Abstract
Background
Herd immunity through vaccination is the target of public health interventions against COVID-19, but vaccine refusal or hesitancy is one of the global threats that make achievement of community immunity very difficult. The aim of this study was to determine negative attitudes and intentions and their predictors towards COVID-19 vaccines.
Methods
This was cross sectional survey, that targeted 1011 Egyptians aged 18 years and above, from 24 governorates, during the period from 7 January 2021, to 30 March 2021. Using a convenient sampling technique, the data were collected through an online self-administered, structured questionnaire, which was composed of two main sections, that involved sociodemographic and health related factors, intentions, and attitudes towards COVID-19 vaccines.
Results
The mean age of participants was 29.35 ± 10.78 years, (16.6 %) of them had COVID-19. (54%) of respondents, reported COVID-19 vaccine hesitancy and 21% of them reported vaccine non-acceptance while (27.1%) of participants preferred receiving Pfizer vaccine. (51.8%) of the respondents expressed strong worries about unforeseen effects of the vaccine which was associated with younger age groups, married, females, absence of history of allergy to food or drugs, perceived susceptibility to COVID 19 and never having flu vaccination. Vaccine hesitancy was associated with female sex, urban residence, university/post graduate, married respondents, those never had flu vaccine, and those did not have confidence in the ability of health system to control the epidemic. Female sex, urban residence and having concerns about unforeseen effects were predictors for vaccine hesitancy and vaccine non-acceptance.
Conclusion
The observed high level of worries about unforeseen effects of COVID-19 vaccines and widespread vaccine hesitancy amongst Egyptians and its predictors should be considered during implementation of public health intervention campaigns to change negative attitudes and improve acceptance and uptake of COVID-19 vaccines in Egypt.
Keywords: Negative attitude, Intentions, COVID-19 vaccine, Egyptians
Introduction
Herd immunity is the goal of the effective response of the public health interventions to coronavirus disease 2019 (COVID-19) pandemic. It is described as acquired community immunity in a sufficiently large proportion of the population, which is estimated to be 67% for COVID-19. If a large proportion of the population becomes infected, this would place immense pressure on healthcare infrastructure and could lead to up to 30 million deaths globally [1].
Widespread vaccination is important for COVID-19 transmission control [2]. However, despite the pandemic, there is a global distrust of vaccine safety and efficacy [3].
Planned behavior theory explains whether or not a person will adhere to a particular behavior. Regarding COVID-19 vaccine, it is dependent on three major factors: the individual’s general attitudes toward vaccination in general and the COVID-19 vaccine in particular, the attitudes of ‘significant others’ toward the vaccine, and the perceived behavioral control, which refers to the perceived difficulty in doing the behavior [4].
In April 2020-, during the early stages of the pandemic, about one-quarter of adults in seven European countries, including the United Kingdom, were unaware or unable to receive a COVID-19 vaccine when it became available [5]. Concerns regarding the vaccine novelty and efficacy, as well as possible side effects, have been reported as reasons for not receiving the COVID-19 vaccine up to date [5,6]. According to a study explored the relationship between general vaccine attitudes and the intention to vaccinate against COVID-19, the belief in vaccine safety was the strongest predictor [7].
There is a critical need for a more updated understanding of public attitudes towards COVID 19 vaccines and associated factors in the light of the COVID-19 pandemic to tailor appropriate public health messages or actions. This research aimed to determine the prevalence of attitudes and intentions towards the COVID 19 vaccine and detect negative attitudes and intentions predictors.
Exploring the predictors of intentions towards the COVID-19 vaccine could help governments and policymakers identify and adopt appropriate interventions to eliminate worries and hesitancy and increase confidence in the vaccine.
Subjects and methods
Study design and participants
This web-based cross-sectional survey targeted Egyptian citizens aged 18 years and above all over the country. The study was conducted during the period from January to March 2021. The exclusion criteria included refusal to participate in the study, age below 18 years old, illiterate or internet non-user and Egyptian adult citizens living abroad during the study period.
Sample size
Sample size was estimated according to the following equation:
n = Z2 P (1 − P)/d2 [8].
Due to limited data about the prevalence of COVID-19 anti-vaccine attitudes in Egypt, we assumed that 50% of the respondents would have anti-COVID-19 vaccine attitudes, 95% confidence level, and 80% power of the study, so the calculated sample size was 385 participants, and the sample was increased to be more representative.
Data collection
The data was collected using a convenient sampling method through an online self-administered, structured questionnaire. Participants completed and submitted the questionnaire after approval on participation in the study (informed consent). The questionnaire was distributed through the most famous platforms in Egypt (Facebook and What’s App groups) or private Facebook & What’s App accounts. To increase the response rate, continuous follow-up & reminder messages were used. Pilot testing was done and involved 20 participants in order to ensure readability & clarity, and results of the pilot were not included in the study.
The data collection tool
The questionnaire was composed of 3 main sections as follows;
-
1)Socio-demographic and health-related factors;
-
•Age, sex, residence, educational level, occupation, marital status, smoking history and history of chronic diseases.
-
•Current perceived state of health, as determined by a single item derived from the General Health Perception Scale [9].
-
•Perceived susceptibility to potential adverse effects of the medication was assessed by a single item based on the Perceived Sensitivity to Medicines scale [10].
-
•Prior Influenza vaccination behavior was assessed by one item.
