Abstract
The choice of the most suitable surgical approach to the elbow forms the foundation of any successful elbow surgery. The surgical approach is based on the injury or pathology to be addressed and therefore specific anatomical details need to be considered. The surgeon must be comfortable with the bony, ligamentous and neurovascular anatomy of the elbow to consider and execute the best approach for each problem. This is an imperative to avoid iatrogenic injury.
This article provides a detailed analysis, valuable technical tips, advantages and disadvantages of the most common approaches to the elbow. The lateral approaches include the Kocher, Kaplan and Extensor Digitorum Communis (EDC) Split approaches, the medial approaches include the Hotchkiss, Flexor carpi ulnaris (FCU) splitting approach, the Taylor and Scham approach. The anterior approach includes the anterior neurovascular interval approach and the posterior approaches include the Olecranon osteotomy, triceps sparing, triceps reflecting approach and finally the Boyd interval approach. The text and illustrations will provide a structured overview for the practicing surgeon.
Keywords: Elbow approaches, Kocher approach, Kaplan approach, Olecranon osteotomy approach, Triceps on and triceps off approaches, Anterior approach
1. Introduction
The recent literature reports a growing recognition of complex injuries of the elbow and their respective anatomical correlates, such as capitellar fractures, anteromedial coronoid fractures, terrible triad injuries, posterolateral and posteromedial rotatory instability along with complex Monteggia fracture dislocations.
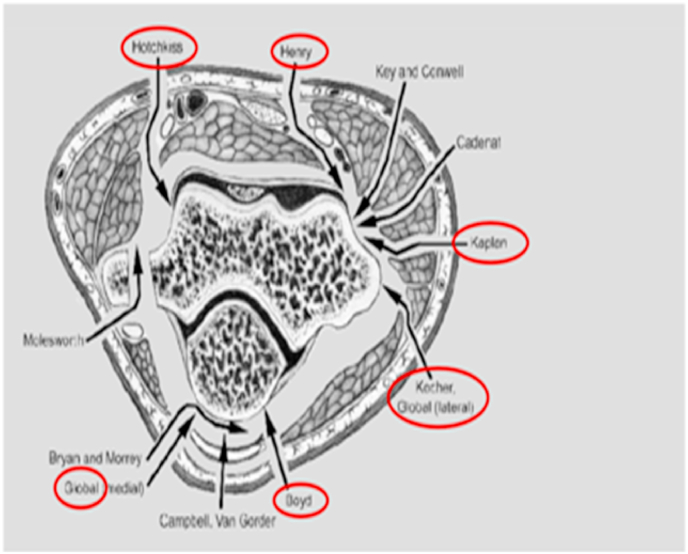
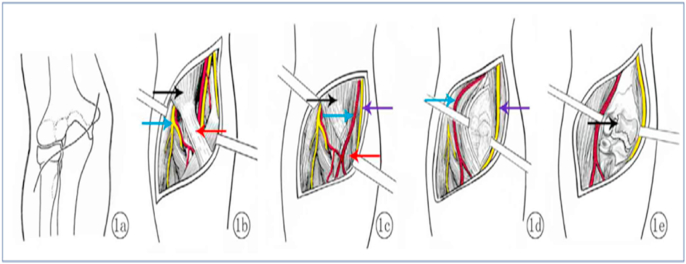
The elbow joint is in close proximity to important anatomical structures, neurovascular and ligamentous, which make any surgical approach and exposure technically demanding. In principal the elbow may either be approached by a universal posterior approach or a number of specific, more limited exposures, medially, laterally or anterior (Fig. 1). In our practice, the posterior universal exposure, through a single long skin incision, allows utilisation of specific lateral and medial access and is the most versatile approach for acute and non-acute elbow pathologies.
Fig. 1.
Overview of the surgical approaches of the elbow.
The posterior approach may be used with the patient positioned in lateral decubitus or supine, both may be chosen according to the surgeons preference regarding ease of access to the elbow, optimal image intensifier positioning and, last but not least, comfort for the surgeon for often lengthy procedures.
The anterior approach to the elbow is seldom required and, in our practice, is reserved for exposing the neurovascular structures of the anterior cubital fossa for specific indications e.g. displaced supracondylar fractures in children with significant vascular impairment.
The ideal surgical approach for treatment of an elbow fracture or other pathology should minimise soft tissue dissection without compromising visualisation and reduce the risk of heterotopic ossification and elbow stiffness.
Pre-operative planning of the approach taking into account specifics of the patient and their injury as well as experience and familiarity of the surgeon is paramount and adherence to principles will ensure safe and efficient surgical approach to the elbow.
2. Lateral approaches
Varieties of lateral approaches include Kocher's, EDC split, Kaplan and the lateral column approach.
2.1. Kocher approach
2.1.1. Indications
Radial head fractures, excision, prosthesis.
2.1.2. Advantages
Low risk of Posterior Interosseus Nerve (PIN) injury (as compared to Kaplan).
May be increased to the Extended Kocher approach to reach the distal lateral humerus.
The Kocher approach, as opposed to the EDC split or Kaplan approach, provides easy access to the supinator crest of the ulna to address a supinator crest fracture or a Lateral Ulnar Collateral ligament (LUCL) avulsion from the supinator crest which may occur in 5% of terrible triad injuries.
The Kocher approach may be extended both proximally and, with caution, distally e.g. to reconstruct the LUCL. Proximal extension is achieved by dissecting and elevating the common extensor origin, Extensor carpi radialis Longus (ECRL) and Brachioradialis (BR), off the supracondylar ridge.
2.1.3. Drawbacks
Distal extension of the approach may endanger the PIN.
2.1.4. Technique
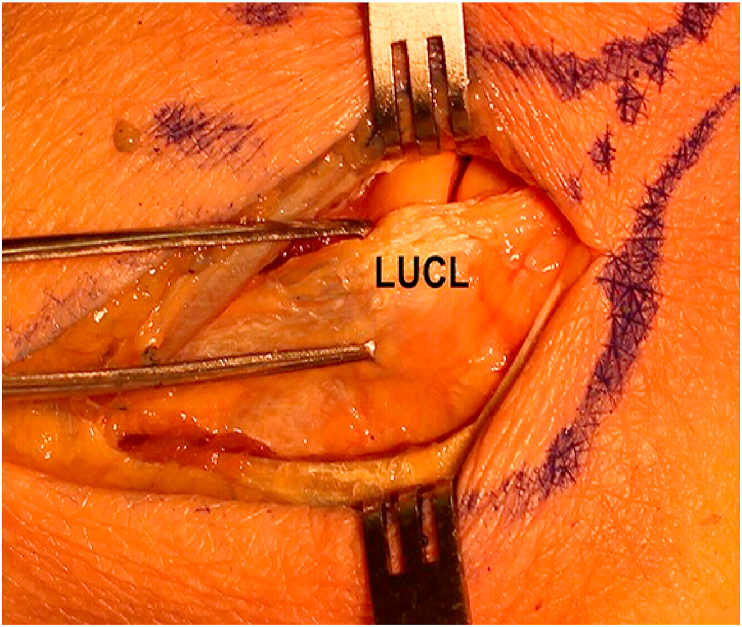
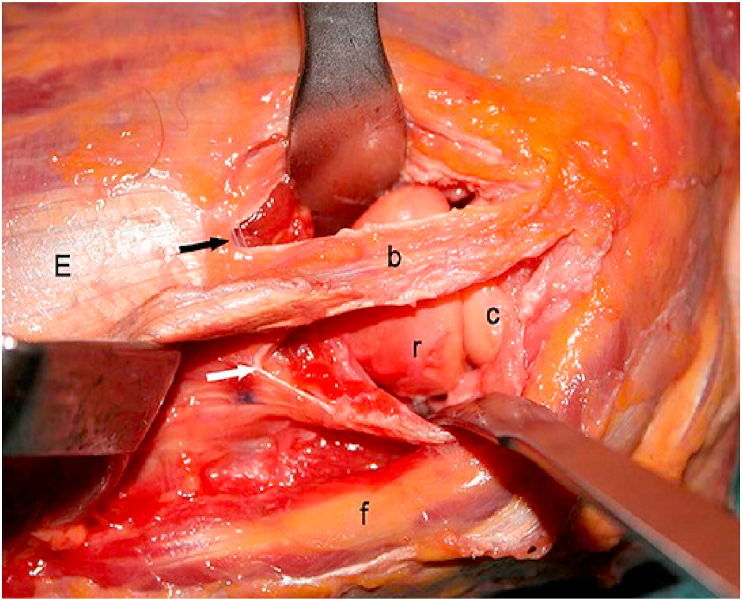
The internervous plane lays between the Anconeus and the Extensor Carpi Ulnaris muscle (ECU) and a characteristic fat stripe defines this interval (Fig. 2, Fig. 3, Fig. 4). The ECU is mobilised anteriorly and the capsule incised along the anterior border of the LUCL, approximately 1 cm above the supinator crest. The radiocapitellar joint is well palpable and the incision should be positioned slightly anterior to the equator of the capitellum. This allows preservation of the LUCL and therefore prevents posterolateral rotatory instability (PLRI) of the elbow1
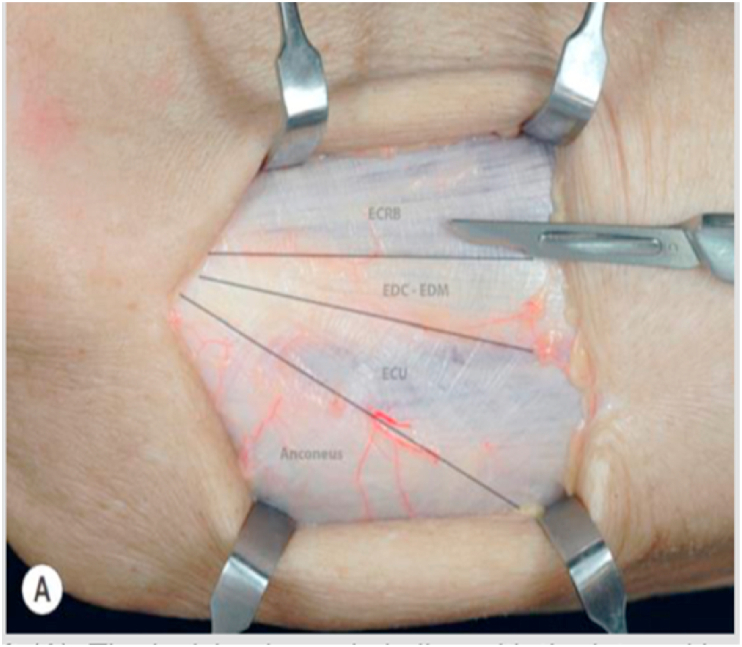
Fig. 2.
