Abstract
Medial closed wedge distal femoral osteotomy (MCWDFO) has been widely performed for lateral-compartment osteoarthritis since the development of a biplanar osteotomy technique using existing MCWDFO-specific plates. To further improve this system and the technique, we have developed a newly designed MCWDFO plate (TriS-MDFO; Olympus Terumo Biomaterials). The improved shape of the plate consists of a larger head–shaft angle to fit the distal femur after MCWDFO, more distally oriented distal screws to enable longer screw insertion, and a diamond-shaped plate head to avoid interference with the medial patellofemoral ligament. Technically, to overcome the difficulty in inserting proximal screws through the vastus medialis muscle, a cannulated screw system was employed. This system can prevent difficulties in removing the screw due to cross-threading when plate removal is required. Furthermore, we designed a novel compression hook device with a bulb-shaped head to hook on a screw hole to apply a compressive force to the osteotomized site. On the plate side, a characteristic 1.5 mm-thickness stopper is installed to prevent slippage of the hook device. This optimal compression system can minimize the risk of lateral hinge fracture during the compression procedure. These improvements in the TriS-MDFO may increase the ease and safety of MCWDFO.
Technique Video
This is a technique video to explain medial closed wedge distal femoral osteotomy with the TriS Medial DFO Plate. We have a consultancy agreement with Olympus Terumo Biomaterials. Here, we demonstrate the surgical procedure of the left knee. The operation was performed with the patient in the supine position under general anesthesia. Arthroscopic resection or repair of a torn lateral meniscus, if present, was performed through an anterolateral portal and an anteromedial portal. A medial parapatellar straight incision is made from the anteromedial portal. The vastus medialis muscle is elevated and a radiolucent retractor is inserted. The muscular branches from the descending genicular artery are coagulated or ligated. The knee is then flexed, keeping enough distance from the neurovascular bundle, and another radiolucent retractor is inserted into the posterior aspect. At the midpoint of the anteroposterior femoral width, the first K-wire is inserted from 4 cm from the medial epicondyle to just below the hinge point. The second K-wire is inserted proximally at the planned distance aimed at above the hinge point. The osteotomy lines are then drawn with an electrosurgical knife. We first cut the ascending osteotomy line, leaving the lateral cortex intact. The knee is then flexed and the distal and the proximal oblique osteotomies are performed between the 2 K-wires. After the wedge is removed, a reciprocating saw is inserted to trim the osteotomy line. Finally, the ascending cut is completed with an oscillating saw and a chisel and the wedge is closed. This plate has characteristic stoppers for a compression hook device at hole 1 and hole 2. The plate is installed and temporarily fixed with 2 K-wires. Using a cannulation technique with a pin, the first locking screw is inserted into hole C. Hole D is then drilled and the cannulated screw is inserted and locked. The compression hook is attached to hole-1 with a thick stopper and a K-wire is inserted into the hook’s end. The hook is aligned as perpendicularly as possible to the oblique osteotomy line. The hook is then tightened with a dedicated cannulated screwdriver using 2 or 3 fingers. Bicortical locking screws are inserted into holes 2 and 3 and locked. The hook is then taken away and additional locking screws are inserted into the remaining holes. If the vastus medialis muscle is not easily retractable, we apply a cannulation technique. A K-wire is inserted through a sleeve and the lateral cortex is penetrated. A monocortical drill hole is made and the screw can then be inserted without cross-threading. We can confirm that the mechanical axis of the corrected knee passes through the center of the knee.
Medial closed wedge distal femoral osteotomy (MCWDFO) is widely performed for valgus knee with lateral-compartment osteoarthritis when the deformity center is located at the distal femur. Although favorable short- to mid-term results have been reported since the development of a biplanar osteotomy with existing plates,1,2 the following problems remain, especially in the Asian population, who have smaller femurs: (1) the straight shape of the plate, which sometimes requires bending; (2) an inappropriate distal screw direction, which sometimes interposes into the osteotomized site; (3) interference with the medial patellofemoral ligament (MPFL); (4) difficulty in inserting proximal screws, and (5) risk of lateral hinge fracture (LHF) during the application of compression to the osteotomized site using a lag screw. To improve these potential disadvantages, the authors have developed a newly designed MCWDFO-specific locking plate made of titanium alloy (TriS Medial DFO Plate [TriS-MDFO], Olympus Terumo Biomaterials, Tokyo, Japan).
