Abstract
Background and aims:
Lockdown measures aimed at limiting the number of infections and deaths from the coronavirus disease 2019 (COVID-19) have introduced substantial psychosocial stressors in everyday life. We aimed to investigate the influence of the Dutch lockdown on cannabis use and cannabis use disorder (CUD) and investigate relations with change in mental wellbeing and experienced psychosocial stressors during the lockdown.
Design:
Explorative longitudinal baseline-, pre- and during lockdown survey study.
Setting:
The Netherlands, online between January 2019 and May 2020.
Participants:
Community sample of 120 monthly to daily cannabis users and reference group of 63 non-using controls.
Measurements:
Change in cannabis use and CUD symptom severity from baseline to pre-lockdown to post-lockdown. Change in cannabis use motives, mental health, quality of social relationships and job status from pre-lockdown to post-lockdown.
Findings:
In cannabis users, lockdown related to increased cannabis use (B = 1.92, 95% CI 0.23–3.61, p = 0.027), but not CUD symptom severity. Cannabis users experienced 30% job loss and increased loneliness (p < 0.001, BF10 > 100), while contact with partners (p = 0.005, BF10=8.21) and families improved (p < 0.001, BF10 = 19.73), with no differences between cannabis users and control. Generally, mental health problems (all p’s > 0.277, all BF10< 0.139) did not change but individual differences were significant and severity of cannabis use pre-lockdown, COVID-19 related worries, change in anxiety, expansion motives, social motives and family contact all uniquely related to variance in change in cannabis use or CUD.
Conclusions:
While cannabis use among daily cannabis users in The Netherlands increased at the group level during the period of COVID-19 lockdown, the effect of the first months of lockdown on cannabis use disorder severity and mental wellbeing varied significantly among individual daily cannabis users.
Keywords: COVID-19, cannabis, cannabis use disorder, mental health, social relationships
Introduction
The social distancing measures aimed at limiting the number of infections and deaths from the novel SARS-CoV-2 virus and associated coronavirus disease 2019 (COVID-19) have introduced substantial psychosocial stressors in everyday life, raising concerns regarding the wellbeing of vulnerable populations, including substance users (1,2). The current explorative study assessed the influence of the Dutch lockdown initiated in March 2020 on cannabis use and Cannabis Use Disorder (CUD) severity in a community sample of monthly to daily cannabis users. Furthermore, we investigated if individual change in use and CUD symptoms was related to change in mental well-being and experienced psychosocial stressors during the lockdown.
The Dutch lockdown measures involved social isolation and prolonged confinement at home, including work and school from home. Pandemic-specific anxieties have emerged in the population, with increased levels of worry around personal health and economic consequences (3). Sudden job loss and unemployment have also been an unfortunate reality for many, particularly individuals who work in the retail and food services, culture, accommodation and cleaning sectors (4). Moreover, emerging evidence suggests a 16-28% increase in anxiety and depression symptoms, and an 8% increase in self-reported stress in the general population (5). The increase in experienced stressors and mental health problems, combined with the reduction in alternative positive activities, led to substantial concern from the scientific community about the potential impact on vulnerable populations like substance users (1,2). From previous research on the effects of economic crises on substance use (e.g., the 2008 global recession), we know that high rates of job loss are associated with increased substance use and addiction, especially in young men (6). Job loss is a demonstrated risk factor for cannabis use and unemployed young adults in particular have higher rates of developing a CUD (7,8). CUD is also highly comorbid with anxiety and depression (9,10), and stress is an important factor in the escalation of use, development of addiction, and relapse (11,12). In regular cannabis users particularly, stress and tension reduction are commonly reported motives for use (13), correlating with CUD severity (14).
To our knowledge, previous studies have only cross-sectionally investigated the effect of the virus and lockdown on cannabis use. Increases in cannabis use have been reported in medical cannabis users from the US (15), adult recreational cannabis users in France (16) and adolescent recreational users from Canada (17). In contrast, a survey conducted among the general population in Belgium reported no increase in use (18). These studies suggest that cannabis use may have increased during the lockdown period. To build upon this, the main aim of this exploratory study was to i) investigate if lockdown was associated with change in cannabis use and CUD symptom severity in cannabis users. We invited a unique sample of cannabis users and non-cannabis using controls who completed a survey about their cannabis use prior to the pandemic (baseline) to fill out an online survey about cannabis use just before (pre-lockdown) and since lockdown (post-lockdown), and other sociopsychological consequences of the lockdown. The second aim was to ii) investigate if pre-to-post-lockdown change in cannabis use and CUD symptom severity related to change in cannabis use motives, mental wellbeing, quality of social relationships, and job status. For reference, we checked iii) if changes observed in cannabis users differed from changes observed in a smaller group of non-cannabis using controls. Given the unique nature of the lockdown, all analyses were explorative. However, we expected a general increase in cannabis use and CUD symptom severity pre-to-post lockdown (16), that related to decreases in general mental wellbeing. We also expected that increases in cannabis use and CUD symptoms would relate to increases in cannabis coping motives (14), decreases in social relationship quality (19,20), and job loss (7,8).
Materials and Methods
Participants
Study protocols were approved by the Ethics Review Board of the Faculty of Social and Behavioral Sciences, University of Amsterdam (2020-DP-12211). Individuals who completed an eligibility screener for a different CUD study and agreed to be contacted for future studies were invited to participate. Individuals were originally recruited using social media advertising and in-person flyers targeted at daily or near-daily cannabis users and non-using controls (<25 lifetime uses) who do not regularly use other illicit substances. Of the 1030 invited individuals, 186 agreed to participate in this new study for which they completed the follow-up survey and consented to merging of the screening data with the follow-up survey. Among those, 8×25 Euro online shop vouchers were raffled. Three participants were excluded due to daily other substance use (1 control for daily GHB use, 1 control for regular use of multiple illicit drugs other than cannabis, and 1 cannabis user for daily methamphetamine use). The final sample consisted of 120 cannabis users aged 18-46 who reported monthly to daily cannabis use before lockdown (baseline and/or pre-lockdown) and, for reference, a group of 63 sporadic to non-cannabis using controls aged 18-31.
Questionnaires
March 12, 2020 marked the onset of the Dutch lockdown. Each participant completed a baseline and follow-up questionnaire. The baseline questionnaire was completed on average 265 days (SD= 144.4; range: 26-467 days) prior to the lockdown and assessed use of cannabis and other substances. The follow-up questionnaire contained retrospective questions about the period before lockdown (pre-lockdown) and during lockdown (post-lockdown) and was conducted on average 59 days (SD= 8.6, range: 47-79) after the lockdown began, before any regulations were loosened. Table 1 shows an overview of the substance use measures collected for the baseline, pre-lockdown and post-lockdown periods. Table 2 shows an overview of all other measures collected at follow-up. The assessment time frames for each participant are shown in Supplementary Figure 1.
