Abstract
We evaluated the association between weight status and motor competence from preschool age (3‐5 years of age) until middle childhood (7‐9 years of age). Longitudinal study with three to five‐year‐old preschool children (n = 1155) enrolled in public and private preschools in Recife, Brazil. Children were followed twice (2010, 2012, and 2014) for four years. Köperkoordinationstest für kinder (KTK) assessed the children's motor competence (KTK Motor Quotient). Weight status (underweight, normal weight, overweight, and obesity) was classified according to the children's sex and age. Preschool children with normal weight exhibited higher motor competence at 5‐7 years of age compared to preschool children with overweight (+3.73 MQ, P = .03) and obesity (+5.09 MQ, P < .01). Preschool children with normal weight presented higher motor competence at 7‐9 years of age compared to their peers with overweight (+6.00 MQ, P = .03) and obesity (+5.88 MQ, P = .01). Children with normal weight at 5‐7 years of age presented higher motor competence at 7‐9 years of age compared to their peers with overweight (+3.33 MQ, P = .02) and obesity (+4.00 MQ, P = .02). Independent of the childhood phase and extension of the period evaluated (2‐ or 4‐year period), children who had excessive weight (overweight or obesity) and changed their weight status to underweight or normal weight presented similar motor competence compared to children who continued underweight or normal weight. Weight status already at preschool age is an important predictor of the children's motor competence until middle childhood. Interventions improving the children's weight status, already at preschool age, might impact their motor competence development positively.
Keywords: longitudinal studies, motor development, obesity, youth
1. INTRODUCTION
Engagement in physical activity in the early years of childhood is associated with lower adiposity levels, higher cognitive performance besides improved psychosocial and cardio‐metabolic health. 1 Furthermore, the ability to move it is an essential aspect to engage in physical activities, especially in early childhood. 2 Acquiring and refining this movement proficiency involves complex interactions between the environment and the neuromuscular systems, and it has often been referred as motor competence. 3
A conceptual framework proposed by Stodden et al 4 suggested a dynamic and synergistic relationship between motor competence, perceived motor competence, physical activity, physical fitness and adiposity during childhood and adolescence. As a result of the publication of this framework, an increasing number of studies have evaluated Stodden's model. Although Stodden et al 4 acknowledged the possible mutual relationship among perceived motor competence, motor competence, physical activity, physical fitness and adiposity, most of the published evidence have focused on the determinants of adiposity. 5 , 6 , 7
On the other hand, with the rise in the number of young children with overweight and obesity, 8 studies need to also consider the impact of weight status in young children on the motor competence development during childhood. Children with excessive weight tend to suffer in weight‐bearing activities, which might become a barrier in developing motor competencies. 9 , 10 , 11 Because motor competence during childhood is associated with physical activity and fitness, 5 , 7 , 12 , 13 evaluating the impact of excessive weight on motor competence development is pivotal. So far, most cross‐sectional 9 , 10 , 11 , 14 , 15 , 16 , 17 , 18 , 19 , 20 and longitudinal 12 , 13 , 21 , 22 , 23 studies reported a negative relationship between weight status or adiposity and motor competence in children. Moreover, longitudinal studies indicate that motor competence and weight status or adiposity might present mutual relationship in children older than 6 years of age. 13 , 24 However, most of the manuscripts are cross‐sectional and were conducted with children older than 6 years of age.
It is also relevant to consider the family socioeconomic status while evaluating the association between weight status and motor competence. Veldman et al 25 reported that lower family income was cross‐sectionally associated with lower motor competence in preschool children. In addition, most aforementioned studies were conducted in high‐income countries (see 6 , 7 for review).
Thus, the aims of this study are twofold: to evaluate the association between weight status (underweight, normal weight, overweight and obesity) and motor competence from preschool age (3‐5 years of age) until middle childhood (7‐9 years of age) in Brazilian children; and, to investigate whether weight status trajectory was associated with motor competence during childhood.
