Abstract
Objective
To identify whether active use of nonsteroidal antiinflammatory drugs (NSAIDs) increases susceptibility to developing suspected or confirmed coronavirus disease 2019 (COVID‐19) compared to the use of other common analgesics.
Methods
We performed a propensity score–matched cohort study with active comparators, using a large UK primary care data set. The cohort consisted of adult patients age ≥18 years with osteoarthritis (OA) who were followed up from January 30 to July 31, 2020. Patients prescribed an NSAID (excluding topical preparations) were compared to those prescribed either co‐codamol (paracetamol and codeine) or co‐dydramol (paracetamol and dihydrocodeine). A total of 13,202 patients prescribed NSAIDs were identified, compared to 12,457 patients prescribed the comparator drugs. The primary outcome measure was the documentation of suspected or confirmed COVID‐19, and the secondary outcome measure was all‐cause mortality.
Results
During follow‐up, the incidence rates of suspected/confirmed COVID‐19 were 15.4 and 19.9 per 1,000 person‐years in the NSAID‐exposed group and comparator group, respectively. Adjusted hazard ratios for suspected or confirmed COVID‐19 among the unmatched and propensity score–matched OA cohorts, using data from clinical consultations in primary care settings, were 0.82 (95% confidence interval [95% CI] 0.62–1.10) and 0.79 (95% CI 0.57–1.11), respectively, and adjusted hazard ratios for the risk of all‐cause mortality were 0.97 (95% CI 0.75–1.27) and 0.85 (95% CI 0.61–1.20), respectively. There was no effect modification by age or sex.
Conclusion
No increase in the risk of suspected or confirmed COVID‐19 or mortality was observed among patients with OA in a primary care setting who were prescribed NSAIDs as compared to those who received comparator drugs. These results are reassuring and suggest that in the absence of acute illness, NSAIDs can be safely prescribed during the ongoing pandemic.
INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS–CoV‐2), was originally declared a public health emergency on January 30, 2020 (1). Since then, the disease has led to the deaths of >700,000 individuals globally (2). Nonsteroidal antiinflammatory drugs (NSAIDs) are widely used to help control pain in chronic diseases such as osteoarthritis (OA) and are often used in groups at high risk for COVID‐19, including older populations. However, concerns have been raised regarding the use of NSAIDs in the treatment of SARS–CoV‐2 infection, particularly after the French Health Minister suggested in March 2020 that NSAIDs might aggravate the infection. Pre‐pandemic evidence has also suggested a potential association between the use of NSAIDs and prolonged or complicated courses of respiratory infection (3, 4, 5, 6, 7).
Furthermore, biologic data raise the possibility of increased risk for COVID‐19. Entry of SARS–CoV‐2 into host cells is dependent on its receptor, angiotensin‐converting enzyme 2 (ACE2) (8), as well as priming of the S protein by transmembrane protease serine 2 (9). Single‐cell RNA sequencing has demonstrated ACE2 messenger RNA expression across multiple epithelial cell types throughout the human body, most notably in the nasal epithelium (10). It has been speculated that ibuprofen, one of the most commonly used NSAIDs, could up‐regulate ACE2 expression and thereby increase susceptibility to SARS–CoV‐2 (11). A single study has previously demonstrated ACE2 up‐regulation in the cardiac tissue in response to ibuprofen in a rat model of diabetes (12). It is unknown if these results would translate to the specific cell types of interest in humans and thereby promote susceptibility to SARS–CoV‐2.
Despite these concerns, NSAIDs have remained an important therapeutic approach to the management of pain, including among older patients (13). However, data on the effects of NSAIDs on susceptibility to SARS–CoV‐2 remain sparse, especially in older cohorts. Both the National Health Service in England and the World Health Organization have conducted rapid reviews to examine the association between the use of NSAIDs and susceptibility to and severity of COVID‐19 (14, 15). In both reviews it was concluded that there was no clear association between NSAIDs and these outcomes but they noted that the evidence was scarce. Several studies examined the impact of NSAIDs on the disease course in patients with COVID‐19 (16, 17), including those with acute respiratory distress syndrome (18). However, smaller‐scale clinical studies to date have been unable to adequately investigate whether use of NSAIDs could confer susceptibility to infection due to SARS–CoV‐2. Challenges in the design of studies attempting to address this concern include selection bias, as well as an inability to account for confounding by indication bias.
To address this question, we conducted a retrospective cohort study exploring the association between NSAID use and the subsequent development of COVID‐19, using real‐world data from primary care (6).
PATIENTS AND METHODS
Study design
This was a population‐based retrospective propensity score–matched cohort study of patients with OA, comparing the risk of suspected or confirmed COVID‐19 infection among patients prescribed an NSAID (excluding topical preparations) to those prescribed either co‐codamol or co‐dydramol as active comparators.
Data source
This cohort study used patient data derived from The Health Improvement Network (THIN) database. The steps involved in data extraction were facilitated by the Data Extraction for Epidemiological Research tool (19). THIN is a collection of routinely collected primary care data from UK general practices, which use Vision electronic medical records software (20). In 2020, THIN included data on ~2.1 million active patients from 357 practices. The database is representative of the UK population in terms of demographic structure and prevalence of key comorbidities (21).