-
•Confidence in the Egyptian government to handle the pandemic.
-
•Perceptions of governmental efforts to raise COVID 19 vaccine awareness.
-
•
-
2)Intentions and attitudes towards COVID-19 vaccination.
-
•Intentions towards the COVID-19 vaccine were based on one item. Response options were vaccine acceptance, vaccine hesitancy, and vaccine non-acceptance.
-
•Vaccine attitudes:
-
•
Using 12-items based on the Vaccination Attitudes Examination (VAX) Scale [11], general negative attitudes towards COVID 19 vaccines were assessed. Participants were asked to focus on COVID 19 specifically.
On a six-point scale, responses were scored from 1 (strongly agree) to 6 (strongly disagree). Four subscales were calculated; skepticism of vaccine benefit, fears regarding unexpected future consequences, commercial profiteering concerns, and natural immunity preference.
Each of the four subscales was classified as having a high level of negative attitudes toward COVID-19 vaccines (score of 5–6 on a scale of 1–6), an intermediate level (score of 3–4), or a low level (score of 1–2).
-
•Type of vaccine preferred.
-
•
Statistical analysis
The data were analyzed using SPSS version 25 and significance level (p < .05). Qualitative data were presented as frequency and percent, while quantitative data were presented as mean ± SD. Chi2 test was used to test the association between categorical variables. Pearson's correlation coefficient (r) was used to test the association between two continuous variables. Multinomial logistic regression analysis was used to identify the predictors.
Ethical issues
The study methodology was approved by the Ethical Committee of Scientific Research, Faculty of Medicine, Benha University, No (RC.3.1.2021). All participants provided electronic informed written consent after clarification of the goals, data confidentiality, voluntary participation, and withdrawal.
Results
One thousand eleven Egyptian citizens were recruited from 24 governorates and submitted the survey. Studied participants’ socio-demographic characteristics were shown in Table 1 . More than half of the participants (58.8%) were males. The mean age was 29.35 ± 10.78 years, and 55.5% of them were from the age group 18–28. More than half (54.3%) were from urban areas. The majority of them were university graduates. About one third (30.8%) worked in the governmental sector, 50% were single, and 86.6% were nonsmoker. The majority of the study participants did not have any chronic disease (77.5%) or any type of medication hypersensitivity (63.3%), and about 30.4%, 38.7% and 18.2% perceived their health as good, very good and excellent, respectively.
Table 1.
Distribution of socio-demographic, health characteristics and attitudes towards the vaccine.
| Variables | Frequency | % | |
|---|---|---|---|
| Age 29.35 ± 10.78 | 18–28 | 557 | 55.1 |
| 29–39 | 280 | 27.7 | |
| 40–50 | 131 | 13.0 | |
| 50+ | 43 | 4.3 | |
| Gender | Male | 417 | 41.2 |
| Female | 594 | 58.8 | |
| Residence | Urban | 549 | 54.3 |
| Rural | 462 | 45.7 | |
| Education | Read and write/primary education | 47 | 4.6 |
| Preparatory education | 22 | 2.2 | |
| Secondary education | 232 | 22.9 | |
| University education | 500 | 49.5 | |
| Post graduate | 210 | 20.8 | |
| Occupation | Student | 418 | 41.3 |
| Not working | 24 | 2.4 | |
| House wife | 83 | 8.2 | |
| Private sector | 81 | 8.0 | |
| Governmental sector | 311 | 30.8 | |
| Others | 72 | 7.1 | |
| Marital status | Single | 505 | 50.0 |
| Married | 479 | 47.4 | |
| Others (divorced–separated–widowed) | 27 | 2.7 | |
| Smoking history | Current smoker | 88 | 8.7 |
| Ex-smoker | 47 | 4.6 | |
| Non smoker | 876 | 86.6 | |
| Chronic disease | No chronic disease | 784 | 77.5 |
| Asthma or respiratory disease | 55 | 5.4 | |
| Cardiac disease | 14 | 1.4 | |
| Hypertension | 27 | 2.7 | |
| Diabetes | 27 | 2.7 | |
| Cancer | 3 | .3 | |
| Kidney or liver disease | 5 | .5 | |
| Autoimmune disease | 15 | 1.5 | |
| Overweight/obesity | 38 | 3.8 | |
| Perceived health status | Poor health | 22 | 2.2 |
| Medium | 107 | 10.6 | |
| Good | 307 | 30.4 | |
| Very good | 391 | 38.7 | |
| Excellent | 184 | 18.2 |
About two-thirds (65.6%) of participants had never received the flu vaccine. In this study, 16.6 % of the study participants had COVID-19, while 37.4% had a family member who had COVID-19. The majority of the study participants thought that the Ministry of Health did not provide adequate information about COVID-19 vaccines. Regarding intentions to receive the COVID19 vaccine, 54% of respondents were hesitant to take the vaccine, 21% were unwilling to take the vaccine, and only 25% were willing to take the vaccine. About 27.1% of the study participant preferred the Pfizer vaccine compared with 6.9%, 4.5%, who preferred the Chinese and AstraZeneca vaccine, respectively (Table 2 ).
Table 2.
