Prostate cancer is the most common cancer diagnosed in Australian men, excluding non‐melanoma skin cancer, and it is estimated that there are over 220 000 Australian men living with a diagnosis of prostate cancer [1]. Survival for men with prostate cancer is excellent in countries that have accessible screening and treatment services, and in Australia 5‐year relative survival is over 95% [1]. High incidence, coupled with improving long‐term survival, leads to a correspondingly high prevalence rate and high community disease burden. Many men with prostate cancer experience long‐term decrements in their mental and physical quality of life, overall they have a greater suicide risk than their non‐cancer peers, and unmet supportive care needs are pervasive [2]. In this context, survivorship care for men with prostate cancer is crucial in both the short and long term. The recent development of a Prostate Cancer Survivorship Essentials Framework in the Australian and New Zealand setting provides an example of a regional response to this issue that delivers guidance for policy makers, clinicians, community and consumers on what is essential for step change in prostate cancer survivorship outcomes [3].
Definitions of survivorship vary, particularly between the medical professional and consumers. Narayan et al. [4] recently proposed that, in the case of prostate cancer, a broad definition where survivorship begins at diagnosis and continues until the end of life was a better fit for a cancer with a prolonged treatment course and often complex and demanding treatment regimens. Current gaps in prostate cancer survivorship evidence and practice are problematic and well described [4, 5]. These include a lack of data on effective models of care coordination, survivorship care implementation, a heavy reliance on expert opinion, and little attention to health disparities, resulting in fragmented care that is not patient‐centred. More broadly, a recent review of cancer survivorship‐focused goals and objectives in comprehensive cancer control plans across the USA concluded that, although in principle support for cancer survivorship was generally strong, evidence of implementation and effect was less evident [6]. The need for multiple coordinated strategies that take a longitudinal focus was noted if indeed the survivorship needs of cancer populations are to be addressed. The question then arises, how do we best advance well‐coordinated and responsive survivorship care for men with prostate cancer?
We would argue that there are three critical elements for forward movement. The first concerns recognition and inclusion of the consumer voice. The second is clarity around the evidence base and where the most likely gains in quality of life and survivorship outcomes might be made. Third, a coalition of the willing is needed. Men with prostate cancer and the health professionals who care for them describe the prostate cancer survivorship experience as challenging, medically focused, and uncoordinated, leading to unmet supportive care needs and anxiety for patients [3]. They report the need for improved communication by healthcare professionals and better coordinated and men‐centred care that responds and articulates with masculine ways of being. Further, although there remain gaps in knowledge around aspects of prostate cancer survivorship care, such as care coordination and surveillance, good evidence exists for effective interventions in many key areas such as psychosocial care, health promotion, physical rehabilitation and exercise medicine [5]. There is much we can do. The Prostate Cancer Survivorship Essentials Framework developed by leading clinical, nursing and allied health groups and agencies and consumer groups in Australia and New Zealand identified six domains of care for which consensus was high: Health Promotion and Advocacy; Shared Management; Vigilance; Personal Agency; Care Coordination and Evidence‐based Survivorship Interventions (Fig. 1) [3]. Stakeholders confirmed that the defined elements within these domains were important. There now exists a critical momentum with a key coalition to improve care for men with prostate cancer in these countries from which real change may occur.
Fig. 1.
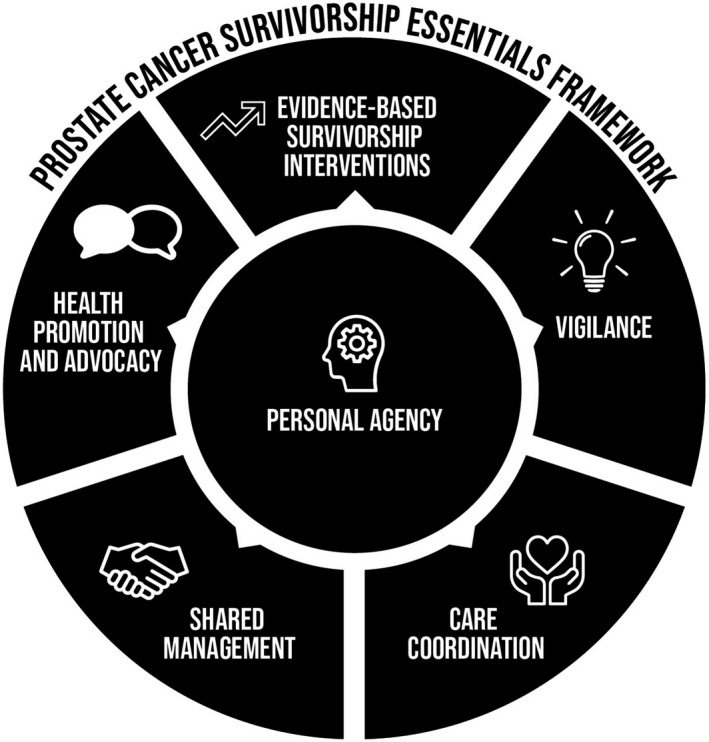
Prostate Cancer Survivorship Essentials Framework.
The Essentials Framework provides a road map for improvements in cancer for men with prostate cancer that can be expressed in multiple policy and programme initiatives to suit different communities and different patient scenarios. One‐size‐fits all is rarely indicated or effective in healthcare system change and improvement and hence we encourage creativity and flexibility in how the framework is applied. It is likely that different settings with different resourcing and specific community characteristics will require different solutions. The key is to act now, because as prostate cancer prevalence continues to grow globally, if not now, when?
Conflict of Interest
None declared.
References
- 1. Australian Institute of Health and Welfare . Cancer data in Australia 2020. Web Report, 20 June 2020, AIHW, Cat no. CAN122. Canberra, ACT: AIHW, 2020. [Google Scholar]
- 2. Chambers SK, Galvão DA, Green A et al. A Psychosocial Care Model for Men with Prostate Cancer. Sydney, NSW: Prostate Cancer Foundation of Australia and University of Technology Sydney, 2019. [Google Scholar]
- 3. Dunn J, Green A, Ralph N et al. Prostate cancer survivorship essentials framework: guidelines for practitioners. BJUI 2020. 10.1111/bju.15159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Narayan V, Harrison M, Cheng H et al. Improving research for prostate cancer survivorship: a statement from the Survivorship Research in Prostate Cancer (SuRECaP) working group. Urol Oncol 2020; 38: 83–93 [DOI] [PubMed] [Google Scholar]
- 5. Crawford‐Williams F, March S, Goodwin BC et al. Interventions for prostate cancer survivorship: a systematic review of reviews. Psychooncology 2018; 27: 2339–48 [DOI] [PubMed] [Google Scholar]
- 6. Mollica MA, Falisi AL, Geiger AM et al. Survivorship objectives in comprehensive cancer control plans: a systematic review. J Cancer Surviv 2020; 14: 235–43 [DOI] [PMC free article] [PubMed] [Google Scholar]