THIN has been used on numerous occasions in pharmacoepidemiologic studies to examine health outcomes and mortality risk in patients with OA or to assess drug safety during the COVID‐19 pandemic (22, 23, 24, 25, 26, 27). Symptoms, examinations, and diagnoses in THIN are recorded using a hierarchical clinical coding system called Read codes (28). Prescriptions are recorded based on the Dictionary of Medicines and Devices and Anatomical Therapeutic Classification systems (29, 30). In order to reduce the underrecording of events, general practices were included 12 months following their installment of electronic practice records or from the practice’s acceptable mortality recording date (31).
Study population
Adults age ≥18 years with a diagnosis of OA who had been registered with an eligible general practice for at least 1 year on or before January 30, 2020 (index date) were included. Patients with OA were specifically selected because they commonly take NSAIDs and other analgesics for chronic pain management, and selecting a specific population group helps to limit confounding by indication bias from other chronic pain conditions that may have differential risks for COVID‐19. Patients with a record of rheumatoid arthritis, systemic lupus erythematosus, juvenile arthritis, enteropathic arthritis, reactive arthritis, scleroderma, or ankylosing spondylitis were thus excluded. In addition, patients with a history of gastrointestinal bleeding, peptic ulcers, or allergy or adverse reactions to NSAIDs were also excluded.
Definition of exposed group and comparator group
Current users of NSAIDs or comparator drugs (co‐codamol/co‐dydramol) were defined as patients with prescriptions that lasted beyond the index date or those with prescriptions that lasted until 90 days preceding the index date and with evidence of further prescription during the pandemic period. NSAIDs included those in chapter 10.1.1 in the British National Formulary, such as ibuprofen, naproxen, and diclofenac, but excluded aspirin 300 mg due to a difference in the biologic mechanism of action (32). The complete list of NSAIDs included in the study is shown in Supplementary Table 1 (available on the Arthritis & Rheumatology website at http://onlinelibrary.wiley.com/doi/10.1002/art.41593/abstract).
Patients with OA with a current prescription for an NSAID (exposed group) were compared to patients with a current prescription for co‐codamol or co‐dydramol (comparator group). The 2 groups were mutually exclusive; patients with a current prescription for both medications were excluded from the study. Co‐codamol and co‐dydramol are analgesics that are alternative treatment options for the management of pain in patients with OA and have not been implicated in increasing susceptibility to COVID‐19. While there is some evidence that opiates have immunosuppressive properties and may increase the risk of community‐acquired pneumonia, this is only clinically evident in patients who are receiving doses of opiates above the equivalent of 20 mg of morphine daily (33). This is greater than the dose of opiates that patients in our active comparator cohort would be exposed to from taking co‐codamol or co‐dydramol.
Matching
Using data from the index date, participants in the exposed group were propensity score matched to participants in the comparator group. Propensity scores for the use of NSAIDs were estimated using a logistic regression model including a set of covariates as described below. To ensure positivity (having adequate variation in the treatment of interest within confounder strata), propensity scores were truncated and only participants with propensity scores that fell within the common support region using a caliper width of 0.2 were eligible for matching. Participants in the exposed group were then matched 1:1 to patients taking comparator drugs, by propensity score using the nearest neighbor algorithm.
Follow‐up period
Patients were followed up from January 30, 2020 (index date) until the earliest of the following dates: date of the outcome, date of death, date patient left practice/data set, date practice ceased contributing to the database, or study end date (July 31, 2020). The latest available covariate data recorded on or before the index date were used to calculate propensity scores and to adjust for covariates in the analysis.
Outcome measures
The primary outcome measure was a composite of confirmed or clinician‐suspected diagnoses of COVID‐19. The secondary outcome measure was the risk of all‐cause mortality and was limited to confirmed COVID‐19 cases in a sensitivity analysis. The outcome measures were defined using the relevant clinical Read codes listed in Supplementary Table 2 (available on the Arthritis & Rheumatology website at http://onlinelibrary.wiley.com/doi/10.1002/art.41593/abstract).
Covariates
The latest available covariate data recorded prior to the index date were obtained and used for propensity score matching and adjustment in the outcome model. The list of covariates included currently known risk factors for the development of COVID‐19 (34). These included 1) sociodemographic characteristics (age and sex); 2) lifestyle and metabolic profile measures (smoking status, body mass index [BMI], systolic and diastolic blood pressure, and estimated glomerular filtration rate); and 3) presence of comorbid conditions such as type 2 diabetes mellitus, cardiovascular disease (peripheral vascular disease, stroke, ischemic heart disease, and heart failure), atrial fibrillation, asthma, chronic obstructive pulmonary disease, cancer, liver disease (mild, moderate, and severe), psoriasis, neurologic disorders (Parkinson’s disease, motor neuron disease, multiple sclerosis, myasthenia gravis, and epilepsy), dementia, vitamin D deficiency, solid organ transplant, and use of immunosuppressive drug therapies.
Smoking status was categorized as nonsmoker, ex‐smoker, or current smoker. BMI was categorized as <25 kg/m2 (normal/underweight), 25–30 kg/m2 (overweight), >30–35 kg/m2 (obese), or >35 kg/m2 (severely obese). Physiologic and laboratory measures were categorized into appropriate clinically meaningful groups. All covariates listed above were included in the propensity score matching process and for adjustment in the analysis.
Missing data
Missing values for smoking status and physiologic/laboratory measures were treated as a separate missing category for each variable. The absence of a record of any diagnosis was taken to indicate the absence of the condition.
