ABSTRACT
Background: Approximately 10% of Syrian refugees currently reside in camp settings, which can impose additional post-migration stressors. With elevated rates of psychological distress and few available resources, task-shifting psychosocial programmes are necessary to provide adequate care. One such programme developed by the World Health Organization (WHO) is Group Problem Management Plus (GroupPM+).
Objective: This study aimed to test the safety and acceptability of GroupPM+ in a refugee camp and to identify areas for adaptation in preparation for a definitive RCT.
Method: A feasibility randomized controlled trial (RCT) was conducted in Azraq refugee camp in Jordan. Inclusion criteria were: (1) Syrian adults aged ≥18 years, (2) parent of a child aged 10–16 years, (3) experiencing psychological distress as defined by a score of ≥16 on the Kessler Distress Scale, and (4) ≥17 on the WHO Disability Assessment Schedule 2.0. Following baseline assessments, participants were randomized to receive GroupPM+ or enhanced treatment-as-usual. Post-assessments were conducted one week following the last GroupPM+ session. Primary outcomes were feasibility and acceptance of GroupPM+; symptoms of anxiety, depression, PTSD, prodromal psychosis, grief, and child’s self-reported psychological distress were also assessed.
Results: Of the 207 persons screened, 64 (31%) screened positive for psychological distress. Of the 35 randomized into the GroupPM+ intervention, 24 (69%) completed the intervention. No adverse events were reported throughout the trial. Children whose parents received GroupPM+ had greater reductions in internalizing and externalizing symptoms at posttreatment. 55 (86%) participants completed the post-assessment follow-up. These results demonstrate both the feasibility of conducting the trial in a camp and acceptance of the GroupPM+ intervention by Syrian refugees.
Conclusions: Following the feasibility trial, both the implementation procedures and intervention were safe and culturally acceptable. The results support the readiness for a definitive RCT to determine the effectiveness and cost-effectiveness of the intervention in camp settings.
KEYWORDS: Psychological intervention, refugee camp, trial, mental health, psychosocial support
HIGHLIGHTS
Feasibility trial of GroupPM+ in a Syrian refugee camp in Jordan.
64 participants randomized; safety and cultural acceptance was observed.
Positive results support the readiness for a definitive RCT to test effectiveness and cost-effectiveness.
Short abstract
Antecedentes: Aproximadamente el 10% de refugiados sirios reside actualmente en campos de refugiados, lo que puede imponer estresores adicionales después de la migración. Con tasas elevadas de angustia psicológica y pocos recursos disponibles, los programas psicosociales de rotación de tareas son necesarios para brindar un cuidado adecuado. Uno de estos programas, desarrollado por la Organización Mundial de la Salud (OMS), es el Programa Grupal para el Manejo de Problemas Plus (‘Group Problem Management Plus’, o GroupPM+).
Objetivos: Este estudio tuvo como objetivo el probar la seguridad y la aceptabilidad del GroupPM+ en un campo de refugiados e identificar las áreas de adaptación en preparación para un ensayo clínico controlado y aleatorizado (ECA).
Métodos: Se llevó a cabo un ensayo clínico controlado y aleatorizado (ECA) de viabilidad en el campo de refugiados de Azraq en Jordania. Los criterios de inclusión fueron (1) ser un adulto sirios con una edad ≥ 18 años, (2) ser padre de un niño de 10 a 16 años, (3) experimentar angustia psicológica, definida mediante un puntaje ≥ 16 en la Escala de Malestar Psicológico de Kessler, y (4) un puntaje ≥ 17 en el Cuestionario para la Evaluación de la Discapacidad 2.0 de la OMS. Después de las evaluaciones iniciales, los participantes fueron distribuidos aleatoriamente para recibir la intervención mediante el GroupPM+ o para recibir el tratamiento usual optimizado. Las evaluaciones posteriores fueron conducidas una semana después de la última sesión del GroupPM+. Los resultados principales fueron la viabilidad y la aceptación del GroupPM+; los síntomas de ansiedad, de depresión, del trastorno de estrés postraumático (TEPT), la psicosis prodrómica, el duelo, y también se evaluó el auto-reporte de la angustia psicológica por parte del niño.
Resultados: De las 207 personas evaluadas, 64 (31%) dieron positivo en presentar angustia psicológica. De las 35 personas incluidas de manera aleatoria en el grupo de intervención mediante el GroupPM+, 24 (69%) completaron la intervención. No se reportaron eventos adversos durante el ensayo clínico. Los niños cuyos padres recibieron la intervención mediante el GroupPM+ tuvieron una mayor reducción en los síntomas internalizantes y externalizantes después del tratamiento. 55 (86%) participantes completaron el seguimiento posterior a la evaluación. Estos resultados demuestran tanto la viabilidad de conducir el ensayo clínico en un campo de refugiados, como la aceptación de la intervención mediante el GroupPM+ por parte de los refugiados sirios.
Conclusiones: De acuerdo con el ensayo de viabilidad, tanto los procedimientos de implementación como la intervención fueron seguros y culturalmente aceptables. Los resultados apoyan la preparación para un ECA definitivo para determinar la efectividad y costo-efectividad de la intervención en los campos de refugiados.
PALABRAS CLAVE: Intervención psicológica, campo de refugiados, ensayo, salud mental, soporte psicosocial
Short abstract
背景: 目前约有10%的叙利亚难民居住在营地中, 这可能是额外的移民后带应激源。随着心理困扰的比率上升及可用资源很少, 有必要进行切换任务的心理社会方案来提供合适的护理。一个由世界卫生组织 (WHO) 开发的此类计划是‘团体问题管理增强版’ (GroupPM +) 。
目的: 本研究旨在考查GroupPM +在难民营中的安全性和接受性, 并确定适应性区域, 以准备确定的RCT。
方法: 在约旦的阿兹拉格难民营进行了可行性随机对照试验 (RCT) 。纳入标准为: (1) 叙利亚≥18岁的成年人; (2) 有10-16岁孩子的父母; (3) 体验到心理困扰, 在凯斯勒困扰量表上得分≥16; 以及 (4) 在WHO残疾评估表2.0中得分≥17。在进行基线评估后, 将参与者随机分组为接受GroupPM +或常规治疗。上一次GroupPM +疗程之后的一周进行了评估后。主要结果是GroupPM +的可行性和接受性; 还评估了焦虑, 抑郁, PTSD, 前驱性精神病, 哀伤和孩子自我报告的心理困扰症状。
结果: 筛查的207人中, 有64人 (占31%) 的心理困扰筛查为阳性。在35名随机分到GroupPM +干预措施组的患者中, 有24名 (69%) 完成了干预措施。整个试验中均未报告不良事件。父母接受GroupPM +组的孩子在治疗后内化和外化症状的减轻程度更大。 55名 (86%) 参与者完成了评估后的随访。这些结果证明了在营地进行试验的可行性以及叙利亚难民对GroupPM +干预的接受程度。
结论: 在可行性试验之后, 实施程序和干预措施都是安全的, 并且在文化上是可接受的。结果支持确定性RCT的准备程度, 以确定在营地环境中干预措施的有效性和成本效益。 。
关键词: 心理干预, 难民营, 试验, 心理健康, 心理社会支持
1. Introduction
As a result of the prolonged crisis stemming from the 2011 civil war, Syrians have become the most globally displaced nationality. There are currently 13.2 million displaced Syrians (6.6 million internally displaced, 6.6 million registered refugees) (UNHCR, 2020a). The number of unregistered Syrian refugees would likely inflate this figure drastically, although estimates are difficult to accurately establish. Approximately 83% of refugees have fled to countries bordering Syria, namely Turkey, Lebanon, Jordan, and Iraq, with almost 300,000 currently residing in camp settings in these countries (UNHCR, 2020b). Persons who have fled from their homeland may experience a range of potentially traumatic events, including war, bereavement, torture, loss of property, forced social separation, and major stressors whilst fleeing to another country (Silove, 1999). Furthermore, for those residing in camps, there are a number of further unique post-migration stressors including restricted movement, limited communication means, scarcity of resources and limited employment opportunities (Riley, Varner, Ventevogel, Taimur Hasan, & Welton-Mitchell, 2017). Unsurprisingly, there is evidence that people exposed to these conditions are at risk of higher rates of common mental disorders, including anxiety and depression (Charlson et al., 2019). Published reports have estimated that the levels of psychological distress and mental disorders are significantly higher in Syrian refugees relative to global estimates (Hassan, Ventevogel, Jefee-Bahloul, Barkil-Oteo, & Kirmayer, 2016).
