Abstract
Postauricular swelling is usually encountered in an emergency setting in otorhinolaryngology, resulting from complication of acute or chronic suppurative otitis media. Besides that, postauricular swelling may occur secondary to various other conditions including infectious disease, tumour, vascular malformation, granulomatous condition and even trauma. Children less than 2 years old are prone to fall and up to 10% sustain traumatic brain injury without any obvious signs of neurological deficit. We describe a rare case of a postauricular swelling in a toddler which turned out to be salmonella extradural abscess from an infected traumatic haematoma. The importance of high clinical suspicion especially in a child with a history of fall cannot be emphasised more because a missed brain abscess could lead to potentially life-threatening problems. We would like to highlight that meticulous history taking along with prompt assessment and intervention is prudent for a better prognosis and recovery.
Keywords: ear, nose and throat/otolaryngology, paediatrics
Background
Brain abscess (BA) has become a rare entity especially over the last decade due to better accessibility to healthcare treatments and greater emphasis to BA-associated conditions like HIV infection and other immunosuppressive disease. Parallel to that, intracranial infections secondary to Salmonella sp are even rarer and scarcely reported whereby less than 100 cases have been reported between 1884 and 2016.1 The reported precipitating factors of acquiring intracranial salmonella infections include primary or metastatic brain tumour, extradural or subdural haematoma, subarachnoid haemorrhage, previous neurosurgery, immunodeficiency and meningitis due to salmonellosis. We would like to illustrate a rare manifestation of extradural abscess caused by Salmonella sp in a toddler with neglected traumatic extradural haematoma presenting as postauricular swelling.
Case presentation
A previously healthy 1 year 5 months old boy was referred to the otorhinolaryngology team in the emergency department with a 1-day history of left postauricular swelling. According to the mother, 1 week prior to presentation the child had fever, lethargy, reduced oral intake and diarrhoea which lasted for 3 days. Otherwise, he had no history of ear infection, facial weakness, fitting or altered level of consciousness. Additionally, no nasal symptoms were noticed by mother.
Further history from the mother revealed a history of fall 2 months prior in which he sustained a chipped left lower incisor but she denied any head injury. However, as the child was active without any concerning symptoms, parents did not seek any medical treatment at that point.
On examination, the child was febrile, irritable and lethargic-looking. There was no obvious facial asymmetry. There was a fluctuant swelling occupying the left temporoparietal region measuring 2×3 cm, tender (figure 1). The overlying skin was mildly erythematous without any overlying punctum. The scalp was otherwise healthy with no signs of infection or trauma. The postauricular sulcus was preserved and the pinna was not protruding forward. Otoscopic examination revealed normal tympanic membrane bilaterally and there was no posterior ear canal wall sagging. There were multiple shotty left cervical lymph nodes palpable.
Figure 1.

Swelling at the left temporoparietal region measuring 2×3 cm.
Investigations
Blood investigations showed raised infective markers with raised white cell count of 18.6×109/L with predominant neutrophilia and C reactive protein of 194. Ultrasonography was initially contemplated with the impression of suppurative postauricular lymph node but due to the unusual presentation and disease severity, a contrast-enhanced CT (CECT) of brain was decided. CECT of the brain revealed a lentiform extradural collection with calcification and rim enhancement measuring 2.2 cm in maximal thickness causing mass effect and a communication through cortical discontinuity of the left temporal bone with the scalp (figure 2).
Figure 2.

Contrast-enhanced CT brain revealed lentiform extradural collection with calcification and rim enhancement.
Treatment
Child was subsequently referred to the neurosurgical team whereby he underwent left craniotomy and drainage of abscess. Intraoperatively, around 15 cc of pus was drained and the underlying temporalis muscle appeared contused with a 4 cm linear fracture found over the left temporal bone (figure 3). Additionally, blackish thick infected haematoma was removed (figure 4). Postoperatively the child recovered well. Pus sent for culture and sensitivity grew non-typhoidal Salmonella sp sensitive to ceftriaxone. Infectious disease team was consulted and the child completed 2 weeks of intravenous ceftriaxone and was discharged home with 3 weeks of oral clotrimazole.