Modified kocher's approach where lateral elbow capsule is identified and incised anteriorly to the lateral ulna collateral ligament.
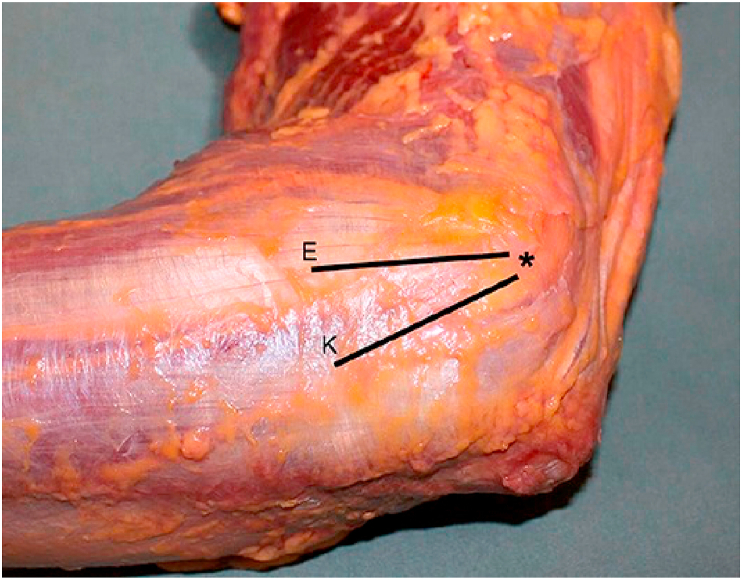
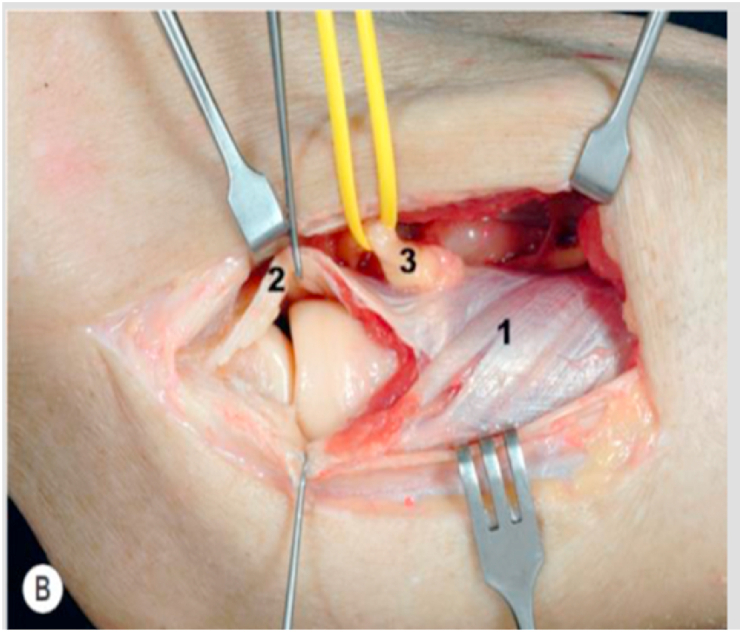
Fig. 3.
Black lines show the Kocher and EDC Split approach. The interval between the anconeus and extensor carpi ulnaris (ECU) can be identified by a thin strip of fat distally.
Fig. 4.
Shows that with a Kocher approach we can see the posterior half of the radial head where as with the EDC split approach we can see the anterior half of the radial head. C = capitellum, R = radial head, B = ECU + half of EDC, white arrow represents retracted anconeus, black arrow represents the split EDC.
2.2. Extensor digitorum communis (EDC) split approach
There is no internervous plane with this approach and the EDC tendon is dissected directly longitudinally starting at its origin at the lateral epicondyle (Fig. 3, Fig. 4). The approach offers a slightly more anterior access than the Kocher's approach.
2.3. Kaplan approach
2.3.1. Indications
Radial head fractures – fixation, excision and prosthesis.
2.3.2. Advantages
Good view of the anterior half of the radial head which is a common site of fracture.
No disruption of the LUCL.
2.3.3. Drawbacks
Inadvertent injury to the PIN if the incision is too anterior.
Distal extension can endanger the PIN.
Remember: If there is a supinator crest of ulna fracture or LUCL avulsion as in 5% of terrible triad injuries, this approach should not be used.
2.3.4. Technique
The incision is performed with the elbow midprone and in 90°of flexion, from the tip of the lateral epicondyle 4–5 cm towards the Listers tubercle. The internervous plane is between EDC and the extensor carpi radialis brevis (ECRB). After the muscle has been split, the capsule and annular ligament are incised anteriorly to the equator of capitellum thus avoiding injury to the LUCL (Fig. 5, Fig. 6).
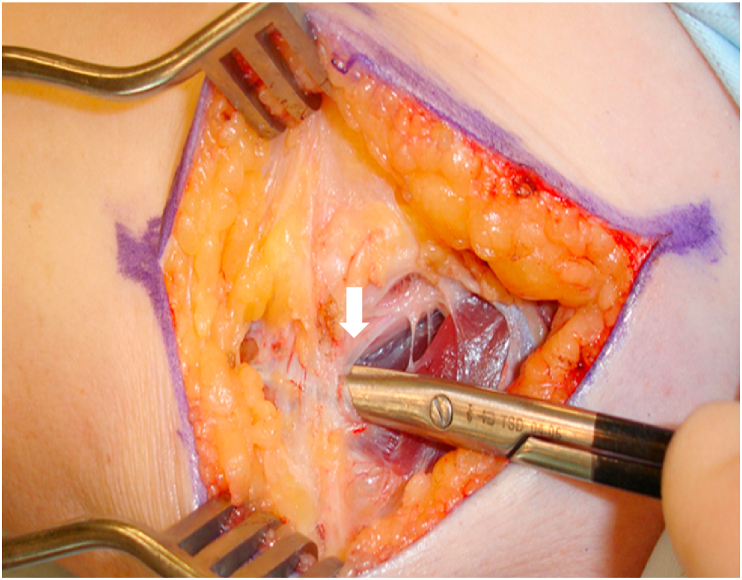
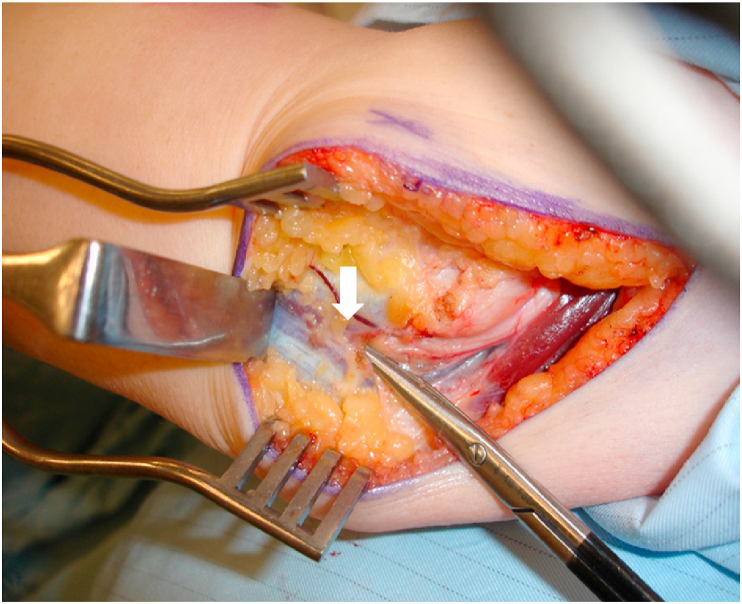
Fig. 5.
Incision is made in line with the interval between the extensor carpi radialis brevis (ECRB) muscle and the extensor digitorum communis (EDC).
Fig. 6.
The underlying capsule shown with white arrow should be longitudinally incised, allowing access to the most anterior part of the radial head. Yellow arrow represents EDC, Red arrow represents ECRB.
A quantitative analysis using computed tomography scans has shown about 79% of Mason type 2 radial head fractures to be positioned within the anteromedial quadrant2 and thus well exposed by the Kaplan approach.
2.3.5. Caution
The PIN is generally at risk with any lateral approach. In a series of 15 cadaveric dissections mean safe zone to avoid injury to the PIN has been measured 48.2±7.9 mm from the radiocapitellar joint to the PIN.4 The shortest distance measured with the forearm in pronation was 29 mm. Therefore, a distance of 25 mm from the radiocapitellar joint should be used as a reference to standardise the distal extension of both, the Kaplan and the modified Kocher approach (After developing inter-nervous plane between ECU and Anconeus; lateral elbow capsule is identified and incised anteriorly to the lateral ulna collateral ligament) Proximal extension of the Kaplan or the modified Kocher approach to the supracondylar ridge should be used for capitellum fractures.
A coronoid fracture may be present with a radial head fracture as part of a terrible triad injury. Open reduction and internal fixation of the coronoid through a lateral approach has been described, but most commonly after radial head excision prior to a radial head arthroplasty.1 Indeed, removal of the radial head provides excellent exposure to the coronoid process using a lateral approach. However, if the radial head is intact, approximately 23% of the coronoid height can be visualised using an extended Kaplan or Kocher approach. Therefore, when the radial head is not excised, Regan and Morrey type 1 and type 2 coronoid fractures may still be addressed through an extended lateral approach avoiding a separate medial approach1. Coronoid fixation may be achieved using a suture lasso technique, or posterior-to-anterior screw fixation.
In conclusion, the Kaplan approach provides a greater and more reliable exposure of the commonly fractured anterior portion of the radial head than the Kocher approach. It minimises the risk of iatrogenic injury to the LUCL and reduces the risk of PLRI. Furthermore, the safe zone for avoiding damage to the PIN is similar for the Kaplan approach and the modified Kocher approach. However, the Kocher approach will give easier access to the supinator crest of the ulna and LUCL avulsion from the supinator crest may be addressed directly for terrible triad injuries or Monteggia fracture dislocations. We therefore recommend choosing between both approaches depending on the nature of the lateral column elbow injury.
2.4. Lateral column procedure
The lateral column procedure has been described for the treatment of severe capsular contracture of the elbow. The lateral skin incision is the same as for the proximal half of Extended Kocher approach and extended 6 cm distally. The origin of the extensor carpi radialis longus (ECRL) and the brachioradialis muscles are released from the lateral column of the distal humerus. The brachialis muscle is separated from the capsule and retracted with a blunt angle retractor which will also protect the median nerve and the brachial artery. The lateral capsule is opened from lateral to medial and a strip of 1 cm capsule is excised. Through the same approach the posterior compartment of the elbow can also be accessed. The triceps muscle is released off the lateral column with a periosteal elevator, retracted and the posterior capsule is exposed. This is excised and the olecranon fossa is cleared off scar tissue and osteophytes. Care should be taken to protect the ulna nerve, when approaching the medial side of the olecranon fossa.
