Abstract
Purpose
We aimed to investigate which changes in the explanatory factors that were associated with positive change in the work ability score (WAS) and degree of work participation (DWP) for participants in a new 1-year vocational rehabilitation (VR) program for people on or at risk of sick leave due to obesity or obesity-related problems.
Patients and Methods
This prospective observational study included 95 participants with a body mass index (BMI) above 30 kg/m2. The 1-year multidisciplinary VR program with an integrated work and lifestyle intervention included 4 weeks of inpatient stay followed-up by five meetings. Differences between baseline and 12-month follow-up data were analyzed for the change in explanatory variables WAS, DWP, health-related quality of life (HRQoL), BMI, and return-to-work self-efficacy (RTWSE). The primary outcome was measured by multiple linear regression for predicting WAS and DWP.
Results
We found significant changes in WAS (1.51, 95% CI: 0.83 to 2.20, p<0.001), DWP (18.69, 95% CI: 8.35 to 29.02, p<0.001), HRQoL (2.57, 95% CI: 1.35 to 3.79, p<0.001), BMI (−2.33, 95% CI: −3.10 to −1.56, p<0.001), and in RTWSE (15.89, 95% CI: 4.07 to 27.71, p = 0.009). Regression analysis yielded a strong association between WAS at 12-month follow-up with an increase in HRQoL (β=0.27, 95% CI: 0.16 to 0.38, p<0.001) and WAS baseline (β=0.49, 95% CI: 0.28 to 0.71, p<0.001). Further, regression analysis demonstrated a strong association between DWP at 12-month follow-up with return-to-work expectancy (RTWEXP) (β=−10.62, 95% CI: −15.25 to −6.03, p<0.001).
Conclusion
The results indicate positive changes in WAS, DWP, HRQoL, BMI, and RTWSE from baseline to 12-month follow-up. For people with BMI above 30 kg/m2, changes in HRQoL are important for an increase in WAS, and a high RTWEXP is essential to achieve work participation. Future studies examining VR programs with lifestyle interventions for people with obesity are recommended.
Keywords: health-related quality of life, return-to-work expectancy, return-to-work self-efficacy
Introduction
People with obesity may have a good working life and health. However, obesity (body mass index [BMI] ≥30 kg/m2) is generally associated with severe health complications, functional impairment and lower self-esteem.1 Obesity is a very complex, multifactorial chronic disease, caused by factors from gut-to-brain mechanisms, energy expenditure, genetics, human energy homeostasis and the gut microbiome and to behavioral, environmental and psychosocial contributors.2 In general, people with obesity report poorer health-related quality of life (HRQoL) when compared with the non-obese population.3,4 Moreover, obesity may affect employee productivity, absenteeism from work, sick leave,5,6 and reduced job productivity.6 Working people with obesity of all ages, struggle to enter and remain in the workforce,6 which can contribute to adverse financial and social consequences, lower self-confidence, a depressed mood, and feelings of isolation.7,8
The Norwegian Government promotes an active labor and welfare policy to view that as many people as possible should participate in working life.9 Therefore, to manage problems related to health and functional capacity and adjust contextual factors, individuals in Norway who struggle to remain in the workforce can receive help through vocational rehabilitation (VR). VR aims not to cure illness but to promote work participation despite health complaints and sickness. Previous research indicates that people attending VR programs may increase work ability, reduce sick leave, earlier return to work (RTW) following sick leave, and reduce work disability.7,10,11 RTW is often the outcome measure and the final goal; however, it explains only a small part of the complex picture of rehabilitation.8 Work participation requires sufficient work ability, which is a key concept in rehabilitation for working-age people.8,12 In a framework of International Classification of Functioning, Disability and Health (ICF),13 the term work ability describes the functional ability to perform work and the interaction between individual physical, mental, and social factors and various environmental factors.12 Work ability is closely associated with HRQoL, which provides information about the burden of obesity, the effects of diseases, and treatment from the individual’s view.12
Systematic reviews have identified positive factors associated with RTW, such as higher education, socioeconomic status, positive perceived health, higher self-efficacy, being employed, and participating in multidisciplinary interventions.7,14 In addition, individuals’ optimistic expectations about length of sick leave7,15 and return-to-work expectancy (RTWEXP) predicted a positive RTW outcome.14 Self-efficacy, the “belief in one’s abilities to organize and execute the courses of action required to produce given attainment”,16 is an important cognitive motivational factor for predicting functional recovery and an individual’s probability of successfully participating in and completing treatment. Self-efficacy describes motivation and the development of coping strategies and may be a useful concept for understanding the self-management aspects of RTW.8 In line with this, a specific measure of RTW self-efficacy (RTWSE) may be useful for evaluating VR interventions and capturing elements of both personal motivation and situational barriers.17
Despite the existing documentation of factors predicting RTW, there is a lack of empirical evidence about factors that generate changes in work participation for people with obesity.18 In Norway, the overall time in VR services for inpatients’ stays is traditionally no more than 4 weeks, only occasionally up to 12 weeks.9 This stands in stark contrast to the length needed for lifestyle changes, which preferably would be over 6 months.19 In addition, VR programs lacks a focus on both lifestyle- and work intervention. Before 2015, no VR program in Norway focused on both work and lifestyle intervention. Therefore, a new, temporary, multidisciplinary VR program for people with obesity focused on enhanced work self-efficacy and lifestyle change was established in a specialized rehabilitation centre in the middle of Norway. The major differences between the traditional and the new VR program are the length and the behavioral- and dietary intervention. The inpatient program was established with several follow-ups for an entire year and combined VR with specific components to address lifestyle change using cognitive approaches to develop skills for coping strategies and to raise self-efficacy. The VR program emphasizes self-efficacy as an essential element of human motivation and behavior, that affect how people embrace and cope with life.20 According to Bandura, higher self-efficacy is an important determinant of behavior change.20,21
The gap is large between published research on results from VR programs with and without lifestyle interventions. Several journal articles22,23 and books24,25 have addressed conceptual models of RTW and work disability,23 but they have little or no focus on obesity and lifestyle change.26 Only a few studies have focused on the association between work ability and multifactorial lifestyle risk.27 For example, in a Norwegian study, low work ability was more likely to be observed in individuals with unhealthy diets, inactivity, obesity, and being former or current smokers.27 In a Polish study, work ability was strongly associated with lifestyle for both men and women.28 To the authors knowledge, no other published research has primarily focused on VR with an integrated work and lifestyle intervention perspective for individuals on or at risk of sick leave from work due to obesity or obesity-related problems. Therefore, the study aim was to investigate which changes in the explanatory factors were associated with positive change in the work ability score (WAS) and degree of work participation (DWP) after participation in a vocational rehabilitation (VR) program for people on or at risk of sick leave due to obesity or obesity-related problems. The study had two research questions.