Statistical analysis
Descriptive statistics were used to describe the exposed and comparator groups and were described for both groups before and after propensity score matching. Histograms of propensity scores in the exposed and the comparator groups were generated before and after matching, for a visual check of the global balance of propensity scores between the 2 groups.
Crude incidence rates per 1,000 person‐years for the primary and secondary outcome measures were estimated for the exposed and comparator cohorts. A Cox proportional hazards regression model was used to determine crude incidence rates and adjusted hazard ratios (HRs) for NSAIDs compared to the comparator drugs for the outcome measure. Survival curves in the exposed and the comparator groups were generated for the unmatched and the propensity score–matched cohorts.
Subgroup analysis
Two subgroup analyses were conducted to assess for differential associations between COVID‐19 and NSAID use by age (<65 years versus ≥65 years) and sex. Both older age and male sex have previously been identified as risk factors for COVID‐19, and we investigated whether this extended to differential effects from NSAID exposure (34).
RESULTS
Study population
We identified 13,202 eligible patients with OA with a current prescription for an NSAID and 12,457 patients with a current prescription for comparator drugs (co‐codamol or co‐dydramol) (Figure 1).
Figure 1.
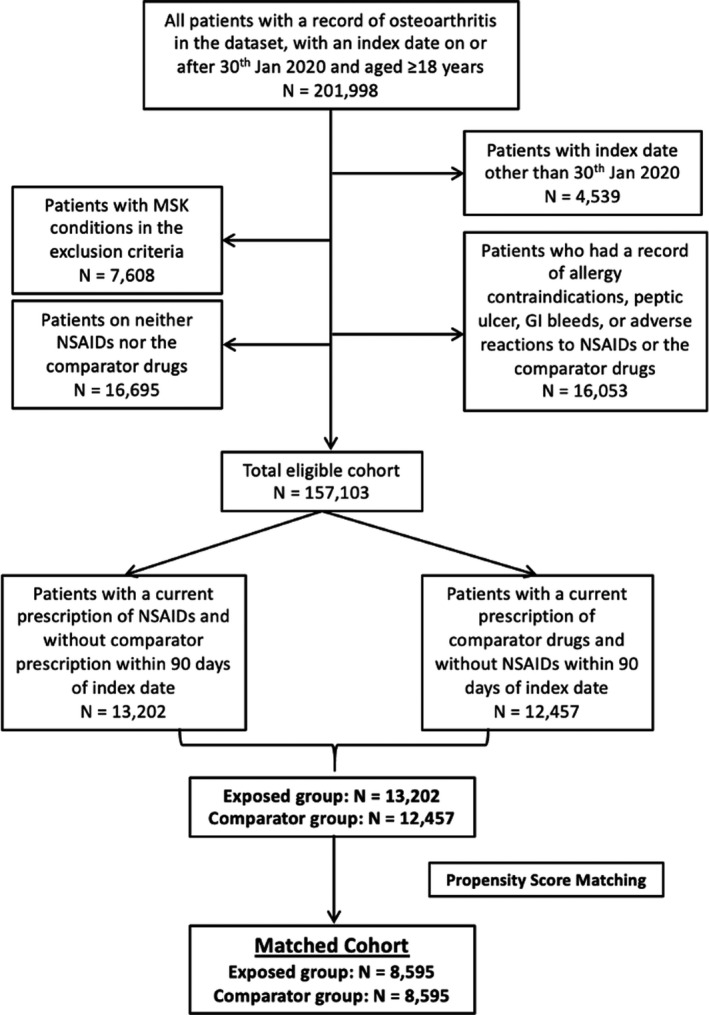
Flow chart showing disposition of the osteoarthritis patients in each group. MSK = musculoskeletal; NSAIDs = nonsteroidal antiinflammatory drugs; GI = gastrointestinal.
Baseline characteristics
In the unmatched cohort (13,202 exposed patients compared to 12,457 comparator patients), the NSAID cohort was younger (mean age 65.4 versus 71.7 years) and had a greater proportion of men (37.8% versus 33.4%) compared to the comparator cohort (Table 1). Compared to the comparator cohort, the NSAID cohort had similar proportions of current smokers and a similar mean BMI. However, those taking NSAIDs had a lower prevalence of comorbidities compared to those taking the comparator drugs, including cardiovascular disease, diabetes, respiratory disease, and cancers.
Table 1.
