Abstract
IgG4 aortitis is a recently recognized entity that can have clinical and imaging features that mimic acute aortic syndrome. Therefore, it is imperative for radiologists to be aware of how to potentially differentiate the two. Although this entity has been previously described via case reports and meta-analysis in the context of inflammatory abdominal aortic aneurysm, very few cases of ascending aortic involvement have been reported. In this case report, we present a case of a 60-year-old female transferred from another facility for an initial diagnosis of intramural hematoma of the ascending aorta and later found to have IgG4 aortitis post aortic root repair. This is a histologically confirmed case of multi-segmented IgG4 aortitis with rare involvement of both ascending and infra-renal aorta. We will briefly discuss the pathophysiology of IgG4 aortitis, along with review of literature.
Keywords: Aortitis, IgG4, intramural hematoma, vasculitis
CASE REPORT
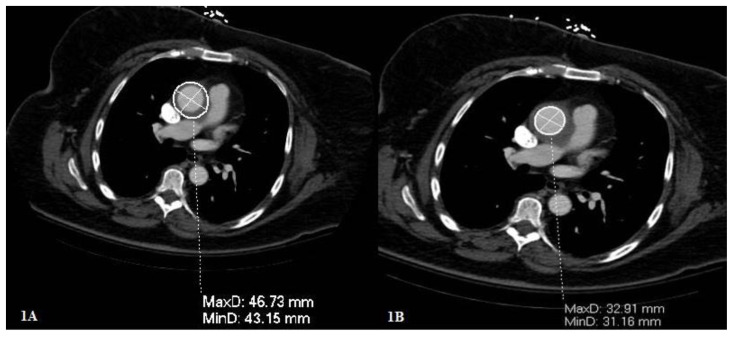
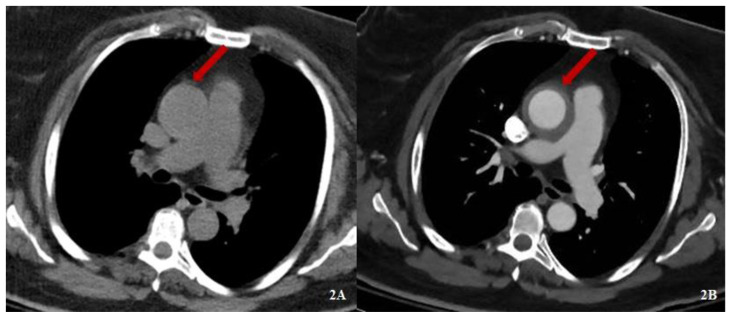
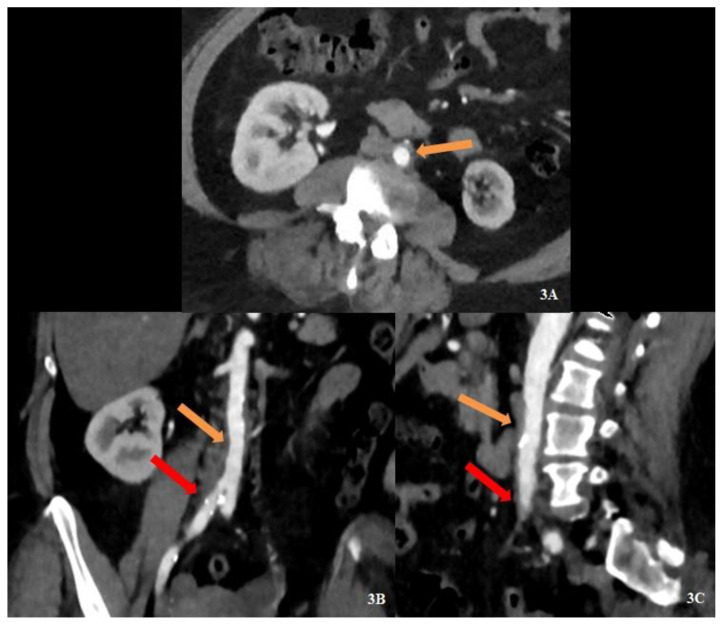
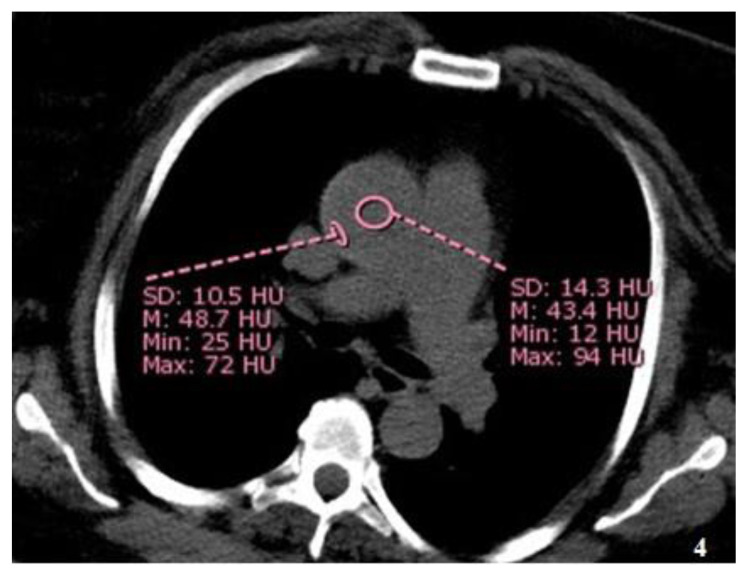
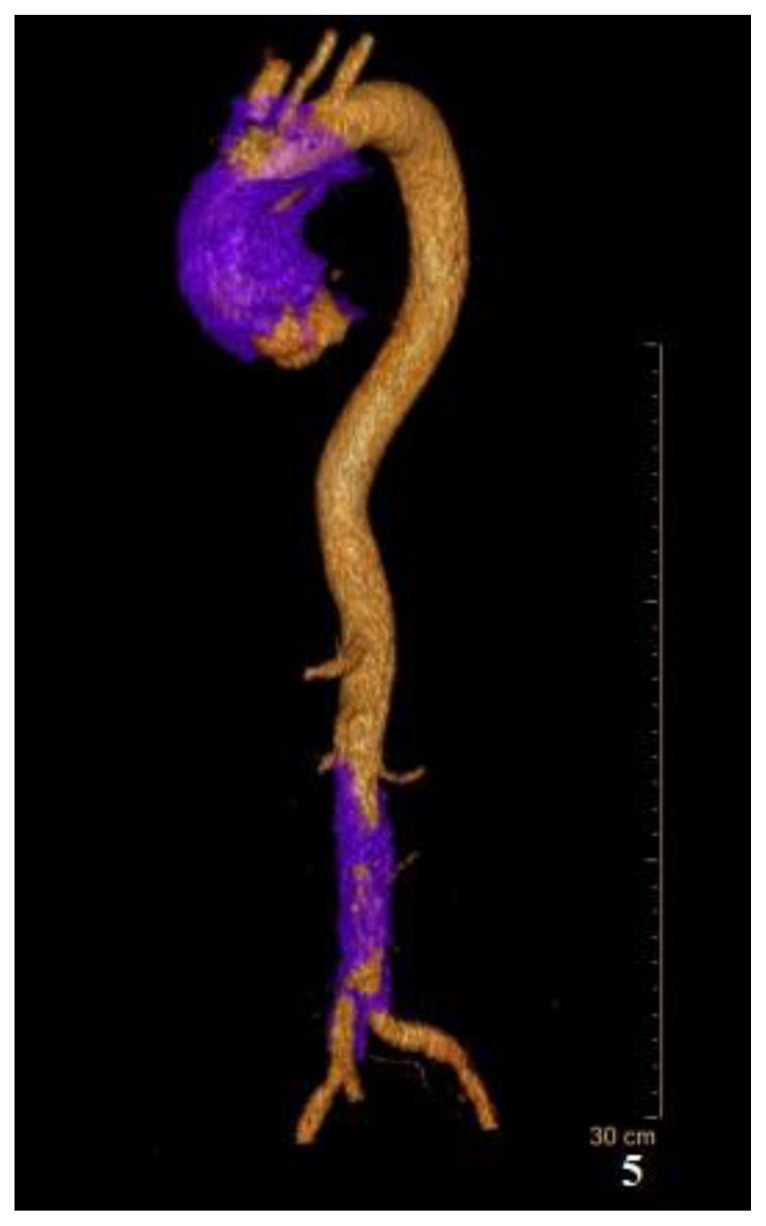
A 60-year-old female was transferred from another facility for tertiary care with a diagnosis of intramural hematoma involving the ascending aorta. Her past medical history was significant for hypertension, hyperlipidemia, type II diabetes