This study used data from Medicare fee-for-service claims to examine characteristics and hospitalization risks among patients with COVID-19 who were aged 65 years or older and to estimate the costs of hospitalizations and outpatient visits associated with the disease.
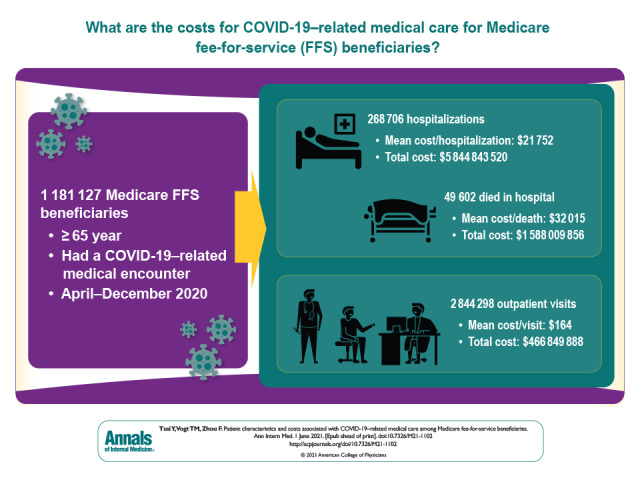
Visual Abstract. COVID-19–Related Medical Care Among Medicare Fee-for-Service Beneficiaries.
This study used data from Medicare fee-for-service claims to examine characteristics and hospitalization risks among patients with COVID-19 who were aged 65 years or older and to estimate the costs of hospitalizations and outpatient visits associated with the disease.
Abstract
Background:
New cases of COVID-19 continue to occur daily in the United States, and the need for medical treatments continues to grow. Knowledge of the direct medical costs of COVID-19 treatments is limited.
Objective:
To examine the characteristics of older adults with COVID-19 and their costs for COVID-19–related medical care.
Design:
Retrospective observational study.
Setting:
Medical claims for Medicare fee-for-service (FFS) beneficiaries.
Patients:
Medicare FFS beneficiaries aged 65 years or older who had a COVID-19–related medical encounter during April through December 2020.
Measurements:
Patient characteristics and direct medical costs of COVID-19–related hospitalizations and outpatient visits.
Results:
Among 28.1 million Medicare FFS beneficiaries, 1 181 127 (4.2%) sought COVID-19–related medical care. Among these patients, 23.0% had an inpatient stay and 4.2% died during hospitalization. The majority of the patients were female (57.0%), non-Hispanic White (79.6%), and residents of an urban county (77.2%). Medicare FFS costs for COVID-19–related medical care were $6.3 billion; 92.6% of costs were for hospitalizations. The mean hospitalization cost was $21 752, and the mean length of stay was 9.2 days; hospitalization cost and length of stay were higher if the patient needed a ventilator ($49 441 and 17.1 days) or died ($32 015 and 11.3 days). The mean cost per outpatient visit was $164. Patients aged 75 years or older were more likely to be hospitalized, but their hospitalizations were associated with lower costs than for younger patients. Male sex and non-White race/ethnicity were associated with higher probability of being hospitalized and higher medical costs.
Limitation:
Results are based on Medicare FFS patients.
Conclusion:
The COVID-19 pandemic has resulted in substantial disease and economic burden among older Americans, particularly those of non-White race/ethnicity.
Primary Funding Source:
None.
As of 15 April 2021, more than 31.1 million confirmed COVID-19 cases and more than 560 000 deaths had been reported in the United States (1). These numbers are expected to increase, and the need for COVID-19 testing and treatments continues. The Families First Coronavirus Response Act ensures zero patient cost sharing for COVID-19 testing to anyone in the United States (2). Treatment after COVID-19 diagnosis is not free; payment is shared by patients, insurance payers, and health care providers, and the amount for which each stakeholder is responsible depends on the patient's insurance status and coverage.
Knowledge of the direct medical costs of COVID-19 treatments is limited. One published study used a simulation model to project direct medical costs during the course of COVID-19, including costs of ambulatory care, telephone consultations, over-the-counter medications, hospitalization, and postdischarge care (3). Because COVID-19–specific medical costs were not available, the study used costs of influenza and pneumonia care as proxies. Another report also used costs of influenza and pneumonia care to project COVID-19–related hospitalization costs (4).