Baseline characteristics of the study population*
| Unmatched cohort | Matched cohort | |||
|---|---|---|---|---|
|
NSAID (n = 13,202) |
Comparator (n = 12,457) |
NSAID (n = 8,595) |
Comparator (n = 8,595) |
|
| Male sex, no. (%) | 4,992 (37.8) | 4,156 (33.4) | 2,990 (34.8) | 2,938 (34.2) |
| Age, years | 65.35 ± 10.7 | 71.71 ± 11.3 | 68.39 ± 10.4 | 68.08 ± 10.5 |
| Age categories, no. (%) | ||||
| <40 years | 123 (0.9) | 69 (0.6) | 48 (0.6) | 66 (0.8) |
| 40–49 years | 727 (5.5) | 308 (2.5) | 283 (3.3) | 297 (3.5) |
| 50–59 years | 3,097 (23.5) | 1,420 (11.4) | 1,372 (16.0) | 1,380 (16.1) |
| 60–69 years | 4,539 (34.4) | 3,177 (25.5) | 2,825 (32.9) | 2,810 (32.7) |
| 70–79 years | 3,484 (26.4) | 4,219 (33.9) | 2,867 (33.4) | 2,859 (33.3) |
| ≥80 years | 1,232 (9.3) | 3,264 (26.2) | 1,200 (14.0) | 1,183 (13.8) |
| Smoking status, no. (%) | ||||
| Nonsmoker | 6,995 (53.0) | 5,966 (47.9) | 4,294 (50.0) | 4,335 (50.4) |
| Ex‐smoker | 4,285 (32.5) | 4,653 (37.4) | 3,004 (35.0) | 2,962 (34.5) |
| Smoker | 1,824 (13.8) | 1,798 (14.4) | 1,259 (14.7) | 1,271 (14.8) |
| Missing data | 98 (0.7) | 40 (0.3) | 38 (0.4) | 27 (0.3) |
| BMI, kg/m2 | 31.03 ± 6.9 | 30.77 ± 7.0 | 30.86 ± 6.9 | 31.09 ± 7.1 |
| BMI categories, no. (%) | ||||
| Normal/underweight (<25) | 2,290 (17.4) | 2,352 (18.9) | 1,535 (17.9) | 1,523 (17.7) |
| Overweight (25–30) | 4,152 (31.5) | 3,906 (31.4) | 2,726 (31.7) | 2,703 (31.5) |
| Obese (>30) | 6,287 (47.6) | 5,908 (47.4) | 4,105 (47.8) | 4,144 (48.2) |
| Missing data | 473 (3.6) | 291 (2.3) | 229 (2.7) | 225 (2.6) |
| Systolic BP, mm Hg | 133.6 ± 14.5 | 133.8 ±14.9 | 133.9 ± 14.5 | 134.2 ± 14.5 |
| Diastolic BP, mm Hg | 78.43 ± 9.1 | 76.60 ± 9.5 | 77.62 ± 9.05 | 77.88 ± 9.19 |
| eGFR, ml/minute | 84.6 ± 18.74 | 79.9 ± 21.55 | 83.1 ± 19.4 | 84.4 ± 19.3 |
| eGFR category, no. (%) | ||||
| >90 (stage 1) | 4,478 (33.9) | 3,601 (28.9) | 2,797 (32.5) | 2,875 (33.5) |
| 60–90 (stage 2) | 7,494 (56.8) | 6,761 (54.3) | 4,853 (56.5) | 4,969 (57.8) |
| 30–59 (stage 3) | 833 (6.3) | 1,830 (14.7) | 764 (8.9) | 598 (7.0) |
| <30 (stage 4) | 13 (0.1) | 92 (0.7) | 13 (0.2) | 2 (0.0) |
| Missing data | 384 (2.9) | 173 (1.4) | 168 (2.0) | 151 (1.8) |
| Baseline conditions, no. (%) | ||||
| AF | 264 (2.0) | 1,309 (10.5) | 263 (3.1) | 70 (0.8) |
| CVD | 1,221 (9.3) | 3,146 (25.3) | 1,173 (13.7) | 831 (9.7) |
| Diabetes | 1,707 (12.9) | 2,816 (22.6) | 1,460 (17.0) | 1,364 (15.9) |
| Dementia | 114 (0.9) | 358 (2.9) | 110 (1.3) | 63 (0.7) |
| Vitamin D deficiency | 249 (1.9) | 375 (3.0) | 202 (2.4) | 186 (2.2) |
| Cancer | 1,188 (9.0) | 1,509 (12.1) | 921 (10.7) | 895 (10.4) |
| Liver disease | 297 (2.3) | 392 (3.2) | 242 (2.8) | 243 (2.8) |
| Asthma | 2,147 (16.3) | 2,488 (20.0) | 1,524 (17.7) | 1,526 (17.8) |
| Psoriasis | 740 (5.6) | 1,506 (12.1) | 694 (8.1) | 610 (7.1) |
| COPD | 740 (5.6) | 1,506 (12.1) | 694 (8.1) | 610 (7.1) |
| Neurologic disorders† | 144 (1.1) | 170 (1.4) | 107 (1.2) | 112 (1.3) |
| Solid organ transplant | 1 (0.0) | 6 (0.1) | 1 (0.0) | 0 (0) |
| Immunologic therapies | 80 (0.6) | 91 (0.7) | 60 (0.7) | 59 (0.7) |
| NSAID use 1 year prior to index date | 4,108 (31.12) | 1,857 (14.91) | 2,769 (32.22) | 1,575 (18.32) |
Except where indicated otherwise, values are the mean ± SD. NSAID = nonsteroidal antiinflammatory drug; BMI = body mass index; BP = blood pressure; eGFR = estimated glomerular filtration rate; AF = atrial fibrillation; CVD = cardiovascular disease; COPD = chronic obstructive pulmonary disease.
Neurologic disorders: Parkinson’s disease, motor neuron disease, multiple sclerosis, myasthenia gravis, and epilepsy.
Following 1:1 propensity score matching, 8,595 eligible patients prescribed NSAIDs were compared to 8,595 matched patients prescribed co‐codamol or co‐dydramol. After matching, the demographic and clinical characteristics of both cohorts were very similar (Table 1).