What changes from baseline to 12-month follow-up in HRQoL, BMI, and RTWSE, in combination with return-to-work expectations, are associated with WAS at 12-month follow-up?
What changes in HRQoL, BMI, RTWSE, and WAS, in combination with return-to-work expectations, are associated with DWP at 12-month follow-up?
Patients and Methods
Participants
This study recruited participants from a publicly funded VR program with a lifestyle intervention at Muritunet Rehabilitation Centre in Western Norway. Individuals were referred to the rehabilitation program by general practitioners according to their right to admission to the Norwegian specialist health services.29 In total, 190 eligible people (divided into 18 groups) had their first stay at the rehabilitation centre between April 2015 and December 2017. Of these, 95 agreed to participate in the study. Due to the nature of the study intervention, blinding the participants was not possible. However, the employees of the VR program were blinded to which individual were participants in the study.
Inclusion criteria were as follows: participants on or at risk of sick leave from work due to obesity or obesity-related problems, had a BMI of more than 30 kg/m2, were 18–67 years old (67 is the age of pension in Norway), and had a realistic opportunity to work part- or full-time. The exclusion criteria included substance and alcohol abuse, unstable medical conditions that prevented physical activity, pregnancy, severe mental illness, disability pension, and disabilities requiring permanently modified work.
Study Design and Procedure
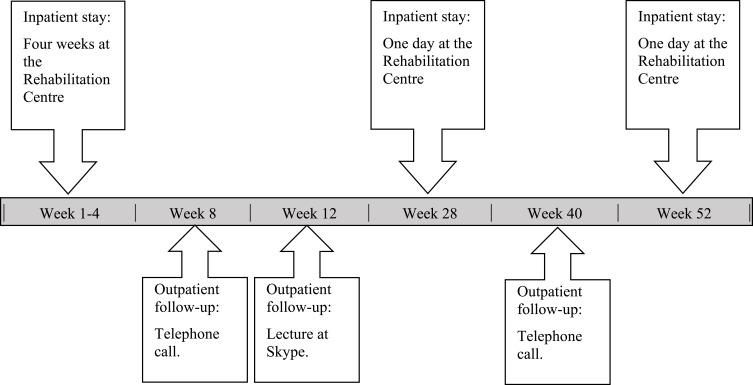
The prospective observational study examined the outcomes of a 1-year VR program. The program commenced with 4 weeks of inpatient stay at the rehabilitation centre, followed by five follow-up meetings at 8, 16, 28, 40 and 52 weeks after baseline (Figure 1). The multidisciplinary team engaged in the rehabilitation program comprised a labor consultant, health-care professionals and a sports educator; they all had complementary roles and collaborated to assess and treat the participants. Each participant developed a plan with goals for work activity, diet, physical activity and coping strategies for the rehabilitation period. The rehabilitation program builds on the framework of WHO International Classification of Functioning, Disability and Health10 combined with the Sherbrooke workplace model and intervention30 and consists of practical and theoretical intervention components in groups and individually.
Figure 1.
A schematic overview above in- and outpatient stays of the vocational rehabilitation program.
During the 4-week inpatient stay, the participants had, on average 17 hours of individual consultation with a labor consultant, medical doctor, dieticians, physiotherapist, psychiatrist, or nurse, all educated in Motivational interviewing.31 They also had 48 hours of group activity and lectures divided as follows: 14 hours of cognitive behavior theory and practice, 20 hours of physical activity, 9.5 hours of education on food, 2.5 hours of work-related education, and 2 hours of lectures about obesity. After the 4 weeks of inpatient stay, the participants received an additional 4 hours of individual consulting, 6 hours of cognitive behavior theory and practice, 2 hours of food education and 4 hours with physical activity. Dietary and physical intervention aims to contribute to 5–10% body weight reduction, following the Norwegian Directorate of Health’s national professional guideline for prevention, assessment, and treatment of obesity.2,32
People who participate in VR programs tend to have more complex needs due to health problems, length of sick-leave, and circumstances at home or work. Contact with appropriate agencies as the workplace and Norwegian Labour and Welfare Administration (NAV) may provide sustained work capacity and job satisfaction among the participants and increase the prerequisite of RTW.
Patient and Public Involvement
Several stages of the study had patient and public involvement, including development of the VR program, parts of the design of the study, and in conducting the trial. Patient involvement ensures patients “and relatives” voices in the program. The patient group consisted of people with different muscle and skeletal disorders, disease of the heart and lungs, of people with a BMI of more than 30 kg/m2, and people with mental health issues. The main results of the study will be disseminated to the participants and to the public and private sectors.
Variables
The study used baseline data that was collected prior to the intervention and data that were collected at the last, 12-month follow-up. At baseline, the participants answered the questionnaires and took the body composition tests on either the first or second day of the inpatient stay. After 12 months, the participants brought completed forms to the follow-up, and took the body composition tests at the rehabilitation centre. Participants who did not attend at 12-month follow-up were encouraged to return completed forms by mail with an updated body weight. Non-responders were sent one reminder.
Work Ability Score
The WAS involved a self-assessment of perceived mental and physical capacity and work demands.27 Self-rated work ability was assessed using a single-item question to determine the WAS, published by Gould et al33 as part of the full work ability index (WAI).34 Previous studies have demonstrated a strong association between WAS and the complete WAI:34 change in the single-item question predicts the future degree of sick-leave, HRQoL, vitality, neck pain, self-rated general physical and mental health, lifestyle, and behavioral, and current stress.34,35 WAS measure the “current work ability compared with your lifetime best,“ using a scale of 0–10 (0 = “completely unable to work” and 10 = ”work ability at its best”). The following measurement classification from Gould et al33 was used: poor (0–5), moderate (6–7), good (8–9), excellent (10).
Degree of Work Participation
DWP ranged from 0 to 100 (in percent) and is the percentage of a full-time position. The first measurement (DWP baseline) was obtained 5 days before the patients enrolled in the program to avoid counting sick leave used to participate in the program. The second measurement was obtained at the 12-month follow-up. If work participation was not continuous for at least 4 weeks after 12-month follow-up due to vacation and temporary absence, DWP was assigned a value of 0%. For those with 4 weeks of continuous work participation after 12-month follow-up, DWP was based on the degree of their current work participation. DWP data was applied for and obtained from NAV’s national registry.
