Abstract
Background:
Objective measurement of alcohol consumption is important for clinical care and research. Adjusting for self-reported alcohol use, we conducted an individual participant data (IPD) meta-analysis to examine factors associated with the sensitivity of phosphatidylethanol (PEth), an alcohol metabolite, among persons self-reporting unhealthy alcohol consumption.
Methods:
We identified 21 eligible studies and obtained 4073 observations from 3085 participants with Alcohol Use Disorders Identification Test – Consumption (AUDIT-C) positive scores (≥3 for women and ≥4 for men) and PEth measurements. We conducted one-step IPD meta-analysis using mixed-effects models with random intercepts for study site. We examined the associations between demographic (sex, race/ethnicity, and age) and biologic (body mass index -- BMI, hemoglobin, HIV status, liver fibrosis, and venous versus finger-prick blood collection) variables with PEth sensitivity (PEth≥8 ng/mL), adjusting for level of alcohol use using the AUDIT-C score.
Results:
One-third (31%) of participants were women, 32% were African, 28% African American, 28% White, and 12% other race/ethnicity. PEth sensitivity (i.e. ≥8 ng/mL) was 81.8%. After adjusting for AUDIT-C, we found no associations of sex, age, race/ethnicity, or method of blood collection with PEth sensitivity. In models that additionally included biologic variables, those with higher hemoglobin and indeterminate and advanced liver fibrosis had significantly higher odds of PEth sensitivity; those with higher BMI and those living with HIV had significantly lower odds of PEth sensitivity. African Americans and Africans had higher odds of PEth sensitivity compared to whites in models that included biologic variables.
Conclusions:
Among people reporting unhealthy alcohol use, several biological factors (hemoglobin, BMI, liver fibrosis, and HIV status) were associated with PEth sensitivity. Race/ethnicity was associated with PEth sensitivity in some models; age, sex and method of blood collection were not. Clinicians should be aware of these factors, and researchers should consider adjusting analyses for these characteristics where possible.
Keywords: Alcohol, phosphatidylethanol, individual participant data meta-analysis, sensitivity
Introduction
Alcohol use is responsible for at least 5.3% of worldwide mortality (2018); reducing this modifiable harmful behavior is urgently needed. However, individual level interventions require reliable detection and measurement of alcohol intake. Self-report of alcohol represents a problematic gold-standard, in that it is low-cost and rapid, but reporting bias can impact measurement, with social desirability bias causing under-reporting (Davis et al., 2010, Miller et al., 2004, Miller et al., 2006). In contrast, direct alcohol metabolites, i.e. substances that are formed in the body as alcohol is metabolized, can serve as objective measures of alcohol use to replace or complement self-report.
Phosphatidylethanol (PEth) is a direct metabolite that is formed only in the presence of alcohol (and is thus highly specific). PEth is detectable for 3–4 weeks after repeated heavy alcohol consumption (defined as >60 g/day, on average), and has a half-life of 4–10 days (Hahn et al., 2016a, Helander et al., 2019a). It is also detectable after a single drinking session for 3–12 days (Schrock et al., 2016). PEth is measured from whole blood or dried blood spots (DBS) and is most frequently analyzed using liquid chromatography with tandem mass spectrometry (LC-MS/MS) (Jones et al., 2011). The most common homologue, PEth 16:0/18:1, has the longest half-life and is frequently the only PEth homologue measured (Gnann et al., 2014). PEth has shown high sensitivity (>88%) and specificity (>90%) for detecting prior month unhealthy drinking, defined as drinking above recommended limits (Ghosh et al., 2019, Bajunirwe et al., 2014, Magidson et al., 2019, Muyindike et al., 2017, Eyawo et al., 2018, Hahn et al., 2018, Walther et al., 2015, Wang et al., 2017, Edelman et al., 2019, Ulwelling and Smith, 2018), and good correlations with total self-reported volume of alcohol consumed ranging from 0.53 to 0.80 (Hahn et al., 2012, Aradottir et al., 2006, Hartmann et al., 2007, Piano et al., 2015, Ferguson et al., 2020, Schröck et al., 2017, Kechagias et al., 2015, Helander et al., 2019b, Walther et al., 2015, Cherrier et al., 2020, Gerbase et al., 2020, Röhricht et al., 2020), although a few studies found correlations of 0.21–0.44 (Littlefield et al., 2017, Wang et al., 2017, Papas et al., 2016). These characteristics make PEth a preferred biomarker of medium-term (several weeks) unhealthy alcohol use (the spectrum from use of risky amounts through alcohol use disorder). However, a few studies have observed low PEth sensitivity (approximately 50%) among persons reporting drinking heavy amounts (Papas et al., 2016, Wang et al., 2017), raising concerns that PEth is not sufficiently sensitive, or that it is less sensitive in certain subgroups of persons.
The level of PEth formation is directly proportional to the available concentration of ethanol in the blood, which is dependent on short-term factors such as the amount and type of alcohol consumed, stomach contents, and the rate of consumption, and factors that impact alcohol metabolism, such as biological sex, lean body mass, genetically determined alcohol and acetaldehyde dehydrogenases, and liver disease (Cederbaum, 2012). PEth formation may also be influenced by the availability of phospholipase D and availability of phosphatidylcholine (Schrock et al., 2018, Stenton et al., 2019). As such, PEth levels have been shown to vary considerably between persons under controlled alcohol administration experiments (Javors et al., 2016), and among persons entering treatment after periods of heavy drinking (Helander et al., 2019a), thus research examining factors that might impact PEth sensitivity is needed.
A handful of small studies have examined factors that might influence PEth sensitivity, including sex (Wurst et al., 2010, Hahn et al., 2012, Stewart et al., 2014), age (Hahn et al., 2012, Cherrier et al., 2020, Hahn et al., 2016b), body mass index (BMI) (Wang et al., 2017), and hemoglobin level (Beck et al., 2018, Nguyen and Seth, 2018) and liver disease (Cherrier et al., 2020); we are aware of none that examined race/ethnicity, or HIV infection status. Lastly, examination of PEth sensitivity in venous versus finger-prick blood collection is needed, due to the increased risk for hemolysis and variability in blood volume and hematocrit from finger-prick blood collection (Kummer et al., 2016b, De Kesel et al., 2013, Kummer et al., 2016a, Beck et al., 2018). Thus study is needed to examine these factors.
Our primary aim was to examine factors that may be associated with PEth sensitivity in persons self-reporting alcohol consumption at a level for which PEth is often detectable, i.e. unhealthy alcohol use. These factors included demographic variables (sex, age, race/ethnicity), and biologic variables (BMI, hemoglobin level, HIV status, liver fibrosis and method of sample collection). To do so, we conducted an individual participant data meta-analysis to leverage the statistical power of multiple studies with PEth testing and self-reported alcohol use. Since social desirability bias suggests a tendency to under-report alcohol consumption (Adong et al., 2019), we have chosen to evaluate the sensitivity of PEth among those volunteering substantial alcohol consumption, i.e. unhealthy alcohol use.
Methods
Search strategy
We searched for studies that had collected self-reported alcohol use measures as well as PEth testing that met the inclusion criteria described below to contribute de-identified data for these analyses. We identified studies by contacting all the Principal Investigators in the National Institutes of Health Consortiums for HIV/AIDS and Alcohol-Related Outcomes Research Trials Consortium (CHAART), and other investigators known to be using PEth based on the first author’s (JAH) personal knowledge; and by searching PubMed using the combination of “phosphatidylethanol” and “alcohol” for the record creation dates of January 1, 2000 (when the first PEth paper was published (Varga et al., 2000)) through December 31, 2019. We (JAH) determined which studies were eligible for inclusion by reading the titles, abstracts, and when needed, the articles, and sent e-mails to the corresponding authors to confirm eligibility criteria. Authors who agreed to contribute data completed a spreadsheet eliciting the requested variable names and their definitions and sent these data electronically without identifiers. We conducted range checks and calculated frequency tables for all variables and corresponded with data managers as needed to resolve discrepancies; only minor issues were identified. We did not evaluate bias within the studies because of the novelty of our study question; all the studies included were designed to answer different study questions. The receipt of these data for this analysis was approved by the University of California, San Francisco Institutional Review Boards, and the data collection by the contributing studies were previously approved at each institution.
Study eligibility
Studies were eligible for inclusion if they included: (1) PEth results for the 16:0/18:1 homologue, tested with the limit of quantification ≥8 ng/mL; (2) self-reported current alcohol use, either by the Alcohol Use Disorders Identification Test (AUDIT)(Babor et al., 2001) or the AUDIT – Consumption (AUDIT-C)(Bradley et al., 2007, Bush et al., 1998), or by another method from which the AUDIT-C could be calculated (e.g. Timeline Follow Back (Sobell and Sobell, 1992)); (3) the data set included at least 30 observations for which the AUDIT-C score was positive, i.e. ≥3 for women, ≥4 for men. The latter eligibility criterion was to enable us to examine PEth sensitivity among observations with “true positive” unhealthy drinking. To further minimize mis-reporting, we excluded studies that focused on populations for whom there may be reasons to mis-report alcohol use (prisoners, persons driving under the influence, persons entering alcohol treatment, liver transplant patients, pregnant women) and clinical trials whose eligibility criteria were based on self-reported alcohol use which may also cause mis-reporting (Devine et al., 2013, Mccaul and Wand, 2018). We made exceptions for clinical trials that confirmed alcohol use at entry via an objective measure such as transdermal alcohol monitoring or a positive alcohol biomarker test. We excluded studies of infants and children.
Variables
The pre-specified outcome variable was PEth sensitivity, i.e., PEth ≥8 ng/mL versus <8 ng/mL. PEth testing was previously conducted at the Karolinska University Laboratory (Stockholm) for one study (Francis et al., 2015), and at the United States Drug Testing Laboratories (USDTL, Des Plaines) for the remainder of studies. We included the following potential demographic predictors: age, sex, race/ethnicity. Sex was recorded as male or female for all but four studies; for those studies we classified persons (n=12) with their assigned sex at birth. To the extent that race/ethnicity data were available, and recognizing that these categories are social constructs and not biological ancestry (Mersha and Abebe, 2015), we categorized race/ethnicity as African-American, White, and other. Other included persons identified as Latinx/Hispanic, Asian/Pacific Islander, Native American, mixed-race, or race/ethnicity not specified. We created a category called African for those recruited from studies that occurred in African countries (Hahn et al., 2016b, Magidson et al., 2019, Myers et al., 2018, Francis et al., 2015). We examined the following biologic variables: BMI (kg/m2), hemoglobin (g/dL) (or hematocrit, where hemoglobin was not available), HIV status (positive vs. negative), and liver fibrosis (measured by FIB-4, calculated using age, alanine aminotransferase, aspartate aminotransferase, and platelets (Sterling et al., 2006)). We also examined the methods of blood collection, which were either venous blood draws pipetted onto DBS cards, or finger-pricks dropped onto DBS cards.
Self-reported alcohol use, measured by the AUDIT-C, was included as a control variable in all analyses. The AUDIT-C was measured directly in most studies, albeit with varying associated time frames, i.e. no time frame, prior one year, and prior three months (Table 1). For the studies that did not collect the AUDIT-C, we calculated approximate scores from the 30-day timeline follow back for two studies (Stewart et al., 2014) (and Miami study) and from a question assessing the number of drinking days in a third study (Jain et al., 2014).
Table 1.
Characteristics of included studies.