2. MATERIALS AND METHODS
2.1. Procedure
A longitudinal study with preschool children aged three to five years started in 2010. The ELOS‐Pre Project (Longitudinal Study of Health and Well‐being in Preschool Children) was designed to assess longitudinal changes in health conditions, physical activity practices, anthropometric parameters, motor competence performance, and other lifestyle factors among preschool children and in school age. Data were collected by trained graduate and Master's students in physical education. Before all the test rounds, researchers conducted training workshops for all testers. The testers trained their skills on fellow testers and on children in similar age group in a school that was not participating in the ELOS‐Pre Project. After the first data collection that occurred in 2010, children were followed for four years with measurements occurring every second year (2012 and 2014) in Recife, Pernambuco State, Brazil. The protocol was approved by the Human Research Ethics Committee of the University of Pernambuco (protocol no. 0096.0.097.000‐10) and informed written consent was obtained from the children's parents or guardians and the respective school principals.
2.2. Participants
The target population of the study at baseline was three to five‐year‐old preschool children who were enrolled in both public and private preschools in the six political administrative regions of Recife. Therefore, we selected the schools (cluster unit) to assess the preschool children. All schools in Recife with preschool children were eligible to be included in the study. Stratification criterion was adopted in order to ensure that the sample represented the target population regarding the distribution: type of school (public and private), size of the school (small: <50 children enrolled in preschool education; medium: 50 to 199 children enrolled; large: 200 children or more) and the distribution of the schools according to the six administrative political regions of the city of Recife. In each selected school, all regularly enrolled children were invited to participate in the study. 26 In total, 1155 children accepted to participate in the baseline (2010). After two years, the project had a follow‐up rate of 76% (n = 784, mean age = 6.0 ± 0.7), and 475 children (mean age = 8.0 ± 0.7) were monitored in 2014 (Figure 1).
Figure 1.
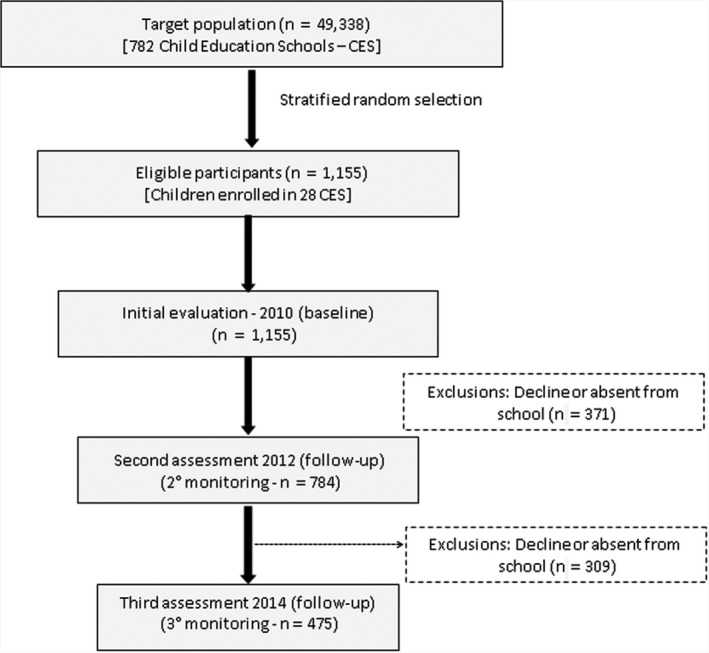
Flow chart of the longitudinal follow‐up of study participants
2.3. Measures
We conducted face‐to‐face interviews with the children's parents to obtain information on their socioeconomic status and health behaviors. Information was collected on sex (male, female), age, and family income.