3. Medial approaches
Medial approaches to the elbow are particularly useful for coronoid fracture fixation, reconstruction and repair of the MCL and capsular release.
3.1. Hotchkiss approach (over-the-top approach)
3.1.1. Indications
The Hotchkiss or ‘over-the-top approach’ is the most anterior of the medial approaches and provides good access to the tip of the coronoid process and the anterior elbow joint.
3.1.2. Advantages
Good view of the coronoid tip fracture site.
3.1.3. Drawbacks
Ulnar nerve exploration and visualisation is required.
Possible injury to medial antebrachial cutaneous nerve.
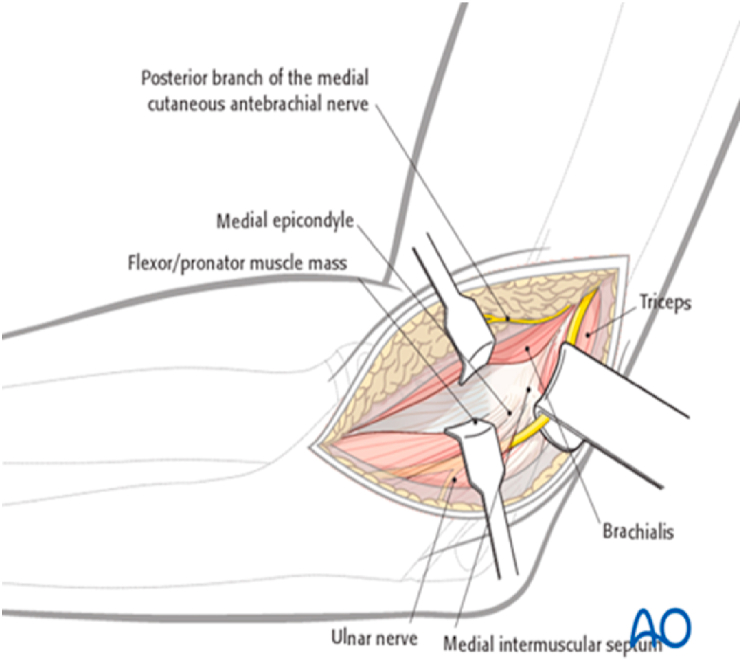
3.1.4. Technique
The skin incision may either be posterior with a medial skin flap or directly medial, taking care to protect the branches of the medial antebrachial cutaneous nerve which travels anteriorly. The ulnar nerve should be identified, usually proximally at the medial edge of the triceps muscle (3–4 cm proximal to the medial epicondyle), and protected. Subsequent decompression should be carried out in the cubital tunnel and distally as the nerve enters the fascia between the two heads of FCU, with care to protect the first motor branch to the FCU (Fig. 7, Fig. 8, Fig. 9). Anterior subcutaneous transposition should be considered to protect the ulnar nerve; especially in revision situations.
Fig. 7.
Shows division of Osborne ligament shown by white arrow.
Fig. 8.
Shows 2 heads of FCU shown by white arrow.
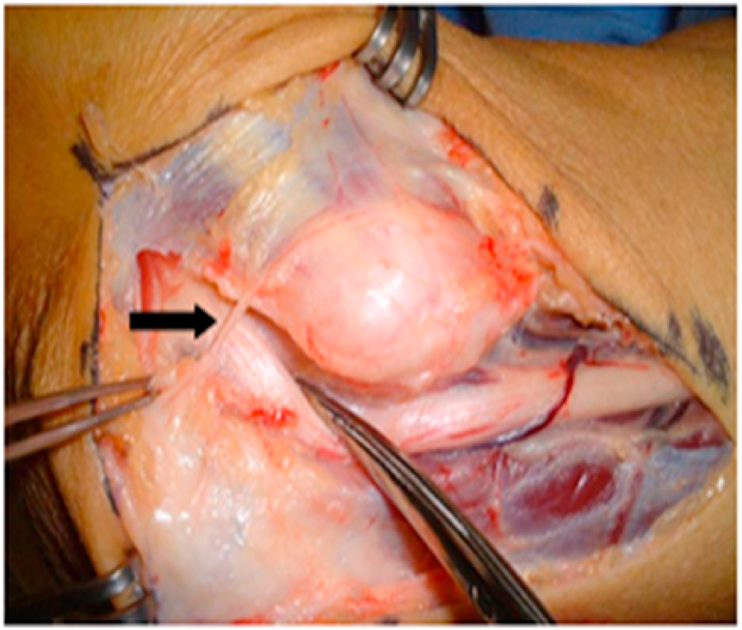
Fig. 9.
Shows black arrow towards medial antebrachial cutaneous nerve.
The flexor pronator mass is split using blunt dissection to identify the common flexor origin on the medial epicondyle. The interval between flexor carpi radialis (FCR) and palmaris longus (PL) is developed. A cuff of tissue may be left at the medial epicondyle when incising the flexor pronator muscle group, which can be repaired at the end of the procedure. Pronator teres (PT), FCR and brachialis are then elevated off the anterior capsule (Fig. 10). Careful subperiosteal dissection deep to the brachialis muscle will protect the brachial artery and median nerve. The elbow joint may be entered at this stage via an anterior capsulotomy. This approach offers good access to the tip of coronoid, but there is a limited access to the anteromedial facet and to the base of coronoid.
Fig. 10.
Hotchkiss approach. Shows the top retractor retracting pronator teres and flexor carpi radialis. Bottom retractor is retracting palmaris longus and FCU.5
3.1.5. Tip
The anterior band of medial collateral ligament is preserved by dissecting anterior to the sublime tubercle, which is easily palpable.
3.2. Flexor carpi ulnaris (FCU) splitting (Ring) approach
3.2.1. Indications
Coronoid fractures.
3.2.2. Advantages
Good view of the fracture site especially the anteromedial facet.
3.2.3. Drawbacks
Ulnar nerve exploration is required.
Possible injury to medial antebrachial cutaneous nerve.
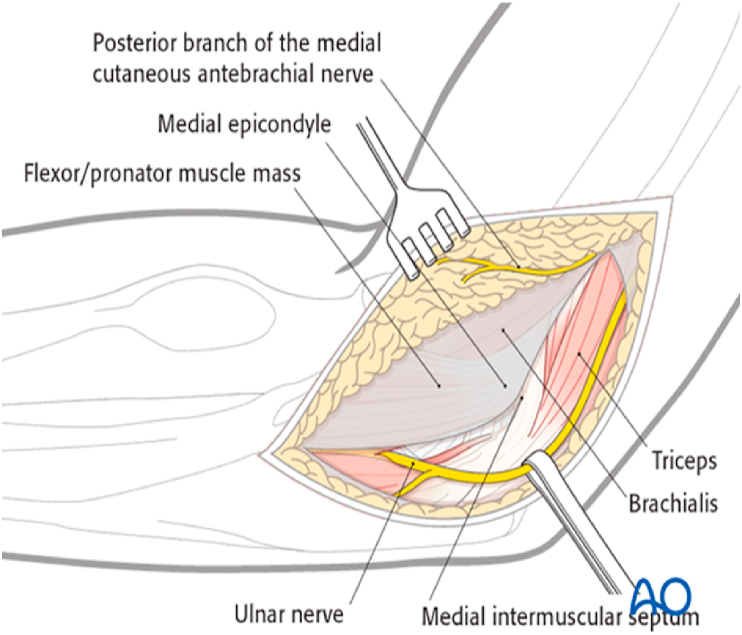
3.2.4. Technique
After the skin incision the ulna nerve is identified proximally and then decompressed distally, as described above. The anterior portion of the FCU along with the entire flexor pronator mass is elevated off the coronoid and retracted anteriorly, exposing the coronoid process and the anterior half of proximal ulna (Fig. 11, Fig. 12, Fig. 13). The exposure is kept anterior to the sublime tubercle to prevent any damage to the anterior band of the MCL. In trauma situations where the anteromedial facet is avulsed the exposure has been usually created by the injury and this may be used after mobilising and protecting the ulna nerve.
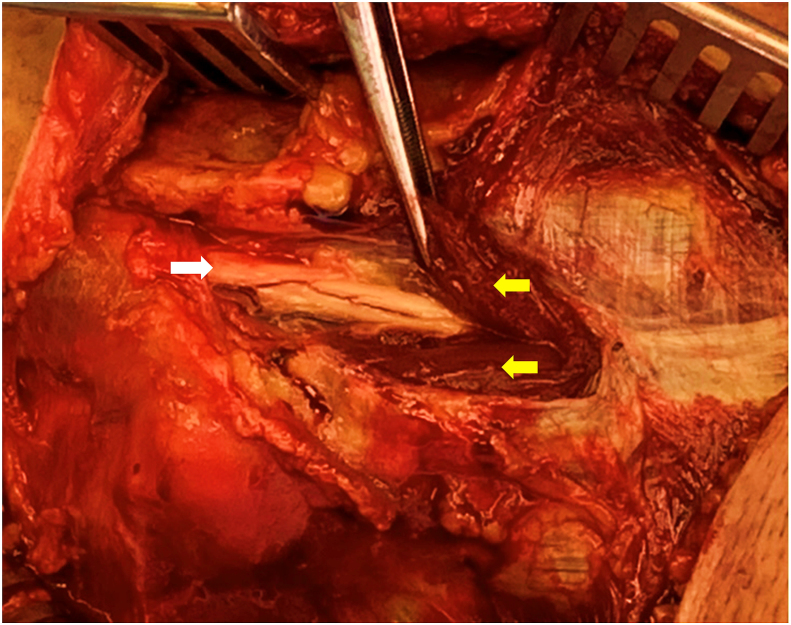
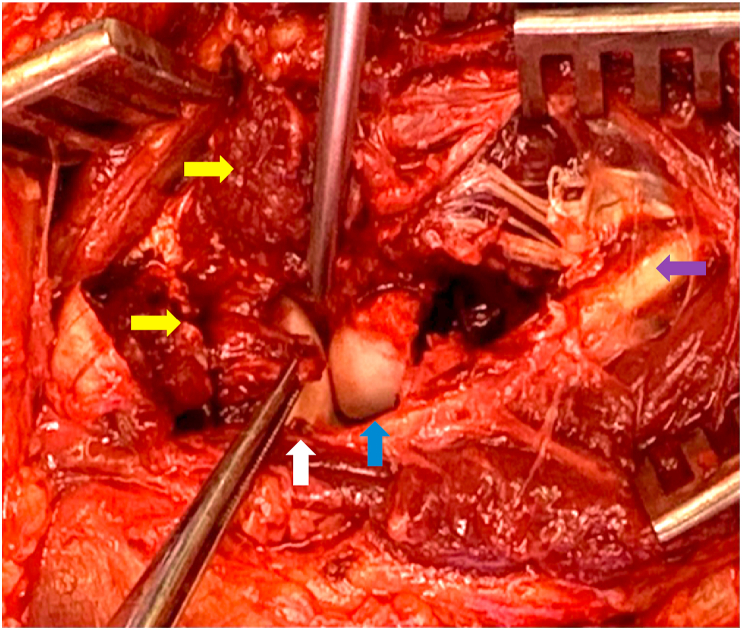
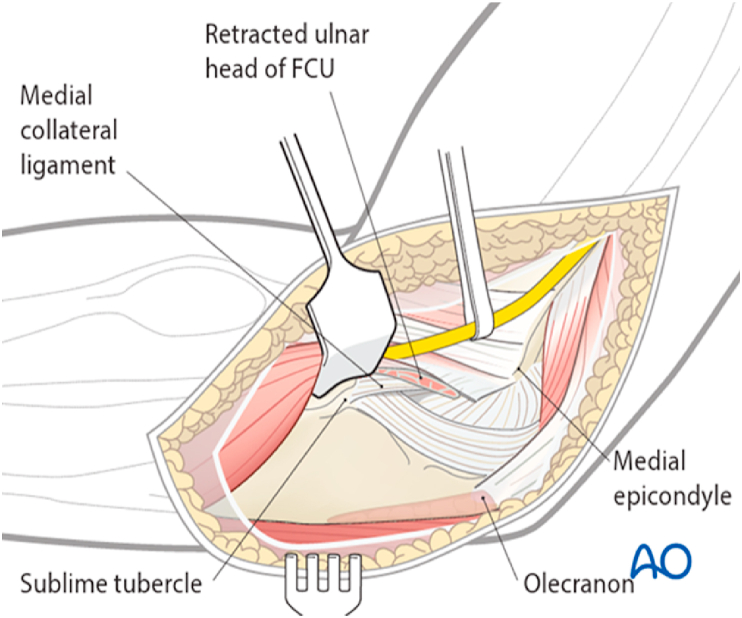
Fig. 11.
