Dear Editor
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel single-stranded RNA-enveloped virus primarily transmitted person-to-person by close contact through respiratory droplets and defined as the causal agent of Coronavirus Disease 2019 (COVID-19). To date, more than 100 million cases and 2.1 million deaths associated to the COVID-19 have been reported worldwide, but the impact of disease has been disproportionate in highly dense areas [1] and among vulnerable populations [2,3].
In this ecological study, we investigated the relationship between population density and COVID-19 estimates in a county-level analysis of Sergipe state, Northeast Brazil, a region with the largest concentration of highly vulnerable people in the country. Sergipe has an area of 21,925 km2, an estimated population of 2,318,822 inhabitants, and a population density of 105.8 inhabitants/km2. The Human Development Index (HDI) is 0.665 and the proportion of illiterate people and those living on per capita income of half minimum wage per month is 14.4% and 40.8%, respectively. The state is divided into 75 counties with population density by county ranging from 17.4 to 3140.6 inhabitants/km2 according to the Brazilian Institute of Geography and Statistics (IBGE, acronym in Portuguese).
COVID-19 estimates by county were extracted from the government's official bulletin until January 27, 2021, and population density using data from Brazilian official census. Counties were categorized into three population density strata: <50 inhabitants/km2 (low density), 50–99 inhabitants/km2 (moderate density), and ≥100 inhabitants/km2 (high density). In addition, population density was natural log-transformed to measure its the strength of association with COVID-19 estimates using the Spearman's Rank Correlation Coefficient (rs) as follows: rs = 0.0–0.19 (very weak), rs = 0.20–0.39 (weak), rs = 0.40–0.59 (moderate), rs = 0.60–0.79 (strong), and rs = 0.80–1.0 (very strong). The significance level was set at 5%. Analyzes were performed by using JASP software version 0.13 (JASP Team, Amsterdam, Netherlands).
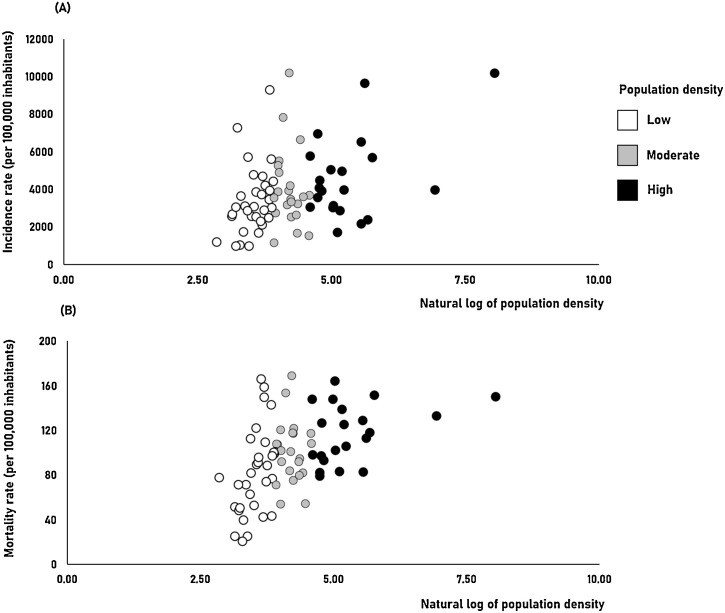
Until January 27, 2021, SARS-CoV-2 has infected 134,556 patients and resulted in 2755 deaths in Sergipe. Currently, the state has the highest incidence (5854 cases per 100,000 inhabitants) and mortality (120 deaths per 100,000 inhabitants) rates of COVID-19 in the Northeast region. Incidence and mortality rates by county ranged from 965 to 10,130 cases of COVID-19 per 100,000 inhabitants and 21 to 169 deaths per 100,000 inhabitants, respectively. Thirty-two (42.7%) counties had less than 50 inhabitants/km2, 22 (29.8%) between 50–99 inhabitants/km2, and 21 (28.0%) a population density ≥ 100 inhabitants/km2. We found a positive correlation between population density and incidence (rs = 0.326, CI 95% 0.106–0.514, p = 0.005; effect size = weak) (Fig. 1 A) and mortality (rs = 0.518, CI 95% 0.329–0.666, p < 0.001; effect size = moderate) (Fig. 1B) rates for COVID-19.