Distribution of socio-demographic, health characteristics and attitudes towards the vaccine.
| Variables | Frequency | % | |
|---|---|---|---|
| Hypersensitivity to drugs or foods | Yes | 120 | 11.9 |
| No | 640 | 63.3 | |
| Don’t know | 245 | 24.2 | |
| Have had flu vaccination | Never | 663 | 65.6 |
| Yes (long time ago) | 225 | 22.3 | |
| Yes last year | 32 | 3.2 | |
| Yes this year | 61 | 6.0 | |
| Yes every year | 30 | 3.0 | |
| Had COVID 19 | Yes | 168 | 16.6 |
| No | 601 | 59.4 | |
| Don’t know | 242 | 23.9 | |
| Family member had COVID 19 | Yes | 378 | 37.4 |
| No | 489 | 48.4 | |
| Don’t know | 144 | 14.2 | |
| Does ministry of health provide adequate information about COVID-19 vaccines? | Yes | 224 | 22.2 |
| No | 584 | 57.8 | |
| Don’t know | 203 | 20.1 | |
| Intentions towards COVID19 vaccine | Vaccine acceptance | 259 | 25.6 |
| Vaccine hesitancy | 543 | 53.7 | |
| Vaccine non-acceptance | 209 | 20.7 | |
| COVID 19 vaccine preferences | Chinese vaccine | 70 | 6.9 |
| Pfizer vaccine | 274 | 27.1 | |
| Moderna vaccine | 14 | 1.4 | |
| AstraZeneca | 46 | 4.5 | |
| Russian vaccine | 20 | 2.0 | |
| don’t know | 587 | 58.1 | |
| Mistrust of vaccine benefit mean ± SD (2.98 ± 1.01) | Low | 205 | 20.3 |
| Moderate | 682 | 67.5 | |
| High | 124 | 12.3 | |
| Worries about unforeseen side effects mean ± SD (4.02 ± 1.30) | Low | 80 | 7.9 |
| Moderate | 407 | 40.3 | |
| High | 524 | 51.8 | |
| Concerns about commercial profiteering mean ± SD (3.15 ± 1.13) | Low | 189 | 18.7 |
| Moderate | 607 | 60.0 | |
| High | 215 | 21.3 | |
| Preference of natural immunity mean ± SD (3.26 ± 1.08) | Low | 154 | 15.2 |
| Moderate | 633 | 62.6 | |
| High | 224 | 22.2 |
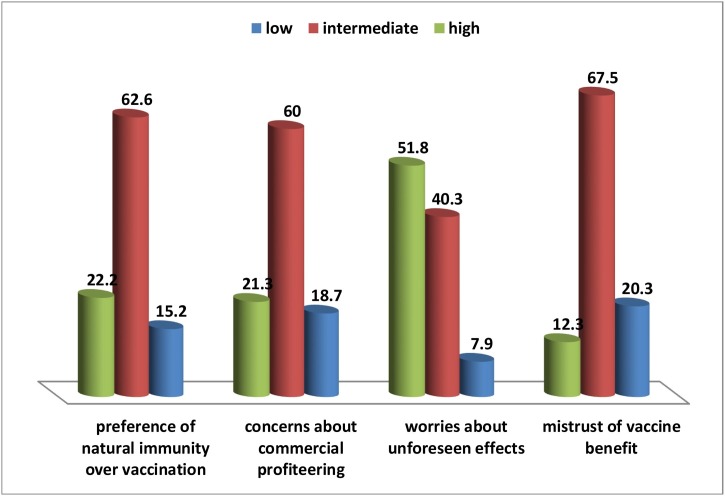
Overall, only 12.3% of respondents revealed high levels of mistrust regarding vaccines benefits and 67.5% reported moderate mistrust, and 20.3% showed low mistrust with a mean score of (2.98 ± 1.01). Half of the study participant (51.8%) showed strong worries about unexpected vaccine effects, while 40.3% showed moderate worries with a mean score of (4.02 ± 1.30). About one-quarter (21.3%) and two thirds (60%) expressed high and moderate concerns, respectively, regarding commercial profiteering with a mean score of (3.15 ± 1.13). About one-quarter (22.2%) revealed a high natural immunity preference, while 62.6 % showed a moderate preference for natural immunity (Table 2 & Fig. 1 ).
Fig. 1.
Participants negative attitudes towards COVID-19 vaccines.
The association between socio-demographic characteristics, health-related factors and worries about unforeseen effects of the vaccines is demonstrated in Table 3 . There were a statistically significant associations between worries level and young age group (p = .006), female gender (p = .034), marriage (p < .001), urban residence (p < .001), university/post-graduate education level (p < .001), working in the governmental sector (p = .016), also with the absence of allergic history to foods or drugs (p = .004), perceived susceptibility to COVID 19 infection (p value <.001), perceived excellent health status (p < .001) and never received flu vaccination (p = .039) (Table 3).
Table 3.