| Study code | Study name and reference | Study design | N persons included | N observations | Region | Location | Participants | AUDIT-C period | How blood collected for PEth |
|---|---|---|---|---|---|---|---|---|---|
| Total | 3,085 | 4,073 | |||||||
| ADEPT | Alcohol Drinking Effects on Progression prior to Treatment (ADEPT) (Hahn et al., 2018) | Observational cohort study | 162 | 315 | Africa | Mbarara, Uganda | PLWH, ART-naïve, over sampling alcohol users, age ≥18 | 3 months | Venously |
| ADEPTT | Alcohol Drinkers’ Exposure to Treatment for TB (ADEPTT) | Trial (no alcohol intervention) | 80 | 162 | Africa | Mbarara, Uganda | PLWH, latent tuberculosis infection, on ART ≥6 months, 2/3 prior 3 months alcohol use, age ≥18 | 3 months | Venously |
| BREATH | BREATH (Biomarker Research on Ethanol Among Those with HIV) (Hahn et al., 2016b) | Observational cohort study | 162 | 301 | Africa | Mbarara, Uganda | PLWH, new to HIV care, prior year alcohol use, age ≥18 | 3 months | Venously |
| DIPT | Drinkers Intervention to Prevent Tuberculosis (DIPT) | Randomized controlled trial (NCT#03492216) | 254 | 461 | Africa | Mbarara, Uganda | PLWH, latent tuberculosis infection, on ART for ≥6 months, unhealthy alcohol use, current alcohol use confirmed by ethyl glucuronide dipstick, age ≥18 | 3 months | Venously |
| META | Monitoring Early Treatment Adherence (Magidson et al., 2019) | Observational cohort study (baseline only) | 79 | 79 | Africa | Cape Town South Africa and southwestern Uganda | PLWH, ART-naïve, age ≥18 | 3 months | Venously |
| TANZANIA | Validation of self-reported alcohol use among young people in northern Tanzania (Francis et al., 2015) | Observational cross-sectional study | 172 | 172 | Africa | Mwanza, Tanzania | Prior year alcohol use, age 15–24 | 1 year | Venously |
| TRUST | The Impact of Alcohol Consumption on TB Treatment Outcomes (TRUST)(Myers et al., 2018) | Observational cohort study (baseline only) | 82 | 82 | Africa | Cape Town, South Africa | Persons initiating TB treatment, age ≥15 | Not specified | Venously |
| SIHANOUK | Sihanouk Risk Study(Couture et al., 2016) | Observational cross-sectional study | 132 | 132 | Asia | Preah Sihanouk, Cambodia | Female sex workers and male clients, age ≥18 | 3 months | Finger-prick |
| Russia Women | Reducing Alcohol Use Among HIV Positive Women in Care (Littlefield et al., 2017) | Observational cohort study | 92 | 130 | Europe | St. Petersburg Russia | PLWH, female, age 18–35 | Not specified | Finger-prick |
| RUSSIA | Alcohol & Zinc Impact on Inflammatory Markers in HIV Disease (So-Armah et al., 2019) | Observational cohort study | 323 | 603 | Europe | St. Petersburg, Russia | PLWH, ART naïve, age 18–70 | 1 year | Venously |
| BOSTON | Addressing Alcohol/HIV in Substance Dependence (Saitz et al., 2018) | Observational cohort study (baseline only) |
159 | 159 | North America | Boston, MA | PLWH; substance dependence or ever injected drugs, age ≥18 | 3 months | Venously |
| CHAMPS | Chronic HepAtitis C Management to ImProve OutcomeS (Irvin et al., 2020) | Randomized controlled trial (no alcohol intervention) (NCT#02402218) | 38 | 38 | North America | Baltimore, MD | PLWH, chronic hepatitis C virus, age ≥18 | Not specified | Venously |
| HOLIDAY | Holiday Heart | Observational cohort study | 58 | 87 | North America | San Francisco, CA | Persons diagnosed with atrial fibrillation and/or atrial flutter, alcohol use ≥1x per month, age ≥21 | Not specified | Finger-prick |
| INVOICE | INVOICE Study | Observational cohort study | 88 | 136 | North America | San Francisco, CA and Syracuse, NY | PLWH, MSM/Transwomen | Not specified | Finger-prick |
| MIAMI | Effects of reductions in alcohol consumption on outcomes in older persons with HIV infection |
Single arm trial (unhealthy alcohol use confirmed alcohol use with a biosensor) (NCT#03353701) | 24 | 36 | North America | Miami, FL | Persons with unhealthy alcohol use, age 50–75 | 1 year | Venously |
| NOAH | New Orleans Alcohol Use in HIV Study (Ferguson et al., 2020) | Observational cohort study (baseline only) |
204 | 204 | North America | New Orleans, LA | PLWH, age ≥18 | 1 year | Venously |
| Young Adults | Binge Drinking and Cardiovascular Risk in Young Adults (Piano et al., 2015) | Observational cohort study | 97 | 97 | North America | Chicago, IL | Persons without risk factors for cardiovascular disease, age 18–30 | Not specified | Venously |
| Stewart | PEth in Liver Disease Patients (Stewart et al., 2014) | Observational cross-sectional study | 66 | 66 | North America | Charleston, SC | Persons with active liver disease, willing to discuss their alcohol use, ag ≥18 | AUDIT calculated from 90-day TLFB | Venously |
| TRAUMA | Phosphatidylethanol to Screen for Alcohol Misuse in Trauma Patients (Afshar et al., 2021) | Observational cohort study (baseline only) | 108 | 108 | North America | Maywood, IL | Trauma center patients, age ≥18 | Not specified | Venously |
| UFO | UFO Study (Jain et al., 2014) | Observational cohort study (baseline only) | 83 | 83 | North America | San Francisco, CA | Injected illicit drugs, prior 30 days, age 15–30 | Calculated from prior 30 days questions | Venous and finger-prick |
| VACS | VACS Blood Study (Eyawo et al., 2018) | Observational cohort study (one visit only) |
622 | 622 | North America | Multiple US sites | US Veterans, including PLWH and persons without HIV | 1 year | Venously |
Abbreviations: PLWH: persons living with HIV; ART: antiretroviral therapy; MSM: men who have sex with men; TLFB: timeline followback
Statistical analyses
After confirming study eligibility and obtaining the individual level data for each study, we included only observations within each study for which AUDIT-C was positive (≥3 for women and ≥4 for men), to study PEth sensitivity among those drinking at a level that should be enough for PEth to develop and be detected (Ghosh et al., 2019). We included multiple observations per person, if available. To account for missing data on the biologic variables within individual studies (all data were complete for AUDIT-C by design, gender, race/ethnicity, and age), we first conducted multiple imputation by chained equations (MICE) within studies, assuming data were missing at random (n=50 imputed datasets). Because the imputation was conducted at the study level, it was not conducted for variables that were not collected within an individual study (e.g. BMI was not collected in 8 of the 21 studies).
We calculated PEth sensitivity overall and within the levels of the variables of interest using the imputed data. We created categories for the continuous variables as follows. We categorized AUDIT-C, as in previous studies (Rubinsky et al., 2013), as medium alcohol use: AUDIT-C 3–5 for women and 4–5 for men; high alcohol use: AUDIT-C 6–7; and very high alcohol use: AUDIT-C 8–12. We categorized age as 17–24, 25–34, 35–44, 45–54, and >=55 years. We used standard cutoffs for BMI with underweight: <18.5 kg/m2; normal/healthy weight: 18.5–24.9 kg/m2; overweight: 25–29.9 kg/m2; and obese: ≥30 kg/m2 (Weir and Jan, 2020). We categorized hemoglobin using standard cutoffs as very anemic: <11 g/dL; anemic: 11–11.9 for women, 11–12.9 for men; no anemia:12–15.5 for women, 13–17.5 for men); and high hemoglobin: >15.5 for women, >17.5 for men (Organization, 2011). Lastly, we categorized liver fibrosis as no fibrosis: FIB-4<1.45; inconclusive fibrosis: FIB-4 1.45–3.25; and fibrosis: FIB-4>3.25 (Vallet-Pichard et al., 2007).
We used a one-step meta-analytic regression approach; we fit mixed effects models using a logit link, a random intercept for each study to account for within study clustering, and robust standard errors to account for clustering within individuals with multiple observations per person. This one-step approach, in contrast to a two-step approach in which individual regressions are conducted and then weighted averages are calculated, is less prone to bias and preferred for individual participant level data when covariate adjustment is needed and when there is heterogeneity between studies (Debray et al., 2013, Debray et al., 2015). This approach also allowed us to include data from studies that did not include all levels of the variables of interest, e.g., studies that included only one gender, a particular age group, or a single racial/ethnic group.
To examine the form of the relationship of the continuous variables with PEth sensitivity for regression modeling, we examined linear, quadratic, and categories (as defined above) variable forms. We fit mixed effects models as described above for each, and chose the model with the lowest Aikake’s Information Criterion (AIC) score. We first determined the form for AUDIT-C, the primary adjustment variable, and then chose the modeling form for age in models adjusted for AUDIT-C, plus gender, and race/ethnicity. Lastly, we conducted similar analyses for BMI, hemoglobin, and FIB-4 score, adjusting for AUDIT-C, gender, race/ethnicity and age. The AIC was minimized for AUDIT-C and age when these variables were quadratic variables, when BMI and hemoglobin were included as linear variables, and when FIB-4 was as a categorical variable (data not shown). We used these forms in further modeling.
To examine the associations of each variable of interest with PEth sensitivity, we calculated minimally adjusted odds ratios for the association with PEth positive results for each variable, by fitting mixed effects models as described above, adjusted for AUDIT-C as a quadratic variable. Finally, we used mixed effects models to examine the independent effects of the variables of interest on PEth sensitivity, adjusting for AUDIT-C. We examined three models, because not all datasets included the biologic variables of interest. In Model 1, we examined age, gender and race/ethnicity, and method of sample collection in all 21 studies. In Model 2, we additionally included BMI, hemoglobin, and HIV status as covariates, using the thirteen studies that included these variables. In Model 3, we additionally included liver fibrosis, using the eight studies that included the measures needed for the FIB-4 score. In all models, AUDIT-C and age were modeled as quadratics. We calculated predicted probabilities for the levels of each variable, with all the others held at their means. For variables that were included in the models as continuous variables, we used the midpoints of previously define categories used in our initial analyses of the form of the relationship of the continuous variables with PEth sensitivity, as described above.
We conducted the following sensitivity analyses to determine the robustness of our regression results: (1) analyses including only the first observation per person, with repeat visits excluded, (2) analyses excluding those who reported no drinking in the prior 30 days, or for whom recency of alcohol use was not measured, (3) analyses including only those with high or very high self-reported alcohol use (AUDIT-C≥6), (4) analyses excluding the largest study, which contributed 20.2% of the participants, and (5) analyses using complete case data, i.e. not using the multiple imputation (Models 2 and 3).
Lastly, we explored interactions of the independent variables in Model 1 by race/ethnicity and by gender; we considered p-values of less than 0.10 to be statistically significant. As a result of interactions of race/ethnicity with more than one other variable, we conducted regression analyses for the three models above, stratified by race/ethnicity. The analyses were performed using Stata statistical software (2019).
Results
Study inclusion
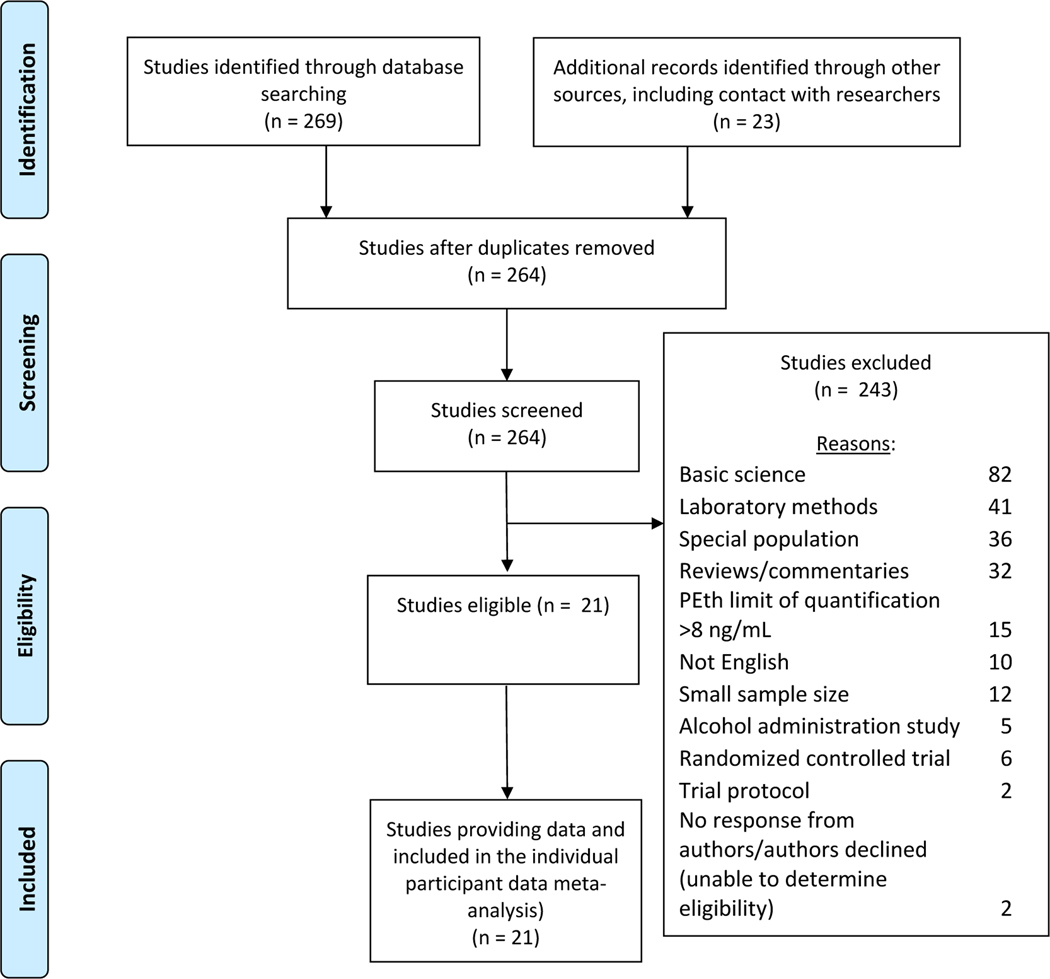
We contacted 15 investigators of CHAART studies, yielding 12 studies that were eligible for inclusion and willing to provide data. We identified an additional 8 studies by the first author’s personal knowledge, yielding 7 studies for inclusion. The PubMed search produced 269 studies, which yielded 2 more eligible studies not previously identified, for a total of 21 (Figure 1). Seventeen of the studies were observational studies, and 2 were alcohol intervention studies (with unhealthy alcohol use confirmed by a biomarker or biosensor), and two were studies of interventions not targeted to alcohol use (Table 1). The number of included study participants (i.e. those with positive AUDIT-C scores and concurrent PEth results) ranged from 36 to 622.
Figure 1.
PRISMA Flow Diagram
Study participants
The 21 included studies yielded 4073 observations meeting the inclusion criteria. These represented 3085 individuals from Africa (32%), Asia (4%), Europe (13%), and North America (50%) (Table 1). One third (30.9%) were women, the median age was 38 years (range: 17–89); and 32% were African, 28% African American, 29% White, and 12% other race/ethnicity (Table 2). At the first available visit, the median AUDIT-C score was 6 (IQR: 4–8), 79% were PEth positive, and the median PEth level was 70.0 ng/mL (IQR: 14.0–233.0). Among all study visits, the proportion PEth positive was 82% (Table 3).