Table 1.
Overview alcohol and substance use measures assessed for baseline, pre-lockdown and post-lockdown periods
| Cannabis Users (N = 120) | Controls (N = 63) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||||||||
| pre-lockdown | post-lockdown | pre-lockdown | post-lockdown | |||||||||
| N | mean (sd, range) | N | mean (sd, range) | N | mean (sd, range) | N | mean (sd, range) | N | mean (sd, range) | N | mean (sd, range) | |
| Substance use | ||||||||||||
| DSM-5 CUD symptoms | 96 | 4.4 (2.9, 0-11) | 104 | 4.6 (3.0, 0-10) | 104 | 4.3 (3.0, 0-11) | -- | -- | 3 | 0.0 (0.0, 0-0) | ||
| Cannabis use, days month | 96 | 22.2 (9.4, 0-30) | 109 | 20.8 (10.7,0-31) | 109 | 22.0 (10.5, 0-31)# | -- | -- | 9 | 6.4 (4.6, 2-15) | ||
| Cannabis use, grams month | -- | 109 | 17.2 (18.4, 0-94.5) | 109 | 21.53 (20.8, 0-105.4)### | -- | -- | 9 | 3.4 (1.8, 1.5-7.5) | |||
| Illicit substance use, n month | 120 | 3.0 (2.8, 0-11) | 120 | 0.8 (1.5, 0-8.3) | 120 | 1.0 (3.8, 0-31.9) | 63 | 1.3 (1.9, 0-9)*** | 63 | 0.3 (0.6, 0-3.6)** | 63 | 0.5 (1.8, 0-13.5) |
| Cigarette use per day | 53 | 7.4 (5.1, 0-22) | 63 | 8.7 (6.5, 0-25) | 64 | 8.4 (7.3, 0-30) | 6 | 7.8 (4.7, 2-15) | 10 | 8.5 (4.2, 4-18) | 8 | 9.9 (8.2, 0-24) |
| Alcohol use, drinks month | -- | 111 | 28.1 (36.4, 0-202) | 111 | 28.9 (46.4, 0-264) | -- | 58 | 26.2 (25.8, 0-118) | 58 | 28.7 (46.6, 0-264) | ||
| AUDIT, past year | 96 | 6.8 (3.9, 0-18) | -- | -- | 115 | 7.9 (5.7, 0-31) | 57 | 7.1 (4.9, 0-24) | -- | 61 | 7.0 (5.0, 0-22) | |
DSM-5: Diagnostic and Statistical Manual of Mental Disorders; CUD: Cannabis Use Disorder; AUDIT: Alcohol Use Disorder Identification Test; Group differences
p < 0.01
p < 0.001
Within-group effects of time
p < 0.05
p < 0.001.
Bold mean refers to significant results with at least moderate Bayesian evidence support.
Table 2.
Overview all measures assessed at follow-up for pre-lockdown and post-lockdown periods and for pre-to-post lockdown change.
| Cannabis Users (N = 120) | Controls (N = 63) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| pre-lockdown | post-lockdown | pre-lockdown | post-lockdown | |||||||||
| mean | sd | range | mean | sd | range | mean | sd | range | mean | sd | range | |
| Motives for cannabis use | ||||||||||||
| Enhancement | 16.4 | 4.1 | 0-23 | 16.6 | 4.4 | 5-25 | -- | -- | -- | -- | -- | -- |
| Coping | 10.6 | 4.7 | 0-23 | 11.6# | 5.4 | 5-25 | -- | -- | -- | -- | -- | -- |
| Expansion | 11.1 | 6.3 | 0-25 | 10.9 | 6.4 | 5-25 | -- | -- | -- | -- | -- | -- |
| Social | 12.7 | 5.6 | 0-25 | 10.5### | 5.4 | 5-25 | -- | -- | -- | -- | -- | -- |
| Mental health (DSM-5-CCSM) | ||||||||||||
| total | 18.1 | 11.9 | 0-55 | 17.9 | 13.4 | 0-68 | 11.1*** | 7.8 | 0-49 | 11.8** | 8.8 | 0-56 |
| depression | 2.7 | 1.8 | 0-8 | 2.9 | 2.1 | 0-8 | 1.9*** | 1.3 | 0-8 | 2.1** | 1.5 | 0-6 |
| anxiety | 3.0 | 2.6 | 0-12 | 2.9 | 3.0 | 0-12 | 4.2 | 1.9 | 0-9 | 2.5 | 2.2 | 0-12 |
| sleep problems | 1.3 | 1.2 | 0-4 | 1.4 | 1.3 | 0-4 | 0.7** | 0.8 | 0-3 | 0.9* | 1.0 | 0-4 |
| COVID-19 related worries | ||||||||||||
| Personal health | -- | -- | -- | 2.2 | 1.0 | 1.0-5.0 | -- | -- | -- | 1.9 | 0.9 | 1.0-5.0 |
| Personal economics | -- | -- | -- | 2.2 | 1.3 | 1.0-5.0 | -- | -- | -- | 2.0 | 1.1 | 1.0-5.0 |
| Contamination | -- | -- | -- | 2.6 | 0.8 | 1.0-4.7 | -- | -- | -- | 2.5 | 0.8 | 1.0-4.3 |
| Societal functioning | -- | -- | -- | 2.6 | 0.8 | 1.0-4.8 | -- | -- | -- | 2.6 | 0.8 | 1.0-4.3 |
| Employment | ||||||||||||
| Weekly working hours | 16.6 | 15.0 | 0-50 | 9.5 | 14.0 | 0-50 | 16.4 | 13.6 | 0-46 | 8.7 | 12.7 | 0-52 |
| Job loss | -- | -- | -- | 30% | -- | -- | -- | 34% | ||||
| pre-to-post lockdown change | pre-to-post lockdown change | |||||||||||
| mean | sd | range | mean | sd | range | |||||||
| Social contact | ||||||||||||
| Loneliness | 3.6 ### | 0.9 | 1-5 | 3.5### | 0.8 | 2-5 | ||||||
| In-person, partner | 3.1 | 0.9 | 1-5 | 3.2 | 0.9 | 1-5 | ||||||
| In-person, family | 2.6### | 1.1 | 1-5 | 2.6# | 1.2 | 1-5 | ||||||
| In-person, friends | 1.8### | 0.9 | 1-5 | 1.5 ###** | 0.7 | 1-5 | ||||||
| Online, partner | 3.0 | 0.9 | 1-5 | 3.1 | 0.9 | 1-5 | ||||||
| Online, family | 3.3### | 0.8 | 1-5 | 3.2# | 0.7 | 1-5 | ||||||
| Online, friends | 3.7### | 1.0 | 1-5 | 4.0### | 0.9 | 1-5 | ||||||
| Quality, partner | 3.2## | 0.7 | 1-5 | 3.2# | 0.7 | 1-5 | ||||||
| Quality, family | 3.2### | 0.5 | 2-5 | 3.1# | 0.5 | 1-4.5 | ||||||
| Quality, friends | 2.8# | 0.9 | 1-5 | 2.9 | 0.8 | 1-5 | ||||||
Group differences
p < 0.05
p < 0.01
p < 0.001
Within-group effects of time
p < 0.05
p < 0.01
p < 0.001.