Association between socio-demographic, health related factors and worries about unforeseen effects of the vaccines.
| Sociodemographic and health variables |
Level of worries about unforeseen side effects |
p | |||
|---|---|---|---|---|---|
| Low | Intermediate | High | |||
| Age groups | 18–28 | 59(5.8%) | 220(21.8%) | 278(27.5%) | .006** |
| 29–39 | 13(1.3%) | 116(11.5%) | 151(14.9%) | ||
| 40–50 | 6(.6%) | 60(5.9%) | 65(6.4%) | ||
| 50+ | 2(.2%) | 11(1.1%) | 30(.3%) | ||
| Sex | Male | 42(4.2%) | 175(17.3%) | 200(19.8%) | .034* |
| Female | 38(3.8%) | 232(22.9%) | 324(32.0%) | ||
| Residence | Urban | 30(3.0%) | 200(19.8%) | 319(31.6%) | .000** |
| Rural | 50(4.9%) | 207(20.5%) | 205(20.3%) | ||
| Education | Read and write/primary | 7(.7%) | 4(.4%) | 36(3.6%) | .000** |
| Preparatory/secondary | 32(3.2%) | 85(8.4%) | 137(13.6%) | ||
| University/post graduate | 41(4.1%) | 318(31.5%) | 351(34.7%) | ||
| occupation | Student | 49(4.8%) | 177(17.5%) | 192(19.0%) | .000** |
| Not working/house wife | 7(.7%) | 25(2.5%) | 75(7.4%) | ||
| Private sector | 9(.9%) | 38(3.8%) | 34(3.4%) | ||
| Governmental sector | 12(1.2%) | 144(14.2%) | 155(15.3%) | ||
| Others | 3(.3%) | 23(2.3%) | 68(6.7%) | ||
| Marital status | Single | 52(5.1%) | 212(21.0%) | 241(23.8%) | .016** |
| Married | 26(2.6%) | 187(18.5%) | 266(26.3%) | ||
| Others (separated–divorced–widowed) | 2(.2%) | 8(.8%) | 17(1.7%) | ||
| Hypersensitivity to drugs or foods | Yes | 19(1.9%) | 44(4.4%) | 57(5.6%) | .004** |
| No | 44(4.4%) | 275(27.2%) | 327(32.3%) | ||
| Don’t know | 17(1.7%) | 88(8.7%) | 140(13.8%) | ||
| Perceived susceptibility to COVID 19 infection | Yes | 39(3.9%) | 258(25.5%) | 404(40.0%) | .000** |
| No | 21(2.1%) | 33(3.3%) | 28(2.8%) | ||
| Don’t know | 20(2.0%) | 116(11.5%) | 92(9.1%) | ||
| Had flu vaccination | Never | 46(4.5%) | 268(26.5%) | 349(34.5%) | .039* |
| Long time ago | 28(2.8%) | 92(9.1%) | 137(13.6%) | ||
| Recently | 6(.6%) | 47(4.6%) | 38(3.8%) | ||
| Perceived health status | Poor to moderate | 6(.6%) | 33(3.3%) | 90(8.9%) | .000** |
| Good to very good | 21(2.1%) | 117(11.6%) | 169(16.7%) | ||
| Excellent | 53(5.2%) | 257(25.4%) | 265(26.2%) | ||
*Significant at the .05 level (2-tailed).
**Significant at the .01 level (2-tailed).
Regarding the association between intentions towards COVID 19 vaccination and some socio-demographic and health-related factors, there was a statistically significant associations between vaccine hesitancy and female gender (p < .001), urban residence (p < .001), university/post-graduate education level (p = .041), working in the governmental sector (p < .001), marriage (p = .009), never received flu vaccine (p = .029), perceived excellent health status (p = .004), belief that The Egyptian Ministry of Health did not provide adequate information about COVID-19 vaccines (p < .001),and lake of confidence that the health system could have the ability to control the epidemic (p < .001) (Table 4 ).
Table 4.
Association between socio-demographic, health related factors and intentions towards COVID 19 vaccination.
| Sociodemographic and health variables | Vaccine acceptance | Vaccine hesitancy | Vaccine non-acceptance | p | |
|---|---|---|---|---|---|
| Age groups | 18–28 | 151(14.9%) | 293(29.0%) | 113 (11.2%) | .225 |
| 29–39 | 61(6.0%) | 155(15.3%) | 64(6.3%) | ||
| 40–50 | 34(3.4%) | 68(6.7%) | 29(2.9%) | ||
| 50+ | 13(1.3%) | 27(2.7%) | 3(.3%) | ||
| Sex | Male | 134(13.3%) | 203(20.1%) | 80(7.9%) | .000** |
| Female | 125(12.4%) | 340(33.6%) | 129(12.8%) | ||
| Residence | Urban | 105(10.4%) | 309(30.6%) | 135(13.4%) | .000** |
| Rural | 154(15.2%) | 234(23.1%) | 74(7.3%) | ||
| Education | Read and write/primary | 6(.6%) | 33(3.3%) | 8(.8%) | .041 |