FCU split approach.6
Fig. 12.
White arrow shows ulna nerve and 2 yellow arrows show two heads of FCU.
Fig. 13.
White arrow shows anterior band of MCL avulsed from the sublime tubercle. 2 yellow arrows show cut surface of flexor muscle origin, purple arrow shows ulna nerve with preserved vascularity decompressed in situ through the two heads of FCU, blue arrow shows displaced anteromedial facet fracture.
The FCU splitting approach provides a better exposure of the anteromedial coronoid, the proximal ulna and the medial ligament structures compared with the Hotchkiss approach.7
3.3. Taylor and Scham approach8
3.3.1. Indications
This is a good approach for a medial plate fixation for a large basilar fracture of the coronoid.
3.3.2. Advantages
Good view of the fracture site.
3.3.3. Drawbacks
Ulnar nerve exploration is required.
Possible injury to medial antebrachial cutaneous nerve.
3.3.4. Technique
After skin incision the ulnar nerve should be identified and protected. Elevate the entire flexor pronator mass from posterior to anterior from the crest of the ulna shaft to the flat surface of olecranon (Fig. 14).
Fig. 14.
Taylor and Scham approach - Shows ulna nerve in sling. Retractor is retracting the entire flexor pronator mass.9
3.3.5. Caution
It is important to preserve the medial collateral ligament. Sometimes it is difficult to distinguish the origin of the FCU from the fibres of the MCL. One pearl is to dissect from distal to proximal up to the sublime tubercle which is usually palpable. As long as the dissection stays extra-periosteal and only muscle fibres are elevated from the bone, the ligament should be safe.
4. Anterior approach
4.1. Indication
Exploration of the anterior neurovascular bundle, fixation of coronoid fractures especially the anterolateral facet, trochlea fractures.
4.2. Advantages
Good exposure of the anterolateral facet of coronoid.
4.3. Drawbacks
Potential injury to anterior neurovascular structures.
4.4. Technique
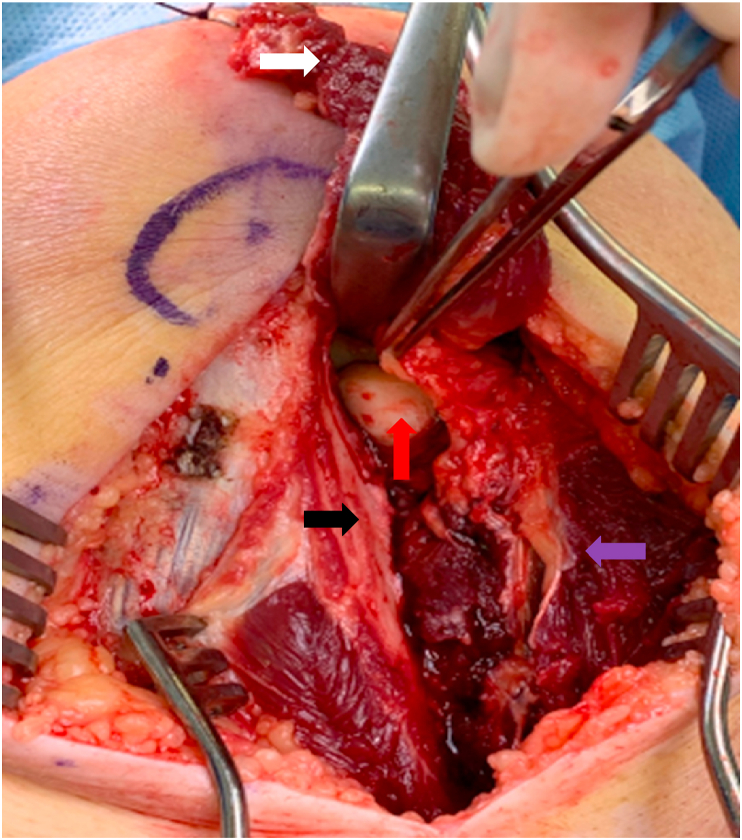
The patient is positioned supine with a tourniquet and a curvilinear S-shaped incision placed across the elbow crease, extending distally along the radial border of the forearm. Superficial dissection is performed and the interval developed between the brachial artery, ulna artery and the median nerve. The brachial artery, ulna artery, biceps tendon and brachioradialis are retracted laterally and the median nerve and pronator teres are positioned medially giving an excellent access to brachialis (Fig. 15). A blunt longitudinal split is performed within the brachialis muscle using a periosteal elevator for exposure of the ulnar aspect of the anterior joint capsule. Incision of the joint capsule will then visualise the articular surface of the trochlea and coronoid process especially the anterolateral facet.10
Fig. 15.
a shows S type incision across the anterior elbow crease. b red arrow shows bicipital aponeurosis covering brachial artery and median nerve. Black arrow shows biceps muscle, blue arrow shows radial nerve dividing into superficial radial nerve and posterior interosseous nerve. 15 c Blue arrow shows brachial artery, violet arrow shows median nerve, black arrow shows biceps, red arrow shows brachial artery dividing into radial and ulna artery. 15 d Shows split brachialis muscle. Blue arrow shows the retracted radial half of the brachialis muscle and brachial artery radially. Violet arrow shows median nerve and the medial half of the brachialis muscle retracted medially. 15 e shows exposure to the coronoid process and the trochlea after splitting the capsule. Black arrow points to the coronal shear fracture of trochlea which can be addressed using this approach.13
This neurovascular interval approach located medial to the biceps tendon is also referred to as the anteromedial approach to the elbow. This access provides full exposure of the neurovascular anatomical structures and thus is different to the anterior Henry approach. The Henry approach may be utilised to expose the radial head, radial neck and proximal radius.
Multiple surgical approaches have been described for coronoid repair. The direct medial approach is recommended for fractures of the anteromedial facet of the coronoid process particularly for those with a varus posteromedial rotation injury. However, it is difficult to reach the anterolateral facet of the coronoid process with the medial approach. This would require a relatively long incision and extensive soft tissue dissection to approach the anterolateral facet through a medial approach with possible untoward consequences 11.
In a cadaveric study the access to coronoid fractures especially the anterolateral facet has been addressed and the anteromedial approach using the space between the brachial artery and median nerve investigated. This particular approach utilises the fact that the brachial artery has no medial branches and the median nerve no lateral branches thus leaving a loose gap which can be separated and retracted easily.
Additionally, no heterotopic ossification was seen; as minimal soft tissue dissection is needed in this approach.12
5. Posterior approaches
The following describes the ‘universal’ posterior approach to the elbow as the majority of the joint can be reached irrespective of whether the surgery is being undertaken for a fracture or an elective procedure. Several variations have been described and the surgeon should select the approach that will optimise exposure for the particular procedure to be performed.14 All posterior approaches will allow good visualisation of the distal humeral articular surface although it has been demonstrated that the olecranon osteotomy provides the most extensive exposure. Wilkinson and Stanley15 quantified the area of the distal humeral articular surface visualised following an olecranon osteotomy (57%), the triceps reflecting/elevating approach (46%) and the triceps split approach (35%) respectively. Disadvantages of osteotomy of olecranon include a small risk of non-union and the possible need for removal of metalwork, constituting second surgery. However, it must be noted, that the other posterior approaches like triceps reflecting also carry risks e. g postoperative triceps weakness and consequently reduced strength which is not seen after an olecranon osteotomy.
