Abstract
Purpose:
To survey TMJ surgeons to determine current practice trends and perceptions regarding the role of discectomy for treatment of temporomandibular joint (TMJ) internal derangements.
Methods:
An anonymous 5-part web-based survey was sent to TMJ surgeons. The survey was created and distributed, and the data were collected with the University of Michigan Qualtrics platform. Responses were compared based on operative volume, tendency to replace the disc, and likelihood of requiring TJR after discectomy. Spearman correlations were used to test statistically significant differences. Domain-level analyses were also performed by summarizing items into 3 domain scores. Analyses were performed in SAS V9.4 (SAS Institute Inc., Cary, NC, USA).
Results:
Fifty-nine surgeons (33.9%) completed the survey. Discectomy was not considered to be a useful procedure by 85% of respondents, and 74% would not consider discectomy as a first surgical option. Most would consider discectomy (64%) before alloplastic total joint replacement. Discectomy was preferred over discopexy for the management of anterior disc displacement with reduction by high volume surgeons (89%), but most (72%) did not feel that discectomy was beneficial over arthroscopy in the treatment of anterior disc displacement without reduction and concomitant degenerative bony changes. In managing symptomatic disc perforation, 66% agreed that discectomy is the procedure of choice and 49% felt that interpositional tissue is indicated in most cases after discectomy. Respondents who reported fewer re-operations requiring alloplastic TJR after discectomy had on average, more positive perceptions of discectomy on the benefit domain (p=0.03), better than alternatives domain (p=0.03), and fewer concerns on the perceived adverse effects domain (p=0.03).
Conclusion:
TMJ surgeons do not employ TMJ discectomy in most cases of TMJ-ID. However, discectomy is considered useful in cases of disc perforation, or for persistent symptomatic disc displacement without reduction, in an attempt to avoid alloplastic TJR. Common adverse effects included joint noises and osteoarthrosis, and the use of interpositional disc replacement tissue did not alter the incidence of adverse effects or complications reported.
Introduction
There is ongoing debate as to the best treatment for internal derangement of the temporomandibular joint (TMJ-ID). Articular disc displacement has been postulated to initiate mechanical problems leading to pain and articular surface degeneration.1,2,3,4,5 Hence, treatments that alleviate this condition by way of disc repositioning or discectomy have been advocated.6,7,8 Proponents of discectomy report high success rates in retrospective studies with long-term follow-up.9,10,11 Some even advocate its use as a primary modality, reasoning that among TMJ surgical procedures, discectomy has the highest probability of success without the need for future interventions.12 However, disc displacement with reduction is also seen as a normal variant in a third of the population without symptoms of pain, nor widespread progression to osteoarthritis.13 Moreover, after discectomy, progressive osteoarthrosis is widely documented14,15, and carries the risk of persistent joint noises, formation of adhesions, ankylosis, malocclusion, decreased joint mobility and limited excursive movement, persistent pain, and possible need for re-reoperation including total TMJ arthroplasty with alloplastic implants. Proponents of disc preservation via discopexy highlight improved outcomes with careful case selection, improved predictability of repair with the advent of bone anchors, and avoidance of progressive osteoarthritis with a chance of condylar regeneration.16
With the increasing recognition of biochemical synovial changes contributing to arthralgia.17,18,19 minimally invasive treatments aimed at tissue preservation and dilution of inflammatory mediators have gained popularity. Proponents of minimally invasive approaches such as arthrocentesis or arthroscopy Pre-prooreport equally high success rates in the management of TMJ arthralgia with TMJ-ID, including several retrospective studies and comparative randomized control trials. Moreover, effective treatment of disc perforation cases have been demonstrated in a significant percentage of subjects undergoing operative arthroscopy, further expanding the application of this minimally invasive modality.20,21
In light of the numerous surgical options and varied opinions in the management of TMJ-ID, this study aims to determine current practice trends and perceptions regarding the role of discectomy for TMJ-ID among TMJ surgeons. Specifically, is discectomy perceived as a useful therapeutic modality for TMJ-ID? How often are surgeons using this modality in their practice? When is discectomy typically employed in the hierarchy of available treatments? When performing discectomy, is there a consensus on the need for disc replacement? What are common complications of discectomy? How often do patients end up needing TJR? Is there a perception among surgeons, that disc replacement prevents any specific side effects of discectomy? What factors contribute to a poor outcome with discectomy? The investigators hypothesize that at least 50% of TMJ surgeons would choose discectomy as the first surgical option for TMJ-ID.
Methods
The Health Sciences and Behavioral Sciences Institutional Review Board (IRB) at the University of Michigan determined on February 25, 2020, that this study was exempt from IRB oversight (#HUM00177009). Recruitment emails were sent to the members of TMJ Concepts Internetwork and American Society of Temporomandibular Joint Surgeons (ASTMJS). Data were collected from the members of TMJ Concepts Internetwork and ASTMJS. In total, surveys were sent to 97 members of ASTMJS and 105 members of the TMJ Concepts Internetwork. A list was created of both groups and cross-referenced to ensure the 27 people who are members of both groups received only 1 email. We received responses from 59 of the 175 members of the TMJ Concepts Internetwork and ASTMJS (response rate 33.7%).
A recruitment email was sent in March 2020 to the members of TMJ Concepts Internetwork and ASTMJS, with a follow-up email sent in May 2020. The email informed the members about the study and asked them to respond to an anonymous web-based survey on the University of Michigan Qualtrics platform, which they could access via a link in the email.
The survey was drafted and piloted with 2 TMJ surgeons (SA and LGM). Feedback was carefully reviewed and a final version was developed. The final survey consisted of 5 parts. The first part collected information on how frequently the surgeon performs discectomy procedures (number of procedures per year), with categories of: 0, 0–10, 11–30, 31–50, and >50. Part 2 asked questions about preferred management of different stages of TMD-ID, and the perceived effectiveness of discectomy, in the form of statements with 5 response choices ranging from “strongly agree” to “strongly disagree”. Part 3 asked about experience seeing adverse effects of discectomy, with answer choices being never, in few cases, in some cases, in most cases, and always. Part 4 asked about avoiding adverse effects of discectomy, with answer choices being never, in few cases,in some cases, in most cases, and always. Part 5 asked about perceptions of the factors that may contribute to unfavorable results after discectomy, with answer choices including: never, in few cases, in some cases, in most cases, and always.
