Abstract
The rapidly spreading COVID-19 pandemic demanded immediate organizational pivots in departments of laboratory medicine and pathology, including development and implementation of severe acute respiratory syndrome coronavirus 2 diagnostics in the face of unprecedented supply chain shortages. Laboratory medicine and pathology educational programs were affected in numerous ways. Here, we overview the effects of COVID-19 on the large, academic Department of Laboratory Medicine and Pathology educational practice at Mayo Clinic, highlighting lessons learned for the post-pandemic era and planning for the possibility of a future pandemic.
Keywords: COVID-19, education, pathology, laboratory medicine, virtual
Since January 2020, the world has experienced the unprecedented impact of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), with more than 119 million people infected and 2.6 million deaths. The rapidly spreading pandemic demanded immediate organizational pivots in departments of laboratory medicine and pathology, including development and implementation of SARS-CoV-2 diagnostics in the face of unprecedented supply chain shortages, and undertaking of studies to rapidly understand transmission pathways, pathogenesis, evolution, and impact on human health, to inform diagnostics, prevention strategies, therapeutics, and vaccines. Laboratory medicine and pathology educational programs were affected in several ways. Here, we overview the effects of COVID-19 on the large, academic Department of Laboratory Medicine and Pathology educational practice at Mayo Clinic, highlighting lessons learned both for the post-pandemic era and planning for the possibility of a future pandemic.
The Department of Laboratory Medicine and Pathology enrolls, on average, 70 resident/fellow learners into 21 unique graduate medical education programs each year. Each program is led by an Education Program Coordinator and a Program Director, with some appointing Associate Program Directors. Over 150 faculty members are responsible for educating involved learners. There are also 4 allied health staff educational programs offered through the Mayo Clinic School of Health Sciences with, on average, 140 learners annually. These programs vary in length from 9 weeks to 12 months. Each of these programs is led by a Program Director and involve faculty and allied health staff in providing education. Finally, extramural education and education of the public are provided. This illustrates the background under which changes in educational programs were executed in response to the COVID-19 pandemic.
There were several major institutional changes implemented due to COVID-19 at Mayo Clinic over time. A travel restriction went into effect on March 10, 2020, with masking of symptomatic patients implemented March 13, 2020. Teleworking prioritization began March 16, 2020. Physical distancing signage was placed, patient door screening implemented, and employee daily self-temperature checks required beginning March 23, 2020. The following day, only essential employees could be on campus. Masking for those involved in patient care took effect March 31, 2020, with universal masking of all patients and staff adopted on April 5, 2020, and mandatory eye protection for frontline staff added in May 2020.
In light of the above, in March 2020, faculty and allied health staff involved in education had to rapidly adapt existing educational programs to accommodate physical distancing requirements, minimize on-site staff, and maintain robust isolation/quarantine restrictions for individuals with COVID-19 or COVID-19 exposures (Table 1). Educators had to harmonize among learners, faculty, mentors, and coordinators to ensure that all had access to online communication platforms (eg, Zoom, Skype, Blackboard) to participate in virtual learning and that all had the training needed to use these platforms effectively. COVID-19 vaccines became available in December 2020, and by the end of the first quarter, staff, students, and trainees needing to be on site, and who agreed to be vaccinated, had been. As of March 1, 2021, in person meetings, including educational activities (with ongoing universal masking), were again permitted.
Table 1.
Anatomic and Clinical Pathology Program Adjustments During the COVID-19 Pandemic.
| Program | Type of programming | Offerings |
|---|---|---|
| Anatomic Pathology Residency and Fellowships | Virtual passive programming | Live lectures (eg, regular structured curriculum, “q3” [see text], Grand Rounds) |
| Virtual active programming | Virtual sign-out sessions “WhatsApp” sharing of online educational resources Virtual meetings Virtual multi-institutional journal club Virtual well-being sessions |
|
| Virtual asynchronous programming | Recorded lectures (eg, regular structured curriculum, Grand Rounds, CAP offerings, USCAP offerings) | |
| Graduation | Virtual | |
| Recruitment | Virtual interviews | |
| Clinical Pathology Residency and Fellowships | Virtual passive programming | Live lectures (eg, regular structured curriculum) |
| Virtual active programming | “WhatsApp” sharing of online educational resources Virtual meetings Virtual multi-institutional journal club Virtual well-being sessions |
|
| Virtual asynchronous programming | Recorded lectures (eg, regular structured curriculum, Grand Rounds, CAP offerings, USCAP offerings) | |
| In-house activities | Transfusion medicine service, autopsy, clinical microbiology | |
| Graduation | Virtual | |
| Recruitment | Virtual interviews | |
| Employee | New employee orientation | Virtual |
| Medical Laboratory Science Program | Programming | Hybrid program: split learners into 2 sections to enable in-person activities with physical distancing with other activities held virtually |
| Recruitment | Virtual interviews | |
| Phlebotomy Technician Program | Programming | Hybrid program: split learners into sections to enable in-person activities with physical distancing with other activities held virtually |
| Recruitment | Telephone interviews | |
| Histology Technician Program | Programming | Virtual One cohort experienced training delay |
| Graduation | Virtual | |
| Recruitment | Virtual interviews | |
| Cytotechnology Technician Program | Programming | Combinational virtual and on-site |
| Recruitment | Telephone interviews | |
| Extramural Continuing Education | Programming | Suspended or offered virtual |
Abbreviations: CAP, College of American Pathologists; USCAP, United States and Canadian Academy of Pathology.