Primary and secondary outcome measures
In the unmatched cohort during the follow‐up period, 101 individuals in the exposed group (current NSAID users only) and 122 in the comparator group (current co‐codamol or co‐dydramol users only) were diagnosed as having suspected or confirmed COVID‐19, corresponding to crude incidence rates (IRs) of 15.4 and 19.9 per 1,000 person‐years, respectively (Table 2). After adjustment for potential confounders, no statistically significant difference in the risk of confirmed or suspected COVID‐19 was observed in users of NSAIDs compared to users of the comparator drugs (adjusted HR 0.82 [95% CI 0.62–1.10]; Figure 2 and Supplementary Figure 1, available on the Arthritis & Rheumatology website at http://onlinelibrary.wiley.com/doi/10.1002/art.41593/abstract).
Table 2.
Risk of developing COVID‐19 or death in patients with osteoarthritis prescribed NSAIDs compared to those who received co‐codamol or co‐dydramol (comparator)*
| Unmatched patients | Propensity score–matched patients | |||||||
|---|---|---|---|---|---|---|---|---|
| Outcome | NSAID‐treated | Comparator |
Unadjusted HR (95% CI) |
Adjusted HR (95% CI)† |
NSAID‐ treated |
Comparator |
Unadjusted HR (95% CI) |
Adjusted HR (95% CI)† |
| Suspected/confirmed COVID‐19 | ||||||||
| n | 13,202 | 12,457 | 8,595 | 8,595 | ||||
| Outcome events, no. (%) | 101 (0.77) | 122 (0.98) | 63 (0.73) | 76 (0.88) | ||||
| Person‐years | 6,551 | 6,127 | 4,263 | 4,254 | ||||
| Crude IR/1,000 person‐years | 15.4 | 19.9 | 14.8 | 17.9 | ||||
| HR (95% CI) | 0.77 (0.59–1.01)‡ | 0.82 (0.62–1.10) | 0.83 (0.59–1.16) | 0.79 (0.57–1.11) | ||||
| Mortality | ||||||||
| n | 13,202 | 12,457 | 8,595 | 8,595 | ||||
| Outcome events, no. (%) | 92 (0.70) | 213 (1.71) | 79 (0.92) | 71 (0.83) | ||||
| Person‐years | 6,574 | 6,151 | 4,276 | 4,270 | ||||
| Crude IR/1,000 person‐years | 14.0 | 34.6 | 18.5 | 16.6 | ||||
| HR (95% CI) | 0.40 (0.32–0.52)§ | 0.97 (0.75–1.27) | 1.11 (0.81–1.53) | 0.85 (0.61–1.20) | ||||
COVID‐19 = coronavirus disease 2019; NSAIDs = nonsteroidal antiinflammatory drugs; HR = hazard ratio; IR = incidence rate.
Adjusted for age, sex, body mass index categories, smoking status, estimated glomerular filtration rate categories, systolic and diastolic blood pressure, type 2 diabetes mellitus, atrial fibrillation, cancer, vitamin D deficiency, cardiovascular disease (peripheral vascular disease, stroke, ischemic heart disease, and heart failure), dementia, liver disease (mild, moderate, and severe), asthma, chronic obstructive pulmonary disease, solid organ transplants, use of immunologic drug therapies, psoriasis, and other neurologic disorders (Parkinson’s disease, motor neuron disease, multiple sclerosis, and myasthenia gravis).
P = 0.06.
P < 0.01.
Figure 2.

Adjusted hazard ratio (aHR) (with 95% confidence interval [95% CI]) for developing suspected/confirmed coronavirus disease 2019 (COVID‐19) or mortality following medication use in both the exposed group and the comparator group. Color figure can be viewed in the online issue, which is available at http://onlinelibrary.wiley.com/doi/10.1002/art.41593/abstract.
During the follow‐up period, 92 patients in the exposed group died (IR 14.0 per 1,000 person‐years), compared to 213 patients in the comparator group (IR 34.6 per 1,000 person‐years). However, following adjustment for confounders, there was no significant difference in mortality between groups (adjusted HR 0.97 [95% CI 0.75–1.27]).
Following propensity score matching, 63 patients in the exposed group and 76 patients in the comparator group were diagnosed as having suspected or confirmed COVID‐19, corresponding to crude IRs of 14.8 and 17.9 per 1,000 person‐years, respectively. Similarly, no statistically significant difference in the risk of COVID‐19 was observed between the 2 groups following adjustment (adjusted HR 0.79 [95% CI 0.57–1.11]). In addition, there was no significant difference in the mortality risk between the groups (adjusted HR 0.85 [95% CI 0.61–1.20]).
Sensitivity analysis
In a sensitivity analysis where outcomes were restricted to only those presenting as confirmed cases of COVID‐19, the results remained similar to the main findings (Supplementary Table 3, available on the Arthritis & Rheumatology website at http://onlinelibrary.wiley.com/doi/10.1002/art.41593/abstract). When this exclusion criterion was applied to the cohort, there were no statistically significant differences in the risk of developing suspected/confirmed COVID‐19 between the exposed and comparator groups in the adjusted unmatched cohort analysis (adjusted HR 0.71 [95% CI 0.35–1.43]) and propensity score–matched cohort analysis (adjusted HR 0.69 [95% CI 0.29–1.61]).