Inclusion criteria included: a completed survey, including an answer to every question. Exclusion criteria included: an incomplete survey.
Item-level analyses were performed by reporting frequencies and percentages for each item-response overall, by number of discectomies (<11 vs. >10), by tendency to replace the disc (replacers vs. non-replacers), and frequencies of discectomy cases requiring TJR (1–10% vs. >10%). Spearman correlations were used to test statistically significant differences. Domain-level analyses were also performed by summarizing items into summary domain scores. The domains are: “perceived benefit domain” representing a mean score of 4 questions concerning the benefits of discectomy, “better than alternatives domain” representing a mean score of 6 questions comparing discectomy to other available surgical options, and “perceived adverse effects domain” representing a mean score of 4 questions concerning the adverse effects of discectomy. Analyses were performed in SAS V9.4 (SAS Institute Inc., Cary, NC, USA)
Results
How often are TMJ surgeons using this modality in their practice?
The majority of respondents (75%) performed 10 or fewer discectomy procedures per year, while 9/59 respondents (15%) performed more than 10 discectomies yearly (high volume surgeons). Another 6 respondents (10%) denied performing discectomy procedures.
Is discectomy perceived as a useful therapeutic modality for the management of TMJ-ID, and if so, when is discectomy employed in the hierarchy of available management options?
In the management of TMJ internal derangements (TMJ-ID), discectomy was not considered to be a useful procedure by most (85%). Similarly, most would not employ discectomy as a first surgical option for TMJ-ID (74%). However, higher volume surgeons were more likely to report good jaw function and pain control with discectomy in the long term (P=0.055), approaching statistical significance, and this group also reported effective control of symptoms after a failed discopexy (P=0.03). Interestingly, 58% would recommend a modified condylectomy instead of discectomy if TMJ symptoms persist after less invasive modalities, and agreement was stronger among those performing fewer TJRs after discectomy (P=0.01). However, in the same scenario, most respondents (64%) would perform discectomy before considering an alloplastic total joint replacement. Table 1 shows the frequencies and percentages for each item-response per question regarding the effectiveness of discectomy, and consideration for its use in the hierarchy of available surgical modalities.
Table 1.
Responses among all providers
| Question | Response n (%)* | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Discectomy is a useful procedure for managing TMJ-ID | 44 (75) | 6 (10) | 6 (10) | 3 (5) | 0 (0) |
| Discectomy is useful as a first surgical option for TMJ-ID | 24 (41) | 20 (34) | 4 (7) | 9 (15) | 2 (3) |
| Discectomy is effective for managing TMJ pain | 15 (26) | 20 (34) | 7 (12) | 9 (16) | 7 (12) |
| Discectomy is effective for managing TMJ locking | 19 (33) | 16 (28) | 10 (17) | 7 (12) | 6 (10) |
| Discectomy is effective if symptoms persist after TMJ arthrocentesis or arthroscopy | 11 (19) | 15 (26) | 13 (22) | 10 (17) | 9 (16) |
| After undergoing TMJ discectomy, most patients have good jaw function and pain control in the long term | 4 (7) | 5 (9) | 19 (33) | 20 (34) | 10 (17) |
| In the management of disc displacement with reduction, discectomy has better outcomes than arthroscopy or arthrocentesis | 18 (32) | 14 (25) | 13 (23) | 6 (11) | 6 (11) |
| In the management of disc displacement without reduction, discectomy has better outcomes than arthroscopy or arthrocentesis | 7 (12) | 9 (15) | 11 (19) | 22 (37) | 10 (17) |
| In the management of disc displacement without reduction and degenerative bony changes, discectomy has better outcomes than arthroscopy or arthrocentesis | 42 (71) | 7 (12) | 4 (7) | 3 (5) | 3 (5) |
| In the management of disc displacement with reduction, discectomy has better outcomes than disc plication (discopexy) | 13 (22) | 7 (12) | 12 (21) | 22 (38) | 4 (7) |
| In the management of disc displacement without reduction, discectomy has better outcomes than disc plication (discopexy) | 8 (14) | 5 (9) | 11 (19) | 23 (40) | 11 (19) |
| Discectomy is effective if symptoms persist after disc plication) | 7 (12) | 5 (9) | 10 (17) | 27 (47) | 9 (16) |
| It is preferable to avoid discectomy and recommend a modified condylotomy if TMJ symptoms persist after conservative measures (may include non-surgical or minimally invasive surgical options) | 7 (12) | 7 (12) | 11 (19) | 25 (42) | 9 (15) |
| An eminectomy should be performed at the time of discectomy | 18 (31) | 15 (25) | 18 (31) | 4 (7) | 4 (7) |
| Osteoplasty of the fossa and/or condyle is usually indicated at the time of discectomy | 19 (32) | 18 (31) | 10 (17) | 11 (19) | 1 (2) |
| Interpositional tissue is indicated in most cases after discectomy | 13 (22) | 11 (19) | 6 (10) | 14 (24) | 15 (25) |
| Interpositional tissue improved pain and function after TMJ discectomy | 11 (19) | 13 (22) | 13 (22) | 13 (22) | 9 (15) |
| A fossa-eminence alloplast should be implanted after discectomy | 44 (75) | 10 (17) | 4 (7) | 0 (0) | 1 (2) |
| The fossa-eminence alloplast improves pain and function after discectomy | 38 (66) | 9 (16) | 10 (17) | 0 (0) | 1 (2) |
| Instead of discectomy, an alloplastic total joint replacement is indicated if TMJ symptoms persist after conservative measures (may include non-surgical or minimally invasive surgical options) | 21 (36) | 17 (29) | 4 (7) | 12 (20) | 5 (8) |
| Discectomy is the procedure of choice before considering alloplastic total joint replacement for patients with symptomatic disc displacement without reduction | 10 (17) | 9 (15) | 6 (10) | 22 (37) | 12 (20) |
| Discectomy is the procedure of choice if the disc is perforated on arthroscopy/MRI and symptoms persist | 10 (17) | 5 (8) | 5 (8) | 22 (37) | 17 (29) |
| Discectomy is the procedure of choice before considering alloplastic total joint replacement for symptomatic patients with late stage TMD-ID and degenerative condylar changes of the TMJ) | 16 (27) | 13 (22) | 6 (10) | 16 (27) | 8 (14) |
| An alloplastic total joint replacement is the procedure of choice if the disc is perforated on arthroscopy/MRI and symptoms persist | 15 (25) | 15 (25) | 11 (19) | 11 (19) | 7 (12) |
| Most patients who undergo TMJ discectomy need additional surgery such as alloplastic total joint replacement | 8 (14) | 15 (25) | 12 (20) | 15 (25) | 9 (15) |
1=Strongly disagree; 2=Somewhat disagree; 3=Neither agree nor disagree; 4=Somewhat agree; 5=Strong agree
ADDwR
In the management of disc displacement with Prereduction, arthroscopy or arthrocentesis were felt to be more useful than discectomy. 89% of high volume surgeons felt that discectomy has better outcomes than discopexy in the management of ADDwR (P<0.01), while only 37% of those performing 10 or fewer discectomies per year agreed with that statement.