Graduate Medical Education Programs
Education
As Mayo Clinic mandated that all nonessential personnel work from home on March 24, 2020, one of the first decisions that needed to be made was to determine which postgraduate trainees might fall into this category. In anatomic pathology, trainees assigned to the surgical pathology (frozen section) and autopsy services were considered essential and kept on-site. In clinical pathology, residents rotating on the transfusion medicine service were considered essential and kept on-site. Clinical microbiology fellows played an essential role in COVID-19 test validation, implementation, and results interpretation, and stayed onsite, at least part-time. Trainees assigned to elective rotations or rotations that could feasibly be completed by faculty without trainee assistance were considered nonessential. Although other training programs redeployed their pathology residents to validate and perform COVID-19 testing, 1,2 we did not do this.
Resident and fellow involvement in both surgical pathology (frozen section) and autopsy were deemed “essential.” Prior to COVID-19, 4 residents and 4 fellows were scheduled on the surgical pathology (frozen section) service. Although workflow (eg, some cases being processed in biohazard hoods) and practice (eg, universal masking) changes occurred, no changes were made in scheduling this service, and grossing/frozen section performance/in person slide sign out sessions continued throughout the pandemic without incident. During the first 3 to 4 months of the pandemic, surgical pathology volumes decreased slightly. Overall surgical pathology case numbers were approximately 119, 000 in 2019, decreasing to approximately 105, 000 in 2020. This 12% decline was associated with decreased elective surgical procedures, with the decline most pronounced in March through June 2020; by the end of 2020, monthly case volumes had returned to pre-COVID-19 levels. Since this is a high-volume practice and reduced volumes were temporary, there was little effect on education.
Similarly, autopsy continued in a status quo fashion during the pandemic. By the end of 2020, the total number of autopsies performed (907) was 8% higher than in 2019 (831). During the 12-month period from March 2019 through February of 2020, 77 autopsies were performed on COVID-19 positive patients. Residents participated in all facets of the autopsy service, including routine medical, forensic, and COVID-19 autopsies.
Trainees rotating on the transfusion medicine service are responsible for direct patient care. For trainees beginning their initial educational month, educational content, consisting of recorded and live lectures, required readings, and online structured content were provided remotely. For trainees providing consultations for therapeutic apheresis and transfusion reactions, and responding to blood donor reactions, and other critical patient/donor care services, the resident and fellow alternated in house coverage on a daily basis, with one trainee in house and the other at home participating in online educational content. Transfusion medicine patient care/educational rounds were moved online via Zoom with participants (allied health staff, nursing staff, attending physicians, and trainee on service) in separate locations, allowing trainees not covering the service to attend from home. Attending physicians alternated being physically present on campus, providing direct supervision, based upon their coverage schedule, with work from home. During this period, patient volumes were adjusted such that only critical apheresis procedures were performed, with delays in procedures such as hematopoietic progenitor cell collection, photopheresis for chronic graft-versus-host disease, and other nonemergent procedures, to avoid patient and staff contact and preserve Personal Protective Equipment (PPE). A description of this has been published. 3 Surgical procedures were also briefly reduced, thereby decreasing blood collections and overall transfusions.