Table 2.
Distributions of the primary variables overall and by study (first observation per participant).
| Race/ethnicity | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study code | N | AUDIT-C score | PEth (ng/mL) | PEth ≥8 ng/mL | Sex=Female | Age | African | African American | White | Other | BMI (kg/m2) | Hemoglobin (g/dL) | FIB-4 score | HIV+ |
| Median (IQR) | Median (IQR) | n (%) | n (%) | Median (IQR) | n (%) | n (%) | n (%) | n (%) | Median (IQR) | Median (IQR) | Median (IQR) | n (%) | ||
| Total | 3,085 | 6 (4–8) | 70.0 (14.0–233.0) | 2,445 (79.3%) | 953 (30.9%) | 38 (28–51) | 991 (32.1%) | 855 (27.7%) | 879 (28.5%) | 360 (11.7%) | 23.6 (21.1–27.3) | 14.1 (12.9–15.2) | 1.2 (0.8–1.9) | 2,074 (67.2%) |
| ADEPT | 162 | 5 (4–7) | 117.0 (29.0–414.0) | 141 (87.0%) | 90 (55.6%) | 32 (27–38) | 162 (100%) | --- | --- | --- | 22.8 (20.4–25.7) | 15.0 (14.0–16.1) | 162 (100%) | |
| ADEPTT | 80 | 5 (4–7) | 124.5 (21.0–253.0) | 65 (81%) | 24 (30%) | 38 (32.5–45) | 80 (100%) | --- | --- | --- | 21.8 (19.5–25.2) | 15.2 (14.1–15.9) | 1.0 (0.7–1.4) | 80 (100%) |
| BREATH | 162 | 4 (4–6) | 110.3 (45.2–310.0) | 146 (90.1%) | 71 (43.8%) | 29 (24–35) | 162 (100%) | --- | --- | --- | 21.8 (19.8–24.2) | 14.2 (13.1–15.7) | 162 (100%) | |
| DIPT | 254 | 7 (5–9) | 266.0 (111.0–512.0) | 251 (98.8%) | 73 (28.7%) | 39 (32–46) | 254 (100%) | --- | --- | --- | 21.5 (19.3–23.9) | 14.8 (13.7–16.0) | 1.0 (0.7–1.4) | 254 (100%) |
| META | 79 | 5 (4–7) | 137.0 (45.0–372.0) | 74 (94%) | 47 (59%) | 31 (26–41) | 79 (100%) | --- | --- | --- | 23.6 (20.7–26.4) |
--- | --- | 79 (100%) |
| TANZANIA | 172 | 6 (4–8) | 7.0 (0.0–63.3) | 80 (46.5%) | 31 (18.0%) | 22 (21–24) | 172 (100%) | --- | --- | --- | --- | --- | --- | |
| TRUST | 82 | 7.5 (6–9) | 144.0 (14.0–378.0) | 68 (83%) | 29 (35%) | 36 (28–48) | 82 (100%) | --- | --- | --- | 18.5 (16.6–20.2) | 12.4 (10.5–13.5) | 0.6 (0.3–0.8) | 26 (32%) |
| SIHANOUK | 132 | 6 (5–8) | 92.9 (24.6–232.6) | 114 (86.4%) | 85 (64.4%) | 25 (22–29) | --- | --- | --- | 132 (100%) | --- | --- | --- | 5 (3.8%) |
| Russia women | 92 | 4 (3–4) | 29.5 (14.0–83.0) | 75 (82%) | 92 (100%) | 30 (28.5–33) | --- | --- | 92 (100%) | --- | --- | --- | --- | 92 (100%) |
| RUSSIA | 323 | 8 (6–10) | 61.0 (12.0–208.0) | 261 (80.8%) | 98 (30.3%) | 33 (30–37) | --- | --- | 323 (100%) | --- | 22.5 (20.7–24.4) | 15.0 (13.4–15.8) | 1.4 (0.9–2.2) | 323 (100%) |
| BOSTON | 159 | 7 (5–10) | 21.0 (1.0–83.3) | 96 (60.4%) | 61 (38.4%) | 48 (41–53) | --- | 81 (50.9%) | 29 (18.2%) | 49 (30.8%) | 25.9 (23.2–29.6) | 13.4 (12.3–14.4) | 1.2 (0.8–1.9) | 159 (100%) |
| CHAMPS | 38 | 5 (4–7) | 199.5 (76.0–444.0) | 34 (89%) | 16 (42%) | 53 (49–57) | --- | 36 (95%) | 2 (5%) | 24.1 (21.3–28.1) | 13.7 (12.3–14.2) | 2.3 (1.4–3.8) | 38 (100%) | |
| HOLIDAY | 58 | 4 (4–5) | 31.5 (14.0–68.0) | 49 (84%) | 12 (21%) | 67 (60–74) | --- | 2 (3%) | 48 (83%) | 8 (14%) | --- | --- | --- | --- |
| INVOICE | 88 | 7 (6–8) | 24.5 (1.0–118.0) | 51 (58%) | 0 (0%) | 43.5 (31.5–50.5) | --- | 56 (64%) | 12 (14%) | 20 (23%) | --- | --- | --- | 88 (100%) |
| MIAMI | 24 | 6 (5–9.5) | 53.5 (11.5–114.0) | 20 (83%) | 10 (42%) | 55 (54–59.5) | --- | 20 (83%) | 3 (12%) | 1 (4%) | 24.4 (21.9–29.1) | 13.2 (11.7–14.1) | 1.3 (0.9–1.7) | 12 (50%) |
| NOAH | 204 | 6 (4–8) | 90.0 (14.5–270.0) | 159 (77.9%) | 61 (29.9%) | 51 (42–56) | --- | 170 (83.3%) | 32 (15.7%) | 2 (1.0%) | 25.3 (22.6–29.8) | 13.6 (12.5–14.5) | 1.2 (0.8–1.7) | 204 (100%) |
| Young adults | 97 | 6 (4–9) | 31.0 (15.1–66.2) | 81 (84%) | 64 (66%) | 22 (20–24) | --- | 4 (4%) | 73 (75%) | 20 (21%) | 22.7 (21.3–24.7) | 13.3 (12.8–13.9) | --- | --- |
| Stewart | 66 | 6 (4–9) | 216.5 (47.0–475.0) | 60 (91%) | 25 (38%) | 52 (42–57) | --- | 22 (33%) | 42 (64%) | 2 (3%) | --- | --- | --- | 2 (3%) |
| TRAUMA | 108 | 6 (4–8) | 148.0 (35.0–454.0) | 98 (90.7%) | 22 (20.4%) | 46 (32.5–61) | --- | 20 (18.5%) | 50 (46.3%) | 38 (35.2%) | 27.4 (23.4–31.1) | 13.7 (12.5–14.8) | --- | --- |
| UFO | 83 | 8 (5–10) | 42.7 (0.0–154.0) | 58 (70%) | 19 (23%) | 25 (22–27) | --- | 4 (5%) | 63 (76%) | 16 (19%) | --- | --- | --- | 3 (4%) |
| VACS | 622 | 5 (4–7) | 42.0 (7.0–147.0) | 464 (74.6%) | 23 (3.7%) | 51 (47–56) | --- | 440 (70.7%) | 110 (17.7%) | 72 (11.6%) | 25.8 (23.0–29.6) | 14.0 (13.1–15.0) | 1.3 (0.9–2.0) | 385 (61.9%) |
Table 3.
PEth sensitivity (≥8 ng/mL) overall and by demographic and biologic variables, all observations. Odds ratios and 95% confidence intervals are from separate mixed effects models, adjusted for AUDIT-C ( N=4073).
| Variable | n PEth positive (≥8 ng/mL)/N (%) | Odds Ratio (95% CI) | p-value |
|---|---|---|---|
| Overall | 3,332/4,073 (81.8%) | ||
| AUDIT-C score | |||
| Medium (4–5 men/3–5 women) | 1,430/1,851 (77.3%) | 1.00 | |
| High (6–7) | 801/963 (83.2%) | 1.81 (1.37–2.39) | <0.001 |
| Very high (8–12) | 1,101/1,259 (87.5%) | 2.89 (1.79–4.66) | <0.001 |
| AUDIT-C, from quadratic model | |||
| 6 vs 4 | 1.86 (1.47–2.36) | <0.001 | |
| 10 vs 4 | 3.59 (2.26–5.71) | <0.001 | |
| Gender | |||
| Male | 2,266/2,756 (82.2%) | 1.00 | |
| Female | 1,066/1,317 (80.9%) | 0.82 (0.58–1.17) | 0.273 |
| Race/ethnicity | |||
| White | 987/1,228 (80.4%) | 1.00 | |
| African | 1,368/1,572 (87.0%) | 2.20 (0.74–6.59) | 0.157 |
| African American | 681/893 (76.3%) | 1.37 (1.02–1.84) | 0.036 |
| Other | 296/380 (77.9%) | 1.18 (0.75–1.87) | 0.481 |
| Age | |||
| 15–24 | 391/546 (71.6%) | 1.00 | |
| 25–34 | 1,013/1,198 (84.6%) | 1.15 (0.72–1.83) | 0.557 |
| 35–44 | 837/961 (87.1%) | 1.44 (0.66–3.16) | 0.358 |
| 45–54 | 643/810 (79.4%) | 1.41 (0.67–2.99) | 0.370 |
| 55+ | 448/558 (80.3%) | 1.44 (0.67–3.05) | 0.358 |
| Age, from quadratic model | |||
| 30 vs 20 | 1.49 (0.97–2.29) | 0.066 | |
| 40 vs 20 | 1.90 (0.94–3.84) | 0.072 | |
| 50 vs 20 | 2.07 (0.90–4.74) | 0.085 | |
| 60 vs 20 | 1.93 (0.84–4.40) | 0.120 | |
| Method of blood collection | |||
| Finger-prick | 436/568 (76.8%) | 1.00 | |
| Venous | 2,896/3,505 (82.6%) | 1.52 (0.60–3.83) | 0.377 |
| Body mass index | |||
| Underweight (<18.5) | 229/247 (92.7%) | 1.00 | |
| Normal (18.5–24.9) | 1,655/1,895 (87.3%) | 0.72 (0.44–1.17) | 0.154 |
| Overweight (25–29.9) | 576/731 (78.8%) | 0.50 (0.32–0.79) | 0.003 |
| Obese (>=30) | 325/427 (76.1%) | 0.44 (0.28–0.69) | <0.001 |
| Body mass index, per 5 units | 0.76 (0.68–0.84) | <0.001 | |
| Hemoglobin* | |||
| Moderate/severe anemia | 121/165 (73.3%) | 1.00 | |
| Mild anemia | 316/400 (79.0%) | 1.71 (1.05–2.79) | 0.031 |
| No anemia | 2,058/2,412 (85.3%) | 2.19 (1.34–3.59) | 0.002 |
| High hemoglobin | 132/140 (94.3%) | 3.54 (1.42–8.85) | 0.009 |
| Hemoglobin, per 5 units | 1.94 (1.41–2.65) | <0.001 | |
| HIV status | |||
| Negative | 615/756 (81.3%) | 1.00 | |
| Positive | 2,533/3,026 (83.7%) | 0.97 (0.82–1.14) | 0.691 |
| FIB-4 score | |||
| No/mild fibrosis: <1.45 | 923/1,169 (79.0%) | 1.00 | |
| 1.45–3.25 | 471/574 (82.1%) | 1.31 (1.05–1.63) | 0.017 |
| Advanced fibrosis: >3.25 | 161/183 (88.0%) | 1.83 (1.24–2.71) | 0.002 |
Hemoglobin (HGB) cutoffs: Moderate/severe anemia: <11 g/dL HGB; Mild anemia =<12 g/dL HGB for women, <13 g/dL HGB for men; No anemia: 12–15.5 g/dL HGB for women, 13–17.5 HGB for men; High hemoglobin: >15.5 g/dL for women, >17.5 g/dL for men.
Associations with PEth sensitivity
Table 3 shows PEth sensitivity by each variable of interest among the 4073 observations. Adjusting for level of alcohol use via the AUDIT-C, BMI, hemoglobin, and liver fibrosis were associated with PEth sensitivity. In the Model 1 multivariable analysis that included all 21 studies, none of the variables of interest (gender, age, race/ethnicity, method of sample collection), were associated with PEth sensitivity, although AUDIT-C, the adjustment variable, was associated with PEth sensitivity (Table 4). In the Model 2 analysis that included the 13 studies in which BMI, hemoglobin, and HIV status data were collected, BMI (aOR=0.74; 95% CI: 0.66–0.83 for +5 kg/m2), hemoglobin (aOR=2.12; 95% CI: 1.52–2.96 for +5 g/dL), and HIV status (aOR=0.77; 95% CI: 0.66–0.89 positive versus negative) were associated with PEth sensitivity; race/ethnicity, age, and AUDIT-C were also associated with PEth sensitivity in this model. When we added FIB-4 to the model (Model 3, 9 studies included), we found the adjusted odds of PEth sensitivity were increased for inconclusive and high FIB-4 scores compared to normal scores (aOR=1.29; 95% CI: 1.02–1.63 and aOR=1.87; 95% CI: 1.28–2.75 for scores of 1.45 to 3.25 and >3.25 compared to <1.45, respectively), while BMI, hemoglobin, HIV status, race/ethnicity, and AUDIT-C remained associated with PEth sensitivity. Predicted PEth sensitivity for each level of categorical and categorized variables range from 0.75 to 0.93 (Table 5).