ADDwoR
In the management of disc displacement without reduction, discectomy was favored over lavage procedures (i.e. arthroscopy), discopexy, and alloplastic TJR, especially among higher volume surgeons and those reporting fewer TJRs after discectomy. However, in considering cases of ADDwoR with concomitant degenerative bony changes, a majority consensus was seen, where 72% strongly disagreed and 12% somewhat disagreed that discectomy has better outcomes than arthroscopy or arthrocentesis.
Disc Perforation
Majority of respondents (66%) agreed that discectomy is the procedure of choice for managing symptomatic disc perforation, and 31% would employ alloplastic TJR. The latter modality was significantly more common among surgeons who reported requiring TJR after discectomy in >10% of cases (P=0.03). Similarly, this group agreed with a higher prevalence (62%), that most patients who undergo TMJ discectomy need additional surgery such as alloplastic TJR (p<0.01).
Late stage TMJ-ID with DJD
However, responses were more heterogeneous in the management of symptomatic late stage TMJ-ID with degenerative condylar changes. In the latter scenario, slightly greater preference was found for alloplastic TJR over discectomy; however, the higher volume surgeons (78%) still favored a discectomy procedure (P=0.01).
Is there a consensus on the need for osteoplasty and disc replacement?
Majority of respondents somewhat disagreed or strongly disagreed (56%) that an eminectomy should be performed at the time of discectomy, and 30.5% neither agreed nor disagreed. Similarly, most disagreed with the need for osteoplasty of the fossa and/or condyle at the time of discectomy. 49% felt that interpositional tissue is indicated in most cases after discectomy, while 41% disagreed. When asked “after discectomy, I replace the disc with” and select all that apply, 46% of all respondents reported replacing the disc with fat, 44.1% chose no replacement, 10% with temporalis fascia, 5% with dermal-fat, 5% with silastic sheet, 5% other, 3% temporalis muscle, and 1.7% with dermis only.
Other responses included cryopreserved umbilical membrane and cryopreserved cartilage allograft. Of the higher volume surgeons, 78% agreed with the use of interpositional tissue in most cases, which was significantly more than the low volume group (P=0.02).
Compared to non-replacers, the majority of respondents (65%) who tended to replace the disc agreed that interpositional tissue improved pain and function after discectomy (P<0.01).
Only 1 respondent felt that a fossa-eminence alloplast is beneficial after discectomy.
After discectomy, 44% of respondents do not replace the disc, while most report replacing the disc, most commonly with autogenous fat (46%).
After discectomy, 10% or fewer patients go on to have a TJR according to 47% of respondents, while 35% of respondents reported that over 25% of patients require TJR after discectomy. However, even among those reporting fewer patients needing TJR, only 42% agreed about discectomy being effective for managing pain (P=0.04), and majority (59%) reported it was not effective for managing locking of the TMJ. An even distribution of responses was seen in response to the effectiveness of discectomy to manage persistent symptoms after TMJ lavage procedures.
After discectomy, how many patients require future TMJR?
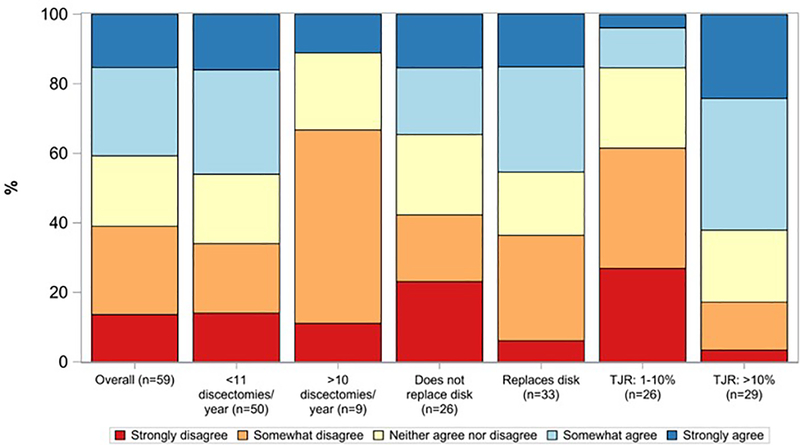
41% of respondents somewhat agreed or strongly agreed that most patients undergoing discectomy need additional surgery such as alloplastic TJR. Another 20% neither agreed nor disagreed with this statement. There was no significant difference in responses between high and lower volume surgeons, or between disc replacers and non-replacers (Figure 1). As expected, respondents reporting higher rates of TJR after discectomy were significantly more likely to agree with this statement (65%) compared to those with lower TJR rates after discectomy (p-<0.01).