Due to the large number of refugees fleeing to neighbouring and other developing nations, the ability to access appropriate treatment is limited and there exists a treatment gap for Syrians suffering from psychological distress (Hendrickx et al., 2020). Countries hosting refugees are often characterized by developing economies, fractured healthcare systems and a lack of specialized staff (World Health Organization, 2013). Low-intensity psychological interventions have been developed to increase access to appropriate mental health care without burdening healthcare systems (Morina, Malek, Nickerson, & Bryant, 2017). A number of these interventions have been shown to be effective in these populations, but not all programmes have been scaled up appropriately (see review (Barbui et al., 2020)). Common barriers preventing widespread implementation include the intervention being too lengthy, expensive to implement and sustain, reliance on skilled professionals, and a focus on single disorders (Eaton et al., 2011).
To overcome the barriers of resource-poor health systems, task-shifting approaches have been developed in which non-specialized staff are trained to provide psychosocial support for people suffering from mild to moderate levels of psychological distress (Barbui et al., 2020; Eaton et al., 2011). A large meta-analysis of programmes that have used a task shifting approach demonstrated that these programmes have a moderate effect in reducing psychological distress (Barbui et al., 2020; Daisy et al., 2017). The World Health Organization (WHO) has developed a number of low-intensity psychological interventions that are administrable by non-specialized staff. The primary principles of these programmes are that they are transdiagnostic (i.e. aimed towards relieving distress occurring across a range of common mental disorders), have a restricted number of sessions, and are deliverable by lay-health workers. One such programme is Problem Management Plus (PM+) which aims to provide a brief transdiagnostic programme to address common mental disorders such as anxiety and depression (Dawson et al., 2015). PM+ has been developed in various formats and can be implemented as an individual or group-based intervention. Randomized controlled trials (RCTs) with a variety of vulnerable populations in Pakistan and Kenya indicate the capacity of PM+ to reduce common mental disorders in both individual (Bryant et al., 2017; Rahman et al., 2016) and group (Rahman et al., 2019) formats.
To date, all trials of PM+ have been conducted in community settings, and there is therefore a gap in our knowledge about the utility of PM+ for refugees hosted or in detention in refugee camps. Considering the specific stressors and restricted opportunities for refugees in this environment, it is important to test PM+ in a camp setting. Accordingly, the current study aims to test feasibility of conducting an RCT to test the efficacy of the group-based PM+ (GroupPM+). Specifically, the aims of this feasibility trial were to test the trial procedures, and safety and acceptability of GroupPM+ in a camp-setting and to identify areas for adaptation in preparation for a definitive RCT.
More than half of refugees are children who are at increased risk for the development of mental disorders (Bronstein & Montgomery, 2011; Charlson et al., 2019). Previous research has shown that parental mental health is a major predictor of children’s mental health, and this is also observed in refugee populations (Bryant et al., 2018). In line with this, a secondary aim was to test the feasibility of assessing the participants’ children for levels of psychological distress and to determine whether parental involvement in GroupPM+ would have a positive effect on their wellbeing.
2. Methods
2.1. Setting
There are currently more than 650,000 Syrians formally registered refugees in Jordan; however, total estimates indicate that more than 1.4 million Syrians actually reside in Jordan (Jordan Ministry of Planning and International Cooperation, 2018; UNHCR, 2020c). There are three refugee camps in Jordan which are home to more than 125,000 Syrians; Azraq is the second largest camp located in the desert near the city of Azraq with a population of 36,657 Syrians (as of June, 2020) of which 61% are children (UNHCR, 2020d). Due to high levels of camp security, internet access is limited as is internal and external mobility. Additionally, there are finite employment opportunities. There are currently 8,660 caravans, housing up to a maximum of six family members, that are in use across four residential villages, two of which were used to recruit participants for this study. Study approval was obtained through the Ministry of Planning and International Cooperation in Jordan, and research ethics were approved by the University of New South Wales (UNSW) and the Institutional Review Board of the King Hussein Cancer Centre. The trial was prospectively registered on the Australia New Zealand Clinical Trials Registry (ACTRN12619000168156).
This study was conducted by UNSW in cooperation with the Jordan country office of International Medical Corps (IMC), an international non-governmental organization.
2.2. Participants
Door-to-door screening of consecutive caravans was conducted in January 2019, across two villages in Azraq camp by Arabic-speaking assessors trained by IMC Jordan. Potential participants were identified and invited to participate in the screening process if they met the following criteria: (1) Syrian refugee, (2) ≥18 years old, (3) had a child or dependent living in the household aged 10–16 years, and (4) scored ≥ 16 on the Kessler 10 distress scale (Kessler et al., 2002) (K10), and ≥ 17 on the WHO Disability Assessment Schedule (WHODAS 2.0) (Ustun, Kostanjesek, Chatterji, Rehm, & World Health Organization, 2010). To minimize contamination of the interventions, only one adult per caravan was invited to participate. The invitation was initially extended to the person answering the door and if declined, the offer was made to another adult living in the household. Following screening, participants were excluded for the following: (1) developmental, cognitive, or neurological impairments, (2) severe mental disorder (e.g. psychotic disorders, substance use disorders), or (3) imminent risk of suicide. Excluded participants were referred to specialized services.
No power calculations were conducted as this was a feasibility study; sample size for this study was based on sample sizes of prior PM+ feasibility trials (Dawson et al., 2016; Rahman et al., 2016). A sample of 60 participants was targeted based on two arms with approximately 30 participants per intervention. GroupPM+ was designed to be conducted in groups of 6–12 participants which would allow for four groups; two female groups (n ≈ 15) and two male groups (n ≈ 15). We were confident this sample size would provide enough information to inform a future definitive RCT.
2.3. Informed consent
Informed consent for entry into the study involved two steps: 1) informed consent to participate in the screening and 2) informed consent for taking part in the feasibility trial. Only participants who screened positive were invited to provide their consent to participate in the feasibility trial. Participants completed a written consent form and those who were illiterate provided witnessed oral consent, in line with recommendations from WHO (Bhutta, 2004). Additionally, caregivers were asked to provide assent from one of their children between the ages of 10 and 16 years. Children were then approached to obtain assent to complete the Paediatric Symptoms Checklist (PSC-35) (Jellinek et al., 1999) during the pre- and post-assessments; children’s assent was not a requirement for participation of their caregiver.
2.4. Procedure
Participants were identified through door-to-door screening. Camp villages are designed to include 12 caravans per park, with varying numbers of parks per block. Screening was conducted in two of the four residential villages which had 29 blocks. Families of up to 6 persons may reside in a single caravan. Assessors provided a brief explanation of the study and took consent from one adult per caravan. Following the consent procedures, assessors conducted the screening assessment which included collecting socio-demographic information, as well as the WHODAS 2.0 and K10. Additionally, assessors asked about suicidal ideation as outlined by the WHO assessment (World Health Organization, 2010) and took note of any observable behavioural, cognitive, or neurological impairment.
