Abstract
Purpose The treatment of acromioclavicular joint (ACJ) osteoarthritis during shoulder arthroscopy is a discussed topic. The aim of this scoping review is to report the current recommendations regarding the management of this disorder in patients undergoing surgery for rotator cuff tears.
Methods A scoping review was performed in Pubmed\Medline and Embase in March 2017, restricted to English language literature. The following keywords were used: (“rotator cuff tear” OR ” rotator cuff” OR “rotator cuff repair”) AND (“acromioclavicular joint arthritis” OR “ac joint arthritis” OR “ac joint” OR “acromioclavicular joint”). Inclusion criteria were randomized controlled trials, prospective cohort studies, retrospective trials, and therapeutic case series. Exclusion criteria were reviews, meta-analyses, and expert opinions.
Results Two retrospective studies and three randomized controlled trials were identified. Clinical studies reported results of 443 shoulders, with an average age of 60.48 years and a mean follow-up of 31.7 months. Many differences were found regarding the design of the studies, patient's selection, surgical procedures, and instrumental and clinical evaluations. No statistically significant differences were found in clinical outcome scores between patients that underwent rotator cuff repair in association with distal clavicular resection and patients with isolated rotator cuff repair.
Conclusion Results of this scoping review underline a lack of evidence-based recommendations about the management of ACJ osteoarthritis in association with arthroscopic rotator cuff repair. Surgical procedures such as distal clavicle resection (DCR) should be performed carefully in this cohort of patients. More prospective randomized studies are needed to reach a consensus about the correct surgical approach to DCR in patients with signs of ACJ osteoarthritis and rotator cuff tears.
Level of Evidence Level III.
Keywords: distal clavicle resection, rotator cuff repair, acromioclavicular joint osteoarthritis, shoulder
Introduction
Acromioclavicular joint (ACJ) osteoarthritis is common, with a radiological prevalence in the general population that can reach 90% in patients over 30 years old. 1 Disorders of ACJ are an usual cause of shoulder pain in primary care, affecting patients of all ages and levels of activity and are often described in patients with rotator cuff (RC) tears. 2 Common treatments in painful ACJ osteoarthritis are oral analgesics, such as acetaminophen, oral nonsteroidal anti-inflammatory drugs, topical analgesics, lidocaine patches, and cortisone articular injections. In patients that do not respond to these pharmacological treatments, a surgical option is considered and arthroscopic resection of the distal clavicle (DCR) is the most commonly performed technique. 3
Different studies have correlated ACJ osteoarthritis to the evolution of RC tears. 4 5 Some authors have described that these anatomical alterations, protruding downward below the level of the adjacent acromion, could be a cause of subacromial impingement with a focal pressure on RC. 6 7 8 9 10 Also, if the pathogenesis of RC lesions is multifactorial, the biomechanical consequences of osteoarthritic changes in ACJ are considered a relevant factor determining RC tears. 6 7
Theoretically, the inferior bony spurs in osteoarthritis of ACJ could cause not only a primary RC lesions but also a delayed tendon healing after RC repair (RCR). 11 Considering that a cuff re-tear could evolve into a massive RC tear and require more demanding surgeries, many authors have proposed the execution of DCR during the surgical procedure of RC tear repair, both in symptomatic and asymptomatic ACJ osteoarthritis. 12 13 Clinical consequences of DCR in these patients are actually discussed among orthopaedic surgeons, without definitive indications from medical literature. 4 14 15
The aim of this scoping review is to determine the clinical consequences of the association of DCR to cuff tears repair in patients with ACJ osteoarthritis.
Methods
A scoping review of the literature was performed using the Pubmed/MEDLINE and Embase databases to identify all studies reporting ACJ osteoarthritis in patients undergoing RCR. Authors followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews checklist for the scoping review. The following search string were used: ((rotator cuff tear[Title/Abstract]) OR (rotator cuff[Title/Abstract]) OR (rotator cuff repair[Title/Abstract])) AND ((acromioclavicular joint arthritis[Title/Abstract]) OR (ac joint arthritis[Title/Abstract]) OR (ac joint[Title/Abstract]) OR (acromioclavicular joint[Title/Abstract])) Medical Subject Headings terms were used for “rotator cuff,” and “acromioclavicular joint.” The search was performed on March 1, 2017, and was restricted to English language literature. A new literature search has been performed on May 5, 2020 with similar keywords and restrictions.