2.3.1. Motor competence
In 2012 (5‐7 years) and 2014 (7‐9 years), we used the Köperkoordinationstest für kinder (KTK) for directly assessing children's motor competence. The KTK is validated for use in children older than five years of age and consists of 4 independent tests: (a) walking backward on balance beams of decreasing width: 6.0, 4.5, and 3.0 cm; (b) moving sideways on wooden boards for 20 seconds; (c) one‐legged hopping over a foam obstacle with increasing height in consecutive steps of 5 cm; and (d) two‐legged jumping from side to side for 15 seconds. We summed the scores of the four‐abovementioned subtests and used for descriptive purposes (KTK sum of raw scores). For the main analysis, we used the KTK Motor Quotient, which is the sum score of the subtests converted based on normative data of the KTK original study. The KTK Motor Quotient is adjusted for age (all subtests) and gender (hopping for height and jumping sideways over a slat), 27 and children's motor competence can be classified as impaired motor competence (KTK Motor Quotient 56‐70; ≤2nd percentile), poor motor competence (KTK Motor Quotient = 71‐85; 3rd–16th percentile), normal motor competence (KTK Motor Quotient = 86‐115; 17th–84th percentile), good motor competence (KTK Motor Quotient = 116‐130; 85th–98th percentile), or high motor competence (KTK Motor Quotient 131‐145; ≥99th percentile. 27
2.3.2. Anthropometric measures
Children were weighed while wearing light clothing with no shoes on a Filizola scale to the nearest 0.1 kg. Their height was measured to the nearest 0.5 cm using a wall‐mounted stadiometer (Welmy, São Paulo, Brazil). Their body mass index (BMI) was calculated by dividing the body weight by the height squared (kg/m2). We classified children with underweight, normal weight, overweight, and obesity according to the children's respective sex and age. 28 Children with overweight or obesity were considered with excessive body weight.
2.4. Statistical analyses
All statistical analyses were conducted in STATA 16 for Windows (StataCorp LP). Chi‐square or t tests were used to examine differences in the descriptive characteristics between children who were followed in the four‐year monitoring period and children who dropped out.
Multilevel mixed‐effects linear regressions were used to analyze the associations between weight status and motor competence. Firstly, we evaluated the motor competence depending on the weight status (underweight, normal weight, overweight, and obesity) of the children during childhood (results presented in Table 3). Secondly, we estimated (using margins command in Stata) the motor competence score of the children based on the weight status trajectory (results presented in Figure 2). As an example, we calculated the motor competence score of the children at 5‐7 years of age who presented excessive weight at preschool age (3‐5 years) and continued with excessive weight in the first follow‐up at 5‐7 years of age. We provide detailed description of the adjustments for each model in the results section, in the respective Tables and Figures legends. In all the multilevel regression models, the variance related to the clusters (school) and the intraclass correlation coefficient (ICC) for each model was calculated to interpret the variation among schools and individuals. In all the regression models, the majority of the variation (ICC) was at the individual level (the ICCs from the schools were always below 3%).
Figure 2.
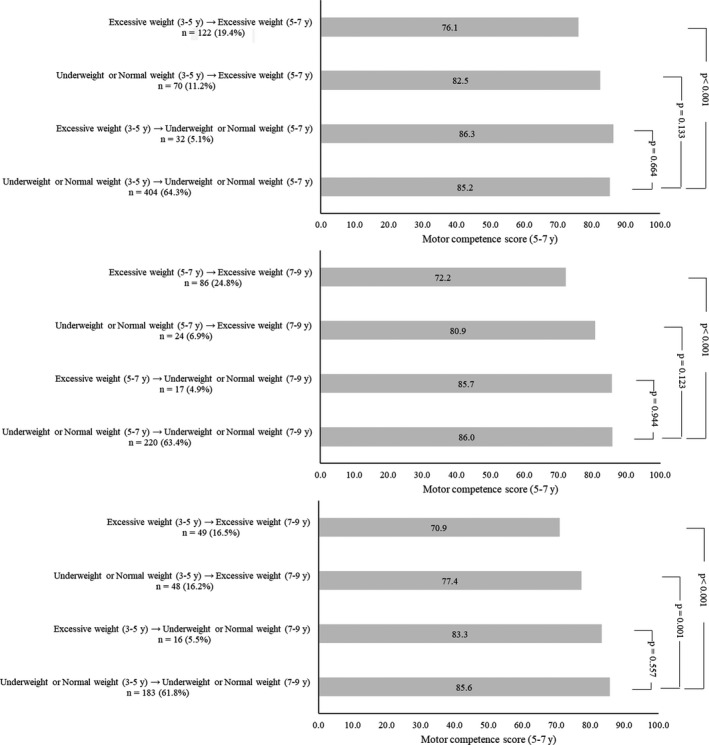
KTK motor Quotient score of the children based on their weight status trajectory during childhood. Legend: Analyses adjusted for family income and the cluster structure of the data (students nested within schools)
3. RESULTS
Table 1 presents descriptive data of the participants followed in each of the measurements and of the participants not followed in 2012 or 2014. We did not observe selection bias in relation to the family income and the children's sex, weight status, and age (all P > .05) by comparing children who dropped out in 2012 or in 2014 with children assessed in 2010 who continued to be monitored in 2012 and 2014. In 2010, on average, children were 4.3 years of age, 51.4% were boys and 26.2% had excessive body weight.