The current study used a large administrative data set to examine characteristics and hospitalization risks among patients with COVID-19 who were aged 65 years or older—the age group most vulnerable to severe COVID-19 illness (5)—and to estimate the costs of hospitalizations and outpatient visits associated with the disease. Although studies have examined characteristics of patients with COVID-19 and hospitalization risks in the older population, these studies were based on small samples, used data from the first few months of the pandemic, and focused on countries outside the United States (6–8). Understanding the medical costs specific to COVID-19 is crucial, particularly for health care providers, insurance payers, and U.S. health care systems, because it provides information needed to plan and allocate resources to treat patients with COVID-19 and also provides insights into the financial sustainability of the U.S. health care system in combating the pandemic. The cost estimates could also be used to assess the economic value of COVID-19 vaccination, which could inform recommendations on immunization schedules as the vaccine becomes available to the general U.S. population.
Methods
Data
This study used 2020 Medicare fee-for-service (FFS) administrative claims data managed by the Centers for Medicare & Medicaid Services (CMS) (9). The CMS FFS database includes about 38 million Medicare beneficiaries enrolled in an FFS insurance plan, representing 62% of the total Medicare population (10). We used 4 data files: 1) the inpatient file, which contains institutional claims submitted by inpatient hospital providers; 2) the outpatient file, which contains institutional claims submitted by institutional outpatient providers (for example, hospital outpatient departments); 3) the carrier file, which contains noninstitutional claims submitted by individual providers and certain freestanding facilities (for example, clinical laboratories and ambulance service providers); and 4) the Master Beneficiary Summary files, which contain beneficiaries' enrollment and demographic information.
Although data through February 2021 are currently available, there is a lag between the date of service and when the claim is processed (11). Accordingly, our analysis included data from 1 April to 31 December 2020.
Study Population and Outcome Measure
The study population included adults aged 65 years or older who resided in any state or the District of Columbia; had a COVID-19–related hospitalization or outpatient visit claim with a date of outpatient visit, in-hospital death, or hospital discharge during 1 April through 31 December 2020; and were continuously enrolled in a Medicare FFS Part A and Part B insurance plan during the entire study period or until death. COVID-19–related medical encounters were identified if a medical claim included a principal or first-listed diagnosis code of U07.1, the International Classification of Diseases, Tenth Revision code that CMS has used since April 2020 to identify such encounters. One hospitalization may have had several claim records and, in a few cases (<1%), patients had more than 1 hospitalization associated with COVID-19. Evidence suggests that COVID-19 reinfections are rare (12, 13); therefore, we combined hospitalization claims if admission dates occurred within 6 months of the discharge date of the previous COVID-19–related hospitalization. Severe cases were defined as those requiring ventilator support and/or involving death. We used Medicare Severity Diagnosis Related Group codes 207 and 208 to define hospitalizations requiring ventilator support (14).
We examined patient characteristics and direct medical costs of COVID-19–related hospitalizations and outpatient visits. Patient characteristics included age (65 to 74, 75 to 84, and ≥85 years), sex (male vs. female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Asian/Pacific Islander, and other), and county of residence (urban vs. rural). We determined whether a county was urban or rural on the basis of the National Center for Health Statistics classification schemes, and we defined rural counties as those in the 2 nonmetropolitan categories and urban counties as those in the 4 metropolitan categories (15). We excluded patients who were missing information on selected characteristics (1.4% [n = 16 786]). Medical costs were defined as the sum of patients' cost sharing (deductibles, coinsurance, and copayments) and Medicare reimbursements for inpatient and outpatient services. Costs for prescription drugs and costs incurred in long-term care facilities (for example, nursing homes and skilled-nursing facilities) were not considered. Our costs were based on Medicare reimbursements, which likely differed from costs for providers and hospitals because COVID-19 does not have historical costs on which the Medicare diagnosis-related group payment system is based. When calculating costs, we excluded the 1.0% (n = 2670) of inpatient claims and the 5.0% (n = 151 581) of outpatient claims that had a reimbursement amount of zero, which resulted from Medicare being the secondary payer (that is, the patient was covered by another insurance plan, such as workers' compensation) (16).