All randomized controlled trials and prospective cohort studies were included, as well as retrospective comparative trials and therapeutic case series. The main inclusion criteria were studies that evaluated patients with a full or partial thickness RC tear treated with arthroscopic repair and symptomatic or asymptomatic ACJ degenerative arthritis. Reviews, meta-analyses, expert opinions, and editorial pieces were excluded. Other exclusion criteria included animal studies, in vitro studies, and biomechanical studies on human cadaver specimens.
All abstracts from the searches were reviewed by two independent authors, who applied the study inclusion and exclusion criteria. In case of disagreement between reviewers (R.C., F.R.), consensus was obtained through discussion and, in case of persistent disagreement, a third reviewer (C.S.) was consulted and the study was included until full-text review could be performed. All full-text articles were then evaluated, and manually cross-referenced to ensure that all potential studies were included. Five studies were included in the review.
The level of evidence of each article was assessed using the 2003 Journal of Bone and Joint Surgery definitions for orthopaedic publications. 16
Information regarding author, data, and journal of publication, study design and level of evidence, patient demographics, modality for ACJ osteoarthritis diagnosis, treatment intervention, follow-up duration, preoperative and postoperative validated outcome measures, failure rates, and evidence of tendon healing, tear size, were extracted. Where possible, the compiled data from individual studies with the same outcome measures were pooled together. Mean weighted values were calculated for these outcomes and minimal clinically important difference has been used as a benchmark of the difference in the clinical postoperative performance. The differences among patients' inclusion criteria in the evaluated studies suggest caution regarding definitive clinical considerations on this aspect. Demographic data were compiled to assess weighted mean ages across groups.
Results
The flowchart describing the selection of included papers is reported Fig. 1 . After application of inclusion and exclusion criteria, two retrospective studies and three randomized controlled trial were identified. 11 17 18 19 20 Clinical studies reported results of 443 shoulders, with an average age of 60.48 years and a mean follow-up of 31.7 months ( Table 1 ). The evaluated outcomes included the Constant score, 21 the American Shoulder and Elbow Surgeons (ASES) 22 score, and the visual analog scale (VAS) that was reported, at least, in 4 of the 5 studies analyzed. All included studies compared isolated RCR with RCR associated to DCR. Many differences were found among preoperative patients' selection, RC tear classifications, associated surgical procedures, and postoperative follow-up. This relevant aspect made difficult to compare clinical outcomes or pooling data of different cohort with a clear statistical relevance. For example, preoperative RC tears were classified in three studies, with different scales. Razmjou et al classified cuff lesions as “large or massive” (33% of patients) or “small or moderate” (67% of patients). 20 Oh et al classified RC lesions as small (< 1 cm, 6 patients), medium (1–3 cm, 17 patients), large (3–5 cm, 2 patients), massive (> 5 cm, 11 patients), or partial (3 patients). 19 Kim et al reported the mean tear size, comparing the two groups (27.2 ± 3.7 mm in group 1 and 24.7 ± 3.1 mm in group 2). 18 The two others studies did not report information about preoperative RC tears size. 17 18 The analyzed studies used different ACJ osteoarthritis classifications: the Collin's system by Razmjou et al, the Stein magnetic resonance imaging (MRI) classification by Kim et al (only patients with a grade 4 were included), and the Cook palpatory tenderness scale by Park et al. 11 18 20 Only two studies, Oh et al and Kim et al, had a comparable population of asymptomatic ACJ osteoarthritis patients, randomized in two groups, the first of DCR and RCR and the second only RCR. 18 19 Acromioplasty was performed in 95% of patients with DCR in Razmjou et al study and 63% of the control group. 20 Kim et al performed a double row fixation in all RCRs, while all the other surgeons performed a single row repair. 18 A lidocaine test was completed only in the study of Park et al, while other papers only included clinical assessment of pain in this district. 11 Postoperative radiological outcomes and re-tear rate were evaluated by Oh et al and Park et al: Oh et al analyzed radiological outcomes using ultrasonography, computed tomography arthrography, MRI, and weighted stress radiography; Park et al performed a MRI 6 months postoperatively and at final follow-up. 18 Results on tendon healing are reported by Oh et al and Park et al. If Oh et al described the percentage of repaired cuffs healed at follow-up (77% with DCR; 74% without DCR), Park et al reported the percentage of re-tear at follow-up, comparing patients with and without DCR (9.5% vs. 15.3%). No statistical differences were found between the groups ( p = 0.95 in the first study, p = 0.678 in the second study), with comparable outcomes on tendon healing and reoperation rate at final follow-up in both the reports. 18 19 Notably, the group of Oh et al patients were asymptomatic for AC pathology before surgery while in the population of Park et al patients reported specific symptoms related to ACJ. 18 19
Fig. 1.
