Abstract
Background
The provision of public adaptive coping strategies to reduce psychological tension during the ongoing COVID-19 pandemic is critical. We sought to provide evidence-based guidance for psychological intervention, exploring the potential mediating roles of three sources of social support (i.e., subjective support, family support and counselor support) between coping strategies (i.e., cognitive coping, emotional coping and behavioral coping), and anxiety among college students at the height of the pandemic in China.
Methods
Using the Coping Strategy Questionnaire, Social Support Questionnaire, and Self-Rating Anxiety Scale, this large-scale online study analyzed the levels of social support, coping, and anxiety among 2640 college students in China from February 21st to 24th, 2020, when the students had been isolated at home for 1 month since the lockdown of Wuhan city.
Results
Students reported high levels of cognitive coping, behavioral coping, and social support. They also experienced low levels of anxiety and emotional coping. Anxiety was significantly and negatively related to coping and social support. The mediating roles of three sources of social support were found between cognitive coping, behavioral coping, and anxiety, respectively. However, the effect of emotional coping on anxiety was not found to be mediated by social support.
Conclusions
Adopting positive coping strategies may enhance social support that in turn relieves anxiety. The effect of social support, especially family and counselor support, should arouse greater awareness in coping with the pandemic cognitively and behaviorally.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-021-11332-4.
Keywords: Coping strategy, Social support, Anxiety, Mediator, COVID-19 pandemic
Background
The outbreak of Coronavirus Disease 2019 (COVID-19) has invoked panic and anxiety in the world. Under this unprecedented circumstance, the Chinese government has taken an active stance and implemented extreme measures to mitigate the dissemination of the disease. Some of these measures include suspending all public emigration in Wuhan on January 23rd, 2020, introduction of forced quarantine for citizens in the peak period, extending holidays, and closing schools [1]. As a result, people resorted to adaptive coping strategies as well. A great deal of attention has been paid by citizens to COVID-19 epidemic news and overreaction triggered by rumors and exaggerated information occurs [2, 3]. In a survey conducted in Canada in early February 2020, 33% of respondents revealed little confidence in the capability of their healthcare system to handle the disease, indicating low emotional coping among individuals [4].
In addition to coping strategies, a range of negative psychological consequences is usually accompanied by physical harm during the outbreak of a pandemic, such as depression, panic, and anxiety [5]. A recent study stated that more than 70% of clinicians who treated confirmed COVID-19 patients had gone through psychological distress, and 44.6% had been experiencing anxiety under the daunting environment [6]. People who are required to quarantine are prone to various mental problems. Self-isolated adults who were suspected COVID-19 cases reported high levels of anxiety with low sleep quality [7]. The reason for this psychological pressure is primarily due to the lack of interpersonal association, and therefore, the significance of social support deserves consideration [8].
Stewart’s coping theory stated that social support should be determined as one of the coping resources [9]. Since seeking social support has been regarded as one of the most adaptive approaches to cope with stress during crises [10], a number of previous COVID-related studies have emphasized the need for social support. A study aimed at clinicians in Wuhan, China, who treated infected patients found that the social support of healthcare professionals had an indirect effect on sleep quality. However, most studies measured general social support rather than specific social support from various sources. To the best of our knowledge, a study sampled by 628 college students is the only one identifying the mediating role of multiple social support from family, friends, and romantic partners, respectively between stress and well-being [11]. Given the limited scope of available studies coupled with specific social support in this crisis, the present study focused on the roles of three sources of social support (i.e., subjective support, family support, and counselor support) in managing the COVID-19 pandemic.
Although a variety of studies have drawn attention to coping strategies, anxiety, and social support [12, 13], few studies have been conducted to identify their relationship under the circumstance of the COVID-19 pandemic. Moreover, to our knowledge, a large-scale empirical study aimed at college students’ mental health condition and coping in the pandemic seems insufficient. Furthermore, there is a lack of research on the role of various sources of social support in coping and anxiety. Therefore, the study aimed to examine the relationships between coping strategies, social support, and anxiety. Also, the study delved into the potential mediating effect of social support on these relationships to disentangle the internal support mechanisms underlying coping and mental health among Chinese college students in January and February when the epidemic peaked in China. The data at that time could reflect the authenticity and reliability of the students’ coping status, which highlighted the significance of this research. Moreover, our study is novel in probing into the mediating roles of differentiated sources of social support in coping and anxiety during this time.
Methods
Design and research questions
Using stratified random sampling in terms of students’ sex, major, and academic degree in this large-scale study, 2640 college students from a comprehensive university in Shenzhen, an important economic zone in China, completed the online survey during February 21st to 24th 2020, when the students had been isolated at home for at least 1 month since the lockdown of Wuhan city. The following research questions and hypotheses in the context of the COVID-19 pandemic are proposed.
RQ1: What is the status of coping strategies, social support, and anxiety among Chinese college students?
RQ2: What are the relationships between coping strategies, social support, and anxiety?
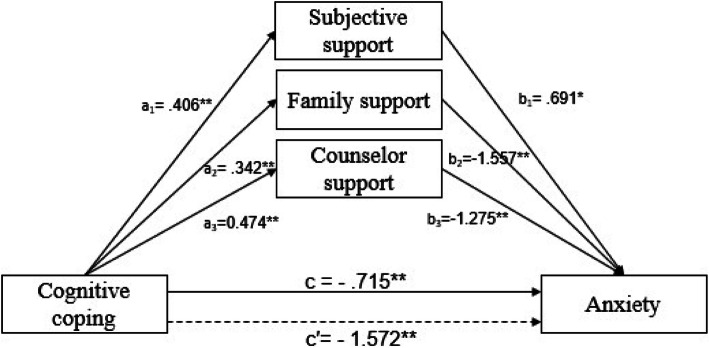
Given the mediating role of social support between performance and mental health, is it plausible that various sources of social support mediate the relationship between coping and anxiety during the pandemic? Based on the findings above, three hypotheses are proposed.