Health-Related Quality of Life Measure 15D
The 15D instrument (15-dimensional), is a generic, comprehensive, self-administered instrument for measuring HRQoL among adults (aged 16+ years). The 15D consists of many different health states and therefore embraces diverse arenas important for people with obesity.1,4 The 15D covers most of the “domains of health” emphasized in the WHO ICF. It measures mobility, vision, hearing, breathing, sleeping, eating, speech, excretion, usual activities, mental function, discomfort and symptoms, depression, distress, vitality, and sexual activity. Health status is described at five ordinal levels for each dimension (1 = no problem with any aspect, 5 = deceased). The score was reversed before the analyses so that a higher score indicated better HRQoL. To obtain adequate score variance in the small sample, the total sum score of all 15 questions were used (range 1–75); previous studies on individuals with musculoskeletal, cardiovascular or psychosomatic disorders and on obese patients, have confirmed better responsiveness to change when assessed by the total scores.36
The 15D instrument is comparable with existing, commonly used profile and single index scoring instruments in terms of reliability, validity, sensitivity, discriminatory power, and response to change.36–38
Body Mass Index
Bodyweight (kg) was measured with a Tanita MC-780U Multi Frequency Segmental Body Composition Analyzer. The participants weight was measured with light clothing and without shoes before breakfast in the morning. Each person’s height (cm) was measured in a standing position without shoes using a stadiometer. Height was added in Tanita MC-780U, and BMI was calculated as weight (kg) divided by height (M) squared and was reported in kg/m2. World Health Organization (WHO) BMI reference values for adults were used as follows: underweight (<18.5), normal weight (18.5–24.9), overweight (25.0–29.9), obesity class I (30.0–34.9), obesity class II (35.0–39.9), and obesity class III (above 40).1 Participants who were unable to attend the follow-up at 12 months reported their self-monitored weight.
Return-to-Work Self-Efficacy
RTWSE is a reliable and valid measurement for assessing working adults with musculoskeletal disorders in terms of their confidence to meet job demands, modify job tasks and communicate needs to co-workers and supervisors.17,39 RTWSE was expected to be a reliable tool for obese individuals with somatic symptoms, as one-third of the present study’s participants reported musculoskeletal problems. To determine RTWSE, 19 questions with a score ranging from 1 (“not sure at all”) to 10 (“very sure”) were used to determine RTWSE. The total score (range, 0–190) was used for the analyses. RTWSE scoring by Shaw et al39 was followed to interpret changes in self-efficacy as follows: <5, low self-efficacy; 5–7.5, medium self-efficacy; and >7.5, high self-efficacy. Higher values indicated a more positive self-reported RTWSE.39
Work Absence
Work absence was measured as the number of days receiving social or medical benefits from 12 months before entering the program and until baseline, as applied and obtained from NAV’s national registry. It was calculated from potential workdays adjusted according to reimbursement of part- or full-time benefits, with normal working hours per week (37.5 hours) for each individual.
Return-to-Work Expectation
RTWEXP was measured at baseline with a single question: “If you expect to return to work (RTW) after rehabilitation (full or part-time), how long will it take you to RTW?” (translated by the authors). Participants were asked to respond on an 9-point scale: 1) immediately, 2) less than 1 month; 3) less than 2 months, 4) less than 3 months, 5) less than 6 months, 6) less than 12 months, 7) 12 months or more, 8) Never, 9) I do not know. None of the observants used the code “Never”, and 3 respondents in category ‘I don’t know’ were categorized as missing.
Sociodemographics
Age, gender, ethnicity, and medical diagnosis were obtained from the patient journal at the rehabilitation clinic. Age refers to the current age of the participants at the start of the intervention.
Education level and years of work experience were obtained from self-reported questions. Education level examined the highest completed education divided into three categories: 1 (elementary school <10 years), 2 (high school <14 years), college/university education (>14 years). Work experience was examined with the question “How many years have you in total been working?” and was divided in a four-point scale: 1 (5 years or less), 2 (6–10 years), 3 (11–19 years) and 4 (above 20 years).
Social benefits, work participation (full or part-time) and sick leave diagnoses were applied and obtained from NAV’s national registry. Diagnoses were coded and grouped according to the International Classification of Primary Care (ICPC-2).
Statistical Analysis
Descriptive statistics were used to characterize the study population with mean or median, standard deviation and range for continuous variables, and with numbers and valid percentage for categorical variables. Assumption of normality was tested with P-P plots. Differences between baseline and 12-month follow-up were analyzed with paired sample t-tests for WAS, DWP, HRQoL, BMI, and RTWSE.
Simple and intermediate multiple linear regression analyses formed the basis for the testing of variables in the final analysis with WAS and DWP as outcomes. We included results of the explanatory variables with p-values less than 0.20 in building the final models. Variables of general interest, like gender, were included. Simple regression analyses were used to produce unadjusted regression effects. The first final regression analysis produced the adjusted regression effect for WAS at the 12-month follow-up relative to the change in HRQoL. The variables were adjusted for gender, sick leave diagnosis, education level, and WAS baseline. The next final multivariate linear regression analysis estimated the association between RTWEXP and DWP at 12-month follow-up, adjusted for gender and sick leave diagnosis.
To detect any potential correlation between the explanatory variables in the final multiple regression analysis, the variance inflation factor (VIF) was examined. Furthermore, P-P-plots were used to examine how closely the data sets agreed and to evaluate the plot distribution’s skewness.40
The sample size calculation was based on the results from a group that had previously participated in a similar vocational rehabilitation intervention at Muritunet Rehabilitation Centre. For HRQoL an effect size of 0.4 was assumed. Therefore, a sample size of 55 was needed to obtain a power of 80% with a significance level of 5%.
Data were analyzed using SPSS, v.26 (Armonk, NY: IBM Corp.).