Within two days of completing the screening procedure, participants were provided with feedback. For those who screened negative, referral options were provided if they remained concerned. For those who screened positive and did not meet any of the exclusion criteria, consent was given to participate in the trial. Further, one of the participant’s children aged 10–16 years was invited to provide assent. Pre-assessment measures were then completed. Following pre-assessment, adults were randomized to receive either the GroupPM+ intervention or Enhanced Treatment as Usual (ETAU). Randomization was conducted on a 1:1 basis by an independent researcher from the University of New South Wales using computerized software for random number generation. Allocation concealment was ensured by keeping the treatment assignments in sequentially numbered, opaque, sealed envelopes. The slight imbalance of allocations to PM+ and ETAU reflects the likelihood of non-even numbers in each condition in a small sample size. Participants randomized into GroupPM+ were contacted and provided details about upcoming group sessions while those in ETAU were contacted to arrange a subsequent meeting. Participants were aware of treatment allocation due to the nature of the intervention. One week following the GroupPM+ intervention, post-assessments were completed by assessors who were blind to treatment condition. This occurred approximately 7 weeks after baseline assessments.
2.5. Measures
2.5.1. Feasibility and acceptability measures
Various indicators were collected to assess the feasibility of trial procedures and acceptability of the GroupPM+ intervention (Arain, Campbell, Cooper, & Lancaster, 2010). To assess safety of the trial and the intervention, we observed the number of adverse and serious adverse events. Adverse events were defined as undesirable experiences occurring during the study, regardless of relation to the intervention (e.g. expressions of suicidal ideation, domestic violence or family conflict). Serious adverse events were defined as suicide attempts, medical occurrences that were life threatening or resulted in death, or any form of child abuse. Feasibility of the trial procedures examined by observing recruitment and retention rates, as well as reviewing missing data of outcome measures. The acceptability of the intervention itself was inferred by percentage of participants completing GroupPM+. Completion of the intervention was defined as participants attending three or more sessions of the intervention.
Although not powered to detect differences between conditions, participants were assessed on key psychological measures planned for the definitive trial. Specifically, participants were assessed using pen and paper measures at screening, baseline, and post-intervention. Participants were provided with assessment packages and asked to complete their answers; assessors were present during the assessments to provide any help or clarity needed. At screening, the thoughts of suicide questionnaire was administered in an interview format due to the sensitive nature. For participants who were illiterate, assessments were administered in an interview format. All assessments were conducted in Arabic.
2.5.2. Screening
The WHODAS 2.0 assesses disability, encompassing six domains (cognition, mobility, self-care, getting along, life activities, and participation), and assesses difficulties people have across these domains during the last 30 days (Ustun et al., 2010). The 12-item Arabic version was used, and the recommended cut-off score of 17 adopted.
The Kessler Psychological Distress Scale (K10) is a questionnaire assessing general psychological distress (Kessler et al., 2002). It consists of ten items indexing anxiety and depression symptoms experienced during the past 30 days. Responses are scored on −5-point scales (1 = none of the time, 5 = all of the time), with higher scores indicating higher levels of distress. A cut-off score of 16 was used because it has been shown to be indicative of moderate levels of distress (Slade, Grove, & Burgess, 2011).
2.5.3. Primary outcome
The intended primary outcome of the definitive trial will be psychological distress. This was measured in the pilot study using the Arabic version of the Hopkins Symptom Checklist (HSCL-25) (Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, 1974; Selmo, Koch, Brand, Wagner, & Knaevelsrud, 2019). The HSCL-25 consists of 25 questions across anxiety and depression subscales. Responses are rated on a 4-point scale (1 = not at all, 4 = extremely), providing total scores of anxiety and depression.
2.5.4. Secondary outcomes
Posttraumatic stress disorder (PTSD) symptoms were measured using the PCL-5 (Arabic version) (Ibrahim, Ertl, Catani, Ismail, & Neuner, 2018; Weathers, Keane, Palmieri, Marx, & Schnurr, 2013), a 20-item checklist corresponding with DSM-5 PTSD symptoms. Items are rated on a 5-point scale (0 = not at all, 4 = extremely).
PSYCHLOPS assesses progress on problems for which the person seeks help (Ashworth et al., 2004). It consists of four questions encompassing three domains: problems (2 questions), functioning (1 question) and wellbeing (1 question). Participants are asked to give free-text responses to the problem and function domains. Responses are scored on an ordinal 6-point scale, producing a maximum score of 20. The PSYCHLOPS version administered at posttreatment and follow-up included an overall valuation question (determining self-rated outcome ranging from ‘much better’ to ‘much worse’).
Prolonged grief was assessed using the PG-13 (Prigerson et al., 2009). The PG-13 is a 13-item self-report measure that indexes core symptoms of prolonged grief disorder (PGD) as defined by the ICD-11. Each symptom is rated on a 5-point scale (1 = not at all, 5 = overwhelmingly). It is the most widely used measure of PGD, represents a unidimensional scale and has been shown to index grief-related impairment.
Prodromal psychotic symptoms were assessed using the Brief Prodromal Questionnaire-16 (PQ-B) (Loewy, Pearson, Vinogradov, Bearden, & Cannon, 2011). The self-reported questionnaire consists of 16 true or false items; items that are endorsed have additional questions that ask about corresponding levels of distress on a 4-point scale (0 = no, 3 = severe). Respondents who endorse ≥ six items are considered at risk for developing psychosis.
Psychological distress in the children of participants was assessed using the youth-reported version of the Paediatric Symptoms Checklist (Jellinek et al., 1999). It comprises 35 items rated on a 3-point scale (0 = never, 2 = often) and measures internalizing, externalizing, and somatic symptoms. The total score is calculated by summing the individual items and ranges from 0 to 70.
2.5.5. Other measures
Previous exposure to traumatic events was assessed using the Traumatic Events Checklist (TEC) (Gray, Litz, Hsu, & Lombardo, 2004). The TEC contains 27 potential events that participants may have experienced, witnessed, or heard about during their displacement and subsequent time residing in the camp. The post-migration living difficulties questionnaire (PMLD) was used to assess specific difficulties experienced by Syrian refugees upon arriving to Jordan (Silove, Sinnerbrink, Field, Manicavasagar, & Steel, 1997). The PMLD has 17-items which are rated on a 5-point scale (0 = was not a problem, 4 = a very serious problem).
2.6. Interventions
2.6.1. Group Problem Management Plus (GroupPM+)
The GroupPM+ programme involves a set of brief psychological interventions that seek to ameliorate symptoms of common mental disorders (e.g. depression, anxiety, stress) (Dawson et al., 2015). Prior to the trial, a comprehensive adaptation of the GroupPM+ manual was conducted to ensure that it was culturally relevant and appropriate for the Syrian population. This included a rapid qualitative review and cognitive interviews with beneficiaries, mental health care providers, and policymakers, followed by a cultural adaptation workshop to directly adapt the manuals. Following this, further work was conducted through focus groups to ensure that the manual was appropriate to the sociocultural context of Syrians residing in a refugee camp. Translation was conducted through an iterative process with feedback between the research team and translators.
PM+ integrates problem-solving and behavioural activation techniques that demonstrate amenability to low-intensity delivery and are evidence-based. GroupPM+ is delivered over 5 weekly sessions of 120 minutes duration. Clients are systematically taught four strategies, including stress management, problem management, behavioural activation, and skills to strengthen social support. In the current RCT, GroupPM+ was tested in the anticipated group size of 6–12 participants. Groups were conducted separately for men and women.