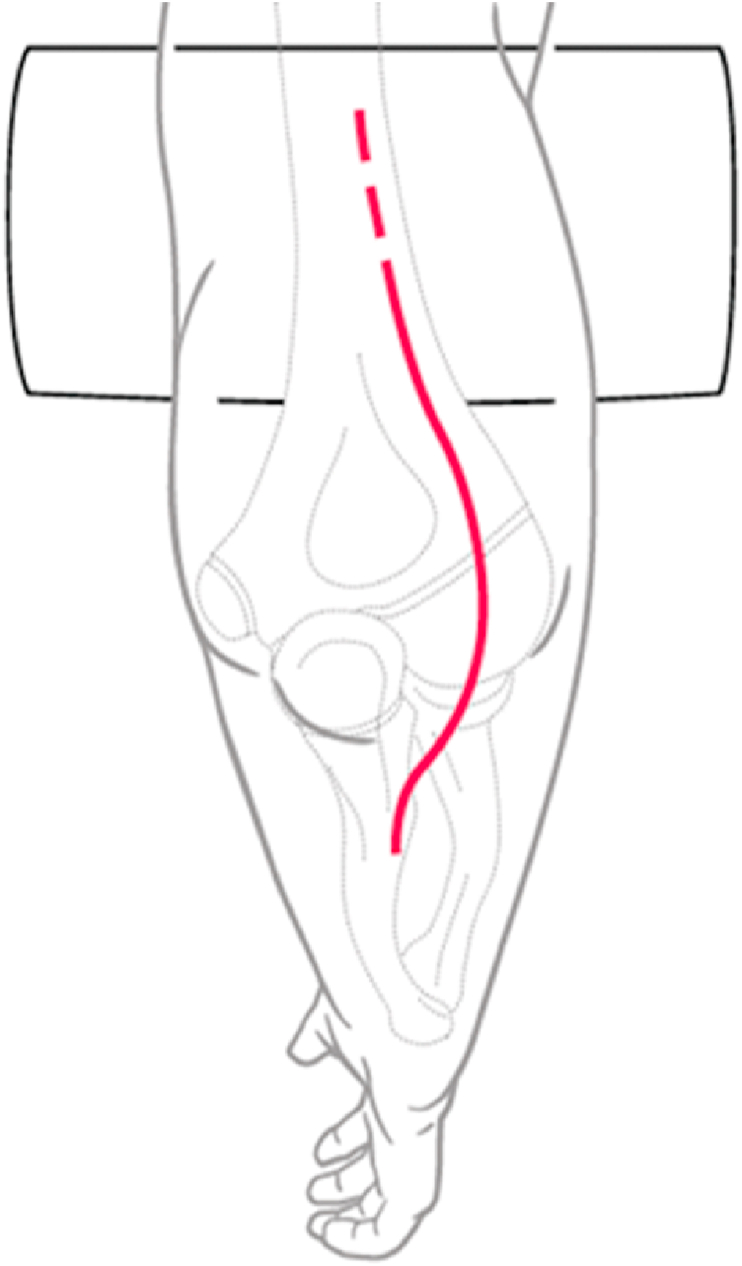
Incision: A posterior incision carries a lower risk of cutaneous nerve injury compared with medial or lateral incisions.16 The incision starts 10 cm proximal to the medial epicondyle curving from the midline around the lateral border of the tip of the olecranon and continuous along the subcutaneous border of the ulna for 5 cm. (Fig. 16). Postoperatively a surgical drain may be used for 24 h combined with a splint in extension for 48 h thus reducing the risk of wound complications associated with long surgical incisions.
Fig. 16.
Shows patient positioned laterally with a curved incision, curving laterally avoiding the ulna nerve.17
Patient position: The patient may be positioned in the supine or lateral position. In the supine position the arm is draped across the chest allowing easy access for the image intensifier as well as other parts of the body e. g for the polytrauma patient, or the iliac crest if bone graft is required. The lateral position however provides a comfortable operating position for the surgeon although intra-operative imaging can be more difficult.
5.1. Olecranon osteotomy
5.1.1. Indications
Distal humerus fracture fixation with intra-articular fracture extension. Of note, this approach is not suitable for total elbow arthroplasty as the repair of the osteotomy site would be impaired by the cemented ulna component.
5.1.2. Advantages
This approach provides the best exposure of the distal humerus for fracture fixation.
5.1.3. Drawbacks
Bone healing at the osteotomy site may delay rehabilitation, possible requirement for metalwork removal at a later date.
5.1.4. Technique
We have described the Mayo modification of the Olecranon osteotomy. The universal posterior approach with a single long skin incision is used and medial and lateral full thickness skin flaps are raised. The ulnar nerve is identified proximally at the medial edge of the triceps, decompressed and protected. The traditional olecranon osteotomy will interfere with the insertion of the anconeus muscle which has been shown to provide dynamic stability to the lateral side of the elbow. The Mayo modification of this approach addresses this problem18 and the anconeus muscle is identified and elevated from its bed by sharp dissection preserving its attachment to the triceps. The hardware to be used to fix the osteotomy at the end of the procedure, usually a pre-contoured metal plate, is placed on the olecranon and proximal and distal screw holes are predrilled before the osteotomy is performed. This step facilitates anatomical alignment at the end of surgery. The osteotomy is performed using an oscillating saw and completed by leverage with an osteotome in the shape of a chevron with its apex distal, through the bare area of the ulna which has almost no articular cartilage. The osteotome creates a slightly irregular surface which will ease repositioning of the olecranon at the end of the procedure. The chevron configuration is preferred over a transverse or an oblique cut due to the increased surface area for stability and compression. The triceps is lifted off the medial and the lateral intermuscular septum and finally the triceps is reflected proximally in toto with the attached olecranon fragment and anconeus (triceps anconeus pedicle - TRAP). Thus excellent exposure of the distal articular surface of the humerus is achieved (Fig. 17, Fig. 18).
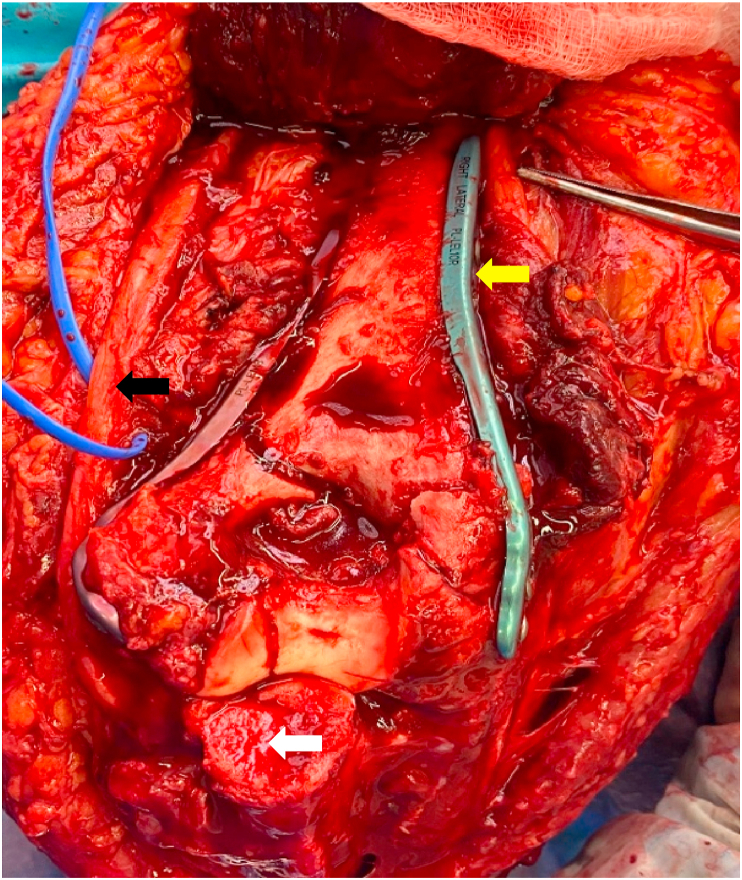
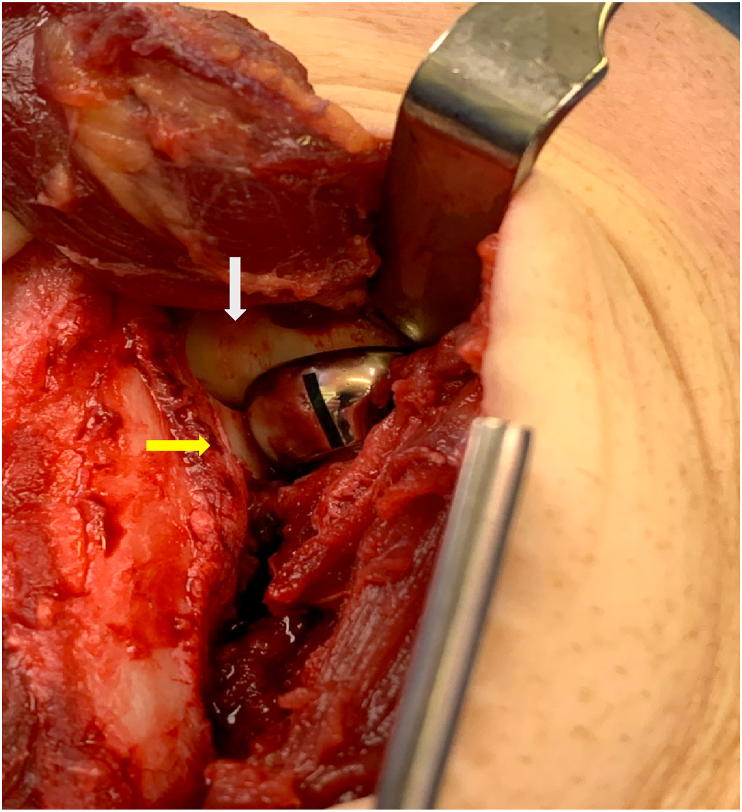
Fig. 17.
Shows a chevron shaped osteotomy with complete retraction of the triceps along with the olecranon tip bringing a wide exposure to the distal posterior humerus. Bi column plate fixation seen. White arrow -chevron olecranon osteotomy. Black arrow - Ulna Nerve. Yellow arrow Radial nerve pointed by the forceps.