Results
For this study, 95 Caucasians consented to participate. Of these, 46.3% were female. At baseline, 61% (n=58) received social benefits from NAV (53% on sick leave, 6% on partly work assessment allowance, and 2% on unemployment benefit), and 39% (n=37) of the participants worked full time. The participants working full time were at risk of sick leave due to obesity or obesity-related problems, ie, health problems causing problems to maintain work participation. Most of the participants (91%) expected to return to work within 6 months. The majority of them (71%) had working experience above 20 years, and only 10% had less than 10 years. From 1 year before entering the program and to the start of the study, the participants had an average of 110 days of work absence. Distribution of BMI reference values among the participants was the following: 15% in obesity class I, 43% in class II, and 41% in class III. Sick leave diagnoses reported by NAV were mostly related to diseases of the musculoskeletal system, and 70% of the subgroup “another diagnoses” reported mental and behavioral disorders. After 12 months, 27 participants (12 females and 15 males) were lost to follow-up. Of these, 1 reported as sick, 1 had moved to another part of Norway, 2 were transitioning to disability pension, 4 could not come due to work, and 19 participants did not report any reason. The 27 missing participants contributed only minimal differences to the background, outcome and explanatory variables. The ‘not on sick leave’ group of 37 participants reported at baseline higher belief on WAS, RTWSE, RTW EXP, and had less work absence days. Moreover, the reported HRQoL and BMI contributed with only minimal differences. The participants who did not participate in this study had lower values in reported age, education level, included more females and body weight (Table 1).
Table 1.
Characteristics of the Participants at Baseline
| Follow-Up(N=68) | Lost to Follow-Up (N=27)d | Not Included (N=95)e | ||||
|---|---|---|---|---|---|---|
| Outcome variables | ||||||
| DWP, median (SDa, rangeb) | 47.23 | (46.68, 0–100) | 41.85 | (48.68, 0–100) | ||
| WAS, mean (SD, range) | 5.7 | (2.7, 0–10) | 5.4 | (3, 0–10) | ||
| Explanatory variables | ||||||
| HRQoL, mean (SD, range) | 64.4 | (5.43, 53–75) | 64 | (5.9, 50–75) | ||
| Body mass index, kg/m2, mean (SDa, rangeb) | 38.8 | (4.2, 29–48.5) | 40.5 | (5.5, 30.2–57.8) | 38.5 | (5.5, 27.3–57.3) |
| Weight, kg | 121.1 | (18.9, 74.9–170.4) | 123.5 | (20.5, 74.9–196) | 116.3 | (20.6, 68.1–165.2) |
| High, cm | 176.4 | (9.9, 521–200) | 174.9 | (10.8, 152–196) | 173.2 | (8.6154–197.5) |
| RTWSE, mean (SD, range) (n = 94) | 124.2 | (38.1, 29–183) | 128.2 | (40, 41–190) | ||
| RTWEXP, mean (SD, range) | 2.43 | (1.84, 1–6) | 2.76 | (1.74, 1–6) | ||
| Work absence daysc, 1 year before, median (25–75th percentile, range) | 101.7 | (106.03, 0–353) | 110.9 | (117.4, 0–364) | ||
| Background variables | ||||||
| Sociodemographic status, n (%) | ||||||
| Age, mean (SD, range) | 47.6 | (9.5, 23–63) | 45.8 | (11.5, 19–64) | ||
| Gender, n (%) | ||||||
| Males | 36 | (53) | 15 | (55.6) | ||
| Females | 32 | (47) | 12 | (44.4) | ||
| Sick leave diagnoses, n (%) | ||||||
| Musculoskeletal system | 23 | (35.9) | 11 | (40.7) | ||
| Endocrine, nutritional, and metabolic diseases | 17 | (26.5) | 12 | (44.4) | ||
| All other reported diagnosis | 24 | (37.5) | 4 | (14.8) | ||
| Education level, n (%) | ||||||
| Collage/university education (>14 years) | 31 | (45.6) | 8 | (29.6) | 31 | (33) |
| High school (<13 years) | 29 | (42.6) | 16 | (59.3) | 43 | (45.7) |
| Elementary school (<10 years) | 8 | (11.8) | 3 | (11.1) | 17 | (18.1) |
Notes: aStandard deviation: SD. bRange: Minimum and maximum value. cWork absence, measured as number of days 1 year before entering the rehabilitation program. dBaseline values for 27 missing participants at 12-month follow-up. eParticipants who declined to participate in the study.
Change from baseline to 12-month follow-up in scores for WAS, DWP, HRQoL, BMI, and RTWSE were calculated for 68 (71.6%), 95 (100%), 68 (71.6%), 65 (68.4%), and 62 (65.3%) respondents, respectively (Table 2). The variables showed a statistically significant change during the rehabilitation program. A total WAS score increased in average, for all participants, from baseline (5.7) to 12-month follow-up (7.2), moving from the poor category to the moderate category during the rehabilitation period. DWP increased from 45.7% at baseline to 64.4% at the 12-month follow-up. Of the 95 participants, 28 of them reported 100% work participation with 0% change from baseline to 12-month follow-up, which subtract all the participants DWP average. After 12 month, 73% of the participants were working part- or full time. The changes in HRQoL from baseline to 12-month follow-up was 2.57, which was approximately half an SD at baseline. Thus, a minimal important difference (MID) for clinically significant change was obtained.41 The average BMI decreased from 38.8 kg/m2 to 36.4 kg/m2, a reduction of 6%, still recorded in the category obesity II (BMI 35–39.6). The RTWSE score increased by 13% from baseline to the 12-months follow-up and the participants scored in the upper level of the moderate belief category concerning RTWSE.
Table 2.
Comparison of WAS, DWP, HRQoL, BMI, and RTWSE from Baseline to 12-Month Follow-Up
| Measure | Mean Changes from Baseline to 12-Month Follow-Up | 95% CIa | p values | |
|---|---|---|---|---|
| (n = 68) | WAS | 1.51 | 0.83: 2.20 | <0.001 |
| (n = 95) | DWP | 18.69 | 8.35: 29.02 | 0.001 |
| (n = 68) | HRQoL | 2.57 | 1.35: 3.79 | <0.001 |
| (n = 65) | BMI | −2.33 | −3.10: −1.56 | <0.001 |
| (n = 62) | RTWSE | 15.89 | 4.07: 27.71 | 0.009 |
Note: A paired sample t-test was conducted for each of the explanatory variables.
Abbreviation: aCI, confidence interval.
Sub-analysis of changes from baseline to 12-month follow-up in the “not on sick leave” group was calculated for 27 participants. Further analyses in this small group are not appropriate due to sample size power of 55 to obtain a power of 80% with a significance level of 5%.