Each session was conducted by two GroupPM+ facilitators. The GroupPM+ facilitators were non-specialists, who held a bachelor degree in a psychology or a field related to health and have proficiency in Arabic. One local supervisor working within the camp provided weekly supervision. The facilitators received eight days of training in the delivery of the GroupPM+ intervention, as well as basic counselling and group facilitation skills. Following training, GroupPM+ facilitators were required to complete two practice cycles, as lead facilitator and co-facilitator, under close supervision.
2.6.2. Enhanced Treatment-as-Usual (ETAU)
Participants randomized into the ETAU group received a home visit from IMC staff and provided with information on where they could seek help for mental health concerns, as well as a range of other activities pertaining to health, parenting, and vocational training. Sessions were approximately 15 minutes in duration. This was considered enhanced in this context as treatment-as-usual in camp settings is often no treatment. Those randomized into the ETAU arm were not offered PM+ for the duration of this study.
2.6.3. Statistical analysis
This feasibility study was not intended to detect significant differences between those receiving GroupPM+ and ETAU, and accordingly no power calculations were conducted. Descriptive statistics were reported as mean and standard deviations or median and inter-quartile range, as appropriate. All analyses were conducted using SAS 9.4 (SAS Institute Inc, 2013).
3. Results
3.1. Recruitment and retention
In January 2019, 207 residents of Azraq camp were screened for psychological distress. Sixty-four (31%) met all inclusion criteria and were invited to participate in the feasibility study (Figure 1). Two individuals were excluded from the study due to suicidal ideation identified during screening. None of the 64 participants who screened positive declined to participate in the study. Socio-demographic characteristics are provided in Table 1.
Figure 1.
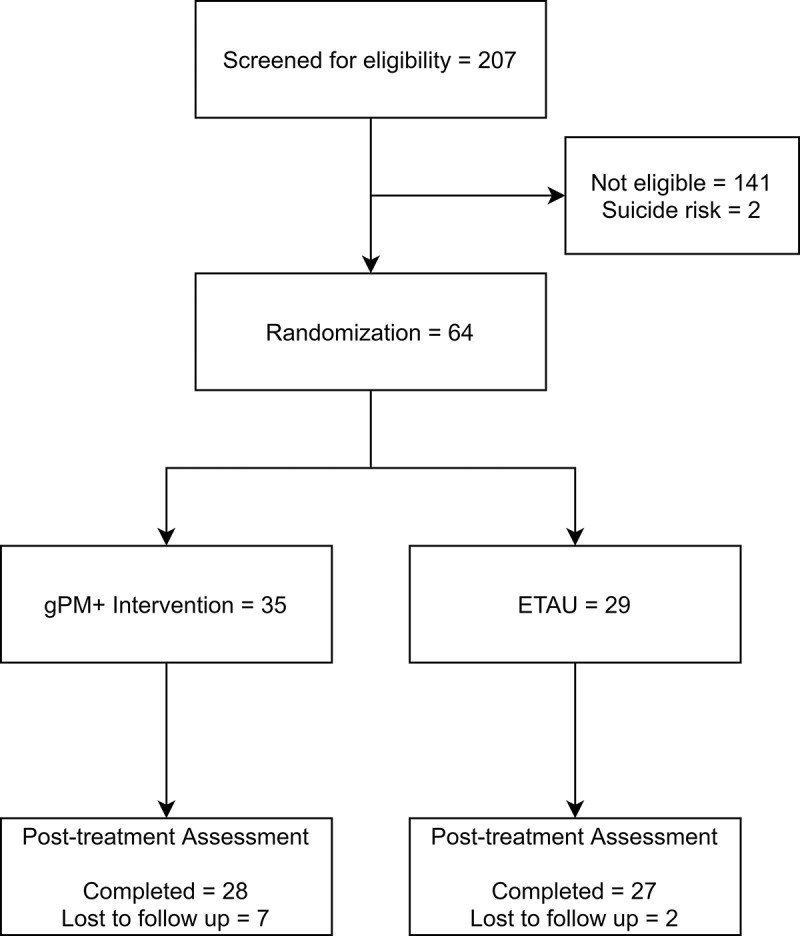
Study flowchart
Table 1.
Participant characteristics
| PM+ (n = 35) | ETAU (n = 29) | Total (n = 64) | |
|---|---|---|---|
| Age (mean, SD) | 43.43 (7.82) | 42.52 (6.42) | 43.02 (7.18) |
| Gender (N = Females, %) | 24 (68.57) | 21 (72.41) | 45 (70.31) |
| Highest Level of Education started? No Education (N,%) Basic Education Certificate (N,%) Technical/Vocational Secondary Education Certificate (N,%) Technical Diploma (N,%) Associate Degree (N,%) General Secondary Education (N,%) Bachelors Degree (N,%) Masters Degree (N,%) PhD (N,%) |
8 (22.86%) 23 (65.71%) 1 (2.86%) 0 (0%) 1 (2.86%) 1 (2.86%) 1 (2.86%) 0 (0%) 0 (0%) |
7 (24.14%) 18 (62.07%) 2 (6.90%) 0 (0%) 0 (0%) 2 (6.90%) 0 (0%) 0 (0%) 0 (0%) |
15 (23.44%) 41 (64.06%) 3 (4.69%) 0 (0%) 1 (1.56%) 3 (4.69%) 1 (1.56%) 0 (0%) 0 (0%) |
| Marital Status? Never Married (N,%) Currently Married (N,%) Separated (N,%) Divorced (N,%) Widowed (N,%) Cohabiting (N,%) |
0 (0%) 31 (88.57%) 0 (0%) 1 (2.86%) 3 (8.57%) 0 (0%) |
0 (0%) 27 (93.10%) 1 (3.45%) 0 (0%) 1 (3.45%) 0 (0%) |
0 (0%) 58 (90.63%) 1 (1.56%) 1 (1.56%) 4 (6.25%) 0 (0%) |
|
Allow to work in Jordan? (N = yes, %) Work status Paid work Self-employed Volunteer/Charity Student Homemaker Retired Unemployed Other |
9 (25.71%) 15 (42.86%) 7 (20%) 1 (2.86%) 1 (2.86%) 9 (25.71%) 0 (0%) 2 (5.72%) 0 (0%) |
8 (27.59%) 9 (31.03%) 3 (10.34%) 2 (6.90%) 0 (0%) 11 (37.93%) 0 (0%) 3 (10.34%) 1 (3.45%) |
17 (26.56%) 24 (37.50%) 10 (15.63%) 3 (4.69%) 1 (1.56%) 20 (31.25%) 0 (0%) 5 (7.81%) 1 (1.56%) |
| Attended ≥ 3 GroupPM+ sessions (N, %) | 24 (68.57%) | - | - |
The mean age of participants was 43 years (SD = 7.2). Participants were primarily women (N = 45, 70%), and most were currently married (N = 58, 91%). The most common level of education started was the basic education certificate (10 years of schooling) (N = 41, 64%) with 15 participants never having received any form of formal education (23%). The mean number of traumatic events experienced was 9.02 (SD = 4.3) with 75% of the sample experiencing between 6 and 12 traumatic events prior to the study (Table 2). The most commonly reported traumas were: (1) residing in a refugee camp (95%), (2) danger faced during the migration journey (89%), and (3) having been present in an active war zone (75%). The least reported traumas were: (1) non-sexual assault by family and friends (8%), (2) having been kidnapped (6%), and (3) having been brainwashed (3%). Participants indicated that they experienced an average of 8.91 (SD = 3.23) post-migration stressors in the previous year while residing in Azraq camp (Appendix).