Other clinical pathology services (eg, hematopathology, chemistry, molecular) moved to either hybrid in person/virtual experiences or completely virtual exchanges, with nonessential laboratory medicine and pathology trainees staying home for 5 weeks, ultimately returning to campus, at least part time. Nonessential laboratory medicine and pathology residents and fellows sent home on short notice took it upon themselves to find and share online pathology educational resources with one another, for example, through a “WhatsApp” group. A more structured live curriculum, along with continued exposure to anatomic pathology cases was considered desirable to prevent trainees from falling behind in pathology education. In anatomic pathology, for example, three 1-hour lecture blocks were set-up each day (9:00 am, 12:00 pm, and 3:00 pm) to engage faculty (many of whom had increased availability because of temporarily decreased clinical volumes) and off-site residents. These “q3” lectures were delivered via Zoom. Residents also made use of external education offerings, such as free lectures offered by the College of American Pathologists and the United States and Canadian Academy of Pathology (USCAP). Many residents and anatomic pathology fellows (eg, gynecologic pathology, urologic pathology, head and neck pathology, breast pathology) also successfully worked from home, with secure remote access to the anatomic pathology laboratory information system, PathDx (SCC Soft Computer) via institutionally supplied laptops, and live viewing of real-time cases with faculty during Zoom anatomic pathology sign-out sessions. Faculty shared their microscope camera feeds via a secure system, recapitulating in-person sign-out sessions. Although trainees were not able to preview cases as they normally would have done, they reviewed cases with faculty members in real time and in some cases, generated draft reports entered into PathDx with the electronic dictation system Fluency Direct (3M) from home (which were subsequently edited by on-site faculty). Faculty and trainees were encouraged to discuss preferences for sign-out format at the beginning of clerkships. This virtual sign-out format was also utilized as an alternative to traditional double scoping, even after trainees returned to campus, to maintain appropriate physical distancing. This format was also adopted for curbside consultations and engaging remote faculty. For those at home, many Program Directors asked trainees to email about their daily academic efforts, enabling Program Directors to give feedback, share resources, and have a record to support completion of training.
Regular structured curricular content, including lectures, slides sessions, and meetings, was ported to a virtual format, which became the “new normal.” Some faculty noted decreased learner interaction in the virtual environment as compared to the traditional (in-person) format. This was partially mitigated by having learners keep their video feed live during educational sessions, allowing for more interactivity and ongoing monitoring of participants by the faculty. Digital disengagement, increased susceptibility to distractions, and teleconferencing fatigue have been noted by others. 4 -6 Hassell et al conducted an online survey of pathology trainees, program directors, and faculty to assess pre- and post-COVID-19 use of, and response to, various digital pathology modalities and found that a majority of faculty and learners assessed that this shift had adversely affected the quality and effectiveness of teaching. 4
Program curriculum was directly affected. The Leadership & Management course, traditionally consisting of 8 full-day in-person sessions, is a program requirement for residents and fellows. During the pandemic, all 8 sessions transitioned to Zoom and were restructured to encourage engagement and try to avoid passive learning. Large and small group discussions, breakout rooms, polls, and message chats were used. Additional breaks were built into daily schedules, to avoid Zoom fatigue. More flipped classroom approaches were used by placing content in the learning management system for trainees to review prior to the sessions. Although trainees were encouraged to keep their webcams on throughout all sessions, most trainees only used their webcams in small group discussions within breakout rooms. A participant survey delivered at the end of the course noted that the course was well-organized, interesting, and “full of good information,” and that while some learners found it to be interactive and engaging, others struggled with engagement, finding it difficult to follow in a virtual format.
Trainee assessments had to be addressed. The process of moving paper-based exams and quizzes to an online format (Blackboard, VA) had begun before the pandemic, but had to be quickly accelerated and completed, and all paper-based forms (eg, training checklists) converted to electronic formats to accommodate rotating residents and fellows.
Many faculty and trainees had rudimentary knowledge of Zoom before the pandemic. There was some experience with it to share cases from the frozen section laboratory with other sites within the institution. Although faculty and trainees wished they had been well-versed with the technology before the pandemic started, they learned fast, and were generally surprised as to how well live real-time pathology sign-out sessions could be executed with trainees at remote locations. Prior to the pandemic, audio-only teleconferences had been commonplace; the transition to Zoom quickly led to recognition of the value of incorporating video and interactive learning. It is an improvement to be able to share screens and see colleagues and trainees. Multi-institutional journal clubs were also transitioned from conference calls to a Zoom format; we partnered with international institutions for further collaborations of journal clubs. Post-pandemic, platforms such as Zoom or Skype will continue to be used for educational case conferences and journal clubs. Historically, there has been a limit on the number of participants in these sessions due to conference room capacity; allied health staff and learners in other training programs have expressed interest in attending these educational sessions but have not always been able to participate due to room size. The use of platforms such as Zoom or Skype allow individuals to “attend” sessions remotely despite space limitations in conference rooms. Tools within Zoom, including breakout rooms, voting polls and chats, encourage interaction, and engagement with learners. Additionally, this allows recording of sessions to be viewed by different learners at any time, enhancing educational experiences of allied health staff, current residents/fellows, nonlaboratory medicine and pathology residents/fellows, and future trainees. Lectures, case conferences, tumor boards, and journal clubs were recorded so that content could be available to fellows and residents if they had technical connection issues at the time of a live conference. This also allowed learners who may have been unavailable during the time of a live session to view the content later; these recorded sessions were repurposed for other educational opportunities at later dates. Anatomic Pathology Grand Rounds were moved to a virtual platform, allowing more participation and attendance of this continuing medical education activity.