Figure 1. Responses to “Most patients who undergo TMJ discectomy need additional surgery such as alloplastic total joint replacement” for the overall group, and stratified by operative volume, tendency to replace the disc, and likelihood of needing TJR after discectomy.
Discectomies/year p=0.12; Replaces disc? p=0.34; TJR (%) p<0.001.
What are common adverse effects of discectomy?
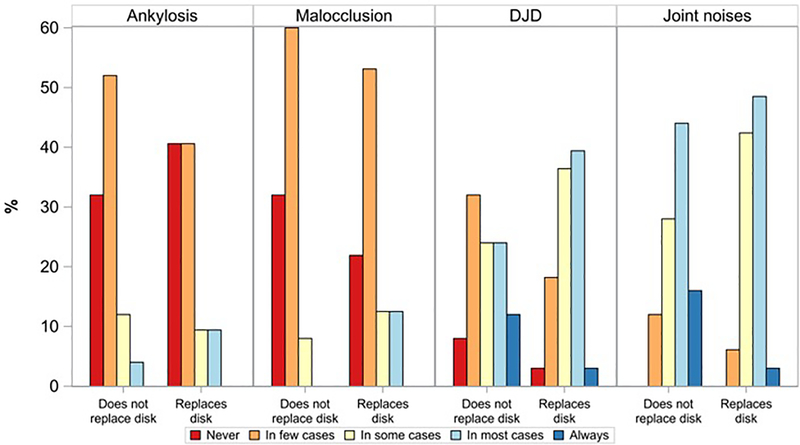
Respondents were queried about the frequency with which they experienced ankylosis, malocclusion, degenerative joint disease (DJD), and joint noises after discectomy. Ankylosis was reported in some or most cases by 18%, and in few cases by 46%. Those with higher rates of TJR after discectomy reported this complication most commonly (p=0.03). Malocclusion was reported in some or most cases by 18% and in few cases by 56%. No statistical differences were seen by respondent volume, tendency to use a disc replacement, or TJR rates after discectomy (Figure 2). DJD or adaptive remodeling of the condyle and/or fossa was reported always by 7%, in some or most cases by 64% and in few cases by 24%. Tendency to replace the disc did not have a significant impact on the likelihood of this observation. Finally, joint noises were reported always by 9%, in some or most cases by 82%, and in few cases by 9% (Table 2).
Figure 2. Responses to “Please indicate how often you have experienced the following adverse effects of TMJ discectomy” stratified by tendency to replace the disc.
Ankylosis p=0.75; malocclusion p=0.12; DJD p=0.41; Joint noises p=0.42.
Table 2.
Responses among all providers
| Please indicate how often you have experienced the following adverse effects of TMJ discectomy | Response n (%)* | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Ankylosis | 21 (37) | 26 (46) | 6 (11) | 4 (7) | 0 (0) |
| Malocclusion | 15 (26) | 32 (56) | 6 (11) | 4 (7) | 0 (0) |
| Degenerative or remodeling condyle and/or fossa changes (DJD) | 3 (5) | 14 (24) | 18 (31) | 19 (33) | 4 (7) |
| Joint noises | 0 (0) | 5 (9) | 21 (36) | 27 (47) | 5 (9) |
1=Never; 2=In few cases; 3=In some cases; 4=In most cases; 5=Always
Avoiding adverse effects of discectomy
Use of disc replacement to avoid adverse effects of discectomy was evaluated by comparing respondents reporting doing so never or in few cases versus some/most/all cases (Table 3). Compared to non-replacers, disc replacers were significantly more likely to replace the disc to avoid ankylosis (p<0.01), to avoid malocclusion (p<0.01), to avoid DJD (p<0.01), and to decrease joint noises (p<0.01). However, our results did not show a statistical difference in the incidence of complications between replacers and non-replacers.
Table 3.
Responses among all providers
| Question | Response n (%) | |
|---|---|---|
| Never/in few cases | In some/most/all cases | |
| I replace the disc with interpositional material to avoid ankylosis | 26 (46) | 31 (54) |
| I replace the disc with interpositional material to avoid malocclusion | 44 (77) | 13 (23) |
| I replace the disc with interpositional material to avoid DJD | 36 (63) | 21 (37) |
| I replace the disc with interpositional tissue to decrease joint noises | 40 (70) | 17 (30) |
| I use an oral appliance after discectomy to avoid malocclusion | 35 (63) | 21 (38) |
| I use guiding elastics after discectomy to avoid malocclusion | 43 (75) | 14 (25) |
To avoid malocclusion after discectomy in some/most/all cases, oral appliances were reported by 38% of respondents and guiding elastics were reported by 25%. No differences were seen between groups of respondents.
What factors contribute to poor outcomes after discectomy?
Strong agreement was seen regarding factors that contribute to poor outcomes after discectomy (Table 4). The following factors were considered likely or very likely to lead to an unfavorable result: 2 or more prior surgery (86%), advanced Wilkes stage (81%), neuropathic pain (81%), myofascial pain (76%), fibromyalgia (74%), catastrophizing character (74%), rheumatological condition (72%), history of bruxism (72%), somatization (71%), muscle spasms (69%), depression (67%), anxiety (64%), subchondral bone disease (66%), chronic fatigue syndrome (62%), malocclusion (53%). Most other respondents were unsure if the above factors contribute to unfavorable outcomes after surgery. Conversely, there was no agreement regarding hypermobility as a risk factor for an unfavorable outcome after discectomy.
Table 4.