Table 2.
Traumatic events
| GroupPM+ (n = 35) |
ETAU (n = 29) |
Total (n = 64) |
|
|---|---|---|---|
| Number of Traumatic Events (Mean, SD) | 8.66 (4.32) | 9.45 (4.3) | 9.02 (4.3) |
| Number of Traumatic Events (Median, IQR) | 9 (5, 12) | 9 (6, 12) | 9 (6, 12) |
|
32 (91.43) | 29 (100) | 61 (95.31) |
|
30 (85.71) | 27 (93.1) | 57 (89.06) |
|
25 (71.43) | 23 (79.31) | 48 (75) |
|
19 (54.29) | 17 (58.62) | 36 (56.25) |
|
17 (48.57) | 18 (62.07) | 35 (54.69) |
|
14 (40) | 18 (62.07) | 32 (50) |
|
16 (45.71) | 15 (51.72) | 31 (48.44) |
|
16 (45.71) | 13 (44.83) | 29 (45.31) |
|
8 (22.86) | 19 (65.52) | 27 (42.19) |
|
16 (45.71) | 10 (34.48) | 26 (40.63) |
|
14 (40) | 9 (31.03) | 23 (35.94) |
|
12 (34.29) | 8 (27.59) | 20 (31.25) |
|
10 (28.57) | 9 (31.03) | 19 (29.69) |
|
10 (28.57) | 9 (31.03) | 19 (29.69) |
|
11 (31.43) | 5 (17.24) | 16 (25) |
|
10 (28.57) | 6 (20.69) | 16 (25) |
|
6 (17.14) | 7 (24.14) | 13 (20.13) |
|
7 (20) | 5 (17.24) | 12 (18.75) |
|
4 (11.43) | 7 (24.14) | 11 (17.19) |
|
7 (20) | 3 (10.34) | 10 (15.63) |
|
3 (8.57) | 6 (20.69) | 9 (14.06) |
|
1 (9.38) | 5 (17.24) | 6 (9.38) |
|
2 (5.71) | 3 (10.34) | 5 (7.81) |
|
5 (14.29) | 0 (0) | 5 (7.81) |
|
3 (8.57) | 2 (6.90) | 5 (7.81) |
|
3 (8.57) | 1 (3.45) | 4 (6.25) |
|
2 (5.71) | 0 (0) | 2 (3.13) |
Following randomization, five GroupPM+ groups were organized. Of those randomized into the intervention arm (N = 35), approximately two-thirds attended three or more of the five sessions (N = 24, 69%), while seven (20%) did not attend any. Of these seven, three returned to Syria during the period between pre-assessment and the first session and two were unable to attend any sessions due to work opportunities. The remaining two participants refused attendance. All 29 participants randomized into the ETAU intervention received home visits by an IMC staff member and were provided with information regarding available resources in the camp. There were nine individuals who did not complete post-assessments (7 GroupPM+, 2 ETAU), four returned to Syria and two were not in the camp – all of whom were randomized into the intervention arm. Table 3 presents the mean scores for the psychological measures at baseline and post-intervention.
Table 3.
Psychological measures
| |
GroupPM+ (N = 35) |
ETAU (N = 29) |
||
|---|---|---|---|---|
| Pre-Assessment | Post-Assessment | Pre-Assessment | Post-Assessment | |
| Adult | N = 35 | N =28 | N =29 | N =27 |
| HSCL-25 Mean (SD) |
2.35 (0.64) | 2.03 (0.68) | 2.57 (0.63) | 2.25 (0.54) |
| Anxiety Mean (SD) |
2.30 (0.72) | 2.01 (0.73) | 2.44 (0.72) | 2.19 (0.65) |
| Depression Mean (SD) |
2.38 (0.69) | 2.04 (0.68) | 2.66 (0.65) | 2.29 (0.55) |
| PCL-5 Mean (SD) |
32.00 (19.21) | 22.86 (17.00) | 37.69 (18.55) | 23.33 (15.52) |
| PSYCHLOPS Mean (SD) |
15.54 (3.89) | 11.89 (5.01) | 16.90 (4.31) | 14.70 (4.45) |
| PQB-16 TOTAL Mean (SD) DISTRESS Mean (SD) |
4.43 (3.18) 7.97 (6.21) (n = 32) |
3.54 (3.65) 6.54 (7.62) (n = 24) |
6.07 (4.04) 10.61 (9.70) (n = 28) |
3.22 (3.21) 6.05 (7.34) (n = 19) |
| PG-13 Mean (SD) |
25.43 (11.98) |
20.64 (12.06) |
27.28 (11.51) |
27.48 (11.51) |
| Child |
N =34 |
N =26 |
N =28 |
N =25 |
| PSC-35 Mean (SD) |
18.41 (7.48) | 13.65 (8.25) | 18.29 (7.33) | 17.48 (10.27) |
| Attention Mean (SD) |
3.62 (2.46) | 3.58 (1.86) | 4.32 (2.07) | 3.80 (2.40) |
| Internalizing Mean (SD) |
3.56 (1.81) | 1.85 (2.13) | 3.00 (2.21) | 2.80 (2.55) |
| Externalizing Mean (SD) |
3.59 (1.81) | 2.08 (1.49) | 2.89 (1.64) | 3.28 (1.59) |
3.2. Safety
As noted above, two individuals were excluded at the screening phase due to suicidal ideation; both individuals were referred to specialized services to receive appropriate treatment. No adverse events were reported by participants throughout the study.
3.3. Missing data
There were nine (14.5%) individuals who did not complete post-assessments (7 GroupPM+, 2 ETAU). For those who completed both assessments, less than 3% of data were missing. Missing data were treated as random and missingness may have involved errors in data entry rather than capture.
4. Discussion
The primary aim of the feasibility study was to improve the implementation of the planned RCT by assessing safety and acceptability of the GroupPM+ intervention, and by identifying areas requiring adaptation. Among those who attended the intervention, retention was high. The study did not aim to explore changes in psychological measures and therefore only utilized a small representative sample. The main lesson to be learned from the outcome measures was that the assessment battery was acceptable insofar as most participants in both arms complied with instructions and completed these questionnaires.
Following screening, of the 64 participants who were eligible to complete the study none declined to participate in the feasibility trial indicating community acceptance. Although nine participants (14%) were lost to follow-up, six of these participants unexpectedly withdrew from the study to return to Syria or to pursue work opportunities and in turn their loss to follow-up was unrelated to the study. Due to limited work opportunities and mandatory appointments related to residence and refugee status within the camp, some loss to follow-up was expected.
During screening, two participants expressed imminent suicidal ideation and risk and were immediately referred to specialized services within the camp. No adverse events were reported during the trial demonstrating safety of the intervention. Overall, 24 of the 35 participants (69%) randomized to receive GroupPM+ completed the intervention and only four participants (14%) who attended at least one session attended fewer than three sessions. This demonstrates that those who attended at least one session generally had good attendance throughout the intervention and in turn indicates there was cultural acceptance of GroupPM+ in the camp. Immediately following the baseline assessment, and before the first GroupPM+ session, three participants randomized to the intervention arm returned to Syria and two others were directed to other activities that precluded participation. In the upcoming large-scale RCT, adjusting recruitment methods to increase engagement numbers of participants that attend the first session of GroupPM+ will hopefully result in increased attendance.