An Anatomic Pathology Academic Achievement Celebration continued to be held, but instead of taking place in-person, used the Zoom platform. This celebration recognizes trainees and other allied health staff members who have contributed to the well-being of Mayo Clinic patients through academia and research. These include achievements such as publications, posters, presentations at academic meetings, awards, and so on.
Graduation
Trainee graduation ceremonies, which are important in terms of providing recognition of trainee achievements, could not occur in-person. Thus, the Zoom format was employed for these as well, to allow for “live” celebrations. The traditional graduation ceremony format recognized all graduate medical education graduates (pathology residency and 20 fellowships) together in one large ballroom. Historically, space limitations meant that only the graduate, one guest, and select faculty could attend. Similarly, time limitations restricted the amount of information that could be shared for each graduate. The virtual format allowed for broader attendance, including an essentially unlimited number of family members from Rochester, Minnesota, and around the world, as well as all faculty and educational staff. Implementation of virtual graduations has prompted us to rethink our format of hosting a large combined graduation and led us to move toward individualized ceremonies for each program or groups of similar programs. Having fewer graduates in each ceremony allows for more customization; pictures and testimonials from each graduate can be included, alongside messages from the Program Director, faculty and allied health staff. Going forward post-pandemic, consideration is being given to offering hybrid virtual and in-person events, to allow more people to join, including faculty, trainees, and family members, who would otherwise be unable to do so. This enhance audience allows participation of those separated by large distances and addresses limits on numbers of guests for live activities.
Recruitment
Recruitment and interviewing were challenges, given that candidates could not be met in-person. Blackboard courses were created within each program for prospective residents and fellows to review prior to their interview. Content included information about the program to which they were applying, as well as the community, including videos, photos, and links. This platform had the benefit of capturing how much time prospective trainees spent in the Blackboard course, and which sections they viewed the most, which is useful for website improvement. The most popular content included welcome messages from Program Directors, messages from current and past trainees, and an overview of Mayo Clinic institutional culture. Prospective residents and fellows were offered individual interviews via Zoom, with assistance and training from Mayo Clinic Media Support Services. Innovative components were added to the interview process, including 3D virtual tours of several laboratories using the Matterport platform. The Matterport scans were a wonderful option for self-guided tours by prospective trainees. These tours have been adapted as teaching tools (via voice-over) describing the testing and technology utilized in the various work areas and are now being used for employee orientation and training, and tours for external Mayo Clinic Laboratories clients and as a component of virtual inspections from accrediting organizations such as the Foundation for the Accreditation of Cellular Therapies, in addition to educating traditional learners. Virtual laboratory tours are also useful for rotating residents and fellows from external areas who cannot physically tour through the spaces. For interviews, virtual Matterport tours were supplemented with real-time tours via Zoom using cell phones, as needed.
Novel elements were offered during virtual interviews to further enhance experiences, including a live Zoom slide session with multiple faculty members presenting unknown slides, small and large group Zoom chat rooms with current fellows, a Zoom “meet and greet” with current faculty, and a Zoom chat with recent alumni. On interview day, a facilitator/host was available to applicants in virtual waiting and breakout rooms. This was well-received by applicants, many of whom reported the experience to be among the most polished and organized virtual interview structure of any program for which they interviewed. Details of our experience implementing virtual interviews in the surgical pathology fellowship program were presented at the USCAP Annual Meeting, March 13-18, 2021. 7 The Anatomic and Clinical Pathology and the Anatomic Pathology/Neuropathology Programs filled all listed positions in the March 2021 National Resident Matching Program.
Going forward, several elements of the virtual interview process will be retained, including virtual materials course applicants can review ahead of time at their convenience, the live virtual meeting with recent alumni, and the virtual slide session featuring multiple diverse faculty members. These options were not available in-person and offer gains in quality over what was offered in-person, exploiting advantages and conveniences of a virtual environment to build upon what had historically been done in live interviews.