Figure 3.

Linear fracture found over the left tempo-parietal bone.
Figure 4.
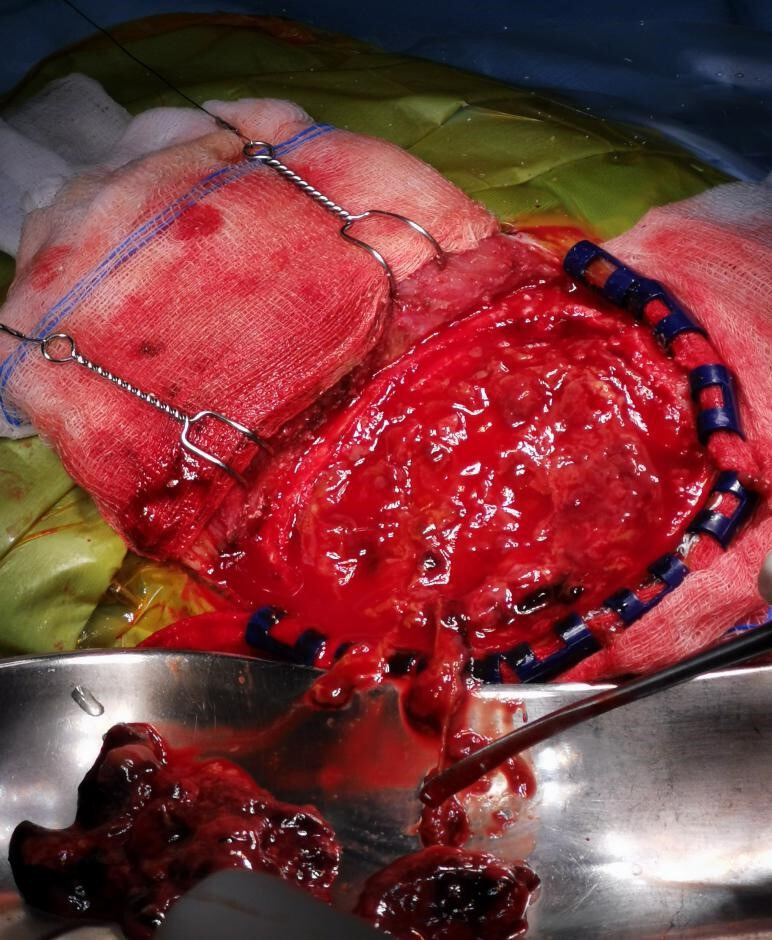
Infected extradural haematoma.
Outcome and follow-up
A repeated CECT brain at 6 weeks showed complete resolution of the abscess.
Discussion
Central nervous system (CNS) infections caused by Salmonella are fortunately rare as the mortality rate is relatively high between 15% and 18%.1 It is also associated with high treatment failures and substantial morbidities.2 The typical serotype in the western countries is non-typhoidal Salmonella which include Salmonella enteritidis and S. typhimurium whereas S. typhi continues to be the most common serotype associated with enteric fever in low-income and middle-income countries.3 Haematogenous seeding to the CNS by Salmonella during gastroenteritis is postulated to be the causative factor in most cases. Some of the predisposing disorders include diabetes mellitus, steroid use, immunosuppression, meningitis, pre-existing CNS disease or malignancy, subdural or extradural haematoma and sickle cell disease. Commonly, patients present with a triad of fever, bacteraemia and meningitis, ensued by focal neurological deficit and altered consciousness.4 However, in our case, the diagnosis was not apparent as the child did not show any sign of meningism or neurological deficit, similar to the report by Yen et al.5
Extradural abscess can occur either intracranially or in the spine in which they are distinctly different in terms of presentation and natural history. Intracranial extradural abscess is less common as compared with spinal extradural abscess and is usually associated with prior otitis media, mastoiditis or sinusitis. Nowadays, it is more common to arise as a complication of neurosurgical procedures. Organisms originating from the paranasal sinuses or ears are often from Streptococci, Cutibacterium and Peptostreptococcus species. Whereas, if the infection results from previous neurosurgery, the expected organisms would be Staphylococci and gram-negative bacteria. These organisms disseminate into extradural spaces from adjacent focus of infection or inoculation during trauma. In our case, transient bacteraemia could have led to infection of the extradural haematoma over the site of skull fracture. Often, the localised collection of pus would be surrounded by a wall of inflammatory reaction which may subsequently calcify necessitating excision during craniotomy and drainage as encountered in our case.