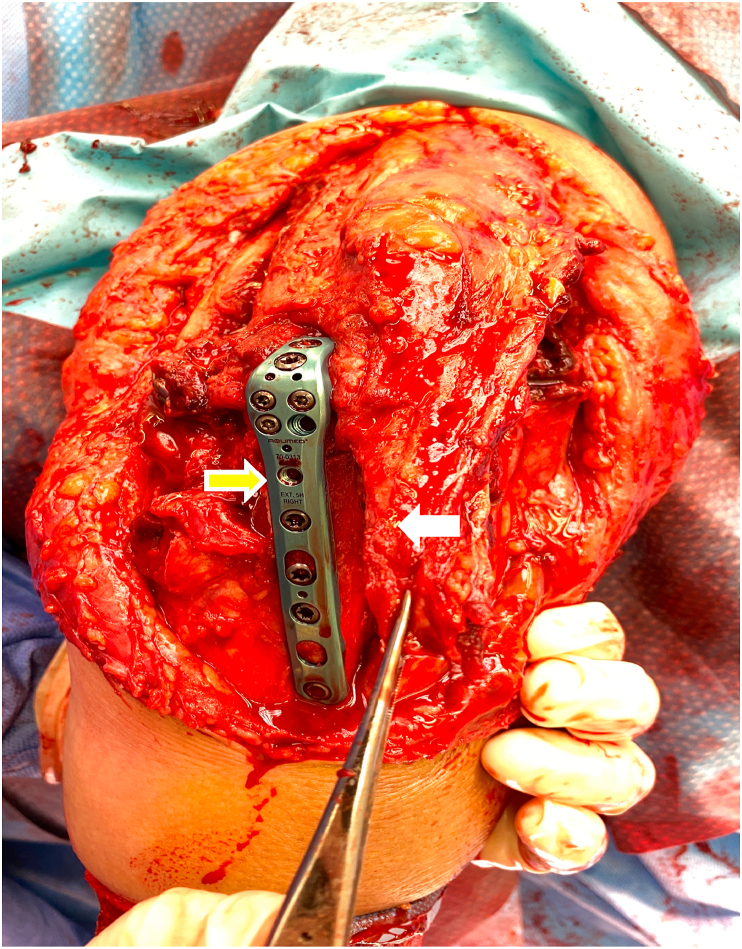
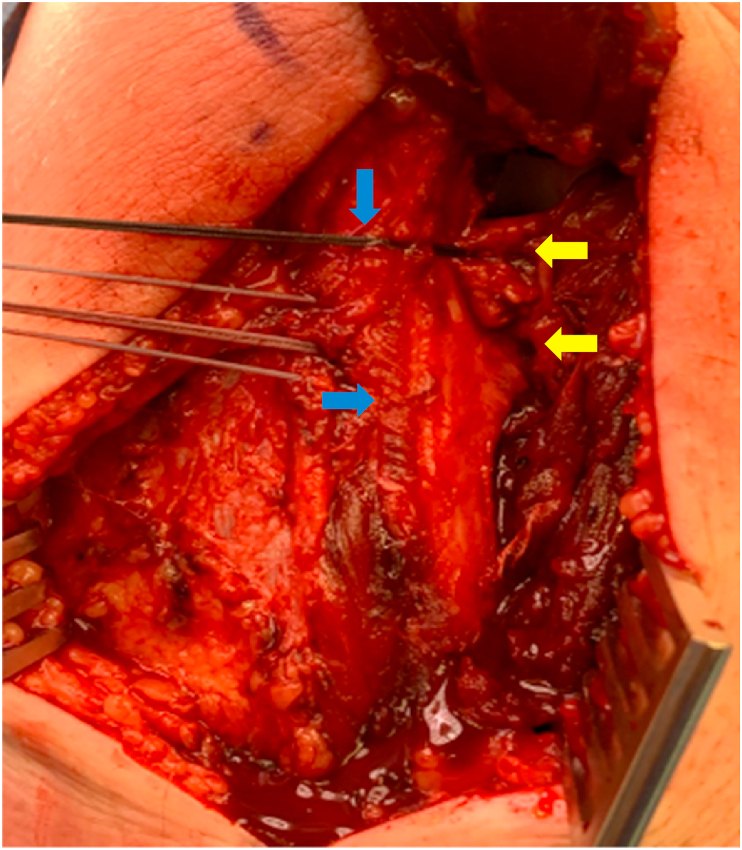
Fig. 18.
Shows plate fixation for olecranon osteotomy pointed by a yellow arrow. Forceps holding Anconeus muscle part of the triceps anconeus pedicle flap (TRAP flap) shown by white arrow.
Overview of Posterior approaches to the elbow.
The Posterior approaches can be broadly categorized into triceps-off and triceps-on.
Triceps off approaches involve some or all of the triceps being taken off its ulna insertion or cutting of the triceps mechanism at some point. The triceps-off group can be subdivided into triceps turndown, triceps elevating or triceps splitting. A triceps turndown involves cutting of the triceps tendon above the ulna insertion. A triceps elevating approach elevates the triceps off the ulna sub-periosteally. A triceps splitting approach divides the triceps tendon longitudinally along its length and through its insertion. Disadvantage being Triceps weakness and risk of triceps avulsion with associated morbidity.
Triceps-on approaches maintain the triceps mechanism and its insertion on the ulna. Disadvantage - Exposure and visualisation of the humeral articular surface using the ‘triceps-on’ approach is not as good as with the ‘triceps-off’ approach. Advantage – As the attachment of triceps tendon is kept intact onto the olecranon, triceps strength is maintained and triceps disruption can be avoided. Other advantage is early active range of motion exercises.
Both these approaches can be used to address variety of elbow conditions like distal humerus intraarticular fractures, Total elbow replacement etc depending upon surgeons discretion.
5.2.1. Triceps reflecting/elevating approach (Bryan-Morrey approach/Triceps off approach)
5.2.1.1. Indication
Total elbow arthroplasty.
5.2.1.2. Advantage
An alternative posterior approach without an olecranon osteotomy.
5.2.1.3. Technique
The triceps tendon, periosteum and fascia are reflected directly off the olecranon from medial to lateral as a continuous sleeve (Fig. 19, Fig. 20, Fig. 21). The triceps may be lifted with a wafer of bone using a thin osteotome, facilitating bone-to-bone rather than tendon-to-bone healing at the triceps insertion site. Finally the triceps is reflected proximally from the posterior distal humerus. For total elbow arthroplasty the medial and lateral collateral ligaments are released off the epicondyles from the distal humerus. The elbow is then flexed to expose the joint. The ulnar nerve should be monitored closely to avoid any traction injury as the triceps is retracted laterally during the exposure.
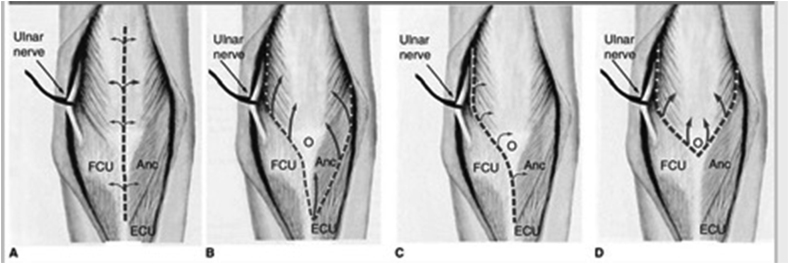
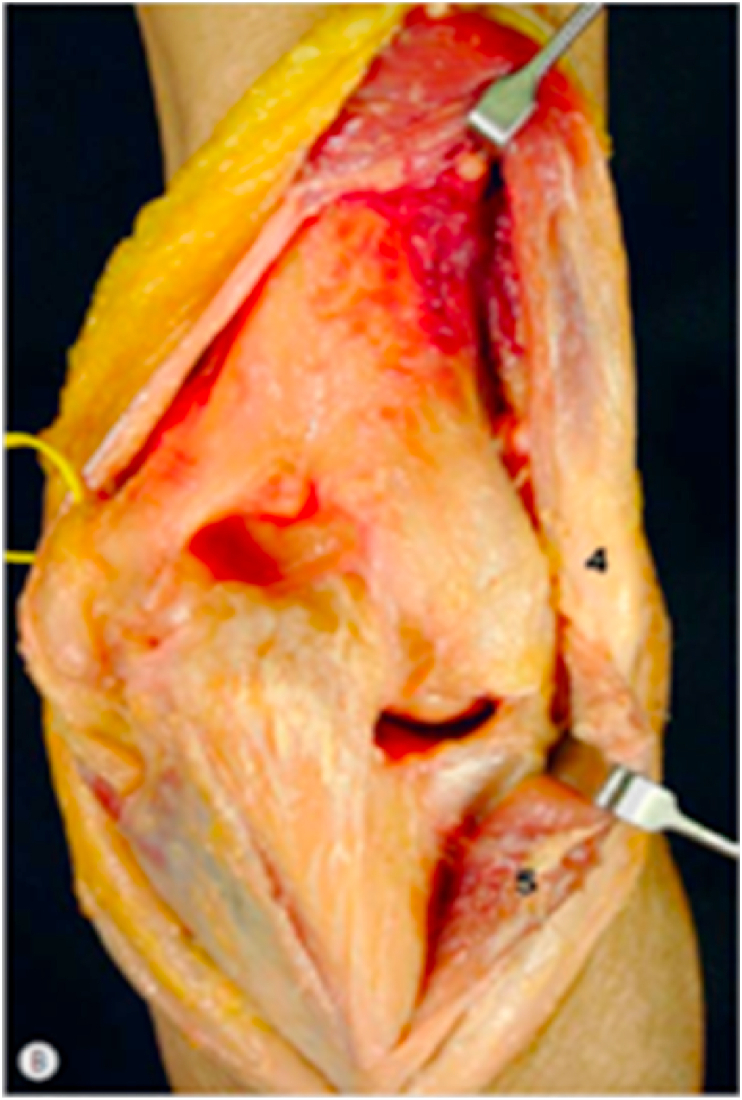
Fig. 19.