Visiting Residents
The visiting resident program was halted during the pandemic, with elective observation rotations by learners from outside of Mayo Clinic put on hold. As this program is used as a recruiting tool, a virtual visiting resident experience (previously approved as an in-person visiting activity) was approved 8 months into the pandemic. Over the course of several months, preparation for this virtual experience ensued, with coordinated efforts by Mayo Clinic School of Graduate Medical Education, information technology, the Department of Laboratory Medicine and Pathology Graduate Medical Education staff, the programs involved, and the visiting resident. Proposed goals and objectives identified by the resident for the virtual rotation included participation in daily sign-out with faculty; independent preview/review of virtual slides; virtual attendance at clinical conferences, journal clubs, and tumor board; and literature searches and presentation preparation. As with in-person visiting residents, the trainee was given a Mayo Clinic identification number and email. A Mayo Clinic laptop was shipped to the visiting resident, but no access was granted to Mayo Clinic clinical applications (eg, PathDx, EPIC); these security measures precluded preview/review of scanned slides. Case follow-up by the visiting resident was limited because of the de-identified case information shared during sign-outs and clinical conferences conducted via Zoom. Lessons learned from this inaugural virtual rotation included the importance of dedicated information technology support to the trainee during a 4-hour block of time allocated to initial computer login, remote access and set up. The virtual rotation worked well from the visiting resident’s perspective with multiple sign-out opportunities each day in addition to conference attendance. The visiting resident’s engagement and drive were considered crucial elements to the success of the experience. Although this experience proved successful, the required administrative efforts and security measures warrant limiting future virtual visiting resident experiences to select situations.
Well-Being
The Graduate Medical Education Well-Being Committee took the initiative to continue offering well-being opportunities for residents and fellows. Virtual workshops conducted by faculty included topics such as cooking, art, and magic. Workshops were well-received and inspired faculty as well as trainees to volunteer to facilitate further virtual workshops. A well-being seminar series with a licensed practicing psychologist offered pre-pandemic transitioned to a virtual setting. Sensitive topics such as burnout and suicide continued, with trainees being engaged in discussions.
Employee Continuing Education Programs
Employee education faced 2 major COVID-19-related challenges. The first and most immediate was the need to transform a 1.5 day, in-person departmental new employee orientation program to a virtual environment in 2 days. This was daunting considering the need to rapidly hire new staff to offer the level of SARS-CoV-2 testing needed to support the clinical practice. Fortunately, many in-person presentations had been recorded prior to the pandemic, in the event a speaker was unavailable for orientation. Staff worked swiftly to edit these recordings, add closed captioning, and build content into a learning management system; changes were communicated to supervisors and made available to laboratories/work units. The second challenge was assisting trainers/educators in the rapid transition to a virtual and/or asynchronous environment. Just-in-time training on tools and technology was provided, a webpage with a list of virtual meeting/learning resources created, and numerous questions answered.
Allied Health Staff Training Programs
Four allied health staff training programs are offered—Medical Laboratory Science, Cytotechnology, Histology Technician, and Phlebotomy Technician Programs. The Medical Laboratory Science Program splits the class of 24 students into 2 sections, with 12 each participating in morning and afternoon sessions. Each group of 12 participated in teaching laboratory experiences together, with universal masking and separation of students by 6 feet or more. Since this program had been designed as a blended learning experience prior to the pandemic, distance education methods were available and/or implemented for nonlaboratory components, and lecturers were given the option to transition their lecture into the distance learning system, Blackboard Collaborate.
The stay-at-home order was more challenging for the Cytotechnology Program as it was difficult to identify activities learners could do from home; when they returned to campus, the issue was more about how to keep them safe. Online resources and new technologies were identified that helped with distance learning and will likely be retained moving forward. Blackboard Collaborate was used to hold review sessions virtually. This application continues to be used if students are unable to attend class on-site (eg, if they test positive for SARS-COV-2 and are not especially ill). Physical barriers were created, and the schedule modified to facilitate physical distancing, where possible.
The Histology Technician Program focused on ensuring adequate clinical time so students could meet program competencies. The program delivered all didactic curriculum online via Blackboard prior to the pandemic so there was little disruption to content delivery. Some faculty were furloughed and some transitioned to working from home, at least part time. Learners were removed from some clinical settings and transitioned to virtual learning with videos created to supplement lost clinical observations. Scope sessions, review quizzes, presentations, and group discussions were delivered remotely using Blackboard Collaborate. Blackboard Collaborate was selected because students and faculty in this program were already familiar with it. Proctorio (an exam proctoring service) was implemented for didactic exams. One cohort graduated in May of 2020, completing their program entirely online. All learners in this cohort successfully completed the program, passed their ASCP certification exam, and are employed at Mayo Clinic. The second cohort graduated in November 2020, with their graduation having been delayed from what had been planned by 4 weeks. They were unable to be on campus from March through June 2020, having to complete some coursework virtually, and ultimately returning to the clinical setting. This cohort also successfully completed the program, passed their ASCP certification exam, and is employed at Mayo Clinic. Graduation ceremonies were delivered virtually via Zoom.