Subgroup analysis
There was no significant difference in the risk of suspected/confirmed COVID‐19 between male patients who were prescribed NSAIDs compared to male patients who were prescribed the comparator drugs in either the unmatched cohort (adjusted HR 0.77 [95% CI 0.48–1.26]) or the propensity score–matched cohort (adjusted HR 0.72 [95% CI 0.40–1.28]) (Supplementary Table 4, available on the Arthritis & Rheumatology website at http://onlinelibrary.wiley.com/doi/10.1002/art.41593/abstract). The results were similar in female patients, both in the unmatched cohort (adjusted HR 0.86 [95% CI 0.60–1.23]) and in the propensity score–matched cohort (adjusted HR 0.83 [95% CI 0.55–1.26]).
No significant difference in the risk of all‐cause mortality was observed between the exposed and comparator groups among men in either the unmatched cohort (adjusted HR 0.83 [95% CI 0.55−1.27]) or the propensity score–matched cohort (adjusted HR 0.78 [95% CI 0.47−1.32]). The same was also true among women in either the unmatched cohort (adjusted HR 1.11 [95% CI 0.78−1.57]) or the propensity score–matched cohort (adjusted HR 0.94 [95% CI 0.59−1.48]) (Supplementary Table 4).
No statistically significant differences in the primary outcome measure were found after stratification by age (patients age <65 and ≥65 years). Among patients age <65 years, there was no significant difference in the risk of developing suspected/confirmed COVID‐19 between those prescribed NSAIDs compared to those prescribed the comparator drugs in either the unmatched cohort (adjusted HR 0.97 [95% CI 0.63–1.49]) or the propensity score–matched cohort (adjusted HR 0.93 [95% CI 0.57–1.51]) (Supplementary Table 5, http://onlinelibrary.wiley.com/doi/10.1002/art.41593/abstract). However, in those age ≥65 years, the adjusted HRs were lower, although not significantly so, when comparing the risk of developing suspected/confirmed COVID‐19 between the NSAID‐exposed and comparator groups in both the unmatched cohort (adjusted HR 0.73 [95% CI 0.49–1.09]) and the propensity score–matched cohort (adjusted HR 0.67 [95% CI 0.42–1.08]).
Similarly, among patients age <65 years, there were no differences in mortality risk between the NSAID‐exposed and comparator groups in either the unmatched cohort (adjusted HR 1.32 [95% CI 0.56−1.11]) or the propensity score–matched cohort (adjusted HR 1.12 [95% CI 0.42–3.01]). There were also no differences in mortality risk between the groups in patients age ≥65 years, either in the unmatched cohort (adjusted HR 0.95 [95% CI 0.71–1.26]) or the propensity score–matched cohort (adjusted HR 0.82 [95% CI 0.57–1.19]).
DISCUSSION
To our knowledge, this is the first population‐based cohort study accounting for confounding by indication bias as well as a wide range of other potential confounders to examine the effect of NSAIDs on subsequent development of suspected or confirmed COVID‐19 or mortality. We found no significant association between NSAID use and confirmed or suspected COVID‐19 or all‐cause mortality, when compared to use of co‐codamol or co‐dydramol in a large primary care cohort of patients with OA. Additionally, there was no significant difference in the association between NSAID use and the risk of suspected or confirmed COVID‐19 or mortality in men compared to women. Reassuringly, we also found no significant difference in the association between NSAID use and the risk of COVID‐19 or mortality in older patients compared to younger patients, although older NSAID users had a reduction, though not statistically significant, in risk of COVID‐19 compared to those prescribed comparator drugs. Overall, the data clearly show that the use of NSAIDs in this population was not associated with increased risk of infection or mortality.
SARS–CoV‐2 enters host cells via the ACE2 receptor, and NSAIDs may increase expression of this enzyme. Therefore, concerns were raised at the outset of the pandemic about the use of NSAIDs and susceptibility to COVID‐19. However, our findings do not support this conjecture. Indeed, there are parallels between our results and those from previous studies investigating the impact of ibuprofen on the severity of COVID‐19 in South Korea (16) and Denmark (17). In those studies, NSAIDs conferred no additional risk of morbidity or mortality. Interestingly, Lund et al also attempted to examine the impact of age and sex on COVID‐19 severity in patients taking NSAIDs compared to their matched controls. They identified no clear differences in outcomes across age or sex, although the study may not have been sufficiently powered to identify these as potential effect modifiers (17).
Our study supports these findings, demonstrating that there is no increased risk of susceptibility to COVID‐19 across age or sex in patients taking NSAIDs. This is important because older patients are at a substantially higher risk of developing COVID‐19 and have a poorer prognosis (34). These results are also reassuring given the high prevalence of NSAID use in this age group (35). Our findings will need to be confirmed in other cohorts, as we restricted our analysis to patients with preexisting OA to reduce the risk of confounding by indication and immortal time bias. Further research into the impact of NSAIDs on the expression of the ACE2 receptor and consequent susceptibility to SARS–CoV‐2 in relevant human cell types is also urgently required.
Although not targeted at population‐based use, the LIBERATE trial is currently exploring outcomes in patients given lipid ibuprofen versus standard care for acute hypoxemic respiratory failure due to COVID‐19 (18). The findings of this trial will help confirm whether NSAIDs could be of benefit in the management of severe COVID‐19.
Our study had several limitations. This was an observational, retrospective cohort study and is therefore prone to the effect of unmeasured confounding and confounding by indication bias. However, we used a propensity score–matched design to minimize the effect of a large number of potential confounders. We also attempted to limit confounding by indication bias by the inclusion of a carefully selected population group commonly prescribed the drugs of interest. The study also explored potential interactions by age and sex. The majority of studies on COVID‐19 are based in secondary care settings, and this study is also one of the few that has explored susceptibility to COVID‐19 in a primary care setting.