Statistical Analysis
Descriptive statistics were used to examine patient characteristics and the mean cost per COVID-19–related outpatient visit and hospitalization. Though we report median cost, we focused on mean cost because our goal was to provide key parameters to calculate total medical costs associated with COVID-19. We used logistic regressions to examine associations between patient characteristics and the probability of being hospitalized; we estimated the adjusted probability of hospitalization and the adjusted risk difference with respect to the reference group for each characteristic. We used linear regressions to examine associations between patient characteristics and COVID-19–related medical costs. All analyses of patient characteristics and medical costs were examined separately based on 5 medical outcomes: outpatient visits only, all hospitalizations, hospitalizations without ventilator support and death, hospitalizations with ventilator support, and in-hospital death. The last 2 outcomes were not mutually exclusive. We used robust SEs clustered at the state level in all regressions to account for the nonindependence of observations within the same state.
We sought to determine if and to what extent disease trends changed among the study population in April through December 2020. We present monthly trends in the number of patients and in the mean hospitalization cost by the month of outpatient visits and hospitalization discharge date. Because the same patient could seek COVID-19–related medical care across different months, we assigned the patient to the month that he or she made the first outpatient visit or had his or her inpatient stay. Statistical analyses were performed using Stata, version 16 (StataCorp).
This study was reviewed by the Centers for Disease Control and Prevention (CDC) and was conducted in accordance with applicable federal law and CDC policy. As an analysis of secondary data without identifiers, the study did not require institutional review board review.
Role of the Funding Source
This study received no external funding.
Results
Patient Characteristics
During April through December 2020, 28.1 million Medicare FFS beneficiaries met our inclusion criteria, and 1 181 127 (4.2%) sought COVID-19–related medical care. Of these patients, 77.0% (n = 909 814) had outpatient visits only, and 23.0% (n = 271 313) had an inpatient stay (Table 1). Among hospitalized patients, 97.0% (n = 263 056) also had outpatient visits, 8.0% (n = 21 775) needed ventilator support, and 18.5% (n = 50 065) died during hospitalization; 68.1% (n = 34 083) of patients who died in the hospital did not have ventilator support. Most patients were female (57.0%), non-Hispanic White (79.6%), and residents of an urban county (77.2%). Patients aged 65 to 74 years accounted for the largest proportion (43.3%), followed by those aged 75 to 84 years (32.9%) and those aged 85 years or older (23.8%).
Table 1.
Characteristics of Patients With COVID-19
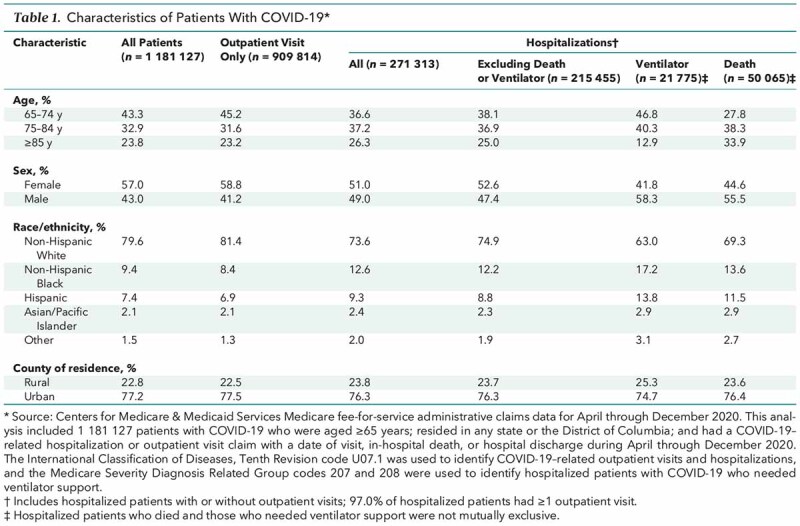
The characteristics of hospitalized patients were similar to those of patients with outpatient visits only, with some exceptions. First, Medicare beneficiaries aged 65 to 74 years accounted for the largest proportion of patients with outpatient visits only, whereas patients aged 75 years or older accounted for 72.2% of those who died during hospitalization. Similarly, males accounted for a larger proportion of patients who died (55.5%) and a larger proportion of those who needed ventilator support (58.3%), but the majority of patients with outpatient visits only were female. Second, although non-Hispanic Black and Hispanic patients respectively made up 8.4% and 6.9% of patients with outpatient visits only, they accounted for 17.2% and 13.8% of hospitalized patients requiring ventilator support and 13.6% and 11.5% of inpatient deaths.