| Preparatory/secondary | 69(6.8%) | 143(14.1%) | 42(4.2%) | ||
| University/post graduate | 184(18.2%) | 367(36.3%) | 159(15.7%) | ||
| Occupation | Student | 129(12.8%) | 205(20.3%) | 84(8.3%) | .000** |
| Not working/house wife | 16(1.6%) | 73(7.2%) | 18(1.8%) | ||
| Private sector | 18(1.8%) | 39(3.9%) | 24(2.4%) | ||
| Governmental sector | 81((.8%) | 161(15.9%) | 69(6.8%) | ||
| Others | 15(1.5%) | 65(6.4%) | 14(1.4%) | ||
| Marital status | Single | 140(13.8%) | 258(25.5%) | 107(10.6%) | .009** |
| Married | 115(11.4%) | 274(27.1%) | 90(8.9%) | ||
| Others (separated–divorced–widowed) | 4(.4%) | 11(1.1%) | 12(1.2%) | ||
| Smoking | Current smoker | 21(2.1%) | 50(4.9%) | 17(1.7%) | .069* |
| Ex-smoker | 20(2.0%) | 22(2.2%) | 5(.5%) | ||
| Non smoker | 218(21.6%) | 471(46.6%) | 187(18.5%) | ||
| Flu vaccination | Never | 163(16.1%) | 351(34.7%) | 149(14.7%) | .029* |
| Long time ago | 79(7.8%) | 140(13.8%) | 38(3.8%) | ||
| Recent | 17(1.7%) | 52(5.1%) | 22(2.2%) | ||
| Perceived health status | Poor to moderate | 22(2.2%) | 83(8.2%) | 24(2.4) | .004** |
| Good to very good | 68(6.7%) | 179(17.7%) | 60(5.9%) | ||
| Excellent | 169(16.7%) | 281(27.8%) | 125(12.4%) | ||
| Does ministry of health provide adequate information about COVID-19 vaccines? | Yes | 93(9.2%) | 97(7.6%) | 34(3.4%) | .000** |
| No | 105(10.4%) | 335(33.1%) | 144(14.2%) | ||
| Don’t know | 61(6.0%) | 111(11.0%) | 31(3.1%) | ||
| Confidence in health system ability to control the epidemic | Disagree | 104 (10.3%) | 245(24.2%) | 126(12.5%) | .000** |
| Neutral | 52(5.1%) | 191(18.9%) | 40(4.0%) | ||
| Agree | 103(10.2%) | 107(10.6%) | 43(4.3%) | ||
Significant at the .01 level (2-tailed).
Significant at the .05 level (2-tailed).
Regarding the association between intentions towards COVID 19 vaccination and attitudes towards vaccines, vaccine hesitancy had highly significant associations with intermediate mistrust level of vaccine benefit (p < .001), high worries about unforeseen effects (p < .001), intermediate concerns about commercial profiteering (p < .001), and intermediate preference of natural immunity (p < .001) (Table 5 ).
Table 5.
Association between intentions towards COVID 19 vaccination and attitudes towards vaccines.
| Variables | Vaccine acceptance | Vaccine hesitancy | Vaccine non-acceptance | p |
|---|---|---|---|---|
| Mistrust of vaccine benefit | .000** | |||
| Low | 24(2.4%) | 76(7.5%) | 105(10.4%) | |
| Intermediate | 160(15.8%) | 425(24.0%) | 97(9.6%) | |
| High | 7(.7%) | 42(4.2%) | 75(7.4%) | |
| Worries about unforeseen effects | .000** | |||
| Low | 35(3.5%) | 32(3.2%) | 13(1.3%) | |
| Intermediate | 122(12.1%) | 211(20.9%) | 74(7.3%) | |
| High | 102(10.1%) | 300(29.7%) | 122(12.1%) | |
| Concerns about commercial profiteering | .000** | |||
| Low | 83(8.2%) | 76(7.5%) | 30(3.0%) | |
| Intermediate | 144(14.2%) | 343(33.9%) | 120(11.9%) | |
| High | 32(3.2%) | 124(12.3%) | 59(5.8%) | |
| Preference of natural immunity over vaccination | .000** | |||
| Low | 56(5.5%) | 74(7.3%) | 24(2.4%) | |
| Intermediate | 167(16.5%) | 341(33.7%) | 125(12.4%) | |
| High | 36(3.6%) | 128(12.7%) | 60(5.9%) | |
*Significant at the .05 level (2-tailed).
**Significant at the .01 level (2-tailed).
Multinomial logistic regression analysis for the predictors of the intentions towards COVID 19 vaccination showed that female gender, urban residence and having concerns about unforeseen effects were significant independent predictors for vaccine hesitancy and vaccine non-acceptance (p = .001, .001, .001, .000, .033, .000, respectively) (Table 6 ).
Table 6.
Multinomial logistic regression for the predictors of the intentions towards COVID 19 vaccination.