Temporal skull injury with extradural haematoma has a marked lucid interval. In children, they initially have decreased level of consciousness which then returns to normal alertness for several hours after which, the condition rapidly deteriorates as the blood gets accumulated in the epidural space causing compression to the brain parenchyma. Nevertheless, among young children especially in toddlers the lucid interval may be overlooked following the subtle changes.6 Our patient had a fall 2 months prior which he remained relatively asymptomatic until the infected intracranial haematoma developed into an abscess, resulting in fever and toxaemia. Extradural collection classically is diagnosed by the appearance of lentiform or biconvex mass that displaces the brain away from the skull on CECT brain. Emergent evaluation by neurosurgery team is warranted and patient should be prepared for craniotomy if they have worsening Glasgow Coma Scale, raised intracranial pressure, focal neurological deficit, large size of extradural haematoma (thickness >10 mm) and midline shift.7 In our patient, the collection measured more than 2 cm with midline shift which could have led to the decision of emergent craniotomy.
It is noteworthy that, although minor blunt head trauma is common among children less than 2 years of age, approximately 10% of children with minor blunt head trauma remain asymptomatic which are only detected on CT brain.8 Moreover, 1% of these children may develop significant traumatic brain injury, while 0.2% of children eventually need surgical intervention.9 Therefore, it is imperative that extra vigilance is exercised when dealing with young children with head injury. Scalp haematoma ought to be recognised as a tell-tale sign of traumatic brain injury until proven otherwise, especially if the haematoma is large and located within the temporal, parietal or occipital regions.10 The infant scalp score (table 1) was recently introduced as a validated tool to stratify infants at risk of traumatic brain injury while limiting unnecessary radiation exposure from neuroimaging.11 Infants younger than 1 year old, non-frontal location and larger size of scalp haematoma have been shown to have higher risk of skull fractures. Meanwhile, most of the skull fractures among these young children are linear and are associated with intracranial injuries in approximately 15–30% of cases.12
Table 1.
| Risk points | Patient age (months) | Hematoma size | Hematoma location |
| 0 | >12 | None | Frontal |
| 1 | 6–11 | Small (<1 cm) | Occipital |
| 2 | 3–5 | Medium (1–3 cm) | Temporal/parietal |
| 3 | 0–2 | Large (>3 cm) |
Lesson from this case, it is of paramount importance to exclude traumatic brain injury in a young child younger than 2 years old, especially if the child presents with scalp swelling although it is closely located to the postauricular region. Additionally, ultrasonography could have missed the underlying cortex breach, and subsequently the extradural collection and the underlying pathology would have been missed leading to a disastrous condition. It is also imperative to screen for non-accidental injuries, especially in a child with delayed scalp swelling presenting with red flag signs such as the facial, neck, trunk bruises, traumatic alopecia, intraoral injuries, genital injuries, complex family structure, history of domestic violence and family history of substance abuse.13 A skeletal survey will help to identify extracranial injuries in 30–70% of abused children.14 Nevertheless, multidisciplinary team discussion especially involving paediatrics, neurosurgery, otorhinolaryngologists, is crucial to determine the best management for the child, which will be life-saving.15
Learning points.
Traumatic epidural haematoma can be complicated with extradural abscess and may present with postauricular swelling.
To avoid this late complication, children with blunt head injury should be screened for traumatic brain injury even in the absence of neurological deficit especially if they are younger than 2 years of age.
Prompt neurosurgical drainage and long-term antibiotics will yield a good outcome in extradural abscess caused by atypical infection such as Salmonella sp.