Table 1.
Sociodemographic characteristics and body measurements of the participants at the baseline (2010), follow‐ups (2012, 2014), and the dropouts
| Variables | 2010 (3‐5 y) | 2012 (5‐7 y) | 2014 (7‐9 y) | Dropouts (2012 or 2014) | P | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |||
| Sex | Male | 594 | 51.4 | 405 | 51.7 | 230 | 52.3 | 364 | 61.3 | .652 a |
| Female | 561 | 48.6 | 379 | 48.3 | 210 | 47.7 | 351 | 62.6 | ||
| Family income | <1 MW | 425 | 42.4 | 287 | 37.1 | 154 | 39.6 | 283 | 64.2 | .126 b |
| 1‐2 MW | 307 | 29.6 | 247 | 32.0 | 111 | 28.5 | 216 | 71.4 | ||
| 2‐4 MW | 152 | 14.6 | 129 | 16.7 | 68 | 17.5 | 104 | 68.4 | ||
| >4 MW | 139 | 13.4 | 110 | 14.2 | 56 | 14.4 | 85 | 61.2 | ||
| BMI | Underweight | 166 | 14.4 | 74 | 9.9 | 43 | 10.8 | 111 | 66.9 | .223 b |
| Normal weight | 645 | 55.8 | 445 | 59.2 | 229 | 57.5 | 414 | 64.2 | ||
| Overweight | 153 | 13.3 | 124 | 16.5 | 74 | 18.6 | 111 | 72.6 | ||
| Obesity | 191 | 16.5 | 108 | 14.4 | 52 | 13.1 | 121 | 63.4 | ||
| n | mean (SD) | n | mean (SD) | n | mean (SD) | n | mean (SD) | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Age (y) | 1555 | 4.3 (0.8) | 783 | 6.3 (0.8) | 440 | 8.4 (0.8) | 715 | 4.3 (0.8) | .125 c |
Abbreviation: MW, minimum wages.
P value from the Fisher chi‐square test comparing dropouts and children monitored in 2010.
P value from the Exact Fisher chi‐square test comparing dropouts and children monitored in 2010.
P value from the dependent t test comparing dropouts and children monitored in 2010.
In 2012 (5‐7 years of age), 18.2% children presented impaired motor competence, 39.3% poor motor competence, 40.8% normal motor competence, 1.6% good motor competence, and 0.1% high motor competence. In 2014 (7‐9 years of age), 22.0% children presented impaired motor competence, 35.7% poor motor competence, 40.2% normal motor competence, 2.1% good motor competence, and none high motor competence. Table 2 describes the children's motor competence scores for each of the KTK tasks, for the KTK sum of raw scores and for the KTK Motor Quotient.
Table 2.
Participants' motor competence scores during childhood
| Motor competence (scores) | 2012 (5‐7 y) | 2014 (7‐9 y) | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| KTK sum of raw scores | 746 | 101.9 (34.8) | 440 | 146.5 (41.2) |
| KTK Motor Quotient | 746 | 83.4 (14.5) | 440 | 82.2 (16.4) |
| KTK tasks (standardized scores) | ||||
| Walking backward | 747 | 89.4 (16.0) | 451 | 94.3 (15.7) |
| Moving sideways | 751 | 94.6 (17.5) | 460 | 88.0 (17.8) |
| One‐legged hopping | 751 | 72.9 (13.3) | 461 | 76.1 (17.6) |
| Two‐legged jumping | 750 | 92.1 (13.5) | 461 | 87.7 (15.2) |
We observed that weight status and motor competence were cross‐sectionally and longitudinally associated throughout childhood (Table 3). Overall, children who were overweight or obese presented lower motor competence score during childhood compared to children who were normal weight. In summary, preschool children with normal weight exhibited higher motor competence at 5‐7 years of age compared to preschool children with overweight (+3.73 MQ points, P = .03) and obesity (+5.09 MQ points, P < .01). Preschool children with normal weight presented higher motor competence at 7‐9 years of age compared to their peers with overweight (+6.00 MQ points, P = .03) and obesity (+5.88 MQ points, P = .01).
