Abstract
Objective
Limited data exist describing possible delays in patient transfer from the emergency department (ED) as a result of language barriers and the effects of interpretation services. We described the differences in ED length of stay (LOS) before intensive care unit (ICU) arrival and mortality based on availability of telephone or in‐person interpretation services.
Methods
Using an ICU database from an urban academic tertiary care hospital, ED patients entering the ICU were divided into groups based on primary language and available interpretation services (in‐person vs telephone). Non‐parametric tests were used to compare ED LOS and mortality between groups.
Results
Among 22,422 included encounters, English was recorded as the primary language for 51% of patients (11,427), and 9% of patients (2042) had a primary language other than English. Language was not documented for 40% of patients (8953). Among encounters with patients with non‐English primary languages, in‐person interpretation was available for 63% (1278) and telephone interpretation was available for 37% (764). In the English‐language group, median ED LOS was 292 minutes (interquartile range [IQR], 205–412) compared with 309 minutes (IQR, 214–453) for patients speaking languages with in‐person interpretation available and 327 minutes (IQR, 225–463) for patients speaking languages with telephone interpretation available. Mortality was higher among patients with telephone (15%) or in‐person (11%) interpretation available compared with patients who primarily spoke English (9%).
Conclusions
Patients with primary languages other than English who were critically ill spent a median of 17 to 35 more minutes in the ED before ICU arrival and experienced higher mortality rates compared with patients who spoke English as a primary language.
Keywords: Communication barriers; Critical care; Emergency service, hospital; Health services accessibility; Language; Length of stay; Telephone
1. INTRODUCTION
1.1. Background
Emergency departments (EDs) in the United States are increasingly crowded, with median waiting times of 2 to 5.5 hours in some regions. 1 Emergency physicians must prioritize patient needs and anticipate which patients require immediate transfer to the intensive care unit (ICU). A longer wait time spent in the ED before ICU admission is linked to poorer patient outcomes such as increased ICU length of stay (LOS) and increased mortality. 2 Disparities in ED wait times and time in the ICU have been observed with patients of minority racial/ethnic groups experiencing longer wait times compared with White patients. 3 , 4 , 5 Furthermore, patients with limited English proficiency (LEP) may be at greater risk for longer delays in transfer from the ED to the ICU because of communication barriers. 6 Professional translation services are largely underused in the ED setting. 7 Many clinicians rely on family members or uncertified bilingual medical staff to interpret during clinical care. 8 , 9 However, studies have shown that professional interpretation services are associated with better patient outcomes compared with relying on someone without formal training to interpret. 8 , 10 Although the effects of using professional versus non‐professional interpreters have been examined, 11 little is known regarding the effects of using an in‐person versus telephone interpreter.
1.2. Importance
Multiple studies have shown negative effects, such as unnecessary intubations or decreased satisfaction with care, when patients with LEP do not have access to professionally trained interpreters. 8 , 9 , 11 Professional interpretation services may be delivered through different modalities, including by telephone or in person. In‐person services offer the benefits of having face‐to‐face interaction between the patient, interpreter, and healthcare professional; however, having constant immediate availability of professionally trained interpretation staff in all needed languages may not be feasible at all facilities. 12 Telephone‐based interpretation offers the potential advantage of faster access to more languages but may be perceived as less personable and result in inferior communication compared with in‐person interpretation. 13 Little is known about the differences in wait times for English‐speaking patients versus patients with LEP who are admitted to the ICU from the ED and the potential effects of the mode of interpretation services. The effect of interpretation service modality on ED LOS before ICU admission is an important potentially modifiable factor that ED leadership can consider to improve patient experience and patient flow.
1.3. Goals of this investigation
Our objective was to describe the association between the availability of in‐person and phone interpretation services and ED LOS before ICU admission for patients with LEP compared with patients who spoke English as a primary language. We also compared mortality after ICU admission between patients with LEP and patients who spoke English as a primary language. We further examined the association between ED LOS and patient race/ethnicity.