mellitus, hypothyroidism, obesity and history of deep venous thrombosis on Eliquis. Upon admission to our facility, the patient had stable vital signs with chief complaint of shortness of breath, cough, and congestion. She underwent an emergent computed tomography angiogram (CTA) of the thorax, abdomen and pelvis which demonstrated an ectatic ascending aorta measuring 4.7 cm (Fig. 1A), with the inner lumen measuring 3.3 cm (Fig. 1B). In addition, the non-contrast CT thorax (Fig. 2A) and the post contrast CTA thorax (Fig. 2B) demonstrated concentric wall thickening of the ascending aorta with adjacent fat stranding. There was an additional area of involvement of the infrarenal aorta and proximal right common iliac artery with similar imaging characteristics as the ascending aorta (Fig. 3A–C). No crescentic hyperdensity was seen in the involved aortic segment on non-contrast images (Fig. 4). A post processed 3D reconstruction of the aorta demonstrates soft tissue thickening surrounding the ascending aorta and infrarenal aorta (Fig. 5).
Figure 1. 60-year-old female with IgG4 aortitis.
FINDINGS: The axial CTA Thorax demonstrates ectatic ascending aortic measuring 4.7cm (1A) although the inner lumen was within normal limits measuring 3.3 cm (1B).
TECHNIQUE: Helical axial angiographic images via Philips IQon Spectral CT of the thorax was obtained after uneventful administration of 100mL of Omnipaque 350 injected at 4.5cc/sec; mAs 308; kV 120; 2mm slice thickness.