Bold means refer to significant results with at least moderate Bayesian evidence support.
Cannabis use and CUD symptom severity:
Our main outcome variables were DSM-5 CUD symptom severity and cannabis use. DSM-5 CUD symptoms were assessed with the MINI 7.0.0 DSM-5 CUD section (21) for the previous year in weekly users at baseline (Cronbach’s α = 0.86), and for the previous year pre-lockdown (Cronbach’s α = 0.83) and the period since lockdown (Cronbach’s α = 0.83) in monthly users, with scores ranging from 0 to 11. At baseline, cannabis use was assessed in days per week for screening purposes. Days per week were multiplied by 4.3 to compute days per month. At follow-up, cannabis use was assessed in days per month over the pre-lockdown and post-lockdown period. Cannabis use in grams per month was assessed over the pre-lockdown and post-lockdown period for descriptive purposes.
Other substance use:
Alcohol use and related problems were assessed with the 10-item Alcohol Use Disorder Identification Test (AUDIT; 22) at baseline (Cronbach’s α = 0.73) and at follow-up (Cronbach’s α= 0.80), both assessments referring to the past year. AUDIT item scores ranged from 0-4 and AUDIT total scores were computed by summing item scores. Alcohol use in drinks per month was assessed at follow-up over the pre-lockdown and post-lockdown period. Cigarette use (yes/no), number of cigarettes per day and frequency of past month illicit substance use were assessed over the baseline, pre-lockdown and post-lockdown period.
Motives for cannabis use:
Motives for use in the year preceding lockdown and period since lockdown were assessed with the 5-item coping (i.e., to reduce negative affect, Cronbach’s α pre-lockdown = 0.81, post-lockdown = 0.88), 5-item social (i.e., to enhance social events, Cronbach’s α pre-lockdown = 0.89, post-lockdown = 0.90), 5-item enhancement (i.e., to enhance positive affect, Cronbach’s α pre-lockdown = 0.74, post-lockdown = 0.81) and 5-item expansion (i.e., expand thoughts and experiences, Cronbach’s α pre-lockdown = 0.96, post-lockdown = 0.96) subscales from the Marijuana Motives Measure (MMM; 23). Each scale contained 5 questions scored on a 5-point Likert scale from ‘almost never’ (1) to ‘almost always’ (5). Scale scores were computed by summing item scores.
Mental Health:
The DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure—Adult (DSM-5-CCSM;5) was administered at follow-up to assess general mental health over the pre-lockdown and post-lockdown period. Substance use items were excluded and assessment time was changed to reflect the year preceding lockdown and period since lockdown. Each item was scored on a 5-point Likert scale from ‘never’ (0) to ‘always’ (4). Given the high comorbidity with CUD (10), we included the total (20-items; Cronbach’s α pre-lockdown = 0.91, post-lockdown = 0.92), depression (2-items; Cronbach’s α pre-lockdown = 0.80, post-lockdown = 0.80), anxiety (4-items; Cronbach’s α pre-lockdown = 0.78, post-lockdown = 0.82) and sleep problems (1-item) scores in further analysis.
COVID-19 related worries: Worries about personal health consequences (2 items; Cronbach’s α = 0.59), personal economic consequences (2 items; Cronbach’s α = 0.80), contamination (2 items; Cronbach’s α = 0.72) and societal consequences (4 items; Cronbach’s α = 0.71) were assessed with a self-developed questionnaire (see Table S1). Each item was scored on a 5-point Likert scale from ‘no worries’ (1) to ‘many worries’ (5). Each worry score reflects the average of the item scores (Cronbach’s α= 0.59-0.80).
Social contact:
Pre to post-lockdown change in frequency of online and in-person contact with partners, family and friends was assessed with 5-point Likert scales from ‘a lot less’ (1) to ‘a lot more’ (5). Pre-post-lockdown change in the quality of contact with partners, family and friend were assessed with 5-point Likert scales from ‘much worse’ (1) to ‘much better’ (5). Change in loneliness pre- to post-lockdown was assessed with a single item, scored on a 5-point Likert scale from ‘a lot less’ (1) to ‘a lot more’ (5).
Statistical analysis
Main analyses in cannabis users
To investigate i) if lockdown was associated with change in cannabis use (days per month) and CUD symptom severity, two separate linear mixed model analyses were conducted. Participants with at least 2 assessments for cannabis use [3 timepoints: N = 96, 2 timepoints: N = 24] or CUD [3 timepoints: N = 81, 2 timepoints: N = 26] were included (missing data resulted from no to minimal cannabis use at either baseline or pre-lockdown). The effects of time [continuous variable with 3 data-points; baseline (minus days before lockdown), pre-lockdown (March 12, 2020 = 0), and post-lockdown (plus days since lockdown)] on both outcomes were assessed using maximum likelihood estimation and a random intercept, with subject and time as random variables to account for repeated measures. Lockdown status (0 at baseline, 0 at pre-lockdown, 1 at post-lockdown) was subsequently added to the model to assess the additional effect of lockdown, followed by the interaction between time and lockdown status. To assess a) individual differences in effects of time and lockdown status, b) potential effects of differences in time between measures, and c) potential non-linear time effects, we assessed model fit after allowing for variable slopes (random slope model), adding a continuous autocorrelation structure of order 1 (with participant as the grouping factor), and assessing quadratic and cubic effects of time respectively. Model fit was assessed using AIC and BIC values of model comparison.