Improvement in the TriS-MDFO
Regarding the plate design, a more anatomically shape was adopted to fit the medial cortex after MCWDFO without bending. The head–shaft angle of the representative existing plate and the TriS-MDFO is 20° and 40°, respectively (Fig 1 A and B). In addition to the difference in the head–shaft angle, the distal screws are aimed 12° more distally compared with the existing plate (Fig 1 A and B). This improvement enables the insertion of longer screws to achieve greater stability, without interference with the oblique osteotomy line (Fig 1B). Furthermore, a square-shaped head sometimes interferes with the MPFL in small femurs, which can result in flexion loss.3 We therefore designed a diamond-shaped head to avoid this (Fig 1 C and D, and 2).
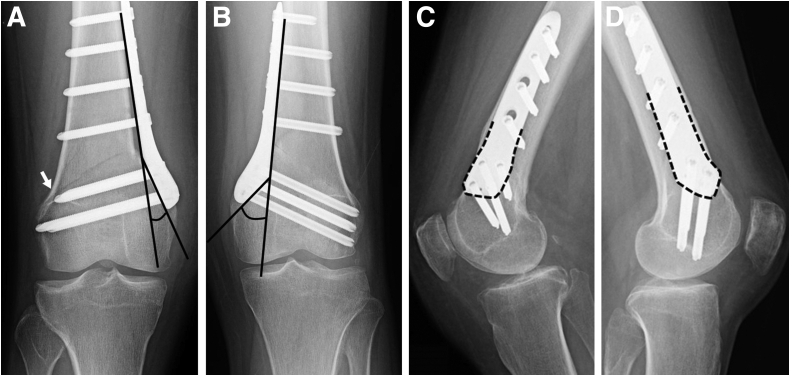
Fig 1.
Postoperative radiographs of 31-year-old female patient who underwent medial closed wedge distal femoral osteotomy with TomoFix MDF (Synthes GmbH; Solothurn, Switzerland) in her right knee and with TriS-MDFO in her left knee. (A) Anteroposterior view of the right knee. The head-shaft angle (black lines) of the TomoFix MDF is 20° and the distal screws are oriented approximately 5° distal to the direction of the proximal screws. Because of the discrepancy between the direction of the osteotomy line and the distal screws, the screws just distal to the transverse cut draw closer to the osteotomized line (white arrow). (B) Anteroposterior view of the left knee. The head–shaft angle (black lines) of the TriS-MDFO is 40° and the distal screws are oriented approximately 17° distal to the direction of the proximal screws. Owing to the improvement in the screw direction, the longer distal screws can be inserted more parallel to the osteotomized line. (C) Lateral view of the right knee demonstrates the square-shaped head design (dashed black line) of the TomoFix MDF. (D) Lateral view of the left knee demonstrates the new diamond-shaped head design (dashed black line) of the TriS-MDFO.
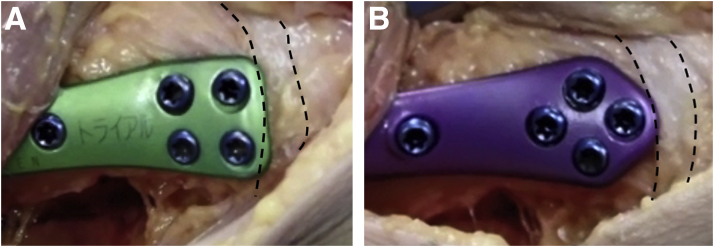
Fig 2.
Interference of the plate head with the medial patellofemoral ligament (MPFL). Trial plates were installed on a cadaveric knee. Dashed lines indicate the proximal and distal margin of the MPFL. (A) The conventional square-shaped head interfered with the MPFL over a large contact area. (B) The newly developed diamond-shaped head decreases the contact area.
Regarding the screws, a cannulated screw system was employed. Insertion of proximal screws can be difficult, especially in patients with obesity and in patients with a thick vastus medialis muscle. The cannulated system helps insertion of the screw in an appropriate direction for such patients, even under the mini-incision technique.