2. METHODS
2.1. Study design, setting, and selection of participants
The Medical Information Mart for Intensive Care III (MIMIC‐III) Critical Care Database 14 from the Massachusetts Institute of Technology Lab for Computational Physiology was used for this project. This database contains information for >53,000 ICU admissions for adult patients (age >16 years) hospitalized from 2001 to 2012 at Beth Israel Deaconess Medical Center in Boston, MA. 14 From this database, the admissions table was used, specifically sections of the language (LANGUAGE), ED registration time (EDREGTIME), ED transfer to ICU time (EDOUTTIME), admission type (ADMISSION_TYPE), death (HOSPITAL_EXPIRE_FLAG), and ethnicity (ETHNICITY). Access and analysis of data were performed under Duke University Hospital institutional review board approval Pro00105982.
We included all patients who were admitted to the ICU from the ED. We excluded patients admitted to the ICU from any other location. We also excluded patients for whom ED LOS could not be calculated because of missing data.
1. The Bottom Line
In this study using a large ICU database (Medical Information Mart for Intensive Care III), patients requiring in‐person or telephone English translation experienced longer times in the emergency department (ED) before ICU transfer (327/309 minutes vs 292 minutes) and higher mortality rates (15%/11% vs 9%). Availability of interpretation services by phone was associated with longer ED times and higher mortality rates compared with in‐person services. Additional study is needed to elicit the reasons for these treatment disparities.
2.2. Measurements
The patient's primary language was ascertained from a language variable recorded during the ED encounter. Language was grouped into the following 3 categories: English, other languages, and unknown (when there was no entry in the language data field). For primary languages other than English, physicians who worked at the medical center during the collection of MIMIC‐III data were consulted to determine whether interpretation services for each language were available in person or by telephone only. Patient race/ethnicity was categorized into the following groups: Asian, Black/African, Hispanic or Latino, other, unknown/not specified. Diagnosis is suspected to play an important role in ED LOS. As such, we evaluated the most common diagnoses for patients in each language group by selecting all diagnoses with ≥300 occurrences in the analysis sample.
Our primary outcome was ED LOS before ICU arrival. ED LOS was calculated as the difference between ED registration time and ICU arrival time. Our secondary outcome was patient mortality after ICU admission. This information was ascertained using the hospital expire flag, which indicated whether a patient died in the hospital after admission to the ICU.
2.3. Analysis
Descriptive statistics were calculated including frequencies and percentages for categorical variables and medians with interquartile ranges for continuous, non‐normally distributed variables. The distribution of ED LOS times was compared between language and interpretation service categories using a Kruskal‐Wallis test. If significance was found, pairwise comparisons were performed using a Wilcoxon rank sum test and a Benjamini‐Hochberg adjustment. A similar approach was undertaken to compare ED LOS between patient race/ethnicity groups. Mortality rates after ICU admission were compared between groups using a chi‐square test.
3. RESULTS
Of 55,976 ICU patients, 22,754 (41%) were directly admitted from the ED. We excluded 332 (1%) patients for missing ED LOS data, leaving 22,422 patient encounters in the analysis sample (Figure 1). A total of 11,427 (51%) encounters had English recorded as the patient's primary language. A language other than English was documented as the primary language for 2042 (9%) encounters. Language was not recorded for 8953 (40%) encounters. Among the 2042 encounters with patients with primary languages other than English documented, interpretation services were most often available in person (1278, 63%), and 764 (37%) of these encounters had documented primary languages for which only telephone interpretation services were available. Primary diagnoses were distributed similarly between language groups with differences not exceeding 3% for any diagnosis category (Table 1).
TABLE 1.
Top diagnoses by patient primary language or available interpretation services category
| Diagnoses within each language category | |||
|---|---|---|---|
| Diagnosis | English speaking, % (n) | In‐person interpretation, % (n) | Phone interpretation, % (n) |
| Pneumonia | 5 (577) | 6 (72) | 8 (61) |
| Sepsis | 3 (337) | 3 (37) | 5 (38) |
| Upper/lower gastrointestinal bleed | 4 (442) | 2 (42) | 4 (29) |
| Congestive heart failure | 3 (298) | 4 (47) | 3 (21) |
| Altered mental status | 3 (324) | 2 (29) | 3 (21) |
| Intracranial hemorrhage | 2 (280) | 2 (20) | 2 (15) |
| Abdominal pain | 2 (231) | 1 (17) | 2 (16) |
| Fever | 2 (236) | 1 (15) | 3 (25) |
| Fall | 2 (191) | 2 (20) | 2 (14) |
| Chest pain | 3 (292) | 3 (34) | 1 (8) |
Table 2 displays the median ED LOS stratified by language or available interpretation services modality. Median ED LOS was 292 minutes (interquartile range [IQR], 205–412) for encounters with English recorded as the patient's primary language. Encounters involving patient primary languages for which in‐person interpretation services were available had a median ED LOS of 309 minutes (IQR, 214–453). Median ED LOS for encounters involving languages for which only telephone interpretation services were available was 327 minutes (IQR, 225–463). Compared with patients with English as a primary language, the increase in ED LOS for patients with telephone‐only interpretation services available was statistically significant (P < 0.01). Similarly, the increase in ED LOS for patients with in‐person interpretation services available achieved statistical significance (P < 0.01).