Next, we ii) exploratively investigated if pre-to-post-lockdown change in cannabis use and CUD symptom severity related to change in cannabis use motives, mental wellbeing, social contact, and job status. This was done in multiple steps, first assessing pre-to-post change in cannabis use motives, mental wellbeing and quality of social relationships. Given the non-normal data distributions, non-parametric repeated-measures Friedman tests and Wilcoxon signed-rank tests were used. Next, pre-to-post-lockdown change scores were computed (pre-lockdown minus post-lockdown, reflecting change between lockdown period and the period just before lockdown onset) for these variables and non-parametric Kendall tau-b correlations were computed to assess if change correlated with pre-to-post-lockdown change in cannabis use and CUD symptom severity. Moreover, non-parametric Kruskal-Wallis tests as part of ANCOVAs were run to investigate if pre-to-post lockdown change in CUD symptoms and use (corrected for baseline CUD symptoms and use respectively) differed between cannabis users that did or did not lose their job. Finally, two explorative regression models with feedforward model selection (Bootstrap = 5000, to account for assumption violations) were run to assess which variable(s) uniquely explained change in CUD symptoms and cannabis use, entering both pre-lockdown and change scores in mental wellbeing, marijuana motives, quality of social relationships, and job status.
Comparison between cannabis users and controls
For reference and descriptive purposes, iii) group differences in sample characteristics (including alcohol, cigarette and illicit substance use) and changes in mental wellbeing, quality of social relationships and job status were assessed. Group differences in pre-to-post-lockdown change scores, i.e., loneliness, alcohol use (AUDIT and drinks per months), illicit substance use and DSM-5-CCSM total and subscores were assessed with ANCOVAs (25), correcting for pre-lockdown scores and gender. Given the non-normal data distributions, non-parametric repeated-measures Friedman tests and Mann Whitney U tests were used. Group differences in repeated measures assessed at follow-up, i.e., COVID-19-related worries and change in social contact, were assessed using linear mixed models with maximum likelihood estimation, random intercept, and the within subject variable as a random effect to account for repeated measures.
Bayesian analyses
Given the novelty of the topic, the explorative nature of this study, and to allow for novel hypothesis formation, we decided not to correct for multiple comparisons. Instead, complementary Bayesian analyses were conducted and interpretation of the evidence strength followed Jeffreys benchmarks (26): anecdotal (i.e., not enough evidence to support or refute H0) = BF 1-3, moderate = BF 3-10, strong = BF 10-30, very strong = BF 30-100, and extremely strong = BF > 100. Analyses were run in JASP (JASP team, 2019) and R (version 4.0.2). We considered an effect significant if both p < 0.05 and BF > 3. Analyses were not preregistered.
Results
Pre-lockdown to post-lockdown change in cannabis users
Cannabis use and CUD symptom severity
While time had a small but significant negative effect on cannabis use (Table 3; B= −0.01, 95%CI= −0.01-−0.00, p= 0.022), lockdown was associated with an increase in cannabis use (B= 1.96, 95%CI = 0.26-3.66, p = 0.024). Similarly, comparing pre-lockdown to post-lockdown cannabis use in grams per week, there was very strong evidence for an increase in use (W= 1488.5, p< 0.001, BF10= 62.5, see Table 1). For CUD symptom severity, there was a small but significant interaction between time and lockdown status (B= −0.04, 95%C= −0.08-−0.01, p= 0.025), indicative of a difference in the effect of time on CUD symptom severity during and before lockdown. Post-hoc regression analyses showed no associations between total assessment time (days between baseline and follow-up) and baseline to post-lockdown change in CUD (B= −0.00, t(79)= −0.75 .34, p= 0.457) or between time (days between baseline and lockdown onset) and change in CUD before lockdown (B= −0.00, t(79)= 0.34, p= 0.729). There was a small negative association between time and change in CUD score during lockdown (B= −0.05, t(105)= 2.40, p= 0.018). There was no evidence for a pre-lockdown to post-lockdown change in CUD symptoms (W= 1509.5, p= 0.66, BF10= 0.57).
Table 3.
Overview of final models to assess change in cannabis use (days per month) and CUD symptom severity as a function of time and lockdown status.
| Model coefficients | |||||||
|---|---|---|---|---|---|---|---|
| Model | Fixed effects | Random effects | |||||
| Cannabis use in days per month | B | 95% CI (B) | SE (B) | t | p | SD | 95% CI |
| (Intercept) | 19.26 | 17.30 – 21.22 | 1.00 | 19.25 | <.001 | 9.16 | 7.91 – 10.65 |
| Time | −0.01 | −0.01 – −0.00 | 0.00 | 2.30 | 0.022 | − | − |
| Lockdown Status | 1.96 | 0.26 – 3.66 | 0.87 | 2.26 | 0.024 | − | − |
| Fixed effects | Random effects | ||||||
| DSM-5 CUD symptom severity | B | 95% CI (B) | SE (B) | t | P | SD | 95% CI |
| (Intercept) | 4.61 | 4.06 – 5.17 | 0.28 | 16.30 | < .001 | 2.67 | 2.31 – 3.09 |
| Time | 0.00 | −0.00 – 0.00 | 0.00 | 0.20 | 0.839 | 0.01 | 0.00 – 0.01 |
| Lockdown Status | 2.30 | 0.04 – 4.55 | 1.15 | 2.00 | 0.047 | − | − |
| Time x Lockdown Status | −0.04 | −0.08 – −0.01 | 0.02 | 2.26 | 0.025 | − | − |
DSM-5: Diagnostic and Statistical Manual of Mental Disorders; CUD: Cannabis Use Disorder; Note: models assessing the effect of a continuous autocorrelation structure of order 1, quadratic effects of time and cubic effects of time did not improve model fit. An overview of the model selection can be found in Table S2.
Marijuana Use Motives
Enhancement motives were most prevalent (Figure 1). A Friedman test assessing differences in change in coping, enhancement, social and expansion motives was significant (X2(3)= 37.36, p< 0.001). Post-hoc tests indicated moderate evidence for no change in enhancement (W= 1289.00, p= 0.732, BF10 = 0.110) and expansion motives (W= 1016.50, p= 0.452, BF10= 0.193), but extremely strong evidence for a decrease in social motives (W= 3077.00, p< 0.001, BF10> 100) and anecdotal evidence for an increase in coping motives (W= 645.50, p= 0.003, BF10= 2.84).
Figure 1.