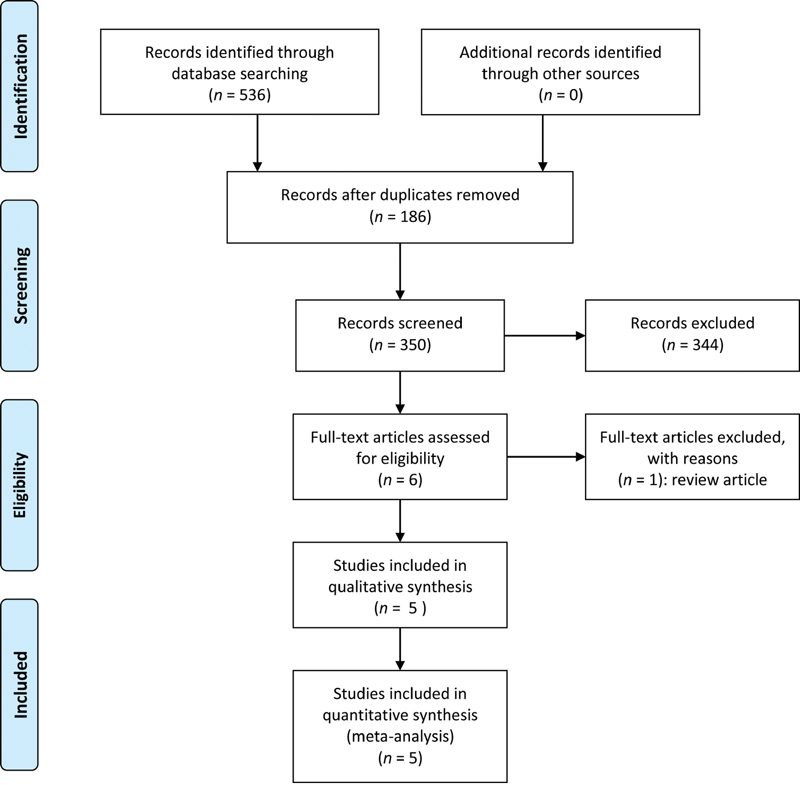
Flowchart of the literature review.
Table 1. Studies included in the review.
| Authors | Year | Study design | Level of evidence | No. shoulders | Sex no. (male/female) |
Age (y) mean ± SD |
Final follow-up (mo) mean ± SD |
|---|---|---|---|---|---|---|---|
| Razmjou et al (Knee Surg Sports Traumatol Arthrosc) | 2015 | Retrospective outcome study | II | 184 | 112/72 | 62 ± 9 | 24 |
| Park et al (Am J Sports Med) | 2015 | Randomized controlled trial | I | 58 (47 analyzed) | 9/38 | 62.6 ± 9.31 | 44.45 |
| 61.7 ± 6.12 | |||||||
| Oh et al (Am J Sports Med) | 2014 | Randomized controlled trial | I | 78 | 44/34 | 63.6 ± 6.5 | 29.2 |
| 64.0 ± 7.5 | |||||||
| Błasiak et al (Pol Orthop Traumatol) | 2013 | Retrospective outcome study | III | 40 | 43/17 | 53.10 ± 13.60 | 54.4 ± 6.4 |
| Kim et al (Arch Orthop Trauma Surg) | 2011 | Randomized controlled trial | II | 83 | 40/43 | 59.8 ± 5.2 | 31.7 |
| 55.2 ± 6.1 |
Abbreviation: SD, standard deviation.
Note: Year of publication, study design, level of evidence, and patients information are described.
Considering the minimal clinically important difference for Constant score (10.4 points), the overall analysis of the reported data showed a relevant increase in the mean Constant score after surgery for both groups (RCR: + 29.7 points; RCR + DCR: + 39.2 points). 23 On the contrary, the difference in the postoperative results between the two groups did not appear significant (Δ: 6.54 points). As reported in Table 2 , similar results have been found for the VAS and the ASES scores. 24 25
Table 2. Clinical results in RCR and RCR + DCR groups.
| Increase in post-operative results | Difference in post-operative results between the two group | Minimal clinically important difference | ||
|---|---|---|---|---|
| RCR | RCR + DRC | |||
| Constant | 29.7 | 39.2 | 6.5 | 10.4 |
| VAS | –5.3 | –5.9 | –0.4 | 1.4 |
| ASES | 36.4 | 38.5 | 1.7 | from 12 to 17 |
Abbreviations: ASES, American Shoulder and Elbow Surgeons Score; DCR, distal clavicle resection; RCR, rotator cuff repair; VAS, Visual Analogue Scale.