H1: The relationship between cognitive coping and anxiety is mediated by social support.
H2: Social support has a mediating effect on the relationship between emotional coping and anxiety.
H3: Social support plays a mediating role in the relationship between behavioral coping and anxiety.
Conceptual model
The conceptual model is presented as follows (Fig. 1):
Fig. 1.
Note: Dashed lines indicate the mediating effect of coping strategy on anxiety
Coping strategies are widely classified as either positive or negative [14]. However, general coping strategies are differentiated from practical coping strategies which refer to specific behaviors in the pandemic context [15].
To address pandemic coping more specifically, the present study adopted Lazarus and Folkman’s theory of psychological stress which divided coping into problem-focused coping (i.e., cognitive and behavioral efforts to solve the problem causing the distress) and emotion-focused coping confronted with stress [16], and classified coping into cognitive, emotional, and behavioral coping. Cognitive coping indicated the awareness of the current crisis and the way pandemic news was handled. Current COVID-19-related studies proved that proper perception of accurate information could predict lower levels of anxiety [5], and adequate information about the acquisition of the virus was negatively related to the emergence of mental problems [17]. Based on the themes drawn by the Cognitive-Motivational-Relational theory of emotion, emotional coping pertained to the emotional experience and adaptive actions that came from them [18], which in the present study referred to the affective uncertainty and worries about the disease. Evidence proved that more intolerance of uncertainty predicted greater reports of anxiety in the 2009 H1N1 pandemic [19]. In addition, Emotion-focused coping employed in the COVID-19 pandemic such as “being angry, and yelling” tended to highlight the sense of powerlessness and anxiety [17]. Behavioral coping signified the activities to alter the stressful encounter [16], indicating the pandemic precautions. Personal preventive measures such as hand washing and wearing face masks were found to be associated with fewer psychiatric symptoms [5, 20].
In the social support norm, subjective support denoted individual resilience targeting the stressors in the pandemic, which comprises personal competence and confidence in one’s instincts to cope with adverse circumstances [21]. Family support herein represented the perceived support quality from family. The Centers for Disease Control and Prevention argued the crucial role of family support in coping with anxiety [22]. Family care could be preferred as a critical source and it is imperative to facilitate meaningful communication between family caregivers and old adults in long-term care facilities [23]. Additionally, counselor support referred to emergent countermeasures implemented by psychological counselors, embracing the issue of self-help manuals, operation of 24-h psychological hotlines, and online survey applications [24]. Since the closing of schools, many universities in China have initiated online psychological counseling services and published mental health guidelines to support college students [25].
Measures
Sociodemographic characteristics questionnaire (SCQ)
The SCQ was designed to collect students’ sociodemographic data, including sex, major, academic attainment (graduate or undergraduate), current location (Hubei Province, the pandemic zone or not), isolation condition (medically observed or not), and self-perceived health status.
Coping strategy questionnaire (CSQ)
The CSQ was used to evaluate coping strategies adopted by the students in the COVID-19 pandemic. This novel questionnaire was framed on the theory of psychological stress [16], and COVID-related coping was then divided into cognitive coping (CC; items 1–3), emotional coping (EC; items 4–6) and behavioral coping (BC; items 7–10) (see Table S1). The 5-point Likert scale was rated from “strongly disagree” to “strongly agree” with the subscale of emotional coping reversely coded, with higher scores indicating higher frequencies of positive coping.
Principal components analyses were conducted to verify the validity of this scale. The Kaiser-Meyer-Olkin test yielded an index of 0.795, and Bartlett’s test of sphericity was significant. Three factors emerged, accounting for a total of 61.396% of the variance, with the factor of CC, EC, and BC accounting for 24.540, 18.674, and 18.183%, respectively. The Cronbach’s alpha coefficient was 0.83 with 0.70, 0.67, and 0.77 for each subscale dimension (CC, EC, BC) respectively.
Social support questionnaire (SSQ)
The SSQ revised from the Chinese version of the SSQ was used to assess the levels of social support perceived by the students [26]. The questionnaire contained three dimensions, including subjective support (items 1–2), family support (items 3–4) and counselor support (items 5–6). Each item is rated from 1 to 5 (1 = strongly disagree, 5 = strongly agree), with a high score reflecting a high level of social support. In the present sample, with 0.89 for the overall SSQ, the Cronbach’s alpha coefficients for the subjective support, family support, and counselor support subscales were 0.93, 0.77, and 0.97, respectively.
Self-rating anxiety scale (SAS)
The anxiety of the students was measured using the SAS [27]. The SAS questionnaire contained 20 four-point-scale items, of which the aggregate score was then multiplied by 1.25, with higher scores indicating more severe levels of anxiety. The scale was reliable, with a Cronbach’s alpha coefficient of 0.89 in this research.