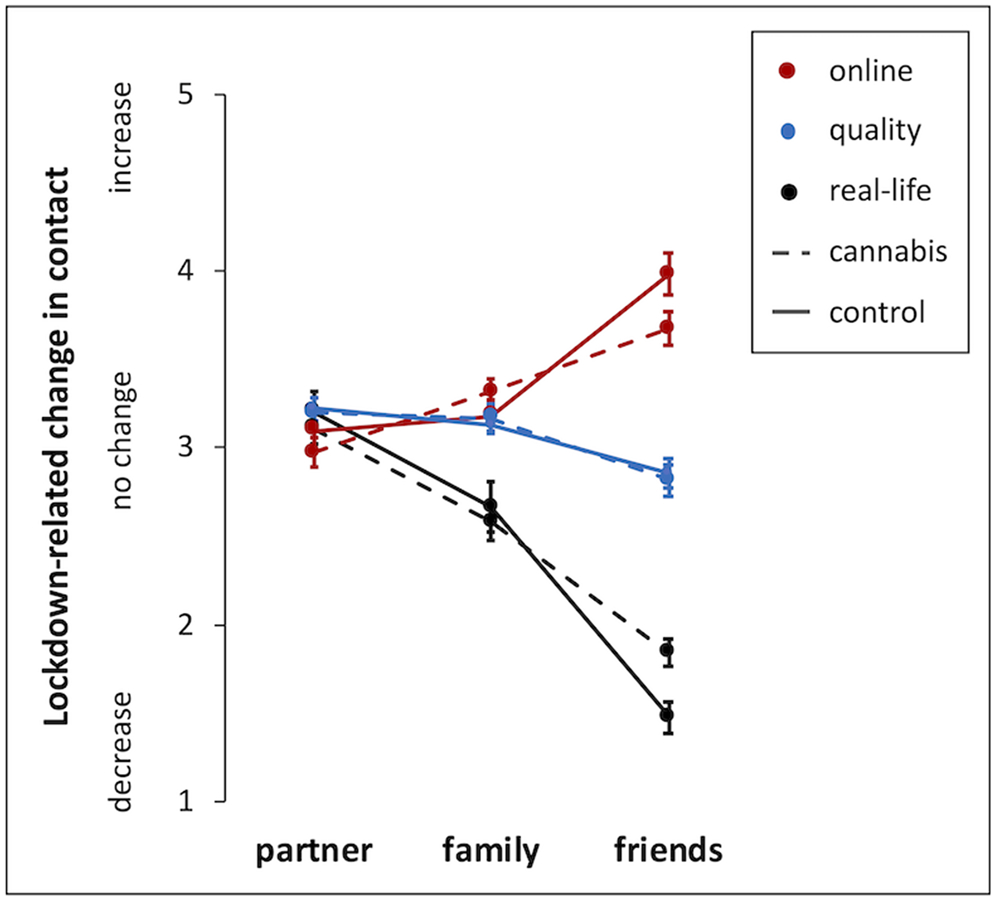
COVID-19 lockdown-related change in in-person, online and quality of contact with partners, family and friends (3 = no change). Means and standard error are reported. A decrease in in-person contact paralleled an increase in online contact with family and friends. Quality increased for partners and family and decreased for friends. Compared to cannabis users, controls showed a larger reduction in in-person contact with friends.
Mental wellbeing
DSM-5-CCSM total, depression, anxiety, and sleep problem scores did not change (all p’s> 0.277, all BF10< 0.139). COVID-19-related worries about personal health, personal economic consequences, contamination, and societal functioning significantly differed from each other (X2(3)= 35.59, p< 0.001). Post-hoc tests indicated equal worries about contamination and societal consequences (W= 3380.00 p= 0.649, BF10= 0.102) that were higher than worries about personal health (contamination-personal health: W= 4741.00, p< 0.001, BF10> 100; societal consequences-personal health: W= 1050.00, p< 0.001, BF10> 100) and economic consequences (contamination-economic consequences: W= 4707.00, p< 0.001, BF10= 25.62; societal-economic consequences: W= 1791.50, p< 0.001, BF10> 100). Participants were equally worried about personal health and economic consequences (W= 2293.00, p= 0.899, BF10= 0.101).
Social contact
Evidence was extremely strong for an increase in loneliness (W= 2690.00, p< 0.001, BF10>100, see Table 2). Regarding pre-to-post lockdown change in social contact (Figure 1, Table 2), change in online (X2(2)= 37.09, p< 0.001), in-person (X2(2)= 73.48, p< 0.001) and quality of (X2(2)= 22.51, p< 0.001) contact differed between partner, family and friends. Post-hoc tests indicated that partner contact in-person (W= 588.00, p= 0.265, BF10= 0.219) and online (W= 344.00, p= 0.675, BF10=0.106) did not change (test-value= 3), but relative to partners, family contact was reduced in-person (W= 2843.00, p< 0.001, BF10> 100) and increased online (W= 918.50, p= 0.002, BF10=15.12). Relative to family, friend contact was reduced in-person (W= 3445.00, p< 0.001, BF10> 100) and increased online (W= 1086.50, p= 0.002, BF10=20.99). Regarding contact quality, there was moderate evidence for improved contact with partners (W= 578.00, p= 0.005, BF10= 8.21) and strong evidence for improved contact with family (W= 1006.00, p< 0.001, BF10= 19.73). Evidence was only anecdotal for decreased contact quality with friends (W= 919.00, p= 0.023, BF10= 1.38).
Pre-to-post lockdown change in cannabis use and CUD symptom severity; associations with change in use motives, mental-wellbeing, social contact, and job status
The current data provide strong evidence for a small positive correlation between change in CUD symptoms and change in enhancement motives and worries about COVID-19 contamination (Table 4). Change in CUD symptoms also correlated weakly positively with DSM-5-CCSM total, anxiety and sleep problems, but with moderate evidence strength. Regarding cannabis use, there was moderate evidence for a weak positive correlation with change in enhancement motives only. Pre-to-post-lockdown change in CUD symptoms (X2(1)= 0.88, p= 0.348) and use (X2(1)= 3.22, p= 0.073) did not differ between cannabis users that did and did not lose their job.
Table 4.