| Intentions | B | S.E. | Wald | Sig. | Exp(B) | 95% CI | ||
|---|---|---|---|---|---|---|---|---|
| Vaccine hesitancy | Concerns about unforeseen effects | .197 | .060 | 10.869 | .001* | 1.218 | (1.083–1.370) | |
| Sex | Male | −.511 | .158 | 10.496 | .001* | .600 | (.440–.817) | |
| Female (ref) | . | . | . | . | . | |||
| Residence | Urban | .535 | .165 | 10.529 | .001* | 1.707 | (1.236–2.358) | |
| Rural (ref) | . | . | . | . | . | |||
| Marital status | Single | .045 | .621 | .005 | .942 | 1.046 | (.310– 3.534) | |
| Married | .021 | .617 | .001 | .973 | 1.021 | (.305–3.421) | ||
| Others (ref) | . | . | . | . | . | |||
| Education | Read & write/primary | .837 | .484 | 2.994 | .084 | 2.310 | (.895–5.963) | |
| Preparatory/secondary | .086 | .183 | .224 | .636 | 1.090 | (.762–1.559) | ||
| University/post (ref) | . | . | . | . | . | |||
| Chronic disease | No | .084 | .208 | .162 | .687 | 1.088 | (.723–1.637) | |
| Yes (ref) | . | . | . | . | . | |||
| Perceived health | Poor/moderate | .462 | .287 | 2.591 | .107 | 1.588 | (.904–2.789) | |
| Good/very good | .415 | .180 | 5.293 | .021* | 1.514 | (1.063–2.156) | ||
| Excellent (ref) | . | . | . | . | . | |||
| Vaccine non-acceptance | ||||||||
| Concerns about unforeseen effects | .329 | .076 | 18.998 | .000* | 1.390 | (1.199–1.612) | ||
| Sex | Male | −.419 | .197 | 4.540 | .033* | .657 | (.447–.967) | |
| Female (ref) | . | . | . | . | . | |||
| Residence | Urban | .931 | .206 | 20.418 | .000* | 2.538 | (1.695–3.802) | |
| Rural (ref) | . | . | . | . | . | |||
| Marital status | Single | −.814 | .622 | 1.713 | .191 | .443 | (.131–1.499) | |
| Married | −1.203 | .618 | 3.786 | .052* | .300 | (.089–1.009) | ||
| Others (ref) | . | . | . | . | . | |||
| Education | Read& write/primary | .278 | .594 | .219 | .640 | 1.321 | (.412–4.234) | |
| Preparatory/secondary | −.265 | .237 | 1.257 | .262 | .767 | (.482–1.220) | ||
| University/post (ref) | . | . | . | . | . | |||
| Chronic dis | No | −.105 | .252 | .175 | .676 | .900 | (.549–1.475) | |
| Yes (ref) | . | . | . | . | . | |||
| Perceived health | Poor/moderate | .037 | .358 | .011 | .917 | 1.038 | (.514–2.096) | |
| Good/very good health | .160 | .225 | .503 | .478 | 1.173 | (.755–1.823) | ||
| Excellent (ref) | . | . | . | . | . |
The reference category is willing to take the vaccine.
Significance at <.05 (B represents the estimated regression coefficients for the explanatory variables, with the standard error (S.E.) given. The Wald statistics is the ratio of B to S.E. of the regression coefficient squared. The significance of each explanatory variable (Sig.) is given by the p-value. Exp (B) is the predicted change in odds for a unit increase in the explanatory variable).
Discussion
Vaccination is one of the most important inventions in the field of public health in the 21st century. Vaccination hesitancy one of the world top ten health challenges. The high level of vaccine hesitancy emphasizes the fact that the availability of COVID-19 vaccines is not the only issue.
The current study found that the most often negative attitude towards COVID-19 vaccines was the concern about unforeseen effects of the vaccine in the future, more than half of participants (51.8%) expressed a high level of worries about unforeseen consequences of the vaccine, which is in line with a US study [12]. Additionally, a Chinese study discovered that 48% of respondents delayed vaccination until vaccine safety was confirmed [13], indicating their concerns about vaccine safety. The fast pace of vaccine production and some scientific and health professionals’ skepticism can raise doubts about the COVID-19 vaccine [14].
According to the study, half of the participants expressed concerns about the vaccine safety once it became accessible, as demonstrated by their worries about potential side effects. This is in line with Pogue et al., who stated that most participants (63%) in the United States of America expressed concerns about the COVID-19 vaccines side effects [15].
Additionally, the majority of respondents who picked preferred vaccine favored the US vaccine. This comes in accordance with a global study [15] and another one in the USA [16].
Regarding intentions to receive the COVID19 vaccine, 54% of respondents reported vaccine hesitancy, 21% reported vaccine non-acceptance, and only 25% decided on vaccine acceptance. An African study on 15 African countries found that intentions to accept a COVID-19 vaccine ranged from higher acceptance reported in Ethiopia and Niger to the lowest acceptance found in Senegal and DR Congo [17].
In the current study, the high level of vaccine hesitancy could be explained by the fact that more than half of the participants had concerns about future unexpected side effects of the vaccine and doubts about vaccine benefit, in addition to the lack of information about available COVID-19 vaccines and characteristics of everyone, which support the emergence of rumors and misleading information, creating negative attitudes, hesitancy, or even refusal of the vaccines. This in line with a study in Portugal, which found that more than one third (35%) of the participants would take the vaccine immediately, more than half (56%) would wait before taking the vaccine, and only 9% would not take the vaccine [18]. Also, this is consistent with an American study which reported that more than half of the participants (57.6%) intended to take the vaccine, about one-third (31.6%) were hesitant, and only 10.8% reported they did not intend to take the vaccine [19]. Also, a study by Tylor et al, stated that about one-quarter of Americans (25%) and Canadians (20%) would not receive the SARS-CoV2 vaccine. Due to the extent of non-adherence, achieving herd immunity would be extremely difficult [20]. In contrast, a Saudi study reported that 64.7% of participants agreed to get the COVID-19 vaccine, 7.0% refused it, and 28.2% were hesitant about it. Additionally, Cordina's studies [21] demonstrated promising findings in terms of vaccine uptake willingness, with more than 50% of participants expressed a clear desire to take the vaccine, one-third (32.6%) expressed uncertainty, and only 15.6% expressed opposition, at the time when knowledge about the safety and effectiveness of the vaccine was scarce. Additionally, a European study recorded a willingness to take the vaccine in about three-quarters (73.9%). Another UK Oxford study reported 71.7%. In a global survey of 19 countries, 71.5% reported a willingness to take the vaccine, and in the United States, about half (52%) were quite likely, and one-quarters (27%) were very likely to take the vaccine [5,22].