Table 3.
Longitudinal associations between weight status and motor competence scores during childhood
| Exposures | KTK motor Quotient score at 5‐7 y (2012) | KTK motor Quotient score at 7‐9 y (2014) | |||||
|---|---|---|---|---|---|---|---|
| n (%) | Mean difference in relation to normal weight (95% CI) | P | n (%) | Mean difference in relation to normal weight (95% CI) | P | ||
| BMI at 3‐5 y (2010) | Underweight | 107 (16.2) | 2.96 (−0.13 to 6.05) | .06 a | 52 (14.8) | 5.95 (1.16 to 10.74) | .02 b |
| Overweight | 83 (12.5) | −3.73 (−7.16 to −0.31) | .03 a | 39 (11.1) | −6.00 (−11.39 to −0.62) | .03 b | |
| Obesity | 98 (14.8) | −5.09 (−8.28 to −1.89) | <.01 a | 55 (15.7) | ‐5.88 (−10.57 to −1.20) | .01 b | |
| BMI at 5‐7 y (2012) | Underweight | 74 (10.1) | 1.51 (−1.90 to 4.92) | .39 c | 35 (9.2) | 2.83 (−0.78 to 6.44) | .12 d |
| Overweight | 121 (16.4) | −4.26 (−7.06 to −1.45) | <.01 c | 73 (19.2) | −3.33 (−6.07 to −0.60) | .02 d | |
| Obesity | 106 (14.4) | −11.12 (−14.07 to −8.17) | <.01 c | 49 (12.9) | −4.00 (−7.30 to −0.70) | .02 d | |
| BMI at 7‐9 y (2012) | Underweight | 40 (11.3) | 2.83 (−2.26 to 7.91) | .28 e | |||
| Overweight | 68 (19.3) | −6.53 (−10.66 to −2.39) | <.01 e | ||||
| Obesity | 44 (12.5) | −19.81 (−24.72 to −14.89) | <.01 e | ||||
that all the models were adjusted for the cluster structure of the data (students nested within schools).
Adjusted for: family income (3‐5 and 5‐7 y).
Adjusted for: family income (3‐5 and 7‐9 y).
Adjusted for: family income (5‐7 y).
Adjusted for: KTK motor Quotient score (5‐7 y), family income (5‐7 and 7‐9 y).
Adjusted for: family income (7‐9 y).
Children with normal weight at 5‐7 years of age presented higher motor competence at 5‐7 years of age compared to their peers with overweight (+4.26 MQ points, P < .01) and obesity (+11.12 MQ points, P < .01). Children with normal weight at 5‐7 years of age presented higher motor competence at 7‐9 years of age compared to their peers with overweight (+3.33 MQ points, P = .02) and obesity (+4.00 MQ points, P = .02). Children with normal weight at 7‐9 years of age presented higher motor competence at 7‐9 years of age compared to their peers with overweight (+6.53 MQ points, P < .01) and obesity (+19.81 MQ points, P < .01) (Table 3).
Figure 2 presents the motor competence score of the children at 5‐7 and at 7‐9 years of age based on the weight status trajectory during childhood. In summary, independent of the childhood phase and extension of the period evaluated (two‐ or four‐year period), children who had excessive weight (overweight or obesity) and changed their weight status to underweight or normal weight presented similar motor competence scores compared to children who continued underweight or normal weight. As an example, preschool children with excessive weight who changed their weight status to underweight or normal weight at 5‐7 years of age presented similar motor competence score at 5‐7 years of age compared to children who continued in the underweight or normal weight groups in the same period (P = .664).