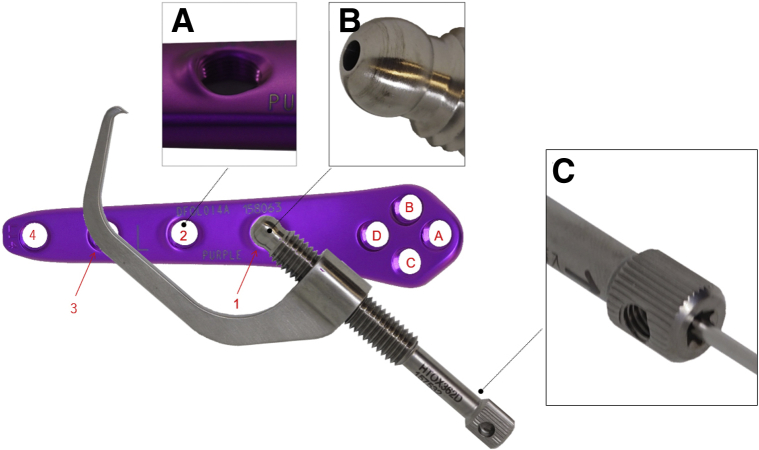
In addition to the plate and the screws, we also designed an original compression hook device (Fig 3), which has a proximal bulb-shaped head to hook onto the screw hole. On the plate side, a characteristic 1.5 mm-thickness stopper (Fig 3) is installed to prevent slippage. After the bulb-shaped head is hooked on the stopper, the lateral cortex is held by the hook, allowing compressive force to be applied with a dedicated screwdriver for the hook. In the event of slippage, a Kirschner wire (K-wire) can be inserted into the hook’s cannulated end (Fig 3). The pearls and pitfalls of the TriS-MDFO are described in the Discussion section and listed in Table 1.
Fig 3.
TriS-MDFO Plate and the compression hook device. The red numbers and letters indicate the name of the screw holes. Hole 1 and 2 have stoppers (A). The combination of the bulb-shaped hook base (B) and the screw hole bumpers (A) prevents slippage of the hook during compression. Any slippage can be addressed by inserting a Kirschner wire into the cannulated hole (C).
Table 1.
Pearls and Pitfalls of the TriS Medial DFO Plate
| Pearls |
| 1. A diamond-shaped plate head instead of a square-shaped head |
|
| 2. More distally aimed distal screws |
|
| 3. Cannulated structure of the screws |
|
|
|
| 4. A specifically designed compression hook |
|
|
|
| Pitfalls |
|
|
|
Surgical Procedure (With Video Illustration)
Approach
We use a conventional medial parapatellar straight incision (Fig 4A) and a subvastus approach (Video 1). The muscular branches from the descending genicular artery4,5 are coagulated or ligated to prevent bleeding (Fig 4B). Not using a tourniquet allows identification of these branches and monitoring of the popliteal artery pulse.
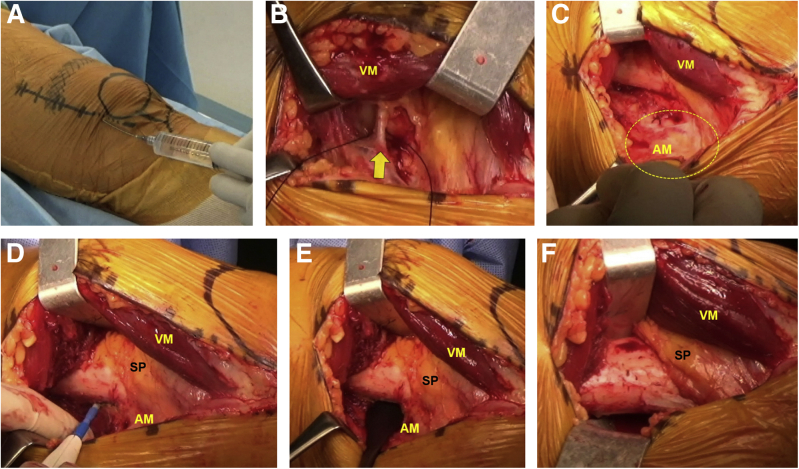
Fig 4.
Surgical exposure (left knee). (A) A medial parapatellar straight incision is made from the anteromedial portal of the arthroscopy. A multimodal drug injection cocktail (epinephrine [0.2 mg]-containing lidocaine [200 mg, 20 mL]; ropivacaine [75 mg, 10 mL]; and dexamethasone sodium phosphate [3.8 mg, 1 mL]) was injected around the skin incision and into the vastus medialis muscle belly. (B) The vastus medialis muscle is elevated and the muscular branches from the descending genicular artery (yellow arrow) are coagulated or ligated. (C) The aponeurotic insertion of the adductor magnus tendon is attached to the posteromedial aspect of the distal femur (yellow dashed line). (D) The aponeurotic insertion is detached from the femur using an electrosurgical knife. (E) The posterior aspect of the femur is retracted with a Cobb elevator. (F) Both the anterior and posterior aspects of the distal femur are well exposed using 2 radiolucent retractors. (AM, adductor magnus tendon; SP, suprapatellar pouch; VM, vastus medialis muscle.)