Figure 2. 60-year-old female with IgG4 aortitis.
FINDINGS: Axial pre-contrast CT Thorax (2A) and axial post-contrast CTA Thorax (2B) through the same level of the ascending aorta demonstrates circumferential soft tissue thickening with subtle adjacent fat stranding (red arrow).
TECHNIQUE: Helical axial angiographic images via Philips IQon Spectral CT of the thorax was obtained before and after uneventful administration of 100mL of Omnipaque 350 injected at 4.5cc/sec. Axial pre-contrast image - mAs 181; kV 120; 2mm slice thickness. Axial post-contrast image - mAs 308; kV 120; 2mm slice thickness.
Figure 3. 60-year-old female with IgG4 aortitis.
FINDINGS: The axial (3A), coronal (3B) and sagittal (3C) CTA abdomen and pelvis demonstrates soft tissue density (orange block arrows - 3A, 3B and 3C) surrounding the infra-renal aorta. There is involvement of the proximal right common iliac artery (red block arrow - 3B and 3C).
TECHNIQUE: Helical axial angiographic images via Philips IQon Spectral CT of the abdomen and pelvis was obtained after uneventful administration of 100mL of Omnipaque 350 injected at 4.5cc/sec; mAs 308; kV 120; 2mm slice thickness.
Figure 4. 60-year-old female with IgG4 aortitis.
FINDINGS: Axial non-contrast CT thorax demonstrates similar Hounsfield units within the aortic lumen and along the periphery, in the region of the thickened aortic wall.