Data collection procedures
This study was granted ethics approval by the Human Research Ethics Committee of City University of Macau (EA2001025). Eligible participants were young adults aged 18 to 25 years who are currently enrolling at a Chinese university. Of the 2680 participants recruited, 2640 students completed the survey, for a return rate of 98.5%. Subsequently, the data of 2640 participants were validly analyzed in this study. The participants were sent an email with the purpose and requirements for the investigation. After granting permission for inclusion, the respondents completed the questionnaires during February 21st and 24th of 2020 anonymously via an online survey with a random gift card distribution as incentives at the end of the questionnaires.
Data analysis
The data were analyzed using IBM SPSS statistics 24.0 for Windows (IBM Corp., Armonk, NY, USA). First, descriptive statistics were used to summarize the demographic characteristics of the participants and the means of the investigated variables. To test the normality of data distribution, one-sample Kolmogorov-Smirnov test and histogram plot were used. Then, correlations between coping, social support, and anxiety were measured by Spearman’s correlation analyses. Finally, to explore the roles of social support in mediating the relationships between coping and anxiety, bootstrapping was applied with 5000 resamples with bias-corrected 95% confidence intervals (CI). In the mediation effect test, if the 95% CI did not contain zero, the mediation effect would be significant at the 0.05 level [28]. Meanwhile, both the direct and total effects were analyzed.
Results
Descriptive statistics
Demographic characteristics are presented in Table 1. The students surveyed were composed of graduates and undergraduates, some of whom were medically observed or isolated in Hubei Province, a province with a comparatively severe pandemic. In addition, the students’ ratings on perceived health condition were collected to assess their current self-efficacy on health.
Table 1.
Sociodemographic characteristics of the participants (n = 2640)
| Sociodemographic variables | Subcategories | n | % |
|---|---|---|---|
| Sex | Male | 824 | 31.21 |
| Female | 1816 | 68.79 | |
| Academic attainment | Graduate student | 383 | 14.51 |
| Undergraduate | 2257 | 85.49 | |
| Current location | Hubei Province (the epicenter) | 62 | 2.35 |
| Other provinces | 2578 | 97.65 | |
| Isolation condition | Medically observed | 24 | 0.91 |
| Not isolated | 2616 | 99.09 | |
| Self-perceived health status | Very healthy | 2136 | 80.91 |
| Healthy | 465 | 17.61 | |
| Not sure | 37 | 1.4 | |
| Not healthy | 2 | 0.08 |
Correlation analyses
The means and standard deviations of coping, social support, and anxiety are given in Table 2. The students showed high levels of cognitive coping (M = 4.53, SD = 0.47), behavioral coping (M = 4.76, SD = 0.37), and social support (M = 4.59, SD = 0.55), and low emotional coping (M = 2.76, SD = 0.87). Compared with the Chinese norm of the SAS (M = 29.78, SD = 0.46) in the ordinary period, the students experienced significantly higher anxiety during the epidemic period (M = 36.25, SD = 4.57, t = 72.815, p = 0.000) [29].
Table 2.
Correlations between coping strategy, social support, anxiety, and subscales
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. CSa | |||||||||
| 2. CC | .560** | ||||||||
| 3. EC | .694** | −.021 | – | ||||||
| 4. BC | .505** | .462** | −.097** | – | |||||
| 5. SSa | .421** | .531** | −.022 | .572** | – | ||||
| 6. SSb | .436* | .469** | .008 | .553** | .782** | – | |||
| 7. FS | .399** | .507** | −.046* | .557** | .883** | .686** | – | ||
| 8. CSb | .376** | .477** | −.024 | .507** | .933** | .616** | .767** | – | |
| 9. A | −.211** | −.218** | −.135** | −.141** | −.295** | −.253** | −.221** | −.283** | – |
| Mean | 4.09 | 4.53 | 2.76 | 4.76 | 4.59 | 4.70 | 4.62 | 4.44 | 36.25 |
| SD | 0.35 | 0.47 | 0.87 | 0.37 | 0.55 | 0.52 | 0.57 | 0.82 | 4.57 |
Note: * p < .05, ** p < .01; CSa Coping Strategy, CC Cognitive Coping, EC Emotional Coping, BC Behavioral Coping, SSa Social Support, SSb Subjective Support, FS Family Support, CSb Counselor Support, A Anxiety
Confirmed as abnormally distributed data, Spearman’s correlation analyses were conducted. The results in Table 2 revealed that anxiety was significantly and negatively associated with coping (r = −.211, p < 0.01), and social support (r = −.295, p < 0.01). More precisely, the correlation coefficient between anxiety and social support (r = −.295, p < 0.01) was distinctly higher than that between anxiety and behavioral coping (r = −.141, p < 0.01). Notably, emotional coping was not significantly correlated with social support (r = −.022, p > 0.01).
Mediation analyses
After finding internal links among coping strategy, social support, and anxiety, the study examined the potential mediating role of social support between coping strategy and anxiety. To obtain a detailed insight into coping strategy, the effect of the mediator variables was explored between the subscales of coping strategy (i.e., cognitive coping, emotional coping, and behavioral coping) and anxiety by bootstrapping. Since sex and academic attainment may serve as covariates, independent sample t-tests were used to compare group differences in the social support (M variable) and anxiety (Y variable). T-tests analyses showed that there were no significant differences in social support, the subscales of social support, and anxiety among students with various academic attainment (p > 0.05). The differences between male and female appeared insignificant in social support and the subscales of social support (p > 0.05), but significant in anxiety (t = − 4.347, p = 0.000). However, G*Power analyses showed that the effect size index d (Cohen’s d = 0.183) was smaller than 0.20, which indicated that the significant difference of sex in anxiety addressed little effect size [30]. Therefore, sex and academic attainment were not treated as covariates in the following mediation effect models.