TABLE 2.
Median emergency department length of stay by patient primary language or available interpretation services
| Language or interpretation services used | Emergency department length of stay in minutes, median (interquartile range) |
|---|---|
| English (n = 11,427) | 292 (205–412) |
| In person (n = 1278) | 309 (214–453) |
| Phone (n = 764) | 327 (225–463) |
| Unknown (n = 8953) | 322 (206–476) |
Overall, 14% (n = 3054) of included ICU patients in this study died. A larger proportion of patients primarily speaking languages with in‐person interpretation services available group died (11%, n = 141) compared with patients in the English as a primary language group (9%, n = 1074) (P < 0.01). Similarly, a larger proportion of patients primarily speaking languages with phone interpretation services available died (15%, n = 115) compared with the English as a primary language group (P < 0.01). In addition, a larger proportion of patients primarily speaking languages with phone interpretation services available died compared with the group with in‐person interpretation services available (P = 0.02). The greatest mortality rate was seen in the group for whom language was unknown or not recorded (19%, n = 1720; Figure 2).
FIGURE 2.
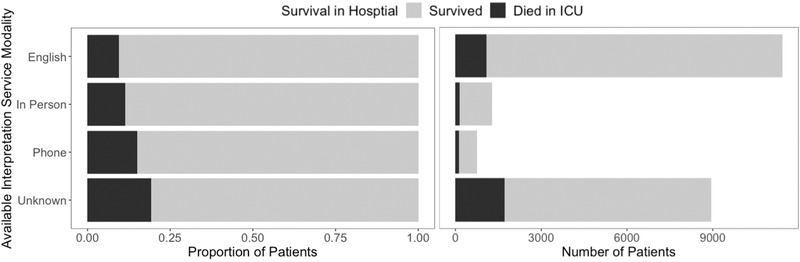
Mortality of ICU patients admitted from the emergency department expressed as percentage of total (left) and count (right) based on patient primary language or available interpretation service modality
FIGURE 1.
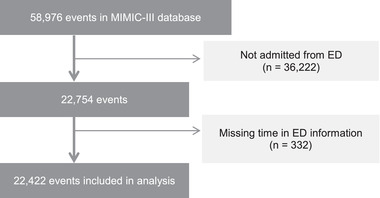
Inclusion of records in the analysis sample, ED, emergency department; MIMIC‐III, Medical Information Mart for Intensive Care III
Table 3 displays the median ED LOS stratified by patient race/ethnicity. Race/ethnicity was documented for 95% (n = 21,312) of patients overall. Of those with documented race/ethnicity, a total of 74% (n = 16,508) of patients were documented as White, 13% (n = 2855) were Black/African, 4% (n = 892) were Hispanic, 3% (n = 539) were Asian, and 2% (n = 518) belonged to other racial/ethnic groups. Black/African patients had a significantly longer median LOS compared with White patients (342 minutes vs 302 minutes; P < 0.05). Hispanic and Asian patients had a similar median LOS compared with White patients.
TABLE 3.