Triceps split and triceps reflection both require a complete removal of triceps from its reflection both require a complete removal of triceps from its attachment from olecranon. For an olecranon osteotomy or triceps sparing approach the triceps attachment is left intact. Although with the osteotomy, the olecranon is completely removed from the ulna.19
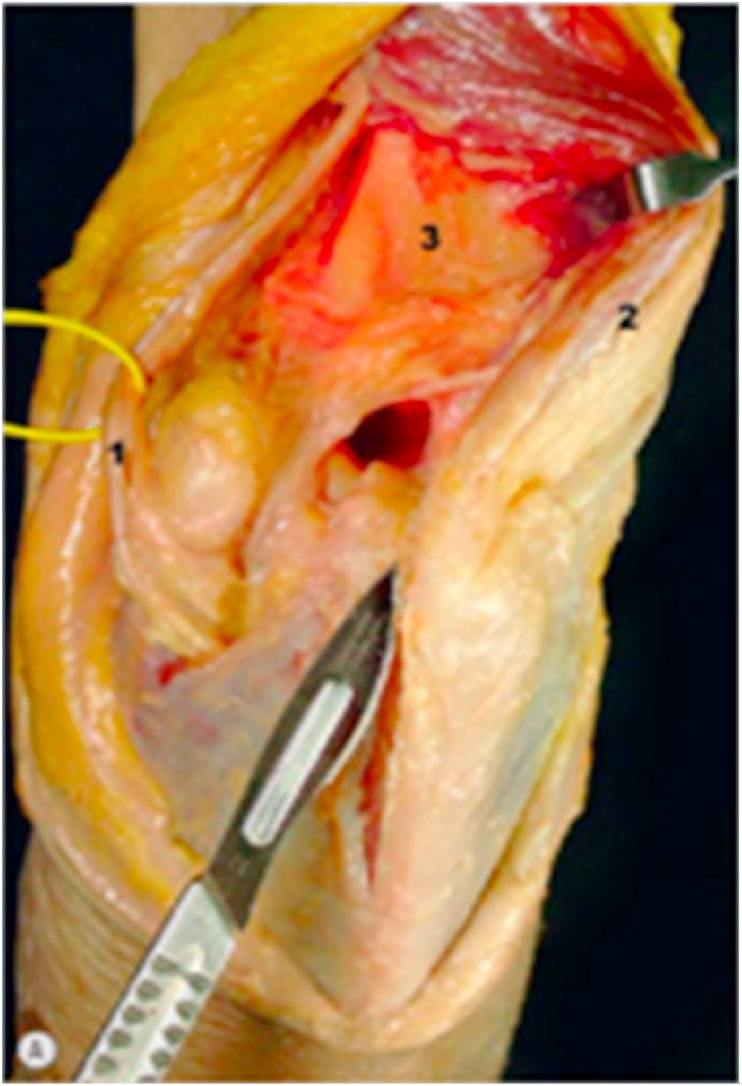
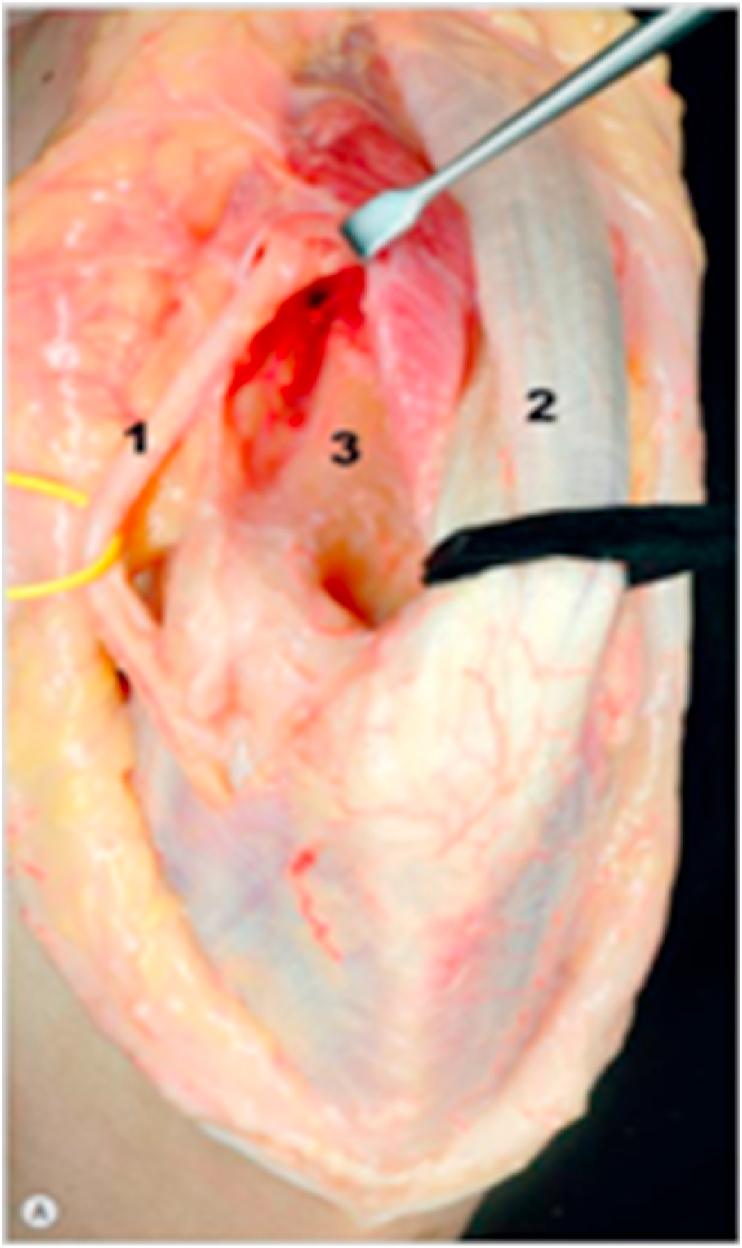
Fig. 20.
After isolation of ulnar nerve (1), the triceps (2) is subperiosteally detached from the posterior aspect of the humerus (3).
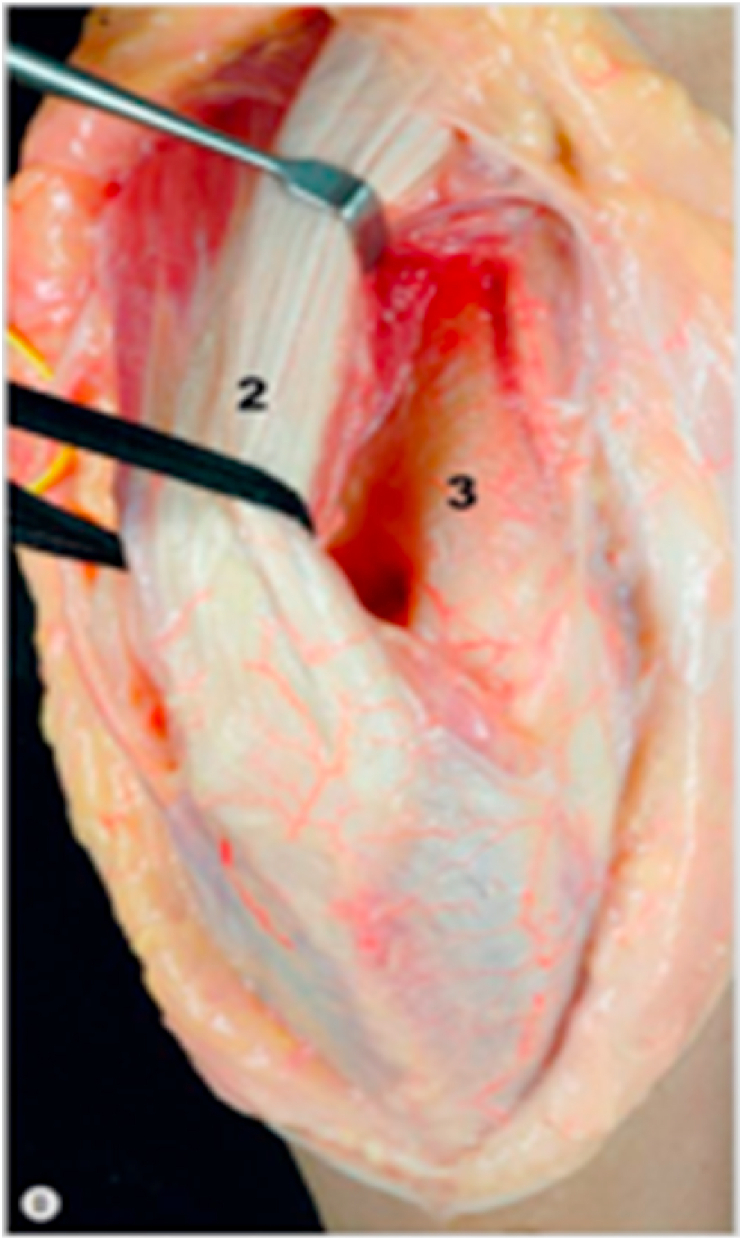
Fig. 21.
The triceps is dissected from its attachment on the olecranon (4) and is reflected laterally together with the anconeus (5).
At the end of the procedure the triceps tendon is repaired to the olecranon by two trans-osseous drill holes placed in a crucifix configuration. An additional drill hole is placed between the two holes in a transverse orientation and the suture is performed using non-absorbable material. The triceps repair should be protected for six weeks postoperatively avoiding active elbow extension against resistance.
5.2.1.4. Drawbacks
Triceps weakness and risk of triceps avulsion with associated morbidity.
5.2.2. Triceps-on approach
5.2.2.1. Indication
An alternative to avoid the disadvantages of an olecranon osteotomy and triceps reflection.
5.2.2.2. Technique
As above, the ulnar nerve is identified and protected (1). The triceps (2) is subperiosteally detached from the posterior aspect of the humerus (3) medially and laterally, however the insertion on the olecranon is preserved (Fig. 22, Fig. 23). The elbow joint is exposed through the medial and lateral windows on each side of the triceps.
Fig. 22.
Showing- Ulnar nerve (1), Triceps (2), humerus (3).
Fig. 23.
Patient is positioned in a lateral position. Incision is around 16–20 cm centred over the olecranon. After developing skin flaps, ulna nerve is identified and protected (1). Then triceps (2) is subperiosteally detached from the posterior aspect of the humerus (3) on both sides, preserving its insertion on the olecranon. Expose the elbow joint through the medial and lateral windows on each side of the triceps.
The medial window to the ulno-humeral joint is created by subperiosteally elevating the MCL and FCU off the medial side of ulna. The flexor pronator mass and MCL are also lifted subperiosteally off the medial epicondyle before retracting the triceps laterally. Hyperpronation of the forearm will expose the articular surface and the proximal ulna.
The lateral window to the radio-capitellar joint and the distal humerus is developed through the distal interval between the anconeus and the ECU exposing the radial head with caution to protect the PIN. The lateral collateral ligament (LCL) and the extensor muscle origin are released from the lateral epicondyle and the triceps is retracted medially whilst the extensor muscles and LCL complex are mobilised laterally.
Tip.
Preparation of the humerus is best performed through the lateral window to avoid traction on the ulnar nerve. The elbow joint may be best viewed through the medial window.
5.2.2.3. Advantages
As the attachment of triceps tendon is kept intact onto the olecranon, triceps strength is maintained and triceps disruption can be avoided. Other advantage is early active range of motion exercises.
Complications to the ulna nerve were similar for all approaches.20
5.2.2.4. Drawbacks
Exposure and visualisation of the humeral articular surface using the ‘triceps-on’ approach is not as good as with the ‘triceps-off’ approach. Similarly implant positioning may be difficult with the ‘triceps-on’ approach, especially the ulna component is at risk of being positioned in flexion. This may be avoided by judicious placement of the provided jigs.20
In summary, the ‘triceps-on’ approach has significant functional advantages but provides reduced exposure with the risk of malposition of the implants.
5.2.3. Boyd interval posterior approach
5.2.3.1. Indication
The Boyd approach is an excellent posterior approach providing access to the radial head and neck and may be considered as an alternative to the Kocher's, Kaplan and EDC splitting approaches.
5.2.3.2. Technique
Approximately an 8 cm longitudinal skin incision is made just lateral to the subcutaneous border of the ulna and full thickness skin flaps are raised. A cuff of fascia approximately 3–5 mm in breadth attached to the ulna is preserved and the fascia longitudinally incised along the anconeus and extensor carpi ulnaris. The anconeus is elevated subperiosteally to reveal the supinator muscle and the lateral collateral ligament complex (Fig. 24). The annular ligament, LUCL and joint capsule are identified and detached directly off the supinator crest of ulna using sharp dissection thus exposing the radial head and neck. Further access to the proximal shaft of the radius may be obtained by elevating the supinator of the supinator crest with the arm in full pronation to protect the PIN.21
Fig. 24.