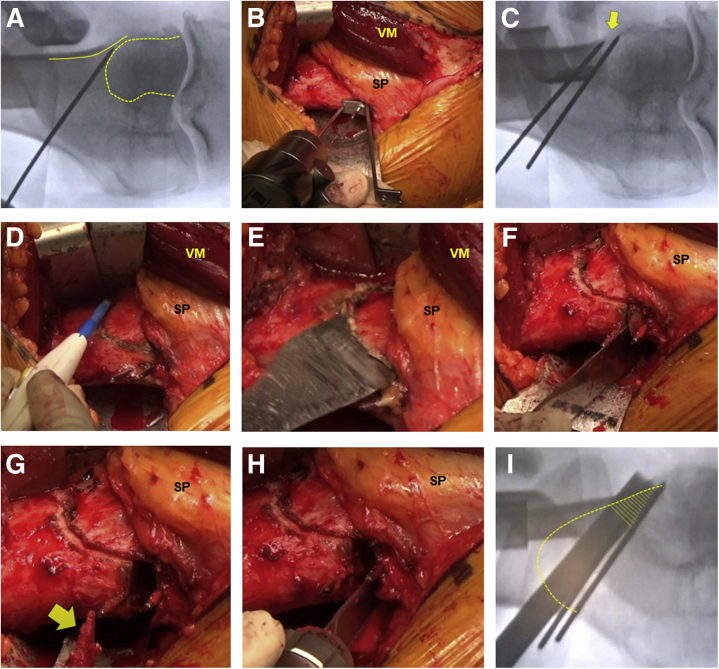
Osteotomy
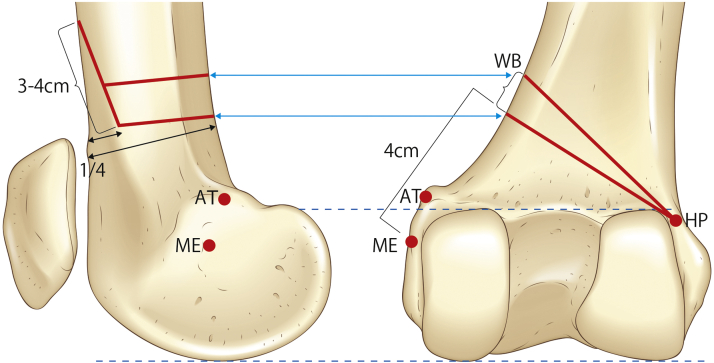
A biplanar MCWDFO1, 2, 3 is performed under K-wire guidance with sufficient retraction (Fig 4 B-F; Video 1). The method used to determine the osteotomy lines is listed in Table 2. Although the conventional hinge point1,2 was usually set just proximal to the upper border of the lateral condyle, a slightly distal hinge is now recommended to prevent an unstable LHF.6 We set the hinge point just distal to the upper border of the lateral condyle and in between the lateral cortex and the contour of the lateral condyle (Fig 5). The distal oblique osteotomy (i.e., transverse cut) is started from 4 cm proximal to the medial femoral epicondyle and the proximal oblique osteotomy is started at the planned distance from the distal oblique osteotomy (Fig 5, 6 A-C). The ascending osteotomy is created with one-fourth of the anteroposterior width and a length of approximately 3 to 4 cm (Fig 5, 6 D and E). Our target postoperative weight-bearing line is aimed to fall between the center of the intercondylar eminence and the top of the medial eminence.
Table 2.
Determination of Osteotomy Lines
|
|
|
|
|
|
Fig 5.
Osteotomy lines. The red lines indicate osteotomy lines on the lateral view from the medial side and on the coronal view from the posterior side. (AT, Adductor tubercle; HP, hinge point; ME, medial epicondyle; WB, wedge base.)
Fig 6.
Biplane osteotomy (left knee). (A) The first K-wire for the distal oblique osteotomy is inserted 4 cm from the medial epicondyle in the direction of a tangent of the lateral condyle (yellow dashed line). The tip of the K-wire is emplaced between the lateral condyle (yellow dashed line) and the lateral cortex of the femoral shaft (yellow line). (B) A second K-wire is inserted proximally at the planned distance using a width gauge. (C) The tips of the K-wires do not meet, allowing a chisel or a saw blade to be inserted into the hinge point. (D) The osteotomy lines are drawn with an electrosurgical knife. (E) The rough cut of the ascending osteotomy, leaving the lateral cortex intact to prevent lateral hinge fracture, is performed previous to the oblique osteotomies. (F) The distal and the proximal oblique osteotomies are performed between the 2 K-wires. (G) Owing to the rough cut of the ascending osteotomy, the wedge can be easily removed (yellow arrow) when the proximal and distal oblique osteotomy lines meet together. (H) The posterior cortices are trimmed using a reciprocating saw. (I) To prevent an unstable lateral hinge fracture, it is crucial to cut the lateral portion of the ascending osteotomy line (yellow shaded area) completely. (SP, suprapatellar pouch; VM, vastus medialis muscle.)