Median time in the emergency department based on patient race/ethnicity
| Patient race/ethnicity | Emergency department length of stay in minutes, median (interquartile range) |
|---|---|
| White (n = 16,508) | 302 (207–433) |
| Black/African (n = 2855) | 342 (241–483) |
| Hispanic (n = 892) | 294 (212–438) |
| Asian (n = 539) | 312 (213–465) |
| Other (n = 518) | 242 (152–387) |
3.1. Limitations
Limitations include the retrospective nature of the data set, which precludes inferences regarding causality; however, these findings indicate important differences that warrant further investigation. In addition, it was not possible to control for potentially important confounding variables, such as income, insurance, or how/when patients arrived at the ED, which could have had significant associations with care. This data set was obtained from a single large academic center in a large city and findings may not be directly generalizable to other settings. With regard to interpretation services, this study used whether in‐person or telephone interpretation services were available for a given language at the facility as a proxy for interpretation services used. Although patients may have had access to professional in‐person or telephone interpretation services, it was not possible to know whether these services were used or if another non‐professional interpreter provided assistance. Availability of in‐person interpretation services may indicate a more commonly spoken language in the area and as such an increased the likelihood of access to non‐professionally trained individuals who may have been able to provide interpretation. Plausibly, the effects reported in this study may not translate across other settings, especially those with only a few languages requiring interpretation services (in this hospital there were 19 languages when this data set was collected). Finally, there was a large number of records where patient language was unknown because the field was left blank. Interpreting this field is challenging as the reasons for leaving the field blank could vary. A blank field could indicate that the patient spoke English and no interpretation services were needed. However, a blank field may possibly indicate that the patient was unable to speak and thus language was not ascertained. The median LOS in the unknown language group was different from the English‐speaking group, suggesting differences that warrant keeping the groups separate for analysis.
4. DISCUSSION
In this large study of ICU patients admitted from the ED, we found disparities in the amount of time patients spent in the ED before ICU admission related to the patient's primary language and type of interpretation services available. Compared with patients who spoke English as a primary language, patients who primarily spoke other languages spent longer amounts of time in the ED before ICU admission, and a larger proportion of these patients died.
Patients with primary languages that had telephone interpretation services available spent even more time in the ED compared with those with primary languages for which in‐person interpretation services were available. Although we were unable to directly measure time to reach an interpreter, the increase in ED LOS is unlikely exclusively attributed to the time it takes for an in‐person interpreter to arrive at the patient's side, as patients with phone interpretation services available spent even more time in the ED than those with in‐person interpretation services available. It is hypothesized that time in the ED is increased for those who need interpretation relative to English speakers as the general process of accessing third‐party interpretation can add time to the visit length. This finding follows the results of a previous study of >2 million patients in Australia's Queensland Public hospitals, which found extended time in the ED for patients who did not speak English. 6
Underlying reasons for prolonged episodes of care in the patient population whose primary language was not English are likely multifactorial and can only be postulated based on this data set. Plausible factors include insurance status as well as other social determinants of health and potentially bias or discrimination. From the documented patient race/ethnicity information, the only group that had a significant difference in ED LOS, when compared with the most common race/ethnicity (White) in the data set was Black/African. This finding suggests that factors beyond language barriers may relate to longer time spent in the ED. Previous studies have found longer ICU LOS for Black versus non‐Black patients for a veteran population 4 and differences in ED time based on ethnicity. 3
The ICU mortality rate for patients whose primary language was not English was significantly higher than among patients with English documented as their primary language. Furthermore, the mortality rate for those who had phone interpretation available was higher than those who had in‐person interpretation available. The distinction between phone and in‐person interpretation service availability was significantly associated with mortality. Mortality was more common in this ICU data set relative to the general ED population. Specifically, in this study, there was a 14% mortality for patients who went from the ED to the ICU versus < 1% mortality for patients within 30 days of entry to the ED in a study by Baker et al. 15 Although many things affect mortality, the ability to communicate with a clinician effectively can be critical for better diagnosis and timely treatment. This communication breakdown could be reflected in the mortality results, where patients primarily speaking English had a lower mortality rate than those who primarily spoke other languages.
As a retrospective observational study, the signal of the importance of access to different forms of interpretation services found in this article warrants further investigation. Differences were found in key metrics including time in ED before ICU admission and death during hospital stay based on the type of interpretation service available for a patient's primary language. Future research should examine the interpretation services used rather than the availability of such services. In addition, data on time to access a professional interpreter and differences in medical interventions based on diagnosis would be critical to fully understand the various medical implications of need and usage of medical interpretation services.