TECHNIQUE: Helical nonenhanced axial image via Philips IQon Spectral CT of the thorax was obtained; mAs 181; kV 120; 2mm slice thickness.
Figure 5. 60-year-old female with IgG4 Aortitis.
FINDINGS: The reconstruction demonstrates soft tissue thickening (purple) surrounding the aortic root and the infra-renal aorta.
TECHNIQUE: Volumetric reconstruction of the aorta utilizing Philips Intellispace portal - AVA software was used to postprocess the contrast enhanced aorta.
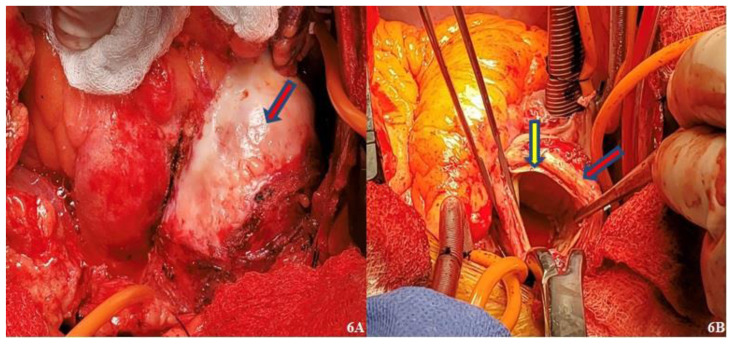
A cardiac catheterization did not reveal obstructive coronary artery disease. Due to her acute presentation and concern for rupture of the ascending aortic aneurysm, patient underwent median sternotomy for repair of the ascending aorta utilizing a hemiarch with Hemashield graft. Intraoperatively, the aortic root demonstrated concentric wall thickening with dense white fibrosis and adhesions (Fig. 6A–B). No intramural hematoma was seen.
Figure 6. 60-year-old female with IgG4 aortitis.
FINDINGS: Concentric thickening and dense white fibrosis of the aortic arch (red block arrow with blue outline - 6A and 6B). The intima was preserved (yellow block arrow with blue outline - 6B) without evidence of an intramural hematoma.
TECHNIQUE: Intraoperative photographs of the aortic arch.
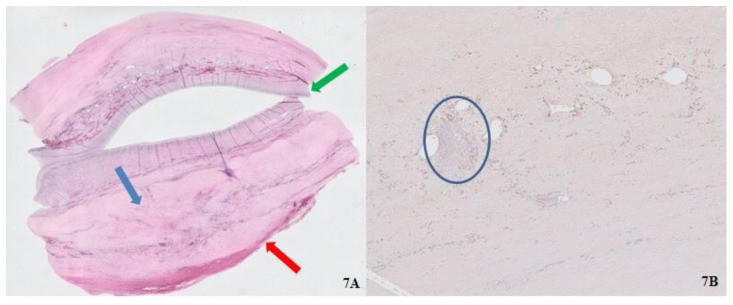
Patient was monitored for 5 days post-operatively and the hospital course was otherwise uneventful. A repeat CTA thorax, abdomen and pelvis revealed expected postoperative changes and the patient was later discharged for outpatient follow-up. The biopsy results of the ascending aorta later returned as Immunoglobulin G4 (IgG4) aortitis (Fig. 7A–B). Patient’s lab work at the time of admission indicated normal serum IgG4 level of 0.3% (normal range 0.0–0.5%), and erythrocyte sedimentation rate of 13 mm/Hr (normal range 0–30). There was mild elevation of C-reactive protein of 1.50 mg/dL (normal range 0.00–0.50).
Figure 7. 60-year-old female with IgG4 Aortitis.
FINDINGS: Low power field (7A) transversely cut surface of the aorta demonstrates circumferentially thickened adventitia (red block arrow) with fibrotic media (blue block arrow), and preserved intima (green block arrow). High power field (7B) image of the adventitia demonstrates fibrosis and lymphoplasmacytic infiltration surrounding the vasa vasorum (blue circle).