Responses among all providers
| How likely are the following factors to contribute to an unfavorable result after discectomy?: | Response n (%)* | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Number of prior surgeries (2 or more) | 1 (2) | 2 (3) | 5 (9) | 20 (34) | 30 (52) |
| Subchondral bone disease (inflammation, edema, sclerosis) | 1 (2) | 2 (3) | 17 (29) | 27 (47) | 11 (19) |
| History of bruxism and/or clenching | 2 (4) | 4 (7) | 10 (18) | 28 (49) | 13 (23) |
| Wilkes stage | 1 (2) | 2 (3) | 8 (14) | 26 (45) | 21 (36) |
| Malocclusion (unstable occlusion of any type | 5 (9) | 2 (3) | 20 (34) | 22 (38) | 9 (16) |
| Neuropathic pain (such as burning or electric pain) | 3 (5) | 0 (0) | 8 (14) | 16 (28) | 31 (53) |
| Fibromyalgia | 2 (3) | 2 (3) | 11 (19) | 24 (41) | 19 (33) |
| Chronic fatigue syndrome | 2 (3) | 4 (7) | 16 (28) | 20 (34) | 16 (28) |
| Depression | 2 (3) | 4 (7) | 13 (22) | 25 (43) | 14 (24) |
| Anxiety | 1 (2) | 5 (9) | 15 (26) | 26 (45) | 11 (19) |
| Catastrophizing character | 3 (5) | 3 (5) | 9 (16) | 24 (41) | 19 (33) |
| Somatization | 2 (3) | 3 (5) | 12 (21) | 21 (36) | 20 (34) |
| Hypermobility | 2 (4) | 18 (32) | 20 (35) | 15 (26) | 2 (4) |
| Rheumatological condition | 1 (2) | 1 (2) | 14 (24) | 28 (48) | 14 (24) |
| Muscle spasms | 0 (0) | 3 (5) | 15 (26) | 29 (50) | 11 (19) |
| Myofascial pain | 1 (2) | 2 (3) | 11 (19) | 31 (53) | 13 (22) |
1=Very unlikely; 2=Unlikely; 3=Unsure; 4=Likely; 5=Very likely
Domain analysis
Respondents who reported fewer re-operations requiring alloplastic TJR after discectomy had on average, more positive perceptions of discectomy on the benefit domain (mean 2.8 vs. 2.2, p=0.03), and fewer concerns on the perceived adverse effects domain (mean 3.2 vs. 3.6 p=0.01). There were no significant differences on the 3 domains between surgeons in terms of operative volume or tendency to replace the disc.
Discussion
Internal derangement of the temporomandibular joint (TMJ-ID) is a term used to refer to an abnormality in articular disc position and morphology, and this has been previously proposed as a possible etiology of TMJ pain and mechanical limitations.1,2,3,4,5 TMJ discectomy was originally described in 1909 by Lanz, and is 1 of the oldest reported open TMJ operations for the management of a painful TMJ-ID.6 However, the role of disc displacement in the pathogenesis of intra-articular TMJ pain has been questioned with data showing that approximately a third of the individuals have asymptomatic disc displacement without dysfunction. In addition, widespread evidence of similar success after lavage procedures that do not alter the disc position cast further doubt on the value of discopexy and discectomy.17,18,19,22,23,24,25 These different conceptual frameworks for the pathogenesis of intra-articular TMJ disease are not mutual exclusive, as many patients with TMJ arthralgia have both an articular disc disorder and inflammatory synovial changes.
This survey study of TMJ surgeons had the goal of understanding current perceptions regarding the role of discectomy for the management of TMJ-ID. Specifically we sought to determine the role of discectomy among other surgical options, the frequency with which it is being employed, the need for a disc replacement after discectomy, common complications, the likelihood of progressing to TJR after discectomy, and concomitant conditions that may negatively impact outcomes after TMJ discectomy.
Significant heterogeneity was seen among respondents, indicative of a multitude of clinical opinions and experiences. The overwhelming majority of surgeons surveyed do not consider discectomy to be a useful therapeutic modality in the management of TMJ-ID. This corresponds with several other survey responses, notably that 75% of TMJ surgeons surveyed perform 10 or fewer discectomies per year, 74% do not consider discectomy as a first surgical option, and 80% did not favor the use of discectomy to manage TMJ pain or locking. This information suggests that discectomy is less often utilized than other surgical modalities. The exception to this included disc perforation, where two thirds of respondents agreed that discectomy is the procedure of choice if symptoms persist after arthroscopy. Moreover, over half of respondents would consider discectomy before TJR for disc displacement without reduction, while fewer would consider this option for late stage ID with degenerative condylar changes.
When comparing discectomy and arthroscopy (or arthrocentesis) for the treatment of patients with Wilkes 3 and 4 staging of TMJ disease, comparative outcome studies indicate that arthroscopy has similar outcomes while also being minimally invasive, cost effective, and results in a short recovery.26,27 Moreover, there is evidence that subjects with chronic disc displacement without reduction (Wilkes stage 4) experience greater improvements in pain and mouth opening than those in other Wilkes stages.28 Despite the advantages of less invasive modalities, respondents in this study favored discectomy over lavage procedures for the treatment of ADDwoR. This may indicate that clinical experience differs from the literature, or that other factors are guiding clinical decisions. Interestingly, for ADDwoR, with concomitant degenerative bony changes, the majority of respondents believed that discectomy has no advantages over arthoscopy or arthrocentesis. However, prior retrospective data demonstrated that discectomy was successful in a majority of Wilkes’ stage IV and V cases.29 In the management of disc displacement with reduction (ADDwR), respondents felt that arthroscopy or arthrocentesis is more useful than discectomy while greater heterogeneity was seen regarding the use of discopexy versus discectomy for ADDwR. While there is merit in disc preservation via discopexy, several host factors and technical details may account for less predictable outcomes as compared to discectomy.
We hypothesized that at least 50% of TMJ surgeons would choose discectomy as the first surgical option for TMJ-ID. When considering TMJ-ID in general, our data does not support our hypothesis. However, our hypothesis is supported in the setting of ADDwoR without bony changes and disc perforation specifically.
Our survey questions aimed to determine the frequency and reasons for use of interpositional tissue (IPT) or material after discectomy. Different types of autogenous, alloplastic, and allogeneic materials have been used as IPT after discectomy with mixed results.30,15,31,32 Overall, studies evaluating outcomes of TMJ discectomy have reported favorable outcomes for most patients whether or not disc replacement was used.32,33 Among our survey respondents, there was significant heterogeneity in the use of IPT after discectomy. Nearly half of surgeons surveyed agreed that it is necessary to replace the disc with IPT (replacers), while half did not (non-replacers). Among replacers, the majority used autogenous fat as the tissue of choice. The majority of high volume surgeons agreed with the use of IPT in most cases, while fewer respondents in the low volume group employed IPT. Additionally, compared to non-replacers, most respondents who replaced the disc agree that the use of IPT improved pain and function after discectomy.