The recruitment of male participants into humanitarian research has often been neglected, with the majority of published papers focusing on the experiences of females (Affleck, Selvadurai, & Sikora, 2018). Males face unique stressors during displacement, and risk experiencing traumas related to combat situations (Affleck et al., 2018). Further strain is often placed on men as they are traditionally viewed as head of the household within the Syrian community, and must seek out scarce income-generating activities to provide for their families’ needs. It is imperative that males are recruited in humanitarian research to seek to understand the mental health impacts and efficacy of interventions in alleviating psychological distress in this population. Camp settings offer a unique opportunity to recruit males as both employment and extra-curricular activities are limited, affording camp-based males more time than those in community settings. In turn, it was anticipated that the study would recruit a sufficient number of male participants to conduct two GroupPM+ groups. In line with the sampling strategy, male and female assessors were asked to discuss the trial with the member of the house who answered the door but were often redirected to females for recruitment. As a result, lower numbers of males were recruited into the study and only eight male participants received GroupPM+. Of those, all participants attended a minimum of two sessions with five completing the intervention. The male participants that did not complete often cited income-generating opportunities as the primary reason for non-attendance during the intervention. Based on these results, the issue of recruiting male participants seems to lie in initial engagement as opposed to retention. Strategies to increase recruitment of males will be discussed prior to commencement of the definitive RCT.
GroupPM+ children were welcoming to the idea of participating in the trial with only three refusing participation. Although this trial was underpowered, the point estimates of PSC-35 displayed that children whose parents were enrolled in the intervention had a larger improvement demonstrated by a reduction in mean levels of psychological distress. Based on these results, we will use the Alabama Parental Questionnaire in the definitive trial to elucidate further the mechanism in which involvement in GroupPM+ may have positive impacts on the wellbeing of participants’ children.
4.1. Limitations
As this was a feasibility study, there was not sufficient power to elucidate effectiveness of the GroupPM+ intervention. However, lessons learned about implementing a trial of GroupPM+ in the context of a camp was the primary goal and this was met. Secondly, not all measures used in the trial have been previously validated for use with Syrian refugees. This is a common shortcoming of global mental health and future work should aim to validate measures during use in research trials. Thirdly, due to the close proximity of caravans to one another, contamination between families participating in the study was a possibility, although the extent to which this occurred was not measured in the present study. We also note that we do not report qualitative interviews with participants, assessors, or facilitators; this source of information can be useful to elucidate the barriers to successfully completing the definitive trial. Finally, during the definitive trial, the primary endpoint for the study will be a three-month follow-up. During the presented trial, we aimed to test the acceptance of the intervention and assessments which did not require the additional time point, although this prevented us from estimating projected retention rates.
4.2. Recommendations for transitioning to definitive trial
There were a number of lessons learned throughout the feasibility study that will help in adapting the upcoming large RCT. Firstly, screening was well accepted in the community with few households refusing participation if criteria were met; we qualify this conclusion, however, by recognizing that females were much more likely to respond to the assessors and thereby enter the trial than males. Additionally, number of households able to be screened was much greater in the assigned timeframe than anticipated. In turn, a greater number of GroupPM+ facilitators will be recruited in proportion to increased demand of the RCT. Increased focus in the RCT will be given to engaging participants prior to commencement of GroupPM+. The majority of those who attended at least one session completed the intervention (86%) which was similar to the completion rate of GroupPM+ in a previous RCT (Rahman et al., 2019). Although 86% recruitment and retention was good, attracting participants to the programme may still be improved. It is anticipated that efforts given to increasing participation in session one will have a positive impact on the proportion who complete the intervention. To attempt to increase participation in the first GroupPM+ session, scripts used by assessors to share details about the intervention will be revised in corroboration with feedback received from previous participants and field-staff to allow for a clearer understanding of the research.
Lastly, four participants returned to Syria during the project (6%). Of these four, three left immediately following baseline assessment and prior to the intervention while the other left after attending all GroupPM+ sessions prior to post-assessment. Since 2016 there have been more than 242,000 self-organized returns to Syria from host countries in the Middle East, of which 22% (53,980) were residing in Jordan. The number of Syrians returning has steadily increased year to year with almost 100,000 returning in 2019 (~30,000 from Jordan). Given this trend, to ensure adequate power for the definitive RCT, an adjusted power calculation is needed to account for attrition.
5. Conclusion
This pilot study demonstrates the GroupPM+ intervention is acceptable to Syrian refugees, as reflected in group attendance. Further, the manner in which refugees were recruited, assessed, and randomized in Azraq camp suggests that conducting this trial is feasible. Issues of limited movement, scarce resources, and accommodation shortages are common in many secure refugee camps; however, the current trial indicates that despite these factors a full definitive RCT of GroupPM+ is feasible in this setting. Further, this study showed promising signs for evaluating the effects of GroupPM+ on participants’ children. Accordingly, a full randomized controlled trial is needed to evaluate the efficacy of this intervention for refugees and their children in a camp setting.
Appendix.
Post-migration living difficulties
| PM+ (n = 35) | ETAU (n = 29) | Total (n = 64) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Difficulties (Mean, SD) | 8.31 (3.34) | 9.62 (2.98) | 8.91 (3.23) | ||||||||||||
| Number of Difficulties (Median, IQR) | 9 (6, 11) | 9 (7, 12) | 9 (6.5, 11) | ||||||||||||
| 0 | 1 | 2 | 3 | 4 | 0 | 1 | 2 | 3 | 4 | 0 | 1 | 2 | 3 | 4 | |
|
20 57.14 |
5 14.29 |
4 11.43 |
3 8.57 |
3 8.57 |
14 48.48 |
8 27.59 |
4 13.79 |
2 6.9 |
1 3.45 |
34 53.13 |
13 20.31 |
8 12.5 |
5 7.81 |
4 6.25 |
|
1440 | 2 5.71 |
4 11.43 |
5 14.29 |
10 28.57 |
14 48.28 |
4 13.79 |
2 6.9 |