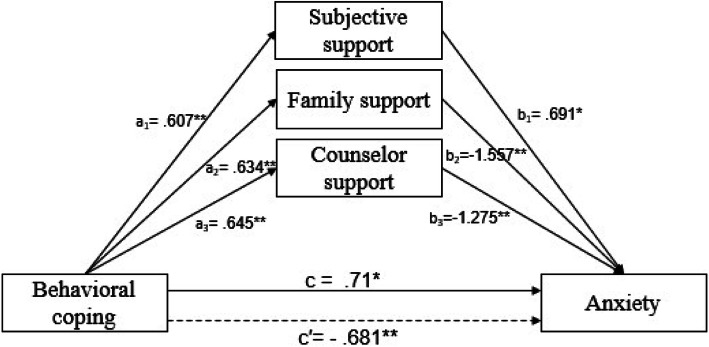
The mediating role of social support between cognitive coping and anxiety was evaluated first (see Fig. 2 and Table 3). In the direct effect model, before adding social support, cognitive coping negatively affected anxiety (c = − 0.715, p = 0.001). After the addition of social support, the indirect effect in the social support and anxiety pathway was negative and significant (c′ = − 1.572, p = 0.000), indicating that social support strengthened the negative effect of coping on anxiety. Furthermore, it is worth noting that subjective support positively and significantly affected anxiety (b1 = 0.691, p = 0.034). The path through the mediation of subjective support (point estimated = 0.28, 95% CI 0.011–0.62), family support (point estimated = − 0.533, 95% CI -0.799 – − 0.217), and counselor support (point estimated = − 0.604, 95% CI -0.923– − 0.419) were statistically significant, which supported H1.
Fig. 2.
Note: All the coefficients are standardized; dashed lines indicate the total effect from cognitive coping to anxiety; * p < .05, ** p < .01
Table 3.
The mediation analysis of social support in the relationship between cognitive coping, behavioral coping and anxiety
| Model pathways | β | SE | t | P | LLCI | ULCI | ||
| Direct effect X1 → Y | c | −.715 | .211 | −3.383 | .001 | −1.129 | −.301 | |
| X1 → M1 | a1 | .406 | .028 | 14.271 | .000 | 0.35 | 0.462 | |
| X1 → M2 | a2 | .342 | .021 | 15.948 | .000 | 0.3 | 0.384 | |
| X1 → M3 | a3 | .474 | .034 | 13.957 | .000 | 0.408 | 0.541 | |
| M1 → Y | b1 | .691 | .326 | 2.117 | .034 | 0.051 | 1.33 | |
| M2 → Y | b2 | −1.557 | .446 | −3.492 | 000 | −2.431 | −0.683 | |
| M3 → Y | b3 | −1.275 | .142 | −8.951 | .000 | −1.554 | −0.996 | |
| Total indirect effect X1 → Y | c′ | −1.572 | .208 | −7.564 | .000 | −1.98 | −1.165 | |
| Effect | Boot SE |
Boot LLCI |
Boot ULCI |
Z | p | |||
| Indirect effect | X1 → M1 → Y | a1 × b1 | 0.28 | .163 | 0.011 | 0.62 | 1.724 | .085 |
| X1 → M2 → Y | a2 × b2 | −0.533 | .178 | −0.799 | −0.217 | −2.991 | .003 | |
| X1 → M3 → Y | a3 × b3 | −0.604 | .12 | −0.923 | −0.419 | −5.047 | .000 | |
| Model pathways | β | SE | t | P | LLCI | ULCI | ||
| Direct effect X2 → Y | c | .71 | .283 | 2.507 | .012 | 0.155 | 1.264 | |
| X2 → M1 | a1 | 0.607 | .036 | 16.915 | .000 | 0.537 | 0.678 | |
| X2 → M2 | a2 | .634 | .027 | 23.394 | .000 | 0.581 | 0.687 | |
| X2 → M3 | a3 | .645 | .043 | 15.058 | .000 | 0.561 | 0.73 | |
| M1 → Y | b1 | .691 | .326 | 2.117 | .034 | 0.051 | 1.33 | |
| M2 → Y | b2 | −1.557 | .446 | −3.492 | 000 | −2.431 | −0 .683 | |
| M3 → Y | b3 | −1.275 | .142 | −8.951 | .000 | −1.554 | - 0.996 | |
| Total indirect effect X2 → Y | c′ | −.681 | .262 | −2.595 | .010 | −1.195 | - 0.167 | |
| Effect | Boot SE |
Boot LLCI |
Boot ULCI |
Z | p | |||
| Indirect effect | X2 → M1 → Y | a1 × b1 | 0.42 | .23 | 0.016 | 0. 944 | 1.827 | .068 |
| X2 → M2 → Y | a2 × b2 | −0.987 | . 328 | −1.557 | − 0.383 | −3.013 | .003 | |
| X2 → M3 → Y | a3 × b3 | −0.823 | . 117 | −1.064 | −0.608 | −7.005 | .000 | |
Note: N = 2640. Number of bootstrap samples for bias-corrected bootstrap confidence intervals: 5000
Level of confidence for all confidence intervals: 95%. The top half is the results of the cognitive coping model, and the bottom half is the results of the behavioral coping model. LLCI lower level of the 95% confidence interval; ULCI upper level of the 95% confidence interval. X1 cognitive coping, X2 behavioral coping, M1 subjective support, M2 family support, M3 counselor support, Y anxiety
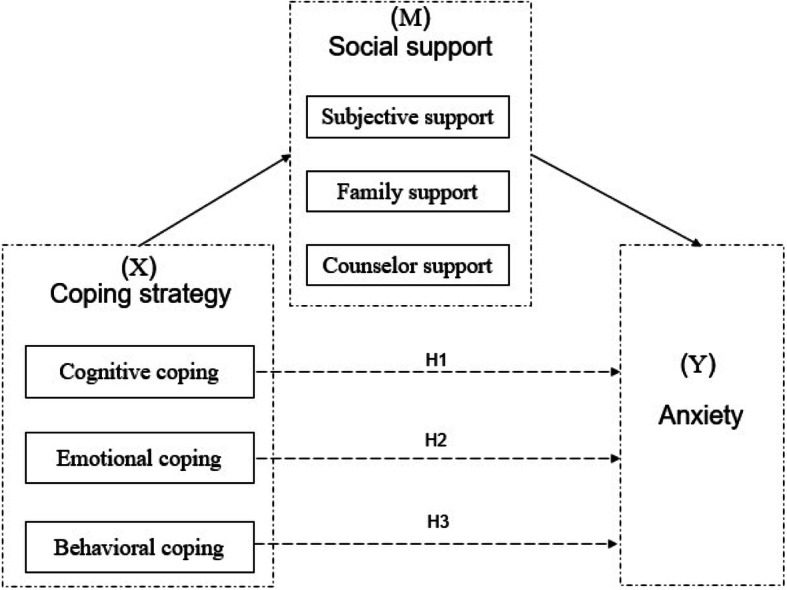
The mediating role of social support between behavioral coping and anxiety was then tested. As shown in Fig. 3 and Table 3, the total indirect effect (c′ = − 0.681, SE = 0.262, 95% CI -1.195 – − 0.167) of behavioral coping on anxiety was significant. The path through mediation of subjective support (point estimate =0.42; 95% CI 0.016–0.944), family support (point estimate = − 0.987; 95% CI -1.557 – − 0.383), and counselor support (point estimate = − 0.823; 95% CI -1.064 – − 0.608) were all statistically significant. Herein, the mediating effects of social support between behavioral coping and anxiety were significant at all social levels, which supported H3. The test also revealed that the positive effect of behavioral coping on anxiety could be reversed by the addition of social support, and then could negatively predict anxiety.