An important limitation of our study relates to data quality, as the use of electronic health records for epidemiologic research largely relies on the accuracy of documentation by health care professionals. While prescription data are adequately recorded in primary care, we could not account for NSAIDs purchased without a prescription nor could we verify medication compliance. However, we anticipate that a large proportion of patients taking NSAIDs for chronic pain associated with OA would receive this by prescription. Although we do not have details relating to patterns of NSAID prescription prior to study entry, we have been able to report the proportion of patients who had at least 1 recorded prescription for NSAIDs in the year preceding the index date (Table 1).
As the data were derived from a primary care setting, we did not have data on hospitalization, inpatient management, or cause‐specific mortality. Additionally, we were unable to access data relating to socioeconomic status, an important risk factor associated with outcomes of COVID‐19 (34). Our study was also limited by the number of outcome events, which were insufficient to explore effects of different types or doses of NSAIDs (36).
Our findings suggest that prescriptions of NSAIDs (excluding topical preparations) in primary care does not increase susceptibility to COVID‐19 or all‐cause mortality, including in older patients. These findings are reassuring given the high prevalence of NSAID use in at‐risk groups. Further research is needed to investigate whether the use of NSAIDs is associated with adverse outcomes from COVID‐19 in patients with confirmed SARS–CoV‐2 infection and whether risks differ by NSAID type and dose.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Chandan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Chandan, Zemedikun, Thayakaran, Gokhale, Thomas, Sainsbury, Subramanian, Cooper, Anand, Okoth, Wang, Adderley, Taverner, Denniston, Lord, Thomas, Buckley, Raza, Bhala, Nirantharakumar, Haroon.
Acquisition of data
Chandan, Zemedikun, Thayakaran, Byne, Dhalla, Acosta‐Mena, Gokhale.
Analysis and interpretation of data
Chandan, Zemedikun, Thayakaran, Gokhale, Subramanian, Wang.
ADDITIONAL DISCLOSURES
Authors Byne, Dhalla, and Acosta‐Mena are employees of Cegedim Rx.
Supporting information
Supplementary Material
The views expressed are those of the authors and not necessarily those of the MRC, Arthritis Research UK, or Health Data Research UK.
Supported in part by the MRC‐ARUK Centre for Musculoskeletal Ageing Research. Drs. Lord, Buckley, and Raza’s work was supported in part by the NIHR Birmingham Biomedical Research Centre. Dr. Nirantharakumar’s work was supported by Health Data Research UK.
Drs. Chandan, Zemedikun, and Thayakaran contributed equally to this work. Drs. Raza, Bhala, Nirantharakumar, and Haroon contributed equally to this work.
No potential conflicts of interest relevant to this article were reported.
Contributor Information
Karim Raza, Email: k.raza@bham.ac.uk.
Krishnarajah Nirantharakumar, Email: k.nirantharan@bham.ac.uk.
References
- 1. World Health Organization . Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019‐nCoV). January 2020. URL: https://www.who.int/news‐room/detail/30‐01‐2020‐statement‐on‐the‐second‐meeting‐of‐the‐international‐health‐regulations‐(2005)‐emergency‐committee‐regarding‐the‐outbreak‐of‐novel‐coronavirus‐(2019‐ncov).
- 2. John Hopkins University . COVID‐19 Cashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). URL: https://coronavirus.jhu.edu/map.html.
- 3. Basille D, Thomsen RW, Madsen M, Duhaut P, Andrejak C, Jounieaux V, et al. Nonsteroidal antiinflammatory drug use and clinical outcomes of community‐acquired pneumonia. Am J Respir Crit Care Med 2018;198:128–31. [DOI] [PubMed] [Google Scholar]
- 4. Le Bourgeois M, Ferroni A, Leruez‐Ville M, Varon E, Thumerelle C, Brémont F, et al. Nonsteroidal anti‐inflammatory drug without antibiotics for acute viral infection increases the empyema risk in children: a matched case‐control study. J Pediatr 2016;175:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Voiriot G, Philippot Q, Elabbadi A, Elbim C, Chalumeau M, Fartoukh M. Risks related to the use of non‐steroidal anti‐inflammatory drugs in community‐acquired pneumonia in adult and pediatric patients [review]. J Clin Med 2019;8:786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Day M. Covid‐19: ibuprofen should not be used for managing symptoms, say doctors and scientists. BMJ 2020;368:m1086. [DOI] [PubMed] [Google Scholar]
- 7. Little P. Non‐steroidal anti‐inflammatory drugs and COVID‐19 [editorial]. BMJ 2020;368:m1185. [DOI] [PubMed] [Google Scholar]
- 8. Zhou P, Lou YX, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020;579:270–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hoffmann M, Kleine‐Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS‐CoV‐2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020;181:271–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M, et al. SARS‐CoV‐2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med 2020;26:681–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID‐19 infection? [letter]. Lancet Respir Med 2020;8:e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Qiao W, Wang C, Chen B, Zhang F, Liu Y, Lu Q, et al. Ibuprofen attenuates cardiac fibrosis in streptozotocin‐induced diabetic rats. Cardiology 2015;131:97–106. [DOI] [PubMed] [Google Scholar]
- 13. COVIDSurg Collaborative . Elective surgery cancellations due to the COVID‐19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg 2020;107:1440–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. NHS England . Acute use of non‐steroidal anti‐inflammatory drugs (NSAIDs) in people with or at risk of COVID‐19. April 2020. URL: https://www.england.nhs.uk/coronavirus/publication/acute‐use‐of‐non‐steroidal‐anti‐inflammatory‐drugs/.