4. DISCUSSION
We observed that motor competence scores throughout childhood were dependent on the children's weight status. Interestingly, even weight status at preschool age‐predicted motor competence scores four years later. To the best of our knowledge, this is the first longitudinal study evaluating the relationship between weight status at preschool age and motor competence scores in early and middle childhood. In general, previous longitudinal investigations reported a deleterious impact of weight status on motor competence during childhood. 12 , 13 , 22 , 29
It is believed that children with excessive weight experience more difficulties in weight‐bearing activities because of the greater weight that must be beared against gravity during these tasks. 9 , 10 , 11 In addition to the biomechanical limitations related to excessive weight, children with higher adiposity or excessive weight are less engaged in physical activities 30 and also present lower physical fitness. 5 , 13 Heavier children are less likely to participate in physical activities, which in turn diminishes the number of opportunities for developing their motor competence and fitness levels. 13 This causal cycle is likely to increase the children's weight status and feedback this vicious cycle. 4
Our results provide new insights in the Stodden's model by showing the importance of weight status already at preschool age on the motor competence development during childhood. Although Stodden et al 4 acknowledged the importance of weight status on the motor competence, perceived motor competence, physical and fitness developments, Stodden's model suggested that participation in physical activities and motor competence would be the most important components in early childhood. A growing body of evidence is highlighting the importance of weight status already at very young ages. 31 , 32 , 33 Nevertheless, future investigations need to provide additional information for better understanding. This is a crucial aspect that needs further investigation to support the design of interventions targeting health behaviors in children.
Moreover, independent of the period evaluated, children who changed their weight status from excessive weight to underweight or normal weight presented similar motor competence scores compared to children who continued underweight or normal weight within the two‐ or four‐year period, which is a novel finding. Although children with excessive weight tend to have lower motor competence, 12 , 22 , 29 interventions improving their weight status might also enhance their motor competence.
Although the current investigation presents novel findings regarding the importance of weight status on the motor competence development, few limitations need to be considered in the interpretation of the findings. First, the KTK battery is only valid for use in children older than 5 years of age, thus we did not assess children's motor competence at preschool age. Nevertheless, the interpretation regarding the importance of weight status on the children's motor competence remained similar in the models in which we were able to adjust for the KTK scores. Second, this was a longitudinal study; therefore, we were not able to infer causality in the weight status‐motor competence relationship.
Our findings support the importance of weight status already at preschool age on the motor competence development of children until middle childhood. Moreover, our results support that changes in the weight status are associated with changes in motor competence scores. Therefore, we recommend that future interventions test the impact of changes in the children's weight status on their motor competence development.
5. PERSPECTIVE
Weight status, as early as preschool age, predicted motor competence scores in early (5‐7 years) and middle (7‐9 years) childhood. In addition, we observed that changes in weight status during childhood were related to the children's motor competence scores. Although the current findings highlight the importance of weight status already at young ages on the motor competence development, it is feasible that both motor competence and weight status are mutually related and equally important during childhood development. 13 Therefore, interventions should target both weight status and motor competence, since their probable synergic relationship stimulates one another.
CONFLICT OF INTEREST
None to declare.
AUTHOR CONTRIBUTIONS
Lima RA contributed to conception, design, data acquisition, analysis, and interpretation; he also drafted and critically revised the manuscript. Queiroz DR, Aguilar JA, and Bezerra J contributed to data acquisition, analysis, and interpretation; they also drafted and critically revised the manuscript. Soares FC and Barros MVG contributed to design, data analysis, and interpretation; they also drafted and critically revised the manuscript. All authors gave their final approval of the text and agree to be accountable for all aspects of the work.
ETHICAL APPROVAL
Where research involves human and/or animal experimentation. The following statements should be included (as applicable): “The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975 as revised in 2008.” and “The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guides on the care and use of laboratory animals.”
ACKNOWLEDGEMENTS
This study was financed by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brazil (CAPES). It was also supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico—Brazil (CNPQ), and Fundação de Amparo à Ciência e Tecnologia do Estado de Pernambuco—Brazil (FACEPE; BCT 0233‐4.09/17 and BFP 0029‐4.09/16).