Students who graduated from the Histology Technician Program in 2020 during the COVID-19 pandemic were surveyed about their experiences, reporting both positive and negative experiences. On the positive side, some felt that the online learning experience allowed improved information retention due to a more relaxed learning setting and not feeling as rushed to complete assignments and learn new topics as they might in person; they were able to decompress and take breaks at home. Some noted that hands-on learning may make it easier to forget little details, and that online activities facilitate topic review. Although the workload remained unchanged, cutting out commuting times and waiting for classes/rotations made it feel less intense and more convenient for some. Students reported having more time to study for the certifying examination. Some learners were used to online coursework from prior experiences and easily transitioned back to it. A rewarding part of virtual learning was noted to be the instant feedback to quizzes and exams. Students valued being able to “see” one another virtually.
There were, however, negative experiences noted with virtual learning. One student noted that virtual education took longer in terms of studying time than did in-person education, and some considered themselves less productive, less motivated/interested, more disassociated from curricular content, and more stressed, when studying at home, noting it to be “…hard to find motivation while staying in my own living space,” and that they, “…didn’t feel like [they were] in ‘school mode’ any longer since [they weren’t] actively going out and attending anything school related.” Having to get up, get ready, and go to classes, and use study and learning areas on campus, had provided some students motivation to succeed that was lost when learning was moved to their living space. Students observed that there might be better tools for virtual learning than Blackboard Collaborate; the platform experienced “…lags, glitches and only allow[ed] for four class members to be seen on the screen at a time.” Some students missed hand-on experiences, noting that, “…actually getting to do it yourself really helps build knowledge.” The loss of interaction with and connection to colleagues and faculty in person and ability to ask a lot of questions was also noted as a downside. Learning concepts virtually and then reinforcing them in the laboratory through clinical rotations, may be a possible option going forward.
The Phlebotomy Technician Program was challenged by space availability to conduct laboratories while maintaining physical distancing. There were appointing and on-boarding challenges since staff supporting students were working from home, sometimes resulting in communication delays. Orientations were conducted online, including presentations such as Academic Success, Title IX, taking of photos and preparation of identification badges, and other human resources tasks. A particular challenge from a human resources standpoint was executing background checks and fingerprinting for incoming matriculates in an online environment. Clinical rotations were confronted by staffing issues limiting trainers/preceptors, a need to change rotations since students could not care for patients with or suspected to have COVID-19, and temporarily decreased outpatient volumes (the setting where the bulk of training typically occurs). The Phlebotomy Program was a hybrid learning program prior to COVID-19, so there was minimal disruption in delivering content. Classes were split, with the cohort divided into 2, allowing one group to attend laboratories/lectures in the morning while the other group was on clinical rotations, with the groups switching in the afternoon. Graduation celebrations were discontinued, with students receiving certification and a graduation package from faculty on the last day of class. There were also training cutbacks; typically, phlebotomy education trains over 300 new hires annually, including internal medicine and pediatric physicians, and mayo medical school, respiratory therapy, physician assistant, nuclear medicine, and medical laboratory science students. Many sessions were reduced/rescheduled because of limitations related to space and trainer availability.
As with the graduate medical education programs, the Medical Laboratory Science and Histology Technician programs implemented virtual interviews via Zoom, which went well, and may be retained beyond the pandemic, since they save time and seem to not negatively impact interview quality or the applicant selection process. Interviews for the Phlebotomy Technician and Cytology Programs were done via telephone.
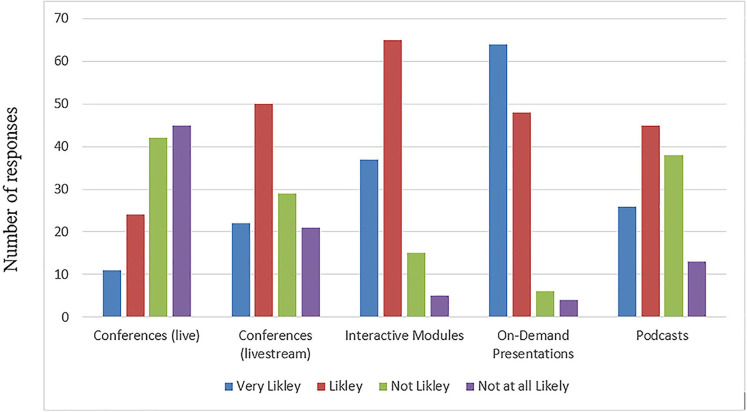
Extramural Continuing Medical Education
Mayo Clinic Laboratories typically hosts medical conferences, 8 of which were cancelled, requiring communication both internally and externally, and negotiating with existing property contracts to claim force majeure. Some programs were suspended because of staff furloughs and pivoting of faculty/content experts to COVID-19 testing, and some accreditation needed to be discontinued due to lack of managing resources. For 2021, Mayo Clinic Laboratories will be providing a virtual/streaming option for conferences to substitute for live/in-person options. Even when in-person events resume, hybrid options will likely be offered, to provide more flexibility to those who want to participate. Results of a survey of 122 participants in extramural offerings administered in February 2021 (Figure 1) showed there to be a preference for on-demand presentations, interactive modules, livestream conferences and podcasts (in decreasing order), over live conferences for the next 12 months’ time.