Associations with Work Ability Score
In the first research question (Table 3), the unadjusted analysis estimated the effect between change from baseline to 12-month follow-up in the explanatory variables HRQoL, BMI, and RTWSE, with work absence 1 year before entering the rehabilitation program with WAS at 12 months, all adjusted for WAS baseline and background variables age, gender, sick leave diagnosis, and education level. Sick leave diagnosis, education level, RTWEXP, absence days, and changes in HRQoL, RTWSE were all significantly associated with the outcome measure WAS. BMI had no significant association to WAS and was excluded from further analysis.
Table 3.
Associations Between Changes in the 12-Month Follow-Up Period in HRQoL, BMI, and RTWSE with WAS in Combination with Work Absence and RTWEXP, Adjusted for the Background Variables. Unadjusted and Adjusted Multiple Regression Analyses
| Unadjusted Analysis | p values | Intermediate Analysis | p values | Final Analysis | p values | ||||
|---|---|---|---|---|---|---|---|---|---|
| Ba | 95% CI | B | 95% CI | B | 95% CI | ||||
| Age | 0.03 | −0.03: 0.1 | 0.335 | ||||||
| Gender | |||||||||
| Male | 0 | 0 | 0 | ||||||
| Females | −0.64 | −1.99: 0.61 | 0.311 | −0.88 | −1.88:0.11 | 0.081 | −0.55 | −1.56: 0.46 | 0.283 |
| Sick leave diagnosis | 0.067 | 0.090 | 0.214 | ||||||
| MS b | 0 | 0 | 0 | ||||||
| EMDc | 1.82 | 0.29: 3.35 | 0.021 | 1.18 | 0.17:2.53 | 0.086 | 1.13 | −0.14: 2.40 | 0.079 |
| All otherd | 0.66 | −0.77:2.08 | 0.362 | −0.22 | −1.43:0.96 | 0.696 | 0.29 | −1.83: 0.36 | 0.184 |
| Educational level (years) | 0.117 | 0.144 | 0.05 | ||||||
| College/university (>14) | 0.48 | −0.82: 1.78 | 0.460 | −1.00 | −2.08:0.08 | 0.067 | −0.73 | −1.83: 0.36 | 0.184 |
| High school (<13) | 0 | 0 | 0 | ||||||
| Elementary school (<10) | −1.74 | −3.88: 0.39 | 0.108 | −1.24 | −3.14:0.67 | 0.198 | −2.04 | −3.71: −0.36 | 0.018 |
| WASe | 0.40 | 0.18: 0.62 | 0.001 | 0.55 | 0.27:0.83 | <0.001 | 0.49 | 0.28: 0.71 | <0.001 |
| HRQoLf | 0.19 | 0.07: 0.31 | 0.003 | 0.31 | 0.17:0.44 | <0.001 | 0.27 | 0.16: 0.38 | <0.001 |
| BMIf | −0.03 | −0.25: 0.18 | 0.749 | ||||||
| RTWSEf | 0.01 | 0.00: 0.03 | 0.026 | 0.00 | −0.01:0.01 | 0.737 | |||
| RTWEXPe | −0.38 | −0.71: −0.05 | 0.025 | 0.20 | −0.19:0.58 | 0.305 | |||
| Work absence daysg | −0.01 | −0.01: −0.00 | 0.004 | 0.00 | −0.01:0.01 | 0.570 | |||
Notes: Univariate and intermediate analyses. p values less than 0.20 are marked with bold and further included in the intermediate analyses. Multiple regression analysis: Intermediate and final analyses are controlled for the effect of background variables and HRQoL baseline. aUnstandardized regression coefficient (B). bMusculoskeletal diagnosis. cEndocrine, metabolic, and nutritional diagnosis. dAll other reported diagnosis. eValue of baseline. fValue of change from baseline to 12 months. gWork absence, measured as the number of days 1 year before baseline. In the final analyses, statistically significant p values (≤ 0.05) marked in bold. R2 = 0.49 for final analysis.
In the final multivariate linear regression analysis, we analyzed the association between the explanatory variable HRQoL with WAS, adjusted for WAS baseline and gender. The analysis demonstrated that education level, WAS baseline, and change in HRQoL were significantly associated with the outcome measure WAS after participation in the rehabilitation program. The regression model explained almost 50% of the variation in WAS (F [7,59] = 7.99, p < 0.001).
Associations with Degree of Work Participation
In the second research question (Table 4), the unadjusted analysis estimated the effect between change from baseline to 12-month follow-up in the explanatory variables HRQoL, BMI, WAS, RTWSE, RTWEXP with DWP at 12 months all adjusted for DWP baseline and background variables age, gender, sick leave diagnosis, and education level. Diseases in the group “all others,” were associated with lower DWP than the other diagnoses. Sick leave diagnosis, DWP baseline, and RTWEXP were all significantly associated with the outcome measure DWP. Age, educational level, HRQoL, BMI, WAS, and RTWSE were not statistically significant and excluded from further analyses.
Table 4.
Associations Between Changes in the 12-Month Follow-Up Period in HRQoL, BMI, WAS, and RTWSE with DWP in Combination with DWP Baseline and RTWEXP, Adjusted for the Background Variables. Unadjusted and Adjusted Multiple Regression Analyses
| Unadjusted Analysis | p values | Intermediate Analysis | p values | Final Analysis | p values | ||||
|---|---|---|---|---|---|---|---|---|---|
| Ba | 95% CI | B | 95% CI | B | 95% CI | ||||
| Age | 0.24 | −0.65: 1.13 | 0.589 | ||||||
| Gender | |||||||||
| Male | 0 | 0 | 0 | ||||||
| Females | −10.13 | −27.9: 7.65 | 0.261 | −3.05 | −19.53:13.42 | 0.713 | −3.21 | −19.49:13.07 | 0.696 |
| Sick leave diagnosis | 0.065 | 0.171 | 0.131 | ||||||
| MSb | 0 | 0 | 0 | ||||||
| EMDc | 18.10 | −2.38: 39.30 | 0.089 | 10.87 | −9.98:31.72 | 0.303 | 11.20 | −9.17:31.57 | 0.277 |
| All otherd | −7.96 | −29.10:13.19 | 0.457 | −10.35 | −29.65:8.95 | 0.289 | −10.56 | −29.59:8.48 | 0.273 |
| Educational level (years) | 0.705 | ||||||||
| Collage/university (>14) | 7.89 | −11.17:26.95 | 0.413 | ||||||
| High school (<13) | 0 | ||||||||
| Elementary school (<10) | 5.89 | −23.41:35.20 | 0.690 | ||||||
| DWPe | 0.35 | 0.17: 0.52 | <0.001 | 0.02 | −0.21: 0.25 | 0.866 | |||
| HRQoLf | 0.60 | −1.52: 2.72 | 0.575 | ||||||
| BMIf | −1.30 | −2.19: 4.79 | 0.460 | ||||||
| WASf | 0.67 | −3.10: 4.43 | 0.725 | ||||||
| RTWSEf | 0.10 | −0.13: 0.33 | 0.382 | ||||||
| RTWEXPe | −11.45 | −15.91: −6.99 | <0.001 | −10.32 | −16.15: −4.49 | 0.001 | −10.62 | −15.25: −6.03 | <0.001 |
Notes: Univariate and intermediate analyses. p values less than 0.20 are marked with bold and further included in the intermediate analyses. aUnstandardized regression coefficient (B). bMusculoskeletal diagnosis. cEndocrine, metabolic, and nutritional diagnosis. dAll other reported diagnoses. eValue of baseline. fValue of change from baseline to 12-month follow-up. Multiple regression analysis: Intermediate and final analyses are controlled for the effect of background variables and HRQoL baseline. In the final analyses, statistically significant p values (≤ 0.05) marked in bold. R2 = 0.27 for final analysis.