Shows reflected Anconeus muscle pointed by a white arrow, black arrow shows the supinator crest. Forceps is holding the annular ligament, capsule and the LUCL complex, red arrow points to radial head, violet arrow points to supinator muscle which is partially reflected.
The incision may be extended proximally and distally to expose the lateral column of the distal humerus and the ulna. The radial head and neck may be addressed for fracture fixation or radial head replacement. (Fig. 25). For plate fixation of the radial head, the forearm should be positioned in maximum supination allowing excellent visualisation of the safe zone thus preventing loss of forearm rotation secondary to impingement of hardware on the proximal radioulnar joint (PRUJ). Radial head screws, if required, should be buried beneath the cartilaginous surface to avoid impingement at the PRUJ. Capitellum fractures may also be reduced and fixed from this exposure. Furthermore proximal extension and raising of the lateral triceps allows visualisation of the lateral column of the distal humerus for lateral or posterior plating.
Fig. 25.
Shows a radial head replacement in situ, yellow arrow points to lesser sigmoid notch. White arrow points to capitellum.
At closure LUCL repair is performed by drilling three bone tunnels from the posterior aspect of the ulna to the supinator crest facilitating bone sutures. The annular ligament may be repaired using an anchor placed in the proximal ulna and Kessler sutures are used to repair the LUCL. The sutures are tied on the medial side of the ulna and tensioned with the forearm in neutral rotation and 30° of elbow flexion (Fig. 26). Finally the fascia is repaired with the anconeus.
Fig. 26.
Shows transosseous suture repair pointed by yellow arrows to LUCL, annular ligament and capsule complex. White arrow shows green sutures representing Mitek anchor for annular ligament repair. Repair done over supinator crest as shown by a blue arrow.
5.2.3.3. Advantage
The Boyd approach may be extended distally with less risk to the PIN than using the Kocher's, Kaplan and EDC splitting approach which are positioned more laterally and anteriorly.
5.2.3.4. Drawback
The PIN is still at risk during the Boyd interval approach, in particular during elevation of the supinator.
5.2.4. Other posterior approaches to elbow
5.2.4.1. Alonso-Liames (Paratricipital approach)22
Indications- Paediatric supracondylar fractures, extra articular distal humerus fractures.
Approach- The universal posterior skin incision is used and full thickness medial and lateral skin flaps raised. The ulnar nerve is identified and protected. The medial and lateral borders of triceps tendon are incised and the muscle is elevated from the posterior border of the distal humerus. The triceps is retracted medially or laterally during the procedure, allowing delivery of the distal humerus into the wound and facilitating the surgical procedure.
5.2.4.2. Van Gorder (Triceps Turn down approach)23
Indications: contracture release, total elbow arthroplasty.
Approach: the universal posterior skin incision is used and full thickness medial and lateral skin flaps are raised. The ulnar nerve is identified and protected. The fascia and triceps aponeurosis are incised, creating a 10 cm length of aponeurosis in the form of an inverted ‘V’ with the base attached to the olecranon. The medial head is then divided in the midline and reflected to expose the posterior aspect of the humerus.
5.2.4.3. Lateral para olecranon approach
Indication
1. Distal humerus intra articular fractures
Technique
Patient is placed in a lateral position. Midline posterior incision is performed. Two fasciocutaneous flaps are elevated off the deep fascia. Ulna nerve is identified and protected.
Then anconeous muscle is incised from the proximal ulna. Incision is extended proximally and triceps is split at the junction of lateral one third and medial two thirds. This will ensure that the insertion of the central triceps tendon on the olecranon tip is maintained. Now MCL and lateral collateral ligament are incised which will give nice exposure of the articular fragments.24
The medial two thirds of the triceps muscle is released from the medial intramuscular septum and from the dorsal aspect of the distal humerus. In cases of intra articular fracture; the joint capsule and the fat pad are excised from the olecranon fossa preserving the medial collateral ligament. The distal humerus is visualised from medial and lateral windows by retracting the medial two thirds of the triceps muscle laterally and medially.
In the modified approach described by Iwamoto et all, the annular ligament and the lateral collateral ligament is not incised.25
Advantage
As the attachment of triceps tendon is kept intact onto the olecranon, triceps strength is maintained and triceps disruption can be avoided. Other advantage is early active range of motion exercises.
Conclusion
The elbow may be reached from a variety of approaches. The surgeon has a multitude of options tailored to the specific problem to be addressed. For medial column injuries, eg anterior medial facet coronoid fractures, a medial approach should be used. For lateral column injuries, eg radial head or capitellum fractures, and LUCL injuries, one of the lateral approaches can be chosen. The anterior approach has a very specific role to address the anterior neuro-vascular bundle. The posterior approach is the universal workhorse by allowing access to both, lateral and medial columns. The olecranon osteotomy has a specific role for comminuted distal humerus fracture but if an arthroplasty is considered the olecranon must be kept intact. The Boyd interval is an excellent approach to treat for Monteggia fracture-dislocation. The surgeon should be aware of advantages and disadvantages of each approach to make the best decision.
Contributor Information
Saurabh Aggarwal, Email: s.aggarwal@nhs.net.
Kiran Paknikar, Email: paknikar.kiran1@gmail.com, kiran.paknikar@nhs.net.
Joydeep Sinha, Email: joydeepsinha@nhs.net.
Jonathan Compson, Email: Jonathan.compson@nhs.net.
Ines Reichert, Email: i.reichert@nhs.net.
References
- 1.William D., Hakim L., Steven R., Whitcomb P J. Objective analysis of lateral elbow exposure with the extensor digitorum communis split compared with the kocher interval. J Bone Joint Surg Am. 2014;96:387–393. doi: 10.2106/JBJS.M.00001. [DOI] [PubMed] [Google Scholar]
- 2.Van Leeuwen D.H., Guitton T.H., Lambers K., Ring D. Quantitative measurement of radial head fracture location. J Shoulder Elbow Surg. 2012. Aug;21(8):1023. doi: 10.1016/j.jse.2011.08.056. 7Epub 2011 Nov 09. [DOI] [PubMed] [Google Scholar]
- 4.Schimizzi A., MacLennanA, Meier K.M., Chia B., Lw3rd Catalano, Gilckel S.Z. Defining a safe zone of dissecting during the extensor digitorum communis splitting approach to the proximal radius and forearm : an anatomical study. J Hand Surg Am. 2009 Sep;34(7):125. doi: 10.1016/j.jhsa.2009.04.026. 5. [DOI] [PubMed] [Google Scholar]
- 5.https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/proximal-forearm/approach/medial-hotchkiss-over-the-top
- 6.https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/proximal-forearm/approach/medial-fcu-split
- 7.Jeannie H., Krueger Chad A. Medial elbow exposure for coronoid fractures: FCU- split versus over the top. J Orthop Trauma. 2013;27:730–734. doi: 10.1097/BOT.0b013e31828ba91c. [DOI] [PubMed] [Google Scholar]
- 8.Taylor T.K., Scham S.M. A posteromedial approach to the proximal end of the ulna for the internal fixation of olecranon fractures. J Trauma. 1969;9:594–602. doi: 10.1097/00005373-196907000-00004. [DOI] [PubMed] [Google Scholar]
- 9.https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/proximal-forearm/approach/medial-taylor-and-scham
- 10.X.-H. Yang, C. Wei, G.-P. Li, et al Anatomical study of the anterior neurovascular interval approach to the elbow : observation of the neurovascular interval and relevant branches . Folia Morphol. Vol.79, No. 2, pp. 387-394. [DOI] [PubMed]
- 12.Shukla D.R., Koehler S.M., Guerra S.M. A novel approach for coronoid fractures. Tech Hand Up Extrem Surg. 2014;18(4):189–193. doi: 10.1097/BTH.0000000000000065. indexed in Pubmed: 25289725. [DOI] [PubMed] [Google Scholar]
- 13.http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-42302019000300355
- 14.Chris P., David S. Surgical approaches to the elbow. Orthopaed Trauma. 2012;26(5):297–302. [Google Scholar]
- 15.Wilkinson J.M., Stanley D. Posterior surgical approaches to the elbow: a comparative anatomic study. J Shoulder Elbow Surg. 2001;10:380–382. doi: 10.1067/mse.2001.116517. [DOI] [PubMed] [Google Scholar]
- 16.Dowdy P.A., Bain G.I., King G.J., Patterson S.D. The midline posterior elbow incision. An anatomical appraisal. J Bone Joint Surg Br. 1995;77:696–699. [PubMed] [Google Scholar]
- 17.https://surgeryreference.aofoundation.org/orthopedic-trauma/pediatric-trauma/proximal-forearm/approach/posterior-approach-to-the-ulna
- 18.Athwal G.S., Rispoli D.M., Steinmann S.P. The anconeus flap transolecranon approach to the distal humerus. J Orthop Trauma. 2006;20:282–285. doi: 10.1097/00005131-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 19.https://www.orthobullets.com/trauma/1017/distal-humerus-fractures
- 20.Simon J.B., Chris D.S. Triceps on approach for total elbow arthroplasty: worth preserving? A review of approaches for total elbow arthroplasty. Shoulder Elbow. 2017;9(2):105–111. doi: 10.1177/1758573216682479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paul M.R., Martin K.-H., Li Rupen D., Lee V.R. The Boyd interval: a modification for use in the management of elbow trauma. Tech Hand Surg. 2016;20:37–41. doi: 10.1097/BTH.0000000000000112. [DOI] [PubMed] [Google Scholar]
- 22.Alonso-Liames M. Bilaterotricipital approach to the elbow . Its application in the osteosynthesis of supracondylar fractures of the humerus in children. Acta Orthop Scand. 1972;43:497–590. doi: 10.3109/17453677208991270. [DOI] [PubMed] [Google Scholar]
- 23.Van Gorder G.W. Surgical approach in posterior dislocation of the elbow. J Bone Joint Surg Am. 1932;14:127–143. [Google Scholar]
- 24.Studer A., Athwal G.S., Macdermid J.C., Faber K.J., King G.J. The lateral para-olecranon approach for total elbow arthroplasty. J Hand Surg Am. 2013;38(11):2219. doi: 10.1016/j.jhsa.2013.07.029. e2226.e2213. [DOI] [PubMed] [Google Scholar]
- 25.Iwamoto T., Suzuki T., Matsumura N., Nakamura M., Matsumoto M., Sato K. The lateral para-olecranon approach for the treatment of Distal Humeral Fracture. J Hand Surg Am. r. May 2017;42:344–350. doi: 10.1016/j.jhsa.2017.02.004. [DOI] [PubMed] [Google Scholar]