Lima RA, Soares FC, Queiroz DR, Aguilar JA, Bezerra J, Barros MVG. The importance of body weight status on motor competence development: From preschool to middle childhood. Scand J Med Sci Sports.2021;31(Suppl. 1):15–22. 10.1111/sms.13787
REFERENCES
- 1. Carson V, Lee EY, Hewitt L, et al. Systematic review of the relationships between physical activity and health indicators in the early years (0–4 years). BMC Public Health. 2017;17(Suppl 5):854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jones D, Innerd A, Giles EL, Azevedo LB. Association between fundamental motor skills and physical activity in the early years: A systematic review and meta‐analysis. J Sport Heal Sci. 2020. 10.1016/j.jshs.2020.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Malina RM. Top 10 research questions related to growth and maturation of relevance to physical activity, performance, and fitness. Res Q Exerc Sport. 2014;85(2):157‐173. [DOI] [PubMed] [Google Scholar]
- 4. Stodden DF, Goodway JD, Langendorfer SJ, et al. A developmental perspective on the role of motor skill competence in physical activity: an emergent relationship. Quest. 2008;60:290‐306. [Google Scholar]
- 5. Cattuzzo MT, Dos Santos HR, Re AHN, et al. Motor competence and health related physical fitness in youth: a systematic review. J Sci Med Sport. 2016;19:123‐129. [DOI] [PubMed] [Google Scholar]
- 6. Barnett LM, Lai SK, Veldman SLC, et al. Correlates of gross motor competence in children and adolescents: a systematic review and meta‐analysis. Sports Med. 2016;45:1273‐1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Robinson LE, Stodden DF, Barnett LM, et al. Motor competence and its effect on positive developmental trajectories of health. Sports Med. 2015;45:1273‐1284. [DOI] [PubMed] [Google Scholar]
- 8. WOF . Atlas of childhood obesity. World Obes J. 2019;1:213. [Google Scholar]
- 9. D’Hondt E, Deforche B, De Bourdeaudhuij I, Lenoir M. Childhood obesity affects fine motor skill performance under different postural constraints. Neurosci Lett. 2008;440:72‐75. [DOI] [PubMed] [Google Scholar]
- 10. D’Hondt E, Deforche B, Vaeyens R, et al. Gross motor coordination in relation to weight status and age in 5‐ to 12‐year‐old boys and girls: a cross‐sectional study. Int J Pediatr Obes. 2011;6:e556‐e564. [DOI] [PubMed] [Google Scholar]
- 11. Gentier I, D’Hondt E, Shultz S, et al. Fine and gross motor skills differ between healthy‐weight and obese children. Res Dev Disabil. 2013;34:4043‐4051. [DOI] [PubMed] [Google Scholar]
- 12. Lima RA, Bugge A, Pfeiffer KA, Andersen LB. Tracking of gross motor coordination from childhood into adolescence. Res Q Exerc Sport. 2017;88:52‐59. [DOI] [PubMed] [Google Scholar]
- 13. Lima RA, Bugge A, Ersbøll AK, Stodden DF, Andersen LB. The longitudinal relationship between motor competence and measures of fatness and fitness from childhood into adolescence. J Pediatr (Rio J). 2019;95:482‐488. [DOI] [PubMed] [Google Scholar]
- 14. Okely AD, Booth ML, Chey T. Relationships between body composition and fundamental movement skills among children and adolescents. Res Q Exerc Sport. 2004;75:238‐247. [DOI] [PubMed] [Google Scholar]
- 15. Lopes VP, Stodden DF, Bianchi MM, , Maia JAR, Rodrigues LP. Correlation between BMI and motor coordination in children. J Sci Med Sport. 2012;15:38‐43. [DOI] [PubMed] [Google Scholar]
- 16. Morrison KM, Bugge A, El‐Naaman B, et al. Inter‐relationships among physical activity, body fat, and motor performance in 6‐ to 8‐year‐old Danish children. Pediatr Exerc Sci. 2012;24:199‐209. [DOI] [PubMed] [Google Scholar]