In summary, this observational study involving a large sample of ICU patients from a single academic medical center examined the effects of primary language and type of interpretation services available on ED LOS and mortality. Patients for whom interpretation services were available spent a median of 17 to 35 minutes longer in the ED before entering the ICU compared with patients whose primary language was English. Interpretation services also were associated with increased mortality rates in the ICU compared with English‐speaking patients, with patients who had access to in‐person interpretation services doing better than those who only had access to phone interpretation. Further work is needed to further explore the underlying causes of these disparities.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Siobhan R. Oca and Daniel M. Buckland designed the study. Siobhan R. Oca conceived the study, analyzed the data, and drafted the article. Erin Leiman provided key information for data analysis. Erin Leiman, Angelo Navas, and Daniel M. Buckland contributed substantially to the article's revision. Siobhan R. Oca and Daniel M. Buckland take responsibility for the article as a whole.
Biography
Siobhan R. Oca, MTM, is a PhD candidate in medical robotics in the Department of Mechanical Engineering and Materials Science at Duke University in Durham, NC.

Oca SR, Navas A, Leiman E, Buckland DM. Effect of language interpretation modality on throughput and mortality for critical care patients: A retrospective observational study. JACEP Open. 2021;2:e12477. 10.1002/emp2.12477
Supervising Editor: Remle Crowe, PhD, NREMT.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
REFERENCES
- 1. Reese P. As ER wait times grow, more patients leave against medical advice. California Healthline. Published 2019. https://khn.org/news/as-er-wait-times-grow-more-patients-leave-against-medical-advice/. Accessed November 20, 2020.
- 2. Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP, DELAY‐ED study group . Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35(6):1477‐1483. [DOI] [PubMed] [Google Scholar]
- 3. Wu B, Banks P, Conwell D. Disparities in emergency department wait times for acute gastrointestinal illnesses: results from the National Hospital Ambulatory Medical Care Survey, 1997–2006. Am J Gastroenterol. 2009;104:1668‐1673. [DOI] [PubMed] [Google Scholar]
- 4. Sonnenfeld N, Pitts SR, Schappert SM, et al. Emergency department volume and racial and ethnic differences in waiting times in the United States. Med Care. 2012;50:335‐341. 10.1097/MLR.0b013e318245a53c. [DOI] [PubMed] [Google Scholar]
- 5. Pines JM, Russell Localio A, Hollander JE. Racial disparities in emergency department length of stay for admitted patients in the United States. Acad Emerg Med. 2009;16:403‐410. [DOI] [PubMed] [Google Scholar]
- 6. Mahmoud I, Hou XY, Chu K, Clark M. Language affects length of stay in emergency departments in Queensland public hospitals. World J Emerg Med. 2013;4(1):5‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Baker DW, Parker RM, Williams MV, et al. Use and effectiveness of interpreters in an emergency department. JAMA. 1996;275(10):783‐788. [PubMed] [Google Scholar]
- 8. Ramirez D, Engel KG, Tang TS. Language interpreter utilization in the emergency department setting: a clinical review. J Health Care Poor Underserved 2008;19(2):352‐362. [DOI] [PubMed] [Google Scholar]
- 9. Bard MR, Goettler CE, Schenarts PJ, et al. Language barrier leads to the unnecessary intubation of trauma patients. Am Surg. 2004;70(9):783‐786. [PubMed] [Google Scholar]
- 10. Sarver J, Baker DW. Effect of language barriers on follow‐up appointments after an emergency department visit. J Gen Intern Med. 2000;15(4):256‐264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bagchi AD, Dale S, Verbitsky‐Savitz N, et al. Examining effectiveness of medical interpreters in emergency departments for Spanish‐speaking patients with limited English proficiency: results of a randomized controlled trial. Ann Emerg Med. 2011;57(3):248‐256.e2564. [DOI] [PubMed] [Google Scholar]
- 12. Joseph C, Garruba M, Melder A. Patient satisfaction of telephone or video interpreter services compared with in‐person services: a systematic review. Aust Health Rev. 2017;42:168‐177. [DOI] [PubMed] [Google Scholar]
- 13. Locatis C, Williamson D, Gould‐Kabler C, et al. Comparing in‐person, video, and telephonic medical interpretation. J Gen Intern Med. 2010;25(4):345‐350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Johnson AEW, Pollard T, Shen L, et al. MIMIC‐III, a freely accessible critical care database. Scientific Data 2016;3:160035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Baker M, Clancy M. Can mortality rates for patients who die within the emergency department, within 30 days of discharge from the emergency department, or within 30 days of admission from the emergency department be easily measured? Emerg Med J. 2006;23(8):601‐603. [DOI] [PMC free article] [PubMed] [Google Scholar]