Fig. 3.
Note: All the coefficients are standardized; dashed lines indicate the total effect from behavioral coping to anxiety; * p < .05, ** p < .01
However, the mediation analysis of social support between emotional coping and anxiety indicates that the path through the mediation of subjective support (point estimate = 0.001; 95% CI - 0.023 – 0.017), family support (point estimate = − 0.001; 95% CI -0.035 – 0.032), and counselor support (point estimate = − 0.035; 95% CI -0.095 – 0.002) were all statistically insignificant, which did not support H2.
Discussion
This study was conducted on a sample of Chinese college students to investigate the relationship between coping, social support, and anxiety during the COVID-19 pandemic. Two research questions and three hypotheses were proposed. The levels of Chinese college students’ coping strategies, social support, and anxiety were described, and a model of the relationship between coping strategies, social support, and anxiety was developed. Accordingly, some meaningful findings and implications were also drawn as follows.
First, this study found that the levels of cognitive coping, behavioral coping, and social support for Chinese college students were high while those of emotional coping were considerably lower. The finding of high cognitive coping is consistent with the finding that more than 90% of the Chinese public kept updating pandemic information [5]. However, this is not the case in 2009 H1N1 influenza survey, in which community awareness and perception of risk were not high [31]. What matters most is that college students are willing to follow the arrangement of the university and government and behave properly to prevent infection. The attached survey of this study showed that 97.05% of the college students supported the Chinese government’s strict lockdown measures, and the supporting rate of the closure of schools was 97.88%. The timely and transparent dissemination of scientific preventive information issued by the government and responsible university administrators, and efficient mechanism of countermeasures throughout the country have played dominant roles in guiding the students [25]. The high levels of social support are not consistent with the U.S. young-adult-sampled study demonstrating low perceived family support during the initial weeks of the pandemic [32]. It is possible that family cohesion, social networking, and ethnic identity serve as protective factors for mental status [33]. Behaviorally, the public is well-informed of the significance of the epidemic and strictly abides by hygiene guidance toward handwashing, mask wearing and social distancing [34]. Moreover, Chinese students’ innate and strong sense of solidarity and patriotism, and their unified trust in government are more likely to be exhibited when they confront crucial emergencies. The low emotional coping of Chinese students demonstrated their worries about the infection. This outcome is in line with the previous study indicating that 56% of respondents in the U.S. poll showed deep concerns about the dissemination of the coronavirus and a quarter of participants felt more nervous than they did during the 2014 Ebola pandemic [4]. According to a study on Weibo users, positive emotions declined after the outbreak of the pandemic [35]. Negative emotional reactions are universal under alarming circumstances.
Furthermore, the mean anxiety scores of the students were found to be higher than the Chinese norm of the SAS in the usual time, but much lower than those self-isolated in central China during the epidemic [7]. Similarly, according to a Chinese online survey from January 31st to February 2nd, 2020, moderate to severe anxiety symptoms appeared in 28.8% of the population [5]. Likewise, previous studies during SARS indicated that severe health emergencies could initiate anxiety [36]. Chinese comparatively low levels of anxiety may result from ethnic identities found in the recent pandemic report, indicating that Asian American young adults tended to experience low levels of anxiety compared to White counterparts [32].