Footnotes
Twitter: @Otology
Contributors: CCL: writing, editing, literature review. JS: writing, editing, literature review. JK: editing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Ponnambath DK, Khimji PB, Kaviyil JE. First report of intracranial epidermoid cyst infection and brain abscess caused by Salmonella paratyphi A. J Acad Clin Microbiol 2019;21:85–8. [Google Scholar]
- 2.Intan HI, Zubaidah CD, Norazah A, et al. Subdural collections due to non-typhi Salmonella infections in two Malaysian children. Singapore Med J 2008;49:e186–9. [PubMed] [Google Scholar]
- 3.Sudhaharan S, Padmaja K, Solanki R, et al. Extra-Intestinal salmonellosis in a tertiary care center in South India. J Infect Dev Ctries 2014;8:831–7. 10.3855/jidc.3731 [DOI] [PubMed] [Google Scholar]
- 4.Kuruvath S, Basu S, Elwitigala JP, et al. Salmonella enteritidis brain abscess in a sickle cell disease patient: case report and review of the literature. Int J Infect Dis 2008;12:298–302. 10.1016/j.ijid.2007.02.004 [DOI] [PubMed] [Google Scholar]
- 5.Yen MH, Huang YC, Chou ML. Non-typhoid Salmonella subdural empyema in children: report of two cases. J Microbiol Immunol Infect 1999;32:289–91. [PubMed] [Google Scholar]
- 6.Heyman R, Heckly A, Magagi J, et al. Intracranial epidural hematoma in newborn infants: clinical study of 15 cases. Neurosurgery 2005;57:924–9. 10.1227/01.NEU.0000180026.73246.bf [DOI] [PubMed] [Google Scholar]
- 7.Bullock MR, Chesnut R, Ghajar J, et al. Surgical management of acute epidural hematomas. Neurosurgery 2006;58:S2-7–S2-15. 10.1227/01.NEU.0000210363.91172.A8 [DOI] [PubMed] [Google Scholar]
- 8.Osmond MH, Klassen TP, Wells GA, et al. CATCH: a clinical decision rule for the use of computed tomography in children with minor head injury. CMAJ 2010;182:341–8. 10.1503/cmaj.091421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuppermann N, Holmes JF, Dayan PS, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet 2009;374:1160–70. 10.1016/S0140-6736(09)61558-0 [DOI] [PubMed] [Google Scholar]
- 10.Bin SS, Schutzman SA, Greenes DS. Validation of a clinical score to predict skull fracture in head-injured infants. Pediatr Emerg Care 2010;26:633–9. 10.1097/PEC.0b013e3181ef0440 [DOI] [PubMed] [Google Scholar]
- 11.Schutzman SA, Nigrovic LE, Mannix R. The infant scalp score: a validated tool to stratify risk of traumatic brain injury in infants with isolated scalp hematoma. Acad Emerg Med 2021;28:92–7. 10.1111/acem.14087 [DOI] [PubMed] [Google Scholar]
- 12.Erlichman DB, Blumfield E, Rajpathak S, et al. Association between linear skull fractures and intracranial hemorrhage in children with minor head trauma. Pediatr Radiol 2010;40:1375–9. 10.1007/s00247-010-1555-4 [DOI] [PubMed] [Google Scholar]
- 13.Sheets LK, Leach ME, Koszewski IJ, et al. Sentinel injuries in infants evaluated for child physical abuse. Pediatrics 2013;131:701–7. 10.1542/peds.2012-2780 [DOI] [PubMed] [Google Scholar]
- 14.Duhaime AC, Christian CW, Rorke LB, et al. Nonaccidental head injury in infants--the "shaken-baby syndrome". N Engl J Med 1998;338:1822–9. 10.1056/NEJM199806183382507 [DOI] [PubMed] [Google Scholar]
- 15.Freni F, Galletti B, Bruno R. Multidisciplinary approach in the removal of post-trauma foreign bodies in the head and neck district: case report and review of literature. Acta Medica Mediterranea 2019;35:405–10. [Google Scholar]