Respondents who replaced the discreported doing so to avoid complications after discectomy; however, our results indicate that there is no difference in incidence of complications, such as joint noises, malocclusion, osteoarthrosis (DJD), and ankylosis, between replacers and non-replacers. Joint noises were reported most commonly after discectomy (91% always/most/some cases), followed by adaptive remodeling or DJD (71%), malocclusion (18%), and ankylosis (18%). Some respondents reported using oral appliances or guiding elastics to prevent malocclusion as well. One study found that discectomy with the use of a dermis graft minimized crepitus, but did not prevent progressive osseous degeneration of the mandibular condyles in any subjects.15
Moreover, a larger study using the condylar morphology scale noted that dermis-fat grafts fail to prevent significant condylar changes in one third of patients who underwent discectomy.31 A recent review of 19 subjects treated with discectomy and abdominal fat graft found that nearly all those with good outcomes post-operatively had progressive flattening of the condylar head at 2 year follow-up, and 3 subjects without improvement had progressive DJD. Among those meeting clinical success criteria, crepitus was noted in 50% prior to surgery, and in 37.5% after surgery.32 We did not assess complications related to facial paralysis, neurosensory function, scar quality, or donor site morbidity. While it is possible that IPT may help prevent ankylosis after discectomy in some cases, or that it may lessen the severity of crepitus in some cases, these hypothetical benefits remains to be elucidated.
In considering factors that may negatively influence outcomes after discectomy, strong agreement was seen with two thirds or more of respondents agreeing that the following factors contribute to an unfavorable result: 2 or more open surgeries, advanced Wilkes stage, neuropathic pain, myofascial pain, fibromyalgia, catastrophizing character, rheumatologic condition, history of bruxism, somatization, muscle spasms, and depression. Studies on outcomes of TMJ TJR have also found that multi-operated patients tend to have less favorable improvements in pain and function.34,35 Similarly, discectomy is less likely to have a successful outcome in the multi-operated patient. Our results also highlight that TMJ surgeons should screen all patients for systemic arthritis, or associated rheumatologic conditions. Targeted questions about pain, stiffness, swelling, redness, warmth, and limited range of motion in other joints may suffice in some cases, while laboratory studies may be indicated in other cases.
Given the high incidence of self-reported bruxism among patients with TMJ disorders36, elucidating the relationship between bruxism and surgical outcomes could prove useful. The use of polysomnography with electromyography (EMG) channels is considered the gold standard in diagnosing sleep bruxism; however, there are contradictory results from studies looking at the association between sleep bruxism and TMJ disorders, with some studies finding a positive association, and others finding no association.37,38 There is recent data in the literature about a portable EMG device for diagnosing sleep bruxism in patients39,40, but a larger, multi-center validation trial is needed for such a device to be viable in diagnosing sleep bruxism.
Our respondents also recognize that while some patients present with isolated intra-articular pathology, a significant number of TMJ disorder cases are multifactorial requiring a comprehensive approach using validated patient questionnaires to objectively screen for and treat concomitant conditions such as fibromyalgia and psychological distress, which may have serious implications on long term prognosis. Fibromyalgia is a central sensitization disorder that exists on a continuum and is based on the widespread pain index and symptoms severity score, with clearly defined diagnostic criteria set forth and refined by the American College of Rheumatology.41,42 Similarly, the presence of neuropathic pain such as burning, electric pain, and severe allodynia may represent a neuroma, peripheral versus central sensitization, or other pain disorders that may not respond to surgery. Screening tools such as the Leeds assessment of neuropathic pain symptoms and signs (LANSS), the neuropathic pain questionnaire (NPQ), the painDETECT questionnaire, the douleur neuropathique en 4 questions (DN4), and the ID-Pain questionnaire have all been validated for screening for neuropathic pain.43,44,45 Catastrophizing character may be assessed via the pain catastrophizing scale or the coping strategies questionnaire catastrophe subscale. Similarly, other instruments are available to assess other psychological disorders, including perceived stress, and other pain processing or sensitization disorders.
Limitations of our study
In this survey of TMJ surgeons, a response rate 33.7% was achieved. This low response rate can be attributed to the frequent low-response rate to web surveys among practitioners.46 It is possible that a larger sample might have yielded different results. Despite this limitation, surveying a group with a special focus in the management of surgical TMJ disorders, we are confident that the results give interesting insights into practicing surgeon’s perceptions and clinical experience with the use of TMJ discectomy. Our survey attempted to understand the factors that influence surgical decisions, specifically with respect to the use of discectomy versus other surgical modalities, however, the basis of clinical decisions for individual cases are complex and may not be captured entirely by this survey. For instance, we did not ask about the effect of age as it pertains to the use of discectomy in different Wilkes stages.
Conclusion and Future considerations
Most respondents feel discectomy is not a useful procedure for managing TMJ-ID and would not consider using it as a first surgical option. The majority did however agree with the use of discectomy in cases of disc perforation and for ADDwoR as an intermediate procedure prior to TJR. However, only 40% agreed with the use of discectomy for advanced stage TMD-ID with DJD before considering alloplastic total joint replacement. The most common adverse effects after discectomy included joint noises and osteoarthrosis, and the incidence of adverse effects or complications were not significantly different between disc replacers and non-replacers.
Looking forward, surgical decision-making for TMJ-ID requires more comparative prospective studies with rigorous methodology and broad patient reported outcome data. This can be accomplished with a standardized multi-institutional study that aims to achieve a larger sample size, and should employ novel methods for long-term electronic outcomes tracking. Such research should not be limited to the assessment of pain and function, but help identify ideal candidates for TMJ surgery, characterize the impact of co-morbid conditions, and factor in data on surgical morbidity, lost productivity, and long-term treatment needs.