Second, Spearman’s correlation analyses found that anxiety was significantly and negatively related to coping and social support and that social support possessed the greatest links with anxiety among these associations. This verified the dominating role of social support in buffering anxiety, which left room for further mediation analysis. There was a mediating effect of social support on the relationship between cognitive coping, behavioral coping, and anxiety, while social support did not mediate emotional coping and anxiety. Moreover, the path through family support and counselor support had stronger mediating power than subjective support. The influence of cognitive coping and behavioral coping on anxiety was mediated by social support, supporting H1 and H3. In the first path, cognitive and behavioral coping positively affected social support. Individuals with a sufficient input of information may be fully aware of the current epidemic situation, delivering an encouraging emotion to their family or themselves [37]. The constructive effect of behavioral coping on social support is probably because a majority of individuals cared for the potential risk for their family being infected and would remind their families to adopt hygiene precautions, which consequently strengthen the links among families [5]. In the second path, social support affected anxiety, with the positive effect of subjective support and the negative effect of family and counselor support. The finding of the prevailing role of family support over counselor support is similar to the pandemic study of U.S. young adults, stating that social support from family other than support from partners or friends could diminish the severity of mental illness [32]. Family support demonstrated a promising function to relegate anxiety in that family members were more likely to share mutual empathy and then social support took into effect emotionally [38]. Compared to individuals, family caregivers played a unique role in better articulating and supporting the emotional, social, and health needs of family members [39]. Further, counseling support could also bolster up the links. The effectiveness of counseling social support in prohibiting anxiety during the social-distancing period is addressed by the previous finding that videoconference, an alternative to in-person counseling, took effect in alleviating anxiety [40]. However, the finding of a positive effect of subjective support on anxiety contradicted the previous finding that patients with a high level of subjective social support tended to perceive fewer life stressors [41]. Subjective support of college students, namely, individual resilience during the pandemic, was associated with high levels of anxiety, considering that they may be young adults and have less capacity to struggle with intense fear and anxiety. The finding that the mediating impact of social support did not exist in emotional coping and anxiety, which contradicted H2, could be probably inferred that emotional coping affected anxiety directly. This is consistent with a prior study on SARS, demonstrating that the symptoms of posttraumatic stress, anxiety, and depression appeared simultaneously in surviving patients [42].
Overall, the finding of the positive mediating effect of social support is of great value because it provides empirical evidence to emphasize the implementation of social support. Therefore, it is urgent to take measures to facilitate social support during the COVID-19 pandemic. For instance, regarding the information about infectious diseases, individuals should avail themselves of the suggestions of professional medical staff [43]. Second, students should communicate more frequently with families, relatives, and friends by phone or via the internet [44]. Under the circumstance of isolation, the use of online networks can augment social support, sustaining the mutual power of online social groups [45]. More importantly, it is indispensable to acquire the engagement of social workers and psychotherapists when individuals are confronted with mental burdens [25]. Third, since routine face-to-face psychological counseling is apparently unavailable during the epidemic period, remote counseling, such as structured letter therapy, e-mail, or other telemediated alternative means of communication, can be a feasible psychological intervention solution to diagnose and treat [46]. In addition, most Chinese university counseling centers could provide hotlines for psychological interventions and online platforms for psychoeducation, such as training programs and curricula, which can be easily accessible for students via WeChat and Tencent [44]. Under the university and community setting, free counseling training clinics and departments of student affairs should be advocated to provide adequate preparation for easing mental distress [47]. To highlight the significance of counselor support, university psychological professionals should harness digital technologies to conduct online counseling or life education during the pandemic, which may be perceived as innovative teaching approaches [25].
Limitations
However, there are some limitations to the current study. First, the samples were restricted to one university, which may be less generalizable to the entire population. Second, the cross-sectional design of this study could not reflect the long-term development of the samples, which needed supplementary findings from longitudinal research. In addition, all the questionnaires were self-reported, and the veracity of the result relied on the self-perception of the subjective and non-subjective methods should be applied. Last but not least, anxiety as a dependent variable involved in the survey could not reflect an intact picture of mental health, and it is necessary to further explore other factors indicating traumatization, such as depression, fear, despair, and irritability.
Conclusion
The findings in this empirical study are supposed to present a clue in psychological interventions and behavioral guidance on the current global crisis. First, this study detected high levels of cognitive coping, behavioral coping, and social support, explored low levels of anxiety and emotional coping for Chinese college students at the peak of the COVID-19 pandemic from January to February 2020. Second, anxiety was negatively associated with coping and social support. Third, social support played as a mediator in the relationships between cognitive coping, behavioral coping, and anxiety, with family support and counselor support exerting a stronger negative power against anxiety than subjective support.
In view of the implications proposed, there appear to be alternate strategies to ease anxiety. These findings may provide evidence for promoting social support, especially family support and counselor support, as facilitating sources to decrease anxiety in coping with the COVID-19 pandemic cognitively and behaviorally. Policymakers and school administrators should encourage meaningful communication between family members and activate effective counseling services to maintain positive mental health.
Supplementary Information
Additional file 1: Table S1. Items of Coping Strategy Questionnaire (CSQ).
Acknowledgements
The authors appreciate the study participants and the funder of this project.