Relations between change cannabis use and change in use motives, mental wellbeing and quality of social relationships
| Self-reported change pre- to post COVID-19 lockdown | |||||
|---|---|---|---|---|---|
| DSM-5 CUD symptoms | Cannabis use, days month | ||||
| Kendall's tau | BF10 | Kendall's tau | BF10 | ||
| Self-reported change pre to post COVID-19 lockdown | Cannabis use, days month | 0.13 | 0.94 | ||
| Social motives | −0.05 | 0.17 | 0.14 | 1.13 | |
| Enhancement motives | 0.23** | 45.85 | 0.19* | 7.32 | |
| Coping motives | 0.08 | 0.28 | 0.15* | 1.71 | |
| Expansion motives | 0.04 | 0.15 | 0.16* | 2.44 | |
| DSM-5-CCSM total | 0.19** | 6.90 | −0.03 | 0.14 | |
| DSM-5-CCSM depression | 0.16* | 2.47 | 0.07 | 0.20 | |
| DSM-5-CCSM anxiety | 0.18* | 4.90 | −0.09 | 0.33 | |
| DSM-5-CCSM Sleep problems | 0.18* | 5.91 | 0.12 | 0.73 | |
| Pre-post change Loneliness | 0.12 | 0.69 | 0.15 | 1.71 | |
| Contact quality partner | −0.06 | 0.18 | −0.03 | 0.14 | |
| Contact quality family | 0.12 | 0.68 | −0.04 | 0.15 | |
| Contact quality friends | −0.06 | 0.20 | 0.06 | 0.20 | |
| COVID-19 related worries | |||||
| - Personal health | −0.00 | 0.13 | 0.04 | 0.15 | |
| - Personal economics | −0.11 | 0.56 | 0.03 | 0.14 | |
| - Contamination | 0.21** | 20.86 | 0.109 | 0.51 | |
| - Societal functioning | −0.00 | 0.13 | −0.03 | 0.14 | |
DSM-5: Diagnostic and Statistical Manual of Mental Disorders; CUD: Cannabis Use Disorder; Motives were measured with the Marijuana Motives Measure; CCSM: Cross-Cutting Symptom Measure
p < 0.05
p < 0.01
p < 0.001
BF10: Bayes factor likelihood H1 relative to H01 with default priors. Bold correlations and Bayes factors refer to significant results with at least moderate Bayesian evidence support.
The regression analysis to explore which variables uniquely explained change in CUD symptoms revealed extremely strong evidence that lower pre-lockdown CUD symptoms, lower worries about personal economic consequences and higher worries about personal health related to increases in CUD symptoms, each significantly explaining unique variance in change (see Table 4). Moreover, larger increases in both anxiety and the quality of family relationships related to increases in CUD symptoms, but with moderate evidence strength. Change in coping motives was a non-significant predictor in the final model.
The regression analysis to explore which variables uniquely explained change in cannabis use revealed very strong evidence that lower pre-lockdown cannabis use and higher expansion motives related to higher increases in cannabis use, each significantly explaining unique variance in change. Moreover, change in CUD symptoms, and social motives also related to increases cannabis use, but with moderate evidence strength. Change in loneliness was a significant predictor in the final model, but with anecdotal evidence strength.
Control analyses adding alcohol, illicit substance use and cigarette use revealed similar results (of note! Power was low due to missing data of non-users).
Cannabis users versus controls
Age (W= 3129.00, p= 0.11, BF10= 0.36) did not differ between groups, but there were more women (cannabis users= 43%; controls= 75%; X2(2)= 17.8, p< 0.001, BF10> 100), more students (cannabis users= 55%; controls= 73%; X2(1)=5.6, p= 0.017, BF10= 3.0) and less cigarette smokers (cannabis users= 55%, controls = 10% at baseline; X2(1)=23.8, p< 0.001, BF10> 100) in the control group. Alcohol use did not change and did not differ between groups (see Table 1). Illicit substance use also did not change, but there was strong evidence for higher baseline (W= 5091.0, p< 0.001, BF10= 16.1) and anecdotal evidence for higher pre-lockdown (W= 4742.5, p= 0.003, BF10= 2.01) use in cannabis users.
Regarding mental wellbeing, cannabis users scored significantly higher on DSM-5-CCSM total, depression and sleep problems (Table 2), however, Bayesian evidence only supported a group difference on pre-lockdown DSM-5-CCSM total (W= 5287.5, p< 0.001, BF10= 62.9) and depression (W= 5287.5, p < 0.001, BF10= 62.9) scores. COVID-19 related worries did not differ between groups (p’s> 0.06, BF10< 0.54). Like in cannabis users, only loneliness significantly increased pre-to-post lockdown in the control group (W= 846.50, p< 0.001, BF10>100), but change in loneliness did not differ between groups.
The percentage of individuals that lost their job during the COVID-19 lockdown did not differ between groups (X2(1)= 0.4, p= 0.51, BF10= 0.23).
Pre-to-post lockdown change in social contact was similar between cannabis users and controls (no main or interaction effects with group, Figure 1), except for frequency of in-person contact (group interaction; χ2(2)= 6.31, p= .04). Post-hoc analysis showed that in-person contact with friends, but not partners of family, was reduced more in controls (W= 4690.50, p= 0.003, BF10= 5.98), with moderate evidence strength.
Discussion
The COVID-19 pandemic and lockdown measures substantially impact daily life, highlighting the importance of monitoring the wellbeing of vulnerable populations, including cannabis users. The cannabis users included in this explorative study used on average 4-5 days per week and 57% had a moderate to severe CUD before lockdown. Our longitudinal survey data showed a significant increase in cannabis use during the first months of lockdown. There was no evidence for a change in CUD symptom severity, but during lockdown, time was weakly associated with reductions in CUD. The increase in use related to an increase in motives to use cannabis for expansion of thoughts and experiences. Moreover, while feelings of loneliness generally increased, both cannabis users and controls reported improved contact with partners and family and no change in symptoms of depression, anxiety or sleep problems, despite ~30% losing their job. These results suggest a minimal impact of the lockdown on mental well-being in cannabis users. However, there were substantial individual differences that need to be taken into account and increased anxiety and worries about the impact of COVID-19 on personal health did relate to increased CUD symptoms.
Which cannabis users are at risk for increasing cannabis use and CUD severity is an important question. We expected lockdown-related decreases in social relationships (19,20), job loss (7,8) and increases in mental health problems to relate to increases in cannabis use and CUD symptoms. Our results reflect changes during the first two months after lockdown and the explorative and partly retrospective nature of this study prevents us from drawing conclusions about causality. Nevertheless, as expected, changes in mental wellbeing covaried with changes in CUD symptom severity, with anxiety explaining unique variance with moderate evidence strength. This relationship is probably bidirectional, with anxiety being both a risk factor for and a consequence of CUD (27). Unexpectedly, job loss did not affect CUD severity or cannabis use and better contact with family predicted an increase in CUD severity. It could be that worries expressed by family members and the feeling of positive family support increased awareness and reporting of the severity of their cannabis use (28), warranting a more long-term and in-depth assessment of lockdown impact on cannabis users’ wellbeing.