In the final multivariate linear regression analysis, we analyzed the association between the explanatory variable RTWEXP measured at baseline with DWP, adjusted for sick leave diagnosis and gender. RTWEXP at baseline was significantly associated with the outcome measure DWP after participating in the rehabilitation program. The regression model explained almost 30% of the variation in the outcome measure DWP (F [2,85] = 7.82, p < 0.001).
No consequential multicollinearity was found between the explanatory variables in the VIF in either of the final models. Mahalanobis and Cook distance indicated no extreme cases that affected the models. The P-P plot between expected and observed cumulative distributions was acceptable.
Discussion
The present study aimed to investigate which changes in the explanatory factors were associated with WAS and DWP after participation in a VR program for people on or at risk of sick leave due to obesity or obesity-related problems. Changes from baseline to 12-month follow-up showed a statistically significant increase in the WAS score from poor to moderate, as did DWP which could contribute to individual well-being and reduced social security costs to society.8 Most of the participants were working part- or full time after 12 months. An increase in HRQoL with approximately half an SD indicate a minimal important difference (MID) for clinically significant change. Furthermore, a BMI loss of 6% contributes to a reduced risk of cardiovascular diseases and helps prevent early mortality.4,19 The participants also increased their RTWSE to moderate belief about their current ability to resume and handle normal job responsibilities. These changes indicated progress in the participants’ RTW progress, HRQoL, self-rated general physical and mental health, vitality, current stress and lifestyle and behaviors.12,34,35 Changes were clinically relevant, but it should be kept in mind that the study design does not permit any conclusion on causality due to lack of comparison group in the study. In addition, changes may also have been influenced of factors outside this study design.
The paper first aimed to examine which changes from baseline to 12-month follow-up in HRQoL, BMI, and RTWSE and RTW EXP, was associated with WAS at 12-month follow-up. We found a strong association between change in HRQoL and WAS baseline with WAS at 12-month follow-up. The final regression model explained the data well with almost 50% of the variance in the outcome variables. In this model, it is surprising that BMI reduction was not associated with work ability as some studies have found that obesity was associated with lower work ability.27,28 However, other studies have also found that a BMI reduction contributes to a better HRQoL.4 HRQoL is a composite measure of symptoms, mental state, and the ability to engage in various activities which are also necessary to perform work-related activities. Thus, some association between HRQoL and work ability should be expected.27,28 Furthermore, work ability and work participation may also depend on factors unrelated to the individual, such as conditions at the workplace. BMI reduction may therefore indirectly affect work ability through changes in health-related quality of life, and we cannot rule out that this type of intervention also improves work ability through lifestyle changes.12
Secondly, the paper aimed to examine which changes in HRQoL, BMI, RTWSE, WAS and RTW EXP, were associated with DWP at 12-month follow-up. In the final multiple linear regression, RTWEXP was a significant variable for DWP at 12-month follow-up. A positive RTWEXP is closely associated with the participants’ attitude about “I believe I can do,” and the strong association between RTWEXP and DWP indicated that the participants’ own expectations about return to work need to be taken into account to predict RTW.7,15 Surprisingly, no other variables predicted work participation after rehabilitation. Weight loss and improvements in work ability were not associated with work participation, which underlines the complex processes involved and the multitude of factors that may influence work participation. Apparently, these factors were not measured in the present study, but the participants themselves seemed to know how long it would take to return to work and maybe also which factors are important to address.
Comparison with Other Studies
Returning to work following a long-term sick leave can be experienced as particularly challenging, both physically and mentally. In addition, people with obesity tend to profit by changing their lifestyle to increase HRQoL. Other studies indicate that weight loss is related to HRQoL.4 The results also concur with other studies that have found improved HRQoL scores with improved work ability.12,27,28 In the present study, a positive RTWEXP is an important factor for DWP, and this study supports existing literature about RTWEXP.7,14,15 To the authors’ knowledge, there are no studies that have investigated VR with a lifestyle intervention. It is surprising that weight loss, work ability, and RTWSE were not associated with work participation. Other studies have found associations between RTWSE, health-related factors, and WAS with RTW in people with neck or low back pain and common mental disorders.7,14,39 Based on the discrepancy between the existing literature and the research findings, it is highly recommended to emphasize and explore further factors associated with work ability and work participation for people with obesity.
Limitations
The study design precludes any conclusion on causality because it did not include a comparison group. Another limitation concern causes of obesity as an explanatory variable which was not examined in this study. Neither was the empirical documentation for the participants sick-leave diagnosis. Therefore, this study cannot know whether sick-leave diagnosis causes obesity or obesity causes sick-leave. Since this was a small-scale study, more extensive studies are called upon to address factors contributing to work ability and work participation for people on or at risk of sick leave due to obesity or obesity-related problems that struggle in their working life. Whether the results were representative of a broader population of obese individuals cannot be determined. Finally, our results may not be valid for non-Caucasian people.
Strengths
The paper’s main strength was its focus on participants who were on or at risk of sick leave from work due to obesity or obesity-related problems, and that work, and lifestyle was integrated in the VR program intervention. Another strength is that data on social benefits, work participation (full or part-time), sick leave diagnoses and DWP data are not self-reported but obtained on all from NAV for all 95 participants. Moreover, due to the prospective observational design, the VR program and the study findings may be generalized more easily than if specially developed interventions and a randomized controlled trial design had been used, for example. Finally, different data sources provide an explanation on factors affecting WAS and DWP.