TECHNIQUE: Immunostains for IgG and IgG4.
DISCUSSION
Etiology & Demographics
IgG4-related disease is a systemic condition that can have nonsynchronous or simultaneous involvement of multiple organs. IgG4-related sclerosing disease (IgG4-RSD) is a well described diagnosis involving autoimmune pancreatitis, in addition to involvement of salivary gland, thyroid, mediastinum, heart, kidneys and the retroperitoneum [1,2]. Few studies and case reports have described IgG4 related aortitis of the abdominal aorta, and even fewer case reports have been published on thoracic aortitis. IgG4 aortitis was first defined by Kasashima and colleagues in 2008 as a primary suspect in inflammatory abdominal aortic aneurysm (IAAA) [3].
Clinical & Imaging findings
Although the exact pathophysiology of IgG4 aortitis remains to be elucidated, Kasashima and colleagues (2018) proposed an inflammatory pathway that activates the T helper cells resulting in release of various cytokines, plasma cell infiltration and fibrosis [4]. The ‘outside-in’ theory suggests that the activated T-helper cells attract IgG4-positive B lymphocytes to the adventitia, which later differentiate into plasma cells [5]. The plasma cell infiltration of the adventitia can result in destruction of aortic wall elasticity and remodeling of the periadventitia via aggregation of cytokines and growth factors, eventually leading to a weakened wall that can predispose to aneurysm [4–6]. Risk of aneurysm increases when the inflammation extends to involve the media and lamellar elastic fibers [6,7].
On the gross specimen, the aorta demonstrates a bluish or whitish tinge superficially and is firm to palpation, which was seen in our patient upon initial incision (Fig. 6A) [8,9]. Histologically there is lymphoplasmacytic infiltration with storiform fibrosis as a dominant component, obliterative phlebitis, IgG4/IgG positive plasma cell ratio ≥ 40% and IgG4 positive plasma cell count >10/hpf (high power field) as seen on immunohistochemistry [1–10]. On imaging, CTA demonstrates soft tissue thickening of the outer aortic wall, which can occasionally be mistaken for acute aortic syndrome such as intramural hematoma due to its overlapping appearance [1,4,10].
Diagnostic criteria suggested based on findings described for IAAA by Kasashima and colleagues (2018) may be extended to diagnose IgG4 aortitis due to similar pathophysiology. The criteria include (a) - hypertrophic lesion of the arterial wall on imaging findings, (b) - increased serum IgG4 (>135mg/dL) and (c) - histopathological findings as described earlier. It is a definitive diagnosis if all three criteria are present. It is semi-diagnostic if (a) and (c) are present and suspected if (a) and (b) are present [4].
Difficulty in performing a biopsy and obtaining a pathology specimen of the aorta due to its location can make the diagnosis of IgG4 aortitis challenging. However, the diagnosis can be made in the presence of multifocal or multi-organ involvement and elevated IgG4-levels, which is >90% sensitive [4]. Based on our case, radiological findings such as aortic wall thickening with fat stranding and multifocal involvement may be helpful as a diagnostic feature. Aguirre and colleagues (2015) suggested involvement of other organs, elevated inflammatory markers and PET/CT may be helpful in diagnosis [6].
Differential Diagnosis
The presentation and involvement of the ascending aorta can result in a diagnostic dilemma especially in the setting of nonspecific patient presentation. Differential diagnosis of circumferential aortic wall thickening includes intramural hematoma, non-infectious aortitis such as vasculitides, and infectious aortitis [1,10,11]. Intramural hematoma can present as circumferential or crescentic wall thickening, which may or may not be hyperdense on non-contrast CT depending on acuity [12]. Additionally, patients with intramural hematoma present with severe acute chest pain that may or may not radiate to the back, changes in blood pressure in the upper extremities, or acute aortic regurgitation [13].