Table 4.
Adjusted odds ratios 95% confidence intervals, and p-values for the associations of demographic and biologic variables with PEth sensitivity (PEth ≥8 ng/mL) among observations with unhealthy drinking reported. Statistically significant comparisons are bolded.
| Predictors | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| N Studies | 21 | 13 | 9 |
| N | 4073 | 3188 | 2367 |
| AUDIT-C score* | |||
| 6 vs 4 | 1.78 (1.40–2.27, p<0.001) | 1.64 (1.28–2.10, p<0.001) | 1.38 (1.11–1.72, p<0.001) |
| 10 vs 4 | 3.37 (2.05–5.53, p<0.001) | 2.62 (1.79–3.83, p<0.001) | 2.10 (1.55–2.87, p<0.001) |
| Sex: Female vs Male | 0.86 (0.61–1.22, p=0.396) | 1.08 (0.82–1.42, p=0.589) | 1.12 (0.81–1.54, p=0.500) |
| Race/Ethnicity | |||
| African vs White | 2.41 (0.81–7.21, p=0.115) | 3.05 (1.07–8.72, p=0.037) | 3.57 (0.73–17.42, p=0.116) |
| African American vs White | 1.30 (0.96–1.76, p=0.090) | 1.54 (1.00–2.37, p=0.047) | 1.70 (1.06–2.72, p=0.027) |
| Other vs White | 1.16 (0.72–1.86, p=0.540) | 1.10 (0.85–1.43, p=0.471) | 1.22 (0.90–1.64, p=0.202) |
| Age* | |||
| 30 vs 20 | 1.44 (0.93–2.23, p=0.098) | 1.68 (1.02–2.76, p=0.041) | 1.10 (0.62–1.95, p=0.737) |
| 40 vs 20 | 1.81 (0.89–3.69, p=0.101) | 2.27 (1.01–5.12, p=0.048) | 1.14 (0.45–2.94, p=0.786) |
| 50 vs 20 | 1.98 (0.86–4.58, p=0.110) | 2.47 (0.95–6.40, p=0.062) | 1.12 (0.36–3.42, p=0.847) |
| 60 vs 20 | 1.88 (0.82–4.32, p=0.135) | 2.17 (0.86–5.45, p=0.099) | 1.03 (0.34–3.11, p=0.965) |
| Method of blood collection: Venous vs finger-prick | 0.92 (0.29–2.93, p=0.885) | --- | --- |
| BMI (per 5 kg/m2) | 0.74 (0.66–0.83, p<0.001) | 0.73 (0.65–0.81, p<0.001) | |
| Hemoglobin (per 5 g/dl) | 2.12 (1.52–2.96, p<0.001) | 2.28 (1.57–3.30, p<0.001) | |
| HIV+ (vs HIV-) | 0.77 (0.66–0.89, p<0.001) | 0.78 (0.64–0.95, p=0.013) | |
| FIB-4 score | |||
| 1.45–3.25 vs <1.45 | 1.29 (1.02–1.63, p=0.032) | ||
| >3.25 vs <1.45 | 1.87 (1.28–2.75, p=0.001) |
Fitted values from quadratic variable
Table 5.
Predicted PEth sensitivity for each variable calculated from the regression models, holding all others at their means. Categories for continuous variables are the midpoints of categories defined in Table 4.
| Predictors | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| AUDIT-C score | |||
| Medium: 4 | 77.1% (68.5–85.6) | 82.5% (76.4–88.6) | 78.9% (70.9–86.9) |
| High: 6 | 84.8% (78.1–91.5) | 88.2% (83.0–93.4) | 83.5% (77.4–89.5) |
| Very high: 10 | 90.9% (86.2–95.5) | 92.1% (88.2–96.1) | 88.2% (84.0–92.3) |
| Sex | |||
| Male | 86.3% (79.8–92.8) | 88.8% (83.8–93.9) | 84.4% (78.8–89.9) |
| Female | 84.6% (77.5–91.8) | 89.5% (84.1–94.9) | 85.7% (79.3–92.0) |
| Race/ethnicity | |||
| African | 90.2% (81.9–98.6) | 93.2% (87.9–98.4) | 91.5% (82.2–100.8) |
| African American | 84.1% (77.1–91.1) | 87.7% (81.3–94.0) | 84.3% (78.2–90.5) |
| White | 80.7% (72.1–89.4) | 82.6% (73.4–91.8) | 76.8% (66.9–86.8) |
| Other | 82.7% (73.7–91.7) | 83.9% (74.8–93.0) | 79.8% (66.9–92.7) |
| Age | |||
| 20 | 78.4% (68.5–88.2) | 79.0% (67.6–90.5) | 83.0% (67.7–98.3) |
| 30 | 83.3% (76.9–89.8) | 85.9% (80.1–91.7) | 84.2% (75.7–92.8) |
| 40 | 86.0% (79.5–92.5) | 89.0% (83.9–94.0) | 84.7% (78.9–90.5) |
| 50 | 86.9% (80.0–93.8) | 89.7% (84.5–95.0) | 84.4% (78.9–89.9) |
| 60 | 86.4% (79.2–93.5) | 88.6% (83.2–93.9) | 83.3% (77.6–89.1) |
| Method of blood collection | |||
| Finger-prick | 86.6% (73.7–99.4) | ||
| Venous blood collection | 85.7% (79.2–92.2) | ||
| Body mass index (kg/m2) | |||
| Underweight: 17.5 | 92.3% (88.4–96.1) | 89.3% (84.2–94.3) | |
| Normal: 22 | 90.3% (85.8–94.9) | 86.5% (81.2–91.9) | |
| Overweight: 27.5 | 87.1% (81.1–93.0) | 82.1% (76.2–87.9) | |
| Obese: 33 | 83.2% (75.2–91.2) | 76.8% (70.1–83.6) | |
| Hemoglobin (g/dL) | |||
| Moderate/severe: 10 | 82.0% (74.1–89.8) | 74.9% (66.4–83.4) | |
| Mild anemia: 11.5 | 84.8% (78.2–91.5) | 78.9% (71.8–86.0) | |
| No anemia: 14 | 88.8% (83.7–94.0) | 84.5% (78.9–90.1) | |
| High hemoglobin: 17.5 | 92.9% (89.0–96.8) | 90.3% (85.6–95.0) | |
| HIV status | |||
| Negative | 90.9% (86.4–95.5) | 87.1% (81.5–92.7) | |
| Positive | 88.6% (83.4–93.8) | 84.3% (78.7–89.9) | |
| FIB-4 score | |||
| No/mild fibrosis: <1.45 | 83.1% (77.3–88.8) | ||
| 1.45–3.25 | 86.1% (80.2–92.1) | ||
| Advanced fibrosis: >3.25 | 89.8% (84.8–94.8) |
We conducted several sensitivity analyses and found no substantial differences in the results (Tables 6, 7, 8, 9, and 10). In exploratory analyses, we found significant interactions (p<0.10) between race/ethnicity and the associations of age, method of sample collection, and AUDIT-C score with PEth sensitivity in Model 1 (data not shown), thus we stratified by race/ethnicity (Table 11). After stratification by race/ethnicity, we found reduced odds of PEth sensitivity for females compared to males among African Americans (aOR = 0.41; 95% CI: 0.29–0.58). In addition, age was associated with PEth sensitivity among Africans in Models 1 and 2.
Table 6.
Adjusted odds ratios,95% confidence intervals, and p-values for the associations of demographic and biologic variables with PEth sensitivity (PEth ≥8 ng/mL) among persons reporting unhealthy drinking, first observation per person included only (sensitivity analyses). Statistically significant comparisons are bolded.
| Predictors | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| N Studies | 21 | 13 | 9 |
| N | 3085 | 2315 | 1786 |
| AUDIT-C score* | |||
| 6 vs 4 | 1.89 (1.46–2.45, p<0.001) | 1.72 (1.34–2.21, p<0.001) | 1.46 (1.20–1.77, p<0.001) |
| 10 vs 4 | 3.39 (1.88–6.11, p<0.001) | 2.53 (1.64–3.91, p<0.001) | 2.05 (1.45–2.88, p<0.001) |
| Sex: Female vs Male | 0.86 (0.58–1.26, p=0.443) | 1.02 (0.75–1.40, p=0.885) | 1.03 (0.73–1.45, p=0.859) |
| Race/ethnicity | |||
| African vs White | 2.26 (0.78–6.60, p=0.135) | 2.76 (1.01–7.57, p=0.049) | 3.36 (0.70–16.09, p=0.129) |
| African American vs White | 1.32 (0.98–1.78, p=0.071) | 1.57 (1.03–2.39, p=0.036) | 1.69 (1.07–2.68, p=0.024) |
| Other vs White | 1.05 (0.79–1.41, p=0.733) | 1.10 (0.85–1.44, p=0.457) | 1.22 (0.91–1.63, p=0.179) |
| Age* | |||
| 30 vs 20 | 1.34 (0.89–2.00, p=0.159) | 1.50 (0.95–2.37, p=0.079) | 1.17 (0.60–2.28, p=0.648) |
| 40 vs 20 | 1.61 (0.84–3.09, p=0.154) | 1.91 (0.91–4.02, p=0.088) | 1.26 (0.42–3.80, p=0.679) |
| 50 vs 20 | 1.75 (0.81–3.75, p=0.152) | 2.05 (0.86–4.89, p=0.105) | 1.26 (0.34–4.65, p=0.727) |
| 60 vs 20 | 1.71 (0.81–3.63, p=0.161) | 1.86 (0.80–4.32, p=0.147) | 1.16 (0.32–4.19, p=0.815) |
| Method of blood collection: Venous vs finger-prick | 0.94 (0.29–3.02, p=0.922) | ||
| BMI (per 5 kg/m2) | 0.71 (0.64–0.79, p<0.001) | 0.71 (0.64–0.79, p<0.001) | |
| Hemoglobin (per 5 g/dl) | 2.29 (1.56–3.36, p<0.001) | 2.43 (1.58–3.75, p<0.001) | |
| HIV+ (vs HIV-) | 0.73 (0.63–0.85, p<0.001) | 0.76 (0.63–0.91, p=0.003) | |
| FIB-4 score | 1.00 | ||
| 1.45–3.25 vs <1.45 | 1.26 (0.99–1.61, p=0.061) | ||
| >3.25 vs <1.45 | 1.77 (1.18–2.65, p=0.006) | ||
Fitted values from quadratic variable
Table 7.
Adjusted odds ratios, 95% confidence intervals, and p-values for the associations of demographic and biologic variables with PEth sensitivity (PEth ≥8 ng/mL) among persons reporting unhealthy drinking, data limited to observations with prior 30-day alcohol use assessed/reported (sensitivity analyses). Statistically significant comparisons are bolded.
| Predictors | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| N Studies | 14 | 10 | 7 |
| N | 2552 | 2173 | 1538 |
| AUDIT-C score* | |||
| 6 vs 4 | 1.50 (1.13–1.97, p<0.001) | 1.41 (1.01–1.96, p=0.043) | 1.13 (0.81–1.57, p=0.471) |
| 10 vs 4 | 3.38 (2.26–5.05, p<0.001) | 2.81 (1.96–4.01, p<0.001) | 2.25 (1.39–3.65, p=0.001) |
| Sex: Female vs Male | 0.82 (0.57–1.17, p=0.269) | 1.05 (0.80–1.38, p=0.743) | 1.14 (0.83–1.55, p=0.412) |
| Race/ethnicity | |||
| African vs White | 2.70 (0.94–7.76, p=0.065) | 3.21 (1.30–7.95, p=0.012) | 3.57 (0.80–15.96, p=0.095) |
| African American vs White | 1.53 (1.01–2.30, p=0.042) | 1.70 (1.07–2.67, p=0.023) | 1.96 (1.11–3.49, p=0.021) |
| Other vs White | 0.76 (0.58–1.00, p=0.048) | 0.78 (0.58–1.07, p=0.123) | 0.79 (0.50–1.26, p=0.322) |
| Age* | |||
| 30 vs 20 | 1.63 (0.90–2.95, p=0.109) | 1.64 (0.83–3.24, p=0.154) | 0.91 (0.47–1.77, p=0.790) |
| 40 vs 20 | 2.20 (0.86–5.65, p=0.102) | 2.07 (0.71–6.04, p=0.182) | 0.81 (0.28–2.31, p=0.689) |
| 50 vs 20 | 2.47 (0.84–7.23, p=0.100) | 2.01 (0.62–6.56, p=0.246) | 0.69 (0.21–2.23, p=0.532) |
| 60 vs 20 | 2.30 (0.79–6.68, p=0.125) | 1.50 (0.53–4.27, p=0.443) | 0.56 (0.19–1.64, p=0.294) |
| Method of blood collection: Venous vs finger-prick | 0.73 (0.19–2.72, p=0.634) | ||
| BMI (per 5 kg/m2) | 0.73 (0.62–0.86, p<0.001) | 0.73 (0.62–0.86, p<0.001) | |
| Hemoglobin (per 5 g/dl) | 2.13 (1.46–3.12, p<0.001) | 2.32 (1.43–3.77, p<0.001) | |
| HIV+ (vs HIV-) | 0.78 (0.39–1.57, p=0.487) | 0.98 (0.48–2.02, p=0.959) | |
| FIB-4 score | 1.00 | ||
| 1.45–3.25 vs <1.45 | 1.43 (0.97–2.11, p=0.074) | ||
| >3.25 vs <1.45 | 2.30 (1.49–3.54, p<0.001) | ||
Fitted values from quadratic variable
Table 8.