2 6.9 |
7 24.14 |
28 43.75 |
6 9.38 |
6 9.38 |
7 10.94 |
17 26.56 |
|
2880 | 3 8.57 |
1 2.86 |
1 2.86 |
2 5.71 |
18 62.07 |
6 20.69 |
2 6.9 |
1 3.45 |
2 6.9 |
46 71.88 |
9 14.06 |
3 4.69 |
2 3.13 |
4 6.25 |
|
10 28.57 |
1 2.86 |
9 25.71 |
3 8.57 |
12 34.29 |
5 17.24 |
0 0 |
4 13.79 |
2 6.9 |
18 62.07 |
15 23.44 |
1 1.56 |
13 20.31 |
5 7.81 |
30 46.88 |
|
7 20 |
3 8.57 |
4 11.43 |
6 17.14 |
15 42.86 |
2 6.9 |
1 3.45 |
5 17.24 |
4 13.79 |
17 58.62 |
9 14.06 |
4 6.25 |
9 14.06 |
10 15.63 |
3250 |
|
13 37.14 |
3 8.57 |
8 22.86 |
1 2.86 |
10 28.57 |
11 37.93 |
4 13.79 |
6 20.69 |
2 6.9 |
6 20.69 |
24 37.5 |
7 10.94 |
14 21.88 |
3 4.69 |
1625 |
|
13 37.14 |
1 2.86 |
2 5.71 |
3 8.57 |
16 45.71 |
4 13.79 |
1 3.45 |
3 10.34 |
4 13.79 |
17 58.62 |
17 26.56 |
2 3.13 |
5 7.81 |
7 10.94 |
33 51.56 |
|
25 71.43 |
1 2.86 |
2 5.71 |
0 0 |
7 20 |
20 68.97 |
1 3.45 |
1 3.45 |
1 3.45 |
6 20.69 |
45 70.31 |
2 3.13 |
3 4.69 |
1 1.56 |
13 20.31 |
|
31 88.57 |
2 5.71 |
2 5.71 |
0 0 |
0 0 |
25 86.21 |
1 3.45 |
1 3.45 |
1 3.45 |
1 3.45 |
56 87.50 |
3 4.69 |
3 4.69 |
1 1.56 |
1 1.56 |
|
34 97.14 |
0 0 |
0 0 |
0 0 |
1 2.86 |
26 89.66 |
1 3.45 |
1 3.45 |
0 0 |
1 3.45 |
60 93.75 |
1 1.56 |
1 1.56 |
0 0 |
2 3.13 |
|
12 34.29 |
3 8.57 |
3 8.57 |
8 22.86 |
9 25.71 |
8 27.59 |
0 0 |
9 31.03 |
3 10.34 |
9 31.03 |
20 31.25 |
3 4.69 |
12 18.75 |
11 17.19 |
18 28.13 |
|
1440 | 2 5.71 |
6 17.14 |
4 11.43 |
9 25.71 |
8 27.59 |
0 0 |
6 20.69 |
6 20.69 |
9 31.03 |
22 34.38 |
2 3.13 |
12 18.75 |
10 15.63 |
18 28.13 |
|
6 17.14 |
3 8.57 |
4 11.43 |
6 17.14 |
16 45.71 |
1 3.45 |
1 3.45 |
1 3.45 |
4 13.79 |
22 75.86 |
7 10.94 |
4 6.25 |
5 7.81 |
10 15.63 |
38 59.38 |
|
10 28.57 |
3 8.57 |
5 14.29 |
4 11.53 |
13 37.14 |
6 20.69 |
1 3.45 |
2 6.9 |
4 13.79 |
16 55.17 |
1625 | 4 6.25 |
7 10.94 |
8 12.5 |
29 45.31 |
|
5 14.29 |
2 5.71 |
12 34.29 |
6 17.14 |
10 28.57 |
2 6.9 |
1 3.45 |
11 37.93 |
7 24.14 |
8 27.59 |
7 10.94 |
3 4.69 |
23 35.94 |
13 20.13 |
18 28.13 |
|
34 97.14 |
0 0 |
0 0 |
0 0 |
1 2.86 |
29100 | 0 0 |
0 0 |
0 0 |
0 0 |
63 97.14 |
0 0 |
0 0 |
0 0 |
1 2.86 |
|
2880 | 0 0 |
3 8.57 |
2 5.71 |
2 5.71 |
21 72.41 |
1 3.45 |
2 6.9 |
2 6.9 |
3 10.34 |
49 76.56 |
1 1.56 |
5 7.81 |
4 6.25 |
5 7.81 |
Funding Statement
This work was supported by a National Health and Medical Research Council-European Union Grant [1142605] and a European Union Horizon 2020 grant [733337]. The study funders had no role in study design; collection, management, analysis, and interpretation of data; writing of the report; or the decision to submit the report for publication.
Availability of data and materials
The data are initially available to the STRENGTHS Consortium to allow individual patient data meta-analyses of all PM+ trials conducted within this consortium. Following this, data will be freely available on request. The deidentified data of this study are available at doi10.6084/m9.figshare.14401289.
Consent for publication
Not applicable.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethics approval and consent to participate
The project has been approved locally by the Institutional Review Board at the King Hussein Cancer Centre in Amman, Jordan and the University of New South Wales Human Research Ethics Committee. Informed consent involved two-steps: 1) consent to conduct the screening and 2) consent for taking part in the GroupPM+ feasibility trial. The latter was only required for participants meeting inclusion criteria following screening. For each step, participating respondents were asked to complete a written consent form. For illiterate participants, witnessed oral consent was collected in line with recommendations from WHO.
References
- Affleck, W., Selvadurai, A., & Sikora, L. (2018). Underrepresentation of men in gender based humanitarian and refugee trauma research: A scoping review. Intervention Intervention, 16(1), 22. doi: 10.1097/WTF.0000000000000157 [DOI] [Google Scholar]
- Arain, M., Campbell, M. J., Cooper, C. L., & Lancaster, G. A. (2010). What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Medical Research Methodology, 10(1), 67. doi: 10.1186/1471-2288-10-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashworth, M., Shepherd, M., Christey, J., Matthews, V., Wright, K., Parmentier, H., … Godfrey, E. (2004). A client-generated psychometric instrument: The development of ‘PSYCHLOPS’. Counselling and Psychotherapy Research, 4(2), 27–13. doi: 10.1080/14733140412331383913 [DOI] [Google Scholar]
- Barbui, C., Purgato, M., Abdulmalik, J., Acarturk, C., Eaton, J., Gastaldon, C., … Thornicroft, G. (2020). Efficacy of psychosocial interventions for mental health outcomes in low-income and middle-income countries: An umbrella review. The Lancet Psychiatry, 7(2), 162–172. doi: 10.1016/S2215-0366(19)30511-5 [DOI] [PubMed] [Google Scholar]
- Bhutta, Z. A. (2004). Beyond informed consent. World Health Organization. Bulletin of the World Health Organization, 82(10), 771–777. https://pubmed.ncbi.nlm.nih.gov/15643799/ [PMC free article] [PubMed] [Google Scholar]
- Bronstein, I., & Montgomery, P. (2011). Psychological distress in refugee children: A systematic review. Clinical Child and Family Psychology Review, 14(1), 44–56. doi: 10.1007/s10567-010-0081-0 [DOI] [PubMed] [Google Scholar]
- Bryant, R. A., Edwards, B., Creamer, M., O’Donnell, M., Forbes, D., Felmingham, K. L., … Hadzi-Pavlovic, D. (2018). The effect of post-traumatic stress disorder on refugees’ parenting and their children’s mental health: A cohort study. The Lancet Public Health, 3(5), e249–e258. doi: 10.1016/S2468-2667(18)30051-3 [DOI] [PubMed] [Google Scholar]
- Bryant, R. A., Schafer, A., Dawson, K. S., Anjuri, D., Mulili, C., Ndogoni, L., & Tsai, A. C. (2017). Effectiveness of a brief behavioural intervention on psychological distress among women with a history of gender-based violence in urban Kenya: A randomised clinical trial. PLOS Medicine, 14(8), e1002371. doi: 10.1371/journal.pmed.1002371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson, F., Van Ommeren, M., Flaxman, A., Cornett, J., Whiteford, H., & Saxena, S. (2019). New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. The Lancet, 394(10194), 240–248. doi: 10.1016/S0140-6736(19)30934-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daisy, R., Singla, D. R., Kohrt, B., Murray, L. K., Anand, A., Chorpita, B. F., & Patel, V. (2017). Psychological treatments for the world: Lessons from low- and middle-income countries. Annual Review of Clinical Psychology, 13(1), 149–181. doi: 10.1146/annurev-clinpsy-032816-045217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson, K. S., Bryant, R. A., Harper, M., Kuowei Tay, A., Rahman, A., Schafer, A., & Van Ommeren, M. (2015). Problem Management Plus (PM+): A WHO transdiagnostic psychological intervention for common mental health problems. World Psychiatry, 14(3), 354–357. doi: 10.1002/wps.20255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson, K. S., Schafer, A., Anjuri, D., Ndogoni, L., Musyoki, C., Sijbrandij, M., & Bryant, R. A. (2016). Feasibility trial of a scalable psychological intervention for women affected by urban adversity and gender-based violence in Nairobi. BMC Psychiatry, 16(1), 1–9. doi: 10.1186/s12888-016-1117-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis, L. R., Lipman, R. S., Rickels, K., Uhlenhuth, E. H., & Covi, L. (1974). The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behavioral Science, 19(1), 1–15. doi: 10.1002/bs.3830190102 [DOI] [PubMed] [Google Scholar]