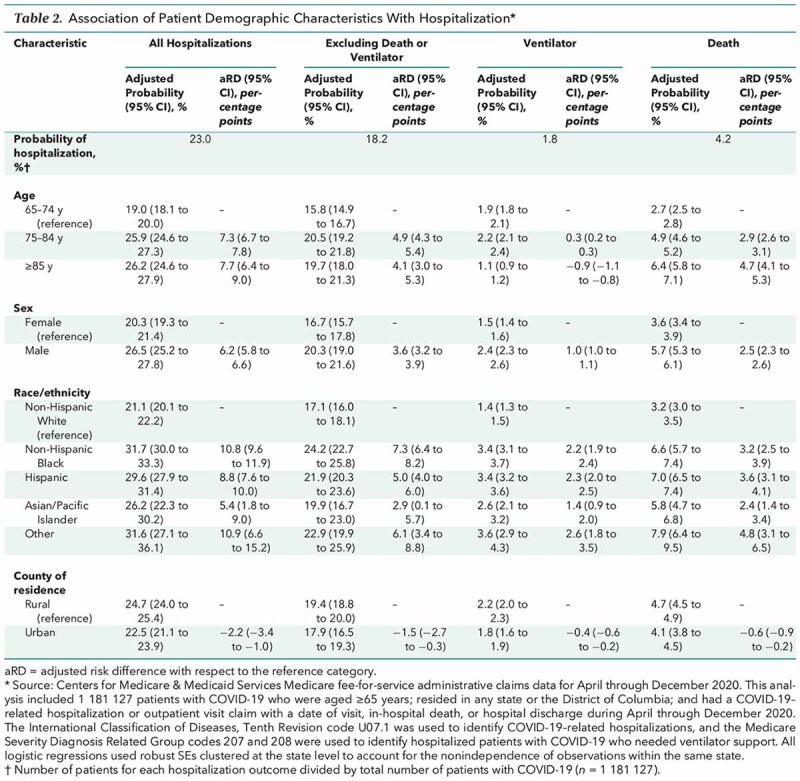
Among Medicare beneficiaries who sought medical care associated with COVID-19, the probabilities of being hospitalized for those aged 75 to 84 years and those aged 85 years or older were 7.3 (95% CI, 6.7 to 7.8) and 7.7 (CI, 6.4 to 9.0) percentage points higher and the probabilities of dying in the hospital were 2.9 (CI, 2.6 to 3.1) and 4.7 (CI, 4.1 to 5.3) percentage points higher than for those aged 65 to 74 years, respectively (Table 2). The probabilities for male patients to be hospitalized and to die in the hospital were 6.2 (CI, 5.8 to 6.6) and 2.5 (CI, 2.3 to 2.6) percentage points higher than for female patients, respectively. Compared with non-Hispanic White patients, the probability of being hospitalized was higher among non-Hispanic Black (10.8 [CI, 9.6 to 11.9] percentage points), Hispanic (8.8 [CI, 7.6 to 10.0] percentage points), and Asian/Pacific Islander (5.4 [CI, 1.8 to 9.0] percentage points) patients. These racial/ethnic groups were also more likely to die or need ventilator support during hospitalization than non-Hispanic White patients. Finally, patients residing in urban counties were 2.2 (CI, −3.4 to −1.0) percentage points less likely to be hospitalized than those residing in rural counties.
Table 2.
Association of Patient Demographic Characteristics With Hospitalization
Costs of COVID-19–Related Outpatient Visits and Hospitalizations
During April through December 2020, total medical costs for COVID-19–related medical care for patients in this study were $6.3 billion, with $466.8 million (7.4%) for outpatient visits and $5.8 billion (92.6%) for hospitalizations (Table 3). Most hospitalization costs (67.4% [$3.9 billion]) were for hospitalizations that did not require ventilator support or involve death. However, 18.3% ($1.1 billion) and 27.2% ($1.6 billion) of hospitalization costs were for those requiring ventilator support and those involving death, although they accounted for only 8.0% and 18.5% of total hospitalizations, respectively.
Table 3.