Adjusted odds ratios, 95% confidence intervals, and p-values for the associations of demographic and biologic variables with PEth sensitivity (PEth ≥8 ng/mL) among persons reporting unhealthy drinking, limited to observations with high/very high drinking (AUDIT-C≥6) only (sensitivity analyses). Statistically significant comparisons are bolded.
| Predictors | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| N Studies | 21 | 13 | 9 |
| N | 2222 | 1799 | 1436 |
| AUDIT-C score* | |||
| 6 vs 4 | 1.66 (0.84–3.29, p=0.143) | 1.59 (0.79–3.20, p=0.192) | 1.41 (0.71–2.80, p=0.327) |
| 10 vs 4 | 3.22 (1.19–8.72, p=0.021) | 2.65 (1.10–6.40, p=0.030) | 2.18 (0.92–5.16, p=0.077) |
| Sex: Female vs Male | 0.93 (0.58–1.51, p=0.783) | 0.98 (0.63–1.54, p=0.946) | 1.07 (0.65–1.77, p=0.745) |
| Race/ethnicity | |||
| African vs White | 1.54 (0.43–5.49, p=0.508) | 2.45 (0.67–8.93, p=0.175) | 3.36 (0.86–13.19, p=0.083) |
| African American vs White | 0.69 (0.32–1.52, p=0.361) | 0.77 (0.26–2.31, p=0.640) | 0.78 (0.26–2.35, p=0.655) |
| Other vs White | 0.72 (0.37–1.42, p=0.344) | 0.67 (0.34–1.32, p=0.246) | 0.54 (0.36–0.82, p=0.004) |
| Age* | |||
| 30 vs 20 | 1.02 (0.69–1.51, p=0.921) | 1.05 (0.76–1.45, p=0.750) | 1.00 (0.62–1.60, p=0.993) |
| 40 vs 20 | 1.08 (0.57–2.04, p=0.814) | 1.15 (0.66–2.01, p=0.612) | 1.03 (0.46–2.29, p=0.940) |
| 50 vs 20 | 1.19 (0.56–2.49, p=0.654) | 1.31 (0.65–2.65, p=0.447) | 1.10 (0.41–2.97, p=0.844) |
| 60 vs 20 | 1.35 (0.65–2.82, p=0.425) | 1.55 (0.71–3.38, p=0.267) | 1.22 (0.43–3.51, p=0.706) |
| Method of blood collection: Venous vs finger-prick | 1.00 (0.22–4.59, p=0.997) | ||
| BMI (per 5 kg/m2) | 0.72 (0.61–0.85, p<0.001) | 0.72 (0.62–0.85, p<0.001) | |
| Hemoglobin (per 5 g/dl) | 2.08 (1.24–3.50, p=0.006) | 2.27 (1.33–3.88, p=0.003) | |
| HIV+ (vs HIV-) | 0.67 (0.49–0.93, p=0.016) | 0.76 (0.65–0.88, p<0.001) | |
| FIB-4 score | 1.00 | ||
| 1.45–3.25 vs <1.45 | 1.32 (0.96–1.81, p=0.091) | ||
| >3.25 vs <1.45 | 2.49 (1.67–3.73, p<0.001) | ||
Fitted values from quadratic variable
Table 9.
Adjusted odds ratios, 95% confidence intervals, and p-values for the associations of demographic and biologic variables with PEth sensitivity (PEth ≥8 ng/mL) among persons reporting unhealthy drinking, excluding the largest single study (sensitivity analyses). Statistically significant comparisons are bolded.
| Predictors | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| N Studies | 20 | 12 | 8 |
| N | 3451 | 2566 | 1745 |
| AUDIT-C* | |||
| AUDIT-C: 6 vs 4 | 1.92 (1.47–2.51, p<0.001) | 1.75 (1.27–2.40, p<0.001) | 1.41 (1.02–1.94, p=0.039) |
| AUDIT-C: 10 vs 4 | 4.26 (2.68–6.78, p<0.001) | 3.25 (2.25–4.69, p<0.001) | 2.46 (1.70–3.58, p<0.001) |
| Sex: Female vs Male | 0.91 (0.62–1.32, p=0.614) | 1.14 (0.84–1.55, p=0.041) | 1.19 (0.81–1.75, p=0.381) |
| Race/ethnicity | |||
| African vs White | 2.37 (0.74–7.62, p=0.148) | 3.29 (1.05–10.26, p=0.041) | 4.46 (0.87–22.82, p=0.073) |
| African American vs White | 1.46 (0.82–2.57, p=0.195) | 2.26 (1.25–4.08, p=0.007) | 2.60 (1.21–5.58, p=0.019) |
| Other vs White | 1.20 (0.60–2.41, p=0.611) | 0.94 (0.70–1.25, p=0.662) | 1.03 (0.68–1.57, p=0.883) |
| Age* | |||
| Age: 30 vs 20 | 1.42 (0.88–2.27, p=0.149) | 1.76 (0.99–3.12, p=0.055) | 1.00 (0.48–2.07, p=0.993) |
| Age: 40 vs 20 | 1.76 (0.82–3.77, p=0.147) | 2.38 (0.94–6.02, p=0.066) | 0.97 (0.30–3.09, p=0.856) |
| Age: 50 vs 20 | 1.92 (0.79–4.66, p=0.149) | 2.50 (0.86–7.21, p=0.091) | 0.92 (0.25–3.36, p=0.896) |
| Age: 60 vs 20 | 1.84 (0.77–4.42, p=0.173) | 2.02 (0.74–5.50, p=0.169) | 0.85 (0.26–2.78, p=0.785) |
| Method of blood collection: Venous vs finger-prick | 0.97 (0.26–3.59, p=0.967) | ||
| BMI (per 5 kg/m2) | 0.77 (0.65–0.90, p<0.001) | 0.74 (0.64–0.86, p<0.001) | |
| Hemoglobin (per 5 g/dl) | 2.20 (1.42–3.39, p<0.001) | 2.34 (1.36–4.01, p=0.002) | |
| HIV+ (vs HIV-) | 0.70 (0.34–1.44, p=0.335) | 1.16 (0.81–1.65, p=0.413) | |
| FIB-4 score | 1.00 | ||
| FIB-4 1.45–3.25 vs <1.45 | 1.33 (0.94–1.89, p=0.113) | ||
| FIB-4 >3.25 vs <1.45 | 2.35 (1.44–3.84, p<0.001) |
Fitted values from quadratic variable
Table 10:
Adjusted odds ratios, 95% confidence intervals, and p-values for the associations of demographic and biologic variables with PEth sensitivity (PEth ≥8 ng/mL) among observations with unhealthy drinking reported and complete case data (sensitivity analyses). Statistically significant comparisons are bolded.
| Predictors | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| N Studies | 21 | 13 | 9 |
| N | 4073 | 3019 | 1773 |
| AUDIT-C score* | |||
| 6 vs 4 | 1.78 (1.40–2.27, p<0.001) | 1.62 (1.29–2.02, p<0.001) | 1.45 (1.21–1.73, p<0.001) |
| 10 vs 4 | 3.37 (2.05–5.53, p<0.001) | 2.62 (1.78–3.87, p<0.001) | 2.12 (1.57–2.85, p<0.001) |
| Sex: Female vs Male | 0.86 (0.61–1.22, p=0.396) | 1.08 (0.80–1.47, p=0.610) | 1.15 (0.76–1.76, p=0.511) |
| Race/ethnicity | |||
| African vs White | 2.41 (0.81–7.21, p=0.115) | 2.96 (1.05–8.36, p=0.040) | 3.59 (0.82–15.72, p=0.089) |
| African American vs White | 1.30 (0.96–1.76, p=0.090) | 1.48 (0.99–2.22, p=0.055) | 1.71 (1.08–2.68, p=0.021) |
| Other vs White | 1.16 (0.72–1.86, p=0.540) | 1.06 (0.79–1.44, p=0.687) | 1.21 (0.90–1.64, p=0.214) |
| Age* | |||
| 30 vs 20 | 1.44 (0.93–2.23, p=0.098) | 1.61 (0.95–2.73, p=0.076) | 1.24 (0.44–3.47, p=0.655) |
| 40 vs 20 | 1.81 (0.89–3.69, p=0.101) | 2.17 (0.92–5.13, p=0.077) | 1.23 (0.37–4.15, p=0.685) |
| 50 vs 20 | 1.98 (0.86–4.58, p=0.110) | 2.45 (0.90–6.66, p=0.078) | 1.14 (0.35–3.72, p=0.734) |
| 60 vs 20 | 1.88 (0.82–4.32, p=0.135) | 2.31 (0.89–6.02, p=0.085) | 1.24 (0.44–3.47, p=0.824) |
| Method of blood collection: Venous vs finger-prick | 0.92 (0.29–2.93, p=0.885) | ||
| BMI (per 5 kg/m2) | 0.74 (0.66–0.83, p<0.001) | 0.72 (0.65–0.80, p<0.001) | |
| Hemoglobin (per 5 g/dl) | 2.19 (1.69–2.84, p<0.001) | 2.63 (1.84–3.74, p<0.001) | |
| HIV+ (vs HIV-) | 0.78 (0.68–0.89, p<0.001) | 0.76 (0.61–0.94, p=0.010) | |
| FIB-4 score | |||
| 1.45–3.25 vs <1.45 | 1.27 (1.02–1.58, p=0.035) | ||
| >3.25 vs <1.45 | 1.81 (1.27–2.59, p=0.001) | ||
Fitted values from quadratic variable
Table 11.
Adjusted odds ratios, (95% confidence intervals, and p-values for the associations of demographic and biologic variables with PEth sensitivity (PEth ≥8 ng/mL) among observations with unhealthy drinking reported; stratified by race/ethnicity. Statistically significant comparisons are bolded.