Fig. 1.
Scatter plots of county-level analysis for relationship between population density and incidence (A) and mortality (B) rates of COVID-19.
The impact of population density on emerging infectious diseases has been rarely studied. Exploratory analyzes on the relationship between population demographics – including density – and COVID-19 estimates are important for the planning of policy and medical resources [4]. Population density has been used as a surrogate measure of social distancing capacity and studies [1,[4], [5], [6], [7], [8]] have shown that SARS-CoV-2 transmission is potentially more likely to occur among cities with higher population densities.
Brazil is a country of continental dimensions that presents regional social inequalities with millions of people living in highly dense communities, with precarious housing conditions and poor sanitation, which increase the risk of SARS-CoV-2 infection and poor outcomes of COVID-19. Despite our results are similar to the found in Japan [4], India [5], Italy [6], United States [1,7], and China [8], differences in the strength of association between population density and COVID-19 estimates may be influenced by other factors including socioeconomic indicators, adherence to social distancing policies, health care infrastructure, and degree of connectivity [9]. Population density has been found as a potential indicator of infection spread which suggests that in densely populated areas more stringent policies or implementations of distancing may be considered [7].
Our results are limited to group-level analysis and did not include other population parameters, but this study provided important information about the relationship between population density and COVID-19 estimates in a county-level analysis. These findings reinforce that strategies and planning for COVID-19 should be based on the differences in population parameters between counties in the same region.
Funding
No funding sources.
Competing interests
None declared.
Ethical approval
Not required.
Acknowledgments
The author is grateful to CAPES and FAPITEC (EDITAL CAPES/FAPITEC N˚ 11/2016 - PROEF) for the financial support.
References
- 1.Chen K., Li Z. The spread rate of SARS-CoV-2 is strongly associated with population density. J Travel Med. 2020;27:taaa186. doi: 10.1093/jtm/taaa186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martins-Filho P.R., de Souza Araújo A.A., Quintans-Júnior L.J., Santos V.S. COVID-19 fatality rates related to social inequality in Northeast Brazil: a neighbourhood-level analysis. J Travel Med. 2020;27:taaa128. doi: 10.1093/jtm/taaa128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martins-Filho P.R., Araújo B.C.L., Sposato K.B., Araújo AA de S., Quintans-Júnior L.J., Santos V.S. Racial disparities in COVID-19-related deaths in Brazil: black lives matter? J Epidemiol. 2021;31:239–240. doi: 10.2188/jea.JE20200589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kodera S., Rashed E.A., Hirata A. Correlation between COVID-19 morbidity and mortality rates in Japan and local population density, temperature, and absolute humidity. Int J Environ Res Public Health. 2020;17:5477. doi: 10.3390/ijerph17155477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhadra A., Mukherjee A., Sarkar K. Impact of population density on Covid-19 infected and mortality rate in India. Model Earth Syst Environ. 2020:1–7. doi: 10.1007/s40808-020-00984-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ilardi A., Chieffi S., Iavarone A., Ilardi C.R. SARS-CoV-2 in Italy: population density correlates with morbidity and mortality. Jpn J Infect Dis. 2021;74:61–64. doi: 10.7883/yoken.JJID.2020.200. [DOI] [PubMed] [Google Scholar]
- 7.Wong D.W.S., Li Y. Spreading of COVID-19: density matters. PLoS One. 2020;15 doi: 10.1371/journal.pone.0242398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen D., Hu C., Su F., Song Q., Wang Z. Exposure to SARS-CoV-2 in a high transmission setting increases the risk of severe COVID-19 compared with exposure to a low transmission setting? J Travel Med. 2020;27:taaa094. doi: 10.1093/jtm/taaa094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hamidi S., Sabouri S., Ewing R. Does density aggravate the COVID-19 pandemic? J Am Plann Assoc. 2020;86:495–509. doi: 10.1080/01944363.2020.1777891. [DOI] [Google Scholar]