Abbreviation
- COVID-19
Corona Virus Disease 2019
Authors’ contributions
YL conducted the conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, validation, wrote and edited the draft; JP administered and supervised the project, and reviewed the manuscript. All authors have read and approved the final version of the manuscript.
Funding
This study was funded by the key project of Physical and Psychological Health and Artistic Expression Studio and mental health education project, Shenzhen University (Grant number 19XSZ03; 21MSZX08). Also, it was supported by the Higher Education Fund of the Macao SAR Government (OTH-2002-03). The views expressed in this article are those of the authors and do not necessarily reflect the position of the Physical and Psychological Health and Artistic Expression Studio. The funder had no role in the decision to publish and preparation of the manuscript.
Availability of data and materials
The data that support the findings of this study are not currently publicly available due to institutional regulations protecting service member survey respondents but are available from the corresponding author on reasonable request (may require data use agreements to be developed).
Declarations
Ethics approval and consent to participate
This study was granted ethics approval by the Human Research Ethics Committee of City University of Macau (EA2001025). All the respondents granted permission for inclusion by reading the introductions for the investigation and provided voluntary responses.
Consent for publication
Not applicable.
Competing interests
The authors have no potential conflicts of interest to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yue XG, Shao XF, Li R, Crabbe M, Mi L, Hu S, Baker J, Liang G. Risk management analysis for novel coronavirus in Wuhan, China. J Risk Financial Manag. 2020;13(2):22. doi: 10.3390/jrfm13020022. [DOI] [Google Scholar]
- 2.Goyal K, Chauhan P, Chhikara K, Gupta P, Singh MP. Fear of COVID 2019: first suicidal case in India ! Asian J Psychiatr. 2020;49:101989. doi: 10.1016/j.ajp.2020.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim S, Pinkerton T, Ganesh N. Assessment of H1N1 questions and answers posted on the web. Am J Infect Control. 2020;40(3):211–217. doi: 10.1016/j.ajic.2011.03.028. [DOI] [PubMed] [Google Scholar]
- 4.Asmundson GJG, Taylor S. Coronaphobia: fear and the 2019-nCoV outbreak. J Anxiety Disord. 2020;70:102196. doi: 10.1016/j.janxdis.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1–25. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, du H, Chen T, Li R, Tan H, Kang L, Yao L, Huang M, Wang H, Wang G, Liu Z, Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.XiaoH, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the Coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit. 2020;26:e923921. 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed]
- 8.Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27(2):1–4. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kassam S. Understanding experiences of social support as coping resources among immigrant and refugee women with postpartum depression: an integrative literature review. Issues Ment Health Nurs. 2019;40(12):999–1011. doi: 10.1080/01612840.2019.1585493. [DOI] [PubMed] [Google Scholar]
- 10.Sun J, Harris K, Vazire S. Is well-being associated with the quantity and quality of social interactions? J Pers Soc Psychol. 2019;119(6):1478–1496. doi: 10.1037/pspp0000272. [DOI] [PubMed] [Google Scholar]
- 11.Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with Coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549. 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed]
- 12.Farris SG, Metrik J, Bonn-Miller MO, Kahler CW, Zvolensky MJ. Anxiety sensitivity and distress intolerance as predictors of cannabis dependence symptoms, problems, and craving: the mediating role of coping motives. J Stud Alcohol Drugs 2016; 77:889–897. doi:10.15288/jsad.2016.77.889 [DOI] [PMC free article] [PubMed]
- 13.Lavigne JV, Saps M, Bryant FB. Models of anxiety, depression, somatization, and coping as predictors of abdominal pain in a community sample of school-age children. J Pediatr Psychol. 2014;39(1):9–22. doi: 10.1093/jpepsy/jst060. [DOI] [PubMed] [Google Scholar]
- 14.Vinothkumar M, Arathi A, Joseph M, Nayana P, Jishma EJ, Sahana U. Coping, perceived stress, and job satisfaction among medical interns: the mediating effect of mindfulness. Ind Psychiatry J. 2016;25(2):195–201. doi: 10.4103/ipj.ipj_98_14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marshall H, Ryan P, Roberton D, Street J, Watson M. Pandemic influenza and community preparedness. Am J Public Health. 2009;99(S2):S365–S371. doi: 10.2105/ajph.2008.153056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- 17.Guo J, Feng XL, Wang XH, Van, IMH. Coping with COVID-19: exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. Int J Environ Res Public Health. 2020; 7(11). doi:10.3390/ijerph17113857 [DOI] [PMC free article] [PubMed]
- 18.Lazarus RS. Hope. An emotion and a vital coping resource against despair. Soc Res. 1999;66:653–678. [Google Scholar]
- 19.Taha S, Matheson K, Cronin T, Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: the case of the 2009 H1N1 pandemic. Br J Health Psychol. 2014;19(3):592–605. doi: 10.1111/bjhp.12058. [DOI] [PubMed] [Google Scholar]
- 20.Tan W, Hao F, McIntyre RS, Jiang L, Jiang X, Zhang L, et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immunity. 2020; doi:10.1016/j.bbi.2020.04.055 [DOI] [PMC free article] [PubMed]
- 21.Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC) Depression Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Groups at higher risk for severe illness. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html