| Model 1 | ||||
|---|---|---|---|---|
| African | African American | White | Other | |
| N Studies | 7 | 11 | 13 | 11 |
| N | 1572 | 893 | 1228 | 380 |
| AUDIT-C score* | ||||
| 6 vs 4 | 2.09 (1.51–2.88, p<0.001) | 1.22 (0.80–1.84, p=0.320) | 2.05 (1.06–3.98, p=0.034) | 1.85 (0.98–3.49, p=0.059) |
| 10 vs 4 | 8.29 (3.95–17.39, p<0.001) | 1.42 (0.68–2.94, p=0.591) | 5.17 (1.87–14.30, p=0.002) | 2.91 (1.23–6.89, p=0.015) |
| Sex: Female vs Male | 1.01 (0.59–1.74, p=0.970) | 0.41 (0.29–0.58, p<0.001) | 1.17 (0.81–1.71, p=0.402) | 1.37 (0.48–3.90, p=0.556) |
| Age* | ||||
| 30 vs 20 | 3.45 (2.24–5.32, p<0.001) | 0.70 (0.33–1.46, p=0.340) | 1.05 (0.73–1.51, p=0.782) | 0.73 (0.39–1.38, p=0.336) |
| 40 vs 20 | 6.77 (3.43–13.37, p<0.001) | 0.57 (0.19–1.74, p=0.323) | 1.05 (0.56–1.97, p=0.872) | 0.68 (0.26–1.74, p=0.417) |
| 50 vs 20 | 7.54 (3.39–16.75, p<0.001) | 0.55 (0.18–1.69, p=0.394) | 1.00 (0.44–2.27, p=997) | 0.78 (0.29–2.09, p=0.624) |
| 60 vs 20 | 4.76 (1.91–11.85, p<0.001) | 0.61 (0.27–1.37, p=−.231) | 0.91 (0.35–2.36, p=0.840) | 1.14 (0.47–2.77, 0.777) |
| Method of blood collection: Venous vs finger-prick | NA | 3.18 (0.49–20.71, p=0.226) | 0.77 (0.18–3.31, p=724) | 1.01 (0.35–2.85, p=0.992) |
| Model 2 | ||||
| African | African American | White | Other | |
| N Studies | 5 | 7 | 8 | 6 |
| N | 1321 | 782 | 903 | 182 |
| AUDIT-C score* | ||||
| 6 vs 4 | 2.07 (1.49–2.89, p<0.001) | 1.28 (0.81–2.03, p=0.285) | 1.77 (0.78–4.00, p=0.169) | 2.01 (1.02–3.95, p=0.044) |
| 10 vs 4 | 5.53 (2.43–12.60, p<0.0001) | 1.18 (0.68–2.05, p=0.551) | 4.16 (1.26–13.72, p=0.019) | 2.61 (0.99–6.88, p=0.052) |
| Sex: Female vs Male | 1.13 (0.64–1.97, p=0.679) | 0.63 (0.43–0.92, p=0.018) | 1.44 (0.90–2.30, p=0.122) | 1.17 (0.43–3.21, p=0.754) |
| Age* | ||||
| 30 vs 20 | 3.11 (1.98–4.91, p<0.001) | 0.72 (0.26–2.00, p=0.525) | 1.18 (0.80–1.76, p=0.404) | 1.29 (0.50–3.37, p=0.597) |
| 40 vs 20 | 5.85 (2.88–11.88, p<0.001) | 0.58 (0.11–3.02, p=0.518) | 1.22 (0.61–2.46, p=0.570) | 1.70 (0.39–7.41, p=0.476) |
| 50 vs 20 | 6.64 (2.89–15.26, p<0.001) | 0.53 (0.08–3.42, p=0.502) | 1.11 (0.44–2.79, p=0.830) | 2.28 (0.47–11.19, p=0.308) |
| 60 vs 20 | 4.54 (1.68–12.29, p=0.003) | 0.53 (0.10–2.93, p=0.472) | 0.87 (0.29–2.63, p=0.810) | 3.11 (0.70–13.76, p=0.134) |
| BMI (per 5 kg/m2) | 1.03 (0.74–1.45, p=0.847) | 0.69 (0.63–0.76, p<0.001) | 0.73 (0.63–0.83, p<0.001) | 0.68 (0.48–0.95, p=0.025) |
| Hemoglobin (per 5 g/dl) | 2.72 (1.33–5.57, p=0.006) | 2.25 (1.43–3.52, p<0.001) | 1.84 (1.28–2.65, p=0.001) | 2.13 (0.61–7.38, p=0.234) |
| HIV+ (vs HIV-) | 0.67 (0.47–0.96, p=0.029) | 0.81 (0.63–1.04, p=0.093) | 0.54 (0.28–1.03, p=0.063) | 0.18 (0.07–0.45, p<0.001) |
| Model 3 | ||||
| African | African American | White | Other | |
| N Studies | 3 | 5 | 6 | 4 |
| N | 7045 | 758 | 780 | 124 |
| AUDIT-C score* | ||||
| 6 vs 4 | 1.83 (0.91–3.65, p=0.089) | 1.23 (0.77–1.98, p=0.285) | 1.54 (0.65–3.63, p=0.324) | 1.38 (0.62–3.05, p=0.426) |
| 10 vs 4 | 9.36 (4.48–19.52, p<0.001) | 1.12 (0.64–1.94, p=0.701) | 3.40 (0.92–12.61, p=0.065) | 1.42 (0.47–4.33, p=0.535) |
| Sex: Female vs Male | 1.68 (0.53–5.28, p=0.374) | 0.68 (0.46–0.99, p=0.045) | 1.49 (0.82–2.71, p=0.181) | 1.02 (0.30–3.47, p=0.980) |
| Age* | ||||
| 30 vs 20 | 1.66 (0.75–3.66, p=0.211) | 0.60 (0.18–1.97, p=0.396) | 1.02 (0.60–1.74, p=0.924) | 2.09 (0.44–9.97, p=0.387) |
| 40 vs 20 | 2.19 (0.49–9.75, p=0.304) | 0.41 (0.06–2.84, p=0.369) | 0.98 (0.37–2.65, p=0.979) | 3.99 (0.32–49.15, p=0.280) |
| 50 vs 20 | 2.30 (0.28–18.96, p=0.438) | 0.34 (0.04–2.98, p=0.328) | 0.89 (0.22–3.53, p=0.867) | 7.01 (0.39–125.67, p=0.186) |
| 60 vs 20 | 1.93 (0.14–27.03, p=0.627) | 0.32 (0.04–2.29, p=0.256) | 0.75 (0.13–4.19, p=0.744) | 11.30 (0.67–189.36, p=0.092) |
| BMI (per 5 kg/m2) | 0.99 (0.54–1.82, p=0.987) | 0.70 (0.64–0.77, p<0.001) | 0.73 (0.63–0.85, p<0.001) | 0.56 (0.37–0.86, p=0.009) |
| Hemoglobin (per 5 g/dl) | 3.26 (0.58–18.25, p=0.178) | 2.31 (1.41–3.78, p=0.001) | 2.27 (1.49–3.47, p<0.001) | 2.24 (0.54–9.36, p=0.267) |
| HIV+ (vs HIV-) | --- | 0.77 (0.57–1.03, p=0.074) | 0.75 (0.37–1.50, p=0.414) | 0.21 (0.05–0.85, p=0.028) |
| FIB-4 score | 1.00 | 1.00 | 1.00 | 1.00 |
| 1.45–3.25 vs <1.45 | 1.67 (0.69–4.06, p=0.246) (merged groups) | 1.65 (1.34–2.03, p<0.001) | 1.19 (0.81–1.75, p=0.382) | 0.26 (0.09–0.81, p=0.020) |
| >3.25 vs <1.45 | 2.01 (1.14–3.54, p=0.014) | 2.13 (1.34–3.37, p<0.001) | 0.59 (0.15–2.39, p=0.458) | |
Fitted values from quadratic variable
Discussion
We leveraged over 4000 observations from 21 studies, spanning 4 continents and including wide representation of men and women, several racial/ethnic groups, and persons with and without HIV, to conduct the largest analyses to date of the demographic and biological factors which impact PEth sensitivity among persons reporting unhealthy alcohol use. These analyses are vital to interpreting PEth results in clinical practice and research. Eighty-two percent (82%) of observations in which unhealthy alcohol use was reported were PEth positive. In overall analyses adjusted for self-reported level of alcohol use, we did not observe associations of gender, age, race/ethnicity and method of blood collection with PEth sensitivity. When we examined biological variables, we found that higher hemoglobin and indeterminate and advanced fibrosis had significantly higher odds of PEth sensitivity, while higher BMI and living with HIV had lower odds of PEth sensitivity. We also found increased odds of PEth sensitivity among Africans and African Americans compared to whites in the analyses that included biologic variables. As expected, PEth sensitivity increased with level of self-reported alcohol use. Our results were robust in sensitivity analyses.
We expected that women might have higher PEth sensitivity compared to men because women have higher peak blood alcohol levels, due to greater body fat and decreased water volume compared to men of the same size (Cederbaum, 2012). However, we did not see a difference in PEth levels by sex, which was consistent with other studies that found no sex differences in PEth sensitivity (Wurst et al., 2010, Helander et al., 2019a, Hahn et al., 2012, Hill-Kapturczak et al., 2018). We did not expect differences in PEth sensitivity by race/ethnicity, and did not find any difference by race/ethnicity in Model 1, however the odds of PEth sensitivity were increased for Africans and African Americans compared to whites in Model 2 and Model 3, which included subsets of the data with biologic measures. These associations may have been caused by residual confounding if the level of alcohol consumption was differentially under-reported by race/ethnicity. We have observed high social desirability and under-report of alcohol use by Ugandans living with HIV in prior studies (Adong et al., 2019, Bajunirwe et al., 2014, Muyindike et al., 2017) and under-report has also been reported for racial and ethnic minorities compared to whites in the United States (Johnson and Bowman, 2003, White et al., 2014).
We hypothesized that PEth might be increased for older persons, due to lower body water, slower alcohol metabolism, and higher prevalence of liver disease than younger persons (Meier and Seitz, 2008). However, we found no association between age and PEth sensitivity overall, consistent with a recent examination of this issue (Cherrier et al., 2020). In our exploratory stratified analyses, we observed higher odds of PEth sensitivity in the older compared to younger ages among Africans, even after adjusting for BMI, thus this deserves more examination.
We examined several biologic variables that have been considered as possible factors in PEth sensitivity. We examined BMI, because ethanol concentration in blood per standard drink is inversely proportional to body weight (Cederbaum, 2012). We found that the odds of PEth sensitivity were lower for those with higher BMI, consistent with two prior studies (Wang et al., 2017, Hahn et al., 2012). In addition, since PEth is formed on the surface of red blood cells, it has been suggested that red blood cell depletion may reduce PEth (Nguyen and Seth, 2018), thus we examined hemoglobin levels. We found increased odds of PEth sensitivity with higher levels of hemoglobin. We also found an association of HIV status and PEth sensitivity. While there have been no published studies of this issue, there is a small and mixed literature on the impact of HIV on alcohol metabolism. One study suggested slower alcohol elimination among persons with HIV (Mcginnis et al., 2016), while another reported lower blood alcohol levels among persons with HIV compared to those without (Shuper et al., 2018). Our results of lower odds of PEth sensitivity among persons with HIV compared to those without HIV are consistent with the latter. Possible mechanisms to explain this might include decreased alcohol absorption in the presence of antiretroviral medications. Further research is needed to explore this finding. Lastly, liver damage slows alcohol elimination (Cederbaum, 2012), and we found that higher fibrosis scores were associated with increased odds of PEth sensitivity, consistent with a recent study (Blomdahl et al., 2020). However, fibrosis is frequently the result of high levels of alcohol consumption, so this finding may instead or in part reflect residual confounding by under-reported alcohol use. We had also hypothesized that PEth sensitivity may be impacted by sample preparation, however we found no differences blood spots prepared from venous blood draws compared to finger-pricks, consistent with prior literature (Kummer et al., 2016a, Beck et al., 2018, Piano et al., 2015).
Our exploratory analyses of interactions showed reduced odds of PEth sensitivity among African Americans for women compared to men. This finding is consistent with a study of women with HIV, predominantly African American (83%), who reported high levels of alcohol use, among whom only 47% tested PEth positive (Wang et al., 2017). This finding deserves further examination, including whether differences in body fat distribution and hemoglobin among African American women compared to African American men explain these results.
The overall clinical significance of these findings are that there are some biologic factors that decrease PEth sensitivity. Thus for some groups, caution should be used in interpreting negative PEth findings. However, the lowest predicted sensitivity was 75%, suggesting that PEth is very sensitive overall, but that sensitivity is reduced for persons with some characteristics (e.g. anemia or high BMI).
Strengths and limitations
The strength of this study is the large sample size, which allowed for analyses of variables not previously systematically examined, including several biologic variables. Another strength is the restriction to those reporting unhealthy alcohol consumption or more severe alcohol use, thereby increasing the likelihood of valid self-report. A limitation is that some studies targeted specialized populations, such as young persons who inject drugs, TB patients, entertainment workers and their clients, and persons with HIV, limiting generalizability, and not all studies collected data on all the variables of interest. However, our findings were consistent across sensitivity analyses. We acknowledge that the race/ethnicity categories included represent social constructs rather than genetic ancestry (Mersha and Abebe, 2015). It is also a limitation that we did not have enough participants in Asian, Latinx/Hispanic, and Native American populations to be able to examine these groups separately. In addition, while we grouped participants recruited in Africa as Africans, immigrants participating in studies in the United States may have been grouped with African Americans. We are also likely underpowered to detect important differences by age. We could not examine the method of sample collection in models that adjusted for the other biologic variables because as of the studies that measured these variables had conducted the blood collection via venous blood draw.
There are limitations to our use of the AUDIT-C to control for the level of alcohol consumption. Systematic reporting bias could lead to spurious conclusions due to residual confounding. We attempted to limit mis-reporting by limiting the analyses to those with positive AUDIT-C scores, and limiting the inclusion criteria to studies for which mis-report was unlikely; we found no substantial differences in sensitivity analyses with even higher cutoffs (AUDIT-C ≥6). However, differences in self-report by certain subgroups, such as those experiencing social desirability bias, could have caused spurious associations. We were reassured that the strongest and most consistent associations were observed with variables which had biologic plausibility to be associated with PEth sensitivity (e.g. the associations of BMI and hemoglobin with PEth sensitivity). Lastly, the self-reported alcohol use referred to time periods ranging from one month to one year, or no time period was specified, while PEth detects alcohol use in the prior 2–4 weeks. Thus, we likely under-estimated PEth sensitivity for detecting recent unhealthy alcohol use. To maximize the sample size, we decided to include all observations without regard to the self-report period, and our sensitivity analyses that limited the data to those with known prior month alcohol use showed results that were consistent with those obtained using the larger sample.
A potential concern is that we did not include studies that used a higher cutoff, such as 20 ng/mL for PEth detection. Among the PEth positive observations in this study, 9% were between 8 and 20 ng/mL, suggesting that detection of unhealthy but not severe drinking may be missed using a cutoff of 20 ng/mL. The use of one laboratory for PEth testing for the majority of the studies may limit the generalizability of our results. A recent study showed similar sensitivity rates and high correlations between testing conducted at an academic laboratory compared to at USDTL, but higher PEth values at the academic laboratory (Javors et al., 2019). We focused on the 16:0/18:1 PEth homologue, although others have differing formation and elimination patterns (Lopez-Cruzan et al., 2018, Hill-Kapturczak et al., 2018).
Conclusions
These findings provide important information for clinicians and researchers using PEth. We found associations of several biological characteristics with PEth sensitivity, with high overall PEth sensitivity among those engaging in unhealthy alcohol use. Clinicians should be aware of these factors, especially when considering negative PEth results, and researchers should consider adjusting analyses for these characteristics where possible.
Acknowledgments
Sources of funding for collecting the data: NIH U01 AA026223 (Hahn), NIH U01 AA020776 (Hahn), NIH R01 AA018631 (Hahn), NIH U01 AA026226 (Chamie), Bill and Melinda Gates Foundation OPP1056051 (Haberer), NIH R01 AI119037 (Jacobson), Pilot award of NIH P30 AI027763 (UCSF, PI Gandhi), NIH R01 DA016017 (Page), NIH R01 AA018096 (DiClemente), NIH U01 AA020784 (Saitz), NIH U01 AA020780 (So-Armah), NIH R01 DA016065 (Sulkowski), NIH R01 AA022222 (Marcus), NIH K01 AA021671 (Woolf-King), NIH U01 AA020797 (Cook), NIH P60 AA009803 (Molina), NIH R21 AA024535 (Piano/Phillips), NIH R01 AA017911 (Stewart), NIH K23 AA024503 (Afshar), NIH U01 AA020790 (Justice), NIH U01 AA020795 (Justice), NIH U01 AA022001 (Justice), NIH U10 AA013566 (Justice)
Source of funding for these analyses: NIH K24 AA022586 (Hahn)
Contributor Information
Judith A. Hahn, Department of Medicine, and Department of Epidemiology & Biostatistics, University of California, San Francisco, San Francisco CA, USA Mailing address: 550 16th Street, 3rd Floor, San Francisco, 94143
Pamela M. Murnane, Department of Epidemiology & Biostatistics, University of California, San Francisco, San Francisco CA, USA.