Some differences were found regarding clinical scores used for measuring clinical outcomes, and the most utilized were Constant, VAS, and ASES scores ( Table 3 ). These scores were used differently among the groups, and this aspect could be considered another bias that makes it difficult to compare outcomes of different studies.
Table 3. Clinical outcomes evaluated in the included studies.
| Authors | Year | Study groups | No. subjects (%) |
Outcomes |
|---|---|---|---|---|
| Razmjou et al (Knee Surg Sports Traumatol Arthrosc) | 2015 | DCR + RCR | 144 (78) | ASES, Constant scores, strength |
| RCR | 40 (22) | |||
| Park et al (Am J Sports Med) | 2015 | DCR + RCR | 26 (21 analyzed) | Clinical outcomes: VAS, ASES, Constant scores, ROM Radiological outcomes: MRI |
| RCR | 32 (26 analyzed) | |||
| Oh et al (Am J Sports Med) | 2014 | DCR + RCR | 39 | Clinical outcomes: VAS, ASES, Constant scores, ROM Radiological outcomes: Ultrasonography, computed tomography arthrography, MRI, weighted stress radiography |
| RCR | 39 | |||
| Błasiak et al (Pol Orthop Traumatol) | 2013 | DCR + RCR | 20 | VAS, Constant scores |
| RCR | 20 | |||
| Kim et al (Arch Orthop Trauma Surg) | 2011 | DCR + RCR | 31 | VAS, UCLA, ASES scores, tenderness on ACJ, and cross-body adduction test |
| RCR | 52 |
Abbreviations: ACJ, acromioclavicular joint; ASES, American Shoulder and Elbow Surgeons Score; DCR, distal clavicle resection; MRI, magnetic resonance imaging; RCR, rotator cuff repair; ROM, range of motion; SD, standard deviation; UCLA, The University of California at Los Angeles Shoulder Score; VAS, visual analog scale.
Discussion
The aim of this study was to perform a systematic review on the management of ACJ osteoarthritis in patients undergoing arthroscopic surgery for RC tears. Results of this literature review underline a lack of evidence-based recommendations about the management of ACJ in these patients, with low quality studies and a weak level of recommendations. Current literature does not clarify the influence of ACJ osteoarthritis on evolution of RC tears and the risk of evolution of the symptoms in patients with asymptomatic shoulder in patients undergoing arthroscopic surgery. Osteoarthritis of the ACJ is a common source of shoulder pain and a proper diagnosis requires a thorough physical exam, plain-film radiograph, and, for a more accurate diagnosis, a local anesthetic injection. 26 Nevertheless, clinical relevance of radiographic signs of osteoarthritis is not clear, with some patients with well-defined degenerative imaging that do not report any pain in this district. The clinical evolution of this condition is discussed, without definitive conclusions, in a recent study regarding asymptomatic ACJ osteoarthritis diagnosed with MRI. 27 Patients included in this study were followed for 7 years to evaluate the progression of this pathology; the authors observed that asymptomatic acromioclavicular osteoarthritis remained asymptomatic in 83% of cases, 7% turned better, and 10% turned worse. 27 The relevance of subacromial decompression on evolution of ACJ osteoarthritis is also an interesting aspect. Some authors examined the differences in the reoperation rate on the ACJ after arthroscopic subacromial decompression with and without concomitant ACJ surgery. Authors concluded that violation of the ACJ during the initial surgery by coplaning or DCR did not alter the reoperation rate due to ACJ symptoms. 28
Focusing on the results of this review, in one study, clinical symptoms were not clearly reported. 20 Oh et al found comparable results in nonsymptomatic patients undergoing lateral clavicle resection plus RCR and patients treated with only RCR. 19 Similar results, but in patients with symptomatic ACJ osteoarthritis previously examined with a lidocaine test, were found by Park et al in a prospective randomized study. 11 Razmjou et al report that mild ACJ osteoarthritis is an independent negative predictor of outcome at 2 years. This consideration supports the execution of DCR in patients with mild ACJ osteoarthritis. 20
This study presents two relevant limits: symptoms related to ACJ are not clearly described in part of the included studies and different classifications of RC tears are used in the included manuscripts. Moreover, the studies' design was different, with some authors comparing treatment of symptomatic and nonsymptomatic AC joint osteoarthritis. Błasiak et al described good results in patients undergoing DCR compared with a control group, but the study has a small number of patients and group population is not the same. 17 Another bias in this study, which should be considered, is the routine execution of acromioplasty in the study published by Oh et al. 19
In general, the surgical approach to ACJ osteoarthritis, when a RC tear repair is performed, is not well studied in recent international literature. Studies have many biases that limit data managements, making it difficult to extrapolate their application to clinical practice. Considering the quality of the analyzed papers, Park et al and Oh et al performed prospective randomized studies with high levels of evidence, ensuring the best quality on this topic. They reported no difference between operative and nonoperative management of ACJ osteophytes in RC tears. 18 19 Consistently with those results, this literature review draws similar conclusion and shows no clinical differences in the two approaches. Surgical procedures such as DCR should be performed carefully in this cohort of patients. Nevertheless, more prospective randomized studies are needed to reach a consensus about the correct surgical approach to DCR in patients with signs of ACJ osteoarthritis and RC tears.