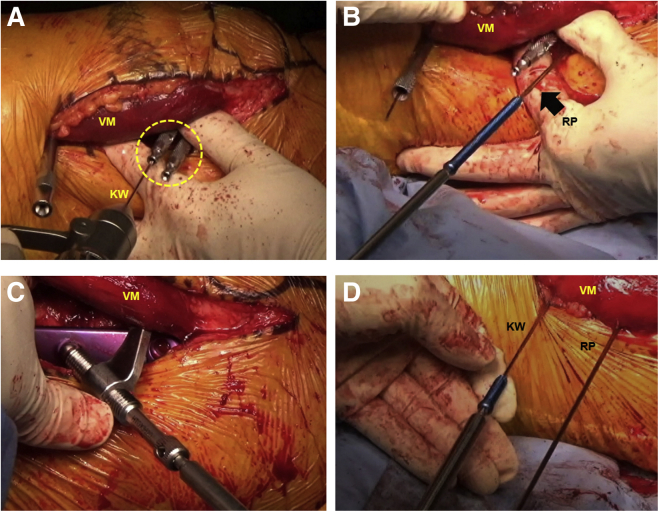
Fixation with Plate
After we remove the bony wedge between the osteotomies, both oblique and ascending cut are completed using a reciprocating saw and chisel (Fig 6 F-I; Video 1). The wedge is then gradually closed and the plate is temporarily fixed with 2 K-wires (Fig 7A). Two distal screws are inserted and locked in place of the distal temporary K-wire. Before each screw is inserted, a round-tip pin, such as a blunt K-wire, is inserted into the drill hole to confirm its direction and to guide insertion of a cannulated screw (Fig 7B).
Fig 7.
Plate fixation (left knee). (A) After gradual wedge closure, the plate is temporarily fixed with 2 K-wires. Because of the interference between sleeves caused by the larger head-shaft angle, it is difficult to use K-wire sleeves of conventional length, and short sleeves are therefore used for the distal part of the osteotomy (yellow dashed line). (B) Distal screws are inserted through a round-tip pin to confirm the appropriate direction. (C) The compression hook is attached to the hole with a thick stopper and tightened with a dedicated screwdriver to compress the osteotomy site. (D) The most proximal monocortical screw (hole 4 of Fig 3) is inserted through a K-wire which penetrates the lateral cortex. The round-tip pin which is inserted into hole 2 or hole 1 also can be used as reference for the appropriate parallel direction of the proximal screws. These procedures can prevent cross-threading. (KW, Kirschner wire; RP, round-tip pin; VM, vastus medialis muscle.)
The compression hook is attached to the hole with a thick stopper and tightened with a dedicated screwdriver to compress the osteotomy site (Fig 7C). The proximal K-wire for the temporary fixation is replaced by a bicortical locking screw and an additional locking screw is added to one of the proximal holes. The hook can then be taken away and more locking screws are inserted into the remaining holes.
Monocortical fixation is recommended for the most proximal hole to prevent stress concentration at the plate end. When the vastus medialis muscle is not easily retractable, a K-wire is inserted through a K-wire sleeve in a drill sleeve between the muscle fibers. After the K-wire penetrates the lateral cortex, a mono-cortical drill hole is made using a cannulated drill. By using the K-wire for guidance in inserting the cannulated screw, cross-threading can be prevented (Fig 7D). A general outline of the surgical procedure is described in Table 3.
Table 3.
Surgical Procedure
| 1. Approach |
|
|
|
|
|
|
| 2. Osteotomy |
|
|
|
|
|
|
| 3. Fixation |
|
|
|
|
|
|
Postoperative Rehabilitation
Range of motion exercise is started on the first postoperative day and is advanced gradually as tolerated. Full weight-bearing begins 4 to 6 weeks after surgery, depending on the situation of the hinge.
Discussion
Our modification of the TriS-MDFO aimed to (1) improve the design issue of the plate itself, (2) overcome the MCWDFO-specific technical difficulty in inserting proximal screws, and (3) avoid technical pitfall in using a lag screw. The improved plate design enabled better plate fitting, insertion of longer distal screws, and less impingement on the MPFL. However, the latter 2 technical problems cannot be solved solely via design modification of the plate. One of the most general problems with locking compression plates is jamming of the screw head into the plate hole by cross-threading.7 Particularly in the MCWDFO, the thick vastus medialis muscle may lead to the insertion of proximal screws in the wrong direction. In bicortical fixation, the screw direction can eventually be controlled even when the screw reaches the lateral screw hole. In monocortical fixation, however, it is not necessarily easy to insert a screw in the appropriate direction because of the lack of this directional correction by the lateral screw hole. Furthermore, this cannulated system can prevent cross-threading of monocortical locking screws, simplifying plate removal surgery if needed.