COVID-19–Related Medical Costs per Outpatient Visit and per Hospitalization, by Patient Demographic Characteristics

The mean cost per hospitalization was $21 752, and the mean length of inpatient stay was 9.2 days. Mean cost was higher if the patient died in the hospital ($32 015) and was highest if the patient needed ventilator support during hospitalization ($49 441). The mean cost per outpatient visit for patients who were not hospitalized was $164; the mean number of outpatient visits per patient was 3.2.
Table 3 presents mean costs by patient characteristics. Male patients incurred higher medical costs than female patients, regardless of medical outcome. The mean hospitalization cost decreased with increasing age; patients aged 65 to 74 years incurred the highest costs compared with patients in older age groups. Non-Hispanic White patients had the lowest outpatient cost ($161 [CI, $152 to $169]) and hospitalization cost ($20 382 [CI, $19 267 to $21 498]) compared with patients in all other racial and ethnic groups, regardless of medical outcome. Finally, cost per outpatient visit was lower for urban residents ($156 [CI, $131 to $182]) than rural residents ($196 [CI, $184 to $208]).
Cost per outpatient visit was $7.8 (CI, $5.2 to $10.5) higher and cost per hospitalization was $2250 (CI, $1906 to $2594) higher for male than female patients (Table 4). Compared with patients aged 65 to 74 years, hospitalization cost was $1712 (CI, −$1937 to −$1488) lower for patients aged 75 to 84 years and $4590 (CI, −$5007 to −$4173) lower for patients aged 85 years or older; the corresponding cost differences were $9349 (CI, −$10 204 to −$8494) and $18 747 (CI, −$20 179 to −$17 315), respectively, when we looked at in-hospital death. All racial/ethnic groups, particularly Hispanics and Asian/Pacific Islanders, incurred higher medical costs than non-Hispanic Whites; outpatient costs for Hispanics and Asian/Pacific Islanders were at least $30 higher and their costs for hospitalizations involving death or requiring ventilator support were atleast $8447 higher than among non-Hispanic Whites. Finally, outpatient cost for urban patients was $42 (CI, −$53 to −$30) lower than for patients in rural counties, and hospitalization cost was $968 (CI, −$528 to $2464) higher for patients in urban counties.
Table 4.
Adjusted Average Differences and 95% CIs in COVID-19–Related Medical Costs, by Patient Demographic Characteristics

Monthly Trends in the Number of Patients With COVID-19 and Hospitalization Costs
The number of patients with COVID-19 generally increased during the study period (Figure, top). The increase primarily occurred during September to December 2020, with patient counts in inpatient and outpatient care more than quadrupling. Trends in the number of hospitalized patients who needed a ventilator or died in the hospital were flat during the study period. For all hospitalization types, the mean cost per hospitalization increased in May and June 2020 and decreased in July 2020; during July to December 2020, the mean hospitalization cost remained steady (Figure, bottom).
Figure. Number of patients with COVID-19 (top) and costs per COVID-19–related hospitalization (bottom), by month.
Source: Centers for Medicare & Medicaid Services Medicare fee-for-service administrative claims data for April through December 2020. The International Classification of Diseases, Tenth Revision code U07.1 was used to identify COVID-19–related outpatient visits and hospitalizations, and the Medicare Severity Diagnosis Related Group codes 207 and 208 were used to identify hospitalized patients with COVID-19 who needed ventilator support. The analysis of the number of patients with COVID-19 included 1 181 127 patients who were aged ≥65 years; resided in any state or the District of Columbia; and had a COVID-19–related hospitalization or outpatient visit claim with a date of visit, in-hospital death, or hospital discharge during April through December 2020. The analysis of costs per COVID-19–related hospitalization included 268 706 hospitalizations.
Discussion
As of 23 January 2021, the U.S. hospitalization rate for COVID-19 was 15.7 per 100 000 persons (17) and the mortality rate was 1.7% (1). Using the uniquely large and representative sample of Medicare FFS beneficiaries, this study showed that COVID-19 disease burden among adults aged 65 years or older was substantially higher than in the general U.S. population: The hospitalization rate was more than 60 times higher (966 per 100 000 Medicare FFS beneficiaries), and the mortality rate was 2.5 times higher (4.2%). Existing data and studies have shown that age and sex are associated with COVID-19 mortality (1, 7, 18, 19). As of 1 March 2021, the CDC COVID Data Tracker reported that the mortality rate was 9.9% among adults aged 65 years or older versus 0.4% among those aged 64 years or younger (1). Yanez and colleagues (19) reported that the mortality rate was more than 62 times higher among adults aged 65 years or older compared with those aged 54 years or younger and was 77% higher in men than in women. Our results are consistent with these findings.