- 15. World Health Organization . The use of non‐steroidal anti‐inflammatory drugs (NSAIDs) in patients with COVID‐19. April 2020. URL: https://www.who.int/publications/i/item/the‐use‐of‐non‐steroidal‐anti‐inflammatory‐drugs‐(nsaids)‐in‐patients‐with‐covid‐19.
- 16. Jeong HE, Lee H, Shin HJ, Choe YJ, Filion KB, Shin JY. Association between NSAIDs use and adverse clinical outcomes among adults hospitalised with COVID‐19 in South Korea: a nationwide study. Clin Infect Dis 2020. E‐pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lund LC, Kristensen KB, Reilev M, Christensen S, Thomsen RW, Christiansen CF, et al. Adverse outcomes and mortality in users of non‐steroidal anti‐inflammatory drugs tested positive for SARS‐CoV‐2: a Danish nationwide cohort study. PLoS Med 2020;17:e1003308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. King’s College London, sponsor . LIBERATE Trial in COVID‐19 (LIBERATE). ClinicalTrials.gov identifier: NCT04334629; 2020.
- 19. Gokhale KM, Chandan JS, Toulis K, Gkoutos G, Tino P, Nirantharakumar K. Data extraction for epidemiological research (DExtER): a novel tool for automated clinical epidemiology studies. Eur J Epidemiol 2020. E‐pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. THIN: The Health Improvement Network. URL: https://www.the‐health‐improvement‐network.com/en/.
- 21. Blak BT, Thompson M, Dattani H, Bourke A. Generalisability of The Health Improvement Network (THIN) database: demographics, chronic disease prevalence and mortality rates. Inform Prim Care 2011;19:251–5. [DOI] [PubMed] [Google Scholar]
- 22. Zeng C, Dubreuil M, Larochelle MR, Lu N, Wei J, Choi HK, et al. Association of tramadol with all‐cause mortality among patients with osteoarthritis. JAMA 2019;321:969–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dubreuil M, Louie‐Gao Q, Peloquin CE, Choi HK, Zhang Y, Neogi T. Risk of myocardial infarction with use of selected non‐steroidal anti‐inflammatory drugs in patients with spondyloarthritis and osteoarthritis. Ann Rheum Dis 2018;77:1137–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wei J, Neogi T, Terkeltaub R, Fenves AZ, Zeng C, Misra D, et al. Thiazide diuretics and risk of knee replacement surgery among patients with knee osteoarthritis: a general population‐based cohort study. Osteoarthritis Cartilage 2019;27:1454–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wei J, Wood MJ, Dubreuil M, Tomasson G, LaRochelle MR, Zeng C, et al. Association of tramadol with risk of myocardial infarction among patients with osteoarthritis. Osteoarthritis Cartilage 2020;28:137–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sainsbury C, Wang J, Gokhale K, Acosta‐Mena D, Dhalla S, Byne N, et al. Sodium‐glucose co‐transporter‐2 inhibitors and susceptibility to COVID‐19: a population‐based retrospective cohort study. Diabetes Obes Metab 2021;23:263–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Haroon S, Subramanian A, Cooper J, Anand A, Gokhale K, Byne N, et al. Renin‐angiotensin system inhibitors and susceptibility to COVID‐19 in patients with hypertension: a propensity score‐matched cohort study in primary care. BMC Infect Dis 2021;21:262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Booth N. What are the Read Codes? Health Libr Rev 1994;11:177–82. [DOI] [PubMed] [Google Scholar]
- 29. World Health Organization . Anatomical Therapeutic Chemical (ATC) classification. URL: https://www.who.int/toolkits/atc‐ddd‐toolkit/atc‐classification.
- 30. National Health Service Business Services Authority . Dictionary of medicines and devices (dm+d). URL: https://www.nhsbsa.nhs.uk/pharmacies‐gp‐practices‐and‐appliance‐contractors/dictionary‐medicines‐and‐devices‐dmd.
- 31. Maguire A, Blak BT, Thompson M. The importance of defining periods of complete mortality reporting for research using automated data from primary care. Pharmacoepidemiol Drug Saf 2009;18:76–83. [DOI] [PubMed] [Google Scholar]
- 32. OpenPrescribing . 10.1.1: Non‐steroidal anti‐inflammatory drugs. URL: https://openprescribing.net/bnf/100101/.
- 33. Edelman EJ, Gordon KS, Crothers K, Akgün K, Bryant KJ, Becker WC, et al. Association of prescribed opioids with increased risk of community‐acquired pneumonia among patients with and without HIV. JAMA Intern Med 2019;179:297–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID‐19 death using OpenSAFELY. Nature 2020;584:430–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Davis JS, Lee HY, Kim J, Advani SM, Peng HL, Banfield E, et al. Use of non‐steroidal anti‐inflammatory drugs in US adults: changes over time and by demographic. Open Hear 2017;4:e000550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Baigent C, Bhala N, Emberson J, Merhi A, Abramson S, Arber N, et al. Vascular and upper gastrointestinal effects of non‐steroidal anti‐inflammatory drugs: meta‐analyses of individual participant data from randomised trials. Lancet 2013;382:769–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