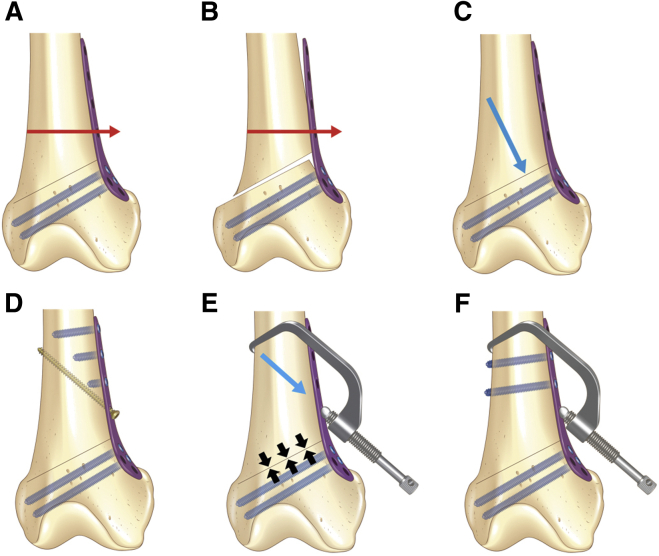
Application of compression to the osteotomized site can also be key to successful MCWDFO. Although compression is conventionally applied with a temporary lag screw (TLS),8 this can be problematic. First, sufficient compression cannot be provided in cases of severe osteoporosis. Even when the femur is not osteoporotic, the tightening procedure of the TLS can generate an LHF with medial translation when it is inserted perpendicular to the plate (Fig 8 A and B). A more perpendicular insertion to the oblique osteotomy line, which aims for the far more proximal cortex, would be theoretically ideal (Fig 8C). However, the direction may cause difficulty in inserting the TLS due to the overlong screw and interference between the proximal locking screws and the TLS (Fig 8D). In the TriS-MDFO, application of the perpendicular compressive force to the oblique osteotomy line can be easily provided by grasping the lateral cortex without any interference (Video 1, Fig 8 E and F). Slippage of the proximal end of the hook from the screw hole can be prevented by its characteristic shape and the thick stopper on the screw hole, and eliminated by K-wire insertion into the cannulated hole of the hook (Fig 3).
Fig 8.
Compressive direction and compression devices. (A) Compressive force in a direction perpendicular to the plate (red arrow). (B) The force causes medial translation of the proximal fragment with a lateral hinge fracture (red arrow). (C) The ideal compressive direction may be perpendicular to the osteotomized line (blue arrow). (D) When the compressive force is applied with a temporary lag screw, the screw direction may hinder insertion of the screw tip into the lateral drill hole due to the overlong screw. The temporary lag screw causes interference with the proximal locking screws. (E) The compression hook is mounted as perpendicularly as possible to the osteotomized line and tightened to provide compressive force (blue arrow). The direction provides an appropriate compressive force to the osteotomized site without lateral hinge fracture (black arrows). (F) As the compression hook does not penetrate the femoral shaft, interference between the compression hook and locking screws is avoided.
A number of possible risks and limitations in the use of this plate should be considered. First, to ensure rigid fixation, it is made of a titanium alloy, which is stiffer than pure titanium. In cases with delayed union, the poor elasticity of the plate induces stress concentration at the plate end when micromotion persists, raising the possibility of stress fracture at the site. Second, the larger head–shaft angle may confer a risk of plate-fracture in return for the better fitting. Data from mid- to long-term follow-up are not yet available, and further careful long-term follow-up studies are required.
In conclusion, the TriS-MDFO Plate with a cannulated system and an optimized compression system represent an improvement over the existing MCWDFO-specific plate and may increase the ease and safety of MCWDFO for valgus knees.