The results of the current study indicated that Egyptians have a high degree of COVID-19 vaccine hesitancy, which is greater than that observed in previous research [5,13,[23], [24], [25]]. The differences between countries regarding COVID-19 vaccine acceptance, non-acceptance or hesitancy may be attributed to differences in socio-demographic characteristics, health characteristics, human behavior, the availability of knowledge about vaccines, control of rumors and misinformation, confidence in the health system, type of vaccines available, worries about side effects, and level of trust in vaccine benefits.
In this study, female gender was significantly associated with concerns about unforeseen effects of the COVID-19 vaccine and hesitancy towards COVID-19 vaccination. This comes in accordance with another study by Ref. [26], who reported that males were more likely to accept the vaccine. Furthermore, an African research on 15 African countries reported that women were more skeptical towards the COVID-19 vaccine [17]. This can be attributed to females’ fears of the vaccine unforeseen and long term side effects on pregnancy and future generations, and a considerable portion of females might be pregnant, lactating or planning to be pregnant in the near future. In contrast, other studies reported higher acceptance of the vaccine among females [27,28].
The current study results revealed vaccine hesitancy was higher among university/post-graduate education level, those working in the governmental sector, married respondents, and those never vaccinated with the flu vaccine. This finding agrees with another study, which reported that not receiving influenza vaccine in the prior year were among factors that were associated with vaccine hesitancy [19]. On the other side, a Saudi study reported that the future COVID-19 vaccine acceptance was relatively high among married participants with a post-graduate degree or higher (68.8%) and governmental employees (68.9%) [28].
Higher odds for COVID-19 hesitancy were associated with the following factors: the presence of concerns about unforeseen effects, lower education level, and poor/moderate perceived health status. This could be explained by the fact that people who perceive their health status as poor are more fearful about health deterioration and vaccination adverse effects which is the major concern of the participants of this study. Participants with lower education level may have limited access to information about COVID-19 vaccines, so they are hesitant about it. In this study, more than one half of participants (58.1%) could not decide on the type of preferred COVID-19 vaccine because they did not have enough knowledge about its types.
Also, higher odds for vaccine non-acceptance were linked to the presence of concerns about unforeseen effects. This comes in accordance with an American/Canadian, which stated that vaccine non-acceptance was most strongly associated with a distrust of vaccine value and also with a fear of unexpected potential consequences. These attitudes would make the achievement of herd immunity difficult or even impossible [20].
In addition, higher odds for vaccine non-acceptance were observed among those who perceived their health as good/very good. This could be explained by the fact that they believe they are not at risk of illness and can fight the infection, hence not needing vaccination that may have adverse consequences.
Although, there are those who support the COVID-19 vaccine without doubts, others absolutely reject it, and in the middle, there is a third hesitated group. These individuals often postpone vaccination or accept it but are uncertain. According to sociological and psychological theories, it is easier for people to adjust their behaviors if they are within the 'latitude of acceptance' [29].
Conclusions
The study findings indicated a high level of mistrust and worries about unforeseen effects of COVID-19 vaccines. Widespread COVID-19 vaccine hesitancy was associated with female gender, urban residence and lower educational levels. Policy makers should consider these findings in planning and implementing public health intervention campaigns to change negative vaccine attitudes and increase the acceptance and uptake of COVID-19 vaccines in Egypt in order to achieve herd immunity and control the pandemic.
Limitations of the study
One of the limitations of this study is the convenient non-probability sampling method. Being on-line survey that involved only internet-users and missed the opportunity of exploring the attitudes of internet non-users.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
We have no conflict of interest.
Ethical approval
The study methodology was approved by the Ethical Committee of Scientific Research, Faculty of Medicine, Benha University, No (RC.3.1.2021). All participants provided electronic informed written consent after clarification of the goals, data confidentiality, voluntary participation, and withdrawal.
Authors contributions
The manuscript has been read and approved by all the authors, that the requirements for authorship have been met, and that each author has substantial contributions to each of the three components mentioned below:
Concept and design of study or acquisition of data or analysis and interpretation of data;
Drafting the article or revising it critically for important intellectual content; and
Final approval of the version to be published.