The strongest evidence was observed between change in CUD symptom severity and COVID-19 specific worries. Interestingly, in a small US sample Rogers et al. (29) showed that individuals who initiated cannabis use during the pandemic had higher COVID-19 related worries than non-users and pre-pandemic users, supporting the inclusion of COVID-19 related worries in future studies. We observed strong evidence for a positive correlation between contamination worries and change in CUD severity. However, we also observed extremely strong evidence for lower worries about personal economic consequences and higher worries about personal health uniquely predicting increasing CUD severity (on top of baseline CUD severity, change in anxiety and quality of family contact). In both cannabis users and controls, these worries were lower than worries about contamination and societal consequences. The relatively low worries about personal economic consequences, but also the 55% student sample (with perhaps other means of financial support) might explain the lack of an effect of job loss on cannabis use. The link between worry about mental and physical health and increased reported CUD severity may be indicative of self-awareness of cannabis use severity. Compromised self-awareness has been linked to poor addiction prognosis (30), highlighting the need to investigate the impact of the lockdown in more severe clinical populations with CUD.
Regarding cannabis use motives, we observed a reduction in social motives that uniquely explained variance in change of cannabis use, such that a larger reduction in social motives was related to a larger reduction in cannabis use frequency. This intuitively follows the implemented social distancing measures and the significant decrease in in-person contact with friends. We also expected increased in coping motives (14), but our data provides insufficient evidence to support or refute associations with change in cannabis use and CUD symptom severity. In contrast, evidence was very strong for increasing expansion motives predicting increasing use, suggestive of use as a result of lockdown induced boredom and the need for a ‘mental breakout’. Like in previous studies, expansion motives correlated with use, but endorsement is generally low compared to enhancement motives (31,32).
Our longitudinal data on cannabis use and CUD severity, including assessments prior and during the first months of the Dutch lockdown is a clear strength. The negative association between time and change in CUD symptom severity during the lockdown (but no main effect of lockdown), may suggest less change in severity the further away from lockdown onset, or even a potential reduction. This highlights the need for studies that assess the long-term impact of the pandemic in vulnerable populations. Importantly, while cannabis outlets remained open in the Netherlands, the lockdown may have significantly impacted the cannabis market in other countries (33). It is therefore recommended that future studies take potentially restricted access and other cultural factors into account. Moreover, given the impact of the lockdown on social and work life, and the fact that severity of CUD is in part measured by the negative impact of cannabis use on social functioning, the lockdown may fundamentally affect CUD pathology. That is, social distancing and work from home may change CUD symptoms in a way not captured by the MINI 7.0.0 DSM-5 CUD section, warranting future qualitative and quantitative investigations of lockdown related changes in CUD pathology and its underlying mechanisms.
Some limitations should be considered. Although internal consistency of our measures was generally good, the restricted time-frame of the post-lockdown assessment (i.e., self-reported changes over a period of 2 months) and online nature of this study may have impacted the validity of our assessments. Moreover, the online nature of this study may have introduced a sampling bias, missing the most problematic users (34) and a larger, matched, reference group is needed for more fine-grained investigations between cannabis users and controls. While in-person research is currently very limited, research via a video connection may be an option, taking issues with poor non-verbal communication, access and privacy into account (35).
In conclusion, our study provides important first insights into psychosocial consequences of the COVID-19 lockdown on cannabis users. Generally, the lockdown was related to increased cannabis use in cannabis users, and increased loneliness and 30% job loss in both cannabis users and control, but the impact on CUD severity and mental health problems seemed minimal and quality of contact with partners and family improved. Pre-lockdown severity of cannabis use, COVID-19 related worries and increases in anxiety, expansion motives, social motives and quality of family contact all uniquely related to increases in cannabis use or CUD. These findings highlight the importance of studying individual differences and long-term effects of the lockdown.
Supplementary Material
Table 5.
Predictors of change in cannabis use: feed forward model selection
| B | 95% CI bca (B) | SE (B) | b | t | p | BF10 | |
|---|---|---|---|---|---|---|---|
|
Pre- to post COVID 19 lockdown change DSM-5 CUD symptoms: Final model F (6,96) = 11.33, adjuster R2 = 0.48, p < 0.001 | |||||||
| DSM-5 CUD, pre-lockdown | − 0.20 | − 0.30 – − 0.09 | 0.05 | − 0.32 | 4.00 | <0.001 | >100 |
| Coping motives, change | 0.09 | − 0.03 – 0.22 | 0.06 | 0.17 | 1.81 | 0.074 | 1.18 |
| DSM-5-CCSM anxiety, change | 0.21 | 0.04 – 0.38 | 0.08 | 0.25 | 2.65 | 0.009 | 6.16 |
| Change contact quality family | 0.72 | 0.19 – 1.27 | 0.28 | 0.20 | 2.46 | 0.016 | 4.07 |
| COVID-19 related worries, personal economic | − 0.49 | − 0.80 – − 0.23 | 0.14 | − 0.35 | 3.79 | <0.001 | >100 |
| COVID-19 related worries, personal health | 0.77 | 0.38 – 1.19 | 0.21 | 0.39 | 4.08 | <0.001 | >100 |
|
Pre- to post COVID 19 lockdown change cannabis use (days per month): Final model F (5,97) = 14.37, adjuster R2 = 0.40, p < 0.001 | |||||||
| Cannabis use, days months, pre-lockdown | − 0.31 | − 0.45 – − 0.18 | 0.07 | − 0.38 | 4.80 | <0.001 | >100 |
| DSM-5 CUD, change | 0.93 | 0.23 – 1.81 | 0.39 | 0.21 | 2.67 | 0.009 | 6.03 |
| Expansion motives, change | 0.83 | 0.32 – 1.33 | 0.25 | 0.29 | 3.67 | <0.001 | 88.90 |
| Social motives, change | 0.35 | 0.03 – 0.66 | 0.16 | 0.21 | 2.61 | 0.011 | 5.20 |
| Loneliness, change | 1.47 | 0.15 – 2.80 | 0.67 | 0.17 | 2.18 | 0.031 | 2.11 |
DSM-5: Diagnostic and Statistical Manual of Mental Disorders; CUD: Cannabis Use Disorder; Motives were measured with the Marijuana Motives Measure; CCSM: Cross-Cutting Symptom Measure; CI bca: Confidence Interval bias corrected accelerated; SE: Standard Error); 95% CI based on bootstrapping 5000 replications. BS10: Bayes factor likelihood H1 relative to H01 with default priors of including all other measures to the null model. Bold regression results refer to significant effects with at least moderate Bayesian evidence support.
Acknowledgements:
This study was supported by grant 1R01 DA042490-01A1 from the National Institute on Drug Abuse. We like to that the ADAPT lab meeting members for their contribution to the discussion of the finding.