One novel finding from this study is that costs of COVID-19–related hospitalization decreased with age for the 5 medical outcomes considered. Possible reasons include higher mortality rates among older patients, resulting in shorter hospital stays and lower costs (our finding that the inpatient length of stay was shorter among patients aged ≥75 years than among those aged 65 to 74 years is consistent with this); the lower likelihood of younger adults to become seriously ill (those who reached the point of hospitalization may have had substantial risks and complications [20]); and less aggressive care with increasing age. Previous studies found that the percentage of hospital admissions that included intensive care unit stays decreased with age, as did the frequency of ventilator use, and that among patients admitted to an intensive care unit, older age was associated with higher rates of decisions to withhold aggressive care (21–23).
We found that 68.1% of patients who died in the hospital did not have ventilator support. The main reason might be related to age. Our data indicated that 80% of these patients were aged 75 years or older. Mortality rates were higher among older patients; the probability of dying before receiving ventilator support might be higher among older than younger hospitalized patients (24). Existing studies and our study showed decreasing ventilator use with advancing age of patients with COVID-19 (25, 26). As mentioned earlier, older patients were more likely to decline aggressive care. One published study also showed that ventilator use was not associated with mortality among older patients with COVID-19 (26). When considering the potential complications of using ventilators and the probability of survival, providers might also be less likely to recommend ventilator support to older patients. This could also explain why a large proportion of older patients died without ventilator support.
Our findings on hospitalization cost ($21 752), length of stay (9.2 days), and outpatient cost ($164) were higher than assumptions used in existing studies. Bartsch and colleagues (3) assumed a cost per COVID-19 outpatient visit of $142 and a cost per COVID-19 hospitalization of $6887 to $12 264, depending on patients' age and disease severity. Using these assumptions, they projected that the median cost during the course of a COVID-19 case that needed only outpatient visits was $96 for adults aged 65 years or older; for cases requiring an inpatient stay, the median cost was $14 859 for adults aged 65 to 84 years and $11 900 for adults aged 85 years or older (3). Using the Medicare reimbursement rate for hospitalizations for influenza and pneumonia, and assuming a length of 6 days for a COVID-19 inpatient stay, FAIR Health estimated an average hospitalization cost of $10 561 per Medicare patient (4). Our results show that the economic burden of COVID-19 is greater than previous studies have suggested. Furthermore, our estimates of the economic burden are likely conservative due to the exclusion of costs incurred in other medical settings and potential long-term sequelae (27, 28).
We observed racial and ethnic disparities in COVID-19–related costs: Racial and ethnic minority patients incurred higher medical costs than non-Hispanic White patients, and non-Hispanic Black and Hispanic patients accounted for disproportionately high numbers of hospitalizations requiring ventilator support and inpatient deaths. As of this writing, 3 COVID-19 vaccines have been authorized for emergency use (29). A nationally representative survey conducted in December 2020 tracked the public's attitudes and experiences with COVID-19 vaccination and reported that 35% of Black adults definitely or probably would not get vaccinated (30); our study found that this population had a higher probability of being hospitalized and higher medical costs per hospitalization. Taken together, our findings suggest that identifying effective strategies to promote COVID-19 vaccine uptake among disproportionately affected racial and ethnic minority populations is critical.
Although public health officials and health care professionals have persistently noted high risks for severe COVID-19 illness among older adults and have strongly advised limiting in-person interactions with other people in addition to other infection control practices (5), our data showed an increasing trend in the number of patients with COVID-19, with the number of hospitalized patients more than quadrupling between September and December 2020. However, the number of severe cases requiring hospitalization was steady during the study period, and the mean hospitalization cost decreased in July 2020 and then remained stable. In addition to providers' growing knowledge about the virus and experiences with treating patients, these results might also be due to new treatments developed over the course of the pandemic (29).