Conclusions
RTW is a complex process affected by a combination of health-related, other individual factors and environmental factors. During the VR program in this study, the participants experienced increased work ability, work participation, health-related quality of life, return-to-work self-efficacy and a positive reduction in BMI. The strongest predictor of increased work ability was improved health-related quality of life. High return-to-work expectancy at the beginning of the VR program predict increased work participation. We hope the findings of this study can inform and inspire future research on VR with a lifestyle intervention for people with a body mass index above 30 kg/m2.
Acknowledgments
The authors thank all participants who completed the study questionnaire and the anthropometrics in the 1-year vocational rehabilitation program with a lifestyle component for people on or at risk of sick leave due to obesity or obesity-related problems.
Funding Statement
The Central Norway Regional Health Authority funded this study. Volda University College provided PhD funding for Anita Dyb Linge.
Abbreviations
VR, cocational rehabilitation; HRQoL, health-related quality of life; BMI, body mass index; RTWSE, return-to-work self-efficacy; WAS, work ability score; DWP, degree of work participation; RTWEXP, return-to-work expectancy; cm, centimetres; 'kg, bodyweight; NAV, Norwegian Labour and Welfare Administration; WHO, World Health Organization; ICPC-2, International Classification of Primary Care; VIF, variance inflation factor; SD, standard derivation; MID, minimal important difference.
Data Sharing Statement
Technical appendix, statistical code, and dataset available only by contacting the corresponding author. Technical information about the study on Clinical Trials NCT03286374.
Ethics Approval and Informed Consent
This study was approved by the Norwegian Regional Committee for Medical and Health Research Ethics Central Norway 2017/573 and is registered in Clinical Trials NCT03286374. All written consents to participate in this study followed the laws and guidelines for proper health research and treatment in the Specialized Health Care services in Norway and are in accordance with the Helsinki Declaration.
Consent for Publication
Not applicable.
Author Contributions
CJ has made a significant contribution to the work reported, including to the design of the study protocol. He has made a substantial contribution to the text and substantively revised both the content and editing and agreed on the journal to which the article will be submitted. He has also reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage. In addition, he has agreed to take responsibility and be accountable for the contents of the article.
PL has made a significant contribution to the work reported, including to the statistical design and analysis. He has made a substantial contribution to the text and substantively revised both the content and editing and agreed on the journal to which the article will be submitted. He has also reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage. In addition, he has agreed to take responsibility and be accountable for the contents of the article.
SKB has made a significant contribution to the work reported, including to the design of the study protocol and the statistical design and analysis. He has made a substantial contribution to the text and substantively revised both the content and editing and agreed on the journal to which the article will be submitted. He has also reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage. In addition, he has agreed to take responsibility and be accountable for the contents of the article.
CJ, PL and SKB have agreed to ensure that issues related to the accuracy or integrity of any part of the work, even those in which they were not personally involved, are investigated, resolved and the resolution properly documented.
Disclosure
All authors declare that they have no conflict of interest in this study.
References
- 1.Colditz GA, Dart H. Epidemiology and health and economic consequences. In: Wadden TA, Bray G, editors. Handbook of Obesity Treatment. Guildford Press; 2018:3–24. [Google Scholar]
- 2.Wadden TA, Bray GA. Handbook of Obesity Treatment. Guilford Publications; 2018. [Google Scholar]
- 3.Lehnert T, Stuhldreher N, Streltchenia P, Riedel-Heller SG, König HH. Sick leave days and costs associated with overweight and obesity in Germany. J Occup Environ Med. 2014;56(1):20–27. doi: 10.1097/jom.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 4.Rejeski WJ, Williamson D. Effects of lifestyle interventions on health related quality of life and physical functioning. In: Wadden TA, Bray G, editors. Handbook of Obesity Treatment. The Guildford Press; 2018:223–240. [Google Scholar]
- 5.Neovius K, Neovius M, Kark M, Rasmussen F. Association between obesity status and sick-leave in Swedish men: nationwide cohort study. Eur J Public Health. 2012;22(1):112–116. doi: 10.1093/eurpub/ckq183 [DOI] [PubMed] [Google Scholar]
- 6.Bajorek Z, Bevan S. Obesity and work. Institute for Employment Studies. 2019;526:27. [Google Scholar]
- 7.de Wit M, Wind H, Hulshof CTJ, Frings-Dresen MHW. Person-related factors associated with work participation in employees with health problems: a systematic review. Int Arch Occup Environ Health. 2018;91(5):497–512. doi: 10.1007/s00420-018-1308-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ekberg K, Ståhl C. Employment as a key rehabilitation outcome. In: Bültmann U, Siegrist J, editors. Handbook of Disability, Work and Health. Springer International Publishing; 2020:364–384. [Google Scholar]
- 9.Norwegian Labour and Welfare Administration (NAV). Arbeidsrettet rehabilitering. NAV. 12.02, 2021; Accessed December2, 2021.