- 23.Hado E, Friss FL. Amid the COVID-19 pandemic, meaningful communication between family caregivers and residents of long-term care facilities is imperative. J Aging Soc Policy. 2020;32(4-5):1–6. doi: 10.1080/08959420.2020.1765684. [DOI] [PubMed] [Google Scholar]
- 24.Zhou X. Psychological crisis interventions in Sichuan Province during the 2019 novel coronavirus outbreak. Psychiatry Res. 2020;286:112895. doi: 10.1016/j.psychres.2020.112895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang C, Cheng Z, Yue XG, McAleer M. Risk management of COVID-19 by universities in China. J Risk Financial Manag. 2020;13(2):36. doi: 10.3390/jrfm13020036. [DOI] [Google Scholar]
- 26.Xiao SY, Yang DS. The impact of social support on physical and mental health. Chin Ment Health J. 1987;1:183–187. [Google Scholar]
- 27.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 28.Hayes AF. An index and test of linear moderated mediation. Multivariate Behav Res. 2015;50(1):1–22. doi: 10.1080/00273171.2014.962683. [DOI] [PubMed] [Google Scholar]
- 29.Li XL, Li XL, ZL. Stress of SARS and psychological health: an investigation of response to SARS stress and anxiety level of nurse students in SARS prevalence period. J West China Medical. 2004;19:596–598. [Google Scholar]
- 30.Cohen J. Statistical power analysis for the behavioral sciences. New York: Academic Press; 1969. p. 38. [Google Scholar]
- 31.Marshall H, Tooher R, Collins J, Mensah F, Braunack-Mayer A, Street J, Ryan P. Awareness, anxiety, compliance: community perceptions and response to the threat and reality of an influenza pandemic. Am J Infect Control. 2012;40(3):270–272. doi: 10.1016/j.ajic.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 32.Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:113172. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leong F, Park YS, Kalibatseva Z. Disentangling immigrant status in mental health: psychological protective and risk factors among Latino and Asian American immigrants. Am J Orthopsychiatry. 2013;83(2):361–371. doi: 10.1111/ajop.12020. [DOI] [PubMed] [Google Scholar]
- 34.Zhang S, Wang Z, Chang R, Wang H, Xu C, Yu X, Tsamlag L, Dong Y, Wang H, Cai Y. COVID-19 containment: China provides important lessons for global response. Front Med. 2020;14(2):215–219. doi: 10.1007/s11684-020-0766-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a Study on active Weibo users. Int J Environ Res Public Health. 2020; 17(6). doi:10.3390/ijerph17062032 [DOI] [PMC free article] [PubMed]
- 36.Tam CWC, Pang EPF, Lam LCW, Chiu HFK. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med. 2004;34(7):1197–1204. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- 37.Carvalho PMM, Moreira MM, de Oliveira MNA, Landim JMM, Neto MLR. The psychiatric impact of the novel coronavirus outbreak. Psychiatry Res. 2020;286:112902. doi: 10.1016/j.psychres.2020.112902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang N, Xiao H, Wang W, Li S, Yan H, Wang Y. Effects of doctors' empathy abilities on the cellular immunity of patients with advanced prostate cancer treated by orchiectomy: the mediating role of patients' stigma, self-efficacy, and anxiety. Patient Prefer Adherence. 2018;12:1305–1314. doi: 10.2147/ppa.S166460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reinhard SC, Feinberg LF, Houser A, Choula R, Evans M. Valuing the invaluable: 2019 update. AARP Public Policy Institute. 2020. https://www.aarp.org/ppi/info-2015/valuing-the-invaluable-2015-update.html Accessed 25 June 2020.
- 40.Rees CS, Maclaine E. A systematic review of videoconference-delivered psychological treatment for anxiety disorders. Aust Psychol. 2015;50(4):259–264. doi: 10.1111/ap.12122. [DOI] [Google Scholar]
- 41.Lin J, Su Y, Lv X, Liu Q, Wang G, Wei J, Zhu G, Chen Q, Tian H, Zhang K, Wang X, Zhang N, Wang Y, Yu X, Si T. Perceived stressfulness mediates the effects of subjective social support and negative coping style on suicide risk in Chinese patients with major depressive disorder. J Affect Disord. 2020;265:32–38. doi: 10.1016/j.jad.2020.01.026. [DOI] [PubMed] [Google Scholar]
- 42.Wu KK, Chan SK, Ma TM. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) J Trauma Stress. 2005;18(1):39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xiao Y, Torok ME. Taking the right measures to control COVID-19. Lancet Infect Dis. 2020;20(5):523–524. doi: 10.1016/s1473-3099(20)30152-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhou X, Snoswell CL, Harding LE, Bambling M, Edirippulige S, Bai X, Smith AC. The role of telehealth in reducing the mental health burden from COVID-19. Telemed J E Health. 2020;26(4):377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
- 45.Utz S, Breuer J. The relationship between use of social network sites, online social support, and well-being: results from a six-wave longitudinal study. J Media Psychol. 2017;29(3):115–125. doi: 10.1027/1864-1105/a000222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xiao C. A novel approach of consultation on 2019 Novel Coronavirus (COVID-19)-related psychological and mental problems: structured letter therapy. Psychiatry Investig. 2020;17:175–176. doi: 10.30773/pi.2020.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhai Y, Du X. Mental health care for international Chinese students affected by the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e22. doi: 10.1016/s2215-0366(20)30089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Items of Coping Strategy Questionnaire (CSQ).
Data Availability Statement
The data that support the findings of this study are not currently publicly available due to institutional regulations protecting service member survey respondents but are available from the corresponding author on reasonable request (may require data use agreements to be developed).