This study has limitations. First, it is based on Medicare FFS claims files because data on managed care claims are not available. Therefore, the results are not generalizable to all Medicare beneficiaries. However, we suspect that the results regarding the characteristics of patients with COVID-19 would be similar between Medicare FFS and managed care beneficiaries given that our results were consistent with those of existing studies that used various data sources (18, 19, 31). Previous studies have documented similar reimbursement rates between Medicare FFS and managed care plans over time (32, 33), suggesting that COVID-19–related medical costs between FFS and managed care beneficiaries might also be similar. However, further investigation is needed to verify the COVID-19–related medical costs of Medicare managed care enrollees. Second, the CMS Medicare database is generated from insurance claims; thus, this study did not capture people with asymptomatic COVID-19 and patients with minor symptoms that did not require medical attention, those who died before receiving care, or those who were misdiagnosed as not having COVID-19. However, misdiagnosis is becoming less common as providers gain knowledge about the virus, and most providers would submit claims to receive payments. In addition, this limitation should not affect our cost estimates because patients who did not seek care would not be included in the analysis.
Using data covering the claims of 28.1 million Medicare FFS beneficiaries, this study showed a high hospitalization and mortality rate among older Americans with COVID-19. The disease and economic burden of COVID-19 was higher among the racial and ethnic minority populations than among non-Hispanic White patients. As the pandemic continues, it is critical to continuously promote mitigation behaviors and vaccination among older adults to prevent infection and transmission of the virus. Identifying effective strategies to promote vaccine uptake is critical, and efforts are particularly needed among non-White persons aged 65 years or older to mitigate the increased disease and economic burden of COVID-19.
Footnotes
This article was published at Annals.org on 1 June 2021.
References
- 1. Centers for Disease Control and Prevention. COVID Data Tracker. Accessed at https://covid.cdc.gov/covid-data-tracker/#cases_casesper100klast7days on 5 March 2021.
- 2. Centers for Medicare & Medicaid Services. FAQs About Families First Coronavirus Response Act and Coronavirus Aid, Relief, and Economic Security Act Implementation Part 43. 23 June 2020. Accessed at www.cms.gov/files/document/FFCRA-Part-43-FAQs.pdf on 4 March 2021.
- 3. Bartsch SM , Ferguson MC , McKinnell JA , et al. The potential health care costs and resource use associated with COVID-19 in the United States. Health Aff (Millwood). 2020;39:927-35. [PMID: ] doi: 10.1377/hlthaff.2020.00426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. FAIR Health. The Projected Economic Impact of the COVID-19 Pandemic on the US Healthcare System. 25 March 2020. Accessed at www.fairhealth.org/article/fair-health-releases-brief-on-covid-19 on 4 March 2021.
- 5. Centers for Disease Control and Prevention. Older adults at greater risk of requiring hospitalization or dying if diagnosed with COVID-19. Updated 16 April 2021. Accessed at www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html on 1 March 2021.
- 6. Wu Z , McGoogan JM . Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239-42. [PMID: ] doi: 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 7. CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) – United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343-6. [PMID: ] doi: 10.15585/mmwr.mm6912e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sun H , Ning R , Tao Y , et al. Risk factors for mortality in 244 older adults with COVID-19 in Wuhan, China: a retrospective study. J Am Geriatr Soc. 2020;68:E19-E23. [PMID: ] doi: 10.1111/jgs.16533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Centers for Medicare & Medicaid Services. Chronic Conditions Data Warehouse. Accessed at www2.ccwdata.org/web/guest/home on 4 March 2021.
- 10. Centers for Medicare & Medicaid Services. Medicare Enrollment Section. Accessed at www.cms.gov/research-statistics-data-systems/cms-program-statistics/2019-medicare-enrollment-section on 12 April 2021.
- 11. Centers for Medicare & Medicaid Services. Chronic Conditions Data Warehouse. CCW White Paper: Medicare Claims Maturity. October 2017. Accessed at www2.ccwdata.org/web/guest/ccw-medicare-data-white-papers on 1 March 2021.
- 12. Lumley SF , O’Donnell D , Stoesser NE , et al; Oxford University Hospitals Staff Testing Group. Antibody status and incidence of SARS-CoV-2 infection in health care workers. N Engl J Med. 2021;384:533-40. [PMID: ] doi: 10.1056/NEJMoa2034545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hansen CH , Michlmayr D , Gubbels SM , et al. Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study. Lancet. 2021;397:1204-12. [PMID: ] doi: 10.1016/S0140-6736(21)00575-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Centers for Medicare & Medicaid Services. COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing. Updated 5 May 2021. Accessed at www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf on 4 March 2021.