Acknowledgments
Funding sources
Jonathan Troost was supported in part by the National Center for Advancing Translational Sciences (NCATS) for the Michigan Institute for Clinical and Health Research (UL1TR002240).
Footnotes
Disclosures
Douglas F. Werkman has nothing to disclose.
Sharon Aronovich has nothing to disclose.
Louis G. Mercuri is compensated as a Clinical Consultant for TMJ Concepts and as a minority shareholder of TMJ Concepts.
Johnathan Troost owns stocks in Procter & Gamble and General Electric.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Douglas F. Werkman, University of Michigan School of Dentistry.
Louis G. Mercuri, Department of Orthopedic Surgery, Rush University Medical Center, Chicago, IL; Adjunct Professor Department of Bioengineering, University of Illinois Chicago, Chicago, IL.
Jonathan P. Troost, University of Michigan, Michigan Institute for Clinical & Health Research.
Sharon Aronovich, University of Michigan, Department of Oral and Maxillofacial Surgery.
References
- 1.Farrar WB: Differentiation of temporomandibular joint dysfunction to simplify treatment. J Prosthet Dent 28:629, 1972. [DOI] [PubMed] [Google Scholar]
- 2.Wilkes CH: Arthrography of the temporomandiubular joint. Minn Med 61:645, 1978. [PubMed] [Google Scholar]
- 3.Bronstein SL, Tomasetti KJ, Ryan DE: Internal derangement of the temporomandibular joint: Correlation of arthrography with surgical findings. J Oral Maxillofac Surg 39:572–584, 1981. [PubMed] [Google Scholar]
- 4.Westesson PL, Bronstein SL, Liedberg J: Internal derangement of the temporomandibular joint: Morphologic description with correlation to joint function. Oral Surg Oral Med Oral Pathol 59:323–331, 1985. [DOI] [PubMed] [Google Scholar]
- 5.Schellhas KP, Wilkes CH, Heithoff KB, et al. : Temporomandibular joint: Diagnosis of internal derangements using magnetic resonance imaging. Minn Med 69:516–519, 1986. [PubMed] [Google Scholar]
- 6.Lanz AB: Discitis mandibularis. Zenralbl Chir 36:289,1909. [Google Scholar]
- 7.McCarty WL, Farrar WB. Surgery for internal derangement of the temporomandibular joint. J Prosthet Dent 42:191, 1979. [DOI] [PubMed] [Google Scholar]
- 8.Wilkes CH. Internal derangements of the temporomandibular joint: Pathological variations. Arch Otolaryngol Head Neck Surg 115:469–477, 1989. [DOI] [PubMed] [Google Scholar]
- 9.Eriksson L, Westesson PL: Long-term evaluation of menisectomy of the temporomandibular joint. J Oral Maxillofac Surg 43:263, 1985. [DOI] [PubMed] [Google Scholar]
- 10.Silver CML: Long-term results of menisectomy of the temporomandibular joint. J Craniomandib Pract. 3:46, 1984. [DOI] [PubMed] [Google Scholar]
- 11.Tolvanen M, Oikarinen VJ, Wolf J: A 30-year follow-up study of temporomandibular menisectomies: A report of 5 patients. Br J Oral Maxillofac Surg 3:46, 1988. [DOI] [PubMed] [Google Scholar]
- 12.Miloro M & Henriksen B: Discectomy as the primary surgical option for internal derangement of the temporomandibular joint. J Oral Maxillofac Surg 68(4):782–789, 2010. [DOI] [PubMed] [Google Scholar]
- 13.Peroz I, Seidel A, Griethe M, etl al. MRI of the TMJ: morphometric comparison of asymptomatic volunteers and symptomatic patients. Quintessence Int 42:659–67, 2011. [PubMed] [Google Scholar]
- 14.McKenna SJ. Discectomy for the treatment of internal derangements of the temporomandibular joint. J Oral Maxillofac Surg 59(9):1051–1056, 2001. [DOI] [PubMed] [Google Scholar]
- 15.Dimitroulis G: The prevalence of osteoarthrosis in cases of advanced internal derangement of the temporomandibular joint: a clinical, surgical and histological study. Int J Oral Maxillofac Surg. 34(4):345–349, 2005. [DOI] [PubMed] [Google Scholar]
- 16.McCain JP, Hossameldin RH, Srouji S, Maher A: Arthroscopic discopexy is effective in managing temporomandibular joint internal derangement in patients with Wilkes stage II and III. J Oral Maxillofac Surg 73(3):391–401, 2015. [DOI] [PubMed] [Google Scholar]
- 17.Chang H, Israel H: Analysis of inflammatory mediators in temporomandibular joint synovial fluid lavages samples of symptomatic patients and asymptomatic controls. J Oral Maxillofac Surg 63:761–765, 2005. [DOI] [PubMed] [Google Scholar]
- 18.Asakawa-Tanne Y, Su S, Kunimatsu R et al. : Effects of enzymatic degradation after loading in temporomandibular joint. J Dent Res 94:337–343, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Israel HA: Internal derangement of the temporomandibular joint: New perspectives on an old problem. Oral Maxillofac Surg Clin North Am 28:313–333, 2016. [DOI] [PubMed] [Google Scholar]
- 20.Machon V, Levorova J, Hirjak D, Drahos M, & Foltan R: Temporomandibular joint disc perforation: a retrospective study. Int J Oral Maxillofac Surg 46(11):1411–1416, 2017. [DOI] [PubMed] [Google Scholar]
- 21.Muñoz-Guerra MF, Rodríguez-Campo FJ, Hernández VE, Sánchez-Acedo C, & Usandizaga JLGD: Temporomandibular joint disc perforation: long-term results after operative arthroscopy. J Oral Maxillofac Surg 71(4):667–676, 2013. [DOI] [PubMed] [Google Scholar]
- 22.Nitzan DW, Dolwick MF: An alternative explanation for the genesis of closed-lock symptoms in the internal derangement process. J Oral Maxillofac Surg 49:810–815, 1991. [DOI] [PubMed] [Google Scholar]