Footnotes
Conflict of Interest P.R. declares consultation for Arthrex and Depuy (Johnson&Johnson), outside the submitted work. All other authors report no conflict of interest.
References
- 1.Stein B E, Wiater J M, Pfaff H C, Bigliani L U, Levine W N. Detection of acromioclavicular joint pathology in asymptomatic shoulders with magnetic resonance imaging. J Shoulder Elbow Surg. 2001;10(03):204–208. doi: 10.1067/mse.2001.113498. [DOI] [PubMed] [Google Scholar]
- 2.Cadogan A, McNair P, Laslett M, Hing W. Shoulder pain in primary care: diagnostic accuracy of clinical examination tests for non-traumatic acromioclavicular joint pain. BMC Musculoskelet Disord. 2013;14(01):156. doi: 10.1186/1471-2474-14-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gokkus K, Saylik M, Atmaca H, Sagtas E, Aydin A T. Limited distal clavicle excision of acromioclavicular joint osteoarthritis. Orthop Traumatol Surg Res. 2016;102(03):311–318. doi: 10.1016/j.otsr.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Petersson C J, Gentz C F. Ruptures of the supraspinatus tendon. The significance of distally pointing acromioclavicular osteophytes. Clin Orthop Relat Res. 1983;(174):143–148. [PubMed] [Google Scholar]
- 5.Watson M. The refractory painful arc syndrome. J Bone Joint Surg Br. 1978;60-B(04):544–546. doi: 10.1302/0301-620X.60B4.711806. [DOI] [PubMed] [Google Scholar]
- 6.Scott T P, Khan A Z, Petrigliano F A. Boston, MA: Springer US; 2015. Pathophysiology of Rotator Cuff Tears; pp. 1–22. [Google Scholar]
- 7.Fukuda H, Hamada K, Yamanaka K. Pathology and pathogenesis of bursal-side rotator cuff tears viewed from en bloc histologic sections. Clin Orthop Relat Res. 1990;(254):75–80. [PubMed] [Google Scholar]
- 8.Zanca P. Shoulder pain: involvement of the acromioclavicular joint. (Analysis of 1,000 cases) Am J Roentgenol Radium Ther Nucl Med. 1971;112(03):493–506. doi: 10.2214/ajr.112.3.493. [DOI] [PubMed] [Google Scholar]
- 9.Pennington R GC, Bottomley N J, Neen D, Brownlow H C. Radiological features of osteoarthritis of the acromiclavicular joint and its association with clinical symptoms. J Orthop Surg (Hong Kong) 2008;16(03):300–302. doi: 10.1177/230949900801600306. [DOI] [PubMed] [Google Scholar]
- 10.Morrison D, Bigliani L. The clinical significance of variations in acromial morphology. Orthop Trans. 1987;11(11):234. [Google Scholar]
- 11.Park Y B, Koh K H, Shon M S, Park Y E, Yoo J C. Arthroscopic distal clavicle resection in symptomatic acromioclavicular joint arthritis combined with rotator cuff tear: a prospective randomized trial. Am J Sports Med. 2015;43(04):985–990. doi: 10.1177/0363546514563911. [DOI] [PubMed] [Google Scholar]
- 12.Mahakkanukrauh P, Surin P. Prevalence of osteophytes associated with the acromion and acromioclavicular joint. Clin Anat. 2003;16(06):506–510. doi: 10.1002/ca.10182. [DOI] [PubMed] [Google Scholar]
- 13.Paribelli G, Boschi S, Randelli P, Compagnoni R, Leonardi F, Cassarino A M. Clinical outcome of latissimus dorsi tendon transfer and partial cuff repair in irreparable postero-superior rotator cuff tear. Musculoskelet Surg. 2015;99(02):127–132. doi: 10.1007/s12306-015-0353-4. [DOI] [PubMed] [Google Scholar]