Footnotes
Declarations of competing interest: none
References
- 1.Dubey MJ, Ghosh R, Chatterjee S, Biswas P, Chatterjee S, Dubey S. COVID-19 and addiction. Diabetes Metab Syndr Clin Res Rev 2020; 14: 817–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marsden J, Darke S, Hall W, Hickman M, Holmes J, Humphreys K, et al. Mitigating and learning from the impact of COVID-19 infection on addictive disorders. Addiction 2020; 115: 1007–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee SA. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud 2020; 44 :393–401. [DOI] [PubMed] [Google Scholar]
- 4.Statistics Netherlands (CBS). Economic impact of Covid-19 2020. [cited 2020 Jul 6]. Available from: https://www.cbs.nl/en-gb/dossier/coronavirus-crisis-cbs-figures/economic-impact-of-covid-19
- 5.Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr 2020; 52: 102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dom G, Samochowiec J, Evans-Lacko S, Wahlbeck K, Van Hal G, McDaid D. The impact of the 2008 economic crisis on substance use patterns in the countries of the European Union. Int J Environ Res Public Health 2016; 13: 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poulton RG, Brooke M, Moffitt TE, Stanton WR, Silva PA. Prevalence and correlates of cannabis use and dependence in young New Zealanders. N Z Med J 1997; 110: 68–70. [PubMed] [Google Scholar]
- 8.Henkel D Unemployment and substance use: A review of the Literature (1990–2010). Curr Drug Abuse Rev 2011;4(1):4–27. [DOI] [PubMed] [Google Scholar]
- 9.Agosti V, Nunes E, Levin F. Rates of psychiatric comorbidity among U.S. residents with lifetime cannabis dependence. Am J Drug Alcohol Abuse 2002; 28(4):643–52. [DOI] [PubMed] [Google Scholar]
- 10.Van der Pol P, Liebregts N, De Graaf R, Ten Have M, Korf DJ, Van den Brink W, et al. Mental health differences between frequent cannabis users with and without dependence and the general population. Addiction 2013; 108: 1459–69. [DOI] [PubMed] [Google Scholar]
- 11.Briand LA, Blendy JA. Molecular and genetic substrates linking stress and addiction. Brain Res 2010; 1314: 219–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sinha R The role of stress in addiction relapse. Curr Psychiatry Rep 2007; 9(5):388–95. [DOI] [PubMed] [Google Scholar]
- 13.Hyman SM, Sinha R. Stress-related factors in cannabis use and misuse: Implications for prevention and treatment. J Subst Abuse Treat 2009;36(4): 400–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benschop A, Liebregts N, van der Pol P, Schaap R, Buisman R, van Laar M, et al. Reliability and validity of the Marijuana Motives Measure among young adult frequent cannabis users and associations with cannabis dependence. Addict Behav 2015; 40: 91–5. [DOI] [PubMed] [Google Scholar]
- 15.Vidot DC, Islam JY, Camacho-Rivera M, Harrell MB, Rao DR, Chavez J V., et al. The COVID-19 cannabis health study: Results from an epidemiologic assessment of adults who use cannabis for medicinal reasons in the United States. J Addict Dis 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rolland B, Haesebaert F, Zante E, Benyamina A, Haesebaert J, Franck N. Global Changes and Factors of Increase in Caloric/Salty Food Intake, Screen Use, and Substance Use During the Early COVID-19 Containment Phase in the General Population in France: Survey Study. JMIR Public Heal Surveill 2020];6(3):e19630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dumas TM, Ellis W, Litt DM. What Does Adolescent Substance Use Look Like During the COVID-19 Pandemic? Examining Changes in Frequency, Social Contexts, and Pandemic-Related Predictors. J Adolesc Heal 2020;67(3):354–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vanderbruggen N, Matthys F, Van Laere S, Zeeuws D, Santermans L, Van den Ameele S, et al. Self-Reported Alcohol, Tobacco, and Cannabis Use during COVID-19 Lockdown Measures: Results from a Web-Based Survey. Eur Addict Res 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mason MJ, Zaharakis NM, Rusby JC, Westling E, Light JM, Mennis J, et al. A longitudinal study predicting adolescent tobacco, alcohol, and cannabis use by behavioral characteristics of close friends. Psychol Addict Behav 2017; 31: 712–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boman JH, Heck C. Friendships and Cannabis Use. In: Handbook of Cannabis and Related Pathologies: Biology, Pharmacology, Diagnosis, and Treatment. Elsevier Inc.; 2017. p. 188–97. [Google Scholar]
- 21.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. In: Journal of Clinical Psychiatry. 1998. p. 22–33. [PubMed] [Google Scholar]
- 22.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction 1993; 88: 791–804. [DOI] [PubMed] [Google Scholar]
- 23.Simons J, Correia CJ, Carey KB, Borsari BE. Validating a Five-Factor Marijuana Motives Measure: Relations with Use, Problems, and Alcohol Motives. J Couns Psychol 1998; 45: 265–73. [Google Scholar]
- 24.American Psychiatric Association. DSM-5 self-rated level 1 cross-cutting symptom measure–adult. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 25.Clifton L, Clifton DA. The correlation between baseline score and post-intervention score, and its implications for statistical analysis. Trials 2019; 20: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jeffreys H Theory of Probability 3rd edition. Oxford, UK: Clarendon Press; 1961. [Google Scholar]
- 27.Richardson TH. Cannabis use and mental health: A review of recent epidemiological research. Int Jour Pharmacology 2010: 6: 796–807. [Google Scholar]
- 28.Templeton L, Velleman R, Russell C. Psychological interventions with families of alcohol misusers: A systematic review. Addict Res Theory 2010; 18: 616–48. [Google Scholar]
- 29.Rogers AH, Shepherd JM, Garey L, Zvolensky MJ. Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Res 2020;293:113407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moeller SJ, Goldstein RZ. Impaired self-awareness in human addiction: Deficient attribution of personal relevance. Trends in Cognitive Sciences 2014.; 18: 635–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buckner JD, Zvolensky MJ, Schmidt NB. Cannabis-related impairment and social anxiety: The roles of gender and cannabis use motives. Addict Behav 2012; 37: 1294–7. [DOI] [PubMed] [Google Scholar]
- 32.Bonar EE, Goldstick JE, Collins RL, Cranford JA, Cunningham RM, Chermack ST, et al. Daily associations between cannabis motives and consumption in emerging adults. Drug Alcohol Depend 2017; 178: 136–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Groshkova T, Stoian T, Cunningham A, Griffiths P, Singleton N, Sedefov R. Will the Current COVID-19 Pandemic Impact on Long-Term Cannabis Buying Practices? J Addict Med 2020;6–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pierce M, McManus S, Jessop C, John A, Hotopf M, Ford T, et al. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020; 7: 567–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dodds S, Hess AC. Adapting research methodology during COVID-19: lessons for transformative service research. J Serv Manag 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