- 23.Nitzan DW, Marmary Y: The “anchored disc phenomenon”: a proposed etiology for sudden-onset severe, and persistent closed lock of the temporomandibular joint. J Oral Maxillofac Surg 55:797–802, 1997. [DOI] [PubMed] [Google Scholar]
- 24.Nitzan DW: The process of lubrication impairment and its involvement in temporomandibular joint disc displacement: a theoretical concept. J Oral Maxillofac Surg 59:36–45, 2001. [DOI] [PubMed] [Google Scholar]
- 25.Dolwick MF: Intra-articular disc displacement part I: Its questionable role in temporomandibular pathology. J Oral Maxillofac Surg 53:1069, 1995 [DOI] [PubMed] [Google Scholar]
- 26.Holmlund AB, Axelson S, Gynther GW: A comparison of discectomy and arthroscopic lysis and lavage for the treatment of chronic closed lock of the temporomandibular joint: A randomized outcome study J Oral Maxillofac Surg 59:972–977,2001. [DOI] [PubMed] [Google Scholar]
- 27.Hall DH, Indresano AT, Krik WS et al. : Prospective multicenter comparison of 4 temporomandibular joint operations J Oral Maxillofac Surg 63:1174–1179,2005. [DOI] [PubMed] [Google Scholar]
- 28.Gonzalez-Garcia R, Rodriguez-Campo FJ: Arthroscopic lysis and lavage versus operative arthroscopy in the outcome of temporomandibular joint internal derangement: A comparative study based on Wilkes Stages. J Oral Maxillofac Surg 69:2513–2524, 2011. [DOI] [PubMed] [Google Scholar]
- 29.Kirk WS Jr Risk factors and initial surgical failures of TMJ arthrotomy and arthroplasty: a 4 to 9 year evaluation of 303 surgical procedures Cranio 16(3):154–161, 1998. [DOI] [PubMed] [Google Scholar]
- 30.Eriksson L, Westtesson PL, Lund S: Temporomandibular Joint Diskectomy: No Positive effect of temporary silicone implant in a 5-year follow-up. Oral Surg Oral Med Oral Pathol 74:259–72, 1992. [DOI] [PubMed] [Google Scholar]
- 31.Dimitroulis G: Condylar morphology after temporomandibular joint discectomy with interpositional abdominal dermis-fat graft. J Oral Maxillofac Surg 69(2), 439–446, 2011. [DOI] [PubMed] [Google Scholar]
- 32.Machon V, Vir J, Leorova J et al. : Discectomy with subsequent free fat flap insertion in disc perforation therapy of temporomandibular joint. Assessment of results 24 months after operation. Prague Med Rep: 121:96–106, 2020. [DOI] [PubMed] [Google Scholar]
- 33.Miloro M, McKnight M, Han MD, & Markiewicz MR: Discectomy without replacement improves function in patients with internal derangement of the temporomandibular joint. J Craniomaxillofac Surg 45(9), 1425–1431, 2017. [DOI] [PubMed] [Google Scholar]
- 34.Wolford LM, Mercuri LG, Schneiderman ED, Movahed R, & Allen W: Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ Concepts device. J Oral Maxillofac Surg 73(5), 952–960, 2015. [DOI] [PubMed] [Google Scholar]
- 35.Burgess M, Bowler M, Jones R, Hase M, & Murdoch B: Improved outcomes after alloplastic TMJ replacement: analysis of a multicenter study from Australia and New Zealand. J Oral Maxillofac Surg 72(7):1251–1257, 2014. [DOI] [PubMed] [Google Scholar]
- 36.Marklund S, Wänman A: Risk factors associated with incidence and persistence of signs and symptoms of temporomandibular disorders. Acta Odontol Scand 68(5):289–99, 2010. [DOI] [PubMed] [Google Scholar]
- 37.Raphael, Karen G et al. : Sleep bruxism and myofascial temporomandibular disorders: a laboratory-based polysomnographic investigation. J Am Dent Assoc 143(11):1223–31, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rossetti LM, Pereira de Araujo Cdos R, Rossetti PH, Conti PC: Association between rhythmic masticatory muscle activity during sleep and masticatory myofascial pain: a polysomnographic study. J Orofac Pain 22(3):190–200, 2008. [PubMed] [Google Scholar]
- 39.Saczuk K, Lapinska B, Wilmont P, Pawlak L, Lukomska-Szymanska M: The Bruxoff Device as a Screening Method for Sleep Bruxism in Dental Practice. J Clin Med 8(7):930, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pigozzi LB, Rehm DDS, Fagondes SC, Pellizzer EP, Grossi ML: Current Methods of Bruxism Diagnosis: A Short Communication. Int J Prosthodont 32(3):263–264, 2019. [DOI] [PubMed] [Google Scholar]
- 41.Wolfe F, Clauw DJ, Fitzcharles MA, et al. : Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol 38(6):1113–22, 2011. [DOI] [PubMed] [Google Scholar]
- 42.Wolfe F, Clauw DJ, Fitzcharles MA, et al. : 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum 46(3):319–329, 2016. [DOI] [PubMed] [Google Scholar]
- 43.Haanpaa, Maija, Attal, Nadine, Backonja, Miroslav et al. : NeuPSIG guidelines on neuropathic pain assessment. Pain 152:14–27, 2011. [DOI] [PubMed] [Google Scholar]
- 44.Bouhassira, Didier & Attal, Nadine: Diagnosis and assessment of neuropathic pain: The saga of clinical tools. Pain 152:74–83, 2011. [DOI] [PubMed] [Google Scholar]
- 45.Attal N, Bouhassira D, Baron R: Diagnosis and assessment of neuropathic pain through questionnaires. Lancet Neurol 17(5):456–466, 2018. [DOI] [PubMed] [Google Scholar]
- 46.Hardiagn PC., Succar CT, Felisher JM: An analysis of response rate and economic costs between mail and webbased surveys among practicing dentists: a randomized trial. J Community Health. 37:383–94, 2012. [DOI] [PubMed] [Google Scholar]