- 17. Luz LGO, Valente‐dos‐Santos J, Luz TDD, et al. Biocultural predictors of motor coordination among prepubertal boys and girls. Percept Mot Skills. 2018;125(1):21‐39. 10.1177/0031512517744471 [DOI] [PubMed] [Google Scholar]
- 18. Chowdhury SD, Wrotniak BH, Ghosh T. Association between body mass index and motor competence in santal children of Purulia district, India. J Mot Behav. 2017;49(3):349‐354. [DOI] [PubMed] [Google Scholar]
- 19. Lopes L, Santos R, Moreira C, Pereira B, Lopes VP. Sensitivity and specificity of different measures of adiposity to distinguish between low/high motor coordination. J Pediatr. 2015;91(1):44‐51. [DOI] [PubMed] [Google Scholar]
- 20. Lopes VP, Malina RM, Maia JAR, Rodrigues LP. Body mass index and motor coordination: non‐linear relationships in children 6–10 years. Child Care Health Dev. 2018;44(3):443‐451. [DOI] [PubMed] [Google Scholar]
- 21. D’Hondt E, Deforche B, Gentier I, et al. A longitudinal study of gross motor coordination and weight status in children. Obesity (Silver Spring). 2014;22:1505‐1511. [DOI] [PubMed] [Google Scholar]
- 22. D’Hondt E, Deforche B, Gentier I, et al. A longitudinal analysis of gross motor coordination in overweight and obese children versus normal‐weight peers. Int J Obes (Lond). 2013;37:61‐67. [DOI] [PubMed] [Google Scholar]
- 23. Cheng J, East P, Blanco E, et al. Obesity leads to declines in motor skills across childhood. Child Care Health Dev. 2016;42:343‐350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Coppens E, Bardid F, Deconinck FJA, et al. Developmental change in motor competence: a latent growth curve analysis. Front Physiol. 2019;10:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Veldman SLC, Jones RA, Chandler P, Robinson LE, Okely AD. Prevalence and risk factors of gross motor delay in pre‐schoolers. J Paediatr Child Health. 2020;56(4):571‐576. [DOI] [PubMed] [Google Scholar]
- 26. Lima RA, Barros SSH, CardosoJúnior CG, et al. Influence of number of days and valid hours using accelerometry on the estimates of physical activity level in preschool children from Recife, Pernambuco, Brazil. Rev Bras Cineantropometria Desempenho Hum. 2014;16:171‐181. [Google Scholar]
- 27. Kiphard E, Schilling V. Körper‐Koordinations‐Test für Kinder KTK: Manual Von Fridhelm Schilling. Weinhein, Germany: Beltz Test; 1974. [Google Scholar]
- 28. Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut‐offs for thinness, overweight and obesity. Pediatr Obes. 2012;7:284‐294. [DOI] [PubMed] [Google Scholar]
- 29. Matarma T, Lagstrom H, Hurme S, et al. Motor skills in association with physical activity, sedentary time, body fat, and day care attendance in 5‐6‐year‐old children‐The STEPS Study. Scand J Med Sci Sports. 2018;28:2668‐2676. [DOI] [PubMed] [Google Scholar]
- 30. Hong I, Coker‐Bolt P, Anderson KR, Lee D, Velozo CA. Relationship between physical activity and overweight and obesity in children: Findings From the 2012 National Health and Nutrition Examination Survey National Youth Fitness Survey. Am J Occup Ther. 2016;70(5):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Spessato BC, Gabbard C, Robinson L, Valentini NC. Body mass index, perceived and actual physical competence: the relationship among young children. Child Care Health Dev. 2013;39:845‐850. [DOI] [PubMed] [Google Scholar]
- 32. Castetbon K, Andreyeva T. Obesity and motor skills among 4 to 6‐year‐old children in the United States: nationally‐representative surveys. BMC Pediatr. 2012;12:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Laukkanen A, Pesola AJ, Finni T, Saakslahti A. Body Mass Index in the early years in relation to motor coordination at the age of 5(‐)7 years. Sport (Basel). 2017;5(3):49. [DOI] [PMC free article] [PubMed] [Google Scholar]