Acknowledgments
We would like to express our appreciation to dr/Eman E.Abd-Elatif, Mansoura University for her assistance in reviewing the research proposal. Also would like to thank all participating Egyptians for their precious time and cooperation.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jiph.2021.06.019.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Randolph H.E., Barreiro L.B. Herd immunity: understanding COVID-19. Immunity. 2020;52(May (5)):737–741. doi: 10.1016/j.immuni.2020.04.012. PMID: 32433946; PMCID: PMC7236739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altmann D.M., Douek D.C., Boyton R.J. What policy makers need to know about COVID-19 protective immunity. Lancet. 2020;395:1527–1529. doi: 10.1016/S0140-6736(20)30985-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Figueiredo A., Simas C., Karafillakis E., Paterson P., Larson H.J. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020 doi: 10.1016/S0140-6736(20)31558-0. published online September 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ajzen I. In: Action control: from cognition to behaviour. Kuhn J., Beckman J., editors. Springer Verlag; New York: 1985. From intentions to actions: a theory of planned behaviour. [Google Scholar]
- 5.Neumann-Böhme S., Varghese N.E., Sabat I. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21(7):977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sherman S.M., Smith L.E., Sim J., Amlôt R., Cutts M., Dasch H. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2020;(November):1–10. doi: 10.1080/21645515.2020.1846397. Epub ahead of print. PMID: 33242386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thunstrom L., Ashworth M., Finnoff D., Newbold S. 2020. Hesitancy towards a COVID-19 vaccine and prospects for herd immunity. Available at SSRN 3593098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daniel W.W. 7th edition. John Wiley & Sons; New York: 1999. Biostatistics: a foundation for analysis in the health sciences.www.wiley.com/college/daniel Available from: [Google Scholar]
- 9.Stewart A.L., Hays R.D., Ware J.E.J. In: Measuring functioning and well-being: the medical outcomes study approach. Stewart E.L., Ware J.E.J., editors. Duke University Press; Durham, NC: 1992. Health perceptions, energy/fatigue, and health distress measure; pp. 143–172. [Google Scholar]
- 10.Horne R., Faasse K., Cooper V., Diefenbach M.A., Leventhal H., Leventhal E. The perceived sensitivity to medicines (PSM) scale: an evaluation of validity and reliability. Br J Health Psychol. 2013;18(February (1)):18–30. doi: 10.1111/j.2044-8287.2012.02071.x. Epub 2012 Apr 23. PMID: 22524270. [DOI] [PubMed] [Google Scholar]
- 11.Martin L.R., Petrie K.J. Understanding the dimensions of antivaccination attitudes: the vaccination attitudes examination (VAX) scale. Ann Behav Med. 2017:652–660. doi: 10.1007/s12160-017-9888-y. [DOI] [PubMed] [Google Scholar]
- 12.Callaghan T., Moghtaderi A., Lueck J., Hotez P., Strych U., Dor A. Correlates and disparities of COVID-19 vaccine hesitancy. SSRN Electron J. 2020 doi: 10.2139/ssrn.366797. [DOI] [Google Scholar]
- 13.Wang J., Jing R., Lai X., Zhang H., Lyu Y., Knoll M.D. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. 2020;8:482. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chou W.-Y.S., Budenz A. Considering emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35:1718–1722. doi: 10.1080/10410236.2020.1838096. [DOI] [PubMed] [Google Scholar]
- 15.Mannan Kazi Abdul, Farhana Khandaker Mursheda. Knowledge, attitude and acceptance of a COVID-19 vaccine: a global cross-sectional study (December 7, 2020) Int Res J Bus Soc Sci. 2020;6(4) doi: 10.2139/ssrn.3763373. Available at SSRN: https://ssrn.com/abstract=3763373 or. [DOI] [Google Scholar]
- 16.Pogue K., Jensen J.L., Stancil C.K., Ferguson D.G., Hughes S.J., Mello E.J. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines (Basel) 2020;8(4) doi: 10.3390/vaccines8040582. Epub 2020/10/08. PubMed PMID: 33022917; PubMed Central PMCID: PMCPMC7711655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CDC Africa . 2021. COVID 19 vaccine perceptions: a 15 country study.https://africacdc.org/download/covid-19-vaccine-perceptions-a-15-country-study/ [Google Scholar]
- 18.Soares P., Rocha J.V., Moniz M., Gama A., Laires P.A., Pedro A.R. Factors associated with COVID-19 vaccine hesitancy. Vaccines (Basel) 2021;9(March (3)):300. doi: 10.3390/vaccines9030300. PMID: 33810131; PMCID: PMC8004673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes toward a potential SARS-CoV-2 vaccine : a survey of U.S. adults. Ann Intern Med. 2020;173(December (12)):964–973. doi: 10.7326/M20-3569. Epub 2020 Sep 4. PMID: 32886525; PMCID: PMC7505019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taylor S., Landry C.A., Paluszek M.M., Groenewoud R., Rachor G.S., Asmundson G.J.G. A proactive approach for managing COVID-19: the importance of understanding the motivational roots of vaccination hesitancy for SARS-CoV2. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.575950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cordina M., Lauri M.A., Lauri J. Attitudes towards COVID-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharm Pract. 2021;19(January–March (1)):2317. doi: 10.18549/PharmPract.2021.1.2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Commun Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harapan H., Wagner A.L., Yufika A., Winardi W., Anwar S., Gan A.K. Acceptance of a COVID-19 vaccine in Southeast Asia: a cross-sectional study in Indonesia. Front Public Health. 2020;8:381. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murphy J., Vallières F., Bentall R.P., Shevlin M., McBride O., Hartman T.K. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;29 doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38(September (42)):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. Epub 2020 Aug 20. PMID: 32863069; PMCID: PMC7440153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26(September) doi: 10.1016/j.eclinm.2020.100495. Epub 2020 Aug 12. PMID: 32838242; PMCID: PMC7423333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K. A global survey of potential acceptance of a COVID-19 vaccine [published correction appears in Nat Med. 2021 Jan 11] Nat Med. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al-Mohaithef M., PadhiB K. Determinants of covid-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. 2020;13:1657–1663. doi: 10.2147/JMDH.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crano W.D., Prisli R. Attitudes and persuasion. Annu Rev Psychol. 2006;57:345–374. doi: 10.1146/annurev.psych.57.102904.190034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.