Acknowledgments
The authors thank Tomoyuki Shimakawa, Mai Nakamiya, Howard Colefield, and MEDICAL VIEW Co., LTD. for shooting the video, editing the video, narrating the video transcript, and drawing the figures, respectively.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: T.A., R.N., H.N., and R.T. report consultancy with Olympus Terumo Biomaterials, outside the submitted work. E.K. reports grants from Olympus Terumo Biomaterials, Smith & Nephew, and Japan Tissue Engineering, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This is a technique video to explain medial closed wedge distal femoral osteotomy with the TriS Medial DFO Plate. We have a consultancy agreement with Olympus Terumo Biomaterials. Here, we demonstrate the surgical procedure of the left knee. The operation was performed with the patient in the supine position under general anesthesia. Arthroscopic resection or repair of a torn lateral meniscus, if present, was performed through an anterolateral portal and an anteromedial portal. A medial parapatellar straight incision is made from the anteromedial portal. The vastus medialis muscle is elevated and a radiolucent retractor is inserted. The muscular branches from the descending genicular artery are coagulated or ligated. The knee is then flexed, keeping enough distance from the neurovascular bundle, and another radiolucent retractor is inserted into the posterior aspect. At the midpoint of the anteroposterior femoral width, the first K-wire is inserted from 4 cm from the medial epicondyle to just below the hinge point. The second K-wire is inserted proximally at the planned distance aimed at above the hinge point. The osteotomy lines are then drawn with an electrosurgical knife. We first cut the ascending osteotomy line, leaving the lateral cortex intact. The knee is then flexed and the distal and the proximal oblique osteotomies are performed between the 2 K-wires. After the wedge is removed, a reciprocating saw is inserted to trim the osteotomy line. Finally, the ascending cut is completed with an oscillating saw and a chisel and the wedge is closed. This plate has characteristic stoppers for a compression hook device at hole 1 and hole 2. The plate is installed and temporarily fixed with 2 K-wires. Using a cannulation technique with a pin, the first locking screw is inserted into hole C. Hole D is then drilled and the cannulated screw is inserted and locked. The compression hook is attached to hole-1 with a thick stopper and a K-wire is inserted into the hook’s end. The hook is aligned as perpendicularly as possible to the oblique osteotomy line. The hook is then tightened with a dedicated cannulated screwdriver using 2 or 3 fingers. Bicortical locking screws are inserted into holes 2 and 3 and locked. The hook is then taken away and additional locking screws are inserted into the remaining holes. If the vastus medialis muscle is not easily retractable, we apply a cannulation technique. A K-wire is inserted through a sleeve and the lateral cortex is penetrated. A monocortical drill hole is made and the screw can then be inserted without cross-threading. We can confirm that the mechanical axis of the corrected knee passes through the center of the knee.
References
- 1.van Heerwaarden R., Brinkman J.M., Pronk Y. Correction of femoral valgus deformity. J Knee Surg. 2017;30:746–755. doi: 10.1055/s-0037-1602138. [DOI] [PubMed] [Google Scholar]
- 2.Brinkman J.M., Freiling D., Lobenhoffer P., Staubli A.E., van Heerwaarden R.J. Supracondylar femur osteotomies around the knee: Patient selection, planning, operative techniques, stability of fixation, and bone healing. Orthopade. 2014;43(suppl 1):S1–S10. doi: 10.1007/s00132-014-3007-6. [DOI] [PubMed] [Google Scholar]
- 3.Nakamura R., Fujita K., Omi R., et al. Closed Wedge Distal femoral osteotomy with a polyaxial locking plate designed for the proximal tibia: Minimum 5-year outcomes. Knee Surg Relat Res. 2017;29:232–236. doi: 10.5792/ksrr.17.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van der Woude J.A., van Heerwaarden R.J., Bleys R.L. Periosteal vascularization of the distal femur in relation to distal femoral osteotomies: A cadaveric study. J Exp Orthop. 2016;3:6. doi: 10.1186/s40634-016-0042-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bakri K., Shin A.Y., Moran S.L. The vascularized medial femoral corticoperiosteal flap for reconstruction of bony defects within the upper and lower extremities. Semin Plast Surg. 2008;22:228–233. doi: 10.1055/s-2008-1081405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nha K.W., Chang Y.S., Shon O.J., et al. Where is the target point to prevent cortical hinge fracture in medial closing-wedge distal femoral varus osteotomy? J Knee Surg. 2019;32:274–279. doi: 10.1055/s-0038-1641144. [DOI] [PubMed] [Google Scholar]
- 7.Fujita K., Yasutake H., Horii T., Hashimoto N., Kabata T., Tsuchiya H. Difficulty in locking head screw removal. J Orthop Sci. 2014;19:304–307. doi: 10.1007/s00776-013-0503-1. [DOI] [PubMed] [Google Scholar]