Figure 1.
Results of a survey of participants in extramural educational activities (eg, technologists, phlebotomists, administrative laboratory directors/managers, laboratory supervisors, medical/scientific laboratory directs, pathologists) administered in February 2021 asking, “please tell us how likely you are to take advantage of educational offerings in the following formats, within the next 12 months.” Three quarters of participants valued receiving educational credit from participation in these activities, especially professional acknowledgment for continuing education.
Education for the Media and General Public
The Department of Laboratory Medicine and Pathology played an essential role in diagnosing patients with COVID-19, and thus we found ourselves in high demand from members of the media. To ensure that we were providing accurate, timely, and consistent messaging to the media, we designated a lead external communications contact to work with Mayo Clinic public relations specialists to screen and respond to media requests and arrange interviews with a small pool of subject matter experts. Individuals who spoke to the media underwent specific training to ensure that they felt confident in addressing difficult topics and delivering appropriate messages. The lead external communications contact founded a weekly podcast with the Chair of the Department of Laboratory Medicine and Pathology and other key members of laboratory leadership to keep employees and the general public up-to-date on important and ever-changing issues.
Stressors and Unanticipated Challenges
An unanticipated challenge was that learners required to be on campus sometimes had a challenge getting to campus due to discontinuation of public transportation in and to Rochester, Minnesota. In addition, faculty and learner stress levels were elevated due to the uncertainty of the situation, social isolation, and concern about SARS-CoV-2 infection. For faculty, the need to rapidly adapt and sometimes deliver the same content multiple times to accommodate smaller group sizes, created additional work. For services with both in-person and distance learners, it was a challenge to remain aware of and integrate those joining remotely, into educational clinical discussions. Some lecturers found it challenging to present to distance learners who had their video feed turned off. Like in-person learning, the ability to “read the room” is important for lecturers to educate. Program directors had increased challenges identifying and assessing mental health issues and were overall more concerned with learners’ emotional well-being than their academic standing. As mentioned above, some learners found online learning itself to create stress because of dissociation from curricular content and lack of in person engagement with colleagues and faculty. Finally, for services where interactions between members of the health care team were essential for providing patient care, such as therapeutic apheresis, both the nursing staff and the residents described difficulties in communicating clearly, misunderstandings, and a “loss of trust” that was felt to be due to the virtual patient/education rounds. This type of situation has prompted a return of many in-person educational activities (with virtual options provided), with masking and physical distancing, as of March 1, 2021.
Lessons Learned
There were several lessons learned (Table 2). Despite the downsides of an almost fully virtual educational system, we anticipate that some educational activities adopted during the pandemic will remain virtual after the pandemic; this includes prerecorded videos, electronic proctoring, hybrid graduations, and the ability to “work from anywhere” for some staff. Lectures, core curriculum sessions, meetings, and interviews from this point forward should consider incorporating a virtual component for remote viewing/participation in addition to traditional in-person options, as this makes them more accessible, practical, and just generally makes life a little easier. We learned that virtual sign-out is a viable option for medical education in pathology and can be used to facilitate education of residents and fellows when the faculty and learner cannot physically be at the same site for any reason and also to educate “virtual visiting learners” (eg, medical students, visiting residents). The Leadership & Management course should return to an in-person format, at least in part, post-pandemic. We made advances in virtual interviewing, and recognized benefits of components of this strategy, such as content applicants can review ahead of time at their convenience, the live virtual meeting with recent alumni, and the virtual slide session featuring multiple diverse faculty members. We also learned that hosting visiting virtual rotations in health care can be challenging, and that the administrative efforts and security measures needed warrant limiting future virtual visiting resident experiences to select situations. We started multi-institutional journal clubs, which continue to this day; others’ success with multi-institutional programs, such as the Breast Cases Challenge, have been described. 8 Nevertheless, trainees recognized value in engaging with faculty in person and the associated positive learning experiences.
Table 2.