- Eaton, J., McCay, L., Semrau, M., Chatterjee, S., Baingana, F., Araya, R., … Saxena, S. (2011). Scale up of services for mental health in low-income and middle-income countries. The Lancet, 378(9802), 1592–1603. doi: 10.1016/S0140-6736(11)60891-X [DOI] [PubMed] [Google Scholar]
- Gray, M. J., Litz, B. T., Hsu, J. L., & Lombardo, T. W. (2004). Psychometric properties of the life events checklist. Assessment, 11(4), 330–341. doi: 10.1177/1073191104269954 [DOI] [PubMed] [Google Scholar]
- Hassan, G., Ventevogel, P., Jefee-Bahloul, H., Barkil-Oteo, A., & Kirmayer, L. J. (2016). Mental health and psychosocial wellbeing of Syrians affected by armed conflict. Epidemiology and Psychiatric Sciences, 25(2), 129–141. doi: 10.1017/S2045796016000044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrickx, M., Woodward, A., Fuhr, D.C., Sondorp, E., & Roberts, B. (2020). The burden of mental disorders and access to mental health and psychosocial support services in Syria and among Syrian refugees in neighboring countries: A systematic review. Journal of Public Health (Oxford). 42(3), e299–e310. doi: 10.1093/pubmed/fdz097 [DOI] [PubMed]
- Ibrahim, H., Ertl, V., Catani, C., Ismail, A. A., & Neuner, F. (2018). The validity of Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) as screening instrument with Kurdish and Arab displaced populations living in the Kurdistan region of Iraq. BMC Psychiatry, 18(1), 1–8. doi: 10.1186/s12888-018-1839-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jellinek, M. S., Murphy, J. M., Little, M., Pagano, M. E., Comer, D. M., & Kelleher, K. J. (1999). Use of the Pediatric Symptom Checklist to screen for psychosocial problems in pediatric primary care: A national feasibility study. Archives of Pediatrics & Adolescent Medicine, 153(3), 254–260. doi: 10.1001/archpedi.153.3.254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan Ministry of Planning and International Cooperation . (2018). Jordan response plan for the Syria crises, 2018–2020. Amman: MOPIC. [Google Scholar]
- Kessler, R. C., Andrews, G., Colpe, L., Hiripi, E., Mroczek, D., Normand, S. L., … Zaslavsky, A. (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32(6), 959–976. doi: 10.1017/S0033291702006074 [DOI] [PubMed] [Google Scholar]
- Loewy, R. L., Pearson, R., Vinogradov, S., Bearden, C. E., & Cannon, T. D. (2011). Psychosis risk screening with the Prodromal Questionnaire–brief version (PQ-B). Schizophrenia Research, 129(1), 42–46. doi: 10.1016/j.schres.2011.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morina, N., Malek, M., Nickerson, A., & Bryant, R. A. (2017). Meta-analysis of interventions for posttraumatic stress disorder and depression in adult survivors of mass violence in low- and middle-income countries. Depression and Anxiety, 34(8), 679–691. doi: 10.1002/da.22618 [DOI] [PubMed] [Google Scholar]
- Prigerson, H. G., Horowitz, M. J., Jacobs, S. C., Parkes, C. M., Aslan, M., Goodkin, K., … Brayne, C. (2009). Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLOS Medicine, 6(8), e1000121. doi: 10.1371/journal.pmed.1000121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, A., Hamdani, S. U., Awan, N. R., Bryant, R. A., Dawson, K. S., Khan, M. F., … Van Ommeren, M. (2016). Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: A randomized clinical trial. JAMA, 316(24), 2609–2617. doi: 10.1001/jama.2016.17165 [DOI] [PubMed] [Google Scholar]
- Rahman, A., Khan, M. N., Hamdani, S. U., Chiumento, A., Akhtar, P., Nazir, H., … Van Ommeren, M. (2019). Effectiveness of a brief group psychological intervention for women in a post-conflict setting in Pakistan: A single-blind, cluster, randomised controlled trial. The Lancet, 393(10182), 1733–1744. doi: 10.1016/S0140-6736(18)32343-2 [DOI] [PubMed] [Google Scholar]
- Rahman, A., Riaz, N., Dawson, K. S., Usman Hamdani, S., Chiumento, A., Sijbrandij, M., … Farooq, S. (2016). Problem Management Plus (PM+): Pilot trial of a WHO transdiagnostic psychological intervention in conflict‐affected Pakistan. World Psychiatry, 15(2), 182. doi: 10.1002/wps.20312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley, A., Varner, A., Ventevogel, P., Taimur Hasan, M. M., & Welton-Mitchell, C. (2017). Daily stressors, trauma exposure, and mental health among stateless Rohingya refugees in Bangladesh. Transcultural Psychiatry, 54(3), 304–331. doi: 10.1177/1363461517705571 [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc (ed.). (2013). The SAS system for Windows. Release 9.2. Cary, NC: ed. S. Inst. [Google Scholar]
- Selmo, P., Koch, T., Brand, J., Wagner, B., & Knaevelsrud, C. (2019). Psychometric properties of the online arabic versions of BDI-II, HSCL-25, and PDS. European Journal of Psychological Assessment, 35(1), 46–54. doi: 10.1027/1015-5759/a000367 [DOI] [Google Scholar]
- Silove, D. (1999). The psychosocial effects of torture, mass human rights violations, and refugee trauma: toward an integrated conceptual framework. The Journal of Nervous and Mental Disease, 187(4), 200–207. doi: 10.1097/00005053-199904000-00002 [DOI] [PubMed] [Google Scholar]
- Silove, D., Sinnerbrink, I., Field, A., Manicavasagar, V., & Steel, Z. (1997). Anxiety, depression and PTSD in asylum-seekers: Associations with pre-migration trauma and post-migration stressors. British Journal of Psychiatry, 170(4), 351–357. doi: 10.1192/bjp.170.4.351 [DOI] [PubMed] [Google Scholar]
- Slade, T., Grove, R., & Burgess, P. (2011). Kessler psychological distress scale: Normative data from the 2007 Australian national survey of mental health and wellbeing. Australian & New Zealand Journal of Psychiatry, 45(4), 308–316. doi: 10.3109/00048674.2010.543653 [DOI] [PubMed] [Google Scholar]
- UNHCR . (2020a). Global trends: Forced displacement in 2019. Geneva: UNHCR. [Google Scholar]
- UNHCR . (2020b, April 9). Figures at a glance. Retrieved from http://www.unhcr.org/uk/figures-at-a-glance.html [Google Scholar]
- UNHCR . (2020c, September 1). Syria regional refugee response: Jordan. Retrieved from https://data2.unhcr.org/en/situations/syria/location/36 [Google Scholar]
- UNHCR . (2020d). Jordan: Azraq refugee camp, June 2020. Geneva: UNHCR. [Google Scholar]
- Ustun, T. B., Kostanjesek, N., Chatterji, S., Rehm, J., & World Health Organization. (2010). Measuring health and disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0). Geneva: World Health Organization. [Google Scholar]
- Weathers, F. W. L. B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). Retrieved from Scale available at from the National Center for PTSD at: www.ptsd.va.gov [Google Scholar]
- World Health Organization . (2010). mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings. Geneva: Author. [PubMed] [Google Scholar]
- World Health Organization . (2013). Building back better: Sustainable mental health care after emergencies. Geneva: WHO. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are initially available to the STRENGTHS Consortium to allow individual patient data meta-analyses of all PM+ trials conducted within this consortium. Following this, data will be freely available on request. The deidentified data of this study are available at doi10.6084/m9.figshare.14401289.