Eric Vittinghoff, Department of Epidemiology & Biostatistics, University of California, San Francisco, San Francisco CA, USA.
Winnie R. Muyindike, Department of Internal Medicine, Mbarara University of Science and Technology, Mbarara..
Nneka I. Emenyonu, Department of Medicine, University of California, San Francisco, San Francisco CA, USA.
Robin Fatch, Department of Medicine, University of California, San Francisco, San Francisco CA, USA..
Gabriel Chamie, Department of Medicine, University of California, San Francisco, San Francisco CA, USA.
Jessica E. Haberer, Massachusetts General Hospital, Center for Global Health, Boston, MA, USA.
Joel M. Francis, National Institute for Medical Research, Mwanza Centre, Mwanza, Tanzania, and Department of Infectious Diseases Epidemiology, London School of Hygiene and Tropical Medicine, and Department of Family Medicine and Primary Care, School of Clinical Medicine, University of the Witwatersrand, Johannesburg, South Africa..
Saidi Kapiga, London School of Hygiene & Tropical Medicine, London, UK.
Karen Jacobson, Boston University School of Medicine, Boston, MA, USA.
Bronwyn Myers, Alcohol, Tobacco and Other Drug Research Unit, South African Medical Research Council, Tygerberg, South Africa, and Department of Psychiatry and Mental Health, University of Cape Town, Cape Town, South Africa.
Marie Claude Couture, University of San Francisco, San Francisco, CA, USA.
Ralph J. DiClemente, Department of Social and Behavioral Sciences, NYU School of Global Public Health, New York, NY, USA.
Jennifer L. Brown, Departments of Psychology and Psychiatry & Behavioral Neuroscience; Center for Addiction Research, University of Cincinnati, Cincinnati, OH, USA.
Kaku So-Armah, Department of Medicine, Boston University School of Medicine, Boston, MA, USA.
Mark Sulkowski, Department of Medicine, Johns Hopkins School of Medicine, Baltimore MD, USA.
Gregory M. Marcus, Department of Medicine, University of California, San Francisco, CA, USA.
Sarah Woolf-King, Syracuse University, Department of Psychology, Syracuse, NY, USA.
Robert L. Cook, Department of Epidemiology, University of Florida, Gainesville, FL.
Veronica L. Richards, Department of Epidemiology, University of Florida, Gainesville, FL.
Patricia Molina, Comprehensive Alcohol-HIV/AIDS Research Center and Department of Physiology & Comprehensive Alcohol Research Center, Louisiana State University Health Sciences Center, New Orleans, LA, USA.
Tekeda Ferguson, Comprehensive Alcohol-HIV/AIDS Research Center and Department of Physiology & Comprehensive Alcohol Research Center, and School of Public Health, Louisiana State University Health Sciences Center, New Orleans, LA, USA.
David Welsh, Comprehensive Alcohol-HIV/AIDS Research Center and Department of Physiology & Comprehensive Alcohol Research Center and School of Medicine, Louisiana State University Health Sciences Center, New Orleans, LA, USA.
Mariann R. Piano, Center for Research Development and Scholarship, Vanderbilt University, Nashville, TN. USA.
Shane A. Phillips, University of Illinois at Chicago, Chicago, IL, USA.
Scott Stewart, Department of Family Medicine, Division of Addiction Medicine, University at Buffalo, Buffalo, NY, USA.
Majid Afshar, Department of Medicine, School of Medicine and Public Health, University of Wisconsin – Madison, Madison, WI, USA.
Kimberly Page, Department of Internal Medicine, University of New Mexico; Albuquerque, NM, USA.
Kathleen McGinnis, West Haven VA Healthcare System, United States Department of Veterans Affairs, West Haven, CT, USA.
David A. Fiellin, Yale School of Medicine and Yale School of Public Health, New Haven, CT, USA.
Amy C. Justice, Yale School of Medicine and Yale School of Public Health, New Haven, CT, and West Haven VA Healthcare System, United States Department of Veterans Affairs, West Haven, CT, USA.
Kendall Bryant, National Institutes of Health, National Institute of Alcohol Abuse and Alcoholism, Bethesda, MD, USA.
Richard Saitz, Department of Community Health Sciences, Boston University School of Public Health, Section of General Internal Medicine, Boston University School of Medicine and Boston Medical Center, and Grayken Center on Addiction, Boston Medical Center, Boston, MA, USA.
References
- 2018. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet. [DOI] [PMC free article] [PubMed]
- 2019. Stata Statistical Software. StataCorp. . College Station, TX. [Google Scholar]
- Adong J, Fatch R, Emenyonu NI, Cheng DM, Muyindike WR, Ngabirano C, Kekibiina A, Woolf-King SE, Samet JH & Hahn JA 2019. Social Desirability Bias Impacts Self-Reported Alcohol Use Among Persons With HIV in Uganda. Alcohol Clin Exp Res. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afshar M, Baker K, Corral J, Ross E, Lowery E, Gonzalez R, Burnham EL, Callcut RA, Kornblith LZ, Hendrickson C, Kovacs EJ & Joyce C. 2021. Internal and External Validation of an Alcohol Biomarker for Screening in Trauma. Annals of Surgery. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aradottir S, Asanovska G, Gjerss S, Hansson P. & Alling C. 2006. Phosphatidylethanol (PEth) concentrations in blood are correlated to reported alcohol intake in alcohol-dependent patients. Alcohol Alcohol, 41, 431–7. [DOI] [PubMed] [Google Scholar]
- Babor T, Higgins-Biddle J, Saunders J. & Monteiro MG 2001. The Alcohol Use Disorders Identification Test: Guidelines for use in primary care. World Health Organization, Department of Mental Health and Substance Dependence. [Google Scholar]
- Bajunirwe F, Haberer JE, Boum Y 2nd, Hunt P, Mocello R, Martin JN, Bangsberg DR & Hahn JA 2014. Comparison of self-reported alcohol consumption to phosphatidylethanol measurement among HIV-infected patients initiating antiretroviral treatment in southwestern Uganda. PLoS One, 9, e113152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck O, Kenan Moden N, Seferaj S, Lenk G. & Helander A. 2018. Study of measurement of the alcohol biomarker phosphatidylethanol (PEth) in dried blood spot (DBS) samples and application of a volumetric DBS device. Clin Chim Acta, 479, 38–42. [DOI] [PubMed] [Google Scholar]
- Blomdahl J, Nasr P, Ekstedt M. & Kechagias S. 2020. Moderate alcohol consumption is associated with advanced fibrosis in non-alcoholic fatty liver disease and shows a synergistic effect with type 2 diabetes mellitus. Metabolism, 115, 154439. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Debenedetti AF, Volk RJ, Williams EC, Frank D. & Kivlahan DR 2007. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res, 31, 1208–17. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, Mcdonell MB, Fihn SD & Bradley KA 1998. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med, 158, 1789–95. [DOI] [PubMed] [Google Scholar]
- Cederbaum AI 2012. Alcohol metabolism. Clin Liver Dis, 16, 667–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherrier MM, Shireman LM, Wicklander K, Yeung W, Kooner P, Saxon AJ, Simpson T, Terman G. & Shen D. 2020. Relationship of Phosphatidylethanol Biomarker to Self-Reported Alcohol Drinking Patterns in Older and Middle-Age Adults. Alcohol Clin Exp Res, 44, 2449–2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couture MC, Page K, Sansothy N, Stein E, Vun MC & Hahn JA 2016. High prevalence of unhealthy alcohol use and comparison of self-reported alcohol consumption to phosphatidylethanol among women engaged in sex work and their male clients in Cambodia. Drug Alcohol Depend, 165, 29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CG, Thake J. & Vilhena N. 2010. Social desirability biases in self-reported alcohol consumption and harms. Addict Behav, 35, 302–11. [DOI] [PubMed] [Google Scholar]
- De Kesel PM, Sadones N, Capiau S, Lambert WE & Stove CP 2013. Hemato-critical issues in quantitative analysis of dried blood spots: challenges and solutions. Bioanalysis, 5, 2023–41. [DOI] [PubMed] [Google Scholar]
- Debray TP, Moons KG, Abo-Zaid GM, Koffijberg H. & Riley RD 2013. Individual participant data meta-analysis for a binary outcome: one-stage or two-stage? PLoS One, 8, e60650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debray TP, Moons KG, Van Valkenhoef G, Efthimiou O, Hummel N, Groenwold RH & Reitsma JB 2015. Get real in individual participant data (IPD) meta-analysis: a review of the methodology. Res Synth Methods, 6, 293–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine EG, Waters ME, Putnam M, Surprise C, O’malley K, Richambault C, Fishman RL, Knapp CM, Patterson EH, Sarid-Segal O, Streeter C, Colanari L. & Ciraulo DA 2013. Concealment and fabrication by experienced research subjects. Clin Trials, 10, 935–48. [DOI] [PubMed] [Google Scholar]
- Edelman EJ, Maisto SA, Hansen NB, Cutter CJ, Dziura J, Deng Y, Fiellin LE, O’connor PG, Bedimo R, Gibert CL, Marconi VC, Rimland D, Rodriguez-Barradas MC, Simberkoff MS, Tate JP, Justice AC, Bryant KJ & Fiellin DA 2019. Integrated stepped alcohol treatment for patients with HIV and alcohol use disorder: a randomised controlled trial. Lancet HIV. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyawo O, Mcginnis KA, Justice AC, Fiellin DA, Hahn JA, Williams EC, Gordon AJ, Marshall BDL, Kraemer KL, Crystal S, Gaither JR, Edelman EJ, Bryant KJ & Tate JP 2018. Alcohol and Mortality: Combining Self-Reported (AUDIT-C) and Biomarker Detected (PEth) Alcohol Measures Among HIV Infected and Uninfected. J Acquir Immune Defic Syndr, 77, 135–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson TF, Theall KP, Brashear M, Maffei V, Beauchamp A, Siggins RW, Simon L, Mercante D, Nelson S, Welsh DA & Molina PE 2020. Comprehensive Assessment of Alcohol Consumption in People Living with HIV (PLWH): The New Orleans Alcohol Use in HIV Study. Alcohol Clin Exp Res. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis JM, Weiss HA, Helander A, Kapiga SH, Changalucha J. & Grosskurth H. 2015. Comparison of self-reported alcohol use with the alcohol biomarker phosphatidylethanol among young people in northern Tanzania. Drug Alcohol Depend, 156, 289–296. [DOI] [PubMed] [Google Scholar]
- Gerbase FE, Tegner M, Krutzmann ME, Muller VV, Alff JA, Da Silva VB, Sagrilo OP, Linden R. & Antunes MV 2020. Blood phosphatidyl ethanol levels as a tool to detect alcohol misuse in trauma patients. Clin Toxicol (Phila), 1–8. [DOI] [PubMed] [Google Scholar]
- Ghosh S, Jain R, Jhanjee S, Rao R. & Mishra AK 2019. Alcohol Biomarkers and their Relevance in Detection of Alcohol Consumption in Clinical Settings. Int Arch Subst Abuse Rehabil, 1. [Google Scholar]
- Gnann H, Thierauf A, Hagenbuch F, Rohr B. & Weinmann W. 2014. Time dependence of elimination of different PEth homologues in alcoholics in comparison with social drinkers. Alcohol Clin Exp Res, 38, 322–6. [DOI] [PubMed] [Google Scholar]
- Hahn JA, Anton RF & Javors MA 2016a. The Formation, Elimination, Interpretation, and Future Research Needs of Phosphatidylethanol for Research Studies and Clinical Practice. Alcohol Clin Exp Res, 40, 2292–2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn JA, Cheng DM, Emenyonu NI, Lloyd-Travaglini C, Fatch R, Shade SB, Ngabirano C, Adong J, Bryant K, Muyindike WR & Samet JH 2018. Alcohol Use and HIV Disease Progression in an Antiretroviral Naive Cohort. J Acquir Immune Defic Syndr, 77, 492–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn JA, Dobkin LM, Mayanja B, Emenyonu NI, Kigozi IM, Shiboski S, Bangsberg DR, Gnann H, Weinmann W. & Wurst FM 2012. Phosphatidylethanol (PEth) as a biomarker of alcohol consumption in HIV-positive patients in sub-Saharan Africa. Alcohol Clin Exp Res, 36, 854–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn JA, Emenyonu NI, Fatch R, Muyindike WR, Kekiibina A, Carrico AW, Woolf-King S. & Shiboski S. 2016b. Declining and rebounding unhealthy alcohol consumption during the first year of HIV care in rural Uganda, using phosphatidylethanol to augment self-report. Addiction, 111, 272–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann S, Aradottir S, Graf M, Wiesbeck G, Lesch O, Ramskogler K, Wolfersdorf M, Alling C. & Wurst FM 2007. Phosphatidylethanol as a sensitive and specific biomarker: comparison with gamma-glutamyl transpeptidase, mean corpuscular volume and carbohydrate-deficient transferrin. Addict Biol, 12, 81–4. [DOI] [PubMed] [Google Scholar]
