Metab. 2021;23:1552–1561. 10.1111/dom.14368
Funding information This study was funded by Eli Lilly and Company
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Beck RW, Miller KM, Foster NC. The T1D exchange clinic network and registry: 10 years of enlightenment on the state of type 1 diabetes in the United States. Diabetes Technol Ther. 2019;21(6):310‐312. [DOI] [PubMed] [Google Scholar]
- 2. Foster NC, Beck RW, Miller KM, et al. State of type 1 diabetes management and outcomes from the T1D exchange in 2016‐2018. Diabetes Technol Ther. 2019;21(2):66‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stark Casagrande S, Fradkin JE, Saydah SH, Rust KF, Cowie CC. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988‐2010. Diabetes Care. 2013;36(8):2271‐2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Carls G, Huynh J, Tuttle E, Yee J, Edelman SV. Achievement of glycated hemoglobin goals in the US remains unchanged through 2014. Diabetes Ther. 2017;8(4):863‐873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Misso ML, Egberts KJ, Page M, O'Connor D, Shaw J. Continuous subcutaneous insulin infusion (CSII) versus multiple insulin injections for type 1 diabetes mellitus. Cochrane Database Syst Rev. 2010;(1):Cd005103. [DOI] [PubMed] [Google Scholar]
- 6. Jeitler K, Horvath K, Berghold A, et al. Continuous subcutaneous insulin infusion versus multiple daily insulin injections in patients with diabetes mellitus: systematic review and meta‐analysis. Diabetologia. 2008;51(6):941‐951. [DOI] [PubMed] [Google Scholar]
- 7. Leohr J, Dellva M, Carter K, LaBell E, Linnebjerg H. Ultra rapid lispro (URLi) accelerates insulin lispro absorption and insulin action vs Humalog (Lispro) consistently across study populations: a meta‐analysis of pharmacokinetic and glucodynamic data. Diabetes. 2020;69:1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Klaff L, Cao D, Dellva MA, et al. Ultra rapid lispro improves postprandial glucose control compared with lispro in patients with type 1 diabetes: results from the 26‐week PRONTO‐T1D study. Diabetes Obes Metab. 2020;22:1799‐1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kazda C, Leohr J, Liu R, et al. Ultra rapid Lispro (URLi) shows faster absorption of insulin lispro vs Humalog® during insulin pump (CSII) use in patients with T1D. Diabetes. 2018;67:1006. [Google Scholar]
- 10. Bode B, Garg S, Norwood P, et al. Compatibility and safety of ultra rapid lispro with continuous subcutaneous insulin infusion in patients with type 1 diabetes: pronto‐pump study. Diabetes Technol Ther. 2021;23(1):41‐50. [DOI] [PubMed] [Google Scholar]
- 11. Bretz F, Posch M, Glimm E, Klinglmueller F, Maurer W, Rohmeyer K. Graphical approaches for multiple comparison procedures using weighted Bonferroni, Simes, or parametric tests. Biom J. 2011;53(6):894‐913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bretz F, Maurer W, Brannath W, Posch M. A graphical approach to sequentially rejective multiple test procedures. Stat Med. 2009;28(4):586‐604. [DOI] [PubMed] [Google Scholar]
- 13. Klonoff DC, Evans ML, Lane W, et al. A randomized, multicentre trial evaluating the efficacy and safety of fast‐acting insulin aspart in continuous subcutaneous insulin infusion in adults with type 1 diabetes (onset 5). Diabetes Obes Metab. 2019;21(4):961‐967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Malecki MT, Cao D, Liu R, et al. Ultra‐rapid lispro improves postprandial glucose control and time in range in type 1 diabetes compared to lispro: PRONTO‐T1D continuous glucose monitoring substudy. Diabetes Technol Ther. 2020;22:853‐860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Leohr J, Dellva MA, Coutant DE, et al. Pharmacokinetics and glucodynamics of ultra rapid lispro (URLi) versus humalog® (lispro) in patients with type 2 diabetes mellitus: a phase i randomised, crossover study. Clin Pharmacokinet. 2020;59(12):1601‐1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Linnebjerg H, Zhang Q, LaBell E, et al. Pharmacokinetics and glucodynamics of ultra rapid lispro (URLi) versus humalog(®) (lispro) in younger adults and elderly patients with type 1 diabetes mellitus: a randomised controlled trial. Clin Pharmacokinet. 2020;59:1589‐1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Study inclusion and exclusion criteria.
Table S2. Insulin dose titration.
Table S3. Fasting and postprandial glucose levels, postprandial glucose excursions, and incremental AUC with meal test at week 16.
Table S4. Duration and percentage of time in ranges overall and by infusion set wear day at week 16.
Table S5. Pump factors.
Table S6. Adverse events from randomisation to week 16.
Table S7. Unplanned infusion set changes by reason and by infusion set wear day.
Figure S1. Study design.
Figure S2. Graphical approach to testing for multiplicity objectives.
Figure S3. Patient disposition from enrollment to week 16.
Figure S4. Mean glucose profiles over the 24‐hour period at week 16.
Figure S5. 10‐Point SMBG profile at week 16.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