- 8.Staubli A.E., De Simoni C., Babst R., Lobenhoffer P. TomoFix: A new LCP-concept for open wedge osteotomy of the medial proximal tibia—early results in 92 cases. Injury. 2003;34:B55–B62. doi: 10.1016/j.injury.2003.09.025. (suppl 2) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This is a technique video to explain medial closed wedge distal femoral osteotomy with the TriS Medial DFO Plate. We have a consultancy agreement with Olympus Terumo Biomaterials. Here, we demonstrate the surgical procedure of the left knee. The operation was performed with the patient in the supine position under general anesthesia. Arthroscopic resection or repair of a torn lateral meniscus, if present, was performed through an anterolateral portal and an anteromedial portal. A medial parapatellar straight incision is made from the anteromedial portal. The vastus medialis muscle is elevated and a radiolucent retractor is inserted. The muscular branches from the descending genicular artery are coagulated or ligated. The knee is then flexed, keeping enough distance from the neurovascular bundle, and another radiolucent retractor is inserted into the posterior aspect. At the midpoint of the anteroposterior femoral width, the first K-wire is inserted from 4 cm from the medial epicondyle to just below the hinge point. The second K-wire is inserted proximally at the planned distance aimed at above the hinge point. The osteotomy lines are then drawn with an electrosurgical knife. We first cut the ascending osteotomy line, leaving the lateral cortex intact. The knee is then flexed and the distal and the proximal oblique osteotomies are performed between the 2 K-wires. After the wedge is removed, a reciprocating saw is inserted to trim the osteotomy line. Finally, the ascending cut is completed with an oscillating saw and a chisel and the wedge is closed. This plate has characteristic stoppers for a compression hook device at hole 1 and hole 2. The plate is installed and temporarily fixed with 2 K-wires. Using a cannulation technique with a pin, the first locking screw is inserted into hole C. Hole D is then drilled and the cannulated screw is inserted and locked. The compression hook is attached to hole-1 with a thick stopper and a K-wire is inserted into the hook’s end. The hook is aligned as perpendicularly as possible to the oblique osteotomy line. The hook is then tightened with a dedicated cannulated screwdriver using 2 or 3 fingers. Bicortical locking screws are inserted into holes 2 and 3 and locked. The hook is then taken away and additional locking screws are inserted into the remaining holes. If the vastus medialis muscle is not easily retractable, we apply a cannulation technique. A K-wire is inserted through a sleeve and the lateral cortex is penetrated. A monocortical drill hole is made and the screw can then be inserted without cross-threading. We can confirm that the mechanical axis of the corrected knee passes through the center of the knee.
This is a technique video to explain medial closed wedge distal femoral osteotomy with the TriS Medial DFO Plate. We have a consultancy agreement with Olympus Terumo Biomaterials. Here, we demonstrate the surgical procedure of the left knee. The operation was performed with the patient in the supine position under general anesthesia. Arthroscopic resection or repair of a torn lateral meniscus, if present, was performed through an anterolateral portal and an anteromedial portal. A medial parapatellar straight incision is made from the anteromedial portal. The vastus medialis muscle is elevated and a radiolucent retractor is inserted. The muscular branches from the descending genicular artery are coagulated or ligated. The knee is then flexed, keeping enough distance from the neurovascular bundle, and another radiolucent retractor is inserted into the posterior aspect. At the midpoint of the anteroposterior femoral width, the first K-wire is inserted from 4 cm from the medial epicondyle to just below the hinge point. The second K-wire is inserted proximally at the planned distance aimed at above the hinge point. The osteotomy lines are then drawn with an electrosurgical knife. We first cut the ascending osteotomy line, leaving the lateral cortex intact. The knee is then flexed and the distal and the proximal oblique osteotomies are performed between the 2 K-wires. After the wedge is removed, a reciprocating saw is inserted to trim the osteotomy line. Finally, the ascending cut is completed with an oscillating saw and a chisel and the wedge is closed. This plate has characteristic stoppers for a compression hook device at hole 1 and hole 2. The plate is installed and temporarily fixed with 2 K-wires. Using a cannulation technique with a pin, the first locking screw is inserted into hole C. Hole D is then drilled and the cannulated screw is inserted and locked. The compression hook is attached to hole-1 with a thick stopper and a K-wire is inserted into the hook’s end. The hook is aligned as perpendicularly as possible to the oblique osteotomy line. The hook is then tightened with a dedicated cannulated screwdriver using 2 or 3 fingers. Bicortical locking screws are inserted into holes 2 and 3 and locked. The hook is then taken away and additional locking screws are inserted into the remaining holes. If the vastus medialis muscle is not easily retractable, we apply a cannulation technique. A K-wire is inserted through a sleeve and the lateral cortex is penetrated. A monocortical drill hole is made and the screw can then be inserted without cross-threading. We can confirm that the mechanical axis of the corrected knee passes through the center of the knee.