- Helander A, Bottcher M, Dahmen N. & Beck O. 2019a. Elimination Characteristics of the Alcohol Biomarker Phosphatidylethanol (PEth) in Blood during Alcohol Detoxification. Alcohol Alcohol, 54, 251–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helander A, Hermansson U. & Beck O. 2019b. Dose-Response Characteristics of the Alcohol Biomarker Phosphatidylethanol (PEth)-A Study of Outpatients in Treatment for Reduced Drinking. Alcohol Alcohol. [DOI] [PubMed] [Google Scholar]
- Hill-Kapturczak N, Dougherty DM, Roache JD, Karns-Wright TE & Javors MA 2018. Differences in the Synthesis and Elimination of Phosphatidylethanol 16:0/18:1 and 16:0/18:2 After Acute Doses of Alcohol. Alcohol Clin Exp Res, 42, 851–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irvin R, Chander G, Ward KM, Manogue S, Falade-Nwulia O, Moon J, Sutcliffe CG, Brinkley S, Haselhuhn T, Katz S, Herne K, Arteaga L, Thomas DL, Mehta SH & Sulkowski MS 2020. Unreported alcohol use was common but did not impact hepatitis C cure in HIV-infected persons who use drugs. J Viral Hepat, 27, 476–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain J, Evans JL, Briceno A, Page K. & Hahn JA 2014. Comparison of phosphatidylethanol results to self-reported alcohol consumption among young injection drug users. Alcohol Alcohol, 49, 520–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javors M, Hill-Kapturczak N, Lopez-Cruzan M, Roache J, Wright T. & Dm D. 2019. Comparison of phosphatidylethanol 16:0/18:1 concentrations of identical quality control samples tested at three clinical bioanalytical laboratories. Research Society on Alcoholism. Minneapolis, MN. [Google Scholar]
- Javors MA, Hill-Kapturczak N, Roache JD, Karns-Wright TE & Dougherty DM 2016. Characterization of the Pharmacokinetics of Phosphatidylethanol 16:0/18:1 and 16:0/18:2 in Human Whole Blood After Alcohol Consumption in a Clinical Laboratory Study. Alcohol Clin Exp Res, 40, 1228–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson TP & Bowman PJ 2003. Cross-cultural sources of measurement error in substance use surveys. Subst Use Misuse, 38, 1447–90. [DOI] [PubMed] [Google Scholar]
- Jones J, Jones M, Plate C. & Lewis D. 2011. The detection of 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphoethanol in human dried blood spots. Analytical Methods, 3, 1101. [Google Scholar]
- Kechagias S, Dernroth DN, Blomgren A, Hansson T, Isaksson A, Walther L, Kronstrand R, Kågedal B. & Nystrom FH 2015. Phosphatidylethanol Compared with Other Blood Tests as a Biomarker of Moderate Alcohol Consumption in Healthy Volunteers: A Prospective Randomized Study. Alcohol Alcohol, 50, 399–406. [DOI] [PubMed] [Google Scholar]
- Kummer N, Ingels AS, Wille SM, Hanak C, Verbanck P, Lambert WE, Samyn N. & Stove CP 2016a. Quantification of phosphatidylethanol 16:0/18:1, 18:1/18:1, and 16:0/16:0 in venous blood and venous and capillary dried blood spots from patients in alcohol withdrawal and control volunteers. Anal Bioanal Chem, 408, 825–38. [DOI] [PubMed] [Google Scholar]
- Kummer N, Lambert WE, Samyn N. & Stove CP 2016b. Alternative sampling strategies for the assessment of alcohol intake of living persons. Clin Biochem, 49, 1078–91. [DOI] [PubMed] [Google Scholar]
- Littlefield AK, Brown JL, Diclemente RJ, Safonova P, Sales JM, Rose ES, Belyakov N. & Rassokhin VV 2017. Phosphatidylethanol (PEth) as a Biomarker of Alcohol Consumption in HIV-Infected Young Russian Women: Comparison to Self-Report Assessments of Alcohol Use. AIDS Behav, 21, 1938–1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Cruzan M, Roache JD, Hill-Kapturczak N, Karns-Wright TE, Dougherty DM, Sanchez JJ, Koek W. & Javors MA 2018. Pharmacokinetics of Phosphatidylethanol 16:0/20:4 in Human Blood After Alcohol Intake. Alcohol Clin Exp Res, 42, 2094–2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Fatch R, Orrell C, Amanyire G, Haberer JE & Hahn JA 2019. Biomarker-Measured Unhealthy Alcohol Use in Relation to CD4 Count Among Individuals Starting ART in Sub-Saharan Africa. AIDS Behav, 23, 1656–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mccaul ME & Wand GS 2018. Detecting Deception in Our Research Participants: Are Your Participants Who You Think They Are? Alcohol Clin Exp Res, 42, 230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcginnis KA, Fiellin DA, Tate JP, Cook RL, Braithwaite RS, Bryant KJ, Edelman EJ, Gordon AJ, Kraemer KL, Maisto SA & Justice AC 2016. Number of Drinks to “Feel a Buzz” by HIV Status and Viral Load in Men. AIDS Behav, 20, 504–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier P. & Seitz HK 2008. Age, alcohol metabolism and liver disease. Curr Opin Clin Nutr Metab Care, 11, 21–6. [DOI] [PubMed] [Google Scholar]
- Mersha TB & Abebe T. 2015. Self-reported race/ethnicity in the age of genomic research: its potential impact on understanding health disparities. Hum Genomics, 9, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller PM, Ornstein SM, Nietert PJ & Anton RF 2004. Self-report and biomarker alcohol screening by primary care physicians: the need to translate research into guidelines and practice. Alcohol Alcohol, 39, 325–8. [DOI] [PubMed] [Google Scholar]
- Miller PM, Thomas SE & Mallin R. 2006. Patient attitudes towards self-report and biomarker alcohol screening by primary care physicians. Alcohol Alcohol, 41, 306–10. [DOI] [PubMed] [Google Scholar]
- Muyindike WR, Lloyd-Travaglini C, Fatch R, Emenyonu NI, Adong J, Ngabirano C, Cheng DM, Winter MR, Samet JH & Hahn JA 2017. Phosphatidylethanol confirmed alcohol use among ART-naive HIV-infected persons who denied consumption in rural Uganda. AIDS Care, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers B, Bouton TC, Ragan EJ, White LF, Mcilleron H, Theron D, Parry CDH, Horsburgh CR, Warren RM & Jacobson KR 2018. Impact of alcohol consumption on tuberculosis treatment outcomes: a prospective longitudinal cohort study protocol. BMC Infect Dis, 18, 488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen VL & Seth D. 2018. Letter to the Editor Regarding Afshar et al. (2017): Cut-Point Levels of Phosphatidylethanol to Identify Alcohol Misuse in a Mixed Cohort Including Critically Ill Patients. Alcohol Clin Exp Res, 42, 2061–2063. [DOI] [PubMed] [Google Scholar]
- World Health Organization 2011. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. V [Online]. Geneva. Available: https://www.who.int/vmnis/indicators/haemoglobin.pdf [Accessed November 24 2020]. [Google Scholar]
- Papas RK, Gakinya BN, Mwaniki MM, Keter AK, Lee H, Loxley MP, Klein DA, Sidle JE, Martino S, Baliddawa JB, Schlaudt KL & Maisto SA 2016. Associations between the phosphatidylethanol (PEth) biomarker and self-reproted alcohol use in a sample of HIV-infected outpatient drinkers in western Kenya. Alcoholism: Clinical & Experimental Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piano MR, Tiwari S, Nevoral L. & Phillips SA 2015. Phosphatidylethanol Levels Are Elevated and Correlate Strongly with AUDIT Scores in Young Adult Binge Drinkers. Alcohol Alcohol, 50, 519–25. [DOI] [PubMed] [Google Scholar]
- Röhricht M, Paschke K, Sack PM, Weinmann W, Thomasius R. & Wurst FM 2020. Phosphatidylethanol Reliably and Objectively Quantifies Alcohol Consumption in Adolescents and Young Adults. Alcohol Clin Exp Res, 44, 2177–2186. [DOI] [PubMed] [Google Scholar]
- Rubinsky AD, Dawson DA, Williams EC, Kivlahan DR & Bradley KA 2013. AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcohol Clin Exp Res, 37, 1380–90. [DOI] [PubMed] [Google Scholar]
- Saitz R, Mesic A, Ventura AS, Winter MR, Heeren TC, Sullivan MM, Walley AY, Patts GJ, Meli SM, Holick MF, Kim TW, Bryant KJ & Samet JH 2018. Alcohol Consumption and Bone Mineral Density in People with HIV and Substance Use Disorder: A Prospective Cohort Study. Alcohol Clin Exp Res. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrock A, Henzi A, Butikofer P, Konig S. & Weinmann W. 2018. Determination of the formation rate of phosphatidylethanol by phospholipase D (PLD) in blood and test of two selective PLD inhibitors. Alcohol, 73, 1–7. [DOI] [PubMed] [Google Scholar]
- Schrock A, Thierauf-Emberger A, Schurch S. & Weinmann W. 2016. Phosphatidylethanol (PEth) detected in blood for 3 to 12 days after single consumption of alcohol-a drinking study with 16 volunteers. Int J Legal Med. [DOI] [PubMed] [Google Scholar]
- Schröck A, Wurst FM, Thon N. & Weinmann W. 2017. Assessing phosphatidylethanol (PEth) levels reflecting different drinking habits in comparison to the alcohol use disorders identification test - C (AUDIT-C). Drug Alcohol Depend, 178, 80–86. [DOI] [PubMed] [Google Scholar]
- Shuper PA, Joharchi N. & Rehm J. 2018. Lower Blood Alcohol Concentration Among HIV-Positive Versus HIV-Negative Individuals Following Controlled Alcohol Administration. Alcohol Clin Exp Res. [DOI] [PMC free article] [PubMed] [Google Scholar]
- So-Armah KA, Cheng DM, Freiberg MS, Gnatienko N, Patts G, Ma Y, White L, Blokhina E, Lioznov D, Doyle MF, Tracy RP, Chichetto N, Bridden C, Bryant K, Krupitsky E. & Samet JH 2019. Association between alcohol use and inflammatory biomarkers over time among younger adults with HIV-The Russia ARCH Observational Study. PLoS One, 14, e0219710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC & Sobell MB 1992. Timeline Follow-back: A technique for assessing self-reported ethanol consumption. . In: ALLEN J. & LITTEN RZ (eds.) Measuring Alcohol Consumption: Psychosocial and Biological Methods. Totowa, NJ: Humana Press. [Google Scholar]
- Stenton J, Walther L, Hansson T, Andersson A. & Isaksson A. 2019. Inter Individual Variation and Factors Regulating the Formation of Phosphatidylethanol. Alcohol Clin Exp Res, 43, 2322–2331. [DOI] [PubMed] [Google Scholar]
- Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, M SS, Torriani FJ, Dieterich DT, Thomas DL, Messinger D. & Nelson M. 2006. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology, 43, 1317–25. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Koch DG, Willner IR, Anton RF & Reuben A. 2014. Validation of blood phosphatidylethanol as an alcohol consumption biomarker in patients with chronic liver disease. Alcohol Clin Exp Res, 38, 1706–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulwelling W. & Smith K. 2018. The PEth Blood Test in the Security Environment: What it is; Why it is Important; and Interpretative Guidelines. J Forensic Sci, 63, 1634–1640. [DOI] [PubMed] [Google Scholar]
- Vallet-Pichard A, Mallet V, Nalpas B, Verkarre V, Nalpas A, Dhalluin-Venier V, Fontaine H. & Pol S. 2007. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology, 46, 32–6. [DOI] [PubMed] [Google Scholar]
- Varga A, Hansson P, Johnson G. & Alling C. 2000. Normalization rate and cellular localization of phosphatidylethanol in whole blood from chronic alcoholics. Clin Chim Acta, 299, 141–50. [DOI] [PubMed] [Google Scholar]
- Walther L, De Bejczy A, Lof E, Hansson T, Andersson A, Guterstam J, Hammarberg A, Asanovska G, Franck J, Soderpalm B. & Isaksson A. 2015. Phosphatidylethanol is superior to carbohydrate-deficient transferrin and gamma-glutamyltransferase as an alcohol marker and is a reliable estimate of alcohol consumption level. Alcohol Clin Exp Res, 39, 2200–8. [DOI] [PubMed] [Google Scholar]
- Wang Y, Chen X, Hahn JA, Brumback B, Zhou Z, Miguez MJ & Cook RL 2017. Phosphatidylethanol (PEth) in Comparison to Self-Reported Alcohol Consumption among HIV-infected Women in a Randomized Controlled Trial of Naltrexone for Reducing Hazardous Drinking. Alcohol Clin Exp Res. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir CB & Jan A. 2020. BMI Classification Percentile And Cut Off Points. [Online]. Treasure Island: StatPearls Publishing. Available: https://www.ncbi.nlm.nih.gov/books/NBK541070/ [Accessed November 23 2020]. [PubMed] [Google Scholar]
- White D, Rosenberg ES, Cooper HL, Del Rio C, Sanchez TH, Salazar LF & Sullivan PS 2014. Racial differences in the validity of self-reported drug use among men who have sex with men in Atlanta, GA. Drug Alcohol Depend, 138, 146–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurst FM, Thon N, Aradottir S, Hartmann S, Wiesbeck GA, Lesch O, Skala K, Wolfersdorf M, Weinmann W. & Alling C. 2010. Phosphatidylethanol: normalization during detoxification, gender aspects and correlation with other biomarkers and self-reports. Addict Biol, 15, 88–95. [DOI] [PubMed] [Google Scholar]