On the other hand, lab values rather than patient presentation allow for an accurate diagnosis in cases of infectious or non-infectious aortitis [11]. Patients with vasculitis and infectious aortitis have abnormal laboratory findings such as elevated acute inflammatory or infectious markers, ESR, CRP and white blood cell (WBC) along with nonspecific systemic manifestations such as fever, and weakness [14]. Infection of the aorta is rare and can form in pre-existing atherosclerotic plaque, which is the most common cause of aortic wall thickening [11].
Treatment & Prognosis
Surgical versus medical management of IgG4 aortitis currently remains controversial due to lack of randomized clinical trials [10]. Several studies have stated that medical management with steroid therapy can improve aortitis both clinically and radiographically [1–4,6,10]. However, risk of persistent luminal dilatation and aneurysmal rupture remains high in a patient undergoing high-dose glucocorticoid therapy alone [2]. Other proposed treatments include immunosuppressive therapy with methotrexate and B-cell depletion therapy with Rituximab [2,6,10]. Surgical management with aortic graft repair has shown improved postoperative course. Some patients have undergone stent repair mitigating the need for adhesiolysis [4].
Conclusion
Presence of multifocal disease and low-density concentric thickening of the aortic wall on non-contrast CT with associated fat stranding can be utilized as an ancillary finding to diagnose aortitis. It is imperative for a radiologist to recognize the signs of IgG4 aortitis and raise the possibility of inflammatory aortitis rather than an acute aortic syndrome. This will allow for appropriate work-up and management of aortitis.
TEACHING POINT
Imaging diagnosis of IgG4 aortitis can be challenging, especially in the absence of fitting clinical presentation or diagnosis, as in our patient who presented with normal IgG4 levels. However, it is the role of a radiologist to recognize the imaging characteristics of vasculitis/aortitis and to raise the possibility of an alternative diagnosis to expediate appropriate clinical management.
Table 1.
Summary table of IgG4 Aortitis.
| Etiology | Unknown |
| Incidence |
|
| Gender Ratio |
|
| Age predilection |
|
| Risk factors |
|
| Treatment |
|
| Prognosis |
|
| Findings on imaging |
|
Table 2.
Differential diagnosis table for IgG4 Aortitis.
| Differential diagnosis | Transesophageal echocardiogram (TEE) | Computed Tomography (CT) | Magnetic Resonance Imaging (MRI) | Fluorodeoxyglucose-Positron Emission Tomography (FDG-PET) |
|---|---|---|---|---|
| Atherosclerosis |
|
|
|
|
| Intramural hematoma (IMH) |
|
|
|
|
| Vasculitis or Aortitis |
|
|
|
|
| Infection |
|
|
|
|
ACKNOWLEDGMENTS
John Fallon, MD. Department of Pathology, Westchester Medical Center, Valhalla, NY
ABBREVIATIONS
- CRP
C-reactive protein
- CT
Computed Tomography
- CTA
Computed tomography angiogram
- ESR
erythrocyte sedimentation rate
- FDG-PET
Fluorodeoxyglucose-positron emission tomography
- IAAA
Inflammatory abdominal aortic aneurysm
- IgG4
Immunoglobulin G4
- IgG4-RSD
Immunoglobulin G4-Related sclerosing disease
- IMH
Intramural hematoma
- MRA
Magnetic Resonance Angiography
- MRI
Magnetic Resonance Imaging
- PET/CT
Positron emission tomography/Computed Tomography
- TEE
Transesophageal echocardiogram
- WBC
White blood cell
REFERENCES