Lessons Learned.
| Electronic proctoring of examinations is acceptable |
| Virtual graduations allow more participation from families, friends, and faculty |
| Work from anywhere is acceptable for some staff |
| Lectures, core curriculum sessions, meetings, and interviews should consider incorporating a virtual component for remote viewing/participation (in addition to traditional in-person options) into the future |
| Virtual sign-out can be used for medical education in pathology when faculty and learners cannot be physically together |
| The Leadership & Management course should be delivered in an in-person format, at least in part |
| Benefits of virtual interviewing include providing content for applicants to review ahead of time at their convenience, live virtual meetings with recent alumni, and virtual slide sessions featuring multiple diverse faculty members |
| Hosting visiting virtual rotations in health care is challenging due to administrative burden and security measures |
| Online learning provides a more relaxing learning setting for some but a more stressful (dissociation from curricular content) learning setting for others |
| Extramural on-demand presentations, interactive modules, livestream conferences, and podcasts are preferred over live conferences in the near-term |
Other institutions have published their experiences with the educational impact of the COVID-19 pandemic. 9,10 Advances being made in digital pathology (eg, whole slide imaging) have been noted to be especially useful in the context of a need for physical distancing. 11,12 Mukhopadhyay et al have compiled curated lists of online resources that can be used for virtual learning in pathology. 13
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Patel reports grants from Merck, ContraFect, TenNor Therapeutics Limited and Shionogi. Dr Patel is a consultant to Curetis, Specific Technologies, Next Gen Diagnostics, PathoQuest, Selux Diagnostics, 1928 Diagnostics, PhAST, and Qvella; monies are paid to Mayo Clinic. Dr Patel is also a consultant to Netflix. In addition, Dr Patel has a patent on Bordetella pertussis/parapertussis PCR issued, a patent on a device/method for sonication with royalties paid by Samsung to Mayo Clinic, and a patent on an anti-biofilm substance issued. Dr Patel receives an editor’s stipend from IDSA and honoraria from the NBME, Up-to-Date and the Infectious Diseases Board Review Course.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Robin Patel  https://orcid.org/0000-0001-6344-4141
https://orcid.org/0000-0001-6344-4141
Jeffrey L. Winters  https://orcid.org/0000-0001-8654-3732
https://orcid.org/0000-0001-8654-3732
References
- 1. Brandler TC, Warfield D, Adler E, et al. Lessons Learned from an anatomic pathology department in a large academic medical center at the epicenter of COVID-19. Acad Pathol. 2021;8. doi: 10.1177/2374289521994248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Monroig-Bosque PDC, Hsu JW, Lin MS, et al. Pathology trainee redeployment and education during the COVID-19 pandemic: an institutional experience. Acad Pathol. 2020;7. doi: 10.1177/2374289520953548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vossoughi S, Winters JL, Burgstaler EA, Schwartz J. The ABC’s of disaster management: managing apheresis operations during the SARS-CoV-2 pandemic. J Clin Apher. 2020;35:243–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hassell LA, Peterson J, Pantanowitz L. Pushed across the digital divide: COVID-19 accelerated pathology training onto a new digital learning curve. Acad Pathol. 2021;8. doi: 10.1177/2374289521994240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lieberman JA, Nester T, Emrich B, Staley EM, Bourassa LA, Tsang HC. Coping with COVID-19. Am J Clin Pathol. 2021;155:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mindiola Romero AE, Black CC, Jackson CR. Overcoming educational challenges and impact of COVID-19 in a pathology residency program. Acad Pathol. 2021;8. doi: 10.1177/2374289521994235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Solanki M, Bowler C, Gilbertson T, et al. Using multiple educational tools for conducting virtual surgical pathology fellowship interviews—innovation in the COVID era. Paper Presented at: USCAP; March 13-18 2021, 2021; Virtual.
- 8. Balakrishnan R, Singh K, Harigopal M, Fineberg S. A novel Google classroom-based pathology education tool for trainees during the COVID-19 pandemic: impactful learning while social distancing. Arch Pathol Lab Med. 2020;144:1445b–1447b. [DOI] [PubMed] [Google Scholar]
- 9. Ahmad Z, Rahim S, Ud Din N, Ahmed A. Practice of academic surgical pathology during the COVID-19 pandemic. Am J Clin Pathol. 2020;154:724–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Parker EU, Chang O, Koch L. Remote anatomic pathology medical student education in Washington State. Am J Clin Pathol. 2020;154:585–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Henriksen J, Kolognizak T, Houghton T, et al. Rapid validation of telepathology by an academic neuropathology practice during the COVID-19 pandemic. Arch Pathol Lab Med. 2020;144:1311–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Samuelson MI, Chen SJ, Boukhar SA, et al. Rapid validation of whole-slide imaging for primary histopathology diagnosis. Am J Clin Pathol. 2021;155:638–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mukhopadhyay S, Booth AL, Calkins SM, et al. Leveraging technology for remote learning in the era of COVID-19 and social distancing. Arch Pathol Lab Med. 2020;144:1027–1036. [DOI] [PubMed] [Google Scholar]