- 15. National Center for Health Statistics, Centers for Disease Control and Prevention. NCHS Urban–Rural Classification Scheme for Counties. Accessed at www.cdc.gov/nchs/data_access/urban_rural.htm on 5 March 2021.
- 16. Centers for Medicare & Medicaid Services. Medicare Secondary Payer. Accessed at www.cms.gov/Medicare/Coordination-of-Benefits-and-Recovery/Coordination-of-Benefits-and-Recovery-Overview/Medicare-Secondary-Payer/Medicare-Secondary-Payer on 2 March 2021.
- 17. Centers for Disease Control and Prevention. Rates of COVID-19-Associated Hospitalization. Accessed at https://gis.cdc.gov/grasp/COVIDNet/COVID19_3.html on 5 March 2021.
- 18. Mallapaty S . The coronavirus is most deadly if you are older and male – new data reveal the risks. Nature. 2020;585:16-17. [PMID: ] doi: 10.1038/d41586-020-02483-2 [DOI] [PubMed] [Google Scholar]
- 19. Yanez ND , Weiss NS , Romand JA , et al. COVID-19 mortality risk for older men and women. BMC Public Health. 2020;20:1742. [PMID: ] doi: 10.1186/s12889-020-09826-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Katz MH . Regardless of age, obesity and hypertension increase risks with COVID-19. JAMA Intern Med. 2020. [PMID: ] doi: 10.1001/jamainternmed.2020.5415 [DOI] [PubMed] [Google Scholar]
- 21. Levinsky NG , Yu W , Ash A , et al. Influence of age on Medicare expenditures and medical care in the last year of life. JAMA. 2001;286:1349-55. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 22. Hamel MB , Lynn J , Teno JM , et al. Age-related differences in care preferences, treatment decisions, and clinical outcomes of seriously ill hospitalized adults: lessons from SUPPORT. J Am Geriatr Soc. 2000;48:S176-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 23. Levinsky NG , Ash AS , Yu W , et al. Patterns of use of common major procedures in medical care of older adults. J Am Geriatr Soc. 1999;47:553-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
- 24. Zane A, Kumar G, Bergl P, et al. Dying from pneumonia without having received mechanical ventilation: a contemporary analysis. Crit Care Med. 2018;46:215. doi:10.1097/01.ccm.0000528481.75970.e7
- 25. Ioannou GN , Locke E , Green P , et al. Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US veterans with SARS-CoV-2 infection. JAMA Netw Open. 2020;3:e2022310. [PMID: ] doi: 10.1001/jamanetworkopen.2020.22310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nicholson CJ , Wooster L , Sigurslid HH , et al. Estimating risk of mechanical ventilation and in-hospital mortality among adult COVID-19 patients admitted to Mass General Brigham: the VICE and DICE scores. EClinicalMedicine. 2021;33:100765. [PMID: ] doi: 10.1016/j.eclinm.2021.100765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Marshall M . The lasting misery of coronavirus long-haulers. Nature. 2020;585:339-41. [PMID: ] doi: 10.1038/d41586-020-02598-6 [DOI] [PubMed] [Google Scholar]
- 28. Carfì A , Bernabei R , Landi F ; Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603-5. [PMID: ] doi: 10.1001/jama.2020.12603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. U.S. Food and Drug Administration. Emergency Use Authorization. Accessed at www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization on 4 March 2021.
- 30. Hamel L, Kirzinger A, Muñana C, et al. KFF COVID-19 Vaccine Monitor: December 2020. Kaiser Family Foundation; 15 December 2020. Accessed at www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020 on 4 March 2021.
- 31. Centers for Disease Control and Prevention. Risk for COVID-19 Infection, Hospitalization, and Death By Age Group. Accessed at www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html on 4 March 2021.
- 32. Berenson RA , Sunshine JH , Helms D , et al. Why Medicare Advantage plans pay hospitals traditional Medicare prices. Health Aff (Millwood). 2015;34:1289-95. [PMID: ] doi: 10.1377/hlthaff.2014.1427 [DOI] [PubMed] [Google Scholar]
- 33. Chen JL , Hicks AL , Chernew ME . Prices for physician services in Medicare Advantage versus traditional Medicare. Am J Manag Care. 2018;24:341-4. [PMID: ] [PMC free article] [PubMed] [Google Scholar]