- 1.Byeon K, Han J, Kim JS, et al. Immunoglobulin G4-related periaortitis mimicking an intramural hematoma. Ann Thorac Surg. 2011;92(4):1506–1508. doi: 10.1016/j.athoracsur.2011.03.141. [DOI] [PubMed] [Google Scholar]
- 2.Luís M, Brites L, Fernandes B, et al. The many faces of IgG4-related disease: report of a case with inaugural recurrent aortic aneurism ruptures and literature review. Rheumatol Int. 2018;38(8):1565–1570. doi: 10.1007/s00296-018-4046-9. [DOI] [PubMed] [Google Scholar]
- 3.Kasashima S, Zen Y, Kawashima A, Endo M, Matsumoto Y, Kasashima F. A new clinicopathological entity of IgG4-related inflammatory abdominal aortic aneurysm. J Vasc Surg. 2009;49(5):1264–1271. doi: 10.1016/j.jvs.2008.11.072. [DOI] [PubMed] [Google Scholar]
- 4.Kasashima F, Kawakami K, Matsumoto Y, Endo M, Kasashima S, Kawashima A. IgG4-Related Arterial Disease. Ann Vasc Dis. 2018;11(1):72–77. doi: 10.3400/avd.ra.18-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kajander H, Paavonen T, Valo T, Tarkka M, Mennander AA. Immunoglobulin G4-positive ascending thoracic aortitis may be prone to dissection. J Thorac Cardiovasc Surg. 2013;146(6):1449–1455. doi: 10.1016/j.jtcvs.2012.09.039. [DOI] [PubMed] [Google Scholar]
- 6.Aguirre V, Connolly C, Stuklis R. IgG4-Aortopathy: An Underappreciated Cause of Non-Infectious Thoracic Aortitis. Hear Lung Circ. 2017;26(11):e79–e81. doi: 10.1016/j.hlc.2017.03.156. [DOI] [PubMed] [Google Scholar]
- 7.Xu L, Heath J, Burke A. Ascending aortitis: A clinicopathological study of 21 cases in a series of 300 aortic repairs. Pathology. 2014;46(4):296–305. doi: 10.1097/PAT.0000000000000096. [DOI] [PubMed] [Google Scholar]
- 8.Moore DW, Hansen NJ, DiMaio DJ, Harrison WL. The great imitator: IgG4 periaortitis masquerading as an acute aortic syndrome on computed tomographic angiography. Radiol Case Reports. 2016;11(4):287–291. doi: 10.1016/j.radcr.2016.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Colombier S, Ruchat P, Gronchi F, Prêtre R, Niclauss L. Surgical procedure in immunoglobulin G4-related ascending aortitis? Ann Thorac Surg. 2014;97(4):3–5. doi: 10.1016/j.athoracsur.2013.11.074. [DOI] [PubMed] [Google Scholar]
- 10.Guler GB. IgG4-related aortitis mimicking intramural hematoma. Anatol J Cardiol. 2016:728–729. doi: 10.14744/AnatolJCardiol.2016.7185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Restrepo CS, Ocazionez D, Suri R, Vargas D. Aortitis: Imaging Spectrum of the Infectious and Inflammatory Conditions of the Aorta. RadioGraphics. 2011;31:435–451. doi: 10.1148/rg.312105069. [DOI] [PubMed] [Google Scholar]
- 12.Gutschow SE, Walker CM, Martínez-Jiménez S, Rosado-de-Christenson ML, Stowell J, Kunin JR. Emerging concepts in intramural hematoma imaging. Radiographics. 2016;36(3):660–674. doi: 10.1148/rg.2016150094. [DOI] [PubMed] [Google Scholar]
- 13.Alomari IB, Hamirani YS, Madera G, Tabe C, Akhtar N, Raizada V. Aortic intramural hematoma and its complications. Circulation. 2014;129(6):711–716. doi: 10.1161/CIRCULATIONAHA.113.001809. [DOI] [PubMed] [Google Scholar]
- 14.Okazaki T, Shinagawa S, Mikage H. Vasculitis syndrome-diagnosis and therapy. J Gen Fam Med. 2017;18(2):72–78. doi: 10.1002/jgf2.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tunick PA, Krinsky GA, Lee VS, Kronzon I. Diagnostic imaging of thoracic aortic atherosclerosis. American Journal of Roentgenology. 2000;174(4):1119–1125. doi: 10.2214/ajr.174.4.1741119. [DOI] [PubMed] [Google Scholar]