- 10.Sewdas R, de Wind A, Abma FI, Boot CRL, Brouwer S. Personal and environmental factors influencing work participation among individuals with chronic diseases. In: Bültmann U, Siegrist J, editors. Handbook of Disability, Work and Health. Springer International Publishing; 2020:385–398. [Google Scholar]
- 11.De Vries H, Fishta A, Weikert B, Rodriguez Sanchez A, Wegewitz U. Determinants of sickness absence and return to work among employees with common mental disorders: a scoping review. J Occup Rehabil. 2018;28(3):393–417. doi: 10.1007/s10926-017-9730-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martimo K-P, Takala E-P. Concepts of work ability in rehabilitation. In: Bültmann U, Siegrist J, editors. Handbook of Disability, Work and Health. Vol. 1. Springer International Publishing; 2020:551–570. [Google Scholar]
- 13.Organization WH. International classification of functioning. Disability and Health (ICF); 2001:28–66. [Google Scholar]
- 14.Cancelliere C, Donovan J, Stochkendahl MJ, et al. Factors affecting return to work after injury or illness: best evidence synthesis of systematic reviews. Chiropr Man Therap. 2016;24(1):32. doi: 10.1186/s12998-016-0113-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aasdahl L, Pape K, Vasseljen O, Johnsen R, Fimland MS. Improved expectations about length of sick leave during occupational rehabilitation is associated with increased work participation. J Occup Rehabil. 2018;29(3):475–482. doi: 10.1007/s10926-018-9808-4 [DOI] [PubMed] [Google Scholar]
- 16.Bandura A. Self-efficacy: the exercise of control. Self-efficacy: the exercise of control. W H Freeman/Times Books/ Henry Holt & Co; 1997:ix, 604–ix, 604. [Google Scholar]
- 17.Nøttingnes C, Fersum KV, Reme SE, Moe-Nilssen R, Morken T. Job-related self-efficacy in musculoskeletal disorders - a questionnaire. Tidsskr nor Laegeforen. 2019;139(11):9. doi: 10.4045/tidsskr.18.0571. [DOI] [PubMed] [Google Scholar]
- 18.Sharples A, Cheruvu C. Systematic review and meta-analysis of occupational outcomes after bariatric surgery. Obes Surg. 2016;27. doi: 10.1007/s11695-016-2367-x [DOI] [PubMed] [Google Scholar]
- 19.Wadden TA, Bakizada ZM, Wadden SZ, Alamuddin N. An overview of the treatment of obesity in adults. In: Wadden TA, Bray G, editors. Handbook of Obesity Treatment. 2nd ed. The Guilford Press; 2018:283–308. [Google Scholar]
- 20.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191. doi: 10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- 21.Bandura A, Adams N, Hardy A, Howells G. Tests of generality of self-efficacy theory. Cognit Ther Res. 1980;4:39–66. doi: 10.1007/BF01173354 [DOI] [Google Scholar]
- 22.Schultz IZ, Stowell AW, Feuerstein M, Gatchel RJ. Models of return to work for musculoskeletal disorders. J Occup Rehabil. 2007;17(2):327–352. doi: 10.1007/s10926-007-9071-6 [DOI] [PubMed] [Google Scholar]
- 23.Kristman VL, Boot CRL, Sanderson K, Sinden KE, Williams-Whitt K. Implementing best practice models of return to work. In: Bültmann U, Siegrist J, editors. Handbook of Disability, Work and Health. Springer International Publishing; 2020:589–613. [Google Scholar]
- 24.Costa-Black KM, Feuerstein M, Loisel P. Work disability models: past and present. In: Loisel Paa JR, editor. Handbook of Work Disability. Springer; 2013:71–93. [Google Scholar]
- 25.Knauf MT, Schultz IZ. Current conceptual models of return to work. In: Schultz I, Gatchel R, editors. Handbook of Return to Work. Springer; 2016:27–51. [Google Scholar]
- 26.Bültmann U, Siegrist J. Handbook of Disability, Work and Health. Springer International Publishing; 2020. [Google Scholar]
- 27.Oellingrath IM, De Bortoli MM, Svendsen MV, Fell AKM. Lifestyle and work ability in a general working population in Norway: a cross-sectional study. BMJ Open. 2019;9(4):e026215. doi: 10.1136/bmjopen-2018-026215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaleta D, Makowiec-Dabrowska T, Jegier A. Lifestyle index and work ability. Person-related factors associated with work participation in employees with health problems: a systematic review. Int J Occup Med Environ Health. 2006;19(3):170–177. doi: 10.2478/v10001-006-0021-x [DOI] [PubMed] [Google Scholar]
- 29.Sick leave recommendations (The Norwegian Directorate of Health); 2015.
- 30.Loisel P, Buchbinder R, Hazard R, et al. Prevention of work disability due to musculoskeletal disorders: the challenge of implementing evidence. J Occup Rehabil. 2005;15(4):507–524. doi: 10.1007/s10926-005-8031-2 [DOI] [PubMed] [Google Scholar]
- 31.Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. Guilford Press; 2012. [Google Scholar]
- 32.Sverre Mæhlum K, Kulseng B, Tonstad S, et al. Forebygging, utredning og behandling av overvekt og fedme hos voksne. Nationale Guidlines for Primary Care. Directorate of Health, Editor; Accessed March2, 2021.
- 33.Gould R, Ilmarinen J, Järvisalo J, Koskinen S Dimensions of work ability: results of the Health 2000 Survey. Finnish Centre for Pensions (ETK), The Social Insurance Institution (Kela), National Public Health Institute (KTL), Finnish Institute of Occupational Health (FIOH); 2008.
- 34.Ahlstrom L, Grimby-Ekman A, Hagberg M, Dellve L. The work ability index and single-item question: associations with sick leave, symptoms, and health-a prospective study of women on long-term sick leave. Scand J Work Environ Health. 2010;36(5):404–412. doi: 10.5271/sjweh.2917 [DOI] [PubMed] [Google Scholar]
- 35.Van den Berg TI, Elders LA, de Zwart BC, Burdorf A. The effects of work-related and individual factors on the Work Ability Index: a systematic review. Occup Environ Med. 2009;66(4):211–220. doi: 10.1136/oem.2008.039883 [DOI] [PubMed] [Google Scholar]
- 36.Moock J, Kohlmann T. Comparing preference-based quality-of-life measures: results from rehabilitation patients with musculoskeletal, cardiovascular, or psychosomatic disorders. Qual Life Res. 2008;17(3):485–495. doi: 10.1007/s11136-008-9317-6 [DOI] [PubMed] [Google Scholar]
- 37.Alanne S, Roine RP, Räsänen P, Vainiola T, Sintonen H. Estimating the minimum important change in the 15D scores. Qual Life Res. 2014;24(3):599–606. doi: 10.1007/s11136-014-0787-4 [DOI] [PubMed] [Google Scholar]
- 38.Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med. 2001;33(5):328–336. doi: 10.3109/07853890109002086 [DOI] [PubMed] [Google Scholar]
- 39.Shaw WS, Reme SE, Linton SJ, Huang YH, Pransky G 3rd. PREMUS best paper competition: development of the return-to-work self-efficacy (RTWSE-19) questionnaire--psychometric properties and predictive validity. Scand J Work Environ Health. 2011;37(2):109–119. doi: 10.5271/sjweh.3139 [DOI] [PubMed] [Google Scholar]
- 40.Laake P, Hjartåker A, Thelle DS, Veierød MB. Epidemiologiske Og Kliniske Forskningsmetoder. Vol. 1. Gyldendal Akademisk; 2007. [Google Scholar]
- 41.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–592. doi: 10.1097/01.mlr.0000062554.74615.4c [DOI] [PubMed] [Google Scholar]