- 14.Duindam N, Kuiper J WP, Hoozemans M JM, Burger B J. Comparison between open and arthroscopic procedures for lateral clavicle resection. Int Orthop. 2014;38(04):783–789. doi: 10.1007/s00264-013-2161-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cuomo F, Kummer F J, Zuckerman J D, Lyon T, Blair B, Olsen T. The influence of acromioclavicular joint morphology on rotator cuff tears. J Shoulder Elbow Surg. 1998;7(06):555–559. doi: 10.1016/s1058-2746(98)90000-3. [DOI] [PubMed] [Google Scholar]
- 16.Wright J G, Swiontkowski M F, Heckman J D. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(01):1–3. [PubMed] [Google Scholar]
- 17.Błasiak A, Mojżesz M, Brzóska R, Solecki W, Binkowska A. Results of arthroscopic treatment of rotator cuff tear with the resection of symptomatic acromioclavicular joint with degenerative changes. Pol Orthop Traumatol. 2013;78:229–234. [PubMed] [Google Scholar]
- 18.Kim J, Chung J, Ok H. Asymptomatic acromioclavicular joint arthritis in arthroscopic rotator cuff tendon repair: a prospective randomized comparison study. Arch Orthop Trauma Surg. 2011;131(03):363–369. doi: 10.1007/s00402-010-1216-y. [DOI] [PubMed] [Google Scholar]
- 19.Oh J H, Kim J Y, Choi J H, Park S M. Is arthroscopic distal clavicle resection necessary for patients with radiological acromioclavicular joint arthritis and rotator cuff tears? A prospective randomized comparative study. Am J Sports Med. 2014;42(11):2567–2573. doi: 10.1177/0363546514547254. [DOI] [PubMed] [Google Scholar]
- 20.Razmjou H, ElMaraghy A, Dwyer T, Fournier-Gosselin S, Devereaux M, Holtby R. Outcome of distal clavicle resection in patients with acromioclavicular joint osteoarthritis and full-thickness rotator cuff tear. Knee Surg Sports Traumatol Arthrosc. 2015;23(02):585–590. doi: 10.1007/s00167-014-3114-2. [DOI] [PubMed] [Google Scholar]
- 21.Constant C R, Murley A H. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160–164. [PubMed] [Google Scholar]
- 22.Richards R R, An K-N, Bigliani L U. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(06):347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 23.Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Aärimaa V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elbow Surg. 2013;22(12):1650–1655. doi: 10.1016/j.jse.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 24.Tashjian R Z, Deloach J, Porucznik C A, Powell A P. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009;18(06):927–932. doi: 10.1016/j.jse.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 25.Tashjian R Z, Deloach J, Green A, Porucznik C A, Powell A P. Minimal clinically important differences in ASES and simple shoulder test scores after nonoperative treatment of rotator cuff disease. J Bone Joint Surg Am. 2010;92(02):296–303. doi: 10.2106/JBJS.H.01296. [DOI] [PubMed] [Google Scholar]
- 26.Buttaci C J, Stitik T P, Yonclas P P, Foye P M. Osteoarthritis of the acromioclavicular joint: a review of anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil. 2004;83(10):791–797. doi: 10.1097/01.phm.0000140804.46346.93. [DOI] [PubMed] [Google Scholar]
- 27.Frigg A, Song D, Willi J, Freiburghaus A U, Grehn H. Seven-year course of asymptomatic acromioclavicular osteoarthritis diagnosed by MRI. J Shoulder Elbow Surg. 2019;28(10):e344–e351. doi: 10.1016/j.jse.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 28.Kharrazi F D, Busfield B T, Khorshad D S. Acromioclavicular joint reoperation after arthroscopic subacromial decompression with and without concomitant acromioclavicular surgery. Arthroscopy. 2007;23(08):804–808. doi: 10.1016/j.arthro.2007.02.003. [DOI] [PubMed] [Google Scholar]


